Abstract
Ammonia has been identified to have a significant role in the long-term damage to dopamine and serotonin terminals produced by methamphetamine (METH), but how ammonia contributes to this damage is unknown. Experiments were conducted to identify whether increases in brain ammonia affect METH-induced increases in glutamate and subsequent excitotoxicity. Increases in striatal glutamate were measured using in vivo microdialysis. To examine the role of ammonia in mediating changes in extracellular glutamate after METH exposure, lactulose was used to decrease plasma and brain ammonia. Lactulose is a non-absorbable disaccharide, which alters the intestinal lumen through multiple mechanisms that lead to the increased peripheral excretion of ammonia. METH caused a significant increase in extracellular glutamate that was prevented by lactulose. Lactulose had no effect on METH-induced hyperthermia. To determine if ammonia contributed to excitotoxicity, the effect of METH and lactulose treatment on calpain-mediated spectrin proteolysis was measured. METH significantly increased calpain-specific spectrin breakdown products, and this increase was prevented with lactulose treatment. To examine if ammonia-induced increases in extracellular glutamate were mediated by excitatory amino-acid transporters, the reverse dialysis of ammonia, the glutamate transporter inhibitor, DL-threo-β-benzyloxyaspartic acid (TBOA), or the combination of the two directly into the striatum of awake, freely moving rats was conducted. TBOA blocked the increases in extracellular glutamate produced by the reverse dialysis of ammonia. These findings demonstrate that ammonia mediates METH-induced increases in extracellular glutamate through an excitatory amino-acid transporter to cause excitotoxicity.
Keywords: methamphetamine, glutamate, excitotoxicity, glutamate transporter, ammonia
INTRODUCTION
Methamphetamine (METH) is an abused psychostimulant that causes persistent damage to dopamine and serotonin terminals in the striatum, prefrontal cortex, and hippocampus (Ricaurte et al, 1980; Seiden et al, 1988; Wagner et al, 1980). The long-term dopamine and serotonin terminal damage is associated with numerous cognitive deficits exhibited by METH users and has more recently been shown to correlate with the potential for relapse of drug use (Clark et al, 2006; Johanson et al, 2006; Rogers et al, 1999; Simon et al, 2002; Volkow et al, 2001; Wang et al, 2012).
Numerous convergent mechanisms have been identified to have a role in the persistent dopamine and serotonin terminal damage produced by METH and include metabolic compromise, oxidative stress, and excitotoxicity (Yamamoto and Raudensky, 2008). Recently, acute liver damage and increases in ammonia have also been implicated (Halpin and Yamamoto, 2012), but how ammonia contributes to this neuronal damage and the mechanisms that mediate the neurotoxic effects of METH remain unknown.
METH has been shown to significantly increase extracellular glutamate within the striatum (Nash and Yamamoto, 1992), a region known to contain calcium-permeable AMPA receptors that are located presynaptically on dopamine and serotonin terminals (Betarbet and Greenamyre, 1999; Hernandez et al, 2003; Keefe et al, 1993; Nash and Yamamoto, 1992). Blockade of METH-induced increases in glutamate, activation of AMPA or NMDA receptors, or NOS-derived peroxynitrite protect against the mitochondrial and neuronal damage produced by the drug and provide evidence for activation of calcium-dependent proteases such as calpain in mediating the long-term damage to dopamine and serotonin terminals elicited by METH (Farfel et al, 1992; Staszewski and Yamamoto, 2006; Tata and Yamamoto, 2007). Calpain is a calcium-activated protease that is activated in the context of excitotoxicity in response to significant increases in intracellular calcium. Calpain causes proteolysis of numerous essential cytoskeletal components including non-erythroid spectrin (Gerencser et al, 2009; Goll et al, 2003; Pike et al, 2001; Saggu et al, 2010; Siman et al, 1989).
Although METH increases corticostriatal glutamate release through a polysynaptic, D1-receptor-mediated disinhibition of corticostriatal projections (Mark et al, 2004), synaptic glutamate is also regulated by amino-acid transporters (EAAT) that are located primarily on astrocytes and transport extracellular glutamate from the synapse into astrocytes. A potential modulator of extracellular glutamate and glutamate uptake by astrocytes is ammonia (Chan et al, 2000; Gorg et al, 2010; Gorg et al, 2007; Norenberg, 1987). This is particularly relevant in the context of the pharmacological actions of METH because ammonia has been identified recently as a novel, peripherally derived mediator of METH neurotoxicity (Halpin and Yamamoto, 2012). Despite this association, the specific mechanism by which ammonia contributes to METH neurotoxicity is unknown, although ammonia at high micromolar to millimolar concentrations caused by hepatotoxicity is known to contribute to global neuronal damage through excitotoxic, oxidative, metabolic, and neuroinflammatory processes (Cauli et al, 2007; Chan et al, 2000; Hawkins et al, 1973; Kosenko et al, 1997; Kosenko et al, 2003).
The objective of the current study is to examine the contribution of peripherally derived ammonia to METH-induced elevations in extracellular glutamate and excitotoxicity in the striatum. It is hypothesized that ammonia increases extracellular striatal glutamate through an alteration in glutamate transporter function, the result of which is calpain-mediated spectrin proteolysis indicative of calcium-dependent excitotoxicity (Siman et al, 1989). To evaluate the role of ammonia, we used the non-absorbable disaccharide lactulose, which is a primary treatment for hepatic encephalopathy and is used to lower elevated plasma ammonia resulting from hepatotoxicity (Al Sibae and McGuire, 2009; Jia and Zhang, 2005; Nicaise et al, 2008). Subsequent to oral administration, lactulose remains in the gut and increases the fecal excretion of ammonia through numerous mechanisms including acidifying the intestinal lumen to trap enterohepatically cycling NH4+, functioning as a laxative to increase intestinal motility and decrease protein absorption, which is the sole dietary source of ammonia, and through increasing ammonia metabolism by intestinal bacteria (Mortensen, 1992; Panesar and Kumari, 2011). To examine a mechanism by which peripheral ammonia contributes to increases in glutamate at the concentrations achieved in the brain during METH exposure, we examined extracellular striatal glutamate in rats treated with lactulose to alter plasma and brain ammonia concentrations. In addition, we also investigated the effects of the local antagonism of EAAT on glutamate during the direct administration of ammonia into the striatum.
MATERIALS AND METHODS
Male Sprague Dawley rats received METH (10 mg/kg, q 2 h × 4, i.p.) or saline (1 ml/kg, q 2 h × 4, i.p.). This dosing paradigm models the concentration and binge paradigm reported in METH-dependent humans and produces long-term depletions of dopamine and serotonin terminals (Cruickshank and Dyer, 2009; McCann et al, 1998; McKetin et al, 2006; Ricaurte et al, 1982; Wagner et al, 1980). Peripheral ammonia excretion was increased using lactulose, as it is a well-known treatment that enhances ammonia excretion and attenuates the increases in plasma ammonia and neurological symptoms of hepatic encephalopathy (Al Sibae and McGuire, 2009; Jia and Zhang, 2005; Nicaise et al, 2008). In lactulose experiments, rats received lactulose (5.3 g/kg) or vehicle via oral gavage every 12 h for 2 days before METH treatment until the day before rats were killed (Halpin and Yamamoto, 2012). This drug treatment is known to fully block the increases in both plasma and brain ammonia concentrations produced by METH. All rats were killed by live decapitation 5 days after the METH or saline treatment.
Subcutaneous temperature transponders were implanted into the rats 2 days before the beginning of each experiment to allow for remote monitoring of temperature and to reduce stress that would otherwise be produced by rectal measures. The transponders used were 2.2 × 14 mm and weighed 120 mg (IPTT-300 transponder, BMDS).
All treatments were carried out in accordance with the National Institute of Health Guide for Care and Use of rats. All treatments are approved by the University of Toledo Institutional Animal Care and Use Committee.
In Vivo Microdialysis
Intracranial probes were constructed using PE 20 tubing (Becton Dickinson), silica tubing (OD of 150 μm, Polymicro Technologies), 26-ga stainless steel hypodermic tubing (Small Parts), hollow fiber microdialysis membrane (4 mm of active membrane, MWCO 13 000, 216 μm, Spectrum Labs), 2-ton waterproof epoxy and tygon microbore tubing. Surgeries were performed the day before drug treatment. Rats were anesthetized using xylazine (5 mg/kg) and ketamine (75 mg/kg) and the probe was stereotaxically lowered into the striatum (AP+1.2, ML+3.0, DV−6.5 mm). One day later and after a 1-h equilibration period, baseline samples were collected every hour for 3 h at a flow rate of 1.5 μl/min. Samples were collected every hour during METH or saline treatment until 2 h after the last drug injection. Artificial cerebrospinal fluid (aCSF), ammonia (200 μM), the EAAT antagonist DL-threo-β-benzyloxyaspartic acid (TBOA; 500 μM), or the combination of ammonia and TBOA were reverse dialyzed into the striatum and extracellular glutamate was measured. The concentration of TBOA administered via microdialysis is based on that which was demonstrated to block glutamate transporter-mediated increases in glutamate without significantly affecting baseline glutamate levels (Haskew-Layton et al, 2008). The concentration of ammonia for reverse dialysis was that which was observed in the striatum during systemic METH treatment (Halpin and Yamamoto, 2012). TBOA treatment began 1 h before ammonia exposure. Samples were collected every 30 min and for 4 h after ammonia or aCSF. Probe placement was verified histologically.
HPLC Analysis of Glutamate
Dialysate samples (20 μl) were injected onto a C18 column (150 × 2 mm, 3 μm particle diameter, Phenomenex) and eluted with a mobile phase containing 0.1 M Na2HPO4, 0.1 mM EDTA, and 7.5% methanol (pH 3.2). Glutamate was derivatized for electrochemical detection with o-pthaldialdehyde and quantitated with an LC-4C amperometric detector (BAS Bioanalytical) as previously described (Donzanti and Yamamoto, 1988). Data were recorded using EZ Chrom Software.
Analysis of Spectrin Breakdown Products and GFAP
The specific spectrin breakdown product at 145 kDa is a marker for excitotoxic damage (Harris and Morrow, 1988, Staszewski and Yamamoto, 2006) and is mediated by calpain, a calcium-activated protease. The spectrin breakdown products at 120 kDa were also measured, as it is specific for caspase-medated spectrin proteolysis (Pike et al, 2001). In addition, protein expression of glial fibrillary acidic protein (GFAP) was measured as an indicator of astrocyte activation.
To examine the contribution of ammonia to METH-induced excitotoxic terminal damage and astrocyte activation, the spectrin breakdown products and GFAP, respectively, were measured via western blot, in the striatum of rats treated with lactulose or vehicle and then challenged with METH or saline. Rats were killed by rapid decapitation 5 days after METH or saline challenge to groups pretreated with lactulose or vehicle treatment. Striata were dissected and homogenized in a buffer containing 10 mM Tris, 10 mM EGTA, 250 mM sucrose, and Halt protease inhibitor cocktail (Thermo Scientific). Equal amounts of protein (30 μg for spectrin and 20 μg for GFAP) from each sample were separated via electrophoresis and transferred to a PVDF membrane. Spectrin breakdown products were examined using an antibody for non-erythroid α-spectrin (MAB1622; Chemicon) and a HRP-conjugated secondary antibody. GFAP was detected using a mouse monoclonal antibody (1 : 3000, cat. no. 814369, Boehringer Mannheim) and a goat anti-mouse HRP-conjugated secondary antibody (Santa Cruz Biotechnology). The loading and transfer control, α-tubulin, was detected using a mouse monoclonal primary antibody (1 : 3000, cat. no. T6074, Sigma) and goat anti-mouse HRP-conjugated secondary antibody (Santa Cruz Biotechnology).
The immunoreactive spectrin breakdown products at 120, 145 and 230 kDa and GFAP were analyzed on membranes by densitometry using the Fuji LAS-400 Mini System. Immunoreactivity of the spectrin breakdown products and GFAP were normalized to α-tubulin and data are expressed as a percentage of vehicle-saline-treated rats.
Statistical Analysis
Calpain-mediated spectrin proteolysis and GFAP levels were analyzed using two-way ANOVA tests followed by Tukey's post-hoc comparisons. These tests were performed using SigmaPlot 11.0 Software (Systat Software, SigmaPlot for Windows). Statistical analysis of brain glutamate levels was carried out using repeated-measures ANOVA tests, with each time point as a within-subjects factor and lactulose and METH treatment as between-subjects factor. These tests were performed using SPSS Statistics 17.0 Software (IBM Corporation). All data are presented as mean±SEM. α level in all studies is 0.05 or less and sample sizes were chosen to result in a power of 0.80 or greater.
RESULTS
Effect of Ammonia on METH-Induced Increases in Extracellular Glutamate
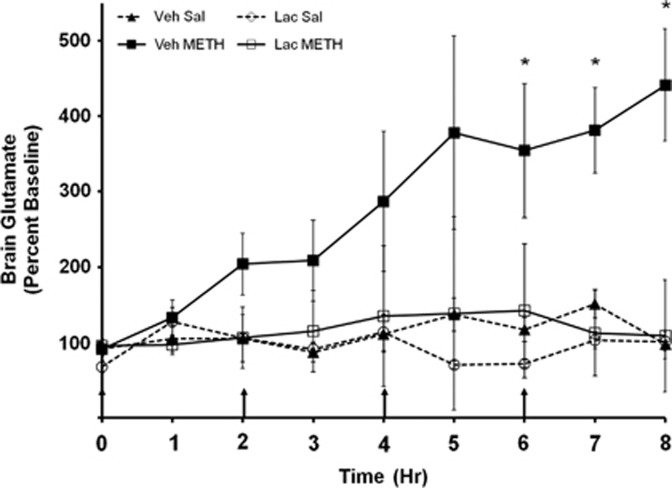
To determine the degree to which ammonia contributes to the increases in extracellular glutamate produced during systemic METH treatment, rats were pretreated with lactulose or vehicle and then treated with METH or saline. Extracellular glutamate was measured in vivo using microdialysis during treatment with METH or saline (Figure 1). Baseline extracellular glutamate concentrations in all groups were 1365.24±183.69 pg/20 μl. A repeated-measures ANOVA shows a main effect of METH treatment (F(7,167)=5.03, P<0.050) and a significant interaction between METH and lactulose treatment (F(7,167)=3.30, P<0.050). Striatal glutamate levels were significantly elevated in METH-treated rats at the 6-h time point (F(3,20)=4.77, P<0.05). These data demonstrate that increasing peripheral ammonia excretion with lactulose blocks METH-induced elevations in glutamate.
Figure 1.
Effect of ammonia on systemic METH-induced increases in extracellular glutamate: rats were treated with METH (10 mg/kg, q 2 h × 4) or saline (1 ml/kg, q 2 h × 4) and lactulose (5.3 g/kg every 12 h) or vehicle (8 ml/kg every 12 h). During METH treatment (arrows denote injections), striatal glutamate concentration was monitored using in vivo microdialysis. Vehicle+METH treatment significantly increases brain glutamate concentrations starting at timepoint 6. Lactulose pretreatment blocks the increase. (*P<0.05; n=8–10 rats per group).
Effect of Ammonia on METH-Induced Calpain-Mediated Spectrin Proteolysis
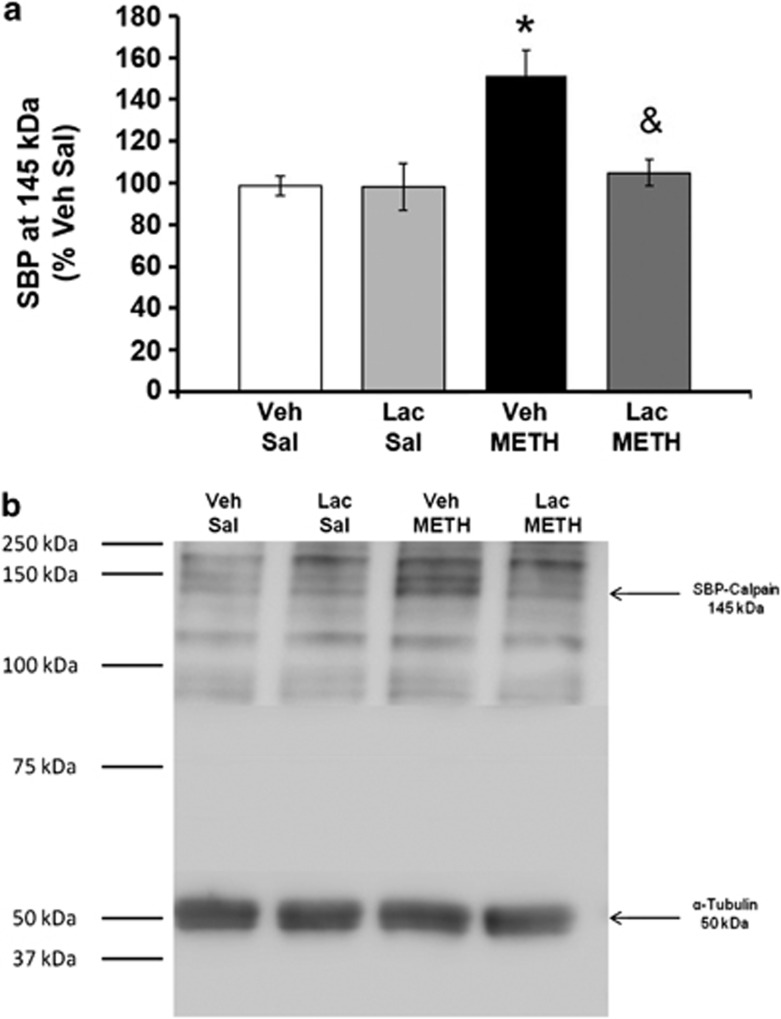
METH produced a 51.2±12.4% increase in calpain-specific spectrin breakdown, which was completely blocked by lactulose treatment. A two-way ANOVA revealed a significant interaction between METH and lactulose treatment (F(3,31)=5.74, P<0.05). Post-hoc Tukey tests indicate that METH has a significant effect on calpain-specific spectrin breakdown (q=6.34, P<0.001) and this effect is blocked by lactulose treatment (q=4.84, P<0.005; Figure 2a). A representative western blot for spectrin and α-tubulin immunoreactivity is also shown (Figure 2b). The caspase-specific spectrin breakdown product at 120 kDa as well as the 230-kDa band indicative of whoel spectrin were also measured and were not affected by METH and/or Lactulose treatments.
Figure 2.
Effect of ammonia on METH-induced increases in calpain-mediated spectrin proteolysis: rats were treated with METH (10 mg/kg, q 2 h × 4) or saline (1 ml/kg, q 2 h × 4) and lactulose (5.3 g/kg every 12 h) or vehicle (8 ml/kg every 12 h) and killed 5 days after drug treatment. (a) Lactulose prevents METH-induced increases in the spectrin breakdown product (SBP), which is specific for calpain proteolysis (*P<0.05 compared with Veh Sal; &P<0.005 compared with Veh METH; n=6–9 per group). (b) Representative western blot for spectrin breakdown products and α-tubulin loading control.
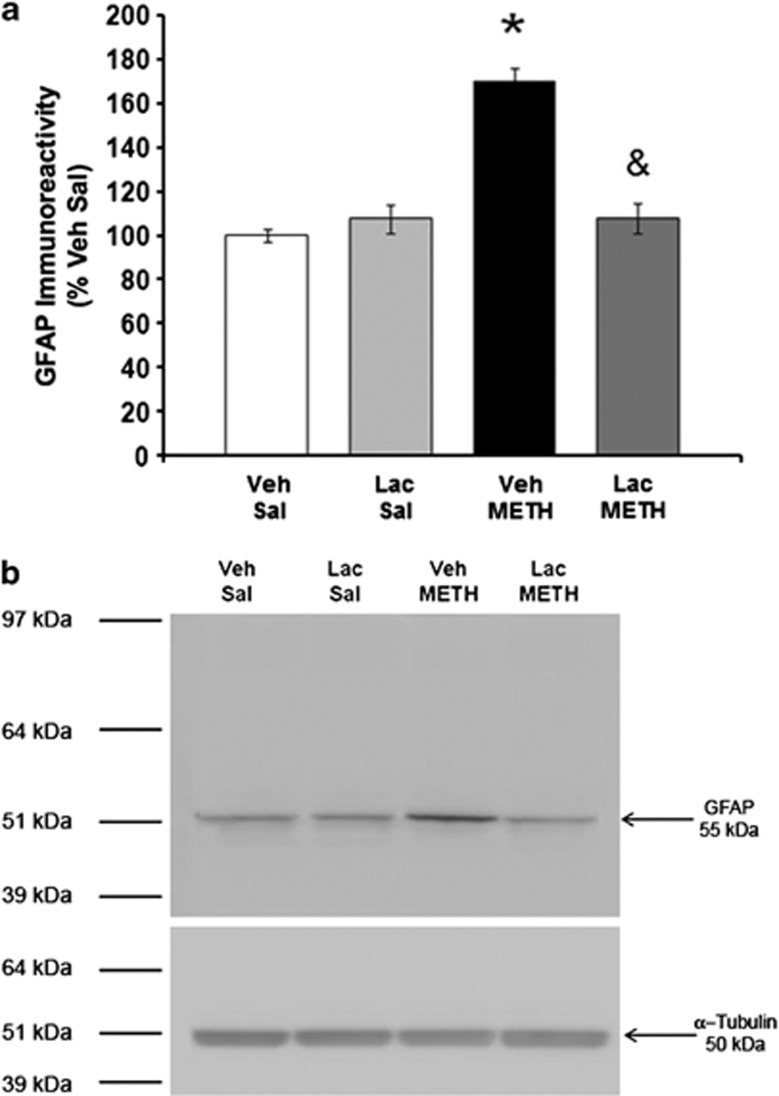
Effect of Ammonia on METH-Induced GFAP Expression
METH increased GFAP protein expression by 70.0±16.5%, and this increase was prevented by lactulose treatment. A two-way ANOVA revealed a significant interaction between METH and lactulose treatment (F(1,31)=5.76, P<0.05). Post-hoc Tukey tests indicate that METH produces a significant increase in GFAP expression (q=4.93, P<0.005) and METH-treated rats that received lactulose treatment had significantly less GFAP expression than those that received vehicle (q=4.35, P<0.005) (Figure 3a). A representative western blot for GFAP and α-tubulin immunoreactivity is presented in Figure 3b, illustrating the GFAP immunoreactive positive band at 55 kDa and the α-tubulin immunoreactive band at 50 kDa.
Figure 3.
Effect of Ammonia on METH-Induced Increases in GFAP. Rats were treated with METH (10 mg/kg, q 2 h × 4) or saline (1 ml/kg, q 2 h × 4) and lactulose (5.3 g/kg every 12 h) or vehicle (8 ml/kg every 12 h) and killed 5 days after drug treatment. (a) METH increases striatal GFAP protein expression (*P<0.05, compared with Veh Sal) and lactulose prevents the METH-induced increases in GFAP (&P<0.005, compared with Veh METH; (n=8–10 per group). (b) Representative western blot image for GFAP and α-tubulin loading control.
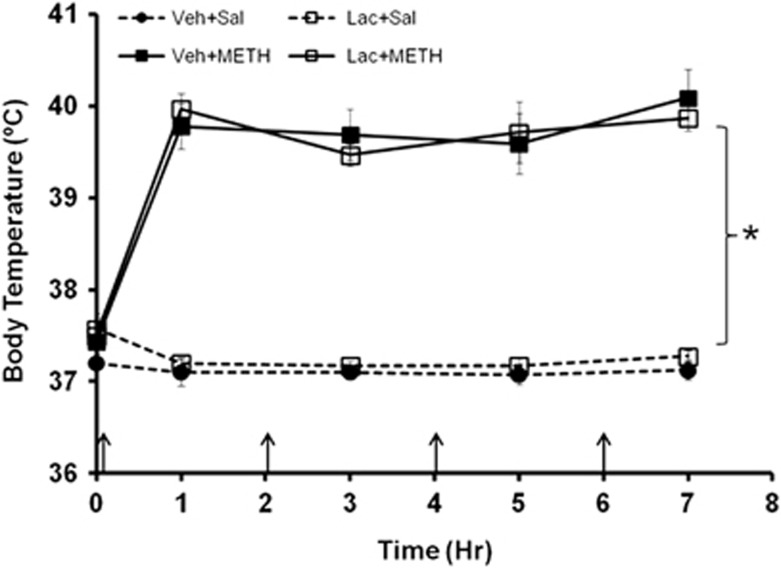
Effect of Lactulose on Body Temperature
To examine if lactulose affected body temperature during METH treatment, temperatures were measured at 1 h after injection with METH or saline in rats that were treated with lactulose or vehicle. METH produced a significant increase in body temperature throughout drug treatment that was not affected by treatment with lactulose (Figure 4).
Figure 4.
Effect of METH and lactulose on body temperature: rats were treated with METH (10 mg/kg, q 2 h × 4) or saline (1 ml/kg, q 2 h × 4) and lactulose (5.3 g/kg every 12 h) or vehicle (8 ml/kg every 12 h) and body temperature was measured after each injection (arrows denote injections). METH produces significant hyperthermia that is not affected by lactulose treatment (*P<0.05, n=8–10 rats per group).
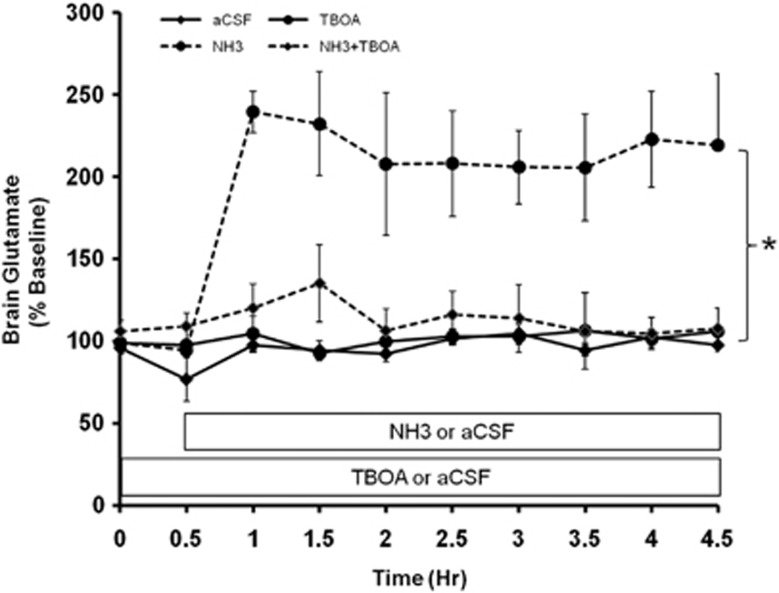
Effect of Locally Administered Ammonia and Glutamate Transporter Function on Extracellular Glutamate
To examine if the elevation of brain ammonia observed during systemic METH treatment alters extracellular glutamate concentrations, ammonia was directly administered via reverse dialysis into the striatum for 8 h during which changes in extracellular glutamate were measured (Figure 5). A repeated-measures ANOVA shows that ammonia significantly increased brain extracellular glutamate concentrations (F(1,18)=11.60, P<0.001). These ammonia-induced increases represent an approximately two- to threefold increase in extracellular glutamate. There also was a significant interaction between treatment with TBOA and ammonia throughout all time points (F(1,18)=13.51, P<0.005) illustrating that TBOA blocked the ammonia-induced increases in glutamate throughout the time course of the experiment.
Figure 5.
Effect of the direct administration of ammonia and TBOA on striatal glutamate: artificial cerebrospinal fluid (aCSF), ammonia (200 μM), DL-threo-β-benzyloxyaspartic acid (TBOA; 500 μM) or the combination of ammonia and TBOA were reverse dialyzed and striatal glutamate was measured every 30 min using in vivo microdialysis. Ammonia significantly increases local striatal glutamate concentrations (*P<0.005) and this increase is blocked by TBOA pretreatment and co-administration (n=5–6 rats per group).
DISCUSSION
These findings demonstrate that ammonia mediates METH-induced increases in extracellular glutamate and excitotoxicity. The prevention of METH-induced increases in ammonia with lactulose treatment eliminated the increases in striatal extracellular glutamate observed during systemic METH treatment. In addition to contributing to METH-induced increases in glutamate, ammonia also mediated METH-induced excitotoxicity, measured by calpain-mediated spectrin proteolysis, and astrocyte activation, measured by increases in GFAP. Moreover, ammonia delivered directly to the striatum at the concentrations measured in the striatum during systemic METH exposure, increased extracellular glutamate concentrations in the striatum. To determine a mechanism underlying the increase in extracellular glutamate by ammonia, antagonism of EAAT within the striatum prevented the increases in striatal glutamate produced by ammonia.
METH produced a significant increase in glutamate starting after the fourth injection of METH that persisted for at least 2 h after that injection (Figure 1). Importantly, treatment with lactulose blocked the increases in striatal extracellular glutamate. As lactulose has been shown to block METH-induced increases in brain ammonia by decreasing plasma ammonia (Halpin and Yamamoto, 2012), the current findings suggest that increases in plasma and therefore brain ammonia are required for METH-induced increases in glutamate. These results are consistent with previous studies that demonstrate ammonia increases glutamate through alterations in the release and reuptake by astrocytes as primary regulators of extracellular glutamate (Benjamin and Quastel, 1975; Chan and Butterworth, 1999; Danbolt, 2001; Gorg et al, 2010; Kosenko et al, 2003). Although METH can increase corticostriatal glutamate release in a dopamine-dependent manner (Mark et al, 2004), METH can also produce increases in striatal glutamate that are independent of increases in dopamine (Stephans and Yamamoto, 1994). In fact, the current findings identify a mechanism by which the drug contributes to increases in glutamate in a dopamine-independent manner. Accordingly, our results suggest that the effects of ammonia on the local release and metabolism of glutamate by astrocytes, in combination with dopamine-mediated increases in glutamate release from corticostriatal projections, are important in mediating METH-induced increases in extracellular glutamate.
To relate the findings of increases in glutamate to neurotoxicity, we examined if ammonia also contributes significantly to METH-induced excitotoxicity through calpain-mediated spectrin proteolysis. Calpain is a protease whose activity increases in response to increases in calcium and promotes excitotoxicity (Harris and Morrow, 1988; Siman et al, 1989). During and shortly after METH exposure, significant increases in extracellular glutamate activate calcium-permeable glutamate receptors, which have been implicated in METH-mediated monoaminergic terminal damage (Farfel et al, 1992; Sonsalla et al, 1991; Stephans and Yamamoto, 1994). Subsequent to calcium-permeable glutamate receptor activation, there is an influx of intracellular calcium, activation of calpain, and excitotoxicity (Staszewski and Yamamoto, 2006). We found that METH produced a 51.2% increase in calpain-mediated spectrin proteolysis (Figure 2). Although this may seem like a quantitatively small increase in calpain activity, especially in comparison with the fourfold increase in glutamate noted after METH exposure (Figure 1), it is worth noting that calpain is a calcium-activated protease whose activity increases in response to extracellular calcium in the micromolar range (Goll et al, 2003). Accordingly, a physiologically significant, multi-fold increase in calcium must be achieved to overcome the homeostatic mechanisms that regulate intracellular calcium for calpain to be activated (Maravall et al, 2000).
When increases in brain ammonia were blocked during and after METH treatment with lactulose, METH-induced increases in calpain-mediated spectrin proteolysis were prevented (Figure 2). Calpain is a protease that is activated subsequent to calcium influx and targets essential cytoskeletal proteins, including spectrin, to mediate the excitotoxic effects of glutamate (Siman et al, 1989). METH has been shown to increase calpain-mediated spectrin proteolysis in an AMPA receptor-dependent manner (Staszewski and Yamamoto, 2006). The finding that ammonia is required for METH-induced calpain-mediated spectrin proteolysis suggests that it is important for increases in both glutamate and excitotoxicity.
METH-induced ammonia also contributes to astrocyte activation, as measured by increases in GFAP protein expression when measured 5 days after drug exposure (Figure 3). The increases in GFAP expression are indicative of astrocyte activation presumably in response to damage and is consistent with previous studies that have demonstrated increases in GFAP expression days to weeks after exposure to a neurotoxic dose of METH (O'Callaghan and Miller 1994; Zhu et al, 2005). Astrocyte activation after METH exposure is a likely consequence of damage to monoamine terminals in the striatum (Bowyer et al, 1994; O'Callaghan and Miller 1994) and cell body damage in the somatosensory cortex (Pu et al, 1996). Furthermore, the prevention of METH-induced dopaminergic terminal damage is associated with blockade of METH-induced increases in GFAP (O'Callaghan and Miller 1994). Therefore, the finding that lactulose prevents METH-induced activation of astrocytes further implicates the role of ammonia in METH-induced neurotoxicity.
It is important to note that although lactulose blocked the increases in calpain-mediated spectrin proteolysis and astrocyte activation, it did not have any effect on METH-induced hyperthermia (Figure 4). Despite the fact that hyperthermia is an important mediator of METH-induced neurotoxicity to dopamine and 5HT terminals (Albers and Sonsalla, 1995; Bowyer et al, 1994; Bowyer et al, 1992; Haughey et al, 2000; Kiyatkin and Sharma, 2009; Xie et al, 2000), this finding supports the conclusion that the protective effects of lactulose are likely due to its ability to reduce brain ammonia and not through an alteration of body temperature.
The finding that ammonia is required for METH-induced increases in glutamate and excitotoxicity prompted us to examine whether ammonia, at the brain concentrations measured after METH treatment, could alter extracellular glutamate levels when administered directly into the striatum. The results illustrated in Figure 5 show that the reverse dialysis of ammonia directly into the striatum increased extracellular glutamate concentrations by two- to threefold. It is interesting that this increase only partially accounts for the four- to fivefold increase in striatal glutamate observed with systemic METH treatment (Nash and Yamamoto, 1992), and suggests that systemic METH treatment contributes to increases in extracellular glutamate through additional mechanisms other than those mediated by ammonia alone. An additional contributor to the increases in glutamate after systemic METH administration is most likely from METH-induced increases in dopamine and D1-receptor-mediated disinhibition of a polysynaptic pathway that lead to increases in corticostriatal glutamate release (Mark et al, 2004). Therefore, the METH-induced increases in striatal glutamate are mediated by both dopamine and ammonia through neuronal and non-neuronal mechanisms, respectively.
Although ammonia is capable of increasing extracellular glutamate, local administration of ammonia alone does not produce the long-term damage to dopamine and serotonin terminals observed after systemic METH treatment (Halpin and Yamamoto, 2012). This finding is consistent with previous reports that the direct administration of glutamate alone into the striatum does not produce long-term depletions in dopamine tissue content (Tata and Yamamoto, 2007). The direct administration of either ammonia or glutamate into the striatum only produces monoaminergic terminal damage when combined with METH (Halpin and Yamamoto, 2012). Accordingly, it appears that increases in extracellular glutamate via increases in ammonia, as well as the pharmacological action of METH at monoamine transporters, interact synergistically to produce the relatively selective long-term monoaminergic terminal damage caused by the drug (Abekawa et al, 1994; Stephans and Yamamoto, 1994). This synergistic interaction may explain why global increases in ammonia can account for the relatively selective damage produced by METH in a manner that targets brain regions where there is a convergence of glutamatergic afferents and innervations by dopamine and serotonin terminals associated with their cognate transporters.
To examine the mechanism by which ammonia may contribute to increases in extracellular glutamate, EAAT activity was blocked using TBOA during ammonia exposure. Ammonia-mediated increases in glutamate were blocked by treatment with TBOA suggesting that excitatory amino-acid transporters are required for this effect (Figure 5). Although ammonia has been shown to affect transporter expression at later and more protracted time points (Chan and Butterworth, 1999; Chan et al, 2000), this finding suggests that it may also affect the function of the transporter more acutely by altering the ionic gradients that are responsible for determining the directionality of the transporter (Barbour et al, 1988; Chan and Butterworth, 1999; Grewer et al, 2008; Szatkowski et al, 1990). The alteration of the directionality of the transporter would prevent the removal of glutamate from the synapse while allowing glutamate within astrocytes to be released into the extracellular space. This reversed action of the transporters has been shown to be dependent on extracellular potassium levels, such that an increase in extracellular potassium prevents uptake and produces non-vesicular release of glutamate from astrocytes (Barbour et al, 1988; Grewer et al, 2008; Szatkowski et al, 1990). In fact, the ammonium ion has a similar ionic radius to the potassium ion and may contribute to increases in glutamate by altering the potassium gradient and reversing the direction of glutamate transporters to cause an efflux of glutamate (Rose, 2002). Accordingly, METH increases excitatory neurotransmission via the ammonia-induced release of glutamate from astrocytes and limiting local astrocytic glutamate metabolism, in addition to increasing release of glutamate from corticostriatal terminals. This alteration in local glutamate metabolism by ammonia may further potentiate the increases in extracellular glutamate.
Overall, these findings identify ammonia as a key mediator of METH-induced increases in glutamate and excitotoxicity. These findings have broader significance as they demonstrate that increases in brain ammonia acutely contribute to increases in extracellular glutamate and suggest ammonia as a small-molecule modulator of glutamatergic neurotransmission and a significant mediator of excitotoxicity. These findings are particularly relevant to overdose and poisoning cases involving experienced METH abusers who administer repeated high doses of METH. The results may also have significance for the role of ammonia in the context of other disorders including Alzheimer's disease, ischemic stroke, Huntington's chorea and neurodegenerative diseases where excitotoxicity has a role (Choi, 1988).
FUNDING AND DISCLOSURE
The authors declare no conflict of interest.
Acknowledgments
This work is supported by NIH grant DA007606.
References
- Abekawa T, Ohmori T, Koyama T. Effects of repeated administration of a high dose of methamphetamine on dopamine and glutamate release in rat striatum and nucleus accumbens. Brain Res. 1994;643:276–281. doi: 10.1016/0006-8993(94)90033-7. [DOI] [PubMed] [Google Scholar]
- Al Sibae MR, McGuire BM. Current trends in the treatment of hepatic encephalopathy. Therap Clin Risk Manag. 2009;5:617–626. doi: 10.2147/tcrm.s4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albers DS, Sonsalla PK. Methamphetamine-induced hyperthermia and dopaminergic neurotoxicity in mice: pharmacological profile of protective and nonprotective agents. J Pharmacol Exp Therap. 1995;275:1104–1114. [PubMed] [Google Scholar]
- Barbour B, Brew H, Attwell D. Electrogenic glutamate uptake in glial cells is activated by intracellular potassium. Nature. 1988;335:433–435. doi: 10.1038/335433a0. [DOI] [PubMed] [Google Scholar]
- Benjamin AM, Quastel JH. Metabolism of amino acids and ammonia in rat brain cortex slices in vitro: a possible role of ammonia in brain function. J Neurochem. 1975;25:197–206. doi: 10.1111/j.1471-4159.1975.tb06953.x. [DOI] [PubMed] [Google Scholar]
- Betarbet R, Greenamyre JT. Differential expression of glutamate receptors by the dopaminergic neurons of the primate striatum. Exp Neurol. 1999;159:401–408. doi: 10.1006/exnr.1999.7154. [DOI] [PubMed] [Google Scholar]
- Bowyer JF, Davies DL, Schmued L, Broening HW, Newport GD, Slikker W, Jr, et al. Further studies of the role of hyperthermia in methamphetamine neurotoxicity. J Pharmacol Exp Ther. 1994;268:1571–1580. [PubMed] [Google Scholar]
- Bowyer JF, Tank AW, Newport GD, Slikker W, Jr., Ali SF, Holson RR. The influence of environmental temperature on the transient effects of methamphetamine on dopamine levels and dopamine release in rat striatum. J Pharmacol Exp Ther. 1992;260:817–824. [PubMed] [Google Scholar]
- Cauli O, Rodrigo R, Piedrafita B, Boix J, Felipo V. Inflammation and hepatic encephalopathy: ibuprofen restores learning ability in rats with portacaval shunts. Hepatology. 2007;46:514–519. doi: 10.1002/hep.21734. [DOI] [PubMed] [Google Scholar]
- Chan H, Butterworth RF. Evidence for an astrocytic glutamate transporter deficit in hepatic encephalopathy. Neurochem Res. 1999;24:1397–1401. doi: 10.1023/a:1022532623281. [DOI] [PubMed] [Google Scholar]
- Chan H, Hazell AS, Desjardins P, Butterworth RF. Effects of ammonia on glutamate transporter (GLAST) protein and mRNA in cultured rat cortical astrocytes. Neurochem Int. 2000;37:243–248. doi: 10.1016/s0197-0186(00)00026-7. [DOI] [PubMed] [Google Scholar]
- Choi DW. Glutamate neurotoxicity and diseases of the nervous system. Neuron. 1988;1:623–634. doi: 10.1016/0896-6273(88)90162-6. [DOI] [PubMed] [Google Scholar]
- Clark L, Robbins TW, Ersche KD, Sahakian BJ. Reflection impulsivity in current and former substance users. Biol Psychiatry. 2006;60:515–522. doi: 10.1016/j.biopsych.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Cruickshank CC, Dyer KR. A review of the clinical pharmacology of methamphetamine. Addiction. 2009;104:1085–1099. doi: 10.1111/j.1360-0443.2009.02564.x. [DOI] [PubMed] [Google Scholar]
- Danbolt NC. Glutamate uptake. Prog Neurobiol. 2001;65:1–105. doi: 10.1016/s0301-0082(00)00067-8. [DOI] [PubMed] [Google Scholar]
- Donzanti BA, Yamamoto BK. An improved and rapid HPLC-EC method for the isocratic separation of amino acid neurotransmitters from brain tissue and microdialysis perfusates. Life Sci. 1988;43:913–922. doi: 10.1016/0024-3205(88)90267-6. [DOI] [PubMed] [Google Scholar]
- Farfel GM, Vosmer GL, Seiden LS. The N-methyl-D-aspartate antagonist MK-801 protects against serotonin depletions induced by methamphetamine, 3,4-methylenedioxymethamphetamine and p-chloroamphetamine. Brain Res. 1992;595:121–127. doi: 10.1016/0006-8993(92)91460-v. [DOI] [PubMed] [Google Scholar]
- Gerencser AA, Mark KA, Hubbard AE, Divakaruni AS, Mehrabian Z, Nicholls DG, et al. Real-time visualization of cytoplasmic calpain activation and calcium deregulation in acute glutamate excitotoxicity. J Neurochem. 2009;110:990–1004. doi: 10.1111/j.1471-4159.2009.06194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goll DE, Thompson VF, Li H, Wei W, Cong J. The calpain system. Physiol Rev. 2003;83:731–801. doi: 10.1152/physrev.00029.2002. [DOI] [PubMed] [Google Scholar]
- Gorg B, Morwinsky A, Keitel V, Qvartskhava N, Schror K, Haussinger D. Ammonia triggers exocytotic release of L-glutamate from cultured rat astrocytes. Glia. 2010;58:691–705. doi: 10.1002/glia.20955. [DOI] [PubMed] [Google Scholar]
- Gorg B, Qvartskhava N, Voss P, Grune T, Haussinger D, Schliess F. Reversible inhibition of mammalian glutamine synthetase by tyrosine nitration. FEBS Lett. 2007;581:84–90. doi: 10.1016/j.febslet.2006.11.081. [DOI] [PubMed] [Google Scholar]
- Grewer C, Gameiro A, Zhang Z, Tao Z, Braams S, Rauen T. Glutamate forward and reverse transport: from molecular mechanism to transporter-mediated release after ischemia. IUBMB Life. 2008;60:609–619. doi: 10.1002/iub.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpin LE, Yamamoto BK. Peripheral ammonia as a mediator of methamphetamine neurotoxicity. J Neurosci. 2012;32:13155–13163. doi: 10.1523/JNEUROSCI.2530-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris AS, Morrow JS. Proteolytic processing of human brain alpha spectrin (fodrin): identification of a hypersensitive site. J Neurosci. 1988;8:2640–2651. doi: 10.1523/JNEUROSCI.08-07-02640.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haskew-Layton RE, Rudkouskaya A, Jin Y, Feustel PJ, Kimelberg HK, Mongin AA. Two distinct modes of hypoosmotic medium-induced release of excitatory amino acids and taurine in the rat brain in vivo. PLoS One. 2008;3:e3543. doi: 10.1371/journal.pone.0003543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haughey HM, Fleckenstein AE, Metzger RR, Hanson GR. The effects of methamphetamine on serotonin transporter activity: role of dopamine and hyperthermia. J Neurochem. 2000;75:1608–1617. doi: 10.1046/j.1471-4159.2000.0751608.x. [DOI] [PubMed] [Google Scholar]
- Hawkins RA, Miller AL, Nielsen RC, Veech RL. The acute action of ammonia on rat brain metabolism in vivo. Biochem J. 1973;134:1001–1008. doi: 10.1042/bj1341001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez LF, Segovia G, Mora F. Effects of activation of NMDA and AMPA glutamate receptors on the extracellular concentrations of dopamine, acetylcholine, and GABA in striatum of the awake rat: a microdialysis study. Neurochem Res. 2003;28:1819–1827. doi: 10.1023/a:1026115607216. [DOI] [PubMed] [Google Scholar]
- Jia L, Zhang MH. Comparison of probiotics and lactulose in the treatment of minimal hepatic encephalopathy in rats. World J Gastroenterol. 2005;11:908–911. doi: 10.3748/wjg.v11.i6.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johanson CE, Frey KA, Lundahl LH, Keenan P, Lockhart N, Roll J, et al. Cognitive function and nigrostriatal markers in abstinent methamphetamine abusers. Psychopharmacology (Berl) 2006;185:327–338. doi: 10.1007/s00213-006-0330-6. [DOI] [PubMed] [Google Scholar]
- Keefe KA, Zigmond MJ, Abercrombie ED. In vivo regulation of extracellular dopamine in the neostriatum: influence of impulse activity and local excitatory amino acids. J Neural Transmission General Sect. 1993;91:223–240. doi: 10.1007/BF01245233. [DOI] [PubMed] [Google Scholar]
- Kiyatkin EA, Sharma HS. Acute methamphetamine intoxication brain hyperthermia, blood-brain barrier, brain edema, and morphological cell abnormalities. Int Rev Neurobiol. 2009;88:65–100. doi: 10.1016/S0074-7742(09)88004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosenko E, Kaminsky Y, Kaminsky A, Valencia M, Lee L, Hermenegildo C, et al. Superoxide production and antioxidant enzymes in ammonia intoxication in rats. Free Radic Res. 1997;27:637–644. doi: 10.3109/10715769709097867. [DOI] [PubMed] [Google Scholar]
- Kosenko E, Llansola M, Montoliu C, Monfort P, Rodrigo R, Hernandez-Viadel M, et al. Glutamine synthetase activity and glutamine content in brain: modulation by NMDA receptors and nitric oxide. Neurochem Int. 2003;43:493–499. doi: 10.1016/s0197-0186(03)00039-1. [DOI] [PubMed] [Google Scholar]
- Maravall M, Mainen ZF, Sabatini BL, Svoboda K. Estimating intracellular calcium concentrations and buffering without wavelength ratioing. Biophys J. 2000;78:2655–2667. doi: 10.1016/S0006-3495(00)76809-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark KA, Soghomonian JJ, Yamamoto BK. High-dose methamphetamine acutely activates the striatonigral pathway to increase striatal glutamate and mediate long-term dopamine toxicity. J Neurosci. 2004;24:11449–11456. doi: 10.1523/JNEUROSCI.3597-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann UD, Wong DF, Yokoi F, Villemagne V, Dannals RF, Ricaurte GA. Reduced striatal dopamine transporter density in abstinent methamphetamine and methcathinone users: evidence from positron emission tomography studies with [11C]WIN-35,428. J Neurosci. 1998;18:8417–8422. doi: 10.1523/JNEUROSCI.18-20-08417.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKetin R, McLaren J, Lubman DI, Hides L. The prevalence of psychotic symptoms among methamphetamine users. Addiction. 2006;101:1473–1478. doi: 10.1111/j.1360-0443.2006.01496.x. [DOI] [PubMed] [Google Scholar]
- Mortensen PB. The effect of oral-administered lactulose on colonic nitrogen metabolism and excretion. Hepatology. 1992;16:1350–1356. doi: 10.1002/hep.1840160608. [DOI] [PubMed] [Google Scholar]
- Nash JF, Yamamoto BK. Methamphetamine neurotoxicity and striatal glutamate release: comparison to 3,4-methylenedioxymethamphetamine. Brain Res. 1992;581:237–243. doi: 10.1016/0006-8993(92)90713-j. [DOI] [PubMed] [Google Scholar]
- Nicaise C, Prozzi D, Viaene E, Moreno C, Gustot T, Quertinmont E, et al. Control of acute, chronic, and constitutive hyperammonemia by wild-type and genetically engineered Lactobacillus plantarum in rodents. Hepatology. 2008;48:1184–1192. doi: 10.1002/hep.22445. [DOI] [PubMed] [Google Scholar]
- Norenberg MD. The role of astrocytes in hepatic encephalopathy. Neurochem Pathol. 1987;6:13–33. doi: 10.1007/BF02833599. [DOI] [PubMed] [Google Scholar]
- O'Callaghan JP, Miller DB. Neurotoxicity profiles of substituted amphetamines in the C57BL/6 J mouse. J Pharmacol Exp Ther. 1994;270:741–751. [PubMed] [Google Scholar]
- Panesar PS, Kumari S. Lactulose: production, purification and potential applications. Biotechnol Adv. 2011;29:940–948. doi: 10.1016/j.biotechadv.2011.08.008. [DOI] [PubMed] [Google Scholar]
- Pike BR, Flint J, Dutta S, Johnson E, Wang KK, Hayes RL. Accumulation of non-erythroid alpha II-spectrin and calpain-cleaved alpha II-spectrin breakdown products in cerebrospinal fluid after traumatic brain injury in rats. J Neurochem. 2001;78:1297–1306. doi: 10.1046/j.1471-4159.2001.00510.x. [DOI] [PubMed] [Google Scholar]
- Pu C, Broening HW, Vorhees CV. Effect of methamphetamine on glutamate-positive neurons in the adult and developing rat somatosensory cortex. Synapse. 1996;23:328–334. doi: 10.1002/(SICI)1098-2396(199608)23:4<328::AID-SYN11>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- Ricaurte GA, Guillery RW, Seiden LS, Schuster CR, Moore RY. Dopamine nerve terminal degeneration produced by high doses of methylamphetamine in the rat brain. Brain Res. 1982;235:93–103. doi: 10.1016/0006-8993(82)90198-6. [DOI] [PubMed] [Google Scholar]
- Ricaurte GA, Schuster CR, Seiden LS. Long-term effects of repeated methylamphetamine administration on dopamine and serotonin neurons in the rat brain: a regional study. Brain Res. 1980;193:153–163. doi: 10.1016/0006-8993(80)90952-x. [DOI] [PubMed] [Google Scholar]
- Rogers RD, Everitt BJ, Baldacchino A, Blackshaw AJ, Swainson R, Wynne K, et al. Dissociable deficits in the decision-making cognition of chronic amphetamine abusers, opiate abusers, patients with focal damage to prefrontal cortex, and tryptophan-depleted normal volunteers: evidence for monoaminergic mechanisms. Neuropsychopharmacology. 1999;20:322–339. doi: 10.1016/S0893-133X(98)00091-8. [DOI] [PubMed] [Google Scholar]
- Rose C. Increased extracellular brain glutamate in acute liver failure: decreased uptake or increased release. Metabolic Brain Dis. 2002;17:251–261. doi: 10.1023/a:1021945515514. [DOI] [PubMed] [Google Scholar]
- Saggu SK, Chotaliya HP, Blumbergs PC, Casson RJ. Wallerian-like axonal degeneration in the optic nerve after excitotoxic retinal insult: an ultrastructural study. BMC Neurosci. 2010;11:97. doi: 10.1186/1471-2202-11-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seiden LS, Commins DL, Vosmer G, Axt K, Marek G. Neurotoxicity in dopamine and 5-hydroxytryptamine terminal fields: a regional analysis in nigrostriatal and mesolimbic projections. Ann N Y Acad Sci. 1988;537:161–172. doi: 10.1111/j.1749-6632.1988.tb42104.x. [DOI] [PubMed] [Google Scholar]
- Siman R, Noszek JC, Kegerise C. Calpain I activation is specifically related to excitatory amino acid induction of hippocampal damage. J Neurosci. 1989;9:1579–1590. doi: 10.1523/JNEUROSCI.09-05-01579.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon SL, Domier CP, Sim T, Richardson K, Rawson RA, Ling W. Cognitive performance of current methamphetamine and cocaine abusers. J Addict Dis. 2002;21:61–74. doi: 10.1300/j069v21n01_06. [DOI] [PubMed] [Google Scholar]
- Sonsalla PK, Riordan DE, Heikkila RE. Competitive and noncompetitive antagonists at N-methyl-D-aspartate receptors protect against methamphetamine-induced dopaminergic damage in mice. J Pharmacol Exp Ther. 1991;256:506–512. [PubMed] [Google Scholar]
- Staszewski RD, Yamamoto BK. Methamphetamine-induced spectrin proteolysis in the rat striatum. J Neurochem. 2006;96:1267–1276. doi: 10.1111/j.1471-4159.2005.03618.x. [DOI] [PubMed] [Google Scholar]
- Stephans SE, Yamamoto BK. Methamphetamine-induced neurotoxicity: roles for glutamate and dopamine efflux. Synapse. 1994;17:203–209. doi: 10.1002/syn.890170310. [DOI] [PubMed] [Google Scholar]
- Szatkowski M, Barbour B, Attwell D. Non-vesicular release of glutamate from glial cells by reversed electrogenic glutamate uptake. Nature. 1990;348:443–446. doi: 10.1038/348443a0. [DOI] [PubMed] [Google Scholar]
- Tata DA, Yamamoto BK. Interactions between methamphetamine and environmental stress: role of oxidative stress, glutamate and mitochondrial dysfunction. Addiction. 2007;102 (Suppl 1:49–60. doi: 10.1111/j.1360-0443.2007.01770.x. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Chang L, Wang GJ, Fowler JS, Leonido-Yee M, Franceschi D, et al. Association of dopamine transporter reduction with psychomotor impairment in methamphetamine abusers. Am J Psychiatry. 2001;158:377–382. doi: 10.1176/appi.ajp.158.3.377. [DOI] [PubMed] [Google Scholar]
- Wagner GC, Ricaurte GA, Seiden LS, Schuster CR, Miller RJ, Westley J. Long-lasting depletions of striatal dopamine and loss of dopamine uptake sites following repeated administration of methamphetamine. Brain Res. 1980;181:151–160. doi: 10.1016/0006-8993(80)91265-2. [DOI] [PubMed] [Google Scholar]
- Wang GJ, Smith L, Volkow ND, Telang F, Logan J, Tomasi D, et al. Decreased dopamine activity predicts relapse in methamphetamine abusers. Mol Psychiatry. 2012;17:918–925. doi: 10.1038/mp.2011.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie T, McCann UD, Kim S, Yuan J, Ricaurte GA. Effect of temperature on dopamine transporter function and intracellular accumulation of methamphetamine: implications for methamphetamine-induced dopaminergic neurotoxicity. J Neurosci. 2000;20:7838–7845. doi: 10.1523/JNEUROSCI.20-20-07838.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto BK, Raudensky J. The role of oxidative stress, metabolic compromise, and inflammation in neuronal injury produced by amphetamine-related drugs of abuse. J Neuroimmune Pharmacol. 2008;3:203–217. doi: 10.1007/s11481-008-9121-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu JP, Xu W, Angulo JA. Disparity in the temporal appearance of methamphetamine-induced apoptosis and depletion of dopamine terminal markers in the striatum of mice. Brain Res. 2005;1049:171–181. doi: 10.1016/j.brainres.2005.04.089. [DOI] [PMC free article] [PubMed] [Google Scholar]