Abstract
Objective
Marijuana is the most frequently reported illicit substance used on college campuses. Despite the prevalence, few published intervention studies have focused specifically on addressing high-risk marijuana use on college campuses. The present study evaluated the efficacy of an in-person brief motivational enhancement intervention for reducing marijuana use and related consequences among frequently using college students.
Method
Participants included 212 college students from two campuses who reported frequent marijuana use (i.e., using marijuana at least 5 times in the past month). Participants completed web-based screening and baseline assessments and upon completion of the baseline survey were randomized to either receive an in-person brief intervention or an assessment control group. Follow-up assessments were completed approximately three and six months post-baseline. Marijuana use was measured by number of days used in the last 30 days, typical number of joints used in a typical week in the last 60 days, and marijuana-related consequences.
Results
Results indicated significant intervention effects on number of joints smoked in a typical week and a trend toward fewer marijuana-related consequences compared to the control group at three-month follow-up.
Conclusion
This study provides preliminary data on short-term effects of a focused marijuana intervention for college students at reducing marijuana use during the academic quarter.
Keywords: college students, marijuana, intervention, prevention, marijuana related-consequences
Marijuana is the most commonly used illicit drug in the United States, with an estimated 17.4 million past month users (Substance Abuse and Mental Health Services Administration [SAMHSA], 2011), and nearly one-third of college students reporting use in the past year (American College Health Association, 2011; Johnston, O’Malley, Bachman, & Schulenberg, 2011). Marijuana use is associated with both short-and long-term consequences, including poor academic performance and attendance, impaired cognitive functioning, deficits related to attention and memory, respiratory problems, and increased heart rate, among others (e.g., Lynskey & Hall, 2000; National Institute on Drug Abuse, 2002; Roebuck, French, & Dennis, 2004; Taylor, Poulton, Moffitt, Ramankutty, & Sears, 2000; Solowij, 1998). Frequent users are at risk for health, psycho-social and legal outcomes across young adulthood and may have difficulties in the achievement of normative developmental tasks, such as graduating college, getting married, and steady employment (Schulenberg et al., 2005; Tucker et al., 2005). Thus, frequent young adult marijuana users are at risk for experiencing more acute and long-term consequences, and are a priority target for the development and evaluation of preventive interventions.
Adolescent and Adult Motivational Enhancement Strategies for Marijuana Use and Abuse
Motivational Interviewing (MI, Miller & Rollnick, 2002) is a non-judgmental, non-confrontational approach designed to enhance intrinsic motivation to change behavior by exploring and resolving ambivalence about change. A small but growing literature focused on intervening with marijuana disorders point to adaptations of MI as being an effective. Motivational enhancement therapy (MET) is an adaptation of MI that includes the provision of personalized feedback. MET has been shown to be an efficacious intervention for reducing marijuana use among non-treatment seeking adults (Stephens, Roffman, Fearer, Williams, & Burke, 2007) and adolescents (Walker et al., 2011) when compared to education. In treatment seeking populations, a five session MET plus Cognitive Behavior Therapy (CBT) was found to be as effective as longer and more intense family based treatments for marijuana abusing adolescents (Dennis et al., 2004). MET in combination with CBT and contingency management is indicated as the gold standard of intervention for treatment seeking adults (for a review see Budney, Roffman, Stephens, & Walker, 2007).
College Student Marijuana Use Intervention Strategies
Comparatively little work has evaluated interventions for marijuana use in the young adult college population, despite the prevalence of use on campuses. Studies of interventions for college student drug use have been limited. Three studies targeting college student drug use through selective and indicated approaches (e.g., McCambridge & Strang, 2004; Miller, Toscova, Miller, & Sanchez, 2001; White et al., 2006) suggest incorporating a motivational framework into an in-person intervention is promising. However, while each was associated with reductions in marijuana use, effect sizes were small, likely in part due to the focus on multiple substances rather than marijuana specifically. Yet, further highlighting the potential impact of a motivational enhancement approach is the finding that an intervention aiming to reduce alcohol-related harm nevertheless impacted marijuana use as well (Grossbard et al., 2010). Regardless, the potential impact of a motivational enhancement approach with a primary focus on marijuana seems indicated and promising.
In an effort to develop a low cost, brief motivational intervention, a web-based personalized feedback intervention for marijuana use geared toward first-year college students was developed and tested (Lee, Neighbors, Kilmer, & Larimer, 2010). Results indicated that while there was no overall intervention effect, this selective intervention targeting any first-year student reporting using any marijuana within the last ninety days was associated with reductions in marijuana use among students who were more contemplative about changing at baseline and/or reported a family history of drug use. Among these students, some effects were evident up to six months after implementation of the web-based personalized feedback intervention. These promising results support the continuation of examining brief motivational enhancement interventions utilizing personalized feedback for marijuana use for college students, however they also suggest that a more intensive (i.e., in-person) targeted intervention is needed for this population, and that greater focus on variables unique to marijuana use may be needed.
The Present Study
The purpose of the present study was to evaluate the efficacy of personalized feedback when delivered in the context of a brief in-person motivational intervention to frequent marijuana using college students. We hypothesized that students who received the in-person intervention would have reduced marijuana use and consequences compared to participants randomized to an assessment-only control condition at three and six month follow-up.
Methods
Participants
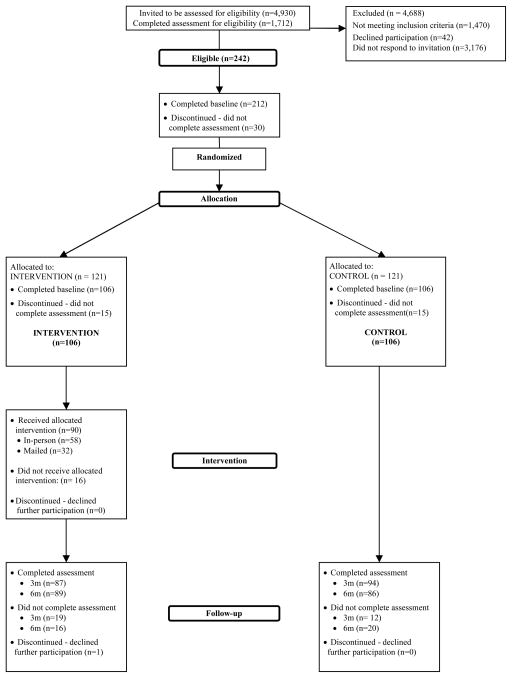
Participant flow through the study is presented in Figure 1. Participants for the present trial included 212 undergraduate college students from two public institutions in the Pacific Northwest (one small state college and one large state university). Across the two campuses, mean age of those enrolled in the trial was 20.0 (SD = 1.6), 45.3% were women, and the ethnicity breakdown was 74.8% Caucasian, 10.5% Asian or Pacific Islander, and 14.7% other, with 5.7% indicating they were Hispanic or Latino(a). Class standing included 23.6% who reported being freshmen, 27.4% sophomores, 23.6% juniors, and 25.5% seniors.
Figure 1.
Participant Flow
Procedure
Approximately 5000 randomly selected college students between the ages of 18–25 were recruited via US mail and email to participate in a brief online screening questionnaire designed to assess health behaviors among college students and to determine eligibility for a larger longitudinal trial (total N = 4930; 4000 from Campus 1 and 930 from Campus 2). Both the mailed letter and email provided a link to the study website. Students who logged on to the study website were presented with an online information statement describing all aspects of the study, and detailing incentives, confidentiality protections, and rights as a participant in human subjects research. Following the information statement, students who actively indicated their consent to participate) were asked to complete a 15–20 minute online screening survey. All procedures were approved by both IRB’s and overseen by the principal investigator’s university IRB. A federal Certificate of Confidentiality was obtained from the National Institutes of Health; there were no adverse events reported.
Eligibility criteria for the current longitudinal trial consisted of reporting marijuana use on five or more days in the prior month and consenting to participation. Participants who completed the screening survey and met eligibility criteria were immediately invited to complete a 30–40 minute online baseline survey assessing marijuana use and consequences in greater detail, as well as other necessary measures utilized in the personalized feedback.
Of the 4930 potential participants, 1712 (34.7%) completed the screening within 23 days of initial invitation and 241 (14.1%) met eligibility criteria. Due to higher rates of frequent marijuana use than planned, we closed the screening survey earlier than expected, as our goal was to enroll approximately 200 students into the trial. Approximately 88% of those eligible (N = 212) completed the baseline survey and were immediately randomized to one of two conditions: intervention (n = 106) or assessment control (n = 106). An algorithm was programmed to utilize a blocked randomized design of two groups based on baseline responses (i.e., using marijuana on 19 or fewer days in the last month and using marijuana 20 or more days in the last month) to randomize participants.
Participants could schedule and attend their in-person intervention directly online after completion of the baseline survey. Of the 106 participants randomized to intervention condition, 58 (54.7%) attended the in-person intervention. In total, 71 participants had scheduled a session, however due to a variety of reasons only 58 actually attended a session. Due to the low numbers of completed in-person interventions, we offered to mail a copy of the personalized feedback with a facilitative guide to reading the feedback to those randomized to intervention but who did not complete the in-person intervention. Forty-eight participants were emailed and telephoned asking if they would like to receive the feedback. In total, 32 participants indicated interest in receiving the feedback by mail. Overall, 90 (84.9%) of participants randomly assigned to the intervention condition received either the in-person or mailed feedback. Participants randomized to intervention condition completed a post-intervention satisfaction assessment after receiving the in-person intervention (or a link to the survey after receiving the mailed feedback). Follow-up data was provided by 181 (85.4%) participants at three months and 175 (82.5%) participants at six months. Students were compensated $10 for completing screening, $25 for baseline, $10 for post-intervention assessment, and $30 for 3- and 6-month follow-ups.
Measures
Two measures of marijuana use were used for the main outcomes, total number of days used marijuana in the past 30 and typical number of joints smoked in a typical week. The total number of days with marijuana use in past 30 days was assessed using a modified 30-day Timeline Followback (Sobell & Sobell, 2000). We also adapted the Daily Drinking Questionnaire (Collins, Park, & Marlatt, 1985) to assess number of joints smoked during a typical week during the past 60 days.
Marijuana-related consequences were assessed with a modified version of the Rutger’s Marijuana Problem Index (RMPI: White, Labouvie, & Papadaratsakis, 2005). Respondents were asked 18 items and to indicate how many times, from 1 (never) to 5 (more than 10 times), during the previous sixty days they experienced these negative consequences while using marijuana or as a result of marijuana use (Simons & Carey, 2000; White et al., 2005). Because the RMPI was directly adapted from the Rutgers Alcohol Problem Index (White & Labovie, 1989), many of the specific effects of marijuana use are not captured by the RMPI. To capture additional experiences unique to the physical and motivational effects of marijuana, ten items were identified by the investigators based on previous work with this population and added (e.g., had intense anxiety or panic attacks, had a cough, had lower motivation to do things). Consequences were coded as 0 (not experienced) or 1 (experienced at least once in last sixty days). A total consequences score was created by summing the twenty-eight consequence scores together.
Intervention
The in-person personalized feedback intervention was adapted from the Teen Marijuana Check-Up (Walker et al., 2010; Swan et al., 2008) and a previous web-based personalized feedback intervention (Lee et al., 2010) and consisted of a one-hour intervention designed to provide the opportunity to discuss the student’s marijuana use and review personalized graphic feedback. Facilitators were instructed to use motivational interviewing principles (Miller & Rollnick, 2002). While the layout of the feedback was consistent across participants, individual content within domains on the feedback was directly tailored to the individual based on his/her survey responses and the conversation was inherently tailored to each participant’s unique reaction to the feedback and his or her concerns, questions, and goals.
The personalized graphic feedback illustrated the impact of marijuana use in multiple domains to facilitate conversations about patterns of use and related consequences, including information regarding participants’ typical pattern of marijuana use (i.e., frequency, quantity, peak occasion, timing of use during the day, and perceived time spent high) and comparison to peers. Students’ self-reported reasons for using marijuana were reviewed. Social/personal, academic/cognitive, and physical/health consequences reported by the student were presented, followed by criteria endorsed by participants reflective of risk for cannabis abuse and/or cannabis dependence. Information was provided detailing estimates of how much students spend on marijuana in a given year, how much of their available spending money is directed toward marijuana, and other possible items that could be purchased with the same amount of money. Perceived costs and benefits of stopping or reducing use was reviewed, followed by feedback about self-reported confidence (or lack of confidence) to avoid smoking in certain situations. Feedback was also provided on family history risk. Students also received feedback on alcohol use, frequency of other drug use, and instances of combining other substances with marijuana such that interaction risks could be described. The final two sections of the feedback were dedicated to exploring students’ social networks and goals for the next year. Related to social networks students listed up to 6 people that they could count on for support, considered if the person knew about their marijuana use, and considered how the person felt about their marijuana use (or would feel about it). Finally, their five most important goals were listed and students were asked to rate how marijuana use affects goal attainment and how reducing marijuana use may positively or negatively affect attainment. At the end of the feedback session, students could ask questions and discuss goals.
Intervention Facilitator Training, Supervision, and Treatment Fidelity
Trained doctoral-level graduate students and doctoral-level professionals provided the in-person personalized feedback interventions. All facilitators participated in a two-day training, read supplemental materials, and attended weekly group and ongoing individual supervision. Feedback from the Motivational Interviewing Treatment Integrity coding system (MITI, Moyers, Martin, Manuel, Hendrickson, & Miller, 2005) was used to assess fidelity.
All sessions were audio-recorded and rated for adherence and competence by trained coders supervised by the investigators. Sessions were rated using the MITI (Moyers et al., 2005) by a team of supervised graduate and undergraduate students for interviewer global ratings (empathy, MI spirit) as well as behaviors (MI adherent and non-adherent statements, open and closed questions, and simple and complex reflections). Inter-rater reliability for coders was high (Intraclass correlations’ ranged from .91 – .95) for a majority of the behavioral counts, however simple reflections was .64. Reliability for global scores was lower (.43 for empathy and .50 for spirit), which is not uncommon often due to restricted range (e.g., Moyers et al., 2005). Facilitator adherence for each of the global codes exceeded beginning competency criteria (Empathy, M = 5.47, SD =.61 and Spirit, M = 5.38, SD =.69).
Data Analyses
Each of the three primary outcomes are types of count variables (i.e., they reflect the total number of something – either days, joints, or problems). Count variables can only assume nonnegative integer values, whereas the normal distribution underlying ordinary least squares regression and ANOVA models assumes all real values, extending theoretically to negative infinity.1 The most common method for addressing potential skew in these types of variables is to transform the outcome (e.g., log or square-root). However, these transformations are often unsuccessful with integer-valued data such as counts, as many observations assume identical values, and statistical research has shown that OLS regression yields biased results with count outcomes, even using a log transformation (King, 1988).
Alternative count regression models include Poisson and negative binomial regression and in the presence of many zeroes, zero-inflated and hurdle models (see, e.g., Atkins & Gallop, 2007; Hilbe, 2007; Neal & Simons, 2007). The present analyses used a negative binomial regression model, which allows for over-dispersion in count outcomes relative to a Poisson model. Our primary model was:
| (1) |
That is, the outcome at either three or six months was modeled by the outcome at the start of the study and dummy-coded indicator variable for group (Control – 0, Intervention – 1). The negative binomial uses a log link function, and similar to logistic regression, raw coefficients are exponentiated (i.e., raised to the base e) and interpreted as rate ratios. Rate ratios are somewhat similar to odds ratios from logistic regression in that a value of 1 signifies no difference. Values above or below one are interpreted as a percentage increase or decrease in the rate of the outcome, respectively. Models including both three and six month outcomes simultaneously were examined using mixed models (i.e., hierarchical generalized linear models, Raudenbush & Bryk, 2002). Substantive conclusions were identical with what was reported here, and thus, the simpler models that were fit separately by assessment point are reported below. Analyses adhered to the intent-to-treat principle and analyzed all available data treating individuals as randomized, regardless of treatment received. Treatment noncompliance and several other considerations were explored in secondary sensitivity analyses. All analyses were done in R v2.12.0 (R Development Core Team, 2010) and made use of the glm.nb() function for negative binomial regression in the MASS package (Venables & Ripley, 2002).
Results
Descriptive Information and Baseline Equivalence
Table 1 reports descriptive information for each outcome by treatment group and assessment period. At baseline, participants reported smoking marijuana on approximately half of the days out of the last month, though with notable variability (and some participants reported smoking every day). Participants reported smoking 8–9 joints in a typical week and reported roughly 10 consequences due to smoking marijuana, at baseline. Baseline data including demographics and treatment outcomes were examined for balance between the treatment groups. Overall, randomization appeared to yield comparable groups at baseline on measured covariates.
Table 1.
Descriptive Statistics for Marijuana Use and Consequences
| Group | Time | n | M | SD | Median |
|---|---|---|---|---|---|
| Days using marijuana in past 30 days | |||||
| Control | Baseline | 106 | 15.64 | 8.8 | 14.00 |
| 3 month | 93 | 14.87 | 10.8 | 12.00 | |
| 6 month | 84 | 11.68 | 11.1 | 8.00 | |
| Intervention | Baseline | 106 | 16.52 | 8.2 | 15.00 |
| 3 month | 86 | 14.06 | 10.1 | 13.00 | |
| 6 month | 89 | 13.21 | 10.6 | 11.00 | |
| Number of joints smoked in typical week | |||||
| Control | Baseline | 106 | 8.29 | 9.5 | 4.25 |
| 3 month | 95 | 8.45 | 9.8 | 5.00 | |
| 6 month | 87 | 7.47 | 10.7 | 3.50 | |
| Intervention | Baseline | 105 | 9.35 | 9.8 | 7.00 |
| 3 month | 89 | 6.91 | 8.2 | 4.00 | |
| 6 month | 90 | 7.26 | 8.4 | 4.00 | |
| Number of marijuana related problems | |||||
| Control | Baseline | 102 | 10.38 | 5.9 | 10.50 |
| 3 month | 90 | 8.67 | 6.0 | 8.00 | |
| 6 month | 83 | 6.75 | 6.5 | 6.00 | |
| Intervention | Baseline | 106 | 10.45 | 4.9 | 10.00 |
| 3 month | 87 | 7.84 | 5.0 | 7.00 | |
| 6 month | 82 | 6.54 | 5.3 | 6.00 | |
Baseline Differences with Respect to Intervention Completion
No significant differences were found in baseline marijuana use (i.e., number of days used marijuana or number of typical joints smoked per week) between those who attended the intervention compared to those who did not attend, however those who did attend the session on average reported more marijuana-related consequences at baseline (M = 11.36, SD = 4.62) compared to those who did not attend (M = 8.84, SD = 4.57, p < .05). There were no baseline differences in marijuana use or consequences among those electing to receive feedback in the mail compared to those who did not.
Intent to Treat Analyses
Negative binomial regression models were used for inferential statistics – to examine whether the descriptive differences noted above met criteria for statistical significance. Table 2 reports rate ratios (RR) and 95% CI for RR for intervention effects at three and six months for each outcome. At three months, intervention participants reported 24% fewer joints smoked per week relative to control participants, but the groups were not statistically different at six months. Similarly, there was a trend for intervention participants reporting 10% fewer marijuana problems relative to control participants at three months, which similarly was not statistically significant at six months. Reported thirty day use was similar across groups at both three and six months, after controlling for baseline use.
Table 2.
Rate Ratio Differences Between Intervention and Control Group Fitted from Negative Binomial Model for Marijuana Use and Consequences.
| Fixed Effect | 3 month
|
6 month
|
||||
|---|---|---|---|---|---|---|
| RR | 95% Confidence Interval
|
RR | 95% Confidence Interval
|
|||
| Lower limit | Upper limit | Lower limit | Upper limit | |||
| Days using marijuana in past 30 days | ||||||
| Intercept | 4.37* | 3.47 | 5.50 | 4.18* | 2.85 | 6.13 |
| Baseline | 1.07* | 1.06 | 1.08 | 1.06* | 1.04 | 1.08 |
| Intervention | 0.96 | 0.80 | 1.15 | 1.11 | 0.85 | 1.43 |
| Number of joints smoked in typical week | ||||||
| Intercept | 3.48* | 2.87 | 4.22 | 3.16* | 2.34 | 4.27 |
| Baseline | 1.08* | 1.06 | 1.09 | 1.07* | 1.05 | 1.08 |
| Intervention | 0.76* | 0.60 | 0.96 | 1.03 | 0.73 | 1.46 |
| Number of marijuana related problems | ||||||
| Intercept | 4.41* | 3.52 | 5.54 | 2.63* | 1.88 | 3.69 |
| Baseline | 1.06* | 1.04 | 1.08 | 1.08* | 1.05 | 1.10 |
| Intervention | 0.90‡ | 0.76 | 1.07 | 1.15 | 0.90 | 1.47 |
Note. RR = rate ratio
p < .10,
p < .05
Sensitivity Analyses
Several considerations were examined in sensitivity analyses. As noted earlier, only 58 participants attended an intervention session. To examine whether treatment effects were stronger for treatment compliers, secondary analyses were run in which the group dummy-variable was shifted to record treatment complier vs. control or treatment non-complier. The conclusions of these analyses were largely in line with the ITT analyses, although some effects were a bit stronger (e.g., treatment effect for consequences at three months: RR = 0.82, 95% CI = 0.68, 0.99, p < .05). In addition, the treatment effect for number of joints smoked at six months was notably lower relative to ITT analyses but the confidence interval was quite wide (RR = 0.45, 95% CI = 0.14, 1.47, p = .22). A second issue was that at some time points there were notable numbers of zeroes on some outcomes. Although negative binomial regression can fit count distributions with many zeroes, analyses were re-run using hurdle models, that include two submodels: a) a logistic model for zero vs. not zero, and b) a (truncated) count model for nonzero outcomes. Substantive results were similar to those found with negative binomial regression.
Discussion
The present research is one of only a handful of RCTs evaluating brief feedback-based interventions for marijuana use among young adults. It builds on previous work evaluating web-based feedback which demonstrated efficacy only among subgroups of college students (i.e., no main effects; Lee et al., 2010). Findings from the present study suggest more encouraging results may be attributed to in-person therapist delivered feedback. Specifically, while intervention participants did not differ from control participants in the number of days they used marijuana, they reported smoking fewer joints per week at the three month follow-up. Differences were no longer evident at six-month follow-up. Thus, the present research provides support for short-term efficacy of in-person therapist delivered feedback in reducing the overall amount of marijuana used but no support for reducing daily frequency and no support for longer term efficacy.
There are several possibilities that could account for the absence of effects at six months. First and foremost, it may be unreasonable to expect long-lasting effects of a single short feedback session in reducing marijuana use in this population. Over time, the effects of this single session may wear off as thoughts and motivations inspired by the intervention become less salient. This might suggest a need for either more intensive multi-session approaches or the addition of one or more booster sessions. The intervention effects at three-month follow-up could be interpreted as a temporary augmentation of a natural decline in use. This does not diminish the significance of the intervention effects but it does suggest that other things may also be affecting marijuana use, including assessment reactivity (e.g., Clifford & Maisto, 2000; Clifford, Maisto, & Davis, 2007; Miller et al., 2001; McCambridge & Day 2008; Walters, Vader, Harris, & Jouriles, 2009) or seasonal or situational factors impacting use (e.g., Martens, Dams-O’Connor, & Kilmer, 2007; Martens, Kilmer, Beck, & Zamboanga, 2010). For example, variations in use of substances over the course of a year have been documented (e.g., Del Boca, Darkes, Greenbaum, & Goldman, 2004), and it is possible that marijuana use has a situational component to it such that actively being in the college setting provides different opportunity and access than would be afforded during the summer (when, many students move back with parents).
Another issue worthy of discussion is the attendance rate. While 85% of the intervention participants received feedback, only 55% attended the in-person session. Results of sensitivity analyses suggested better effect in reducing problems among those who attended the in-person session. Effects were actually reduced for joints per week and were associated with large confidence intervals, making this difficult to interpret. On the one hand, finding significant results even with relatively low compliance is encouraging. On the other hand, low compliance raises additional questions. As a general rule it can be challenging to get non-treatment seeking, non-mandated individuals to attend an intervention (particularly when recruited through the general registrar’s list), even when offered monetary incentives. In our experience in previous trials we have worked hard to get 70–80% of heavy drinking students to come in for in-person interventions. It may be that frequent marijuana users are less motivated to attend in-person interventions. In combination these issues suggest a need to compare alternative delivery strategies and/or recognize that additional incentives may be needed to recruit non-treatment seeking frequent marijuana users. It might also suggest that campuses considering adopting brief intervention approaches for marijuana use might consider personalized feedback as an option among potential sanction for violating substance use policy.
There are a number of future directions to consider based on the present findings. Some of these stem from limitations in this study. While the present research established support for the in-person motivational personalized feedback intervention relative to no intervention, the absence of a separate intervention condition precludes our ability to draw firm conclusions about our intervention relative to other possible interventions. Future research is needed to evaluate comparative efficacy of alternative interventions to allow definitive conclusions about this or any other specific intervention relative to assessment, general intervention effects, or other non-specific factors. It would worthwhile to consider whether intervention effects would vary between same-age college and non-college users. Additionally, unlike consumption of alcohol, marijuana’s current illicit status also raises concerns about what messages can be communicated about continued use (for those who choose to do so) in a college environment that do not seem to send “mixed messages” (particularly given state and federal laws, as well as any campus-specific policies). Unlike alcohol interventions that emphasize a blood alcohol content (BAC) for which those who make the choice to drink can do so in a less dangerous or less risky way, there are no identified guidelines with marijuana for a point at which consequences can be minimized and positives can be maximized. In addition, future trials in the college population may want to explicitly consider potential seasonal variability in use or assessment reactivity.
In conclusion, the propose research provides some support for in-person feedback-based brief interventions for frequent marijuana using college students. While more research is needed, we would tentatively endorse this approach for campuses considering options for responding to students who violate substance use policies related to marijuana.
Acknowledgments
The project described and manuscript preparation was supported by Award number R21DA025833 the National Institute on Drug Abuse. The content of this manuscript is solely the responsibility of the author(s) and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
We thank our project coordinator Theresa Walter; our study facilitators Irene Geisner, Brent Hopkins, Kelly Koo, Diane Logan, Mandy Owens, Andy Paves, Eric Pedersen, and Kaitlyn Taylor; Dr. Helene White for her input on the intervention and study design; and the participants who made this study possible.
Footnotes
Not surprisingly, in the current sample all outcomes demonstrated notable skew and significant departure from normality, tested via a Kolmogorov-Smirnoff test (all ps < .01)
References
- American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Fall 2011. Hanover, MD: American College Health Association; 2012. [Google Scholar]
- Atkins DC, Gallop RJ. Rethinking how family researchers model infrequent outcomes: A tutorial on count regression and zero-inflated models. Journal of Family Psychology. 2007;21:726–735. doi: 10.1037/0893-3200.21.4.726. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Stephens RS, Roffman R, Walker DD. Marijuana dependence and its treatment. Science and Practice Perspectives. 2007;4:4–16. doi: 10.1151/ascp07414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA. Subject reactivity effects and alcohol treatment outcome research. Journal of Studies on Alcohol. 2000;61:787–793. doi: 10.15288/jsa.2000.61.787. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA, Davis CM. Alcohol treatment research assessment exposure subject reactivity effects: part I. Alcohol use and related consequences. Journal of Studies on Alcohol and Drugs. 2007;68:519–528. doi: 10.15288/jsad.2007.68.519. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J, Greenbaum PE, Goldman MS. Up Close and Personal: Temporal Variability in the Drinking of Individual College Students During Their First Year. Journal of Consulting and Clinical Psychology. 2004;72:155–164. doi: 10.1037/0022-006X.72.2.155. [DOI] [PubMed] [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, Liddle H, Titus JC, Kaminer Y, Webb C, Hamilton N, Funk R. The Cannabis Youth Treatment (CYT) Study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Grossbard JR, Mastroleo NR, Kilmer JR, Lee CM, Turrisi R, Larimer ME, Ray A. Substance use patterns among first-year college students: Secondary effects of a combined alcohol intervention. Journal of Substance Abuse Treatment. 2010;39:384–390. doi: 10.1016/j.jsat.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbe JM. Negative Binomial Regression. New York: Cambridge University Press; 2007. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2010: Volume II, College students and adults ages 19–50. Ann Arbor: Institute for Social Research, The University of Michigan; 2011. [Google Scholar]
- King G. Statistical Models for Political Science Event Counts: Bias in Conventional Procedures and Evidence for The Exponential Poisson Regression Model. American Journal of Political Science. 1988;32:838–863. [Google Scholar]
- Lee CM, Neighbors C, Kilmer JR, Larimer ME. A brief, web-based personalized feedback selective intervention for college student marijuana use: A randomized clinical trial. Psychology of Addictive Behaviors. 2010;24(2):265–273. doi: 10.1037/a0018859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynskey M, Hall W. The effects of adolescent cannabis use on educational attainment: A review. Addiction. 2000;95:1621–1630. doi: 10.1046/j.1360-0443.2000.951116213.x. [DOI] [PubMed] [Google Scholar]
- Martens MP, Dams-O’Connor K, Kilmer JR. Alcohol and drug abuse among athletes: Prevalence, etiology, and interventions. In: Tenenbaum G, Ecklund RC, editors. Handbook of Sports and Exercise Psychology. 3. New York: John Wiley & Sons, Inc; 2007. pp. 859–878. [Google Scholar]
- Martens MP, Kilmer JR, Beck NC, Zamboanga BL. The efficacy of a targeted personalized drinking feedback intervention among intercollegiate athletes: A randomized controlled trial. Psychology of Addictive Behaviors. 2010;24:660–669. doi: 10.1037/a0020299. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Day M. Randomized controlled trial of the effects of completing the Alcohol Use Disorders Identification Test questionnaire on self-reported hazardous drinking. Addiction. 2008;103:241–248. doi: 10.1111/j.1360-0443.2007.02080.x. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: Results from a multi-site cluster randomized trial. Addiction. 2004;99:39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. New York: Guilford; 2002. [Google Scholar]
- Miller WR, Toscova RT, Miller JH, Sanchez V. A theory-based motivational approach for reducing alcohol/drug problems in college. Health Education & Behavior. 2001;27:744–759. doi: 10.1177/109019810002700609. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. NIH Publication No. 02-3859. 2002. NIDA Research Report – Marijuana Abuse. [Google Scholar]
- Neal DJ, Simons JS. Inference in regression models of heavily skewed alcohol use data: A comparison of ordinary least squares, generalized linear models, and bootstrap resampling. Psychology of Addictive Behaviors. 2007;21:441–452. doi: 10.1037/0893-164X.21.4.441. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. [Software] Vienna: R Foundation for Statistical Computing; 2010. http://www.R-project.org. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and data analysis methods. 2. Thousand Oaks: Sage Publications; 2002. [Google Scholar]
- Roebuck MC, French MT, Dennis ML. Adolescent marijuana use and school attendance. Economics of Education Review. 2004;23:133–141. doi: 10.1016/S0272-7757(03)00079-7. [DOI] [Google Scholar]
- Schulenberg JE, Merline AC, Johnston LD, O’Malley PM, Bachman JG, Laetz VB. Trajectories of marijuana use during the transition to adulthood: The big picture based on national panel data. Journal of Drug Issues. 2005;35:255–280. doi: 10.1177/002204260503500203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association; 2000. Alcohol Timeline Followback (TLFB) pp. 477–479. [Google Scholar]
- Solowij N. Cannabis and Cognitive Functioning. Cambridge, England: Cambridge University Press; 1998. [Google Scholar]
- Simons J, Carey KB. Attitudes toward marijuana use and drug-free experience: Relationships with behavior. Addictive Behaviors. 2000;25:323–331. doi: 10.1016/S0306-4603(99)00016-7. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, Fearer SA, Williams C, Burke RS. The Marijuana Check-up: Promoting change in ambivalent marijuana users. Addiction. 2007;102(6):947–957. doi: 10.1111/j.1360-0443.2007.01821.x. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-41, HHS Publication No. (SMA) 11-4658. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- Swan M, Schwartz S, Berg B, Walker D, Stephens R, Roffman R. The teen marijuana check-up: An in-school protocol for eliciting voluntary self-assessment of marijuana use. Journal of Social Work Practice In The Addictions. 2008;8:284–302. doi: 10.1080/15332560802223305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RD, Poulton R, Moffitt ET, Ramankutty P, Sears RM. The respiratory effects of cannabis dependence in young adults. Addiction. 2000;95:1669–1677. doi: 10.1046/j.1360-0443.2000.951116697.x. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Ellickson PL, El OM, Martino SC, Klein DJ. Substance use trajectories from early adolescence to emerging adulthood: A comparison of smoking, binge drinking, and marijuana use. Journal of Drug Issues. 2005;35:307–332. [Google Scholar]
- Venables WN, Ripley BD. Modern Applied Statistics with S. 4. Springer; New York: 2002. [Google Scholar]
- Walker DD, Stephens RS, Roffman R, Towe S, DeMarce J, Lozano B, Berg B. Randomized controlled trial of motivational enhancement therapy with nontreatment-seeking adolescent cannabis users: A further test of the teen marijuana check-up. Psychology of Addictive Behaviors. 2011;25:474–484. doi: 10.1037/a0024076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Jouriles EN. Reactivity to alcohol assessment measures: an experimental test. Addiction. 2009;104:1305–1310. doi: 10.1111/j.1360-0443.2009.02632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW, Papadaratsakis V. Changes in substance use during the transition to adulthood: A comparison of college students and their noncollege age peers. Journal of Drug Issues. 2005;35:281–306. [Google Scholar]
- White HR, Morgan TJ, Pugh LA, Celinska K, Labouvie EW, Pandina RJ. Evaluating two brief substance-use interventions for mandated college students. Journal of Studies on Alcohol. 2006;67:309–317. doi: 10.15288/jsa.2006.67.309. [DOI] [PubMed] [Google Scholar]