Abstract
Background:
A proliferating trichilemmal cyst (PTC) is an uncommon, rapidly-reproducing cutaneous epithelial cyst, differentiating from the isthmic portion of the outer hair root sheath. It is usually described as a benign tumor, but malignant transformation has been reported and is then denominated as a malignant proliferating trichilemmal tumor. Ki67 immunostaining has been used as a methodology for the evaluation of tumor grade in other tumors, due to its distinctive reaction patterns which exclusively involve proliferating cells.
Objectives:
(1) To report the incidence of cases of PTCs in a General Hospital during a 12 years period. (2) To determine the expression of ki67 using immunohistochemical staining. (3) To correlate ki67 reaction patterns with clinical prognosis.
Materials and Methods:
The dermatology department's files during a period of 12 years were reviewed; cases with a diagnosis of PTC were selected, and ki67 immunostaining was done when enough biological material was available.
Results:
A total of 15 cases with a diagnosis of PTC were identified. In 12 cases, ki67 immunostaining was carried out. In 9 of the 12 cases, ki67 was observed in the basal cells of the cystic epithelium, one case was moderately positive in palisading epithelial cells; in the other two cases ki67 immunostaining was negative. Clinical follow-up was done and revealed that no patient had local recurrence in 5 years after surgical removal of PTC. We therefore consider this immunostaining technique is probably correlated with low recurrence potential.
Keywords: Hair follicle, ki67, pilar tumor, proliferating trichilemmal cyst
INTRODUCTION
A proliferating trichilemmal cyst (PTC),[1] is a rapidly-reproducing cutaneous epithelial cyst, differentiating from the isthmic portion of the outer hair root sheath.[2] These tumors are usually found on the scalps of women in their seventies and eighties.[3,4] It is frequently described as a benign neoplasm, but potential for malignant transformation has been reported.[5,6] Alternatively, some authors have recently suggested that PTC is a squamous cell carcinoma.[7,8,9,10] Nevertheless the malignant potential of these tumors is still debated[11] and new strategies for the evaluation of tumor grade are needed. On the other hand, major association between the presence of ki67 and the grade of malignancy has been observed in all tumors which have been studied by ki67 immunostaining. In addition, an obvious variation in the amount of ki67 within different tumor grades has been observed, showing that ki67 immunostaining may be of use in individual tumor diagnosis and prognosis.[12,13,14] Considering this information, we decided to review the incidence of PTC and the expression of ki67 using immunohistochemical staining in our patients during a period of 12 years.
MATERIALS AND METHODS
This proposed study was reviewed and approved by the Ethics Committee of the Institution. In accordance with the Helsinki declaration, the Dermatology Department's files during a period of 12 years (1996-2008) were reviewed and the cases classified. Cases with a diagnosis of PTC were selected, but cases where sufficient biological material was not available for histological diagnosis and evaluation were excluded. In the remaining cases, the biological material was reviewed independently by one general pathologist and one dermatophatologist, differential diagnosis with other tumors such as malignant proliferating trichilemmal tumor (PTT), squamous cell carcinoma and trichilemmal carcinoma was performed.[1,15] Both agree that all the cases correspond to PTC, and when enough biological material was available, ki67 immunostaining was carried out.
RESULTS
We found 15 cases corresponding with clinical and histopathological diagnosis of PTC, 11 (73.33%) women and 4 (26.66%) men. The average age was 56.60 years. 13 cases (86.66%) tumors were located on the scalp [Figure 1]; one lesion was in the trunk and another one in the neck. 5 (33.33%) tumors were cystic in appearance, 10 (66.66%) were indurate tumors; the smallest was of 1 cm × 1.5 cm and the biggest was 11.5 cm × 8 cm in diameter. Review of the clinical files revealed that no patient had any recurrence within 5 years post-surgical follow-up.
Figure 1.

A multilobulated tumor is observed in the scalp
Microscopic examination of all the tumors revealed variously shaped and sized lobules formed by aggregations of squamous epithelial cells and peripherally-palisading epithelial cells maturing into large pale-staining cells displaying an abrupt trichilemmal type of keratinization [Figure 2]. The mitotic activity and necrosis were variable, but all tumors belonged to group I in accord with the classification proposed by Ye et al.[16] None of the tumors presented infiltrative margins or metastasis. In 12 (80%) cases, ki67 immunostaining was performed. In nine of these cases, ki67 immunostaining was observed in the basal cells of the cystic epithelium [Figure 3], without evidence of a malignant proliferation pattern. One case was moderately positive in palisading epithelial cells. Finally in the other two cases, ki67 immunostaining was negative.
Figure 2.
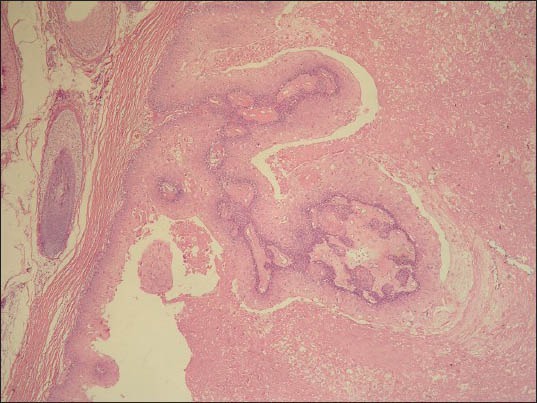
Panoramic view of the lesion, showing lobules formed by aggregations of squamous epithelial cells, peripherally palisading epithelial cells maturing into large pale-staining cells displaying an abrupt trichilemmal type of keratinization
Figure 3.
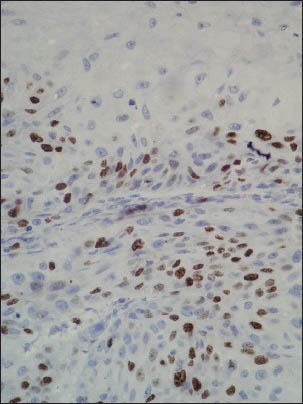
Immunohistochemical staining with ki67 observed in the palisading epithelial basal cells of the cystic epithelium
DISCUSSION
PTCs display structures typical of pilar cysts, but additionally exhibit extensive epithelial proliferation, variable cytological atypia and mitotic activity. The definition of proliferation potential and consequential malignant development should be considered in PTCs in order to offer adequate treatment with extensive local excision and long term follow-up, mainly in large and long-standing lesions.[17]
In this series of cases, immunohistochemical staining with ki67 was observed mostly in the palisading epithelial cells of the cystic epithelium, which suggested that only basal epithelial cells were proliferating in these tumors. This correlated with the clinical evolution observed in our patients without tumor recurrence and suggested an association between this immunostaining distribution and low recurrence potential. In contrast, Park et al.,[18] studied ki67 immunostaining in one patient, described as a case of malignant PTT. This patient showed at the end of his evolution multiple distant metastases, during a few years consecutive histological specimens revealed a PTT with increasing nuclear atypia. Serial specimens showed growing Ki-67 positivity as the extent of the tumor progressed.
CONCLUSIONS
We believe ki-67 expression has a close relationship with the recurrence potential, but like carcinogenesis theory explains, multiple molecular changes are necessary for malignant development in PTCs. Supporting this idea, analyses on the p53 mutation suggested that an important event responsible for the progression from the pre-existing PTC to the trichilemmal carcinoma could be bi-allelic loss of wild-type p53.[19]
In relation to clinical evolution, PTC recurrence was not observed in our cases, possibly because we have considered PTCs as low-grade malignant tumors with potential to malignant transformation. Consequently the surgical treatment performed comprised wide local excision with 1 cm margin of normal tissue to prevent recurrence, as suggested in the latest publication.[20] Consequently, we believe that the ki67 reaction patterns are in fact directly related to the probability of malignant development. Nevertheless our sample did not show extensive ki67 immunostaining, this work clearly indicated that low extension of ki67 immunostaining was directly related to a good prognosis and the absence of recurrence or malignant extension, while the literature reports that extensive ki67 patterns are associated with malignancy. Additional studies on other series will help to reinforce the prognostic value of ki67 immunostaining in PTCs.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Headington JT. Tumor of the hair follicle. Am J Pathol. 1976;85:480–514. [PMC free article] [PubMed] [Google Scholar]
- 2.Sau P, Graham JH, Helwig EB. Proliferating epithelial cysts. Clinicopathological analysis of 96 cases. J Cutan Pathol. 1995;22:394–406. doi: 10.1111/j.1600-0560.1995.tb00754.x. [DOI] [PubMed] [Google Scholar]
- 3.Erdem H, Yildirim U, Uzunlar AK, Sahiner C, Ozcelik D, Toplu G. Posttraumatic giant proliferating trichilemmal cysts on the parietal region of the scalp. Indian J Dermatol Venereol Leprol. 2011;77:707–9. doi: 10.4103/0378-6323.86488. [DOI] [PubMed] [Google Scholar]
- 4.Sethi S, Singh UR. Proliferating trichilemmal cyst: Report of two cases, one benign and the other malignant. J Dermatol. 2002;29:214–20. doi: 10.1111/j.1346-8138.2002.tb00252.x. [DOI] [PubMed] [Google Scholar]
- 5.Mathis ED, Honningford JB, Rodriguez HE, Wind KP, Connolly MM, Podbielski FJ. Malignant proliferating trichilemmal tumor. Am J Clin Oncol. 2001;24:351–3. doi: 10.1097/00000421-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Goyal S, Jain BB, Jana S, Bhattacharya SK. Malignant proliferating trichilemmal tumor. Indian J Dermatol. 2012;57:50–2. doi: 10.4103/0019-5154.92679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernández-Figueras MT, Casalots A, Puig L, Llatjós R, Ferrándiz C, Ariza A. Proliferating trichilemmal tumour: P53 immunoreactivity in association with p27Kip1 over-expression indicates a low-grade carcinoma profile. Histopathology. 2001;38:454–7. doi: 10.1046/j.1365-2559.2001.01149.x. [DOI] [PubMed] [Google Scholar]
- 8.Casas JG, Woscoff A. Giant pilar tumor of the scalp. Arch Dermatol. 1980;116:1395. [PubMed] [Google Scholar]
- 9.Folpe AL, Reisenauer AK, Mentzel T, Rütten A, Solomon AR. Proliferating trichilemmal tumors: Clinicopathologic evaluation is a guide to biologic behavior. J Cutan Pathol. 2003;30:492–8. doi: 10.1034/j.1600-0560.2003.00041.x. [DOI] [PubMed] [Google Scholar]
- 10.Chaichamnan K, Satayasoontorn K, Puttanupaab S, Attainsee A. Malignant proliferating trichilemmal tumors with CD34 expression. J Med Assoc Thai. 2010;93(Suppl 6):S28–34. [PubMed] [Google Scholar]
- 11.Noto G, Pravatà G, Aricò M. Malignant proliferating trichilemmal tumor. Am J Dermatopathol. 1997;19:202–4. doi: 10.1097/00000372-199704000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Duchrow M, Gerdes J, Schlüter C. The proliferation. associated Ki-67 protein: Definition in molecular terms. Cell Prolif. 1994;27:235–42. doi: 10.1111/j.1365-2184.1994.tb01421.x. [DOI] [PubMed] [Google Scholar]
- 13.Hall PA, Levison DA. Review: Assessment of cell proliferation in histological material. J Clin Pathol. 1990;43:184–92. doi: 10.1136/jcp.43.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ross W, Hall PA. Ki67: From antibody to molecule to understanding? Clin Mol Pathol. 1995;48:M113–7. doi: 10.1136/mp.48.3.m113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mane DR, Kale AD, Hallikerimath S, Angadi P, Kotrashetti V. Trichilemmal carcinoma associated with xeroderma pigmentosa: Report of a rare case. J Oral Sci. 2010;52:505–7. doi: 10.2334/josnusd.52.505. [DOI] [PubMed] [Google Scholar]
- 16.Ye J, Nappi O, Swanson PE, Patterson JW, Wick MR. Proliferating pilar tumors: A clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol. 2004;122:566–74. doi: 10.1309/0XLEGFQ64XYJU4G6. [DOI] [PubMed] [Google Scholar]
- 17.López-Ríos F, Rodríguez-Peralto JL, Aguilar A, Hernández L, Gallego M. Proliferating trichilemmal cyst with focal invasion: Report of a case and a review of the literature. Am J Dermatopathol. 2000;22:183–7. doi: 10.1097/00000372-200004000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Park BS, Yang SG, Cho KH. Malignant proliferating trichilemmal tumor showing distant metastases. Am J Dermatopathol. 1997;19:536–9. doi: 10.1097/00000372-199710000-00109. [DOI] [PubMed] [Google Scholar]
- 19.Takata M, Rehman I, Rees JL. A trichilemmal carcinoma arising from a proliferating trichilemmal cyst: The loss of the wild-type p53 is a critical event in malignant transformation. Hum Pathol. 1998;29:193–5. doi: 10.1016/s0046-8177(98)90234-9. [DOI] [PubMed] [Google Scholar]
- 20.Satyaprakash AK, Sheehan DJ, Sangüeza OP. Proliferating trichilemmal tumors: A review of the literature. Dermatol Surg. 2007;33:1102–8. doi: 10.1111/j.1524-4725.2007.33225.x. [DOI] [PubMed] [Google Scholar]


