Abstract
Background
Patients with traumatic brain injury (TBI) face increased risk of stroke. Whether acupuncture can help to protect TBI patients from stroke has not previously been studied.
Methods
Taiwan's National Health Insurance Research Database was used to conduct a retrospective cohort study of 7409 TBI patients receiving acupuncture treatment and 29,636 propensity-score-matched TBI patients without acupuncture treatment in 2000–2008 as controls. Both TBI cohorts were followed until the end of 2010 and adjusted for immortal time to measure the incidence and adjusted hazard ratios (HRs) with 95% confidence intervals (CIs) of new-onset stroke in the multivariable Cox proportional hazard models.
Results
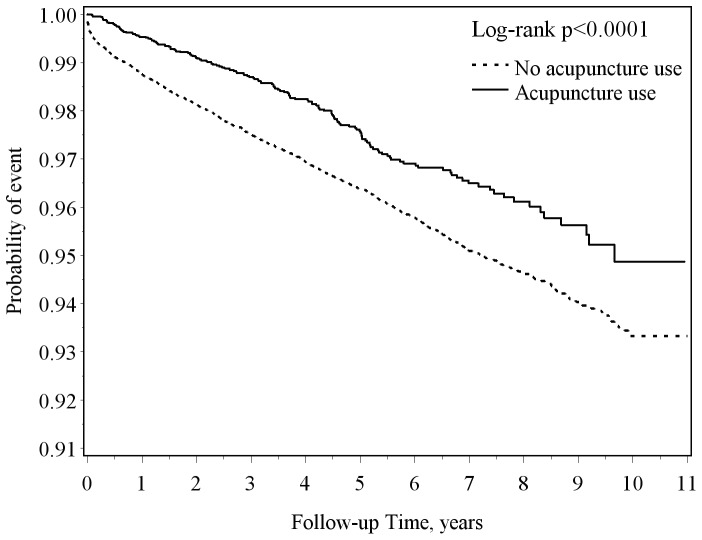
TBI patients with acupuncture treatment (4.9 per 1000 person-years) had a lower incidence of stroke compared with those without acupuncture treatment (7.5 per 1000 person-years), with a HR of 0.59 (95% CI = 0.50–0.69) after adjustment for sociodemographics, coexisting medical conditions and medications. The association between acupuncture treatment and stroke risk was investigated by sex and age group (20–44, 45–64, and ≥65 years). The probability curve with log-rank test showed that TBI patients receiving acupuncture treatment had a lower probability of stroke than those without acupuncture treatment during the follow-up period (p<0.0001).
Conclusion
Patients with TBI receiving acupuncture treatment show decreased risk of stroke compared with those without acupuncture treatment. However, this study was limited by lack of information regarding lifestyles, biochemical profiles, TBI severity, and acupuncture points used in treatments.
Introduction
Traumatic brain injury (TBI) is a common cause of disability and death in every age group and both sexes worldwide [1]–[3]. Health problems after TBI include neurologic deficit, cognitive impairment, psychiatric illness, poor social functioning, and other significant adverse outcomes such as brain tumors and mortality [2], [4]–[7]. This burden of disease calls for further investigation to prevent and treat complications after TBI [8].
Stroke is the second leading cause of death worldwide and the leading cause of acquired disability in adults in most regions [9]. An international multicenter study has identified cardiac diseases, hypertension, diabetes, smoking, alcohol intake, unhealthy diet, abdominal obesity, lack of exercise, psychosocial stress and depression as risk factors associated with 90% of stroke risk [10]. Prevention is an important way to reduce stroke incidence and mortality.
An increased risk of stroke among individuals who survive TBI has been documented [11], [12]. Acupuncture is a traditional Chinese medicine (TCM) treatment that is commonly used in Taiwan [13]–[17]. Acupuncture has been found to improve cognition and sleep quality for patients with TBI [18], and our previous report found that patients with TBI who receive acupuncture treatment had reduced use of emergency care and hospitalization in the first year after injury [19]. Acupuncture has been documented as part of rehabilitation for patients with TBI [20]. However, whether acupuncture is effective in preventing stroke for patients with TBI is unknown. This study investigates the effectiveness of acupuncture in decreasing stroke risk among patients with TBI using multivariate and immortal time adjustment in a nationwide population-based cohort study.
Methods
Ethics Statement
Insurance reimbursement claims used in this study were from Taiwan's National Health Insurance Research Database, which is available for public access. This study was conducted in accordance with the Helsinki Declaration. To protect personal privacy, the electronic database was decoded with patient identifications scrambled for further public access for research. Although National Health Research Institutes regulations do not require informed consent due to decoded and scrambled patient identification, this study was approved by Taiwan's National Health Research Institutes.
Study Design and Population
Taiwan's National Health Research Institutes set up the National Health Insurance Research Database to allow access to all medical claims for insured beneficiaries since 1996. With patient identification numbers scrambled, data files can be secured to protect patient privacy. Information available for this study included gender, birth date, disease codes, health care rendered, medicines prescribed, diagnoses for admissions and discharges, and medical institutions and physicians providing services. This database was described in detail in our previous studies [1]–[3], [19], [21]–[25].
From a longitudinal cohort population-based database of a randomly selected one million insured subjects in 2000, we identified persons aged ≥20 years old with newly diagnosed TBI who made visits for medical care in 2000–2008 as our eligible study patients. In order to confirm that all patients with TBI in our study were incident cases, only new-onset TBI cases were included in this study; people with previous medical records of TBI within five years before the index date were excluded. The diagnosis of TBI was validated in previous studies [1]–[3]. Overall, we identified 37,045 new-onset TBI survivors aged ≥20 years; 7409 of them had used at least two courses (one course including six consecutive treatments) of acupuncture after TBI. We compared TBI patients receiving at least two courses of acupuncture treatment with patients without acupuncture treatment. TBI patients with only one course of treatment were excluded from this study. Each TBI patient was either followed up from the index date until 31 December 2010 or was censored. The follow-up time, in person-years, was calculated for each TBI patient until the diagnosis of stroke or until being censored due to death, withdrawal from the insurance system or loss to follow-up. The non-acupuncture group included patients with TBI who did not have acupuncture treatment before the end-point of follow-up. The person-years of TBI patients with acupuncture were calculated from the beginning of receiving acupuncture treatment corrected by immortal time [26].
Criteria and Definition
We defined TBI according to the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM 800–805, 850–854) [1]–[3], [19]. The primary outcome as the incident event of stroke was defined as ICD-9-CM 430–438. Coexisting medical conditions – hypertension (ICD-9-CM 401–405), mental disorders (ICD-9-CM 290–319), diabetes (ICD-9-CM 250), ischemic heart disease (ICD-9-CM 410–414), hyperlipidemia (ICD-9-CM 272.0–272.4), migraine (ICD-9-CM 346), and epilepsy (ICD-9-CM 345) – were considered as confounding factors due to documented increased risk of stroke in patients with these coexisting medical conditions [10], [11], [27]. TCM physicians were defined as physicians licensed by Taiwan's Department of Health who practiced TCM in regulated clinics or hospitals. We calculated the density of TCM physicians (TCM physicians/10,000 persons) using the number of TCM physicians per 10,000 residents for each administrative unit. The first, second, and third tertiles were considered as areas with low, moderate, and high physician density.
We identified stroke-related medications such as anticoagulants, antiplatelet agents, and lipid-lowering agents as potential confounding factors in the association between acupuncture treatment and stroke. National Health Insurance-covered anticoagulant included warfarin, dabigatran, heparin, and enoxaparin. Antiplatelet agents included aspirin, dipyridamole, ticlopidine, cilostazol, clopidogrel, tirofiban, aggrenox, abciximab, and eptifibatide. Lipid-lowering agents included atorvastatin simvastatin, rosuvastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, vytorin (ezetimibe with simvastatin), gemfibrozil, and fenofibrate.
The selection of acupuncture point was determined by TCM doctors who made clinical assessment in accordance with TCM principles, such as the GV26 (Shuigou) point at the junction of the upper and middle third of the philtrum. [28] Acupuncturists used commercially available, single-use, sterile, and disposable stainless steel needles [18]. After the needles placed manually, they were left in place for around 15 minutes. All of this group of doctors obey these standard TCM guidelines to perform acupuncture treatments in the licensed clinical settings.
Statistical Analysis
To reduce confounding effects, we developed a non-parsimonious multivariable logistic regression model to estimate a propensity score for acupuncture treatment. Clinical significance guided the initial choice of covariates, which included age, sex, low-income status, density of TCM physicians, types of TBI, mental disorders, hypertension, diabetes mellitus, ischemic heart disease, hyperlipidemia, migraine, and epilepsy. We used a structured iterative approach to refine this logistic regression model to achieve balance of covariates within the matched pairs. We then matched (without replacement) patients who had acupuncture treatment to those who did not by using a greedy matching algorithm with a calliper width of 0·2 SD of the log odds of the propensity score. Nearest-neighbor algorithm was applied to construct matched pairs, assuming that the proportion of 0·95 to 1·0 is perfect.
The chi-square tests were used to analyze categorized data (age group, sex, low income, density of TCM physicians, types of TBI, mental disorders, hypertension, diabetes mellitus, ischemic heart disease, hyperlipidemia, migraine, epilepsy, anticoagulants, antiplatelet agents, lipid-lowering agents, and new-onset stroke events) between patients with TBI who had received acupuncture treatment and those who had not. The mean and standard deviation of age for TBI patients with and without acupuncture treatment was compared by t-tests. We performed the multivariable Cox proportional hazard model to analyze the adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) of stroke associated with acupuncture treatment in patients with TBI. All analyses were performed using Statistical Analysis Software version 9.1 (SAS Institute Inc., Cary, North Carolina, USA). A two-sided probability value of <0.05 was considered significant.
Results
After propensity-score matching procedure ( Table 1 ) there was no significant difference in age, sex, low income, area with TCM physician density, types of TBI, mental disorders, hypertension, diabetes, ischemic heart disease, hyperlipidemia, migraine and epilepsy between TBI patients with and without acupuncture treatment. Patients with acupuncture treatment had higher proportions of using anticoagulants (2.3% vs. 1.7%, p = 0.0003), antiplatelet agents (28.7% vs. 22.3%, p<0.0001), and lipid-lowering agents (24.7% vs. 18.4%, p<0.0001) compared with those had no acupuncture treatment. TBI patients who underwent acupuncture treatment had a lower proportion of new-onset stroke events than those without acupuncture treatment (2.2% vs. 4.2%, p<0.0001).
Table 1. Baseline characteristics and stroke events for traumatic brain injury patients with and without acupuncture treatment.
| Acupuncture | p-value | ||
| No (N = 29636) | Yes (N = 7409) | ||
| Sex | n (%) | n (%) | 1.00 |
| Female | 14056 (47.4) | 3514 (45.4) | |
| Male | 15580 (52.6) | 3895 (52.6) | |
| Age, years | 1.00 | ||
| 20–29 | 9068 (30.6) | 2267 (30.6) | |
| 30–39 | 5824 (19.7) | 1456 (19.7) | |
| 40–49 | 5544 (18.7) | 1386 (18.7) | |
| 50–59 | 3804 (12.8) | 951 (12.8) | |
| 60–69 | 2844 (9.6) | 711 (9.6) | |
| 70–79 | 2080 (7.0) | 520 (7.0) | |
| ≥80 | 472 (1.6) | 118 (1.6) | |
| Mean±SD | 42.6±17.1 | 42.5±16.9 | 0.52 |
| Low income | 1.00 | ||
| No | 29228 (98.6) | 7307 (98.6) | |
| Yes | 408 (1.4) | 102 (1.4) | |
| Density of TCM physicians | 1.00 | ||
| Low | 4352 (14.7) | 1088 (14.7) | |
| Moderate | 11744 (39.6) | 2936 (39.6) | |
| High | 13540 (45.7) | 3385 (45.7) | |
| Type of TBI | 1.00 | ||
| Mild | 12868 (43.4) | 3217 (43.4) | |
| Moderate | 5780 (19.5) | 1445 (19.5) | |
| Severe | 10988 (37.1) | 2747 (37.1) | |
| Coexisting medical conditions | |||
| Mental disorders | 2708 (9.1) | 677 (9.1) | 1.00 |
| Hypertension | 3084 (10.4) | 771 (10.4) | 1.00 |
| Diabetes mellitus | 1324 (4.5) | 331 (4.5) | 1.00 |
| Ischemic heart disease | 608 (2.1) | 152 (2.1) | 1.00 |
| Hyperlipidemia | 452 (1.5) | 113 (1.5) | 1.00 |
| Migraine | 124 (0.4) | 31 (0.4) | 1.00 |
| Epilepsy | 60 (0.2) | 15 (0.2) | 1.00 |
| Stroke-related medications | |||
| Anticoagulants | 493 (1.7) | 169 (2.3) | 0.0003 |
| Antiplatelet agents | 6617 (22.3) | 2127 (28.7) | <0.0001 |
| Lipid-lowering agents | 5462 (18.4) | 1826 (24.7) | <0.0001 |
| New stroke events | 1250 (4.2) | 163 (2.2) | <0.0001 |
During the follow-up period ( Table 2 ), TBI patients with acupuncture treatment (4.9 per 1000 person-years) had a lower incidence of new-onset stroke than those without acupuncture treatment (7.5 per 1000 person-years), with a HR of 0.59 (95% CI = 0.50–0.69) after adjustment for age, gender, low income, TCM physician density, type of TBI, diabetes mellitus, hypertension, hyperlipidemia, mental disorder, ischemic heart disease, migraine, epilepsy, anticoagulants, antiplatelet agents, and lipid-lowering agents. Among patients with TBI, the decreased risk of new-onset stroke associated with acupuncture treatment showed no significant gender difference in (men, HR = 0.57, 95% CI = 0.46–0.71; women, HR = 0.62, 95% CI = 0.48–0.79). The age stratified results showed that the adjusted HR of stroke associated with acupuncture treatment for TBI patients was the lowest in the younger group aged 20–44 years. The further log-rank test ( Figure 1 ) showed that TBI patients with acupuncture treatment had a lower probability of new-onset stroke events than those without acupuncture treatment (p<0.0001).
Table 2. Incidence, adjusted hazard ratios and confidence intervals of new-onset stroke for TBI patients with and without acupuncture treatment in the stratification of sex and age.
| Non-acupuncture | Acupuncture treatment | |||||||||
| n | Events | Person-years | Incidence* | n | Events | Person-years | Incidence* | IRR (95% CI) | HR (95% CI) | |
| Overall† | 29636 | 1250 | 173682 | 7.5 | 7409 | 163 | 33071 | 4.9 | 0.68 (0.58–0.81) | 0.59 (0.50–0.69) |
| Sex‡ | ||||||||||
| Female | 14056 | 550 | 84939 | 6.5 | 3514 | 73 | 15890 | 4.6 | 0.71 (0.55–0.91) | 0.62 (0.48–0.79) |
| Male | 15580 | 700 | 88743 | 7.9 | 3895 | 90 | 17181 | 5.2 | 0.66 (0.53–0.83) | 0.57 (0.46–0.71) |
| Age§ | ||||||||||
| 20–44 | 17781 | 235 | 109647 | 2.1 | 4420 | 24 | 20054 | 1.2 | 0.56 (0.35–0.85) | 0.46 (0.30–0.71) |
| 45–64 | 7854 | 480 | 45206 | 10.6 | 1997 | 66 | 8953 | 7.4 | 0.69 (0.53–0.90) | 0.64 (0.50–0.83) |
| ≥65 | 4001 | 535 | 18829 | 28.4 | 992 | 73 | 4064 | 18.0 | 0.63 (0.49–0.81) | 0.60 (0.47–0.76) |
*Per 1000 person-years with calculated by correcting immortal time.
Adjusted for age, gender, low income, density of TCM physicians, types of TBI, diabetes mellitus, hypertension, hyperlipidemia, mental disorders, ischemic heart disease, migraine, epilepsy, anticoagulants, antiplatelet agents, and lipid-lowering agents.
Adjusted for all covariates in the full model except gender.
Adjusted for all covariates in the full model except age.
CI, confidence interval; HR, hazard ratio; IRR, incidence rate ratio; TBI, traumatic brain injury; TCM traditional Chinese medicine.
Figure 1. The stroke-free proportions estimated for TBI patients with and without acupuncture treatment using the Kaplan-Meier method.
Discussion
Using Taiwan's National Health Insurance Research Database, we conducted a retrospective cohort study with comprehensive design (matching procedure of propensity score) and showed significantly decreased risk of new-onset stroke events for patients with TBI who received acupuncture treatment. The present study is the first to report that acupuncture treatment was associated with reduced stroke risk for patients with TBI.
Confounding Effects
Male, older age, low income and coexisting medical conditions are risk factors for TBI and post-TBI outcomes [1]–[3]. The use of TCM or acupuncture was associated with age, sex, low-income status and chronic diseases such as hypertension, mental disorders, diabetes, stroke, ischemic heart diseases, hyperlipidemia, migraine, and epilepsy. [13]–[17], [19]. To properly evaluate whether acupuncture treatment is associated with reduced stroke risk in TBI patients, we used propensity score to match the difference of age, sex, low income, and density of TCM physicians, mental disorders, hypertension, diabetes, ischemia heart disease, hyperlipidemia, migraine and epilepsy between TBI patients with and without acupuncture treatment. To accurately estimate risk of stroke after TBI for patients with and without acupuncture treatment, residual confounding effects were adjusted in the multivariable Cox proportional hazard models.
Possible Explanations
Our previous study found that patients with TBI who received acupuncture treatment had less emergency care and hospitalization in the first year after injury compared with control [19]. In a small sample of patients with TBI, Zollman et al. proved that acupuncture improves cognition and perception of sleep or sleep quality [18]. A clinical trial showed the intervention of acupuncture combined with point-injection in TBI patients improved post-TBI aphasia, hemiplegia, and injuries of cranial nerves (including injuries of the facial, oculomotor and abducent nerves) [29]. This study found that TBI patients who had acupuncture had decreased risk of stroke.
We propose two possible explanations. First, acupuncture has biological benefits for TBI patients. Several studies show acupuncture's effectiveness in improving stroke patients' physical abilities [30], [31]. It has been shown that acupuncture is useful in lowering blood pressure [32], [33], reducing inflammatory mediators [34], and improving lipid profile [35], [36]. Acupuncture may also mediate anti-pain, anti-anxiety, and other therapeutic effects via intrinsic neural circuits that influence the affective and cognitive dimensions of pain [37]. Modulation of subcortical structures may also be an important mechanism by which acupuncture exerts complex multisystem effects [38]. This modulation and sympathy-vagal response may relate to acupuncture's analgesia and other potential therapeutic effects [39]. These findings implied that acupuncture might improve physical activity to reduce the risk of stroke. Second, patients with TBI who choose acupuncture treatment may have better knowledge, attitudes and practices regarding physical rehabilitation and disease prevention, which we believe could also contribute to reduce new-onset stroke event after TBI.
Study Strengths
Among this study's strengths is its large sample, as it uses a representative sample of one million subjects from Taiwan's National Health Insurance Research Database. Second, our study design was a retrospective cohort; this provides more evidence than case-control or cross-sectional designs. Third, to eliminate the interference of sociodemographics and coexisting medical conditions between TBI patients with or without acupuncture treatment, we used propensity score matching procedure to select acupuncture treatment and non-treatment controls. To control residual confounding effects in the association between decreased risk of stroke after TBI and acupuncture treatment, we applied the multivariable Cox proportional hazard models to calculate adjusted HRs and 95% CIs of stroke associated with acupuncture treatment. Finally, immortal time in observational studies can bias the results in favor of the treatment group, but it is difficult to identify and avoid [27]. To reduce such bias, we calculated person-years to correct immortal time in the group with acupuncture treatment.
Study Limitations
This study has several limitations. First, we used retrospective medical claims data from health insurance that lacked detailed patient information on lifestyle as well as physical, psychiatric, and laboratory examinations. Second, we used ICD-9-CM codes claimed by physicians for TBI without clarifying the severity of disease using means such as the Glasgow coma scale. Third, the data provided by insurance claims might underestimate the prevalence of TBI due to cases in which patients with very minor TBI might not seek medical treatment. In addition, the beneficial effects from acupuncture were somewhat different from individual acupuncture points [40]. Our study could not validate the actual acupuncture points used in treatment due to the limited information from the National Health Insurance Research Database. Finally, the mode of acupuncture treatment for patients with TBI varied with TCM physicians. We could not confirm every TCM physician performed the same procedures and acupuncture points for patients with TBI.
Conclusions
From the results of this nationwide retrospective cohort study with matching procedure by propensity score, multivariable adjustment and immortal time correction, we suggested that TBI patients with acupuncture treatment had lower risk of new-onset stroke compared with TBI patients without acupuncture treatment. The association between acupuncture treatment and decreased risk of stroke among TBI patients existed in both sexes and among all age groups. However, further investigation is needed on specific acupuncture points to detail the mechanisms for such effects.
Acknowledgments
This study is based in part on data from the National Health Insurance Research Database provided by the National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of the National Health Research Institutes.
Funding Statement
This study is supported in part by a Grant from the Committee on Chinese Medicine and Pharmacy, Department of Health, Taiwan (CCMP98-RD-038 and CCMP99-RD-035), the National Science Council, Taiwan (102-2314-B-038-021-MY3), and Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH102-TD-B-111-004). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the paper.
References
- 1. Liao CC, Chiu WT, Yeh CC, Chang HC, Chen TL (2012) Risk and outcomes for traumatic brain injury in patients with mental disorders. J Neurol Neurosurg Psychiatry 83: 1186–1192. [DOI] [PubMed] [Google Scholar]
- 2. Yeh CC, Chen TL, Hu CJ, Chiu WT, Liao CC (2013) Risk of epilepsy after traumatic brain injury: a retrospective population-based cohort study. J Neurol Neurosurg Psychiatry 84: 441–445. [DOI] [PubMed] [Google Scholar]
- 3. Liao CC, Chang HC, Yeh CC, Chou YC, Chiu WT, et al. (2012) Socioeconomic deprivation and associated risk factors of traumatic brain injury in children. J Trauma Acute Care Surg 73: 1327–1231. [DOI] [PubMed] [Google Scholar]
- 4. Hesdorffer DC, Rauch SL, Tamminga CA (2009) Long-term psychiatric outcomes following traumatic brain injury: a review of the literature. J Head Trauma Rehabil 24: 452–459. [DOI] [PubMed] [Google Scholar]
- 5. Bazarian JJ, Cernak I, Noble-Haeusslein L, Potolicchio S, Temkin N (2009) Long-term neurologic outcomes after traumatic brain injury. J Head Trauma Rehabil 24: 439–451. [DOI] [PubMed] [Google Scholar]
- 6. Dikmen SS, Corrigan JD, Levin HS, Machamer J, Stiers W, et al. (2009) Cognitive outcome following traumatic brain injury. J Head Trauma Rehabil 24: 430–438. [DOI] [PubMed] [Google Scholar]
- 7. Ishibe N, Wlordarczyk RC, Fulco C (2009) Overview of the Institute of Medicine Committee's search strategy and review process for “Gulf War and Health: Long-term Consequences of Traumatic Brain Injury.”. J Head Trauma Rehabil 24: 424–429. [DOI] [PubMed] [Google Scholar]
- 8. Engberg AW (2007) A Danish national strategy for treatment and rehabilitation after acquired brain injury. J Head Trauma Rehabil 22: 221–228. [DOI] [PubMed] [Google Scholar]
- 9. Feigin VL (2007) Stroke in developing countries: can the epidemic be stopped and outcomes improved? Lancet Neurol 6: 94–97. [DOI] [PubMed] [Google Scholar]
- 10. O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, et al. (2010) Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 376: 112–123. [DOI] [PubMed] [Google Scholar]
- 11. Chen YH, Kang JH, Lin HC (2011) Patients with traumatic brain injury: population-based study suggests increased risk of stroke. Stroke 42: 2733–2739. [DOI] [PubMed] [Google Scholar]
- 12. Burke JF, Stulc JL, Skolarus LE, Sears ED, Zahuranec DB, et al. (2013) Traumatic brain injury may be an independent risk factor for stroke. Neurology 81: 33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liao CC, Lin JG, Tsai CC, Lane HL, Su TC, et al. (2012) An investigation of the use of traditional Chinese medicine in stroke patients in Taiwan. Evid Based Complement Alternat Med 2012: 387164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shih CC, Liao CC, Su YC, Tsai CC, Lin JG (2012) Gender differences in the use of traditional Chinese medicine among adults in Taiwan. PLoS One 7: e32540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shih CC, Su YC, Liao CC, Lin ZG (2012) The association between socioeconomic status and the utilization of traditional Chinese medicine among children in Taiwan. BMC Health Serv Res 12: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shih CC, Su YC, Liao CC, Lin ZG (2010) Patterns of medical pluralism among adults: results from the 2001 National Health Interview Survey in Taiwan. BMC Health Serv Res 10: 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shih CC, Lin JG, Liao CC, Su YC (2009) The utilization of traditional Chinese medicine and associated factors in Taiwan in 2002. Chin Med J 122: 1544–1548. [PubMed] [Google Scholar]
- 18. Zollman FS, Larson EB, Wasek-Throm LK, Cyborski CM, Bode RK (2012) Acupuncture for treatment of insomnia in patients with traumatic brain injury: a pilot intervention study. J Head Trauma Rehabil 27: 135–142. [DOI] [PubMed] [Google Scholar]
- 19. Shih CC, Lee HH, Chen TL, Tsai CC, Lane HL, et al. (2013) Reduced use of emergency care and hospitalization in patients with traumatic brain injury receiving acupuncture treatment. Evid Based Complement Alternat Med 2013: 262039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wong V, Cheuk DK, Lee S, Chu V (2013) Acupuncture for acute management and rehabilitation of traumatic brain injury. Cochrane Database Syst Rev 3: CD007700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yeh CC, Wang HH, Chou YC, Hu CJ, Chou WH, et al. (2013) High risk of gastrointestinal hemorrhage in patients with epilepsy: a nationwide cohort study. Mayo Clin Proc 88: 1091–1098. [DOI] [PubMed] [Google Scholar]
- 22. Yeh CC, Liao CC, Chang YC, Jeng LB, Yang HR, et al. (2013) Adverse outcomes after non-cardiac surgery for patients with diabetes: a nationwide population-based retrospective cohort study. Diabetes Care 36: 3216–3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lin JA, Liao CC, Lee YJ, Wu CH, Huang WQ, et al. (2013) Postoperative adverse outcomes in surgical patients with systemic lupus erythematosus: A nationwide population-based study. Ann Rheumatol Dis [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 24. Liao CC, Shen WW, Chang H, Chang CC, Chen TL (2013) Surgical adverse outcomes in patients with schizophrenia: a population-based study. Ann Surg 257: 433–438. [DOI] [PubMed] [Google Scholar]
- 25. Chang CC, Chang HC, Wu CH, Chang CY, Liao CC, et al. (2013) Postoperative adverse outcomes in surgical patients with idiopathic thrombocytopenic purpura: a population-based study. Br J Surg 100: 684–692. [DOI] [PubMed] [Google Scholar]
- 26. Lévesque LE, Hanley JA, Kezouh A, Suissa S (2010) Problem of immortal time bias in cohort studies: example using statins for preventing progression of diabetes. BMJ 340: b5087. [DOI] [PubMed] [Google Scholar]
- 27. Liao CC, Su TC, Sung FC, Chou WH, Chen TL (2012) Does hepatitis C virus infection increase risk for stroke? A population-based cohort study. PLoS One 7: e31527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tseng YJ, Hung YC, Hu WL (2013) Acupuncture helps regain postoperative consciousness in patients with traumatic brain injury: a case study. J Altern Complement Med 19: 474–477. [DOI] [PubMed] [Google Scholar]
- 29. He J, Wu B, Zhang Y (2005) Acupuncture treatment for 15 cases of post-traumatic coma. J Tradit Chin Med 25: 171–173. [PubMed] [Google Scholar]
- 30. Wu P, Mills E, Moher D, Seely D (2010) Acupuncture in poststroke rehabilitation: A systematic review and meta-analysis of randomized trials. Stroke 41: e171–e179. [DOI] [PubMed] [Google Scholar]
- 31. Sze FK, Wong E, Or KK, Lau J, Woo J (2002) Does acupuncture improve motor recovery after stroke? A meta-analysis of randomized controlled trials. Stroke 33: 2604–2619. [DOI] [PubMed] [Google Scholar]
- 32. Flachskampf FA, Gallasch J, Gefeller O, Gan J, Mao J, et al. (2007) Randomized trial of acupuncture to lower blood pressure. Circulation 115: 3121–3129. [DOI] [PubMed] [Google Scholar]
- 33. Kim DD, Pica AM, Duran RG, Duran WN (2006) Acupuncture reduces experimental renovascular hypertension through mechanisms involving nitric oxide synthases. Microcirculation 13: 577–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Choi DC, Lee JY, Moon YJ, Kim SW, Oh TH, et al. (2010) Acupuncture-mediated inhibition of inflammation facilities significant functional recovery after spinal cord injury. Neurobiol Dis 39: 272–282. [DOI] [PubMed] [Google Scholar]
- 35. Cabioğlu MT, Ergene N (2005) Electroacupuncture therapy for weight loss reduces serum total cholesterol, triglycerides, and LDL cholesterol levels in obese women. Am J Chin Med 33: 525–533. [DOI] [PubMed] [Google Scholar]
- 36. Hsieh CH (2010) The effects of auricular acupuncture on weight loss and serum lipid levels in overweight adolescents. Am J Chin Med 38: 675–682. [DOI] [PubMed] [Google Scholar]
- 37. Fang J, Jin Z, Wang Y, Li K, Kong J, et al. (2009) The salient characteristics of the central effects of acupuncture needling: limbic-paralimbic-neocortical network modulation. Hum Brain Mapp 30: 1196–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hui KK, Liu J, Makris N (2000) Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Mapp 9: 13–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dhond RP, Yeh C, Park K, Kettner N, Napadow V (2008) Acupuncture modulates resting state connectivity in default and sensorimotor brain networks. Pain 136: 407–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Quah-Smith I, Sachdev PS, Wen W, Chen X, Williams MA (2010) The brain effects of laser acupuncture in healthy individuals: an FMRI investigation. PLoS One 5: e12619. [DOI] [PMC free article] [PubMed] [Google Scholar]