Abstract
Purpose
Cardiopulmonary resuscitation (CPR) is commonly performed in high-risk, high intensity situations and is therefore a good procedure around which to develop and implement safety culture strategies in the hospital. The purpose of this study was to evaluate the impact of a hospital-wide quality improvement program on the management of sudden cardiac arrests by assessing healthcare providers' attitudes towards patient safety.
Materials and Methods
This study was designed as a prospective cohort study at a single academic medical center. The comprehensive hospital-based safety program included steps to identify areas of hazard, partner units with the Resuscitation Committee, and to conduct a Safety Attitudes Questionnaire (SAQ). The SAQ evaluated 35 questions in seven domains to assess changes in patient safety culture by comparing the results before and after the hospital-wide high risk patient care improvement program.
Results
The response rates of the pre- and post-SAQ survey were 489 out of 1121 (43.6%) and 575 out of 1270 (45.3%), respectively. SAQ survey responses revealed significant improvement in all seven domains of the questionnaire (p-values of 0.006 and lower). In a subgroup analysis, doctors and nurses showed improvement in five domains. Both doctors and nurses did not show improvement in the "sharing information" domain.
Conclusion
A hospital-wide quality improvement program for high-risk, high reliability patient care involving CPR care was shown to be associated with a change in healthcare providers' attitudes towards patient safety. Through an immersive and active program on CPR care, change in healthcare providers' attitudes towards patient safety was initiated.
Keywords: Cardiopulmonary resuscitation, Safety Attitudes Questionnaire, system improvement
INTRODUCTION
A recent review confirmed widespread patient safety problems in hospitals.1 This review stated that the occurrence of preventable adverse events for patients in hospitals is about ten percent. These adverse events have significant economic costs and losses due to litigation.2 Among such events, sudden cardiac arrest prolongs length-of-stay in the intensive care unit, resulting in higher health care costs.3
Timely management of life-threatening cardiac arrest is extremely stressful and critical, and cardiopulmonary resuscitation (CPR) is commonly performed in high-risk, high intensity situations. Accordingly, the safety culture concerning CPR could be considered a marker for the overall safety culture of a hospital. Moreover, CPR could be a good procedure around which to develop and implement safety culture improvement strategies in the hospital.
This project was proposed to improve resuscitation performance, and thus, improve patient outcomes from cardiac arrest by improving the structure and process of providing patient care. As safety attitudes contribute to the safety climate of a healthcare institution and are believed to lead to improvements in overall patient safety, we hoped to cultivate a culture of patient safety throughout our organization.4,5 We hypothesized that a quality improvement program concerning management of cardiac arrest patients would improve healthcare providers' attitudes towards patient safety.
MATERIALS AND METHODS
This prospective cohort study described safety climate improvements occurring between 2008 and 2010 at a large academic medical center of over 800 inpatient beds in Seoul, Korea. This hospital is located in a densely populated area of 40 km2 with an estimated population of 570000 people. It sees, on average, 3000 daily outpatient visits and 700 inpatient admissions. There are over 2000 full-time employees with professional healthcare providers forming 60% of the workforce (35% registered nurses, 25% medical doctors). The hospital started building the infrastructure to support safety culture in 2008. Getting healthcare providers actively involved in an organization-wide quality improvement program was thought to help integrate a culture of patient safety into their routines and regular working patterns. This included performing a baseline safety attitude survey and prioritizing high-risk, high reliability care processes for improvement.
The hospital was experiencing an average of five sentinel events per year. One of the main causes of these events was sudden cardiac arrests; therefore, a Resuscitation Committee was formed to initiate and improve the CPR process. The committee consisted of faculty from various clinical departments (cardiology, anesthesiology, surgery, pediatric, emergency), the nursing division, and the quality improvement office. The committee also formed a resuscitation team to be activated during a cardiac arrest code. The series of interventions implemented to develop a hospital-wide safety culture are described below. This study was exempted from the hospital's ethics review board because it was chosen as a hospital-wide quality improvement program. Informed consent was obtained from all survey participants prior to the study.
Program development
The national hospital accreditation system was recently revised to emphasize patient safety and to change healthcare provider culture concerning patient safety.6 Consequently, many hospitals started to focus on quality improvement programs, previously undertaken only on an as-needed basis. Our institution decided to expand the quality improvement program through an organized and structured process.
The baseline assessment started with exploring and analyzing problems and barriers in current CPR performance. The committee reviewed sentinel events through root cause analysis, chart audit, focused interviews with the staff, and a simulation study, which was aimed to assess response times, nurse preparation, and action competencies during a cardiac arrest event. After an extensive review of the system, the committee came up with four major areas of improvement needing prioritization: activation system, equipment standardization, training, and proper role definition. The hospital was operating in a single open announcement system. There was a need for a dedicated communication system for activating a code event in the hospital. Therefore, a separate hotline was established between the operator and all areas of the hospital. Once the code was activated, the operator would make an open announcement and then send a mobile phone short message system to the responsible resuscitation team on duty.
Through simulation education for sudden cardiac arrest, the committee recognized and standardized the nurses' essential roles during a code event. The contents of the role were reviewed and validated by the emergency physician faculties of the committee. Along with role definition, all equipment, including a defibrillator, code cart, and bag-valve mask, were standardized and provided by the hospital where necessary. Areas remote from the inpatient ward were equipped with automated external defibrillators. The code cart contents were re-organized and standardized by the nursing and pharmacy division. All medications were placed in the same order for every code cart in the hospital. The bag-valve mask was sterilized and packed in a visible plastic wrap and was ready for use when needed.
Training was provided to all nurses in the hospital and to the training residents who would be part of a code team. The training program emphasized the first five minutes of cardiac arrest response. Training comprised a 3-hour session that covered the new policies and standard processes of CPR, skill competencies for the initial steps of the code process, and the post-event reporting system. One hour was dedicated to the didactic part of the training and the rest was utilized for practicing CPR skills and participating in a simulation scenario with debriefing. Each class had a maximum of 30 participants. It took five months to train over 600 nurses and residents in the hospital.
After interventions for structural and process improvements, the committee developed a standard reporting system. The nurse in charge during the code of a patient had the obligation of reporting the event online and sending it to the committee. The nurse would also attach the nursing record as well. One member of the committee was designated to be the reviewer. After the report was reviewed, the reviewer would audit the nursing record if necessary, as well as interview the resuscitation team who was at the scene. Once all the information was gathered, the reviewer would write a feedback report on things done well, things needing improvement, and any further comments that might need attention. All the feedback would be reviewed at a regular tri-monthly committee meeting, and any important issues would be documented and submitted to the hospital executive board.
Data gathering and analysis
To assess the impact of our program on healthcare providers' attitudes towards patient safety, we generated a brief survey instrument using items from the Safety Attitudes Questionnaire (SAQ) developed at the University of Texas.5 The SAQ was administered before the introduction of CPR response and at the end of the year in 2010. The SAQ is a 60-item survey, with several versions available for different healthcare settings. All versions consist of 30 identical core questions, eliciting caregiver attitudes through six subscales or domains: 'teamwork climate,' 'safety climate,' 'perceptions of management,' 'job satisfaction,' 'working conditions,' and 'stress recognition' using a 5-point Likert scale. The remaining 30 items investigate additional aspects of safety, which vary according to the particular unit type being surveyed. The SAQ has undergone comprehensive psychometric testing7 and has been shown to have good construct validity and internal consistency;8 it is reported to have an internal consistency with a Cronbach's alpha of 0.90.9 This consistency was also evidenced from a Korean study on nurses from general wards that showed the SAQ to have a Cronbach's alpha of 0.91.10 We based our survey on the 30 core items plus an additional five items related to management, rather than the total 60 items from the SAQ. The subscales and domains of our survey have been reorganized and renamed to be more appropriate for our system and understanding. The survey development team, comprised of the quality improvement office staff, validated the revised survey, and it was piloted by a group of healthcare providers from our affiliated organization. The SAQ was translated to Korean and reverse translated to confirm proper translation.
Statistical analysis was performed with the Statistical Package for Social Sciences (PASW Statistics 17.0, New York, NY, USA). Continuous variables were analyzed by t-test or ANOVA. Categorical variables were analyzed by χ2-test. Continuous variables were expressed in mean±standard deviation, while categorical variations were expressed in numbers and percentage. All values of p<0.05 were considered statistically significant.
RESULTS
A total of 425 code cases were included in the study during the 3-year period. The mean number of code cases per 1000 hospital days was 0.58. The mean interval for arrest recognition to code activation was 1.43±3.16 minutes in year 2008 and 2.34±5.24 minutes in year 2010. The mean interval for code activation to CPR team arrival was 1.12±1.56 minutes in year 2008 and 0.92±1.59 minutes in year 2010. No significant differences were found between these two years (Table 1).
Table 1.
Outcomes of Coded Cases
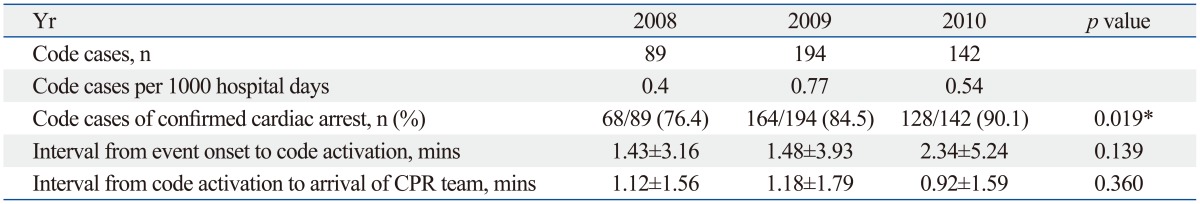
CPR, cardiopulmonary resuscitation.
Data was given as mean±standard deviation or number (%).
*p<0.05 based on χ2-test between 2008, 2009 and 2010 data.
The response rates of the pre- and post-intervention survey were 489 out of 1121 (43.6%) and 575 out of 1270 (45.3%), respectively. Response rates for medical doctors decreased in 2010 (26.3%), compared to 2008 (32.2%), while response rates for nurses increased in 2010 (72.6%), compared to 2008 (52.4%). The ages of the responders were mostly in the twenties and the thirties. Work experience varied from 2 to 10 years (Table 2).
Table 2.
Homogeneity Test of General Characteristics between before and after Groups
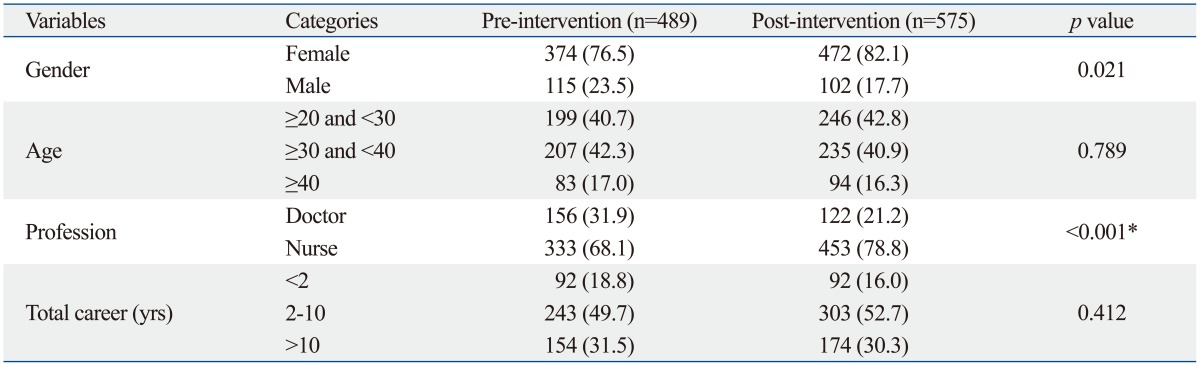
Data was given as number (%).
*p<0.05 based on χ2-test.
The pre- and post-intervention surveys revealed changes in the healthcare providers' attitudes. Improvement was statistically significant in all of seven domains (Table 3). In a subgroup analysis, doctors and nurses showed improvement in five domains (Table 4). Doctors did not show improvement in the domains of 'sharing information' and 'training,' while nurses did not show improvement in the domains of 'sharing information' and 'job satisfaction.' Both doctors and nurses showed no improvement in the "sharing information" domain.
Table 3.
Overall Responses to the Safety Attitudes Questionnaire
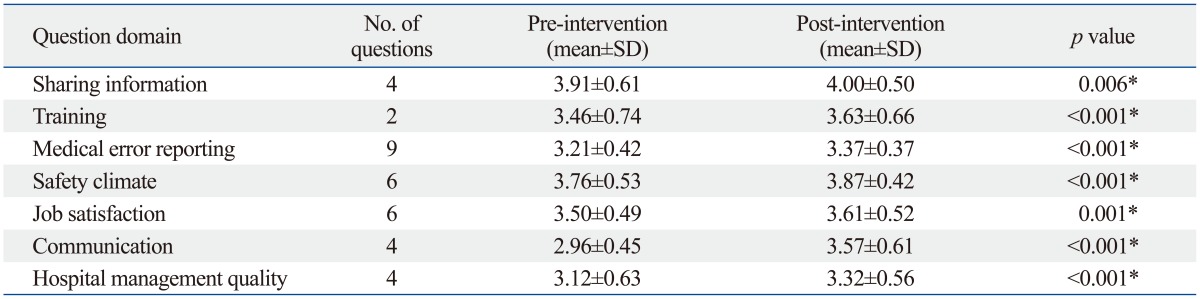
Statistical comparisons are based on the mean of individual domain scores. Individual scores to each item in a domain were summed and then divided by the number of items in that domain to create an individual domain score. If some items in a domain did not get an answer, an individual domain score was calculated by splitting the sum of scores to the number of item in that domain that were answered.
*p<0.05 based on t-test.
Table 4.
Responses to the Safety Attitudes Questionnaire According to Profession
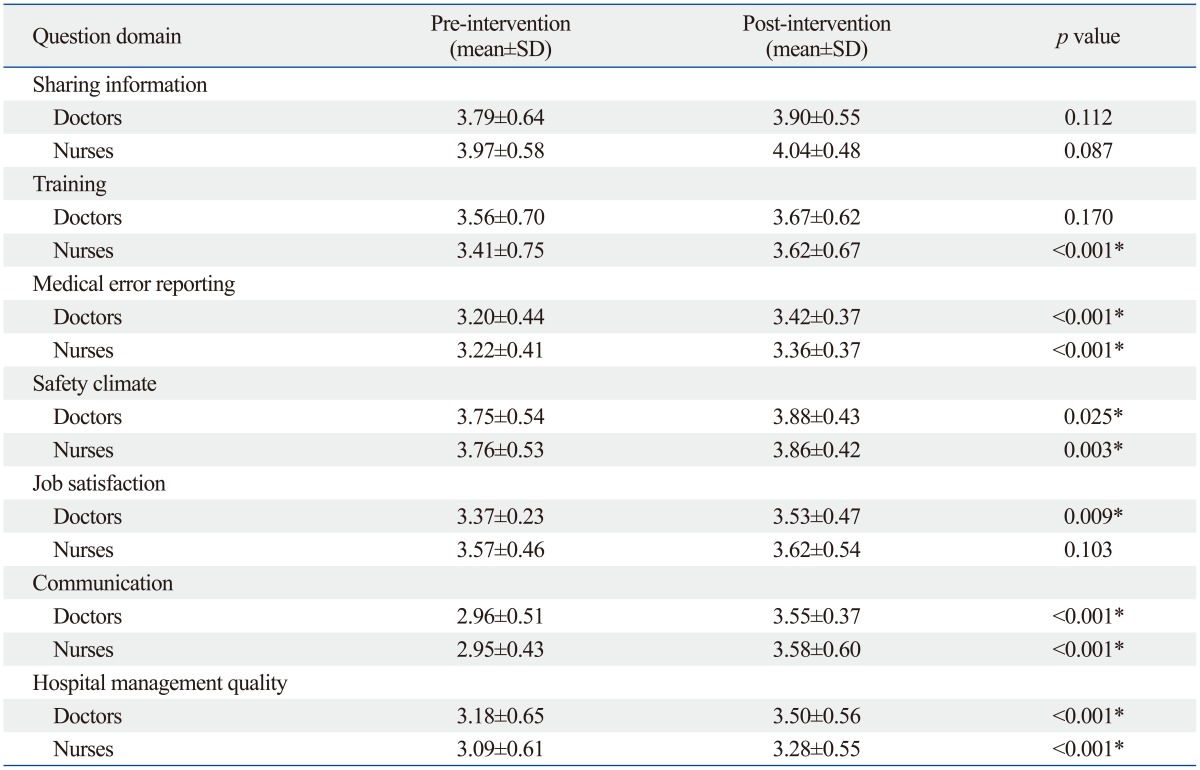
*p<0.05 based on t-test.
Detailed response scores to the Safety Attitudes Questionnaire among doctor and nurse are given in Supplementary Table 1 and 2 (only online).
DISCUSSION
The purpose of this study was to assess changes in attitudes on safety among healthcare providers after developing a program for altering high risk, high reliability patient care processes, such as CPR. The reported survival rate from in-hospital cardiac arrest varies from 5% to 37%, but in the majority of hospitals, it is around 15 percent.11 Many factors such as arrival time, initial rhythm, and availability of staff and/or equipment are strongly correlated with mortality.12,13 The formation of a resuscitation team, widespread resuscitation training, and improvement in resuscitation equipment have been adopted in many hospitals to improve in-hospital cardiac arrest survival.14,15 Unfortunately, survival rates have remained unchanged, despite continuous improvements in training methods and equipment.11 CPR is a team endeavor. However, so far, such endeavors have not brought about clear successful improvements in organizations. Nevertheless, the transformation of hospitals into safer organizations requires time to evidence visible, long lasting, positive effects.
Our study results revealed some improvement in delivering CPR care. The numbers of cardiac arrest cases increased significantly from year 2008 to 2010. Although not statistically significant, the interval from code activation to arrival of CPR team improved from 1.12 minutes to 0.92 minutes. The interval from event onset to code activation was steady before and after the training program. The training program emphasized the first five minutes of cardiac arrest response. The program stresses the implementation of early recognition of critical patients in order to improve the interval from onset to code activation. The safety attitude survey results reflected the effects of the training program, as the survey results among doctors showed no improvement in the "training" domain after the implementation of the program.
Conducting a survey to determine attitudes and perceptions that make up the safety culture is a beginning step in the process of improving patient safety. One commonly used and rigorously validated tool to measure safety culture is the SAQ.16 Higher scores on this questionnaire are associated with lower rates of nurse turnover, catheter-related bloodstream infections, postoperative sepsis, decubitus ulcers, and inpatient mortality.16 The SAQ has been administered in a variety of inpatient and outpatient settings in over 200 sites across the United States, United Kingdom, and New Zealand.5 Results have been used to benchmark safety cultures internationally in healthcare organisations.5,16
In this study, both doctors and nurses showed no improvement in the 'sharing information' Domain. This may due to a lack of training in the areas of teamwork and leadership. Teamwork and leadership training have been shown to improve subsequent team performance during resuscitation and have recently been included in many training programs.17 Implementing a multidisciplinary, simulation-based curriculum emphasizing teamwork and communication was previously shown to improve patient safety in a pediatric emergency department.18 In the 'training' domain, only nurses improved significantly, as the training curriculum focused primarily on the first five minutes of care after cardiac arrest. Since the training program emphasized the first five minutes of cardiac arrest, nurses tended to be more motivated in learning, and thus more able to recognize the importance of safety-oriented culture in their work areas. For the domains 'medical error reporting,' 'safety climate,' and 'communication,' attitudes among both doctors and nurses improved. These three domains improved significantly due to regular and continuous constructive feedback that was provided to the nurses and doctors that administered CPR. The feedback system allowed the healthcare providers to openly communicate about medical errors, thus changing the culture of placing blame that existed previously. The open communication culture eventually also led to increased job satisfaction. After implementation of the high risk, high reliability patient care program, unit managers began to provide safety briefings to nurses that affected the safety attitudes of nurses. This also led to improvement in the domain addressing hospital management quality. This domain improved among both doctors and nurses. The standardization and support of equipment, along with efforts to improve the code activation system, has led to improvements in safety attitudes.
There are several limitations to the study. First, this study was conducted in one academic medical center, and may not be generalizable to other hospitals. Second, the assessment relied on self-reported survey data, and respondents may have answered falsely to justify improvement. Third, the start of the movement, both nationally and institutionally, might have influenced the healthcare providers' responses. Fourth, our survey consisted of a 35-item survey, while only 30 items have been validated in multiple other studies.7-10 The additional five items that measured management have not been validated yet, and thus, might influence the results of this study. The CPR response time outcomes did not improve significantly; these times can be impacted by a number of factors - changes in staff availability, the implementation of the new CPR team notification system, etc. These factors should be included for future analysis of improvement in cardiac arrest performance and patient prognosis. Another factor that could be included in the analysis is training. The training program focused on the first five minutes of the code response. We will need to expand training curriculum to address the whole process of the arrest response in order to improve survival rates among arrest patients.
In conclusion, our hospital-wide quality improvement program for high-risk, high reliability patient care initiated a change in healthcare providers' attitudes towards patient safety. Through an immersive and active alteration in CPR care, major structural and process improvements were noticed. Our hospital will continue to promote cultural change and conduct further hospital-wide quality improvement projects in various clinical areas.
ACKNOWLEDGEMENTS
The authors are grateful to the leadership of the Resuscitation Committee. We also thank the Quality Improvement Division for their assistance in data gathering. And last, but not least, we would like to acknowledge the Nursing Division and all the nurses for their participation in this study.
Footnotes
The authors have no financial conflicts of interest.
Supplementary Material
Doctor Responses to the Safety Attitudes Questionnaire
Nurse Responses to the Safety Attitudes Questionnaire
References
- 1.de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17:216–223. doi: 10.1136/qshc.2007.023622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kohn LT, Corrigan JM, Donaldson MS America. Institute of Medicine, editors. To err is human: building a safer health system. Washington, DC: Committee on Quality, National Academic Press; 2000. [PubMed] [Google Scholar]
- 3.Graf J, Mühlhoff C, Doig GS, Reinartz S, Bode K, Dujardin R, et al. Health care costs, long-term survival, and quality of life following intensive care unit admission after cardiac arrest. Crit Care. 2008;12:R92. doi: 10.1186/cc6963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singer SJ, Gaba DM, Geppert JJ, Sinaiko AD, Howard SK, Park KC. The culture of safety: results of an organization-wide survey in 15 California hospitals. Qual Saf Health Care. 2003;12:112–118. doi: 10.1136/qhc.12.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006;6:44. doi: 10.1186/1472-6963-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korea Institute for Healthcare Accreditation. [accessed on 2013 February 1]. Available at: https://www.koiha.or.kr/english/index.act?page=AP.
- 7.Colla JB, Bracken AC, Kinney LM, Weeks WB. Measuring patient safety climate: a review of surveys. Qual Saf Health Care. 2005;14:364–366. doi: 10.1136/qshc.2005.014217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pronovost P, Sexton B. Assessing safety culture: guidelines and recommendations. Qual Saf Health Care. 2005;14:231–233. doi: 10.1136/qshc.2005.015180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sexton JB1, Thomas EJ, Helmreich RL. Error, stress, and teamwork in medicine and aviation: cross sectional surveys. BMJ. 2000;320:745–749. doi: 10.1136/bmj.320.7237.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim M. [The effectiveness of error reporting promoting strategy on nurse's attitude, patient safety culture, intention to report and reporting rate] J Korean Acad Nurs. 2010;40:172–181. doi: 10.4040/jkan.2010.40.2.172. [DOI] [PubMed] [Google Scholar]
- 11.Schneider AP, 2nd, Nelson DJ, Brown DD. In-hospital cardiopulmonary resuscitation: a 30-year review. J Am Board Fam Pract. 1993;6:91–101. [PubMed] [Google Scholar]
- 12.Cooper S, Cade J. Predicting survival, in-hospital cardiac arrests: resuscitation survival variables and training effectiveness. Resuscitation. 1997;35:17–22. doi: 10.1016/s0300-9572(97)00020-8. [DOI] [PubMed] [Google Scholar]
- 13.Sandroni C, Cavallaro F, Ferro G, Fenici P, Santangelo S, Tortora F, et al. A survey of the in-hospital response to cardiac arrest on general wards in the hospitals of Rome. Resuscitation. 2003;56:41–47. doi: 10.1016/s0300-9572(02)00283-6. [DOI] [PubMed] [Google Scholar]
- 14.Zafari AM, Zarter SK, Heggen V, Wilson P, Taylor RA, Reddy K, et al. A program encouraging early defibrillation results in improved in-hospital resuscitation efficacy. J Am Coll Cardiol. 2004;44:846–852. doi: 10.1016/j.jacc.2004.04.054. [DOI] [PubMed] [Google Scholar]
- 15.Gabbott D, Smith G, Mitchell S, Colquhoun M, Nolan J, Soar J, et al. Cardiopulmonary resuscitation standards for clinical practice and training in the UK. Resuscitation. 2005;64:13–19. doi: 10.1016/j.resuscitation.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Pronovost PJ, Miller MR, Wachter RM. Tracking progress in patient safety: an elusive target. JAMA. 2006;296:696–699. doi: 10.1001/jama.296.6.696. [DOI] [PubMed] [Google Scholar]
- 17.Hunziker S, Johansson AC, Tschan F, Semmer NK, Rock L, Howell MD, et al. Teamwork and leadership in cardiopulmonary resuscitation. J Am Coll Cardiol. 2011;57:2381–2388. doi: 10.1016/j.jacc.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 18.Patterson MD, Geis GL, LeMaster T, Wears RL. Impact of multidisciplinary simulation-based training on patient safety in a paediatric emergency department. BMJ Qual Saf. 2013;22:383–393. doi: 10.1136/bmjqs-2012-000951. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Doctor Responses to the Safety Attitudes Questionnaire
Nurse Responses to the Safety Attitudes Questionnaire


