Laparoscopic intervention may be a safe and effective alternative to open surgery for management of perforation during colonoscopic examination. A simple algorithm is presented that may be helpful for those considering a laparoscopic approach to managing this condition.
Keywords: Colonoscopy, Iatrogenic perforation, Laparoscopic surgery
Abstract
Background and Objectives:
The role of laparoscopy in the management of iatrogenic colonoscopic injuries has increased with surgeons becoming facile with minimally invasive methods. However, with a limited number of reported cases of successful laparoscopic repair, the exact role of this modality is still being defined. Drawing from previous literature and our own experiences, we have formulated a simple algorithm that has helped us treat colonoscopic perforations.
Methods:
A retrospective review was undertaken of patients treated for colonoscopic perforations since the algorithm's introduction. For each patient, initial clinical assessment, management, and postoperative recovery were carefully documented. A Medline search was performed, incorporating the following search words: colonoscopy, perforation, and laparoscopy. Twenty-three articles involving 106 patients were identified and reviewed.
Results:
Between May 2009 and August 2012, 7 consecutive patients with colonoscopic perforations were managed by 2 surgeons using the algorithm. There were no complications and no deaths, with a mean length of stay of 4.43 days (range, 2–7 days). Of the 7 patients, 6 required surgery. A single patient was managed conservatively and later underwent an elective colon resection.
Conclusions:
Traditionally, laparotomy was the preferred method for treating colonoscopic perforations. Our initial experience reinforces previous views that laparoendoscopic surgery is a safe and effective alternative to traditional surgery for managing this complication. We have formulated a simple algorithm that we have found helpful for surgeons considering a laparoscopic approach to managing this condition.
INTRODUCTION
Iatrogenic perforations of the colon after colonoscopy have traditionally been managed with exploratory laparotomy and primary perforation closure or bowel resection with or without ostomy.1 However, the role of laparoscopy in the management of iatrogenic colonoscopic injuries has increased as more reports of successful treatments have emerged. Numerous case reports and case series have described the successful management of this complication using various laparoscopic approaches.2–28 The main advantages conferred by the laparoscopic approach include an improved ability to localize the site of the perforation and, where appropriate, secure repair under direct vision through a small incision.29 The benefits of minimally invasive surgery are reduced postoperative ileus and pain, leading to a reduced length of stay.23 Furthermore, patients undergoing laparoscopy return to normal activities earlier.23 Thus the outcomes of a cohort of patients who have sustained an unexpected complication from a common procedure have improved.
Laparoscopic surgeons have differing levels of skill and institutional resources when facing the aforementioned complication. With limited reported cases of successful laparoscopic repair in the literature and with prospective studies being impractical, the exact role of this modality is still being shaped. Although laparoscopic repair has gathered increasing support since it was first described almost 20 years ago, to our knowledge, a system that attempts to unify the ideas conveyed by the various authors does not exist. The only algorithm described in the previous literature to date provided a method of deciding between laparoscopic techniques in managing iatrogenic perforations.13
Drawing from the previous experiences identified through a comprehensive literature review and those from our own institution, we formulated a system that aims to define the role of laparoscopic surgery in the management of colonoscopic perforation. This system is a simple algorithm that guides laparoscopic surgeons with varied means in treating this complication.
METHODS
A review was undertaken of patients admitted to our institution after iatrogenic colonic perforation under the care of 2 colorectal surgeons. This was performed retrospectively on prospectively collected data. All patients with iatrogenic perforations were included. For each patient, the details of the initial encounter, management, and recovery were documented from a carefully studied chart review. The algorithm was formulated before starting the study. No patients were excluded, and the investigators were not blinded.
Surgical Technique
In the operating room, diagnostic laparoscopy is performed through a periumbilical port placed by the Hasson technique. Additional ports are placed according to the suspected perforation site to allow for easy triangulation and enhance exposure, facilitating a safe repair. In small tears without significant contamination, we advocate simple one-layer suture closure and, if possible, omental or pericolonic fat patch placement. For larger tears, we recommend stapling. In those rare circumstances in which there is associated necrosis, significant contamination, and/or abscess formation, resection and possible temporary diversion with drain placement comprise our preference. An air insufflation leak test is performed for lower descending colon, sigmoid, and/or rectal repairs.
A Medline search was performed, incorporating the following search words: colonoscopy, perforation, and laparoscopy. Twenty-three articles involving 106 patients were identified and reviewed, focusing on the patients' clinical presentations, laparoscopic interventions, and outcomes. Our algorithm is presented.
RESULTS
Between May 2009 and August 2012, 7 patients with colonoscopic perforations were treated by 2 surgeons. Detailed data are summarized in Table 1.
Table 1.
Patient Clinical Presentation
| Patient | Age (y) | Sexa | CT Findingsa | Perforation Type |
|---|---|---|---|---|
| A | 59 | F | Retroperitoneal air at level of rectosigmoid and small amount of free air | Avulsion of rectosigmoid |
| B | 51 | M | Intraperitoneal air and pelvic fluid collection | Linear tear in descending colon |
| C | 51 | F | NA | Linear tear |
| D | 80 | F | Free intraperitoneal air and cecal dilatation | Blowhole tear in cecum |
| E | 60 | M | NA | Post-sigmoid polypectomy |
| F | 84 | M | No free air | Post-cecal polypectomy |
| G | 55 | M | Free intraperitoneal air | Post-polypectomy |
F = female; M = male; NA = not applicable.
The mean patient age was 63 years (range, 51–84 years). Of the patients, 3 were women and 4 were men. None of the patients had undergone surgery previously. Four patients had sustained the injury after a diagnostic colonoscopy, whereas the remaining 3 had undergone a therapeutic colonoscopy with associated polypectomies. During the initial clinical evaluation, 5 of the 7 patients had an abdominal flat plate radiograph that showed pneumoperitoneum. A computed tomography (CT) scan was obtained in 5 of 7 patients during their evaluation, whereas in 2 patients the endoscopist reported visualizing the peritoneum through a perforation site with an obvious location.
Of the 7 patients, 6 were managed surgically acutely; all 6 underwent surgery within 12 hours of their reported injury. The surgical outcomes are summarized in Table 2. During surgery, 2 of the 6 patients were found to have a linear tear, which was found in the descending colon in both patients. One of these cases was managed with a laparoscopic linear stapler, whereas the other patient underwent intracorporeal suturing. In a single patient, an avulsion injury of the rectosigmoid was found and was managed with a laparoscopic-assisted low anterior resection and a loop ileostomy. In the fourth patient, a “blowhole” tear was found in the cecum and was managed with laparoscopic intracorporeal suturing, whereas in the fifth case, a small perforation was seen in the ascending colon with surrounding necrosis necessitating a laparoscopic right colectomy. In the sixth patient, a similar perforation in the sigmoid was managed with a laparoscopic sigmoidectomy. There were no intraoperative complications, and all 6 patients made an uneventful recovery, with a mean length of stay of 4.43 days (range, 2–7 days).
Table 2.
Management of Colonoscopic Perforations
| Patient | Perforation Location | Operation | Hospital Stay (d) |
|---|---|---|---|
| A | Rectosigmoid | Laparoscopy-assisted low anterior resection and loop ileostomy | 4 |
| B | Descending colon | Laparoscopic linear stapler repair | 7 |
| C | Descending colon | Laparoscopic intracorporeal suturing | 2 |
| D | Cecum | Laparoscopic intracorporeal suturing | 4 |
| E | Sigmoid | Laparoscopic sigmoidectomy | 3 |
| F | Cecum | Conservative | 6 |
| G | Ascending colon | Laparoscopic right hemicolectomy | 5 |
The single case in our series that was managed by the conservative approach was an 84-year-old man in whom a perforation was suspected by the endoscopist after a cecal polypectomy; endoscopic clipping was performed at the time of the initial procedure. The patient, who was hemodynamically stable, underwent a CT scan that showed a small retrocecal perforation. He was managed with intravenous antibiotics, bowel rest, and serial abdominal examinations for 2 days. He was subsequently discharged from the hospital and underwent a laparoscopic cecectomy electively at a later date. He had a sessile polyp of the cecum.
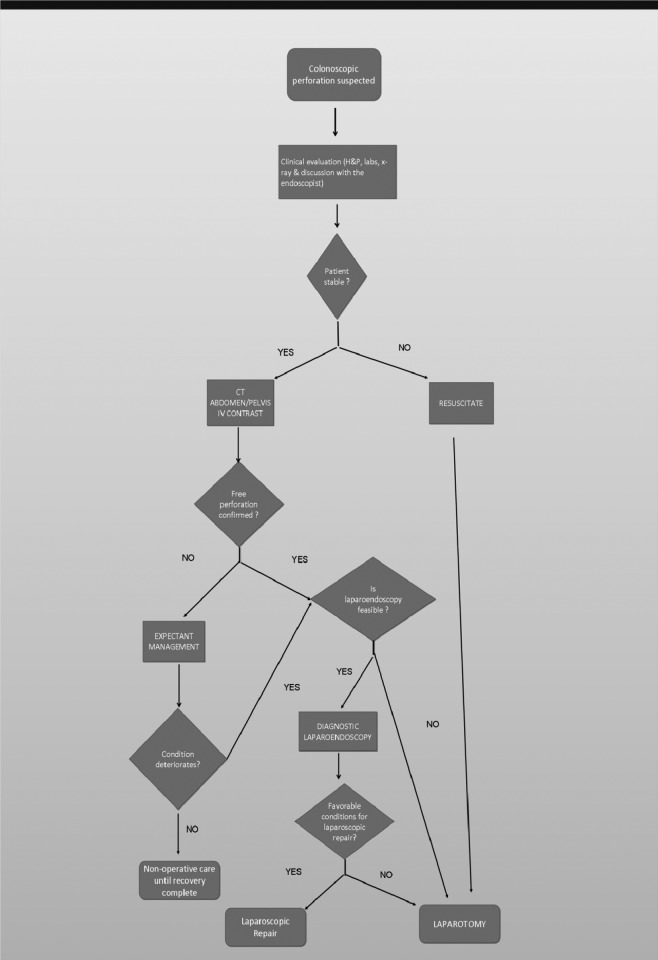
The details of the previously reported cases identified by our extensive literature search are summarized in Table 3. We therefore present our algorithm (Figure 1), which is in line with the previously reported case series and has assisted in the care of our patients.
Table 3.
Previous Cases/Series Presenting Entirely Laparoscopic Repair of Colonoscopic Perforations
| Authors | Year | No. of Patients | No. Patients Operated on within 24 hrs of Perforation | Mean Operative Time (min) | Mortality Rate (%) | Mean Length of Stay (d) |
|---|---|---|---|---|---|---|
| Schlinkert and Rasmussen4 | 1994 | 3 | — | — | 0 | 6 |
| Regan et al3 | 1994 | 1 | 1 | 60 | 0 | 3 |
| Goh et al2 | 1994 | 1 | — | — | 0 | 5 |
| Miyahara et al7 | 1996 | 1 | 1 | — | 0 | 15 |
| Mehdi et al6 | 1996 | 1 | — | — | 0 | 11 |
| Hayashi et al5 | 1996 | 1 | 1 | 80 | 0 | — |
| Allam et al8 | 1997 | 1 | 1 | — | 0 | 5 |
| Velez et al11 | 1997 | 1 | — | — | 0 | 3 |
| Di Marco et al9a | 1997 | 2 | — | — | 0 | — |
| Ibrahim et al10 | 1997 | 1 | 1 | — | 0 | — |
| Nassiopoulos et al12a | 1999 | 3 | — | — | 0 | — |
| Wullstein et al13 | 1999 | 4 | 4 | 129 | 0 | 7.4 |
| Agresta et al14 | 2000 | 2 | — | — | 0 | — |
| Yamamoto et al15 | 2001 | 5 | — | 65.4 | 0 | 34.4b |
| Zippel et al16a | 2002 | 4 | — | — | — | — |
| Alfonso-Ballester et al33 | 2006 | 1 | 1 | 58 | 0 | 7 |
| Hansen et al19 | 2007 | 7 | — | — | 0 | 7.6 |
| Pilgrim and Nottle20 | 2007 | 1 | 1 | 61 | 0 | 6 |
| Busic et al18 | 2007 | 1 | 1 | — | 0 | 4 |
| Bleier et al21 | 2008 | 11 | — | 104 | 0 | 5.1 |
| Rumstadt et al22 | 2008 | 10 | 10 | — | 0 | 7.1 |
| Kilic and Kavic28 | 2008 | 1 | 1 | — | 0 | 4 |
| Rotholtz et al23 | 2010 | 14 | 13c | — | 0 | 4.2 |
| Thill et al24 | 2010 | 13 | 13 | — | 0 | 14.4 |
| Coimbra et al25 | 2011 | 16 | 15c | — | 0 | 10.1 |
| Miranda et al26 | 2011 | 9 | 9 | 82 | 0 | 5.8 |
| Schlöricke et al27a | 2013 | 8 | — | 165 | 0 | 11 |
Case reports and series not written in English.
Significant outlier patient with prolonged length of stay of 101 days because comorbidities affected final mean length of stay.
One patient did not have surgery within 24 hours of the perforation.
Figure 1.
Laparoscopic repair algorithm. H&P = history and physical; IV = intravenous.
Algorithm
When colonoscopic perforation is suspected, the first step is to obtain a focused history and physical examination, laboratory tests, and an abdominal flat plate radiograph (Figure 1). A corroborative history regarding procedure details should also be obtained from the endoscopist involved. Intravenous antibiotics should be started as soon as a perforation is confirmed.
When patients present with hemodynamic instability, this is often associated with a delay in recognition. Subsequent to the initial workup and resuscitation, we recommend that patients undergo emergent exploratory laparotomy. Laparotomy is also reserved for patients whose surgical history precludes a laparoscopic approach or when the perforation is not amenable to the minimally invasive technique.
In the stable patient in whom the perforation location remains unknown, the next step is to perform a CT scan of the abdomen and pelvis (Figure 2). CT can further assist in determining the degree of perforation sustained. In some patients a small contained perforation on the CT scan can still be managed conservatively with serial clinical evaluations. If a free perforation is found on the CT scan, however, emergent laparoscopy is necessary. Intraoperatively, we have also found the review of the CT scan during laparoscopy to be of great help in subsequent decision making regarding the mode of repair.
Figure 2.
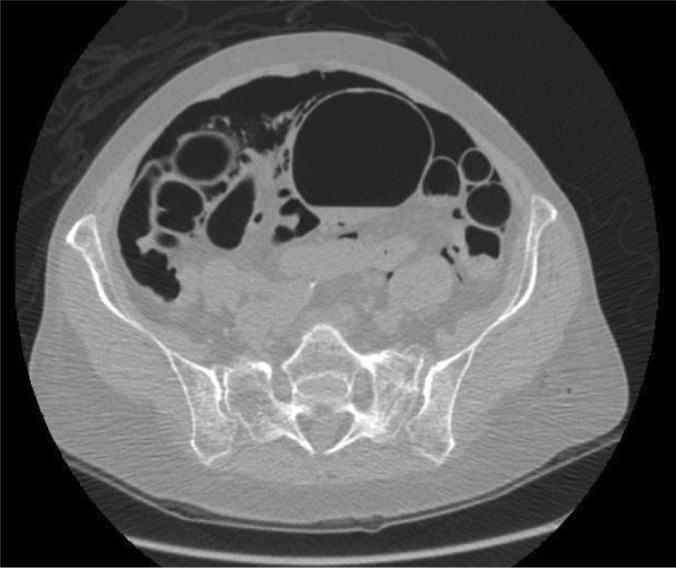
CT scan of patient D showing free intraperitoneal air and colonic dilation.
At laparoscopy, depending on the complexity of the perforation, degree of contamination, and surgeon's skills and available tools, the repair can be performed by one of several methods (Figure 3). The options include intracorporeal suturing, stapler, formal resection, or diversion. In the rare situations in which the perforation cannot be identified or repaired laparoscopically, laparotomy and conventional repair methods would be indicated.
Figure 3.
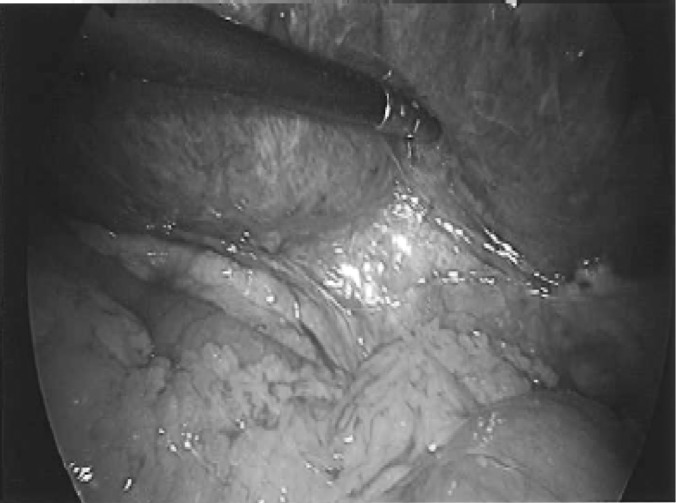
Laparoscopic grasper placed within colonic perforation.
DISCUSSION
Colonoscopic perforations are rare but potentially serious complications occurring in between 0.03% and 0.8% of diagnostic procedures and 0.15% and 3% of cases in therapeutic studies.23 With increasing acceptance of colorectal screening and the advancement of colonoscopic therapeutic procedures, the incidence of colonoscopic perforation has begun to increase.17
The laparoscopic approach to repair has been described since the 1990s, initially in the form of case reports and case series. More recently, comparative studies have shown advantages in patient outcomes after laparoscopic repair versus conventional laparotomy.19,21,23,25 Therefore the laparoscopic option has gained increasing acceptance as an alternative to managing iatrogenic perforations, although a clearer role has yet to be defined in the literature. We thought that a defined algorithm would further assist practitioners in the treatment of this rare but dangerous clinical scenario.
A detailed history and physical examination are of paramount importance. A key aspect of this step involves communication with the endoscopist because this often yields important information that becomes relevant in how treatment is approached. Specifically, information regarding the indication for the procedure and quality of bowel preparation may assist in the forthcoming decision making26 while presenting clues regarding contamination. Furthermore, discussion with the endoscopist may yield details regarding the suspected perforation site, cause of the perforation, other polyp location(s), and whether the injury and its extent were visualized,19 which are also vital adjuncts to decision making.
Traditionally, obtaining an abdominal flat plate radiograph that showed a free perforation was considered sufficient preoperative workup. In our algorithm for laparoscopic repair, it is important to perform a CT scan because it provides a roadmap to allow expedited attention to the injured area. To begin with, it allows differentiation between a free perforation and a contained perforation, a difference that, in a stable patient, would assist in deciding between expectant and operative management.30 Obtaining a CT scan has the added advantage of identifying an incidental rare splenic injury after colonoscopy in cases in which the clinical scenario may be confusing.22 Nonetheless, visualization of the intraperitoneal cavity by the endoscopist through a well-documented perforation site sometimes negates the need for a CT scan, as was found in 2 of our 7 cases. In addition, a preoperative CT scan is helpful intraoperatively because it can help delineate the extent of injuries particularly on the mesenteric or retroperitoneal aspects that are sometimes not as accessible with the laparoscope. Furthermore, in rare cases in which the perforation is not identifiable with the laparoscopic instrument, an intraoperative review of the scan is a great adjunct that may point the surgeon in the right direction.
In the 2 cases in which a CT scan was not ordered, the endoscopist had described the perforation site as being just proximal to the third valve of Houston, diminishing the need for the CT scan. As was the case in the single patient managed conservatively, expectant management should be applied with the premise that frequent clinical observation and immediate intervention can be performed if the patient's condition deteriorates.31
The timely use of laparoendoscopy in evaluating suspected perforations, limiting intraperitoneal contamination and inflammation progression, is another vital aspect of our algorithm. This follows the principle that the sooner the operation is performed, the less invasive the technique required is.13 All the patients in this series underwent surgery within 12 hours of their reported endoscopic injury. Previous series have safely managed colonoscopic perforation laparoscopically up to 24 hours after the diagnosed injury,25 beyond which it may become significantly challenging to successfully achieve, leading to exploratory laparotomy.
Included in the laparoendoscopy evaluation step of the algorithm is intraoperative colonoscopy using carbon dioxide for insufflation. Though not needed in any of our cases, it has been described by previous authors to be of some benefit in identifying the site of injury.21 Carbon dioxide quickly dissipates, allowing for a less challenging operative field. The use of endoscopic clipping to close iatrogenic perforations has been described in case series including 58 patients to date with a success rate of 89.6%.32 The benefits of this strategy could afford the clinician an even less invasive approach to managing this complication particularly in patients with smaller, well-defined perforations with little or no evidence of surrounding thermal injury. Careful observation would be necessary to monitor the success of this method.
A variety of approaches with varied indications for repairing perforations have been described in the literature. Previously, some authors have proposed that perforation size is the determining factor when deciding among suture repair, wedge resection, and colonic resection.13,21 Other authors have used the level of intraperitoneal contamination as a determining factor, with high amounts requiring colonic resection.19,26 A further suggestion has been to only place sutures when there are no signs of thermal damage.13 In agreement with our colleagues,19,23,26 we suggest that the approach to managing a perforation should be tailored to the surgeon's preference but should still adhere to the principles applied to performing an open repair. Our intraoperative decision making is based on 4 factors: the size and location of the defect, the quality of the preparation, and lastly, whether the defect involves compromise to the mesentery (ie, avulsion injuries). Primary repair is used if the tissue in question is well vascularized and approximation can be performed without tension and/or narrowing of the lumen. Avulsion defects would have natural elements of ischemia and therefore would require a formal resection with fresh, healthy tissues used for anastomosis. Finally, in cases in which the injury is recognized late with associated significant intraperitoneal contamination or injuries of the low rectum, we consider staged repair. It must be stated that although robotic colon surgery may offer advantages with regard to ease of repair by intracorporeal suturing, the adynamic nature of this device once docked, especially in cases in which the location of perforation is unknown, makes it cumbersome to perform timely repair, and this method is not advocated by us at this time.
With consideration of all of the previously mentioned points, the decision to convert to a laparotomy should always be entertained and selected based on the surgeon's skill, the stability of the patient's condition, and concern regarding the integrity of repair19 or difficulty identifying the perforation site4,19 that prevents an entirely laparoscopic approach. The application of exploratory laparoendoscopy to identify the perforation site, followed by conversion to focused mini-laparotomy, has also been described8,21,29 and is a safe option to add to the armamentarium of the surgeon facing this situation.
The rarity of colonoscopic perforations has meant that the management of this complication, particularly incorporating newer techniques such as laparoscopic surgery, has been poorly defined. Similarly, the low incidence of this condition has contributed to the lack of prospective randomized studies that would solidify current evidence showing the benefits of laparoscopic repair. With the expectation that the prompt and appropriate management of these patients minimizes their morbidity and mortality rates, we believe that a simple algorithm unifying the ideas from previous literature and incorporating our own experiences provides a clearer management plan that will lead to better outcomes.
CONCLUSIONS
Traditionally, laparotomy has been the standard of care for treating colonoscopic perforations when conservative management is deemed inappropriate. Our experience reinforces previous views that laparoendoscopic surgery is a safe and effective alternative to managing this complication. We have formulated a simple algorithm that we have found helpful in guiding the surgeon considering a laparoscopic approach to managing this condition.
Contributor Information
Tafadzwa Patrick Makarawo, Department of Surgery, Providence Hospital and Medical Centers, Southfield, MI, USA.
Amir Damadi, Department of Surgery, Providence Hospital and Medical Centers, Southfield, MI, USA.
Vijay K. Mittal, Department of Surgery, Providence Hospital and Medical Centers, Southfield, MI, USA.
Ed Itawi, Department of Surgery, Providence Hospital and Medical Centers, Southfield, MI, USA.
Gurteshwar Rana, Department of Surgery, Providence Hospital and Medical Centers, Southfield, MI, USA.
References:
- 1. Danmore LJ, II, Rantis PC, Vernava AM, III, Longo WE. Colonoscopic perforations. Etiology, diagnosis and management. Dis Colon Rectum. 1996;39:1308–1314 [DOI] [PubMed] [Google Scholar]
- 2. Goh PM, Kum CK, Chia YW, Ti TK. Laparoscopic repair of perforation of the colon during colonoscopy. Gastrointest Endosc. 1994;40(4):496–497 [DOI] [PubMed] [Google Scholar]
- 3. Regan MC, Boyle B, Stephens RB. Laparoscopic repair of colonic perforation occurring during colonoscopy. Br J Surg. 1994;81:1073. [DOI] [PubMed] [Google Scholar]
- 4. Schlinkert RT, Rasmussen TE. Laparoscopic repair of colonoscopic perforations of the colon. J Laparoendosc Surg. 1994(4):51–54 [DOI] [PubMed] [Google Scholar]
- 5. Hayashi K, Urata K, Munakata Y, Kawasaki S, Makuuchi M. Laparoscopic closure for perforation of the sigmoid colon by endoscopic linear stapler. Surg Laparosc Endosc. 1996;6(5):411–413 [PubMed] [Google Scholar]
- 6. Mehdi A, Closset J, Gay F, Deviere J, Houben J, Lambilliotte J. Laparoscopic treatment of a sigmoid perforation after colonoscopy. Case report and review of literature. Surg Endosc. 1996;10:666–667 [DOI] [PubMed] [Google Scholar]
- 7. Miyahara M, Kitano S, Shimoda K, et al. Laparoscopic repair of a colonic perforation sustained during colonoscopy. Surg Endosc. 1996;10:352–353 [DOI] [PubMed] [Google Scholar]
- 8. Allam M, Piskun G, Fogler R. Laparoscopic-assisted repair of extensive rectosigmoid injury after colonoscopy. J Laparoendosc Adv Surg Tech A. 1997;7:127–130 [DOI] [PubMed] [Google Scholar]
- 9. Di Marco L, Occhionorelli S, Schettino AM, Carcoforo P, Navarra G, Pollinzi V. Laparoscopy in iatrogenic lesions of the colon during operative endoscopy [in Italian]. Ann Ital Chir. 1997;68:859–862 [PubMed] [Google Scholar]
- 10. Ibrahim IM, Sussman B, Wolodiger F, Silvestri F. Laparoscopic management of iatrogenic colon perforation. N J Med. 1997;12:35–37 [PubMed] [Google Scholar]
- 11. Velez MA, Riff DS, Mule JM. Laparoscopic repair of a colonoscopic perforation. Surg Endosc. 1997;14:387–389 [DOI] [PubMed] [Google Scholar]
- 12. Nassiopoulos K, Chanson C, Petropoulos P. Perforation of the colon during colonoscopy [in French]. Swiss Surg. 1999;5(1):2–5 [DOI] [PubMed] [Google Scholar]
- 13. Wullstein C, Koppen M-O, Gross E. Laparoscopic treatment of colonic perforations related to colonoscopy. Surg Endosc. 1999;13:484–487 [DOI] [PubMed] [Google Scholar]
- 14. Agresta F, Michelet I, Mainente P, Bedin N. Laparoscopic management of colonoscopic perforations. Surg Endosc. 2000;14:592–593 [DOI] [PubMed] [Google Scholar]
- 15. Yamamoto A, Ibusuki K, Koga K, Taniguchi S, Kawano M, Tanaka H. Laparoscopic repair of colonic perforation associated with colonoscopy: use of passing sutures and endoscopic linear stapler. Surg Laparosc Endosc Percutan Tech. 2001;11(1):19–21 [PubMed] [Google Scholar]
- 16. Zippel R, Meyer L, Koch A, Marusch F, Gastinger I. Laparoscopic treatment of iatrogenic perforations of the colon [in German]. Zentralbl Chir. 2002;127(4):307–309 [DOI] [PubMed] [Google Scholar]
- 17. Tulchinsky H, Madhala-Givon O, Wasserberg N, Lelcuk S, Niv Y. Incidence and management of colonoscopic perforations: 8 years experience. World J Gastroenterol. 2006;12(26):4211–4213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Busic Z, Lovric Z, Busic V, Cavka M, Lemac D. Laparoscopic treatment of iatrogenic endoscopic sigmoid colon perforation: a case report and literature review. J Laparoendosc Adv Surg Tech A. 2007;17(3):324–325 [DOI] [PubMed] [Google Scholar]
- 19. Hansen AJ, Tessier DJ, Anderson ML, Schlinkert RT. Laparoscopic repair of colonoscopic perforations: indications and guidelines. J Gastrointest Surg. 2007;11:655–659 [DOI] [PubMed] [Google Scholar]
- 20. Pilgrim C, Nottle PD. Laparoscopic repair of iatrogenic colonic perforation. Surg Laparosc Endosc Percutan Tech. 2007;17(3):215–217 [DOI] [PubMed] [Google Scholar]
- 21. Bleier JI, Moon V, Feingold D, et al. Initial repair of iatrogenic colon perforation using laparoscopic methods. Surg Endosc. 2008;22:646–649 [DOI] [PubMed] [Google Scholar]
- 22. Rumstadt B, Schilling D, Sturm J. The role of laparoscopy in the treatment of complications after colonoscopy. Surg Laparosc Endosc Percutan Tech. 2008;18(6):561–564 [DOI] [PubMed] [Google Scholar]
- 23. Rotholtz NA, Laporte M, Lencinas S, Bun M, Canelas A, Mezzadri N. Laparoscopic approach to colonic perforation due to colonoscopy. World J Surg. 2010;34:1949–1953 [DOI] [PubMed] [Google Scholar]
- 24. Thill V, Simoens C, da Costa M. Management of iatrogenic perforation after gastrointestinal endoscopy. Hepatogastroenterology. 2010;57:1465–1468 [PubMed] [Google Scholar]
- 25. Coimbra C, Bouffioux L, Kohnen L, et al. Laparoscopic repair of colonoscopic perforation: a new standard? Surg Endosc. 2011;25:1514–1517 [DOI] [PubMed] [Google Scholar]
- 26. Miranda L, Settembre A, Piccolboni D, Capasso P, Corcione F. Iatrogenic colonic perforation: repair using laparoscopic technique. Surg Laparosc Endosc Percutan Tech. 2011;21(3):170–174 [DOI] [PubMed] [Google Scholar]
- 27. Schlöricke E, Bader FG, Hoffmann M, Zimmermann M, Bruch HP, Hildebrand P. Open surgical versus laparoscopic treatment of iatrogenic colon perforation—results of a 13-year experience. Zentralbl Chir. 2013;138(3):257–261 [DOI] [PubMed] [Google Scholar]
- 28. Kilic A, Kavic SM. Laparoscopic colotomy repair following colonoscopic polypectomy. JSLS. 2008;12:93–96 [PMC free article] [PubMed] [Google Scholar]
- 29. Ng WT. Re: Laparoscopic repair of colonoscopic perforations. Surg Laparosc Endosc Percutan Tech. 2006;16:49–51. Surg Laparosc Endosc Percutan Tech. 2007;17(1):68. [DOI] [PubMed] [Google Scholar]
- 30. Kavin H, Sinicrope F, Esker AH. Management of perforation of the colon at colonoscopy. Am J Gastroenterol. 1992;87:161–167 [PubMed] [Google Scholar]
- 31. Hall C, Doricott NJ, Donovan IA, Neoptolemos JP. Colon perforation during colonoscopy; surgical versus conservative management. Br J Surg. 1991;78:542–544 [DOI] [PubMed] [Google Scholar]
- 32. Mangiavillano B, Viaggi P, Masci E. Endoscopic closure of acute iatrogenic perforations during diagnostic and therapeutic endoscopy in the gastrointestinal tract using metallic clips: a literature review. J Dig Dis. 2010;11:12–18 [DOI] [PubMed] [Google Scholar]
- 33. Alfonso-Balester R, LóPez-Mozos F, Marti-Obiol R, et al. Laparoscopic treatment of endoscopic sigmoid colon perforation: a case report and literature review. Surg Laparosc Endosc Percutan Tech. 2006;16:49–51 [DOI] [PubMed] [Google Scholar]