Transvaginal endoscopic salpingectomy for tubal ectopic pregnancy appears to be feasible and safe and may result in less postoperative pain compared with a laparoscopic approach.
Keywords: Transvaginal endoscopic surgery, Ectopic pregnancy, Salpingectomy
Abstract
Objective:
To explore the feasibility, safety, efficacy, and cosmetic outcomes of transvaginal endoscopic salpingectomy for tubal ectopic pregnancy.
Methods:
From May 2009 to May 2012, we prospectively enrolled 40 patients, each of whom had been scheduled for a salpingectomy because of a tubal ectopic pregnancy, and randomized them into two groups: transvaginal endoscopic surgery and laparoscopic approach. We recorded the estimated blood loss, time of anal exhaust, postoperative pain score, length of stay, and scar assessment scale associated with transvaginal endoscopic access (n = 18) (natural orifice transluminal endoscopic surgery) and laparoscopic salpingectomy (n = 20) (control group) for tubal ectopic pregnancy. The transvaginal salpingectomy was performed with a double-channel endoscope through a vaginal puncture. A single surgeon performed the surgical procedures in patients in both groups.
Results:
The group that underwent the transvaginal endoscopic procedure reported lesser pain at all postoperative visits than the group that underwent the laparoscopic approach. The duration of time for transvaginal endoscopic surgery was slightly longer than that for the laparoscopic approach. However, there was no statistically significant difference between the two groups in the duration of operative time. The group that underwent transvaginal endoscopic surgery was more satisfied with the absence of an external scar than the group that underwent the laparoscopic procedure, which left a scar. The estimated blood loss, time of anal exhaust, and length of stay were the same in both groups.
Conclusion:
The safety and efficacy of transvaginal endoscopic salpingectomy for tubal ectopic pregnancy are equivalent to those of the laparoscopic procedure. Lesser postoperative pain and a more satisfactory cosmetic outcome were found with the transvaginal endoscopic procedure, making it the more preferred method and superior to the laparoscopic approach.
INTRODUCTION
In recent decades, new techniques for minimally invasive surgery have experienced numerous changes and developments.1 Laparoscopy has a well-established role in the modern era of surgery, yielding less postoperative pain, a shorter hospital stay, a faster recovery, and better esthetic results.2,3 Recently, natural orifice transluminal endoscopic surgery (NOTES), as a new minimally invasive surgical approach, has been increasingly reported.4–6 This approach yields an access to the abdominal cavity without any incisions in the abdominal wall (scarless surgery), and the natural orifices (mouth, urethra, anus, and so on) serve as the gateway to the peritoneal cavity. Theoretical advantages of NOTES over the laparoscopic approach include less invasiveness, elimination of any abdominal incision, and reductions in postoperative abdominal wall pain, wound infection, hernia formation, and adhesions.7
Given the established safety profile of the colpotomy, the transvaginal approach has been adopted clinically,8,9 with the proposed benefits of reduced surgical trauma and cosmetic outcomes compared with standard laparoscopic approaches. Numerous data have been reported on NOTES with transvaginal access to perform cholecystectomy,10–12 appendectomy,13 and peritoneoscopy. NOTES for gynecologic surgery, including transvaginal hydrolaparoscopy,12,14 tubal ligation, and so on, has advanced slowly and has been reported rarely. Ectopic pregnancy is the most common life-threatening emergency in early pregnancy. Currently, the surgical treatment for tubal ectopic pregnancy is laparotomy and laparoscopic surgery, and laparotomy has generally been replaced by laparoscopic surgery because of its minimal invasiveness and cosmetic outcomes. The purpose of this randomized study was to prospectively compare the feasibility, safety, efficacy, and cosmetic outcomes of the transvaginal endoscopic approach with laparoscopic salpingectomy for tubal ectopic pregnancy.
MATERIALS AND METHODS
Patients
The study was reviewed and approved by the human investigation review board. Consecutive patients undergoing salpingectomy for tubal ectopic pregnancy were eligible for participation. Potential candidates had to meet the following inclusion criteria: (1) the serum concentration of β-human chorionic gonadotropin is >2000 IU/L and (2) the diameter of sonolucent cul-de-sac fluid is <4 cm (the amount of bleeding may be <800 mL). Exclusion criteria included a history of abdominal surgery except cesarean delivery, pelvic inflammatory disease, suspected severe endometriosis, or vaginitis. Forty patients consented to participate in this study from May 2009 to May 2011. After informed consent was obtained, patients were randomized to undergo salpingectomy with either transvaginal endoscopic access (NOTES group) or laparoscopic access (control group).
Surgical procedure
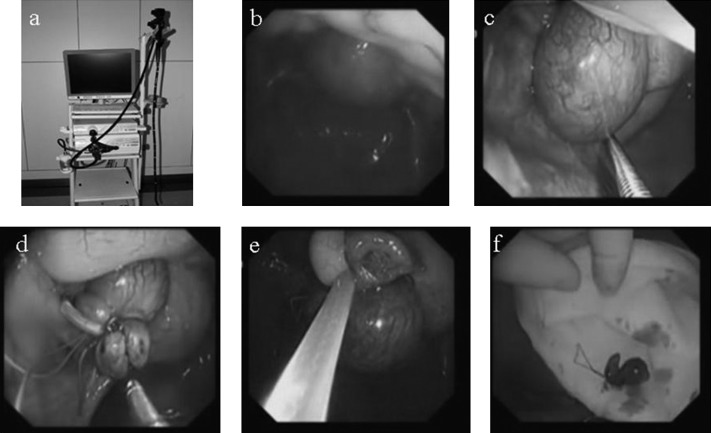
The surgical instruments for transvaginal NOTES salpingectomy consisted of a double-channel endoscope (Olympus GIF-2TQ260M; Olympus, Center Valley, PA, USA) (Figure 1a), nylon loop (Olympus Loop MAJ-340), surgical snare (Olympus SD-210U-15), endoscopic forceps, and high-frequency electric coagulating apparatus (ERBE ICC-200).
Figure 1.
a. Double-channel endoscope (Olympus GIF-2TQ260M). b. Endoscopic image of pelvic cavity. c. Endoscopic image of gestational sac. d. Endoscopic image showing looped ligature around fallopian tube containing ectopic pregnancy. e. Endoscopic image showing electric coagulation and resection of fallopian tube by use of surgical snare. f. Photograph of fallopian tube containing ectopic pregnancy that was removed through vaginal incision.
Under general anesthesia, each patient randomized to undergo transvaginal NOTES was placed in the Trendelenburg position, with the legs bandaged and supported in stirrups. Each operation started with conventional vaginal surgery by creating a 1.5-cm posterior colpotomy. The incision was just 2 mm below the point at which the vaginal mucous wall attached to the cervix. A 10-mm trocar was put into the pelvic cavity through the incision. The posterior colpotomy site was closed with purse-string sutures temporarily to fixed cannulas, and a port in the vagina was established. The double-channel endoscope was inserted into the vaginal puncture, and adequate pneumoperitoneum was established. After the endoscope had entered the pelvic cavity (Figure 1b), the uterus and bilateral adnexa were inspected in detail and salpingectomy was performed (Figure 1c). The fimbrial portion of the oviduct was raised with endoscopic forceps inserted from one channel of the endoscope. The fallopian tube containing the ectopic pregnancy was looped around (Figure 1d), ∼0.5 cm inside of the gestational sac, by a nylon loop inserted from another channel. A surgical snare was used to electrically coagulate and resect the fallopian tube 0.5 cm away from the location of the nylon loop (Figure 1e). The fallopian tube was looped and removed through the vaginal incision (Figure 1f). After hemostasis was verified, the incision in the posterior vaginal wall was manually sutured.
In each patient randomized to laparoscopic salpingectomy, the procedure was performed in standard fashion. On completion of the surgery, the attending surgeon completed a self-administered survey that graded the technical components associated with each procedural step of the salpingectomy using a visual analog scale (VAS) score.
Treatment protocol and follow-up visit
Parenteral cefazolin was administered preoperatively and postoperatively for 24 hours as prophylactic antibiotic therapy. No other oral antibiotic agents were prescribed thereafter if patients were afebrile or without evidence of pelvic infection. Patients were discharged, according to our regulations, with afebrile status for at least 24 hours, no evidence of surgical complications, good wound healing, and full recovery of gastrointestinal function with satisfactory oral intake and stool passage. Postoperative pain was assessed at 4 hours after surgery and then every 24 hours until discharge. Pain was graded with a self-administered VAS score. The time of anal exhaust after operation was recorded to weigh the recovery of gastrointestinal function. The length of stay (LOS) was defined as the number of hours that elapsed between the time when the dressing was applied and the time when the patient was discharged.
At a follow-up visit 1 month after surgery, two supplemental questions were added to assess the patient's satisfaction with the appearance of the wound and the impact the incision had on the patient's life. The responses to these two questions were structured as VAS scores.
All data were prospectively collected and entered into a database. Statistical analysis was performed with the Student t test, after we validated assumptions of normality and homoscedasticity.
RESULTS
Forty patients were randomized. Of the 40 patients, 2 ultimately did not undergo surgery: 1 underwent emergency surgery in the inspection process, and 1 declined participation after randomization. The remaining 38 patients underwent either salpingectomy with transvaginal endoscopic access (n = 18) or laparoscopic salpingectomy (n = 20) (Table 1).
Table 1.
Comparison of Select Perioperative and Postoperative Parameters
| Parameter | Transvaginal Endoscopic Salpingectomy (n = 18) | Laparoscopic Salpingectomy (n = 20) | P Value |
|---|---|---|---|
| Age (y) | 31.72 ± 3.66 | 32.44 ± 3.53 | .48 |
| Duration of amenorrhea (min) | 49.44 ± 4.23 | 49.72 ± 3.83 | .67 |
| Serum concentration of β-HCGa (mIU/mL) | 3418 ± 1732 | 3509 ± 1332 | .68 |
| Duration of surgery (min) | 53.33 ± 7.27 | 49.17 ± 10.45 | .3 |
| Estimated blood loss (>50 mL) | 0 | 0 | — |
| Allogeneic PRBCa transfusion | 0 | 0 | — |
| Time of anal exhaust (h) | 17.44 ± 2.77 | 17.95 ± 3.30 | .61 |
| Global difficulty (score) | 1.56 ± 0.78 | 1.35 ± 0.67 | .39 |
| Postoperative pain score | |||
| Immediate (4 h postoperatively) | 2.22 ± 0.65 | 2.75 ± 0.72 | .02 |
| Day 1 (morning) | 1.78 ± 0.64 | 1.65 ± 0.49 | .49 |
| Day 2 (morning) | 1.06 ± 0.64 | 1.10 ± 0.79 | .85 |
| LOS (d) | 2.2 ± 0.43 | 2.3 ± 0.47 | .6 |
| Satisfaction with incision (score) | 9.17 ± 0.86 | 8.47 ± 0.96 | .03 |
| Impact of incision on patient's life (score)b | 0.18 ± 0.33 | 0.35 ± 0.81 | .28 |
The values are given as mean ± standard deviation or count.
β-HCG = β-human chorionic gonadotropin; PRBC = packed red blood cell.
For the subscale, a VAS was used, which ranged from 1 to 10. The closer the response was to 1, the closer the response paralleled normal skin.
Our data show that patients in the two groups were similar in age, duration of amenorrhea, serum concentration of β-human chorionic gonadotropin, maximum diameter of the adnexal or tubal masses, diameter of cul-de-sac fluid sonolucent area, and pretreatment Gleason score. The duration of time for transvaginal endoscopic surgery was slightly longer than that for the laparoscopic approach. However, there was no statistically significant difference between the two groups in duration of operative time. In addition, technical difficulty and LOS were similar in both groups. The estimated blood loss of each patient in the two groups was <100 mL. None of the patients required blood transfusion. None of the patients had intraoperative cavitas pelvis organ injury or other postoperative complications. Transvaginal NOTES was associated with lower pain scores at the first postoperative visit. The change in postoperative pain scores after that time did not reach statistical significance.
The VAS score for satisfaction with the incision in the transvaginal NOTES group was higher than that in the control group. Overall, 84% of patients in the two groups reported that the incision did not change their life at all, and the VAS scores regarding the incision were similar in the two groups.
DISCUSSION
The first clinical NOTES procedure was carried out by Rao and Reddy in India in a patient whose severe burn injuries to the abdominal wall prohibited safe entry into the peritoneal cavity for conventional surgery (N. Reddy, oral communication, September 2004). Through a transoral, transgastric approach, these surgeons carried out a successful appendectomy.15 In 2007, Marescaux et al.,4 from France, introduced the use of total NOTES cholecystectomy in a human patient. Since then, many further series of pure and hybrid NOTES procedures have been attempted worldwide, and NOTES has improved tremendously in a short time. Numerous procedures have recently been performed through the transvaginal approach, and NOTES surgery is almost always performed with a cholecystectomy or appendectomy.16–19 NOTES for gynecologic surgery, including transvaginal hydrolaparoscopy, transgastric adnexectomy, tubal ligation, and so on, has advanced slowly.
Between May 2009 and April 2012, in our hospital, gynecologists have collaborated with gastroenterologists to successfully complete transvaginal endoscopic salpingectomy (n = 18). The transvaginal endoscopic approach (n = 18) and laparoscopic approach (n = 20) for tubal ectopic pregnancy were performed.
In our prospective research, several factors were compared in the two groups, such as operative time, estimated blood loss, time of anal exhaust, degree of difficulty of surgery, postoperative pain, and patient satisfaction with the incision and quality of life relating to the incision. The purpose was to explore the feasibility, safety, efficacy, and cosmetic outcomes of transvaginal endoscopic salpingectomy for tubal ectopic pregnancy.
Data such as patient age, size of ectopic pregnant sac, and estimated difficulty of salpingectomy by surgery before operation were similar in both groups.
In our patients no pelvic organ damage or other complications occurred as a result of surgery. The amount of blood loss was <100 mL in both groups, and there was no significant difference in blood loss, operative time, time of anal exhaust after operation, and estimated blood loss between the two groups. It was shown that the transvaginal endoscopic approach is repeatable and a safe, minimally invasive surgery as compared with the laparoscopic approach.
It has been reported that hybrid NOTES is safer than pure NOTES. We performed hybrid NOTES in the first case and pure NOTES in 17 cases. There was no pelvic organ damage or other complications. Therefore, the pure NOTES procedure is safe for two reasons. First, the indication for the transvaginal endoscopic approach is strictly limited. Second, the incision that was chosen by us was located just 2 mm below the point at which the vaginal mucous wall attaches to the cervix. To avoid damage to the patient's bladder and rectum, it is important for the trocar to be inserted into the pelvic cavity because the location is far from both organs and easy to puncture. Although pure NOTES is safe, it can be converted to hybrid NOTES, a laparoscopic approach, or even open surgery, if necessary, at any time during surgery. Safety is most important factor during surgery.
As scarless surgery (no incisions in the abdominal wall), transvaginal NOTES eliminates the risk of trocar-site complications, such as bleeding at the trocar site, and induces less postoperative pain and shortens LOS. Our data show that in the group that underwent transvaginal endoscopic salpingectomy, the procedure was associated with lower pain scores at the first postoperative visit. Because there is almost no postoperative pain and no skin incisions, LOS in the NOTES group was shorter than that in the control group. The patient cannot provide a direct assessment scale score regarding the incision because there is no skin incision. Therefore the patient's self described degree of satisfaction and influence on her life were scored by a recorder 1 week after the operation. Even though most patients in both groups did not think that their incisions affected their lives, the scales for patient satisfaction with the incision in the NOTES group are higher than those in the control group because of the scores regarding the abdominal skin in the group. Obviously, NOTES reduced the psychological effect on patients because it caused less pain and yielded higher satisfaction regarding the incision after the operation and decreased cost because of the shorter LOS.
The described surgery involves a transvaginal approach and is thus applicable only to women, and entering the pelvic cavity is direct and safe. In addition, the transvaginal approach is concealing. The specimen is easily removed from the vagina, and the wound is then sutured. Thus the transvaginal approach is the first choice for NOTES regarding gynecologic surgery. Compared with the transvaginal approach, healing of the surgical wound caused by the transgastric approach is difficult and gastric contents always flow outward. Park and Bergstrom20 closed the stomach wall using T-tags in humans, but severe complications developed in one of two cases. Transvaginal gynecologic surgery has evolved over many years and has become very effective. Transvaginal procurement of oocytes has been in practice for >20 years.21 However, it may result in injury to nearby structures, such as the rectum and sigmoid colon. Published studies have shown a higher incidence of certain complications (bladder injury, blood loss, and vaginal hematoma) with a vaginal approach.22 To avoid pelvic cavity infection, we usually use iodophors to scrub the vaginal area preoperatively and anti-infective prophylactic therapy postoperatively.
The key point of the surgery is exposure of the field of vision. One of the 18 cases involved endoscopic and laparoscopic pneumoperitoneum. This is more secure than the other cases, which were completed with endoscopic pneumoperitoneum only, because it can avoid inadvertent injury. The pressure of the pneumoperitoneum is monitored. Carbon dioxide is passed until the pressure reaches 14 to 15 mm Hg and the vision is clear. The double-channel endoscopes can retroflex to provide a 360° visual field.
A difficulty with the surgery is looping of the ligature around the fallopian tube containing the ectopic pregnancy and gestational sac. The double-channel endoscope is flexible, and it is too soft and long to offer the required pulling force when the fallopian tube shifts. In addition, endoscopic forceps have high elasticity and low hardness. The procedure should completely resolve ectopic pregnancy because the fallopian tube containing the ectopic implantation is completely removed. When performing this procedure, we need to pay attention to avoid looping other organs. It is easy and safe to electrically coagulate and resect the fallopian tube after the fallopian tube and gestational sac have been looped and ligated because this method can avoid saturation and stop bleeding completely. If controlling bleeding and serious adherence with this instrumentation and technique are difficult, the surgery may need to be changed to a laparoscopic operation or abdominal incision.
In most reports, laparoscopy and/or digestive endoscopy was used for NOTES. Lee et al.23 used conventional laparoscopic instruments to perform transvaginal NOTES; the limitation is frequent clashing of the instruments, as well as the inability to explore the entire pelvic area and, in particular, the anterior cul-de-sac. In this report we used a double-channel, flexible endoscope in a single vaginal port to complete the surgical procedures. The tip of the endoscope can be turned in 4 different directions to increase surgical exposure. The surgical instruments were used through the different channels of the double-channel endoscope to avoid clashing of the instruments frequently after endoscopic exposure of the pelvic cavity was achieved and the pregnant sac was located.
Only two surgical instruments can be used in the cavitas pelvis simultaneously during the operation, proper exposure in endoscopic surgery is more difficult, and the procedure is interrupted frequently to form pneumoperitoneum. It causes a prolonged operative time. In this study the mean operative time in the NOTES group was 53 minutes, which was slightly longer than that in the control group, at 49 minutes. There was no statistically significant difference between the two groups.
Novel, more sophisticated advanced technologies and instruments have to be developed specifically for NOTES. According to the limited instruments, the candidates of this study were highly selected. In our study, if the diameter of the sonolucent cul-de-sac fluid in the patients was >4 cm, the patients did not meet our criteria. Because the endoscope was in the posterior cul-de-sac, the downward flow of the massive hemoperitoneum and the large amount of irrigation used to wash the pelvic cavity continuously blurred the endoscopic view. At the same time, if a patient had a history of abdominal surgery except cesarean delivery, pelvic inflammatory disease, suspected severe endometriosis, or vaginitis, the patient was not selected for inclusion in either group. Because all of the previously mentioned situations would increase pelvic adhesion and the difficulty of surgery, there was some risk of damage to the pelvic organs. In this report the patient with a maximum diameter of the adnexal or tubal masses >8 cm was excluded from the study because the specimen being removed was prone to damage the adjacent organs of the posterior cul-de-sac, such as the rectum and sigmoid colon. However, the size of the tubal mass was not limited in our study because the sample bag was used to take out large samples. The bag entry was pulled out from a 1.5-cm vaginal incision, and the samples in bags were removed by clamps in small increments. In this manner, we can avoid damage to the pelvic organs.
To our knowledge, this is the first prospective randomized study of NOTES with transvaginal access for salpinges. This study provides new perspective on the application of transvaginal NOTES for salpingectomy, although salpingectomy is one of the more uncomplicated procedures for gynecologic surgery.
In conclusion, the safety and efficacy in the NOTES group for tubal ectopic pregnancy are equivalent to those in the control group. Compared with the control group, there was a slightly longer duration of surgery, less postoperative pain, and a more satisfactory cosmetic outcome in the NOTES group. For ectopic pregnancy in simple cases, the transvaginal endoscopic procedure is the preferred method and is superior to the laparoscopic approach.
Contributor Information
Boqun Xu, Department of Obstetrics and Gynecology, Second Affiliated Hospital of Nanjing Medical University, Nanjing, China..
Yawen Liu, Institute of Digestive Endoscopy & Medical Center for Digestive Diseases, Second Affiliated Hospital of Nanjing Medical University, Nanjing, China..
Xiaoyan Ying, Department of Obstetrics and Gynecology, Second Affiliated Hospital of Nanjing Medical University, Nanjing, China..
Zhining Fan, Department of Obstetrics and Gynecology, Northern Jiangsu People's Hospital, Yangzhou, China..
References:
- 1. Olweny EO, Best SL, Tracy CR, et al. New technology and applied research: what the future holds for LESS and NOTES. Arch Esp Urol. 2012;65(3):434–443 [PubMed] [Google Scholar]
- 2. Masoomi H, Mills S, Dolich MO, et al. Comparison of outcomes of laparoscopic versus open appendectomy in adults: data from the Nationwide Inpatient Sample (NIS), 2006–2008. J Gastrointest Surg. 2011;15(12):2226–2231 [DOI] [PubMed] [Google Scholar]
- 3. Trastulli S, Cirocchi R, Listorti C, et al. Laparoscopic vs open resection for rectal cancer: a meta-analysis of randomized clinical trials. Colorectal Dis. 2012;14(6):e277–e296 [DOI] [PubMed] [Google Scholar]
- 4. Marescaux J, Dallemagne B, Perretta S, et al. Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg. 2007;142(9):823–826; discussion 826–827 [DOI] [PubMed] [Google Scholar]
- 5. Lehmann KS, Ritz JP, Wibmer A, et al. The German registry for natural orifice translumenal endoscopic surgery: report of the first 551 patients. Ann Surg. 2010;252(2):263–270 [DOI] [PubMed] [Google Scholar]
- 6. Zornig C, Siemssen L, Emmermann A, et al. NOTES cholecystectomy: matched-pair analysis comparing the transvaginal hybrid and conventional laparoscopic techniques in a series of 216 patients. Surg Endosc. 2011;25(6):1822–1826 [DOI] [PubMed] [Google Scholar]
- 7. Moris DN, Bramis KJ, Mantonakis EI, et al. Surgery via natural orifices in human beings: yesterday, today, tomorrow. Am J Surg. 2012;204(1):93–102 [DOI] [PubMed] [Google Scholar]
- 8. Campo R, Gordts S, Brosens I. Minimally invasive exploration of the female reproductive tract in infertility. Reprod Biomed Online. 2002;4(Suppl 3):340–345 [DOI] [PubMed] [Google Scholar]
- 9. Gordts S, Watrelot A, Campo R, et al. Risk and outcome of bowel injury during transvaginal pelvic endoscopy. Fertil Steril. 2001;76(6):1238–1241 [DOI] [PubMed] [Google Scholar]
- 10. Targarona EM, Maldonado EM, Marzol JA, et al. Natural orifice transluminal endoscopic surgery: the transvaginal route moving forward from cholecystectomy. World J Gastrointest Surg. 2010;2(6):179–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Auyang ED, Hungness ES, Vaziri K, et al. Human NOTES cholecystectomy: transgastric hybrid technique. J Gastrointest Surg. 2009;13(6):1149–1150 [DOI] [PubMed] [Google Scholar]
- 12. Zorron R, Palanivelu C, Galvao Neto MP, et al. International multicenter trial on clinical natural orifice surgery—NOTES IMTN study: preliminary results of 362 patients. Surg Innov. 2010;17(2):142–158 [DOI] [PubMed] [Google Scholar]
- 13. Chu T, Chandhoke RA, Smith PC, et al. The impact of surgeon choice on the cost of performing laparoscopic appendectomy. Surg Endosc. 2010;25(4):1187–1191 [DOI] [PubMed] [Google Scholar]
- 14. Darai E, Dessolle L, Lecuru F, et al. Transvaginal hydrolaparoscopy compared with laparoscopy for the evaluation of infertile women: a prospective comparative blind study. Hum Reprod. 2000;15(11):2379–2382 [DOI] [PubMed] [Google Scholar]
- 15. Buyske J. Natural orifice transluminal endoscopic surgery. JAMA. 2007;298(13):1560–1561 [DOI] [PubMed] [Google Scholar]
- 16. Hazey JW, Narula VK, Renton DB, et al. Natural-orifice transgastric endoscopic peritoneoscopy in humans: initial clinical trial. Surg Endosc. 2008;22(1):16–20 [DOI] [PubMed] [Google Scholar]
- 17. Palanivelu C, Rajan PS, Rangarajan M, et al. Transvaginal endoscopic appendectomy in humans: a unique approach to NOTES—world's first report. Surg Endosc. 2008;22(5):1343–1347 [DOI] [PubMed] [Google Scholar]
- 18. Palanivelu C, Rajan PS, Rangarajan M, et al. Transumbilical flexible endoscopic cholecystectomy in humans: first feasibility study using a hybrid technique. Endoscopy. 2008;40(5):428–431 [DOI] [PubMed] [Google Scholar]
- 19. Forgione A, Maggioni D, Sansonna F, et al. Transvaginal endoscopic cholecystectomy in human beings: preliminary results. J Laparoendosc Adv Surg Tech A. 2008;18(3):345–351 [DOI] [PubMed] [Google Scholar]
- 20. Park PO, Bergstrom M. Transgastric peritoneoscopy and appendectomy: thoughts on our first experience in humans. Endoscopy. 2010;42(1):81–84 [DOI] [PubMed] [Google Scholar]
- 21. Schulman JD, Dorfmann AD, Jones SL, et al. Outpatient in vitro fertilization using transvaginal ultrasound-guided oocyte retrieval. Obstet Gynecol. 1987;69(4):665–668 [PubMed] [Google Scholar]
- 22. Milad MP, Morrison K, Sokol A, et al. A comparison of laparoscopic supracervical hysterectomy vs laparoscopically assisted vaginal hysterectomy. Surg Endosc. 2001;15(3):286–288 [DOI] [PubMed] [Google Scholar]
- 23. Lee CL, Wu KY, Su H, et al. Transvaginal natural-orifice transluminal endoscopic surgery (NOTES) in adnexal procedures. J Minim Invasive Gynecol. 2012;19(4):509–513 [DOI] [PubMed] [Google Scholar]