Abstract
The global spread of the 2009 pandemic H1N1 (pH1N1) virus in humans increases the likelihood that this influenza virus strain could undergo antigenic drift in the coming years. Previous seasonal H1N1 and H3N2 influenza strains acquired additional glycosylations in the globular head of their hemagglutinin (HA) proteins as they evolved over time; these are believed to shield antigenically relevant regions. We used influenza A/Netherlands/602/2009 recombinant (rpH1N1) viruses to which we added additional HA glycosylation sites reflecting their temporal appearance in previous seasonal H1N1 viruses. Additional glycosylations resulted in substantial attenuation in mice and ferrets, while deleting HA glycosylation sites from a pre-pandemic 1991 seasonal H1N1 influenza virus resulted in increased pathogenicity in mice. Sera from mice infected with wild type (WT) rpH1N1 virus showed a considerable loss of HA inhibitory (HI) activity against rpH1N1 viruses glycosylated at sites 144 or 144-172, indicating that the polyclonal antibody response elicited by WT rpH1N1 HA seems to be directed against an immunodominant region, likely site Sa, shielded by glycosylation at 144. Sera from humans vaccinated with the pH1N1 inactivated vaccine also showed reduced activity against the 144 and 144-172 mutant viruses. Remarkably, the HI activity of sera from virus-infected mice demonstrated that glycosylation at position 144 resulted in the induction of a broader polyclonal response able to cross-neutralize all WT and glycosylation mutant pH1N1 viruses. Mice infected with a recent seasonal virus in which glycosylation sites 71, 142 and 177 were removed, elicited antibodies that protected against challenge with the antigenically distant pH1N1 virus. Thus, acquisition of glycosylation sites in the HA of H1N1 human influenza viruses not only affects their pathogenicity and ability to escape from polyclonal antibodies elicited by previous influenza virus strains, but also their ability to induce cross-reactive antibodies against drifted antigenic variants. These findings provide the basis for designing improved vaccines and immunization strategies capable of protecting against a broader range of influenza virus strains.
Introduction
Influenza A virus infections remain a major concern causing a substantial burden to public health, with estimated annual medical costs of approximately $10.4 billion dollars in the US (1). The emergence of the 2009 pandemic H1N1 (pH1N1) virus provided the first direct evidence that previously circulating subtypes, given enough time, can cause a novel pandemic due to the increased proportion of the human population being naïve to the hemagglutinin (HA) of this new strain (a re-emerging subtype) (2). Thus, the level and quality of cross-protective HA antibodies play an important role in determining the pandemic potential of a novel influenza A virus strain.
We and others have previously demonstrated that the HA of the 2009 pH1N1 strain shares antigenic similarities to the HA of human H1N1 viruses that circulated prior to 1950, including substantial homology to the 1918 virus (3–6), specifically around antigenic site Sa (3, 7, 8). In contrast, vaccination (3, 6) or infection (4) with contemporary seasonal H1N1 strains induces little or no cross-reactivity to the 2009 pH1N1 virus, which correlates with a greater difference at the amino acid level seen at or near the known antigenic sites located in the globular head of the HA (3).
Previous seasonal H1N1 and H3N2 influenza viruses circulating in humans have been shown to undergo antigenic drift (a gradual accumulation of amino acid changes in or around the HA antigenic sites) due to immune selection pressure. Some of these residue changes resulted in the acquisition of glycosylation sites in the HA, some of which are maintained, while others are replaced or disappear over time, suggesting that HA glycosylation plays an important evolutionary role in human influenza A viruses (9–11). Recent studies have shown that HA glycosylation can affect the antigenic and receptor binding properties of this viral protein (12), as well as the virulence of influenza viruses (13–15). Of interest, a number of glycosylation sites on the globular head of the HA were temporally acquired from 1918 to 2009 by the seasonal H1N1 viruses and most of these are located within or near antigenic site Sa (9–11). In contrast, the 2009 pH1N1 virus lacks these additional glycosylation sites and shares the same glycosylation pattern as the 1918 H1N1 pandemic virus. Importantly, the HA glycosylations acquired by the seasonal H1N1 viruses have been proposed to shield antigenic sites from antibody mediated neutralization and to be an important factor influencing the serum cross-reactivity seen in the general population between the recently extinguished seasonal H1N1 viruses and the 2009 pH1N1 and 1918 pandemic viruses (6, 16, 17). However, the specific role that each of the H1 glycosylation sites plays in the virulence and antigenic properties of the 2009 pH1N1 has not been addressed.
The 2009 pH1N1 strain has spread globally since its original outbreak in North America, and it is now circulating seasonally in the Northern and Southern hemispheres, replacing the previous H1N1 viruses. It is expected that the pH1N1 virus will start to undergo antigenic drift driven by immune selection pressure. Acquisition of glycosylations might contribute to the emergence of H1N1 drift variants. In this study we investigated the specific effects of the acquisition of glycosylations in the globular head of the H1N1 HA on virulence and antigenic properties of H1N1 viruses. Our results indicate that HA glycosylation plays a crucial role in both pathogenesis and in escape from pre-existing immunity, as well as in induction of cross-reactive polyclonal antibody responses.
Results
H1N1 human viruses acquired glycosylation sites in the globular head of the HA protein over time
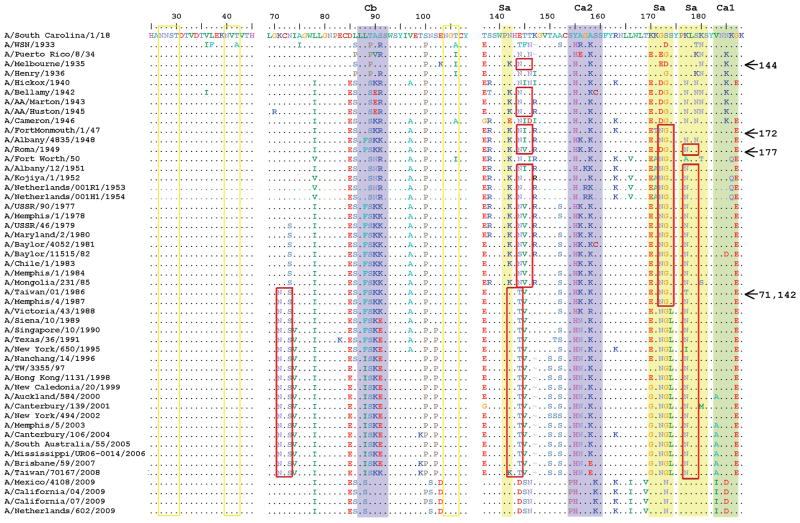
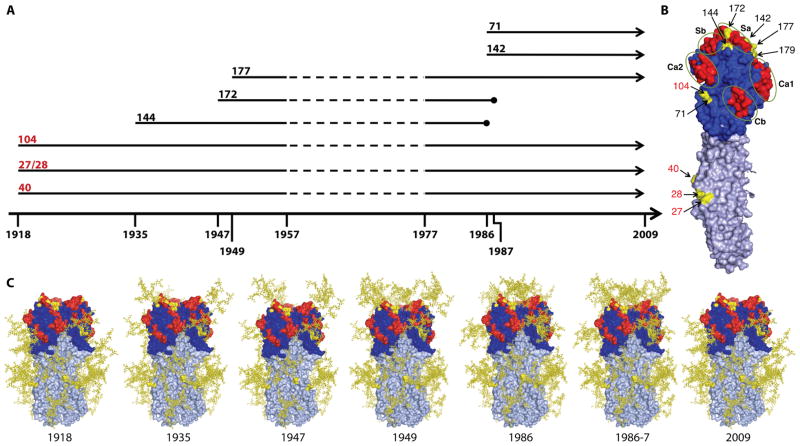
A complete analysis of the amino acid sequence of the 1918 and the 2009 H1N1 pandemic viruses revealed that the HA1 of these viruses are putatively glycosylated at the same sites. On the other hand, the 2009 H1N1 HA protein showed distinct antigenic properties with respect to previously circulating seasonal H1N1 strains. To better understand the differences that might be responsible for these different properties, we focused our analysis on the amino acid sequences around the known antigenic sites. Sequence alignments revealed that since the introduction of the H1N1 viruses into humans in 1918, a number of glycosylation sites, as predicted by the motif N-X-S/T, have been acquired in the HA globular head over time (Fig. 1). Of interest, these glycosylation sites appeared predominantly near or within antigenic site Sa (Fig. 1). Although there are no sequences available of human influenza viruses between 1918 and 1933, and with the caveat that most of the sequences from early H1N1 viruses are from strains that have been passaged extensively in eggs and/or nonhuman mammalian laboratory cell cultures, it appears that during the years 1935 to 1957, three different HA glycosylations were acquired sequentially (at amino acid residues 144, 172 and 177 [H3 numbering: 130, 158 and 163, respectively], highlighted in Fig. 1 and 2) that were consistently found in human isolates. The emergence of the H2N2 pandemic influenza virus in 1957 displaced the H1N1 viruses, which disappeared from human circulation. The H1N1 virus strain re-emerged in humans in 1977 and contained the same HA glycosylation sites as the H1N1 viruses circulating in the 1950s. In 1986, glycosylation site 144 was replaced by a glycosylation on position 142 (H3 numbering: 128; these glycosylation sites are incompatible), and an additional glycosylation on site 71 (H3 numbering: 59) was acquired almost simultaneously. In 1987 glycosylation site 172 was lost, and since then the circulating H1N1 viruses, including those circulating just prior to the emergence of 2009 pH1N1, contained glycosylation sites 71, 142 and 177 in the globular head of HA (Fig. 2A–C). Since the glycosylation status of the 2009 pH1N1 is the same as that of the 1918 H1N1 pandemic virus, the 2009 pH1N1 virus has the potential to acquire the same or similar glycosylations over time as a result of immune selection pressure (6). We then assessed the specific effect of additional glycosylations on virulence and antigenic properties of the 2009 pH1N1 virus.
Fig. 1. Acquisition of glycosylation sites in HA of human H1N1 subtype over time prior to the emergence of the 2009 H1N1 virus.
Amino acid alignment of antigenic sites in the HA1 of seasonal H1N1 strains circulating in humans since 1918 until just prior to the emergence of the 2009 H1N1 pandemic virus. Four representative 2009 H1N1 pandemic isolates are also included as reference. Alignment shows selected prototypical reference strains. Colored shading (purple, yellow and green) depicts known antigenic sites listed on top. Yellow boxes represent conserved glycosylations and red boxes represent glycosylations that appear and disappear over time. Arrows on the right show the year glycosylations appeared at the indicated residue positions.
Fig. 2. Modeling of H1N1 glycosylations over time.
(A) Time line illustrating the year of acquisition of glycosylations in the globular head of the HA protein. Numbers in red indicate the amino acid position of the glycosylation site that are conserved amongst human H1N1 isolates since their emergence in 1918, and numbers in black indicate the amino acid position of the glycosylation sites that appeared in the specific years shown at the bottom. Arrows denote the persistence of glycosylation sites through time, and circles represent their disappearance. Discontinuous lines indicate the time period from 157 to 177 when H1N1 viruses did not circulate in humans. (B) Representation of an HA monomer with the antigenic sites highlighted in red and the glycosylation sites in yellow. The stem region of HA is denoted in silver. Amino acid positions refer to the H1 nomenclature (sites 71, 142, 144, 172 and 177 correspond to H3 numbering 58, 128, 130, 158 and 163, respectively). Numbers in red indicate conserved glycosylation sites. (C) Structural modeling of the trimeric HA with glycosylations as they appeared over time from 1918 to the emergence of the 2009 pH1N1 virus. The glycan structures for the sites shown in yellow have been modeled onto the Cal/09 HA (PDB 3LZG) and are also depicted in yellow. All models were made with MacPyMol.
Additional glycosylations in the globular head of the HA attenuate the pH1N1 virus in vivo but not in vitro
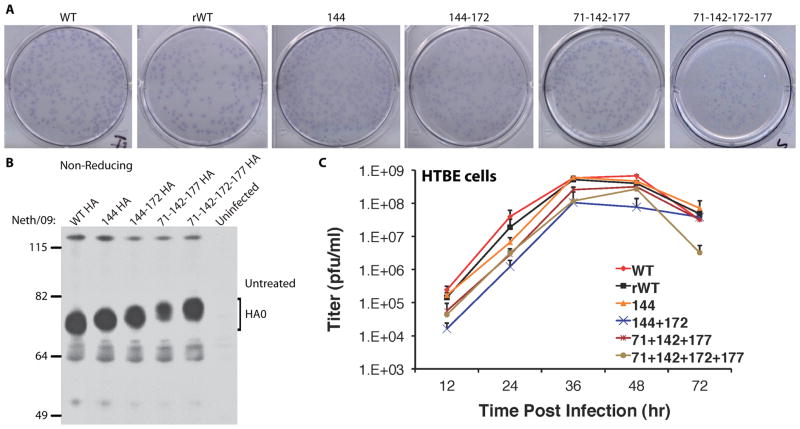
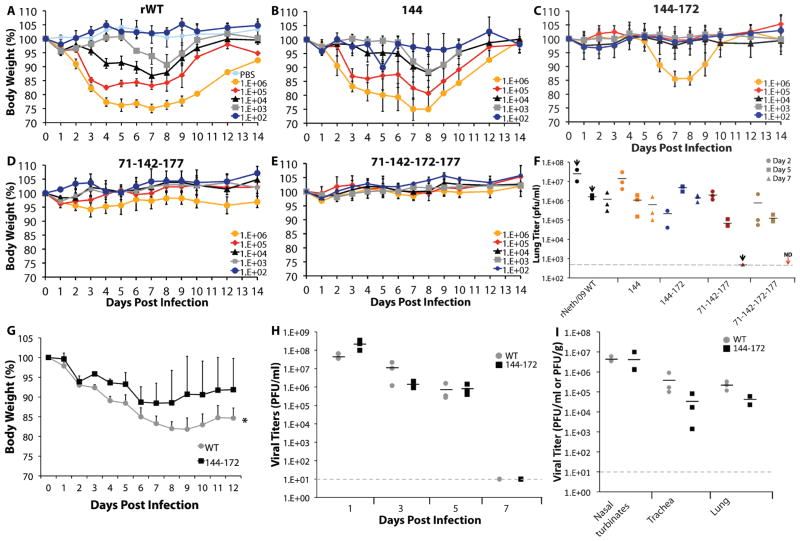
We generated 2009 pH1N1 (Neth/09 strain) recombinant viruses differing only by the sequential addition of HA glycosylations to mimic the temporal appearance of these sites in the seasonal H1N1s. Despite several attempts we were unable to rescue a virus containing the HA glycosylation sites 144, 172 and 177 in the Neth/09 background, suggesting that the combination of these specific glycosylations might require additional compensatory mutations. Nevertheless, all other mutant viruses were successfully rescued. In vitro phenotypic analyses of these recombinant viruses showed that only the virus containing 4 additional glycosylations (Neth/09 HA 71-142-172-177) had a smaller plaque phenotype in MDKCs (Fig. 3A). Addition of HA glycosylation sites resulted in slower mobility of the HA in SDS-PAGE, consistent with the use of these sites (Fig. 3B). Analysis of the HA content of each of the mutant viruses revealed that the glycosylation mutants had a decreased amount of HA incorporated into virions as compared to the rWT virus (Supp. Fig. 1). When we assessed the viruses’ susceptibility to the antiviral drug oseltamivir, a neuraminidase inhibitor, we found no detectable differences amongst all the recombinant viruses utilizing the NA Star chemiluminescent substrate cleavage assay. In a tissue culture virus replication assay we observed that all viruses displayed similar sensitivity to oseltamivir (Supp. Fig. 2A and B). We performed growth kinetics to evaluate the effects of these glycosylations on the virus’ ability to replicate in primary differentiated human tracheobroncheal epithelial cells (HTBE). All viruses replicated at high levels (>107 pfu/ml), similar to those of the original WT Neth/09 isolate virus (Fig. 3C), indicating that these additional glycosylations did not affect infection of human cells. We next evaluated the pathogenic potential of the recombinant glycosylated viruses in C57BL/6 mice. We found a glycosylation dependent attenuation of virulence in mice (i.e. the more glycosylation sites in the HA the less pathogenic), as assessed by body weight loss (Fig. 4A–E). Only the virus containing glycosylation site 144 showed weight loss patterns similar to those seen in mice infected with WT Neth/09 virus (Fig. 4B). All viruses with two or more extra glycosylation sites were severely attenuated (Fig. 4C–E). Morbidity correlated with lung viral titers in mice during the initial 7 days of infection. Animals infected with the 144-172, 71-142-177 and 71-142-172-177 had substantially lower titers as compared to WT Neth/09.
Fig. 3. Phenotypic characterization of HA glycosylation mutant 2009 pH1N1 viruses.
(A) Plaque morphology of rescued A/Netherlands/602/2009 HA glycosylation mutant viruses in MDCK cells. (B) Western blot analysis of whole cell lysates obtained from MDCK cells infected at an MOI of 5 for 12 h. Lysates were run under non-reducing conditions and blots were detected with rabbit polyclonal antiserum 3951 raised against a PR8 virus lacking H1, which had been removed by acid and DTT treatment. (C) Growth kinetics of rescued viruses in differentiated human tracheobrochial epithelial cells infected at an MOI of 0.001. Data are shown as the average of virus titrations conducted in triplicates for each time point shown by standard plaques assay in MDCK cells. The error bars represent the +/− SD at each time point.
Fig. 4. 2009 pH1N1 viruses with additional glycosylations in the HA are attenuated in mice and ferrets.
(A – E) Infection of 9-week-old female C57B/6 mice with Neth/09 glycosylation mutant viruses. Groups of 5 mice per recombinant virus were infected i.n. with the indicated doses. Body weight represents the average of each group and the error bars indicate the +/− SD at each time point. (F) Viral titer in the lungs of mice infected with 1×103 pfu of each mutant virus were obtained on days 2 (circle), 5 (square), and 7 (triangle) p.i. as shown. Black bars represent the average viral titer for 2 (arrows) or 3 mice per group at each time point as compared to the rNeth/09 WT virus. N.D. = Not detected. (G) Body weight changes in ferrets infected (n=3 per group) with the indicated viruses. Weights are shown as the average and the error bars represent the +/− SD. at each time point. Statistically significant difference (*) of the overall body weight of ferrets during the infection period was estimated with the Wilcoxon-matched pairs test. (H) Viral titers in nasal washes obtained every other day from ferrets shown in (G). (I) Viral load in tissues from ferrets (n=3) at day 3 p.i. with the indicated viruses. Values are represented as in (F).
To determine if this is also the case in a different animal model, we assessed the virulence of the first mutant virus that demonstrated a drastic difference in morbidity in mice, the144-172 glycosylated virus, as compared to the WT virus in ferrets, which is widely accepted as one of the best animal models to study pathogenesis of influenza viruses. There was a statistically significant decrease in the overall weight loss seen in the animals infected with the 144-172 virus (Fig. 4G). Interestingly, the nasal wash titers obtained from both groups through day 7, and titers of the nasal turbinates on day 3 showed no differences (Figs. 4H and I). However, the trachea and the lungs of ferrets at day 3 showed a lower virus titer for the 144-172 virus as compared to WT Neth/09 (Fig. 4I). This suggests that while glycosylated H1N1 viruses can replicate to similar levels in the upper respiratory track (in the nose), they are less able to infect and replicate in the lower respiratory track (trachea and lungs).
HA glycosylation site 144 evades the polyclonal antibody response against WT HA while inducing a broader polyclonal response in mice
To gain insights into the effects of glycosylation on the antigenic properties of the H1N1 viruses, we tested the HA inhibitory (HI) activity of sera obtained from mice infected with each of the glycosylation mutant viruses against each other (Table 1). We attempted to confirm the antigenic integrity of the mutant viruses during infection by sequencing the HA and NA genes. No compensatory changes were found for virus with glycosylation 144 during the first 5 days of infection. At the dose given (1×103 pfu), no sequences were obtained at day 2 p.i. for the other glycosylated viruses, suggesting that they are cleared soon after the infection and that the humoral response observed is raised against the original inoculums. Nevertheless, we cannot rule out that compensatory mutations might still arise during this short period of infection. The WT 2009 H1N1 virus is highly immunogenic (3), therefore mice infected with rWT virus had consistently higher HI titers than mice infected with any of the glycosylation mutant viruses. In order to compare the cross-reactivity of sera, we used samples that had a homologous HI titer of 320–160, except for samples obtained from infection with a virus glycosylated only on site 177 that had a homologous HI titer of 80 (Table 2). Infection of mice with rWT virus or the 71-142-177 or 71-142-172-177 glycosylated viruses resulted in low or no detectable sera HI activity to the glycosylated viruses 144 and 144-172, while varying levels of cross-reactivity remained against the other viruses. Surprisingly, infection with viruses containing the 144 or the 144-172 glycosylations elicited antibody responses capable of cross-reacting with all of the HA glycosylation mutant viruses and the WT Neth/09 virus in the HI assay. This was also true when we tested the neutralizing activity of sera obtained from mice infected with the rWT and 144 viruses. The 144 sera neutralized both viruses at similar levels, while the rWT sera had a 4 fold lower neutralizing activity against the 144 glycosylated virus as compared to its homologous neutralizing activity (Supp. Fig 3). We speculated that glycosylation site 142, which is only two amino acids apart from site 144, might also confer the same HI activity. Thus, to determine whether the specific effects on the breadth of neutralization seen was a distinct feature of glycosylation site 144, we generated additional viruses carrying a single glycosylation site at position 142 or 172 or 177, as well as a virus with two glycosylation sites at positions 71 and 142. The viruses containing 142, 172 and 71-142 were severely attenuated in mice, similar to the viruses carrying two or more glycosylations, whereas the virus containing a glycosylation at site 177 caused weight loss similar to that caused by the virus containing site 144 (Suppl. Fig 4). Remarkably, analysis of HI activity elicited by infection with these viruses showed that other single or double glycosylations, including site 142, resulted in a narrower humoral response that had no activity against viruses containing site 144 (Table 2). Taken together, this indicates that most of the polyclonal HI activity induced by the viruses is directed against one site, likely site Sa. This site seems to be efficiently masked by the 144 glycosylation and thus viruses carrying the 144 glycosylation can escape the response elicited by all other glycosylation mutant viruses. Moreover, glycosylation at position 144 changes the pattern of the polyclonal antibody response, which now appears to be against multiple antigenic regions in the HA and is not masked by a single or multiple glycosylation events. In contrast, infection with viruses containing other single glycosylations or glycosylations at positions 71-142, 71-142-177 or 71-142-172-177 induce a narrower cross-reactivity pattern, suggesting that the polyclonal humoral response is slightly changed but remains focused, possibly around site Sa.
Table 1.
HI titers of mouse sera after infection with 2009 pH1N1 HA glycosylation mutant viruses.
| Virusb,c | Seraa | ||||
|---|---|---|---|---|---|
| rWT | 144 | 144-172 | 71-142-177 | 71-142-172-177 | |
| rWT | 320 | 320 | 160 | 40 | 20 |
| 144 | 10 | 160 | 80 | <10 | <10 |
| 144-172 | 20 | 80 | 160 | <10 | 40 |
| 71-142-177 | 80 | 160 | 160 | 160 | 160 |
| 71-142-172-177 | 160 | 160 | 320 | 160 | 160 |
Mice were infected with the recombinant Neth/09 virus containing HA glycosylations at the indicated residues.
HI titers represent the reciprocal of the highest dilution that displayed hemagglutination inhibitory activity.
Homologous titers are in bold.
Table 2.
HI titers of mouse sera after infection with 2009 pH1N1 HA single and double glycosylation mutant viruses.
| Virusb,c | Seraa | |||
|---|---|---|---|---|
| 142 | 172 | 177 | 71-142 | |
| rWT | 80 | 80 | 80 | 80 |
| 144 | <10 | <10 | <10 | <10 |
| 144-172 | <10 | 10 | <10 | <10 |
| 71-142-177 | 160 | 40 | 80 | 320 |
| 71-142-172-177 | 80 | 160 | 40 | 80 |
| 142 | 160 | 160 | 160 | 160 |
| 172 | 160 | 320 | 320 | 160 |
| 177 | 80 | 80 | 80 | 80 |
| 71-142 | 80 | 40 | 80 | 320 |
Mice were infected with the recombinant Neth/09 virus containing HA glycosylations at the indicated residues.
HI titers represent the reciprocal of the highest dilution that displayed hemagglutination inhibitory activity.
Homologous titers are in bold.
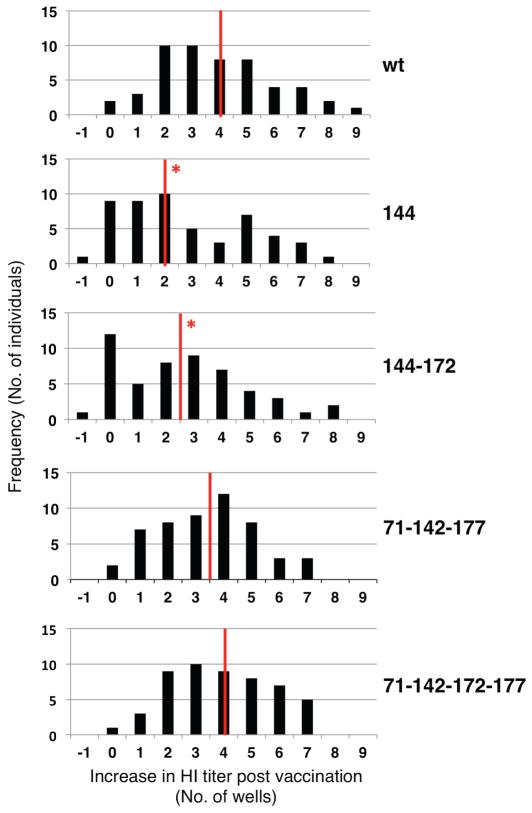
HA glycosylation site 144 evades the polyclonal antibody response against pH1N1 inactivated vaccine in humans
We next tested whether the 2009 pH1N1 inactivated vaccine (study DMID 09-0047) elicited antibody responses in humans with inhibitory activity against 2009 H1N1 viruses bearing glycosylated HAs. We found that most adult individuals that received the 2009 pH1N1 monovalent vaccine had detectable antibody responses to all the glycosylation mutant viruses (Fig. 5 and Supp. Table 1). Nonetheless, the lowest cross-reactivity was seen with viruses containing the 144 (and the 144-172) glycosylation sites. Since the level of previous exposure to influenza virus in humans could impact their polyclonal antibody responses, we also assessed the sera HI titers in a more naïve population (children <18 years of age) that were immunized with the monovalent p2009 H1N1 inactivated vaccine. The sera activity of pediatric individuals also had a similar cross-reactivity pattern to the ones of adults, showing lower HI activity against the 144 and the 144-172 glycosylation mutant viruses compared to WT, 71-142-177 or 71-142-172-177 glycosylated viruses (Supp. Table 1). Overall, 10 to 13 individuals showed undetectable increases in HI activity levels when tested against the 144 and the 144-172 viruses (versus only 2 individuals when the other viruses were used, including the WT). When we analyzed the distribution of the increase in HI activity against each glycosylation mutant virus, we found that there was a significantly lower median of the distribution for viruses 144 and 144-172 but not for viruses 71-142-177 and 71-142-172-177 (Fig. 5). This is in close agreement with the mouse serology results, emphasizing the masking effects of glycosylation at site 144. As expected, the trivalent seasonal vaccine of 2009 containing a previously circulating seasonal H1N1 virus, did not induce significant HI titers against pH1N1 viruses, independently of their level of glycosylation (Supp. Table 1).
Fig. 5. HI activity of human sera after vaccination against pandemic 2009 H1N1.
Pre- and post-vaccination sera samples obtained from 52 subjects enrolled in clinical trials to test the safety and immunogenicity of an inactivated 2009 H1N1 influenza vaccine, were tested for their HI activity against WT Neth/09 and the glycosylation mutant viruses. For each subject the difference in HI activity between post- and pre-vaccination (HI titer post-vaccination – HI titer pre-vaccination in number of wells) was determined to normalize for pre-existing HI activity. For each virus the distribution of increase in HI activity post vaccination is plotted. The median of the distribution is marked with a red line and statistically significant differences were determined with the Wilcoxon rank sum test.
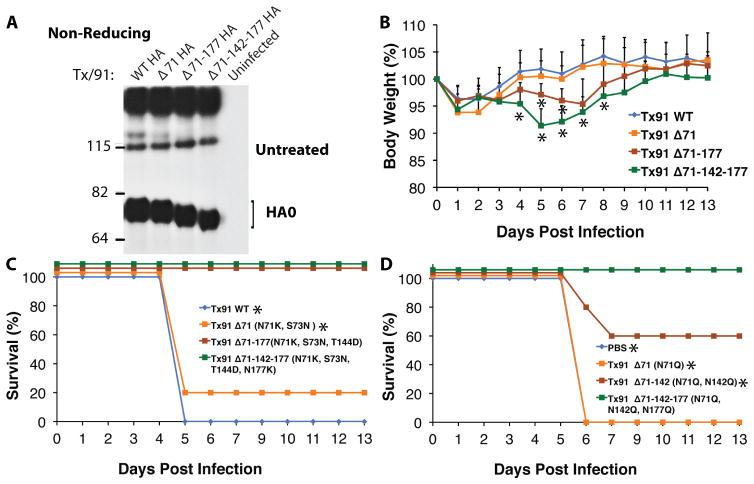
Glycosylation deletions in a recent seasonal H1N1 virus increase its in vivo virulence and elicit cross-protection against pH1N1 2009 virus challenge
To further elucidate the role of HA glycosylations in the pathogenic and antigenic properties of H1N1 viruses, we generated a set of recombinant A/PR8/34 7:1 Tx/91 HA (rWT Tx/91) glycosylation deletion viruses. The contemporary Tx/91 seasonal strain contains three extra glycosylation sites, on sites 71, 142 and 177. Elimination of HA glycosylation sites resulted in faster HA mobility in SDS-PAGE, as expected (Fig. 6A). Infection with a sublethal dose of rWT Tx/91 virus (at 1×103 pfu) did not result in morbidity in mice. However, infection with viruses containing deletions of 2 or 3 glycosylations (rTx/91 Δ71-177 and rTx/91 Δ71-142-177) resulted in a significant level of weight loss as compared to the rWT Tx/91 virus (Fig. 6B). The highest morbidity was observed in the Δ71-142-177 virus, a virus that resembles the 2009 pH1N1 in that it has no glycosylation sites in the globular head of HA. This again confirms that glycosylations of HA negatively affect the in vivo pathogenic potential of human H1N1 viruses. To investigate if infection with these glycosylation deletion viruses can elicit cross-protective humoral responses to the antigenically highly distant WT 2009 H1N1 virus, we challenged these animals on day 27 p.i. with 100 times the 50% lethal dose (LD50) of WT Neth/09 virus. The mice previously infected with rWT Tx/91 all succumbed to the Neth/09 challenge, and the mice infected with the virus containing a single deleted glycosylation on site 71 (Δ71) showed substantial weight loss and only a 20% survival rate (Fig. 6C). In contrast, although the animals infected with viruses with glycosylation deletions on sites 71-177 (Δ71-177) and 71-142-177 (Δ71-142-177) showed a substantial loss in body weight (up to ~20%) they all survived the lethal challenge with Neth/09, with animals infected with Δ71-142-177 showing an overall lower morbidity level (Fig. 6C). We sequenced lung homogenates at 2 and 5 days p.i. to evaluate if additional adaptive or compensatory mutations emerged during infection in mice. No sequence changes were detected in the homogenates analyzed, indicating that removal of the HA glycosylations in these viruses was responsible for the increased pathogenicity and cross-reactive humoral response observed. Since the introduced amino acid substitutions (N71K, S73N, T144D and N177K) not only deleted the glycosylations sites at positions 71, 142 and 177 but also made the Tx/91 antigenic site Sa resemble that of Neth/09, we generated a second set of mutant viruses containing the non-related amino acid substitutions N71Q, N142Q and N177Q, respectively. Mice infected with the viruses with two or three glycosylation deletions also showed an increased weight loss (Suppl. Fig 5) and when challenged 29 days p.i. they also had an enhanced protection against a lethal challenge with 100 LD50 of WT Neth/09 (fig. 6D). These data show that HA glycosylations play an important role in masking antigenic sites and in eliciting protective immune responses against antigenically diverse H1N1 influenza virus strains.
Fig. 6. Deletion of glycosylation sites in the HA of Tx/91 increases virulence in mice and cross-protects against the 2009 pH1N1 strain.
Phenotypic characterization of recombinant influenza A viruses carrying either the wild type or glycosylation deletion mutant A/Texas/36/1991 HAs (N71K + S73N, T144D, N177K) and the remainder 7 genes from PR8 (viruses are 7:1 rPR8 expressing Tx/91 HA). (A) Western blot analysis of lysates obtained from MDCK cells infected at an MOI of 5 for 12 h with the respective glycosylation deletion mutant viruses. Lysates were run under reducing conditions and blots were detected with the polyclonal 3951 antibody. (B) 8-week-old female C57B/6 mice infected with 1×104 pfu of each virus shown. Average body weight of mice n=5 per group. Error bars denote the +/− SD for each time point. (C) Mice infected in panel B were allowed to seroconvert for 27 days at which time they were challenged with 100 LD50 of Neth/09. Percent survival is shown. (D) Mice infected with 1×104 pfu of each glycosylation deletion mutant, in which the same glycosylation sites were removed by an alternative set of amino acid substitutions to those used in B and C. At 29 days p.i. mice were challenged with 100 LD50 of Neth/09. Percent survival after challenge is shown. The student’s t-test was used to determine significance of body weight loss and the log-rank test was used to assess significance (* P<0.05) of survival outcome.
Discussion
In this study we have evaluated the effect of glycosylations in the HA protein on virulence and antigenic cross-reactivity in the context of the current 2009 pH1N1 strain. Utilizing a set of recombinant 2009 pH1N1 viruses engineered to mimic the temporal acquisition of glycosylations in the HA protein as those observed for the historical seasonal H1N1 viruses, we demonstrate that glycosylations play an important role in modulating the pathogenesis and the antigenic properties of these viruses.
Initial sequence analysis of the 2009 pH1N1 virus revealed a drastic difference as compared to the seasonal H1N1 viruses (Bris/59-like) that were circulating worldwide at the time of the outbreak (18–20). Close analysis of the HA protein, and experimental studies from us and others (3–6), showed that the 2009 pandemic virus was more closely related to older H1N1 viruses that circulated in humans before the 1950’s. The HA of the H1N1 seasonal viruses has acquired glycosylation sites during its evolution in humans, likely as a result of immune selection pressure. Of interest, a number of glycosylations have emerged but eventually disappeared and some became fixed in time (Fig. 1)(9). This suggests that during viral evolution, some of these glycosylations can be deleterious for the virus, while others might provide fitness and/or an immune escape advantages resulting in the emergence of drift variants in humans. Because the 2009 pH1N1 and the 1918 H1N1 pandemic viruses have the same glycosylation pattern in HA1, there is a possibility that with time the 2009 pH1N1 strain might undergo a similar evolutionary pattern and might acquire similar glycosylations in the HA as observed previously with the seasonal H1N1 (Fig. 1 and 2). We therefore engineered 2009 pH1N1 viruses with additional glycosylation motifs that occurred naturally in human H1N1 viruses since their emergence in 1918. This also allowed us to investigate the potential significance of such mutations in the context of protective antibody responses elicited by the 2009 pH1N1 vaccine in humans.
The recombinant Neth/09 viruses containing additional glycosylation sites in the HA were attenuated in mice and ferrets (Fig. 4). This could be partly due to the reduced amount of the mutant HAs incorporated into virions as compared to WT (Supp. Fig. 1). Nonetheless, the infection and replication capacity of the glycosylated viruses in MDCK and primary HTBE cells were not significantly affected (Fig. 3), including when assessing their susceptibility against antiviral drug oseltamivir (Supp. Fig. 2). These results are consistent with studies demonstrating that glycosylated viruses are more sensitive to the innate immune activity of collectins present in lung fluid, but replicate equally well in mouse airway macrophages or MDCK cells in vitro (13, 14, 21–23). However, this sensitivity to collectins appears to be dependent on the number and position of the glycosylations added onto the HA (22). Indeed, our results in mice infected with single glycosylations showed attenuation for some of the mutants (e.g. 142 and 172), but not for others (e.g. 177), suggesting that the selection of glycosylations in human influenza viruses is modulated by both pre-existing immunity (antibodies) and the activity of collectins. Nonetheless, here we have not tested the neutralizing activity of collectins found in the lung fluid of humans. Therefore it is currently unclear whether influenza virus pathogenesis in humans is also regulated in similar manner and to the same extent by collectins and thus this warrants further investigation. Moreover, glycosylations can also result in decreased binding to the viral receptor (lower avidity), becoming attenuated due to compromised viral fitness (15). When we infected naïve ferrets with the WT and the 144-172 viruses, we observed differences in viral load in the lungs and trachea of the 144-172 infected animals, but not in the nasal turbinates. Infection in these animal model with glycosylated pH1N1 viruses is largely reminiscent of infection with H1N1 seasonal viruses, which generally do not produce disease in mouse models (24, 25) and in ferrets replicate to high titers in the upper respiratory tract but not in the lower respiratory tract (26, 27). Of interest, not only was virulence decreased by adding the naturally occurring glycosylation sites in the pH1N1 viruses, but also virulence was increased by deleting these glycosylations in the HA of the Tx/91 seasonal H1N1 virus. Therefore acquisition of glycosylations in the HA seems to reduce the virulence of the human H1N1 viruses due to multiple mechanisms (15, 22, 23). Interestingly, the lack of these oligosaccharides in the globular head of the HA is a feature shared with the old seasonal H1N1, the classical swine influenza viruses and the current 2009 pH1N1 strains, which display increased virulence in mice (4, 5, 25). One caveat of this study is that we have not tested the effect of these glycosylation in the background of other human influenza H1N1 viruses, which might have additional compensatory mutations as they circulate in humans. In fact, we were unable to rescue a virus containing HA glycosylation sites 144, 172 and 177 in the Neth/09 background, indicating that specific HA structures might or not allow the deletion or introduction of certain glycosylations or combinations of them. Additional studies utilizing HA from diverse H1N1 strains would aid our understanding of the role glycosylations in the evolution of influenza virus in humans.
Antigenic characterization of the Neth/09 glycosylation mutant viruses suggested that site Sa in the HA is a dominant antigenic region for mice and humans, since adding 1 or 2 glycosylation on residues around this site (e.g. sites 144 and 144-172) was sufficient to significantly reduce the HI activity of the polyclonal response elicited by the WT unglycosylated virus. Of these two sites, 144 seems to be the one responsible for this effect, as a dramatic reduction in HI was not seen in the 71-142-172-177 virus or viruses carrying single glycosylations at 142, 172, or 177. We speculate that glycosylation at 144 covers a different area than glycosylations at positions 142, 172 and 177 (Fig. 2B and C), or it might be placed in a different orientation, thus making it unique in its ability to modulate the antigenic effects of HA. In agreement, immunization of human adults with the current inactivated 2009 pH1N1 vaccine strain induced an overall polyclonal antibody response reminiscent of the one in pH1N1 infected mice (Table 1, Fig. 5 and Supp. Table 1), as glycosylation at site 144 was the most efficient in escaping HI reactivity. Similarly, the pediatric post-vaccination sera analyzed showed considerable activity against the 71-142-177 and the 71-142-172-177 viruses, but less against the 144 and144-172 viruses (Fig. 5 and Supp. Table 1). Overall this indicates that glycosylation of human H1N1 viruses greatly affects their antigenic properties. Of note however, in our study we only analyzed glycosylations that have previously appeared in human H1N1 viruses. Nonetheless, it is possible that as a consequence of immune mediated antigenic pressure, new changes in HA will occur and drive the appearance of new glycosylation sites in the 2009 pH1N1 strain modulating its antigenic properties as it continues to circulate seasonally worldwide. If this is the case, the impact of such glycosylations in virulence and antigenicity will have to be further investigated.
Importantly, infection with viruses harboring glycosylation sites 144 and 144-172 induced a broader polyclonal response capable of cross-reacting with all the WT and Neth/09 glycosylated viruses generated (Tables 1 and 2). The increased breadth of the polyclonal response is likely due to shielding of the immunodominant site Sa, causing a change of the antigenic focus that redirects the humoral response to other epitopes. This is in agreement with a recent study demonstrating that over time changes in the globular head of HA are focused on antigenic regions that are unmasked by changes in glycosylations (9). It should be noted that here we have analyzed sera from mice infected with the 144 and 144-172 viruses and thus, whether these viruses in humans could also induce a similar broad polyclonal response can only be speculated. Remarkably, the cross-protection against the WT Neth/09 virus observed in the mice infected with a sub-lethal dose of the Tx/91 deletion mutants Δ71-177 and Δ71-142-177 emphasizes the importance of glycosylations in “distracting” or redirecting the humoral response. These results also point to the crucial evolutionary role of the appearance of glycosylations around site Sa, since deleting glycosylations within or close to this region has a profound effect on cross-reactivity. Altogether, these findings highlight the immune-modulatory effects of specific glycosylations in the antigenic properties of HA, and also provide a powerful rationale to investigate the effects of glycosylations on the breadth of immune responses to infection and vaccination.
Materials and Methods
Human specimens
The studies involving the use of human serum specimens (Clinical Trial DMID 09-0047) were reviewed and approved by the Institutional Review Boards of both the Saint Louis University School of Medicine and of Icahn School of Medicine at Mount Sinai School. We utilized pre- and post-vaccination sera obtained from subjects who were 18 years of age or older (adults) and from individuals ages 1 to 17 (pediatric), that were enrolled in clinical trials to assess the safety and immunogenicity of an inactivated 2009 pH1N1 influenza vaccine based on strain A/California/07/2009 performed at the National Institute of Allergy and Infectious Disease Vaccine and Treatment Evaluation Unit at Saint Louis University. The sample size of our study was 52 pairs of pre- and post-vaccination sera. Samples were selected randomly upon availability of pre- and post sera, to cover age ranges for pediatric (1 to 17 years of age, n=14) and adult (18 to 74 years of age, n=36), and vaccination status (i.e. individuals that had received at least 1 dose of the 2009 pH1N1 influenza vaccine). As controls we also used pre- and post-vaccination sera from 2 adults that were immunized with the seasonal 2009 TIV, but that did not received the 2009 pH1N1 (Table S1). These samples were obtained under approved protocols where informed consent was obtained after the nature and possible consequences of the studies were explained. Samples used were deidentified of any patient information. The experiments conducted to assess the reactivity of these human sera against seasonal H3N2, H1N1, 2009 H1N1 and the glycosylation mutant HAs were performed blinded in duplicate.
H1N1 HA virus sequences and alignment
The HA sequence from all the H1N1 human viruses available through the Influenza Research Database and the Influenza Virus Resource Database were downloaded and aligned utilizing ClustalW and edited manually with the BioEdit Sequence Alignment Editor software. HA1 sequences containing representative glycosylation patterns based on at least two original isolates per year were selected for further analysis. Years not represented correspond to either a lack of an isolate sequence for that year or an unclear prototype sequence due to few sequences available. The GenBank accession numbers of the HAs depicted in Fig. 1 are: AF117241.1, CY034132, AF389118, CY009324, CY020445, CY013271, CY009276, CY020285, CY021709, CY009596, CY009612, CY019947, CY019971, CY009332, CY021821, AB043482, CY077748, CY077725, CY009340, CY021053, L19023, DQ508897, CY011296, CY021909, CY020181, CY021029, CY010364, Z54286, CY036823, L20111, CY020437, CY021725, DQ508873, CY019779, CY033655, CY012872, CY017011, DQ415317, EU103824, CY025026, CY010332, CY006675, CY019883, U53162, CY007467, CY016675, CY027875, AF386775, CY058487.1, CY040114, FJ984355, GQ150342, GQ149654, GQ117044, FJ966974, CY039527.2. The glycosylation sites were predicted by the motif N-X-S/T.
Cell lines and Viruses
Human embryonic kidney (293T) cells were maintained in DMEM supplemented with 10% FBS and 1000 U/ml penicillin/streptomycin. Madin–Darby canine kidney (MDCK) cells were maintained in MEM supplemented with 10% FBS and penicillin/streptomycin. Reagents for cell culture were purchased from Gibco Life Technologies. The virus strains A/Texas/36/1991 H1N1 (Tx/91), A/Brisbane/59/2007 H1N1 (Bris/59) and A/Brisbane/10/2007 H3N2 (Bris/10) were grown in 10-day-old embryonated eggs. The A/California/04/2009 (Cal/09) and A/Netherlands/602/2009 (Neth/09) isolates and all recombinant virus stocks were grown in MDCK cells.
Generation of recombinant viruses
a. A/Netherlands/602/2009 isolate rescue plasmids
Sequence analysis showed that segments encoding the PB2, PB1, M and NS proteins were identical between the A/California/04/2009 and A/Netherlands/602/2009 isolates. We thus used the plasmids pDZ-PB2, -PB1, -M and -NS of strain A/California/04/2009 described previously (28, 29). We cloned the remaining segments by isolating viral RNA from supernatants obtained from MDCK cells infected with the A/Netherlands/602/2009 virus isolate using the QIAamp viral RNA mini kit (Qiagen) and used segment-specific primers containing the SapI restriction sites to clone NP, HA and NA into the pPolI plasmid as previously described (29). For PA, we performed site-directed mutagenesis using the A/California/04/2009 pPolI-PA plasmid as template and mutated 3 nt to obtain the WT Neth/09 PA gene. Next, segments PA and NP were sub-cloned from vector pPolI into the bidirectional vector pDZ using SapI restriction sites. Constructs encoding the glycosylation mutants were generated by site-directed mutagenesis of the WT Neth/09 pPol-HA using the Quick Change Site-Directed Mutagenesis Kit (Stratagene). The amino acid changes made in each case to add glycosylation sites were as follows: K71N and N73S for site 71, D144T for site 142, D144N and N146T for site 144, G172N for site 172, and K177N for site 177.
b. Rescue of WT A/Netherlands/602/2009 and respective glycosylation mutant viruses
The Neth/09 based recombinant influenza A viruses were generated by transfecting 293T cells with 0.5 μg of each of ten plasmids utilizing Lipofectamine 2000 (Invitrogen) according to the manufacturer’s instructions. The plasmid mixture contained the six pDZ vectors encoding the PB2, PB1, PA, NP, M and NS genes and two pPolI vectors encoding the HA and NA genes. We included the A/WSN/33 expression plasmids pCAGGS-HA and pCAGGS-NA to enhance rescue efficiency. At 16–20 hr post-transfection, MDCK cells were added onto the 293T cells and medium was changed to DMEM with penicillin/streptomycin, 0.3% bovine albumin and 1ug/ml TPCK-treated trypsin (Sigma-Aldrich, St. Louis, MO). Supernatants were harvested 24–36 hr post addition of the MDCK cells. The rescued viruses were plaque purified and re-grown in MDCK cells for 48 hrs to make passage 1 stocks, which were used for all experiments shown. Titers of virus stocks were determined in triplicate by plaque assay on MDCK cells. The sequence of each recombinant virus was confirmed by sequencing the entire genome.
c. Generation and rescue of A/PR8/34 7:1 Tx/91 HA glycosylation deletion viruses
We performed fusion PCR to generate pDZ-HA plasmids containing glycosylation mutants of the Tx/91 HA to delete 1, 2 or 3 glycosylation sites located in the globular head of this contemporary seasonal H1N1 HA. The following amino acid changes were made to delete each glycosylation site to match the residues found in the Neth/09 isolate: N71K and S73N to delete site 71, T144D to delete site 142, and N177K to delete site 177. A second set of glycosylation deletion mutants was generated to contain the non-related amino acids N71Q to delete site 71, N142Q to delete site 142 and N177Q to delete site 177. We utilized the remaining 7 genes of A/PR8/34 (PR/34) cloned into the pDZ plasmid to rescue PR/34 7:1 TX/91 HA wild type and mutant recombinant viruses as described above.
Plaque phenotype and in vitro virus growth analysis
The plaque size phenotype was evaluated by performing a plaque assay after infecting MDCK cells with ~100 pfu of each recombinant virus as shown. At 48 hr p.i. the cells were fixed with 4% formaldehyde and plaques were visualized by immunostaining with the mouse monoclonal antibody E10 that recognizes the amino-terminal peptide common to the M1 and M2 proteins. Growth curves were performed in differentiated primary human tracheobronchial epithelial (HTBE) cells (Lonza). Approximately 1×105 HTBE cells were seeded onto collagen-coated 12-mm permeable membrane transwell inserts (0.4 μm) in a 12 well plate (Corning). The cells were grown submerged in BEGM Bronchial Epithelial Cell Growth Medium (Lonza) for 4 days until confluence was achieved and then differentiation was established by removing the media from the apical surface and further culturing the cells for 4 weeks in this air-liquid interface. During this time the media on the basolateral side was replaced every 2 days. Prior to virus infection the cell monolayers were washed thoroughly with PBS to remove the mucus accumulating on the apical surface of the cells. Triplicate wells were inoculated with each virus shown at a multiplicity of infection (MOI) of 0.001 pfu/cell. Virus was collected at the indicated time points by adding 100 μl of PBS to each well for 30 mins at 37C. Viral titers were determined by standard plaque assay using MDCK cells.
Western blot assays
MDCK cells infected at an MOI of 5 for 12 h with the indicated viruses were lysed in NP-40 lysis buffer (50 nM Tris, 150 nM NaCl, 5 mM EDTA, 30 mM NaF, 40 mM β-glycerophosphate, 10 % glycerol and 0.25% NP-40) containing Complete Mini protease inhibitor (Roche). Clarified lysates were boiled for 5 min and proteins were separated on a NuPAGE 4–12% Bis-Tris gradient gel (Invitrogen) under non-reducing conditions for the WT and mutant Neth/09 viruses, or under reducing conditions for the Tx/91 WT and the respective glycosylation deletion mutant viruses. Western blots were performed to detect proteins transferred to PVDF membranes, by incubation with the rabbit polyclonal antiserum 3951 raised against a PR8 virus lacking H1, which had been removed by acid and DTT treatment (30).
Mouse experiments
For mouse experiments groups of five mice were used to determine weight loss and survival. Unless stated otherwise groups of three mice were used to determine lung virus titers.
a. Infections, body weight loss and survival
All mouse experiments were carried out in strict accordance with institutional Animal Care and Use Committee (IACUC) guidelines, and have been approved by the IACUC of Icahn School of Medicine at Mount Sinai. 7 to 9-week-old C57BL/6 female mice (Jackson Laboratories) were anesthetized by intraperitoneal injection of ketamine-xylaxine before intranasal infection with the indicated virus at doses of the virus diluted in 50 μl of PBS. Body weight and survival were monitored daily for 14 days. Mice showing more than 25% of body weight loss were considered to have reached the experimental end point and were humanely euthanized.
b. Lung viral titers and sequencing
Lungs of infected mice were excised aseptically on the indicated days post-infection and stored at −80°C until further processing. For virus titrations the tissues were homogenized in 1ml of PBS using a mechanical homogenizer (MP Biochemicals). The viral titers in the clarified supernatant homogenates were quantified by standard plaque assay on MDCK cells. To determine the presence of compensatory mutations during infection, viral RNA was also extracted from the homogenate using the QIAamp Viral RNA Mini Kit (Qiagen) following the manufacturer’s instructions. The HA and NA genes corresponding to each mouse at the different time points were amplified and sequenced by standard methods.
c. Neth/09 challenge
8-week old mice were infected with the indicated rTx/91 viruses. Mice were allowed to seroconvert for 27 days at which time they were challenged with 100 times the 50% lethal dose (LD50%) of A/Netherlands/602/2009. Survival and body weight loss were monitored for 13 days p.i.
Ferret experiments
Animal research was conducted under the guidance of the Centers for Disease Control and Prevention’s IACUC in an Association for Assessment and Accreditation of Laboratory Animal Care International-accredited animal facility.
a. Infections, body weight loss and nasal wash titers
We used 8 to 12 months old male Fitch ferrets, (Triple F Farms) that were serologically negative by hemagglutination inhibition for currently circulating seasonal H3N2, the previously circulating seasonal H1N1 and the pandemic 2009 H1N1 influenza A viruses, to assess the virulence of the indicated viruses. Three ferrets per group were anesthetized with an intramuscular injection of a ketamine hydrochloride (24 mg/kg)-xylazine (2 mg/kg)-atropine (0.05 mg/kg) cocktail and were infected intranasally with either the WT Neth/09 HA or the HA 144-172 glycosylation mutant virus at 106 pfu in a final volume of 1 ml of PBS. Body weights were measured daily for 12 days and are represented as the percentage weight compared to the initial weight. The nasal cavities of the ferrets were washed with 1 ml of PBS on days 1, 3, 5 and 7 p.i.. The viral titers of the nasal washes were determined by standard plaque assay on MDCK cells.
b. Tissue viral titers
Three ferrets per indicated group were infected with 106 pfu of each virus as described above. On day 3 p.i. the ferrets were euthanized and the lungs, trachea and nasal turbinates were aseptically collected. The tissue specimens were immediately frozen on dry ice and stored at −70°C until processed. Frozen tissue specimens were thawed, weighed, and then homogenized in cold PBS using disposable sterile tissue grinders (Kendall). Tissue homogenates were clarified and virus titers in the clear supernatants were determined by standard plaque assay on MDCK cells.
Hemagglutination inhibition (HI) assay of mouse and human sera
Mouse sera were obtained from animals infected with the indicated viruses on day 28 p.i. HI assays were performed with sera pooled from 3 infected animals per virus that were selected to contain at least 160 HI units against the homologous virus, except for the virus containing glycosylation on site 177 that only elicited HI titers of 80. The HI assays were conducted essentially as previously described (3, 31). Briefly, we used trypsin-heat-periodate treatment to inactivate the mouse, ferret and human sera by mixing a half volume of trypsin 8 mg/ml (Sigma-Aldrich) in 0.1 M phosphate buffer, pH 8.2, with one volume of serum and the samples were incubated for 30 min at 56°C. The samples were cooled to RT, mixed with three volumes of 0.11 M metapotassium periodate and further incubated at RT for 15 min. The samples were then mixed with three volumes of 1 % glycerol saline and incubated for 15 min at RT. The samples were finally mixed and incubated with 2.5 volumes of 85 % saline to dilute the samples to a concentration of 1:10. We performed HI assays of sera following standard protocols (32). Briefly, two-fold serial dilutions of mouse or human sera were mixed and pre-incubated in 96-well plates with 8 HA units of virus per well for 30 min at 4°C. Turkey (for Bris/10 and Neth/09) or chicken (for Bris/59) red blood cells were added at a final concentration of 0.25 %, and the plates were incubated at 4°C for 30 min. HI titers were determined as the reciprocal of the highest dilution that displayed haemagglutinating activity.
Statistical analysis
For mouse studies we assessed statistical significant differences (P < 0.05) in body weight loss in groups of five mice (n=5) using a two-tailed unpaired Student’ s t –test, and for establishing statistical differences for survival curves we utilized the log-rank test. For the ferret experiments statistical significance (P < 0.05) of the weight loss over time was performed by analysis of the area under the curve (AUC), interpreted as the total weight loss of the animal group (n=3) as a function of time, using the Wilcoxon-matched pairs test. For the human sera (n=52) statistical significance was tested using the Wilcoxon rank sum test on the distributions.
Supplementary Material
Fig. S1 HA/NP ratio in virions of glycosylation mutant viruses.
Fig. S2 Sensitivity of the glycosylation mutant viruses to the Oseltamivir antiviral.
Fig. S3 Neutralization activity of sera from mice infected with rWT and 144 glycosylation mutant viruses.
Fig. S4 Pathogenesis of Neth/09 viruses containing single and double glycosylations.
Fig. S5 Pathogenesis of Tx91 viruses containing glycosylation deletions by alternative mutations.
Table S1 HAI titers of adult and pediatric human sera after vaccination with 2009 pH1N1 inactivated vaccine.
Acknowledgments
We thank Alejandra Galvez Fuenzalida, Richard Cadagan, Osman Lizardo and Karla Tapia for excellent and invaluable technical assistance during the course of this study. We are also thankful to William Pressley, Gorky Estrella, Paul Gonzalez and the CCMS staff at MSSM for facilitating animal studies.
Funding: These studies were partially supported by a NIAID Program Project grant (P01AI058113) and by CRIP, an NIAID funded Center for Research in Influenza Pathogenesis contract (HHSN266200700010C, CEIRS program) to A.G.S, and a contract (HHSN272200800003C) to R.B.B., all from the National Institutes of Health. R.A.M. is supported by CONICYT through an Insertion of Human Capital to the Academy grant (79100014), and a Fondecyt grant (1121172) and by the Program Iniciativa Científica Milenio from the Chilean Ministry of Economy, Development and Tourism; and B.M. is supported by NIAID K99/R00 Pathway to Independence award (1K99AI095320-01).
Footnotes
Authors contribution: R.A.M., S.S. and B.M. conceived and designed the study, conducted all the experiments, analyzed the results and co-wrote the paper. T.M.T. and X.S. conducted ferret experiments, analyzed the data and co-wrote the paper. P.Z., H.U.-K., R.A. conducted experiments and co-wrote the paper. O.Z. helped with statistical analysis. D.E. prepared protein model structures. R.B.B. and S.E.F. provided human sera and co-wrote the paper. A.G.S. supervised the overall study, analyzed the data and co-wrote the paper.
Competing Interest: The authors declare no competing interests. The findings and conclusions in this report are those of the authors and do not necessarily reflect the views of the funding agency.
REFERENCES AND NOTES
- 1.Molinari NA, Ortega-Sanchez IR, Messonnier ML, Thompson WW, Wortley PM, Weintraub E, Bridges CB. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25:5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 2.Medina RA, Garcia-Sastre A. Influenza A viruses: new research developments. Nature reviews. 2011;9:590–603. doi: 10.1038/nrmicro2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manicassamy B, Medina RA, Hai R, Tsibane T, Stertz S, Nistal-Villan E, Palese P, Basler CF, Garcia-Sastre A. Protection of Mice against Lethal Challenge with 2009 H1N1 Influenza A Virus by 1918-Like and Classical Swine H1N1 Based Vaccines. PLoS Pathog. 2010;6:e1000745. doi: 10.1371/journal.ppat.1000745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kash JC, Qi L, Dugan VG, Jagger BW, Hrabal RJ, Memoli MJ, Morens DM, Taubenberger JK. Prior infection with classical swine H1N1 influenza viruses is associated with protective immunity to the 2009 pandemic H1N1 virus. Influenza Other Respi Viruses. 2010;4:121–127. doi: 10.1111/j.1750-2659.2010.00132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skountzou I, Koutsonanos DG, Kim JH, Powers R, Satyabhama L, Masseoud F, Weldon WC, Martin MD, Mittler RS, Compans R, Jacob J. Immunity to Pre-1950 H1N1 Influenza Viruses Confers Cross-Protection against the Pandemic Swine-Origin 2009 A (H1N1) Influenza Virus. J Immunol. 2010 doi: 10.4049/jimmunol.1000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei CJ, Boyington JC, Dai K, Houser KV, Pearce MB, Kong WP, Yang ZY, Tumpey TM, Nabel GJ. Cross-neutralization of 1918 and 2009 influenza viruses: role of glycans in viral evolution and vaccine design. Sci Transl Med. 2010;2:24ra21. doi: 10.1126/scitranslmed.3000799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krause JC, Tumpey TM, Huffman CJ, McGraw PA, Pearce MB, Tsibane T, Hai R, Basler CF, Crowe JE., Jr Naturally Occurring Human Monoclonal Antibodies Neutralize both 1918 and 2009 Pandemic Influenza A (H1N1) Viruses. J Virol. 2010;84:3127–3130. doi: 10.1128/JVI.02184-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu R, Ekiert DC, Krause JC, Hai R, Crowe JE, Jr, Wilson IA. Structural basis of preexisting immunity to the 2009 H1N1 pandemic influenza virus. Science. 2010;328:357–360. doi: 10.1126/science.1186430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Das SR, Puigbo P, Hensley SE, Hurt DE, Bennink JR, Yewdell JW. Glycosylation focuses sequence variation in the influenza A virus H1 hemagglutinin globular domain. PLoS Pathog. 2010;6:e1001211. doi: 10.1371/journal.ppat.1001211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun S, Wang Q, Zhao F, Chen W, Li Z. Glycosylation site alteration in the evolution of influenza A (H1N1) viruses. PloS one. 2011;6:e22844. doi: 10.1371/journal.pone.0022844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Igarashi M, Ito K, Kida H, Takada A. Genetically destined potentials for N-linked glycosylation of influenza virus hemagglutinin. Virology. 2008;376:323–329. doi: 10.1016/j.virol.2008.03.036. [DOI] [PubMed] [Google Scholar]
- 12.Wang CC, Chen JR, Tseng YC, Hsu CH, Hung YF, Chen SW, Chen CM, Khoo KH, Cheng TJ, Cheng YS, Jan JT, Wu CY, Ma C, Wong CH. Glycans on influenza hemagglutinin affect receptor binding and immune response. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:18137–18142. doi: 10.1073/pnas.0909696106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tate MD, Brooks AG, Reading PC. Specific sites of N-linked glycosylation on the hemagglutinin of H1N1 subtype influenza A virus determine sensitivity to inhibitors of the innate immune system and virulence in mice. J Immunol. 2011;187:1884–1894. doi: 10.4049/jimmunol.1100295. [DOI] [PubMed] [Google Scholar]
- 14.Tate MD, Job ER, Brooks AG, Reading PC. Glycosylation of the hemagglutinin modulates the sensitivity of H3N2 influenza viruses to innate proteins in airway secretions and virulence in mice. Virology. 2011;413:84–92. doi: 10.1016/j.virol.2011.01.036. [DOI] [PubMed] [Google Scholar]
- 15.Das SR, Hensley SE, David A, Schmidt L, Gibbs JS, Puigbo P, Ince WL, Bennink JR, Yewdell JW. Fitness costs limit influenza A virus hemagglutinin glycosylation as an immune evasion strategy. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:E1417–1422. doi: 10.1073/pnas.1108754108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reichert T, Chowell G, Nishiura H, Christensen RA, McCullers JA. Does Glycosylation as a modifier of Original Antigenic Sin explain the case age distribution and unusual toxicity in pandemic novel H1N1 influenza? BMC infectious diseases. 2010;10:5. doi: 10.1186/1471-2334-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Igarashi M, Ito K, Yoshida R, Tomabechi D, Kida H, Takada A. Predicting the antigenic structure of the pandemic (H1N1) 2009 influenza virus hemagglutinin. PloS one. 2010;5:e8553. doi: 10.1371/journal.pone.0008553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith GJ, Vijaykrishna D, Bahl J, Lycett SJ, Worobey M, Pybus OG, Ma SK, Cheung CL, Raghwani J, Bhatt S, Peiris JS, Guan Y, Rambaut A. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459:1122–1125. doi: 10.1038/nature08182. [DOI] [PubMed] [Google Scholar]
- 19.Dawood FS, Jain S, Finelli L, Shaw MW, Lindstrom S, Garten RJ, Gubareva LV, Xu X, Bridges CB, Uyeki TM. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605–2615. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 20.Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, Sessions WM, Xu X, Skepner E, Deyde V, Okomo-Adhiambo M, Gubareva L, Barnes J, Smith CB, Emery SL, Hillman MJ, Rivailler P, Smagala J, de Graaf M, Burke DF, Fouchier RA, Pappas C, Alpuche-Aranda CM, Lopez-Gatell H, Olivera H, Lopez I, Myers CA, Faix D, Blair PJ, Yu C, Keene KM, Dotson PD, Jr, Boxrud D, Sambol AR, Abid SH, St George K, Bannerman T, Moore AL, Stringer DJ, Blevins P, Demmler-Harrison GJ, Ginsberg M, Kriner P, Waterman S, Smole S, Guevara HF, Belongia EA, Clark PA, Beatrice ST, Donis R, Katz J, Finelli L, Bridges CB, Shaw M, Jernigan DB, Uyeki TM, Smith DJ, Klimov AI, Cox NJ. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vigerust DJ, Ulett KB, Boyd KL, Madsen J, Hawgood S, McCullers JA. N-linked glycosylation attenuates H3N2 influenza viruses. Journal of virology. 2007;81:8593–8600. doi: 10.1128/JVI.00769-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hillaire ML, van Eijk M, Nieuwkoop NJ, Vogelzang-van Trierum SE, Fouchier RA, Osterhaus AD, Haagsman HP, Rimmelzwaan GF. The number and position of N-linked glycosylation sites in the hemagglutinin determine differential recognition of seasonal and 2009 pandemic H1N1 influenza virus by porcine surfactant protein D. Virus research. 2012;169:301–305. doi: 10.1016/j.virusres.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 23.Job ER, Deng YM, Barfod KK, Tate MD, Caldwell N, Reddiex S, Maurer-Stroh S, Brooks AG, Reading PC. Addition of Glycosylation to Influenza A Virus Hemagglutinin Modulates Antibody-Mediated Recognition of H1N1 2009 Pandemic Viruses. J Immunol. 2013 doi: 10.4049/jimmunol.1202433. [DOI] [PubMed] [Google Scholar]
- 24.Bouvier NM, Lowen AC. Animal Models for Influenza Virus Pathogenesis and Transmission. Viruses. 2010;2:1530–1563. doi: 10.3390/v20801530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pica N, Iyer A, Ramos I, Bouvier NM, Fernandez-Sesma A, Garcia-Sastre A, Lowen AC, Palese P, Steel J. The DBA.2 mouse is susceptible to disease following infection with a broad, but limited, range of influenza A and B viruses. Journal of virology. 2011 doi: 10.1128/JVI.05930-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maines TR, Jayaraman A, Belser JA, Wadford DA, Pappas C, Zeng H, Gustin KM, Pearce MB, Viswanathan K, Shriver ZH, Raman R, Cox NJ, Sasisekharan R, Katz JM, Tumpey TM. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science. 2009;325:484–487. doi: 10.1126/science.1177238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Munster VJ, de Wit E, van den Brand JM, Herfst S, Schrauwen EJ, Bestebroer TM, van de Vijver D, Boucher CA, Koopmans M, Rimmelzwaan GF, Kuiken T, Osterhaus AD, Fouchier RA. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science. 2009;325:481–483. doi: 10.1126/science.1177127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hai R, Schmolke M, Varga ZT, Manicassamy B, Wang TT, Belser JA, Pearce MB, Garcia-Sastre A, Tumpey TM, Palese P. PB1-F2 expression by the 2009 pandemic H1N1 influenza virus has minimal impact on virulence in animal models. Journal of virology. 2010;84:4442–4450. doi: 10.1128/JVI.02717-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quinlivan M, Zamarin D, Garcia-Sastre A, Cullinane A, Chambers T, Palese P. Attenuation of equine influenza viruses through truncations of the NS1 protein. Journal of virology. 2005;79:8431–8439. doi: 10.1128/JVI.79.13.8431-8439.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steel J, Lowen AC, Wang T, Yondola M, Gao Q, Haye K, Garcia-Sastre A, Palese P. Influenza virus vaccine based on the conserved hemagglutinin stalk domain. mBio. 2010;1 doi: 10.1128/mBio.00018-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Medina RA, Manicassamy B, Stertz S, Seibert CW, Hai R, Belshe RB, Frey SE, Basler CF, Palese P, Garcia-Sastre A. Pandemic 2009 H1N1 vaccine protects against 1918 Spanish influenza virus. Nat Commun. 2010;1 doi: 10.1038/ncomms1026. 10.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yu X, Tsibane T, McGraw PA, House FS, Keefer CJ, Hicar MD, Tumpey TM, Pappas C, Perrone LA, Martinez O, Stevens J, Wilson IA, Aguilar PV, Altschuler EL, Basler CF, Crowe JE., Jr Neutralizing antibodies derived from the B cells of 1918 influenza pandemic survivors. Nature. 2008;455:532–536. doi: 10.1038/nature07231. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. S1 HA/NP ratio in virions of glycosylation mutant viruses.
Fig. S2 Sensitivity of the glycosylation mutant viruses to the Oseltamivir antiviral.
Fig. S3 Neutralization activity of sera from mice infected with rWT and 144 glycosylation mutant viruses.
Fig. S4 Pathogenesis of Neth/09 viruses containing single and double glycosylations.
Fig. S5 Pathogenesis of Tx91 viruses containing glycosylation deletions by alternative mutations.
Table S1 HAI titers of adult and pediatric human sera after vaccination with 2009 pH1N1 inactivated vaccine.