Abstract
Background
Although a single dose of etomidate can cause relative adrenal insufficiency the impact of etomidate exposure on postoperative outcomes is not known. The objective of this study was to examine the association between a single induction dose of etomidate and clinically important postoperative outcomes following cardiac surgery.
Methods
We retrospectively examined the association between etomidate exposure during anesthetic induction and postoperative outcomes in patients undergoing cardiac surgery from January 2007 to December 2009 using multivariate logistic regression analyses and Cox proportional hazards regression analyses. Postoperative outcomes of interest were severe hypotension, mechanical ventilation hours, hospital length of stay and in-hospital mortality.
Results
Sixty-two percent of 3,127 patients received etomidate. Etomidate recipients had a higher incidence of preoperative congestive heart failure (23.0% vs. 18.3%, p = 0.002) and a lower incidence of preoperative cardiogenic shock (1.3% vs. 4.0%, p < 0.001). The adjusted odds ratio for severe hypotension and in-hospital mortality associated with receiving etomidate was 0.80 (95% CI: 0.58 to 1.09) and 0.75 (95% CI: 0.45 to 1.24) respectively, and the adjusted hazard ratio for time to mechanical ventilation removal and time to hospital discharge were 1.10 (95% CI: 1.00 to 1.21) and 1.07 (95% CI: 0.97 to 1.18) respectively. Propensity score analysis did not change the association between etomidate use and postoperative outcomes.
Conclusions
In this study, there was no evidence to suggest that etomidate exposure was associated with severe hypotension, longer mechanical ventilation hours, longer length of hospital stay or in-hospital mortality. Etomidate should remain an option for anesthetic induction in cardiac surgery patients.
Introduction
Etomidate, an imidazole derivative, is an important drug used for anesthetic induction in high-risk cardiac surgery patients because of its hemodynamic stability.1 Many clinicians have abandoned this potent and hemodynamically forgiving drug due to concern for relative adrenal insufficiency contributing to poor outcomes. There is little controversy that a single dose of etomidate can inhibit adrenal steroidogenesis and cause relative adrenal insufficiency.2–5 There is, however, controversy regarding the impact of etomidate-induced relative adrenal insufficiency on clinical outcomes. In sepsis and critically ill patients, various studies suggest either an increase 2,4,6 or no change 3,7–11 in mortality risk associated with etomidate use. In addition, a large randomized prospective study evaluating the effect of etomidate or ketamine as induction agent in the emergency department found etomidate use was not associated with a significant increase in morbidity or mortality compared to ketamine.12
The impact of a single dose administration of etomidate on clinical outcomes, other than vasopressor requirements, is not known in cardiac surgery patients. A small prospective cohort study in cardiac surgery patients concluded that the use of etomidate might increase vasopressor requirements but with no increase in mortality.13 A randomized controlled trial in elective cardiac surgery patients, however, demonstrated an increased rate of relative adrenal insufficiency in patients that received etomidate but no increase in vasopressor requirements.14 Thus, while a single dose of etomidate increases the risk of relative adrenal insufficiency, its impact on postoperative outcomes in cardiac surgery patients remains largely unknown. Despite the fact that the effect of etomidate administration on postoperative outcomes is controversial, there continues to be proponents that call for the use of alternative anesthetic induction agents 15,16 or are developing analogues of etomidate that do not produce adrenocortical dysfunction.17 This goal of this study is to examine whether there is evidence suggesting that etomidate administration is associated with any/all of increased severe hypotension, longer time on mechanical ventilation, longer length of hospital stay, and/or increased in-hospital mortality. We hypothesized that even in a sample as large as ours (N = 3,127), no such evidence would exist.
Material and Methods
After obtaining a waiver of informed consent from the Institutional Review Board (Human Research Protection Program, Vanderbilt University, Nashville, Tennessee), we performed a retrospective single institution review of all cardiac surgery patients between January 2007 and December 2009. Patient information was obtained from the Society of Thoracic Surgeons Database at Vanderbilt University Medical Center and included age, gender, body mass index (BMI), race, type of surgery, history of diabetes mellitus, history of congestive heart failure, preoperative angiotensin-converting enzyme (ACE) inhibitor use, ejection fraction, last preoperative creatinine level, presence of cardiogenic shock, status of surgery (elective, urgent and emergent), mechanical ventilation hours, hospital length of stay, and in-hospital mortality. The use of etomidate, propofol, midazolam, and fentanyl during induction of anesthesia was obtained from our Perioperative Data Warehouse that electronically captures the use of these drugs. As this is a retrospective review, anesthetic drug choices were up to the discretion of the anesthesiologist. Patients that were intubated on arrival may have not received intravenous anesthetic induction. Prior to 2008 etomidate was used more commonly for cases with concern for hemodynamic stability, while after 2008 the consensus of the group was to use it more sparingly because of the concerns from sepsis data about relative adrenal insufficiency. Anesthesia was maintained with a combination of oxygen, air and isoflurane. Isoflurane was administered in the pump circuit to all patients that underwent cardiopulmonary bypass. All patients received a propofol infusion at the end of the anesthetic case for transfer to the intensive care unit (ICU). Severe hypotension in the ICU was defined as a norepinephrine requirement of greater than or equal to 15 mcg/min for greater than 1 h to maintain a specified target mean arterial pressure of 60–70 mmHg. Our ICU clinical protocol during this study period mandated that a baseline cortisol level and corticotropin stimulation test be obtained on these hypotensive patients. This protocol did not take other vasopressor and inotropic drugs, cardiac output or systemic vascular resistance into account. We did not analyze the effect of etomidate on relative adrenal insufficiency in the hypotensive cohort because it is already well established that etomidate causes relative adrenal insufficiency.2–5 Mechanical ventilation hours were defined as time from arrival in the ICU to extubation. If a patient was taken off mechanical ventilation and then put back on it, we used the total number of hours on mechanical ventilation as opposed to the time until it was first removed. The length of hospital stay was defined as time from ICU admission until discharge from the hospital.
Statistical Methods
Characteristics of the study sample (e.g., demographics and baseline variables) are summarized with the median, 10th, and 90th percentiles for continuous variables and with percentages for categorical variables. To test for unadjusted differences between those who did and did not receive etomidate, the Wilcoxon Rank Sum test and the Pearson Chi-Square test were used for continuous and categorical variables, respectively. Logistic regression analyses and Cox proportional hazards regression analyses were used to examine covariate-adjusted associations between etomidate administration and outcomes. In particular, logistic regression was used to model the binary outcomes mortality and severe hypotension and Cox proportional hazards regression was used to model the number days from surgery until hospital discharge and the number of hours from start until removal of mechanical ventilation. Multivariate regression models were adjusted for an a priori determined sets of potential confounders including 1) other anesthetics and medications used (propofol, midazolam, ACE inhibitors); 2) patient demographics (age, gender, and race); 3) patient health and past medical history (body mass index, ejection fraction, presurgery creatinine concentration, history of diabetes, history of congestive heart failure, history of cardiogenic shock, emergency vs. elective surgery), and 4) type of surgery (off-pump coronary artery bypass graft (CABG) surgery, on-pump CABG surgery, valve surgery, valve and on-pump CABG surgery, and other surgery). Etomidate administration curtailed dramatically beginning in October 2008, and so calendar month (ranging from 1 to 36) was included as an adjustment variable in all regression models. For the continuous covariates, age, ejection fraction, BMI, presurgery creatinine, and calendar month, we examined whether associations with outcomes exhibited evidence of nonlinearity using restricted cubic splines with four knots. In at least one of the outcome models, BMI, creatinine, and calendar month associations with outcomes exhibited nonlinearity according to a likelihood ratio test and so we modeled each of these three variables flexibly (without assuming linearity) in all models. In contrast, age and ejection fraction did not exhibit obvious evidence for nonlinearity and so such effects were modeled assuming linearity in all models.
For the severe hypotension and mortality analyses, where logistic regression was used, etomidate and other covariate effects are summarized with odds ratios (OR) and 95% confidence intervals (CI). For the time to hospital discharge and time to removal of mechanical ventilation analyses, where Cox proportional hazards models were used, etomidate and other covariate effects are summarized with hazard ratios (HR) and 95% CI. It is worth noting that even though an OR greater than one is associated with increased risk of severe hypotension and mortality, a HR less than one is associated with lower rates of mechanical ventilation removal and hospital discharge, and therefore denotes longer time on mechanical ventilator and longer length of hospital stay. Ejection fraction was missing in 16.1% of patients and race was missing in 6.7% of patients. We therefore used multiple imputation analyses with 25 imputation datasets to summarize effects of covariates on outcomes.
Since there was concern regarding model over-fitting with covariate adjusted regression analyses (particularly for the mortality analyses where there were approximately 100 events) we conducted propensity score analyses in parallel. For the propensity score analyses, all covariates used in covariate-adjusted analyses were entered into a logistic regression model of etomidate exposure (yes/no), and for each subject we calculated the propensity score using estimated log-odds of etomidate exposure. Etomidate exposure (yes/no) and the propensity score (flexibly modeled using restricted cubic splines with four knots) were then entered into each outcome regression model and we report estimated etomidate associations with the four outcomes. The etomidate associations with outcomes were remarkably similar using both covariate-adjusted and propensity score approaches and both are reported. For covariate-adjusted analyses, bootstrap-based validation and calibration analyses were performed to assess model over-fitting.18,19 In all models except for the mortality model, regression calibration slopes exceeded 0.95 thus pointing towards little to no model overfitting. In the mortality model, the calibration slope was 0.82 thus pointing towards modest overfitting. Finally, in the covariate-adjusted Cox models, we tested the proportional hazards assumption for the etomidate effects. There was no evidence to suggest violation of the proportional hazards assumption in either the time to hospital discharge or the time to mechanical ventilation removal models.
For all regression analyses, two-sided, type 1 error rates of 0.05 were used for statistical significance. Because we examined four outcomes, for regression analysis reporting, we include Bonferroni-adjusted estimates of confidence intervals in addition to the unadjusted estimates. All statistical analyses were performed using the R programming language version 3.0.1 (Vienna, Austria).
Results
A total of 3,294 cardiac surgery patients were reviewed from January 2007 to December 2009. Etomidate usage information was available for 3,219 patients. We excluded patients that received ketamine (1%), patients that did not receive fentanyl (2%), patients with ejection fraction out of range (5 to 80), BMI greater than 80 or those with creatinine level equal to zero. Our analyses are therefore based on patients that received fentanyl and did not receive ketamine (N = 3,127). A total of 1,928 (61.7%) patients received etomidate. Tables 1 and 2 summarize covariate and outcome distributions, respectively, for etomidate recipients and nonrecipients. Many of the covariate distributions appeared similar between etomidate recipients and nonrecipients. Etomidate recipients, however, appeared to be more likely to present with a history of congestive heart failure (23% vs. 18.3%, p = 0.002) and were less likely to present with cardiogenic shock (1.3% vs. 4%, p < 0.001). The decreased use of etomidate in patients that presented with cardiogenic shock may be explained by the fact that many of these patients arrived in the operating room already intubated with no need for induction drugs. This is supported by the fact that in patients that presented with cardiogenic shock, 28% received only midazolam and 22% received no induction drug at all. Patients that underwent on-pump CABG surgery were more likely to receive etomidate whereas patients that underwent off-pump CABG surgery were less likely to receive etomidate. Similarly, in unadjusted analyses of outcomes, etomidate recipients and nonrecipients appeared to have similar distributions for all outcomes except mechanical ventilation hours. Etomidate recipients were observed to be exposed to mechanical ventilation for longer periods of time compared to non-recipients (median hours: 8.5 vs. 7.4 p = 0.005).
Table 1.
Summary Statistics for Demographics and Baseline Variables by Presence of Etomidate
| Characteristic | N | Etomidate (N = 1,928) | No Etomidate (N = 1,199) | P-value |
|---|---|---|---|---|
| Induction Agent | ||||
| Etomidate Only | 3,127 | 5.5% | 0.0% | <0.001 |
| Propofol Only | 3,127 | 0.0% | 3.9% | <0.001 |
| Midazolam Only | 3,127 | 0.0% | 38.9% | <0.001 |
| Etomidate and Propofol | 3,127 | 1.6% | 0.0% | <0.001 |
| Etomidate and Midazolam | 3,127 | 81.5% | 0.0% | <0.001 |
| Propofol and Midazolam | 3,127 | 0.0% | 54.0% | <0.001 |
| All three (E+P+M) | 3,127 | 11.4% | 0.0% | <0.001 |
| No agent | 3,127 | 0.0% | 3.2% | <0.001 |
| Propofol (Total) | 3,127 | 13.0% | 58.0% | <0.001 |
| Midazolam ( Total) | 3,127 | 92.9% | 92.9% | 0.97 |
| Age (years) | 3,127 | 63 (47 to 78) | 64 (45 to 79) | 0.45 |
| Male Gender | 3,127 | 66.1% | 64.6% | 0.38 |
| BMI (kg/m2) | 3,069 | 28.3 (22.2 to 37.4) | 28.1 (21.9 to 37.3) | 0.42 |
| Race | 0.44 | |||
| Caucasian | 2,917 | 91.3% | 89.9% | |
| Black | 2,917 | 7.5% | 8.5% | |
| Other | 2,917 | 1.3% | 1.6% | |
| History of Diabetes | 3,127 | 31.7% | 31.1% | 0.71 |
| Creatinine (mg/dL) | 3,103 | 1.07 (0.77 to 1.69) | 1.08 (0.79 to 1.72) | 0.38 |
| Ejection Fraction (%) | 2,623 | 55 (25 to 65) | 55 (25 to 65) | 0.05 |
| History of CHF | 3,127 | 23.0% | 18.3% | 0.002 |
| ACE inhibitor use | 3,127 | 35.0% | 33.5% | 0.40 |
| Cardiogenic Shock | 3,127 | 1.3% | 4.0% | <0.001 |
| Valve Surgery Only | 3,127 | 32.1% | 30.4% | 0.33 |
| Valve and CABG Surgery | 3,127 | 9.4% | 9.8% | 0.73 |
| CABG surgery on-pump | 3,127 | 15.8% | 7.8% | <0.001 |
| CABG surgery off-pump | 3,127 | 34.2% | 40.5% | <0.001 |
| Other surgery | 3,127 | 8.5% | 11.4% | 0.006 |
| Surgery Status | 0.49 | |||
| Elective | 3,122 | 66.7% | 65.5% | |
| Urgent and Emergent | 3,122 | 33.3% | 34.5% | |
Continuous variables were summarized with Median (10th, 90th percentile) and tested with Wilcoxon Rank Sum Test. Categorical variables were summarized with percentages and tested with Chi-Square test. ACE = angiotensin-converting enzyme; BMI = body mass index; CABG = coronary artery bypass graft; CHF = congestive heart failure.
Table 2.
Unadjusted Postoperative Outcomes
| Characteristic | N | Etomidate N = 1,928 | No Etomidate N = 1,199 | P-value |
|---|---|---|---|---|
| Severe hypotension | 3127 | 9.6% | 10.8% | 0.26 |
| Total time on mechanical ventilation (hours) | 2978 | 8.5 (3.3 to 51.6) | 7.4 (2.9 to 117.2) | 0.005 |
| Hospital length of stay (days) | 3120 | 6.0 (3.0 to 13.0) | 6.0 (3.0 to 18.0) | 0.96 |
| Mortality | 3127 | 3.0% | 4.2% | 0.07 |
Continuous variables were summarized with Median (10th, 90th percentile) and tested with Wilcoxon Rank Sum Test. Categorical variables were summarized with percentages and tested with Chi-Square test.
Table 3 shows results from the primary analyses that include adjustments for potential confounders. There was no evidence in this analysis to suggest that etomidate exposure increases patients’ risk of adverse outcomes. The adjusted odds ratio for severe hypotension and mortality associated with receiving etomidate was 0.80 (95% CI: 0.58 to1.09) and 0.75 (95% CI: 0.45 to 1.24), respectively, and the adjusted hazards ratio for time to mechanical ventilation removal and time to hospital discharge were 1.10 (95% CI: 1.00 to1.21), and 1.07 (95% CI: 0.97 to1.18) respectively. Propensity score analysis, with adjustment for confounders, did not change the effect of etomidate on severe hypotension, length of hospital stay or mortality. In addition, there was no evidence that etomidate exposure increases mechanical ventilation time by propensity score analysis. We also performed a sensitivity analysis in which patients that did not receive any induction drugs were excluded from the analysis. The results from the sensitivity analysis were qualitatively similar to those reported in table 3.
Table 3.
Adjusted Postoperative Outcomes
| Severe Hypotension OR (95% CI) | Total Mechanical Ventilation Time HR (95% CI) | Length of Hospital Stay HR (95% CI) | Mortality OR (95% CI) | ||
|---|---|---|---|---|---|
| Regression model approach | |||||
| Etomidate Effect | Original analysis | 0.80 (0.58 to 1.09) | 1.10 (1.00 to 1.21) | 1.07 (0.97 to 1.18) | 0.75 (0.45 to 1.24) |
| + Bonferroni | 0.80 (0.53 to 1.20) | 1.10 (0.97 to 1.25) | 1.07 (0.94 to 1.21) | 0.75 (0.39 to 1.45) | |
| Propensity Score approach | |||||
| Etomidate Effect | Original analysis | 0.79 (0.58 to 1.08) | 1.12 (1.02 to 1.23) | 1.07 (0.98 to 1.18) | 0.74 (0.44 to 1.23) |
| + Bonferroni | 0.79 (0.53 to 1.19) | 1.12 (0.99 to 1.27) | 1.07 (0.95 to 1.21) | 0.74 (0.38 to 1.44) | |
| Regression model approach include severe hypotension | |||||
| Etomidate Effect | Original analysis | 1.10 (1.00 to 1.22) | 1.06 (0.96 to 1.17) | 0.79 (0.48 to 1.32) | |
| + Bonferroni | 1.10 (0.97 to 1.25) | 1.06 (0.93 to 1.20) | 0.79 (0.41 to 1.55) | ||
| Propensity Score approach include severe hypotension | |||||
| Etomidate Effect | Original analysis | 1.11 (1.01 to 1.22) | 1.06 (0.96 to 1.16) | 0.77 (0.46 to 1.29) | |
| + Bonferroni | 1.11 (0.98 to 1.25) | 1.06 (0.94 to 1.20) | 0.77 (0.39 to 1.51) | ||
CI = confidence interval; HR = hazard ratio; OR = odds ratio.
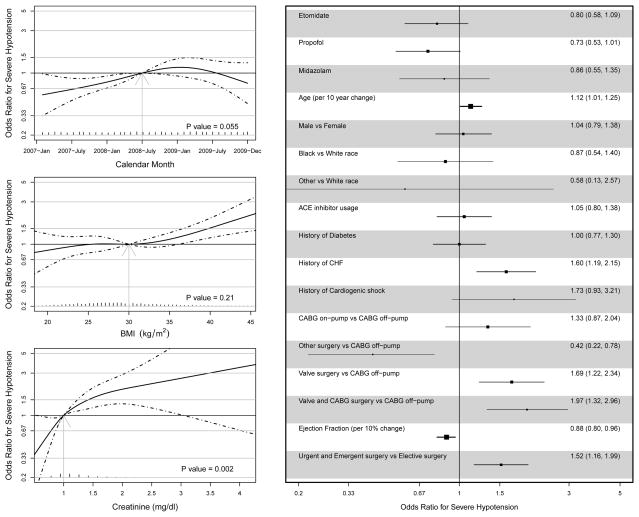
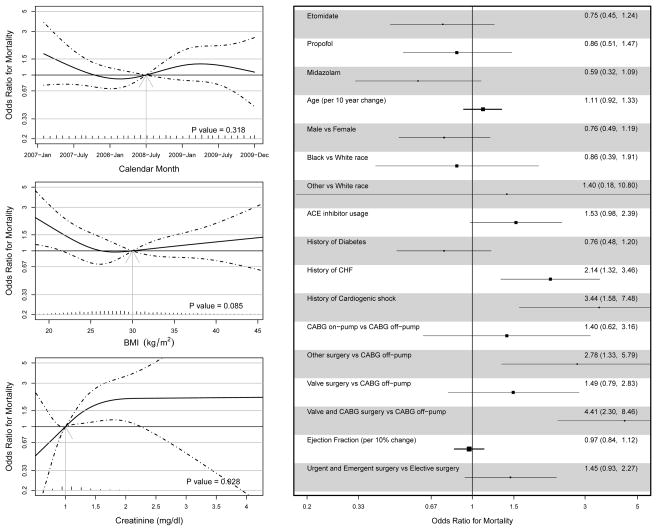
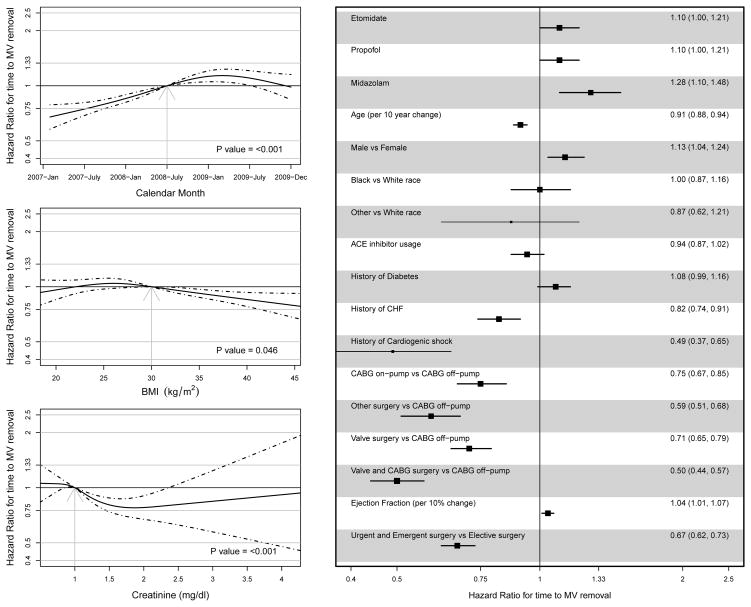
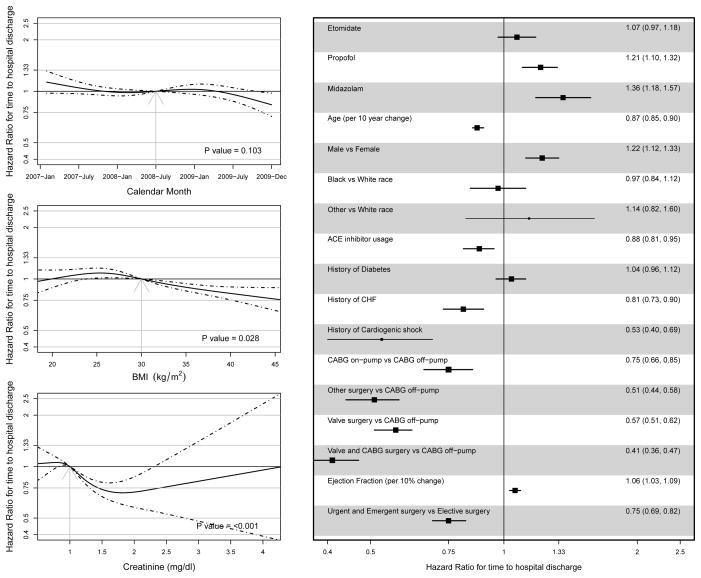
Other covariate effects are also shown in figures 1–4. Severe hypotension was independently predicted by preoperative creatinine, age, history of congestive heart failure (CHF), type of surgery, ejection fraction and surgery status. Independent predictors of longer time to mechanical ventilation removal included calendar month, BMI, preoperative creatinine, age, female gender, history of CHF, cardiogenic shock, type of surgery, lower ejection fraction and surgery status. Longer time to hospital discharge was independently predicted by BMI, preoperative creatinine, age, female gender, ACE inhibitor use, history of CHF, cardiogenic shock, type of surgery, lower ejection fraction and surgery status. Mortality was independently predicted by preoperative creatinine, a history of CHF, cardiogenic shock, and type of surgery. We also conducted additional analyses that examined the outcomes time to mechanical ventilation removal, time to hospital discharge, and in-hospital mortality with severe hypotension (yes/no) included as an independent variable (table 3). While severe hypotension was associated with increased time to mechanical ventilation removal (adjusted HR 0.49; 95% CI: 0.43 to 0.55), increased time to hospital discharge (adjusted HR 0.51; 95% CI: 0.45 to 0.58) and increased inhospital mortality (adjusted OR 3.6; 95% CI: 2.25 to 5.77), inclusion of it into the regression models did not have a notable impact on the relationship between etomidate use and time to mechanical ventilation removal, time to hospital discharge or in-hospital mortality.
Fig. 1.
Severe Hypotension Regression Analysis: Results are based on a multivariable logistic regression model, and odds ratios (OR) and 95% confidence intervals summarize the relative odds of severe hypotension. Calendar month, body mass index (BMI) and creatinine concentration were entered into the regression model flexibly using restricted cubic splines with four knots. To display effects sizes for the nonlinear effects, we chose a single reference value for each variable (calendar month = July 2008, BMI = 30 kg/m2, creatinine concentration = 1 mg/dl) and compared all other values to it. Due to lack of evidence suggesting a nonlinear relationship with any of the outcomes, the other continuous variables (age and ejection fraction) were modeled with linear terms and are included on the right with categorical variables. Categorical variables effects characterize the adjusted association between the outcome and the presence (vs. absence) of the risk factor. ACE = angiotensin-converting enzyme; CABG = coronary artery bypass graft; CHF = congestive heart failure.
Fig. 4.
In Hospital Mortality Regression Analysis: Results are based on a multivariable logistic regression model, and odds ratios (OR) and 95% confidence intervals summarize the relative odds of mortality during the hospitalization. Calendar month, body mass index (BMI) and creatinine concentration were entered into the regression model flexibly using restricted cubic splines with four knots. To display effects sizes for the nonlinear effects, we chose a single reference value for each variable (calendar month = July 2008, BMI = 30 kg/m2, creatinine concentration = 1 mg/dl) and compared all other values to it. Due to lack of evidence suggesting a nonlinear relationship with any of the outcomes, the other continuous variables (age and ejection fraction) were modeled with linear terms and are included on the right with categorical variables. Categorical variables effects characterize the adjusted association between the outcome and the presence (vs. absence) of the risk factor. ACE = angiotensin-converting enzyme; CABG = coronary artery bypass graft; CHF = congestive heart failure.
Discussion
We evaluated the association between single dose etomidate administration and important postoperative outcomes in a large cohort of cardiac surgery patients. After adjusting for potential confounders, there was no evidence to suggest that etomidate exposure was associated with severe hypotension, longer mechanical ventilation hours, longer length of hospital stay or inhospital mortality. Postoperative severe hypotension was an independent risk factor associated with an increased risk for longer mechanical ventilation hours, longer length of hospital stay and mortality.
Etomidate and Mortality
Etomidate, because of its neutral hemodynamic profile, is used to facilitate tracheal intubation in the operating room, ICU and emergency department. A single dose of etomidate causes temporary relative adrenal insufficiency. 2–5 This relative adrenal insufficiency associated with etomidate administration has raised concern that etomidate may increase morbidity and mortality in critically ill and septic patients that already have perturbations of the hypothalamic-pituitary -adrenal axis. The evidence supporting an increased mortality or morbidity in these patient populations, however, remains controversial.20 This is due to the fact that the majority of studies are retrospective in nature. A meta-analysis of 19 studies, four of which were randomized controlled trials of etomidate versus comparators,5,12,21,22 found a significant increase in mortality in patients that received etomidate (RR = 1.19; 95% CI 1.10 to 1.30).4 The retrospective analysis of the Corticosteroid Therapy of Septic Shock study23 suggested that etomidate use was associated with a 1.8 fold increased risk of mortality although the 95% CI ranged from 0.5 to 6.4. 24 A more recent retrospective review of 824 septic patients found a trend for increased mortality associated with etomidate use (RR = 1.20; 95% CI 0.99 to 1.45).6 Contrary to the previous studies, several retrospective studies have reported no significant increased risk of mortality associated with etomidate use in septic patients.7–10,25 In a prospective randomized study, Jabre et al 12 compared etomidate with ketamine as induction agent in 469 critically ill patients requiring emergency intubation. Not surprisingly, etomidate use was associated with more frequent adrenal insufficiency but no significant increase in mortality (OR 1.2; 95% CI 0.8 to 1.8). In the subgroup of 76 septic patients the odds ratio for mortality associated with etomidate use was 1.4 (95% CI 0.5 to 3.5). In addition, a smaller randomized prospective study comparing etomidate with midazolam for intubation in 122 septic patients found no significant difference in length of hospital stay or mortality (RR 1.2; 95% CI 0.8 to 1.9).11 Thus, although some retrospective studies suggest an increased mortality risk with etomidate use, none of the prospective studies support this finding.
Clinicians may be inclined to use etomidate in cardiac surgery patients with poor ventricular function and significant preoperative comorbidities as indicated by the more frequent use of etomidate in patients with a history of congestive heart failure. Thus, these patients maybe more likely to suffer adverse outcomes from etomidate-induced relative adrenal insufficiency. In our large heterogeneous cardiac surgery cohort, however, there was no evidence to suggest that etomidate exposure was associated with an increased risk of in-hospital mortality. The wide confidence intervals for the effect of etomidate on mortality is consistent with the odds of dying being 55% lower to 24% higher. In order to definitively address the potential impact of etomidate on mortality in a cardiac surgery population, a very large prospective randomized study will be needed to detect a difference in mortality between experimental and control subjects given that the observed mortality in our cohort was 3.4%.
Etomidate and Hypotension
In cardiac surgery patients most studies have focused on the effect of etomidate administration and vasopressor requirements. Iribarren et al13 examined a prospective cohort of 120 patients and found etomidate to be a risk factor for relative adrenal insufficiency and higher vasopressor requirements after surgery up to four hours after ICU admission. In the only prospective blinded randomized trial in cardiac surgery patients, Morel et al 14 evaluated the effect of etomidate or propofol on relative adrenal insufficiency and vasopressor requirements in 100 patients with normal left ventricular ejection fraction. The incidence of relative adrenal insufficiency was higher in the etomidate group up to 24 h after surgery but there was no difference in vasopressor requirements. Although hospital length of stay and mortality was similar between the two groups, their study was underpowered to detect a difference in these outcomes. Again, in our cardiac surgery cohort there was no evidence to suggest that etomidate exposure was associated with severe hypotension. Retrospective studies in cardiac surgery patients also suggest that preoperative ACE inhibitor use is associated with an increased risk of postoperative hypotension, renal dysfunction and death.26,27 After controlling for potential confounders, there was no evidence to suggest that preoperative ACE inhibitor use was associated with severe hypotension in our study cohort. This finding is consistent with a prospective randomized study in 445 cardiac surgery patients that did not demonstrate an increased risk of vasopressor requirements, renal dysfunction, prolonged mechanical ventilation hours or death in patients randomized to preoperative treatment with an ACE inhibitor.28 It is important to note that although etomidate use was not associated with postoperative severe hypotension, including severe hypotension as a covariate in the regression models indicated that severe hypotension was an independent predictor for, longer mechanical ventilation hours, longer length of hospital stay and mortality. The increased risk of adverse postoperative outcomes associated with postoperative hypotension in cardiac surgery patients is consistent with previous studies.29,30
Etomidate, Prolonged Mechanical Ventilation and Hospital Length of Stay
No large studies have evaluated the effect of etomidate use on prolonged mechanical ventilation or hospital length of stay in a cardiac surgical cohort. Our study had no evidence to suggest that etomidate exposure was associated with longer mechanical ventilation hours, or longer length of hospital and is consistent with one of the largest retrospective studies in sepsis patients where etomidate use did not associate with longer mechanical ventilation hours or hospital length of stay.8
Study Limitations
Our retrospective study has several limitations. While we controlled for most of the variables that might confound the relationship between etomidate use and adverse outcomes, there is always a possibility than an unmeasured variable might explain the lack of evidence between etomidate use and adverse outcomes. Our definition and identification of patients with severe hypotension was based on our clinical ICU protocol at the time and is different from vasoplegia definitions used in prior studies.26,29 Despite using a different definition for hypotension, we identified a high-risk group that was associated with a significant increased risk of adverse postoperative outcomes including death. The majority of our CABG surgeries is performed off-pump and may explain the observation that CABG only surgery was associated with shorter mechanical ventilation hours and shorter length of hospital stay compared to on-pump CABG surgery. The improvement in clinical outcomes associated with off-pump CABG surgery compared to on-pump CABG surgery is supported by some but not other large prospective clinical trials.31,32 Because of the change in etomidate administration over the study period we investigated the effect of calendar month in the multivariate models. For three of the four outcomes calendar month was not associated with worse outcomes. Calendar month, however, was a significant predictor of mechanical ventilation hours with shorter mechanical ventilation hours in the latter part of the study. One potential explanation for this decrease in mechanical ventilation hours may be improvement in ICU clinical protocols that allows for more rapid tracheal extubation. Finally, we did not assess adrenal function in all patients and therefore cannot comment on the effect of etomidate on adrenal function or on the potential impact of relative adrenal insufficiency on postoperative outcomes.
Conclusion
In this large retrospective cohort of cardiac surgical patients, there was no evidence to suggest that etomidate exposure was associated with postoperative severe hypotension, longer mechanical ventilation hours, longer length of hospital stay or in-hospital mortality. Thus, etomidate should remain an acceptable option for the induction of anesthesia in cardiac surgery patients despite the known risk of relative adrenal insufficiency. Only a large prospective randomized study will definitively address the effect of etomidate on postoperative outcomes in cardiac surgical patients.
Fig. 2.
Time to Mechanical Ventilation (MV) Removal Regression Analysis: Results are based on a multivariable Cox proportional hazards model, and hazard ratios (HR) and 95% confidence intervals summarize the relative rates at which MV was removed. Calendar month, body mass index (BMI) and creatinine concentration were entered into the regression model flexibly using restricted cubic splines with four knots. To display effects sizes for the nonlinear effects, we chose a single reference value for each variable (calendar month = July 2008, BMI = 30 kg/m2, creatinine concentration = 1 mg/dl) and compared all other values to it. Due to lack of evidence suggesting a nonlinear relationship with any of the outcomes, the other continuous variables (age and ejection fraction) were modeled with linear terms and are included on the right with categorical variables. Categorical variable effects characterize the adjusted association between the outcome and the presence (vs. absence) of the risk factor. Note that HR greater than (less than) one implies shorter (longer) time on MV. ACE = angiotensin-converting enzyme; CABG = coronary artery bypass graft; CHF = congestive heart failure.
Fig. 3.
Time to Hospital Discharge Regression Analysis: Results are based on a multivariable Cox proportional hazards model, and hazard ratios (HR) and 95% confidence intervals summarize the relative rates at which patients were discharged from the hospital. Calendar month, body mass index (BMI) and creatinine concentration were entered into the regression model flexibly using restricted cubic splines with four knots. To display effects sizes for the non-linear effects, we chose a single reference value for each variable (calendar month = July 2008, BMI = 30 kg/m2, creatinine concentration = 1 mg/dl) and compared all other values to it. Due to lack of evidence suggesting a nonlinear relationship with any of the outcomes, the other continuous variables (age and ejection fraction) were modeled with linear terms and are included on the right with categorical variables. Categorical variable effects characterize the adjusted association between the outcome and the presence (vs. absence) of the risk factor. Note that HR greater than (less than) one implies shorter (longer) length of stay. ACE = angiotensin-converting enzyme; CABG = coronary artery bypass graft; CHF = congestive heart failure.
Acknowledgments
Funding Sources: This research was funded by Vanderbilt Institute for Clinical and Translational Research grant support (UL1 TR000445 from National Center for Advancing Translational Science/National Institute of Health, Bethesda, Maryland) and Vanderbilt University Department of Anesthesiology, Nashville, Tennessee.
Footnotes
The authors declare no competing interests
References
- 1.Budde AO, Mets B. Pro: Etomidate is the ideal induction agent for a cardiac anesthetic. J Cardiothorac Vasc Anesth. 2013;27:180–3. doi: 10.1053/j.jvca.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 2.Cuthbertson BH, Sprung CL, Annane D, Chevret S, Garfield M, Goodman S, Laterre PF, Vincent JL, Freivogel K, Reinhart K, Singer M, Payen D, Weiss YG. The effects of etomidate on adrenal responsiveness and mortality in patients with septic shock. Intensive Care Med. 2009;35:1868–76. doi: 10.1007/s00134-009-1603-4. [DOI] [PubMed] [Google Scholar]
- 3.Hohl CM, Kelly-Smith CH, Yeung TC, Sweet DD, Doyle-Waters MM, Schulzer M. The effect of a bolus dose of etomidate on cortisol levels, mortality, and health services utilization: A systematic review. Ann Emerg Med. 2010;56:105–13. e5. doi: 10.1016/j.annemergmed.2010.01.030. [DOI] [PubMed] [Google Scholar]
- 4.Albert SG, Ariyan S, Rather A. The effect of etomidate on adrenal function in critical illness: A systematic review. Intensive Care Med. 2011;37:901–10. doi: 10.1007/s00134-011-2160-1. [DOI] [PubMed] [Google Scholar]
- 5.Absalom A, Pledger D, Kong A. Adrenocortical function in critically ill patients 24 h after a single dose of etomidate. Anaesthesia. 1999;54:861–7. doi: 10.1046/j.1365-2044.1999.01003.x. [DOI] [PubMed] [Google Scholar]
- 6.Sunshine JE, Deem S, Weiss NS, Yanez ND, Daniel S, Keech K, Brown M, Treggiari MM. Etomidate, adrenal function, and mortality in critically ill patients. Respir Care. 2013;58:639–46. doi: 10.4187/respcare.01956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dmello D, Taylor S, O’Brien J, Matuschak GM. Outcomes of etomidate in severe sepsis and septic shock. Chest. 2010;138:1327–32. doi: 10.1378/chest.10-0790. [DOI] [PubMed] [Google Scholar]
- 8.McPhee LC, Badawi O, Fraser GL, Lerwick PA, Riker RR, Zuckerman IH, Franey C, Seder DB. Single-dose etomidate is not associated with increased mortality in ICU patients with sepsis: Analysis of a large electronic ICU database. Crit Care Med. 2013;41:774–83. doi: 10.1097/CCM.0b013e318274190d. [DOI] [PubMed] [Google Scholar]
- 9.Ray DC, McKeown DW. Effect of induction agent on vasopressor and steroid use, and outcome in patients with septic shock. Crit Care. 2007;11:R56. doi: 10.1186/cc5916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riche FC, Boutron CM, Valleur P, Berton C, Laisne MJ, Launay JM, Chappuis P, Peynet J, Vicaut E, Payen D, Cholley BP. Adrenal response in patients with septic shock of abdominal origin: Relationship to survival. Intensive Care Med. 2007;33:1761–6. doi: 10.1007/s00134-007-0770-4. [DOI] [PubMed] [Google Scholar]
- 11.Tekwani KL, Watts HF, Sweis RT, Rzechula KH, Kulstad EB. A comparison of the effects of etomidate and midazolam on hospital length of stay in patients with suspected sepsis: A prospective, randomized study. Ann Emerg Med. 2010;56:481–9. doi: 10.1016/j.annemergmed.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 12.Jabre P, Combes X, Lapostolle F, Dhaouadi M, Ricard-Hibon A, Vivien B, Bertrand L, Beltramini A, Gamand P, Albizzati S, Perdrizet D, Lebail G, Chollet-Xemard C, Maxime V, Brun-Buisson C, Lefrant JY, Bollaert PE, Megarbane B, Ricard JD, Anguel N, Vicaut E, Adnet F, Group KCS. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: A multicentre randomised controlled trial. Lancet. 2009;374:293–300. doi: 10.1016/S0140-6736(09)60949-1. [DOI] [PubMed] [Google Scholar]
- 13.Iribarren JL, Jimenez JJ, Hernandez D, Lorenzo L, Brouard M, Milena A, Mora ML, Martinez R. Relative adrenal insufficiency and hemodynamic status in cardiopulmonary bypass surgery patients. A prospective cohort study. J Cardiothorac Surg. 2010;5:26. doi: 10.1186/1749-8090-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morel J, Salard M, Castelain C, Bayon MC, Lambert P, Vola M, Auboyer C, Molliex S. Haemodynamic consequences of etomidate administration in elective cardiac surgery: A randomized double-blinded study. Br J Anaesth. 2011;107:503–9. doi: 10.1093/bja/aer169. [DOI] [PubMed] [Google Scholar]
- 15.Malhotra AK. Con: Etomidate-the ideal induction agent for a cardiac anesthetic? J Cardiothorac Vasc Anesth. 2013;27:178–9. doi: 10.1053/j.jvca.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 16.Annane D. ICU physicians should abandon the use of etomidate! Intensive Care Med. 2005;31:325–6. doi: 10.1007/s00134-005-2560-1. [DOI] [PubMed] [Google Scholar]
- 17.Ge R, Pejo E, Cotten JF, Raines DE. Adrenocortical suppression and recovery after continuous hypnotic infusion: Etomidate versus its soft analogue cyclopropyl-methoxycarbonyl metomidate. Crit Care. 2013;17:R20. doi: 10.1186/cc12494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrell FE., Jr . Springer Series in Statistics. NY: Springer; 2001. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis; pp. 87–101. [Google Scholar]
- 19.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 20.Walls RM, Murphy MF. Clinical controversies: Etomidate as an induction agent for endotracheal intubation in patients with sepsis: Continue to use etomidate for intubation of patients with septic shock. Ann Emerg Med. 2008;52:13–4. doi: 10.1016/j.annemergmed.2008.01.344. [DOI] [PubMed] [Google Scholar]
- 21.Hildreth AN, Mejia VA, Maxwell RA, Smith PW, Dart BW, Barker DE. Adrenal suppression following a single dose of etomidate for rapid sequence induction: A prospective randomized study. J Trauma. 2008;65:573–9. doi: 10.1097/TA.0b013e31818255e8. [DOI] [PubMed] [Google Scholar]
- 22.Schenarts CL, Burton JH, Riker RR. Adrenocortical dysfunction following etomidate induction in emergency department patients. Acad Emerg Med. 2001;8:1–7. doi: 10.1111/j.1553-2712.2001.tb00537.x. [DOI] [PubMed] [Google Scholar]
- 23.Sprung CL, Annane D, Keh D, Moreno R, Singer M, Freivogel K, Weiss YG, Benbenishty J, Kalenka A, Forst H, Laterre PF, Reinhart K, Cuthbertson BH, Payen D, Briegel J. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358:111–24. doi: 10.1056/NEJMoa071366. [DOI] [PubMed] [Google Scholar]
- 24.Lipiner-Friedman D, Sprung CL, Laterre PF, Weiss Y, Goodman SV, Vogeser M, Briegel J, Keh D, Singer M, Moreno R, Bellissant E, Annane D. Adrenal function in sepsis: The retrospective Corticus cohort study. Crit Care Med. 2007;35:1012–8. doi: 10.1097/01.CCM.0000259465.92018.6E. [DOI] [PubMed] [Google Scholar]
- 25.Mohammad Z, Afessa B, Finkielman JD. The incidence of relative adrenal insufficiency in patients with septic shock after the administration of etomidate. Crit Care. 2006;10:R105. doi: 10.1186/cc4979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mekontso-Dessap A, Houel R, Soustelle C, Kirsch M, Thebert D, Loisance DY. Risk factors for post-cardiopulmonary bypass vasoplegia in patients with preserved left ventricular function. Ann Thorac Surg. 2001;71:1428–32. doi: 10.1016/s0003-4975(01)02486-9. [DOI] [PubMed] [Google Scholar]
- 27.Miceli A, Capoun R, Fino C, Narayan P, Bryan AJ, Angelini GD, Caputo M. Effects of angiotensin-converting enzyme inhibitor therapy on clinical outcome in patients undergoing coronary artery bypass grafting. J Am Coll Cardiol. 2009;54:1778–84. doi: 10.1016/j.jacc.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Pretorius M, Murray KT, Yu C, Byrne JG, Billings FTt, Petracek MR, Greelish JP, Hoff SJ, Ball SK, Mishra V, Body SC, Brown NJ. Angiotensin-converting enzyme inhibition or mineralocorticoid receptor blockade do not affect prevalence of atrial fibrillation in patients undergoing cardiac surgery. Crit Care Med. 2012;40:2805–12. doi: 10.1097/CCM.0b013e31825b8be2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Byrne JG, Leacche M, Paul S, Mihaljevic T, Rawn JD, Shernan SK, Mudge GH, Stevenson LW. Risk factors and outcomes for ‘vasoplegia syndrome’ following cardiac transplantation. Eur J Cardiothorac Surg. 2004;25:327–32. doi: 10.1016/j.ejcts.2003.11.032. [DOI] [PubMed] [Google Scholar]
- 30.Carrel T, Englberger L, Mohacsi P, Neidhart P, Schmidli J. Low systemic vascular resistance after cardiopulmonary bypass: Incidence, etiology, and clinical importance. J Card Surg. 2000;15:347–53. doi: 10.1111/j.1540-8191.2000.tb00470.x. [DOI] [PubMed] [Google Scholar]
- 31.Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Paolasso E, Straka Z, Piegas LS, Akar AR, Jain AR, Noiseux N, Padmanabhan C, Bahamondes JC, Novick RJ, Vaijyanath P, Reddy S, Tao L, Olavegogeascoechea PA, Airan B, Sulling TA, Whitlock RP, Ou Y, Ng J, Chrolavicius S, Yusuf S. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med. 2012;366:1489–97. doi: 10.1056/NEJMoa1200388. [DOI] [PubMed] [Google Scholar]
- 32.Shroyer AL, Grover FL, Hattler B, Collins JF, McDonald GO, Kozora E, Lucke JC, Baltz JH, Novitzky D. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med. 2009;361:1827–37. doi: 10.1056/NEJMoa0902905. [DOI] [PubMed] [Google Scholar]