Abstract
Few studies have longitudinally examined suicidal ideation in those with adolescent-onset BPD. The current study aimed to examine the trajectory of suicidal ideation in adolescents with BPD longitudinally over six months, with follow-ups at 2, 4, and 6 months post-hospitalization for elevated suicide risk. Resulted indicated that the BPD group exhibited a greater decrease in suicidal ideation in the months following hospitalization than those without a BPD diagnosis. The findings of this study indicated that suicidal ideation in adolescents with BPD is not stable, and although ideation may decrease quickly after hospitalization, regular assessment of ideation is recommended.
Keywords: adolescents, borderline personality disorder, suicidal ideation, instability
The experiences of suicidal ideation and behavior are well documented in adults diagnosed with borderline personality disorder (BPD; Links et al., 2007; Yen et al., 2004), and suicidal ideation appears to be chronic for many with this diagnosis (Mehlum et al., 1994; Paris, 2002). However, consistent evidence has emerged indicating that BPD is likely to remit within 6–10 years following diagnosis, even without treatment (Gunderson et al., 2011; Zanarini et al., 2004). This suggests that BPD may not be as stable as once thought, and that further longitudinal investigation of BPD symptoms and suicidal ideation is needed. Furthermore, BPD has generally been considered a disorder that emerges in adulthood and is unusual, though diagnosable if present for at least one year, in adolescents (APA, 2000). Yet again, studies are finding that this is likely inaccurate, with diagnostic-level symptoms of the disorder emerging for a number of patients in middle to late adolescence (Miller, Muehlenkamp, & Jacobson, 2008; Winograd, Cohen, & Chen, 2008). Diagnostic rates may even reach as high as 8% in adolescents (Bernstein et al., 1993). Furthermore, when adult criteria for BPD are applied to adolescent samples, a distinct group appears to meet criteria for BPD and they appear distinguishable on a number of factors relative to comparison groups (Bradley, Conklin & Westen, 2004; Garnet et al., 1994; Ludolph et al., 1990).
Given these changes in long-held clinical beliefs about BPD, it would be a mistake to assume that adolescent-onset BPD presents in the same manner as in adults. Additional attention needs to be paid to understanding BPD as it presents in adolescents specifically, and to determine whether adolescent BPD may be fundamentally different than adults with BPD, or if it is merely early-detected BPD. Understanding the development of BPD from adolescence into adulthood will likely improve our ability to diagnose and treat BPD better at both stages of development.
One area in particular need of research is the examination of suicidal ideation in adolescents with BPD, which may not necessarily be as chronic as in adult patients with BPD (Mehlum et al., 1994; Paris, 2002). It is important to further refine our understanding of suicidal ideation in adolescents with BPD, because BPD is a disorder characterized by frequent emotion dysregulation. Adolescence is a time of frequent changes and potential emotion dysregulation, and given the link between adolescent emotion dysregulation and suicidal behavior (Esposito et al., 2003; Spirito et al., 2003), adolescents with BPD may require even closer monitoring than other suicidal adolescents. Research examining the experience of suicidal ideation in adolescents with BPD is rare; most extant studies of adolescent BPD have focused only on suicide attempts. One study found that a large portion of adolescents who had recently attempted suicide met DSM-III diagnostic criteria for BPD (Crumley, 1979). In another study, suicide attempt in adolescents was predictive of the number of BPD symptoms endorsed (Brent, et al. 1993). When compared to depressed adolescents, another study found that adolescents with BPD had more anger and impulsivity, which was related to their suicidal ideation; however, those with depression diagnoses reported more intent at their last suicidal attempt than the BPD group (Netta et al., 2003). Thus, the research on suicidal behavior and adolescents with BPD indicates that suicidal ideation is an important concern, although the nature of suicidal ideation and behavior in this group still has yet to be clarified.
When studying suicidal ideation and BPD in adolescents, it would seem practical to extend many of the findings from the adult literature for BPD to adolescents (e.g., assuming more chronic levels of suicidal ideation relative to those without BPD). But there are three issues that should be fully considered when making such hypotheses. First, evidence continues to indicate that BPD is a disorder that has many acute qualities, as opposed to being a disorder that is chronic across the lifetime (Bornovalova, Hicks, Iacono, & McGue, 2009; Gunderson et al., 2011; Shea et al, 2002; Zanarini et al., 2004). This means that those with BPD do not appear to experience consistent year after year of highly elevated BPD symptoms. Rather, their symptoms appear to wax and wane over the years. When their symptoms are at their highest, it is likely due in part to particularly bad environmental circumstances (Crowell, Beauchaine, & Linehan, 2009; Selby & Joiner, 2009). When their symptoms wane, they may experience a decreased number and severity of symptoms, but it is unlikely that they are symptom free. These findings of variability over time in the number and severity of symptoms in adults with BPD begets the question of how stable BPD symptoms are in adolescents as well. Second, adolescence itself is a time characterized by frequent change. Most adolescents experience their identity as changing on a regular basis, as are their peer groups, general interests, and methods of coping (Bleiberg, 1994; Westen, Betan, & Defife, 2011; Shapiro, 1990). All of these issues suggest that fluctuations in number and severity of BPD symptoms may be worse in adolescents than adults. This notion is consistent with findings that BPD symptoms appear somewhat unstable in adolescent samples (Bernstein et al., 1993; Bondurant, Greenfield, & Tse, 2004; Mattanah et al., 1995; Meijer, Goedhart, & Treffers, 1998). However, more research is needed on the stability of BPD symptoms in adolescents, given some studies suggest stability of adolescent-onset BPD diagnosis (Chanen et al., 2004; Miller et al., 2008).
Finally, suicidal ideation is itself a variable that is somewhat unstable. Research has indicated that the dichotomous experience of suicidal ideation (present or absent) tends to be somewhat more stable (Beck, Brown, Steer, Dahlsgaard, & Grisham, 1999). However, for those who experience suicidal ideation, the range from mild to severe suicidal ideation actually tends to be more unstable, varying on a daily and weekly basis and as a function of previous number of suicide attempts (Witte et al., 2005; Witte et al., 2006). In fact, one recent study on suicidal adolescents found that weekly changes in the experience of emotion dysregulation, as well as family and peer invalidation, predicted subsequent increases in suicidal ideation the next week (Selby, Yen, & Spirito, 2013). These findings suggest that suicidal ideation may be particularly unstable in adolescents, and that adolescents with BPD may experience even larger changes in suicidal ideation over time. Given these three caveats, we refrained from hypothesizing that adolescents with BPD would experience chronically elevated suicidal ideation, despite the more chronic pattern of suicidal ideation that may be exhibited by adults with BPD.
The purpose of the current study was to address the lacunae in the literature regarding post-hospital trajectory of suicidal ideation in adolescents with BPD relative to suicidal adolescents without BPD. To do this we examined a sample of adolescent patients who were recently hospitalized for suicidal crisis, many of whom met criteria for BPD. These adolescents were assessed at baseline, and again at 2, 4, and 6 months post-hospitalization, with each assessment including the experience of current and recent suicidal ideation. Adults with BPD frequently experience chronic suicidal ideation despite hospitalization (Mehlum, Friis, Vaglum, & Karterud, 1994; Paris, 2004), so extending the hypothesis of more chronic suicidal ideation to adolescents with BPD would seem to make sense. But given our concerns about the instability of BPD in adolescents, and issues with instability of suicidal ideation in general, we refrained from making any specific hypotheses regarding the trajectory of suicidal ideation in this group. However, we expected to observe one of two potential patterns. First, suicidal ideation in adolescents with BPD could be consistently high and stable for the duration of follow-up, following patterns of chronic elevations in suicidal ideation identified in adults (Paris, 2002). Second, ideation could decrease subsequent to baseline risk assessment, suggesting that suicidal ideation in adolescents with BPD is not necessarily stable over time.
Methods
Participants
Participants consisted of 119 suicidal adolescents who were recruited for a naturalistic follow-up study on the course of social and emotional functioning over the 6-month period following a psychiatric hospitalization. Data were obtained from the participants as well as the legal guardians/primary caregivers of the participants. Participants were recruited from the adolescent inpatient unit of a psychiatric hospital in New England on the basis of having been recently hospitalized for elevated suicide risk (e.g., recent suicide attempt, self-injury with SI, or SI). Adolescents and parents were compensated for their time with a payment of $50 each, for the baseline interview and for the 6-month follow-up interview. Of the 119 adolescents, 81 were female (68%), and the sample was 78.5% Caucasian, 10.0% African American, and 1.7% American Indian/Alaskan native; 9.8% of the sample reported identifying multiple races, without one race being primary.. Twenty-two patients (18%) endorsed Hispanic ethnicity. The patients’ ages ranged from 12 to 18 years old with a mean age of 15.3 (SD=1.4). This study was approved by the Institutional Review Boards of Brown University and the respective hospital. All participants completed parental consent and adolescent assent before the intake assessment. Previous studies on suicidal ideation and suicidal behavior have been published using these data (Yen, Weinstock, Andover, Sheets, Selby, & Spirito, 2013; Selby, Yen, & Spirito, 2013); however, no studies using these data have examined the longitudinal course of suicidal ideation in adolescents with and without BPD.
Procedure
During hospitalization, participants and caregivers completed baseline interviews and assessment batteries. When patient and caregiver reports were discrepant, consensus scores for those symptoms were determined during weekly case review meetings using all available information, including chart review and information from treating physician on the adolescent unit. Following the baseline assessments, patients were later contacted by phone for 2 and 4-months follow-up assessments, and for a final in-person 6-month assessment. Interviews were administered by members of the research team including post-doctoral fellows, master’s level clinical psychology students, and research assistants with at least a bachelors degree. All were trained to threshold ability on administration of interviews by the principal investigator (S.Y.).
Baseline Assessment Measures
Schedule for Affective Disorders and Schizophrenia for School Aged Children – Present and Lifetime Versions (K-SADS-PL)
The K-SADS-PL (Kaufman et al., 1997) was administered to assess baseline psychiatric diagnoses. The K-SADS is a reliable and valid assessment of DSM-IV psychopathology in children and adolescents, with high inter-rater agreement generally found by the developers (kappa range: .93–1.0). In the current sample, interrater reliability for all K-SADS diagnoses ranged from 0.61–1.00, indicating good agreement (Yen et al., 2013). In this study, current depression, bipolar I, conduct disorder, posttraumatic stress disorder (PTSD), and alcohol dependence were utilized as covariates given their association with suicidal ideation and attempts in adolescents in clinically ascertained and epidemiologic samples (Linker, Gillespie, Maes, Eaves, & Silberg, 2012; Nock et al., 2008; Nock, Hwang, Sampson, & Kessler, 2010). We also included family history of a suicide attempt (0=no, 1=yes) as a covariate to account for family influences on suicidal ideation.
Childhood Interview for Borderline Personality Disorders (CI-BPD)
The CI-BPD is the adolescent adaptation of the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini et al., 1996), a semi-structured diagnostic interview that assesses the DSM-IV personality disorders. The CI-BPD focuses only on BPD and was administered at baseline. The DIPD-IV compares favorably to other structured interviews for personality disorders, with excellent inter-rater reliability and test-retest reliability (kappa coefficients for BPD = .94 and .85 respectively; Zanarini et al., 1987). Each BPD diagnostic criterion was assessed with multiple questions, and coded as absent, subthreshold, or present. To meet criteria for a BPD diagnosis participants needed to meet full threshold level for at least 5 of the BPD diagnostic symptoms. Regarding inter-rater reliability in the present sample, the kappa coefficient based on twenty interviews was 0.82, indicating adequate inter-rater agreement.
Longitudinal Interval Follow-Up Evaluation - Adolescent version – Baseline (LIFE; Keller et al., 1987)
The LIFE is a semi-structured interview rating system with demonstrated reliability for assessing the longitudinal course of psychiatric disorders (Warshaw, Dyck, Allsworth, Stout, and Keller, 2001; Warshaw, Keller, & Stout, 1994). The LIFE methodology and rating system has also been applied to the assessment of suicidal ideation in large psychiatric adolescent samples (e.g. the Course and Outcome of Bipolar Youth [COBY] Study; Birmaher et al., 2009), which have found strong interrater reliability for this scale. The present study used this same methodology and rating scale to establish a baseline level of suicidal ideation. To determine Psychiatric Status Ratings (PSR) for suicidal ideation, participants are asked the following questions in a semi-structured manner:
“Sometimes when people are upset or feel bad they think about dying or even killing themselves. Do you have these thoughts during these past six months? How often did you have these thoughts? When you had them, how long did they last – a few minutes, an hour or more, almost always? Did you have these thoughts throughout the past month or where there times when you did not have these thoughts? Do you have those thoughts now? Do you have a plan? What is it? Have you told anyone about these thoughts or plans?”
This baseline PSR score takes into consideration data gathered from other diagnostic clinical interviews (in the present study, the KSADS-PL) such that baseline PSR scores are obtained for disorders in which the participant meets criteria and functioning across multiple domains. The PSR utilized a 6-point scale interview rating with scores assigned as: PSR 6 = extremely intense, PSR 5 = high, PSR 4 = moderate, PSR 3 = somewhat, PSR 2 = minimal, PSR 1 = not present. Baseline inter-rater reliability for PSR ratings was assessed with a random sample of 10% of the participants whose interviews were reviewed and rated by a second blind reviewer. Rater agreement was good for the suicidal ideation PSR at baseline (κ = .90).
Follow-Up Assessment Measure
Longitudinal Interval Follow-Up Evaluation - Adolescent version – Follow-up
Follow-up assessments were completed with the LIFE interview at the 2, 4, and 6-months after hospitalization. During these assessments, a weekly PSR variable was established for suicidal ideation. As part of the interview, patients were asked to identify time anchors (e.g., life events, birthdays, holidays) in the preceding time intervals to assist with recall of suicidal ideation level. Patients were reminded of their original response at the previous assessment and asked whether changes had occurred during the follow-up interval. For each period of change, suicidal ideation was re-evaluated for the present and previous weeks, yielding PSR values for each week of follow-up (i.e. 26 weeks), although we only used the assessments at 2, 4, and 6 months follow-up in data analysis because these assessments were current rather than retrospective. The follow-up suicidal ideation PSR rating used the same scale as the baseline rating described above. Good to excellent inter-rater and test-retest reliabilities have been established for the LIFE Follow-up using a different sample in another longitudinal, naturalistic study with a similar assessment protocol (Warshaw, Dyck, Allsworth, Stout, and Keller, 2001; Warshaw, Keller, & Stout, 1994). The baseline and follow-up LIFE suicidal ideation PSR variables in this sample were found to have good interrater reliability with both kappas being over .90 (Selby, Yen, & Spirito, in press).
Data Analysis
The purpose of the current study was to examine the course of suicidal ideation in adolescents diagnosed with BPD in comparison to a group of suicidal adolescents without BPD. To examine the course of suicidal ideation in this sample, we utilized repeated measures ANOVA analyses with four time-points: baseline and follow-up at 2, 4, and 6 months. The follow-ups at 2, 4, and 6 months were chosen for the model because these were the points that adolescents were contacted for assessment, and at each time their current level of suicidal ideation was assessed. Ideation was also assessed for the previous weeks at each assessment, but we only used the current assessment to reduce potential for issues with retrospective recall. The repeated measures ANOVA approach is also ideal for examining trajectory of suicidal ideation over follow-up because it takes into account change based on baseline and previously assessed levels of ideation. To account for sphericity between measurements, the analysis was corrected using the Greenhouse-Geisserê statistic. Finally, the following were used as covariates in the model to ensure that potential group differences were not driving any observed effects: age, sex, race, medication prescription at baseline, major depression, bipolar 1, conduct disorder, PTSD, alcohol dependence, and family history of a suicide attempt. These covariates were selected based on potential relationship to suicidal ideation in adolescents, and to demonstrate that the association between BPD and suicidal ideation over time was beyond the contributions of these factors.
Results
Preliminary Analyses
A total of 48 (40%) of the adolescents met diagnostic criteria for BPD. Regarding other psychiatric diagnoses in the sample, the most commonly diagnosed Axis I disorder was major depressive disorder (85%). Bipolar I disorder (N=7, 6%) and conduct disorder (N=28, 24%) diagnoses were also represented in the sample. Those with BPD diagnoses had did not have a higher proportion of depression diagnoses (χ2(1)=1.43, p=.23), bipolar 1 (χ2(1)=.93, p=.35), or conduct disorder (χ2(1)=1.58, p=.21) than the main sample. Overall, there were 107 (88%) patients being prescribed psychotropic medication at the baseline assessment, but rates did not differ for the BPD group (χ2(1)=.52, p=.47). Patient functioning at baseline, as measured by GAF scores from the KSADS, was essentially the same for both groups, with an average of 42.75 (SD=7.70) for those without BPD and 42.75 (SD=7.46) for those with BPD, which was not a significant difference. In the current sample, the only difference in outpatient treatment post-hospitalization between those with and without BPD was that those with BPD were more likely to be in a group versus individual treatment modality (Yen, 2013).
Attrition
Due to the intensive nature of collecting data over a period of 6 months, some participant drop out or loss of contact was expected. Overall, 20 patients dropped out after the baseline assessment and during the course of the follow-up assessments, meaning that 82% of the sample completed the full study. The pattern of drop-out consisted of 15 patients who did not provide any follow-up data, 2 who provided only 2 months of follow-up data, and 3 who provided only 4 months of follow-up data. Group comparisons indicated that those who dropped out were not more suicidal (t(118)= -1.13, p>.05), and they were not more likely to have a BPD diagnosis (χ2(1)=.335, p>.05). We further probed the potential that those who dropped out and had BPD diagnoses might have had higher baseline suicidal ideation, so we examined the interaction with linear regression. This interaction term was not significant (B=−.19, t=.111, p>.05), indicating that it was unlikely those who dropped out had BPD diagnoses and were highly suicidal.
Changes in Suicidal Ideation Over 6 Months
The group differences in average levels of suicidal ideation at each assessment are graphed in Figure 1. We examined only baseline and the three 2-month follow-up assessments of suicidal ideation, and included them in the repeated measures model, because including assessments with retrospective recall from the weeks between phone assessments could increase chances of recall bias. Regarding group differences in suicidal ideation, there were no significant differences at baseline (F(1, 117)=.03, p>.05); this did not change when covariates were included in the model. The follow-up sessions were examined, after controlling for baseline SI and the covariates, and significant group differences were found such that BPD was prospectively associated with lower suicidal ideation at 2-months (F(1, 77)=5.82, p=.018, ηp2=.071), 4-months follow-up (F(1, 77)=4.31, p=.041, ηp2=.054), and 6 months follow-up (F(1, 77)=7.41, p=.008, ηp2=.089)1. In the multivariate model with all covariates, age, sex, race, medication at baseline, bipolar I, alcohol dependence, PTSD, conduct disorder, and family history of a suicide attempt did not significantly predict suicidal ideation six months later. The only other variables that indicated significant differences at 6-month follow-up were baseline suicidal ideation (F(1, 77)=10.635, p=.002, ηp2=.123) and major depression diagnosis (F(1, 77)= 19.85, p<.001, ηp2=.207).
Figure 1.
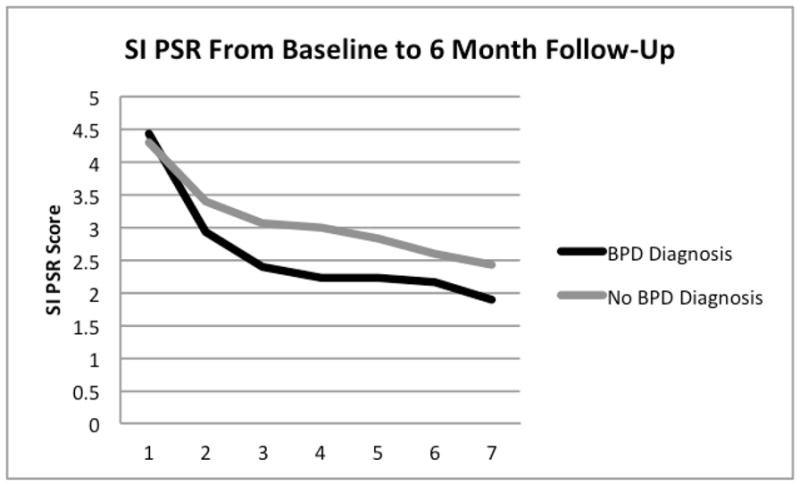
Caption: Changes in suicidal ideation (SI) psychiatric status rating (PSR) for those adolescents with and without BPD diagnoses from baseline over the course of 6-months of follow-up assessments. Note: For Months 1 pertains to the baseline assessment.
Because significant spehericity was indicated (W=.723, χ2(5)=42.52, p<.001), we used the Greenhouse-Geisserê statistic to correct for significance when determining if there was a group difference in trajectory of change in the repeated measures model. As can been seen in Figure 1, there was a significant time interaction with BPD diagnosis, such that the BPD group showed larger linear decreases in suicidal ideation over the duration of the follow-up (F(1, 77)=5.128, p<.05, ηp2=.062) than those without a BPD diagnosis. Despite the potential curve in Figure 1, the quadratic time interaction with BPD diagnosis was not significant (F(1, 77)=2.59, p>.05), indicating that the rate of decrease in suicidal ideation for the BPD group was relatively constant throughout follow-up. These results again held after accounting for all covariates. Regarding covariates, the only significant predictor of change in suicidal ideation during follow-up was baseline diagnosis of depression (F(1, 77)=14.81, p<.05, ηp2=.17), with findings indicated that those with depression also experienced a decrease in suicidal ideation over time.
Discussion
More research on the stability of the experience of suicidal ideation over time in adolescents with BPD is needed. The purpose of the current study was to examine trajectory of suicidal ideation post-hospitalization in suicidal adolescents with BPD, and to compare this trajectory to that of suicidal adolescents without BPD diagnoses. The findings of this study indicated that, despite the potential for chronic suicidal ideation in adults with BPD assessed longitudinally (Mehlum et al., 1994), the BPD adolescents in this study experienced greater decreases in suicidal ideation over 6 months post-hospitalization than those without BPD diagnoses. Although suicidal ideation in adolescents with BPD may be just as intense or severe as those with other diagnoses who are hospitalized, the experience of suicidal ideation following discharge may be less persistent in this group.
The finding of greater reductions in suicidal ideation following hospitalization is both potentially promising and a point of caution. The promising aspect is that hospitalization may have helped the patients (those with BPD in particular) and treatment may have effectively ameliorated the problems they were experiencing. This could potentially indicate a positive prognosis for some adolescents with BPD, supporting the treatment role of hospitalization.
On the other hand, the finding of sharp decreases in the suicidal ideation of adolescents with BPD is consistent with emerging research that some aspects of BPD in adolescents may be unstable. In fact, BPD symptom in adolescents may be even more unstable than BPD symptoms in adults. Greater instability of BPD symptoms of adolescents would seem consistent with developmental stage, given that adolescence is characterized by frequent changes in identity, peer group, and environment. In the case of suicidal ideation in adolescents with BPD, instability is not a reason for less concern, but rather potential cause for more concern. The finding that adolescents with BPD exhibited instability of suicidal ideation does not necessarily mean that ideation is less severe, but rather that it may be more transient, making it potentially more difficult to predict its course. Thus, instability of suicidal ideation in adolescents with BPD could be cause for closer monitoring and care.
This study enhances current understanding of the longitudinal experience of suicidal ideation in adolescents with BPD. However, additional questions remain about the potential differences between adolescents and adults with this disorder. The current study suggests that there may be a difference in the experience of suicidal ideation between these groups, with adolescents potentially exhibiting less chronic suicidal ideation than has been previously identified in adults (Paris, 2002). However, this study did not compare adolescents and adults with BPD, and no studies to our knowledge have done this. Future studies should examine specific differences in these two samples, particularly the experience of suicidal ideation.
The findings of the current study should be interpreted in light of some limitations. One important limitation was that this study, despite its longitudinal design, is that it did not extend even further with follow-up. It’s possible that with more time the level of suicidal ideation in the BPD group may have eventually increased, while those without BPD may have experienced a continuing decreasing trend. Furthermore, even if suicidal ideation is acutely less chronic in adolescence, this experience likely changes during adulthood, as findings indicate much more chronic suicidal ideation in adults. Another important limitation to acknowledge with the current study is that suicidal ideation was only assessed ever couple of months, but suicidal ideation can vary largely between and even within days. However, this study was useful in that it assessed average level of suicidal ideation, which may serve to illustrate an average set point at which suicidal ideation fluctuates around. Furthermore, suicidal ideation in adolescents with BPD who were not hospitalized may change differentially over time relative to those with BPD who were hospitalized, as hospitalization is likely to influence the experience of subsequent suicidal ideation. Therefore, these findings may not necessarily generalize to adolescents with BPD who have not been hospitalized. Another limitation to note was that the effect sizes obtained for BPD on suicidal ideation over time were medium, indicating that although BPD has important influences on suicidal ideation, it is just one of many factors to consider when assessing and treating suicidal ideation in adolescents. Finally, because this was a sample of adolescents hospitalized for suicidal ideation, the findings of decreased suicidal ideation may have been directly related to treatment received in the hospital, and without intervention the suicidal ideation of the BPD group may have been more chronic.
Another issue was that although those with BPD exhibited sharper decreases in suicidal ideation over follow-up, high levels of the variability of suicidal ideation were not observed at each assessment point. Such a finding would have been indicated with more peaks represented in Figure 1. This finding may have been the result of the length between our assessments, which were every two months (with retrospective report of the previous weekly levels of suicidal ideation at those assessments). This assessment interval may have smoothed-over variability in suicidal ideation that occurs from day-to-day. Thus, although our approach demonstrated instability of suicidal ideation over a time scale of months, there are other alternatives and time scales that can be used to examine instability. With future research, the experience of suicidal ideation in adolescents with BPD should be examined with a finer time scale, examining suicidal ideation within and between days.
There are multiple directions for future research to expand on the current study. As previously mentioned, an important future direction involves examining suicidal ideation in adolescents with BPD with a finer time scale. Such research could be conducted using ecological momentary assessment, where participants rate their emotional and cognitive experiences multiple times daily over a period of multiple days using smartphone technology, and would allow for within- and between-day analysis of fluctuation in suicidal ideation. Furthermore, additional research should examine moderators of changes in suicidal ideation in adolescents with BPD, such as potential influences from peer and family interactions that may lead to increases in ideation (Selby, Yen, & Spirito, 2013). Additional research should also examine individual differences that may moderate changes in the suicidal ideation of adolescents with BPD, such as major personality traits (e.g., introversion, low conscientiousness; Hopwood & Zanarini, 2010) or specific forms of emotion dysregulation (e.g., rumination; Selby & Joiner, 2013). Such research would increase our understanding of the factors that may lead to transient increases in suicidal ideation in adolescents with BPD.
The findings of this study serve to highlight the need for more research on adolescents with BPD. Even though adults with BPD may experience chronic suicidal ideation, this may not necessarily be the case with adolescent-onset BPD. Given how tumultuous the adolescent experience can be, it may be that suicidal ideation in this group is highly linked to environmental circumstances, and if those circumstances change their ideation may decrease. Thus, it may be important to identify other areas for potential differences in those with adolescent-onset BPD, such as level of intent and lethality of suicide attempts, amount of planning engaged in, and interpersonal factors influencing suicidal behavior.
Table 1.
Suicidal Ideation Level at Baseline and Follow-Up Assessments
| BPD | no-BPD | F(df) | p | ηp2 | |
|---|---|---|---|---|---|
| M(SD) | M(SD) | ||||
| Baseline Suicidal Ideation | 4.42(1.12) | 4.31(1.38) | .03(1, 117) | .862 | .001 |
| 2 Month Follow-up | 2.42(1.44) | 3.02(1.50) | 5.82(1, 77) | .018 | .071 |
| 4 Month Follow-Up | 2.21(1.43) | 2.83(1.76) | 4.31(1, 77) | .041 | .054 |
| 6 Month Follow-Up | 1.88(1.34) | 2.42(1.54) | 7.41(1,77) | .008 | .089 |
| BPD by Time Interaction | 5.13(1, 77) | .026 | .062 | ||
| BPD by Time2 Interaction | 2.59(1, 77) | .112 | .033 | ||
Note: BPD= borderline personality disorder
Acknowledgments
Funding for this project was provided by National Institute of Mental Health grant K23 MH069904 to Shirley Yen. Support was also provided by a Brain and Behavior Research Foundation NARSAD Young Investigator Grant to Edward Selby, with support from the Families for Borderline Personality Disorder Research.
Footnotes
Note that an effect size of ηp2=.06 is considered a medium effect, while ηp2=.14 is considered large (Cohen, 1988).
Contributor Information
Edward A. Selby, Rutgers University.
Shirley Yen, Brown University –Warren Alpert Medical School.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of mental Disorders. 4. Washington, D.C: American Psychiatric Association; 2000. text revision. [Google Scholar]
- Beck AT, Brown GK, Steer RA, Dahlsgaard KK, Grisham JR. Suicide ideation at its worst point: A predictor of eventual suicide in psychiatric outpatients. Suicide and Life-Threatening Behavior. 2010;29:1–9. [PubMed] [Google Scholar]
- Bernstein DP, Cohen P, Velez CN, Schwab-Stone M, Siever LJ, Shinsato L. Prevalence and stability of the DSM-III-R personality disorders in a community based survey of adolescents. American Journal of Psychiatry. 1993;150:1237–1243. doi: 10.1176/ajp.150.8.1237. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, Houck P, Ha W, Iyengar S, Kim E, Yen S, Hower H, Esposito C, Goldstein T, Ryan N, Keller M. Four-year longitudinal course of children and adolescents with bipolar spectrum disorder: The Course and Outcome of Bipolar Youth (COBY) Study. American Journal of Psychiatry. 2009;166:795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleiberg E. Borderline disorders in children and adolescents: The concept, the diagnosis, and the controversies. Bulletin of the Menninger Clinic. 1994;58:169–196. [PubMed] [Google Scholar]
- Bondurant H, Greenfield B, Tse SM. Construct validity of the adolescent borderline personality disorder: A review. Canadian Child and Adolescent Psychiatry Review. 2004;13:53–57. [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Development and Psychopathlogy. 2009;21:1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley R, Conklin CZ, Westen D. The borderline personality diagnosis in adolescents: Gender differences and subtypes. Journal of Child Psychology and Psychiatry. 2004;46:1006–1019. doi: 10.1111/j.1469-7610.2004.00401.x. [DOI] [PubMed] [Google Scholar]
- Brent DA, Johnson B, Bartle S, Bridge J, Rather C, Matta J, Connolly J, Constantine D. Personality disorder, tendency to impulsive violence, and suicidal behavior in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:69–75. doi: 10.1097/00004583-199301000-00010. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Jackson HJ, McGorry PD, Allot KA, Yuen HP. Two-year stability of personality disorder in older adolescent outpatients. Journal of Personality Disorders. 2004;18:526–541. doi: 10.1521/pedi.18.6.526.54798. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin. 2009;135:495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crumley FE. Adolescent suicide attempts. Journal of the American Medical Association. 1979;241:2404–2407. [PubMed] [Google Scholar]
- Esposito C, Spirito A, Boergers J, Donaldson D. Affective, behavioral, and cognitive functioning in adolescents with multiple suicide attempts. Suicide and Life-Threatening Behavior. 2003;33:389–399. doi: 10.1521/suli.33.4.389.25231. [DOI] [PubMed] [Google Scholar]
- Garnet KE, Levy KN, Mattanah JJF, Edell WS, McGlashan TH. Borderline personality disorder in adolescents: Ubiquitous or specific? American Journal of Psychiatry. 1994;151:1380–1382. doi: 10.1176/ajp.151.9.1380. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, Zanarini MC, Yen S, Markowitz JC, Sanislow C, Ansel E, Pinto A, Skodol AE. Ten-year course of borderline personality disorder: Psychopathology and function from the Collaborative Longitudinal Personality Disorders Study. Archives of General Psychiatry. 2011;68:827–837. doi: 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Zanarini MC. Five factor trait instability in borderline relative to other personality disorders. Personality Disorders: Theory, Research, and Treatment. 2010;1:58–66. doi: 10.1037/a0018230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-age Children- Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Linker J, Gillespie NA, Maes H, Eaves L, Silberg JL. Suicidal ideation, depression, and conduct disorder in a sample of adolescent and young adult twins. Suicide and Life-Threatening Behaviors. 2012;42:426–436. doi: 10.1111/j.1943-278X.2012.00101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Links PS, Eynan R, Heisel MJ, Barr A, Korzekwa M, McMain S, Ball JS. Affective instability and suicidal ideation and behavior in patients with borderline personality disorder. Journal of Personality Disorders. 2007;21:72–86. doi: 10.1521/pedi.2007.21.1.72. [DOI] [PubMed] [Google Scholar]
- Ludolph PS, Westen D, Misle B, Jackson A, Wixom J, Wiss FC. The borderline diagnosis in adolescents: Symptoms and developmental history. American Journal of Psychiatry. 1990;147:470–476. doi: 10.1176/ajp.147.4.470. [DOI] [PubMed] [Google Scholar]
- Mattanah JJF, Becker DF, Levy KN, Edell WS, McGlashan TH. Diagnostic stability in adolescents followed up 2 years after hospitalization. American Journal of Psychiatry. 1995;152:889–894. doi: 10.1176/ajp.152.6.889. [DOI] [PubMed] [Google Scholar]
- Mehlum L, Friss S, Vaglum P, Karterud S. The longitudinal pattern of suicidal behavior in borderline personality disorder: A prospective follow-up study. Acta Psychiatrica Scandinavica. 1994;90:124–130. doi: 10.1111/j.1600-0447.1994.tb01567.x. [DOI] [PubMed] [Google Scholar]
- Meijer M, Goedhart AW, Treffers PDA. The persistence of borderline personality disorder in adolescence. Journal of Personality Disorders. 1998;12:13–22. doi: 10.1521/pedi.1998.12.1.13. [DOI] [PubMed] [Google Scholar]
- Miller AL, Muehlenkamp JJ, Jacobson CM. Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clinical Psychology Review. 2008;28:969–981. doi: 10.1016/j.cpr.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Netta H, Orbach I, Gothelf D, Efrati M, Apter A. Comparison of the suicidal behavior of adolescent inpatients with borderline personality disorder and major depression. Journal of Nervous and Mental Disease. 2003;191:582–588. doi: 10.1097/01.nmd.0000087184.56009.61. [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angemeyer M, Beautrais A, Bruffaerts R, Chiu WT, de Girolamo G, Gluzman S, de Graaf R, Gureje O, Haro JM, Huang Y, Karam E, Kessler RC, Lepine JP, Levinson D, Medina-Mora ME, Ono Y, Posada-Villa J, Williams D. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. British Journal of Psychiatry. 2008;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15:868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paris J. Chronic suicidality among patients with borderline personality disorder. Psychiatric Services. 2002;53:738–742. doi: 10.1176/appi.ps.53.6.738. [DOI] [PubMed] [Google Scholar]
- Paris J. Is hospitalization useful for suicidal patients with borderline personality disorder? Journal of Personality Disorders. 2004;18:240–247. doi: 10.1521/pedi.18.3.240.35443. [DOI] [PubMed] [Google Scholar]
- Selby EA, Joiner TE., Jr Cascades of emotion: The emergence of borderline personality disorder from emotional and behavioral dysregulation. Review of General Psychology. 2009;13:219–229. doi: 10.1037/a0015687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Joiner TE., Jr Emotional cascades as prospective predictors of dysregulated behaviors in borderline personality disorder. Personality Disorders: Theory, Research, & Treatment. 2013;4:168–174. doi: 10.1037/a0029933. [DOI] [PubMed] [Google Scholar]
- Selby EA, Yen S, Spirito A. Time varying prediction of suicidal ideation in adolescents: Weekly ratings over six month follow-up. Journal of Clinical Child and Adolescent Psychology. 2013;42:481–495. doi: 10.1080/15374416.2012.736356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro T. Debate forum – resolved: Borderline personality disorder exists in children under twelve. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:478–483. [PubMed] [Google Scholar]
- Shea MT, Stout R, Gunderson J, Morey LC, Grilo CM, McGlashan T, Skodol AE, Dolan-Swewell R, Dyck I, Zanarini MC, Keller MB. Short-term diagnostic stability of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. American Journal of Psychiatry. 2002;159:2036–2041. doi: 10.1176/appi.ajp.159.12.2036. [DOI] [PubMed] [Google Scholar]
- Spirito A, Valeri S, Boergers J, Donaldson D. Predictors of continued suicidal behavior in adolescents following a suicide attempt. Journal of Clinical Child and Adolescent Psychology. 2003;32:284–289. doi: 10.1207/S15374424JCCP3202_14. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term monitoring program using the longitudinal interval follow-up evaluation. Journal of Psychiatric Research. 2001;35:297–305. doi: 10.1016/s0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. Journal of Psychiatric Research. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Westen D, Betan E, Defife JA. Identity disturbance in adolescence: Associations with borderline personality disorder. Development and Psychopathology. 2011;23:305–313. doi: 10.1017/S0954579410000817. [DOI] [PubMed] [Google Scholar]
- Winograd G, Cohen P, Chen H. Adolescent borderline symptoms in the community: Prognosis for functioning over 20 years. Journal of Child Psychology and Psychiatry. 2008;49:933–941. doi: 10.1111/j.1469-7610.2008.01930.x. [DOI] [PubMed] [Google Scholar]
- Witte TK, Fitzpatrick KK, Joiner TE, Jr, Schmidt NB. Variability in suicidal ideation: A better predictor of suicide attempts than intensity or duration of ideation? Journal of Affective Disorders. 2005;88:131–136. doi: 10.1016/j.jad.2005.05.019. [DOI] [PubMed] [Google Scholar]
- Witte TK, Fitzpatrick KK, Warren KL, Schatschneider C, Schmidt NB. Naturalistic evaluation of suicidal ideation: Variability and relation to attempt status. Behaviour Research and Therapy. 2006;44:1029–1040. doi: 10.1016/j.brat.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Yen S. Outpatient treatment in adolescents with borderline personality disorder following hospitalization for elevated suicide risk. 2013. Manuscript in Preparation. [Google Scholar]
- Yen S, Weinstock L, Andover M, Sheets E, Selby EA, Spirito A. Prospective predictors of adolescent suicidality: Six month post-hospitalization follow-up. Psychological Medicine. 2013;43:983–993. doi: 10.1017/S0033291712001912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, McGlashan TH, Zanarini MC, Morey LC. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. American Journal of Psychiatry. 2004;161:1296–1298. doi: 10.1176/appi.ajp.161.7.1296. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Chauncey DL, Gunderson JG. The diagnostic interview for personality disorders: Interrater and test-retest reliability. Comprehensive Psychiatry. 1987;28:467–480. doi: 10.1016/0010-440x(87)90012-5. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorder. Belmont, MA: McLean Hospital, Laboratory for the Study of Adult Development; 1996. [Google Scholar]
- Zanarini MC, Frankenburg FR, Vujanovic AA, Hennen J, Reich DB, Silk KR. Axis II comorbidity of borderline personality disorder: Description of 6-year course and prediction to time-to-remission. Acta Psychiatrica Scandinavica. 2004;110:416–420. doi: 10.1111/j.1600-0447.2004.00362.x. [DOI] [PubMed] [Google Scholar]


