Abstract
Objective
To evaluate the initial safety and effectiveness of the Intrauterine Ball, a copper intrauterine device which upon insertion in the uterus takes a three dimensional spherical form.
Study Design
Fifteen women were followed for one year, with follow-up visits at 1, 3, 6, 9, and 12 months.
Results
The physician reported that all devices were very easy to insert. One subject discontinued before the 6 month visit (at 119 days post insertion) for a reason not related to the device. There were no perforations, expulsions, mal-positions or complications, or pregnancies.
Conclusion
No safety or efficacy concerns were raised.
Implications
Due to its form and deployment process the IUB™ is expected to ease insertion and reduce perforation, malposition and expulsion rates and may also reduce dysmenorrhea and menorrhagia.
Keywords: safety, efficacy, discontinuation, expulsion, ease of insertion, satisfaction
Introduction
The field of LARC in general and IUDs in particular has seen few innovations in the last few decades. Most IUDs manufactured to date are T shaped or a version of T shape and only a few are different (thread, rings, and others), however when deployed in the uterus they all take a 2 dimensional shape. We report here on a new IUD, the IUB (Intrauterine Ball).
The SCu300A IUB™ (hereafter “IUB™”) is a copper intrauterine device which upon insertion in the uterus takes a three dimensional spherical form. The IUB™ is deployed and removed in the same manner as standard IUDs and is expected to have the same efficacy. Due to its form and deployment process the IUB™ is expected to reduce perforation, malposition and expulsion rates and may also reduce dysmenorrhea and menorrhagia.
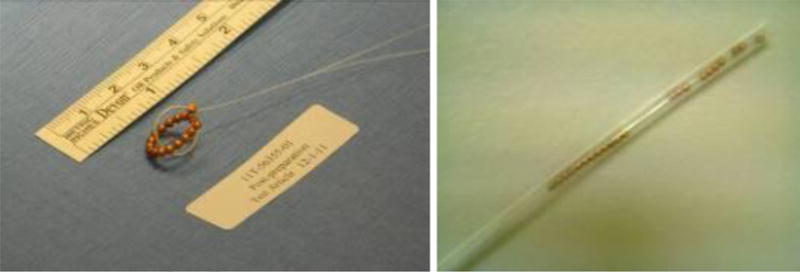
The IUB™ is a single use IUD and is supplied sterile, pre-loaded into a simple tube (outer diameter = 3.2mm) and rod insertion kit. The IUB™ is made of a shape memory alloy wire, a material with superior elastic characteristics which tolerates flexion well while always returning to its preset shape. The wire is covered with a thin white polymer coating, applied mostly to improve visibility. 17 pure copper spheres are threaded over the wire (see Figures 1 and 2 below). The distal sphere is attached at one end to reduce sharpness and the proximal sphere is attached together with the thread. The total copper surface area is 300mm2 (a version of 380 also exists). A 20cm long double-tailed uncolored nylon monofilament thread is attached for removal. Once deployed, the IUB™ is approximately 12mm in diameter; however, it is likely to accommodate its shape to the uterine cavity. The IUB™ is intended to have a lifetime of five years.
Figure 1. The IUB™.

Figure 2. The IUB™ in its free form (Left), and loaded into the insertion tube (right).
The IUB™ offers the following advantages attributable to its unique three-dimensional ball-like structure:
During insertion, the tip of the IUB turns 180 degrees as it exits the insertion tube, away from the uterine fundus, thus reducing the risk of fundal perforation during insertion. This attribute simplifies the process for operators with less experience in IUD insertion who are more prone to uterine perforation.1
The diameter of the IUB (12±2mm) is ∼14-25% smaller than each arm of current T-shaped lUDs. The smaller size is expected to reduce irritation to the uterine wall while being large enough not to clear the cervix internal os, thus nullifying the probability of expulsion.
The IUB lacks sharp edges thus possibly preventing uterine wall irritation and distortion.
Mal-positioning within the uterine cavity is prevented through the spherical shape of the IUB.
Materials and Methods
Fifteen women were recruited to assess the initial safety and efficacy of the IUB. Subjects were required to be married (or in a steady relationship) healthy women aged 25-42 with blood hemoglobin >11.5gr%. Women were followed for one year, with follow-up visits at 1, 3, 6, 9, and 12 months. Women rated satisfaction with the IUB™ device and change in menstrual bleeding level compared with before insertion and the physician rated ease of insertion on a 5-point Likert scale. Abdominal discomfort, lower abdominal pain, change in bleeding pattern, and cramping were binary responses. All devices were inserted by the same provider; the lead author supervised the PI for the first patient.
The upper limits of the exact binomial one-sided 95% confidence intervals for proportions were computed in JavaStat (http://statpages.org/confint.html). The study was approved by the Hungarian Scientific and Medical Research Council Ethics Committee.
Results
Women participating in the study were between 25 and 41 years old (mean=33.9), on average they had 2 children (only 1 was nilliparous), 60% were married, and 47% had not used contraception in the past. All wanted to prevent pregnancy and agreed to use no other contraceptive. The device was inserted within between 12 and 25 minutes (from entering to exiting the room). The physician reported that all 15 devices were very easy to insert (100%, with lower one-sided 95% exact binomial CL: 81.9%).
One subject discontinued the study before the 6 month visit (at 119 days post insertion) for a reason not related to the device (D&C performed for excessive bleeding; pathology result = simple endometrial hyperplasia). The 12-month discontinuation rate has an upper one-sided 95% confidence limit of 28%. There were no perforations, expulsions, mal-positions or complications, or pregnancies; therefore these rates are 0%. The upper limits of the one-sided 95% confidence intervals are all 18% (19% for the 14 women observed for a year).
3 women reported abdominal discomfort after 1 month, and again after 1 year, but there were no reports of this discomfort at 3m, 6m, or 9m. Lower abdominal pain was reported at 1 month by 1 woman and by 2 women at 3 months and then again by 2 women at 12 months, with no reports of abdominal pain at the 6 and 9 months visits. 10 women claim they had a change in their bleeding pattern one month after IUB insertion, this percentage varied across the visit with finally 43% of the women reporting changes in bleeding pattern after 1 year. Mean menstrual bleeding level fell steadily from month 1 through month 9, followed by a rise at month 12 (which was lower than month 1). In addition, altogether 3 women reported having cramps one year after IUB insertion. With regard to patient satisfaction, 12 women reported a score of very satisfied, 1 woman as staisfied and another as moderately satisfied.
Discussion
A prospective, randomized, single blind study of the safety and efficacy of the IUB™ spherical copper intrauterine ball (220 women) in comparison to the TCu 380 intra-uterine device IUD (110 women) is now underway in Romania and Bulgaria. Both objective outcomes (pregnancy, perforation, expulsion and malposition rates, changes in endometrial thickness, rates of complications such as infection and anemia and discontinuation rates after 1 year) and subjective outcomes (pain during insertion, menstrual characteristics and pain, bleeding in correlation to the bleeding pattern prior to insertion) will be compared.
Acknowledgments
This work was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant for Infrastructure for Population Research at Princeton University, Grant R24HD047879 (JT). Ilan Baram, MD is Chief Medical Officer and Ariel Weinstein is CEO at OCON Medical, which owns the IUB. Address reprint requests to Ilan Baram (ilan@oconmed.com).
Funding: This work was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant for Infrastructure for Population Research at Princeton University, Grant R24HD047879 (JT). Funding for the clinical study was provided by OCON Medical, where IB is chief Medical Officer and AW is CEO.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ilan Baram, Ariel Weinstein, OCON Medical, 15 The Central Avenue, Ligad Center 1, POBox 552, Modiin 7171801, Israel.
James Trussell, Office of Population Research, Princeton University, Princeton, NJ 08544, The Hull York Medical School, Hull, England HU6 7RX.
References
- 1.Harrison-Woolrych M, Ashton J, Coulter D. Uterine perforation on intrauterine device insertion: is the incidence higher than previously reported? Contraception. 2003;67:53–6. doi: 10.1016/s0010-7824(02)00417-1. [DOI] [PubMed] [Google Scholar]


