Abstract
Small pericardial effusion (PE) is not an infrequent manifestation in primary hypothyroidism. But massive PE with or without cardiac tamponade is rare and often associated with severe form of the disease. Here we report an eight-year-old boy who was admitted with massive PE that required repeated pericardiocentesis. Detailed examinations failed to identify the etiology initially. Five months later, child was readmitted with massive PE with impending cardiac tamponade. Primary hypothyroidism was diagnosed based on the clinical and laboratory finding and was thought to be the underlying etiology of previously encountered undiagnosed massive PE. Beside pericardiocentesis, child was treated with thyroid hormone replacement. Condition gradually improved without further recurrence of PE till date. Therefore, irrespective of the presence of clinical signs, primary hypothyroidism should be suspected in every patient presenting with massive PE to prevent recurrence as well as its serious complications like cardiac tamponade.
Keywords: Pericardial effusion, Primary hypothyroidism, Cardiac tamponade, Levo-thyroxine
1. Introduction
Hypothyroidism is a common endocrinal disorder with multi-organ involvement including cardiovascular system. The occurrence of pericardial effusion (PE) in hypothyroidism is related to the severity and duration of the disease. Although small PE is a frequent occurrence but moderate to massive PE with or without tamponade is rare and often associated with severe form of the disease or myxedema.1,2 Here, we report an eight-year-old boy who was admitted initially with massive PE but detailed examinations failed to discover the exact etiology. A diagnosis of primary hypothyroidism was made based on clinical and laboratory finding later on when he was readmitted with massive PE with impending cardiac tamponade.
2. Case history
An eight-year-old boy presented to our emergency department in June, 2011 with complains of intermittent fever for last seven days associated with cough, breathlessness, and chest pain. There was no important family, traumatic or surgical history. His psychomotor development was normal. On physical examination, he was conscious but irritable, febrile (temperature: 39 °C) having tachypnea (respiratory rate: 32/min), tachycardia (heart rate: 108/min), narrow pulses, blood pressure: 108/80 mmHg, and raised jugular venous pressure. The cardiovascular examination revealed poorly localized cardiac apex, distant, muffled heart sounds and absence of murmur. He had normal facies and skin. Examination of other systems including ankle jerks was normal.
Chest X-ray showed marked cardiomegaly with normal lung field. Urgent echocardiogram was arranged that revealed large PE without tamponade (Fig. 1). Sub-xiphoid pericardiocentesis was performed and 250 ml of sero-sanguinous fluid was aspirated. Initial blood investigations like complete hemogram, serum electrolytes, renal and liver function test were within normal limit except serum albumin which was 2.7 g/dl (range: 3.5–5 g/dl). Blood and urine culture were negative. Examination of sputum and Mantoux test were negative. Cytological, microbiological and biochemical examination of the aspirated fluid were inconclusive other than increased protein content (5 g/dl) and a predominance of mononuclear cells in the differential count. Smear examination of pericardial fluid by Gram stain and Ziehl–Neelsen stain failed to demonstrate the presence of bacteria or tubercle bacilli. Cultures of the pericardial fluid were negative for both bacteria as well as Mycobacterium tuberculosis and the activity of adenosine deaminase (ADA) was not elevated.
Fig. 1.
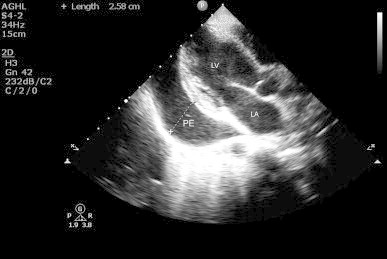
Transthoracic echocardiogram: parasternal long axis view showing massive pericardial effusion.
Following an initial improvement of several days' duration, symptoms recurred. Repeat echocardiography revealed moderate collection of serous clear pericardial fluid. Child was subjected for further investigations. Serology for selected viral pathogens like human immunodeficiency virus, Epstein–Barr virus, cytomegalovirus and herpes virus were all negative. Serologic markers for autoimmune diseases and streptococcal infection were negative. Considering exudative nature of the pericardial fluid and definite positive history of contact to tuberculosis, tubercular pericarditis was suspected and anti-tubercular drugs and oral prednisolone were added empirically. General condition of the patient became improved within few days following initiation of anti-tubercular therapy. The patient was discharged home with the advice to attend follow-up clinic.
Following four months of anti-tubercular treatment, in the beginning of November 2011, symptoms recurred and got hospitalized. Urgent chest X-ray showed cardiomegaly and echocardiogram revealed massive PE with impending cardiac tamponade (Fig. 2). Evidence of constrictive pericarditis was detected neither on echocardiographic finding nor in chest computed tomography scan. Patients became hemodynamically stable following aspiration of 350 ml of straw color fluid but developed unexplained bradycardia (pulse rate: 52/min). General examination revealed mild puffiness of face and non-pitting pedal edema. His deep tendon reflexes showed delayed relaxation. Analysis of pericardial fluid again was inclusive other than exudative character due to high protein content (6 g/dl).
Fig. 2.
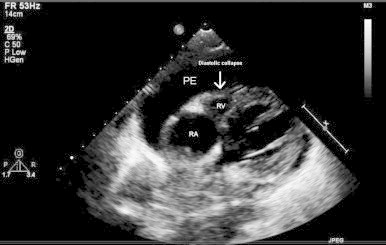
Transthoracic echocardiogram: subcostal view showing massive pericardial effusion with diastolic collapse of right ventricle (arrow) suggestive of impending cardiac tamponade.
Considering recurrent PE and clinical features, thyroid function was ordered. The result showed low free thyroxine (FT4): 0.28 ng/dl [range: 0.9–2.6 ng/dl], free tri-iodothyronine (FT3): 180 pg/dl [range: 240–560 pg/dl] and thyroid stimulating hormone (TSH): 22.51 mIU/l [range: 1.7–9.1 mIU/l]. Ultrasound of thyroid gland was performed showing normally located gland. Both anti-thyroid peroxidase antibodies and anti-thyroglobulin antibody test results were negative. Child was diagnosed as primary hypothyroidism and levo-thyroxine replacement therapy was started at a dose of 5 μg/kg/day. On follow-up visit at six week, repeat thyroid function showed FT4: 2.3 ng/dl and TSH: 3.5 mIU/l. Follow-up echocardiography revealed minimal PE. Till date, child is on levo-thyroxine replacement, maintaining euthyroid state without further recurrence of PE. It was concluded that primary hypothyroidism was the etiology of initial massive PE which was not suspected due to absence of common clinical findings.
3. Discussion
Cardiovascular manifestations in hypothyroidism include dyspnea and decreased exercise tolerance. Bradycardia, diastolic hypertension, muffled heart sounds, cardiomegaly, and non-pitting or pitting peripheral edema may be revealed on physical examination.1,2 Accumulation of transudate, exudate or blood in the pericardial sac is a common complication of pericardial heart disease which results from several conditions; hypothyroidism is one of them.3 The reported incidence PE varies from 3% in early mild stage to 80% when the disease becomes advanced.4 Small PE is frequently found in patients with hypothyroidism whereas moderate to large PE is relatively rare. Massive PE with tamponade as an initial clinical presentation of primary hypothyroidism was reported in a few English literature.5–10 This low incidence is probably due to the pericardial distensibility and the slow accumulation of fluid, allowing significant fluid accumulation without hemodynamic compromise. Though heart failure is unusual in hypothyroidism, but should be distinguished from tamponade because of similar presentations.10
Tuberculous pericarditis should be considered as an important etiology in the evaluation of all cases of pericarditis without a rapidly self-limiting course. Its presentation may vary as purulent pericardial effusion with predominance of polymorphonuclear leukocytes and relatively abundant mycobacterial; sero-sanguinous effusion with predominantly lymphocytic exudates; absorption of effusion with pericardial thickening and ultimately fibrosis and constrictive pericarditis. Definite tubercular pericarditis can be diagnosed by one or more of the following criteria: (a) Isolation of M. tuberculosis from pericardial fluid or pericardial biopsy; (b) Demonstration of granulomatous inflammation on histological examination of pericardial biopsy; (c) Isolation of M. tuberculosis from sputum or non pericardial effusion exudates in the presence of clinical and/or radiological evidence of tuberculosis, associated with positive response to antitubercular therapy (ATT) and in the absence of any other obvious cause of pericarditis.11 In the present case we could isolate M. tuberculosis neither from smear examination nor from culture of the pericardial fluid. Pericardial biopsy was not performed. ADA activity was also not elevated. Antitubercular therapy along with oral prednisolone was started empirically and the child showed initial improvement. But the condition recurred within four months and the child got re-hospitalized. This transient improvement could be due to the anti-inflammatory effect of oral prednisolone and the condition started to relapse when the steroid have been tapered.
PE in hypothyroidism is considered to be a part of the generalized polyserousopathy and the accepted pathogenic mechanism being a combination of extravasation of albumin and inadequate lymphatic drainage, accounts for the exudative nature of the accumulated fluid in this disorder. The pericardial fluid in hypothyroidism is characteristically straw color due to high content of alpha and beta globulins with predominance of lymphocytes.8 In our case, the fluid obtained in initial pericardiocentesis was sero-sanguinous with predominantly lymphocytic exudates and we consider trauma as a possible cause, but in second aspiration it was serous in nature.
Treatment of hypothyroidism is always mandatory following pericardiocentesis. There is generally a residue of effusion, which disappears following appropriate therapy over a period varying between one month and one year and for this reason treatment with increasing doses of Levo-thyroxine is necessary. Thyroid replacement therapy is necessary over a long period of time and requires close follow-up.1,2,8
Key messages
Though it's unusual that primary hypothyroidism presents with massive PE before its common clinical features become overt, but it can happen. Therefore, physicians should consider primary hypothyroidism as differential diagnosis in patients with massive PE which may prevent its recurrence as well as serious complications.
Conflicts of interest
All authors have none to declare.
References
- 1.Wiersinga W.M. Hypothyroidism and myxedema coma. In: De Groot L.J., Jameson J.L., editors. Endocrinology Adult and Pediatric. 6th ed. Saunders; Philadelphia: 2010. pp. 1607–1622. [Google Scholar]
- 2.Larsen P.R., Davies T.F. Hypothyroidism and thyroiditis. In: Larsen P.R., Kronenberg H.M., Melmed S., Polonsky K.S., editors. Williams Textbook of Endocrinology. 10th ed. Saunders; Philadelphia, Pennsylvania: 2003. pp. 423–455. [Google Scholar]
- 3.Hoit B.D. Pericardial disease. In: Faster V., Walsh R.A., O'Rourke R.A., Poole-Wilson P., editors. Hurst's the Heart. 12th ed. McGraw-Hill Companies, Inc.; China: 2008. pp. 1951–1974. [Google Scholar]
- 4.Kabadi U.M., Kumar S.P. Pericardial effusion in primary hypothyroidism. Am Heart J. 1990;120:1393–1395. doi: 10.1016/0002-8703(90)90253-t. [DOI] [PubMed] [Google Scholar]
- 5.Delgado Hurtado J.J., Guevara W., Ramos E., Lorenzana C., Soto S. Hypothyroidism in a five-year-old boy with rhabdomyolysis and recent history of cardiac tamponade: a case report. J Med Case Rep. 2011;5:515. doi: 10.1186/1752-1947-5-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patil V.C., Patil H.V., Agrawal V., Patil S. Cardiac tamponade in a patient with primary hypothyroidism. Indian J Endocrinol Metab. 2011;15:S144–S146. doi: 10.4103/2230-8210.83358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lim A.S., Paz-Pacheco E., Reyes M., Punzalan F. Pericardial decompression syndrome in a patient with hypothyroidism presenting as massive pericardial effusion: a case report and review of related literature. BMJ Case Rep. 2011 Oct 4 doi: 10.1136/bcr.04.2011.4117. pii: bcr0420114117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shastry R.M., Shastry C.C. Primary hypothyroidism with pericardial tamponade. Indian J Pediatr. 2007;74:580–581. doi: 10.1007/s12098-007-0097-8. [DOI] [PubMed] [Google Scholar]
- 9.Karu A.K., Khalife W.I., Houser R., VanderWoude J. Impending cardiac tamponade as a primary presentation of hypothyroidism: case report and review of literature. Endocr Pract. 2005;1:265–271. doi: 10.4158/EP.11.4.265. [DOI] [PubMed] [Google Scholar]
- 10.Rachid A., Caum L.C., Trentini A.P., Fischer C.A., Antonelli D.A., Hagemann R.P. Pericardial effusion with cardiac tamponade as a form of presentation of primary hypothyroidism. Arq Bras Cardiol. 2002;78:580–585. doi: 10.1590/s0066-782x2002000600005. [DOI] [PubMed] [Google Scholar]
- 11.Mayosi B.M., Burgess L.J., Doubell A.F. Tuberculous pericarditis. Circulation. 2005;112:3608–3616. doi: 10.1161/CIRCULATIONAHA.105.543066. [DOI] [PubMed] [Google Scholar]


