Abstract
Diurnal variations in central corneal thickness (CCT) and intraocular pressure (IOP) and their relationships were studied in healthy dogs. Central corneal thickness was measured by ultrasonic pachymetry and IOP by applanation tonometry in 16 beagle dogs. Measurements were taken every 90 min over 12 h (08:00 am to 08:00 pm). The mean CCT and IOP values obtained during the sampling period were 545.6 ± 21.7 μm (range: 471 to 595 μm) and 15 ± 2.2 mmHg (range: 10 to 19 mmHg), respectively. The CCT and IOP showed statistically significant decreases at 6:30 pm and 5:00 pm, respectively (P < 0.001). Central corneal thickness and IOP values were lower in the afternoon/evening than in the morning and were positively correlated. Both findings are important for the diagnostic interpretation of IOP values in dogs.
Résumé
Variations diurnes de l’épaisseur de la cornée centrale et de la pression intraoculaire chez les chiens, de 8 heures à 20 heures. Les variations quotidiennes de l’épaisseur de la cornée centrale (ECC) par pachymétrie ultrasonore, ainsi que la pression intraoculaire (PIO) obtenue par tonométrie à aplanissement, ont été étudiées chez seize chiens beagle en bonne santé. La relation entre ces deux paramètres a aussi été évaluée. Les mesures ont été effectuées toutes les 90 minutes durant douze heures (08:00 am à 08:00 pm). Les valeurs moyennes de ECC et PIO obtenues durant la période de l’expérience ont été respectivement de 545,6 ± 21,7 μm (valeurs extrêmes de 471 à 595 μm) et de 15 ± 2,2 mmHg (valeurs extrêmes de 10 à 19 mmHg). La mesure de l’épaisseur cornéenne ainsi que la pression intraoculaire ont montré statistiquement une baisse significative après 6:30 pm et 05:00 pm (P < 0,001) respectivement. Les valeurs de l’ECC et de la PIO étaient plus basses l’après-midi que le matin, avec une corrélation positive entre les deux.
(Traduit par les auteurs)
Introduction
Measurement of central corneal thickness (CCT) has become more common in ophthalmic practice. An accurate determination of intraocular pressure (IOP) may need to be modified according to CCT to avoid pressure overestimation or underestimation which is important in the clinical evaluation of glaucoma (1–3). This relationship between CCT and IOP has been demonstrated in several studies in human ophthalmology (4–6). Recently a correlation was made between CCT readings and IOP values obtained by rebound and applanation tonometry in normal dogs suggesting that CCT is a factor to be considered in IOP measurements in this species (7).
The CCT is measured in vivo by means of corneal pachymetry, using optical, digital, or ultrasonic means, the latter being the most commonly used method for determining CCT in animals and humans (8–9). In dogs CCT varies from 377 μm to 657 μm (7,8,10–12) with a mean value around 550 μm (7,8). Variability exists between individuals due to weight (8), breed (13), gender and age (7,8,10,12,13) as has been reported in humans (14). Diurnal changes in CCT values have been reported in numerous species including rabbits (15), cats (16), primates (17), and humans with thickest corneas after awakening (18).
Significant diurnal variations in IOP have also been observed in normal dogs (19–21), cats (22,23), and rabbits (24–26) with highest values in the early morning and troughs occurring during the day. Correlation between diurnal variations of IOP and CCT has been shown in humans for the first 2 h after awakening (18) but the authors were unable to find data concerning CCT variation or IOP-CCT correlations through the day in dogs.
Based on IOP and CCT variations occurring during the day in humans, we hypothesized that these changes will also be observed in dogs. The aim of this study was to determine the fluctuation in CCT and IOP during the 12-hour period from 8.00 am to 8.00 pm and the relationship between CCT and IOP in healthy beagle dogs.
Materials and methods
Animals
The study population consisted of 16 beagle dogs (14 females and 2 males) aged between 1 and 4 y and with an average weight of 14 kg (range: 10 to 16 kg). Healthy animals, without previous systemic or ocular disease, were selected by means of general physical and ophthalmological examination; including biomicroscopy (SL-5; Kowa, Tokyo, Japan), tonometry (Tonopen XL; Mentor Ophthalmics, Santa Barbara, California, USA), direct ophthalmoscopy (Beta 200; Heine, Herrsching, Germany) and indirect ophthalmoscopy (Omega 180; Heine). This study was in accord with European legislation (86/609/EU) and the experimental protocol was approved by the Ethics and Animal Welfare Committee of the University of Córdoba, Córdoba, Spain.
Experimental procedure
Diurnal measurements of pachymetry (PachPen; Accutome, Malvern, Pennsylvania, USA) and tonometry (Tonopen XL; Medtronic, Minneapolis, Minnesota, USA) were taken in the left eye of the 16 dogs. Measurements were taken every 90 min during the 12-hour period 8:00 am to 8:00 pm.
The dogs were placed on the examination table and held by an assistant to reduce stress, taking care not to put pressure on soft periocular structures or the neck. Pachymetry was performed 1 min after applying topical anesthesia (Prescaine 0.2%; Llorens Laboratory, Barcelona, Spain). The CCT was the average of 9 successive measurements with standard deviations below 5% taken at a single point on the cornea situated in the center of the pupil. The IOP was measured 2 min after measuring corneal thickness. The IOP was calculated as the average of 3 successive values with standard deviations < 5% measured in the center of the cornea. After IOP and CCT measurements, corneal integrity was determined by slit lamp biomicroscopy and staining with fluorescein and rose Bengal (Rosix; Dioptrix, Toulouse, France).
The sleeping pattern of these dogs was monitored and all the dogs were kept awake during the sampling period. The dogs rested in a dark environment from 10 pm to 7:30 am, when the lights were switched off and on, respectively. The dogs spent the daytime in a sunlit room and were taken for a 20-minute walk 3 times/day. During the day, someone was present to ensure that none of the animals went to sleep.
The percentage of diurnal variation (% DV) in CCT was estimated using the difference between the maximum and minimum readings measured in 1 day (from 8:00 am to 8:00 pm) as described by Harper et al (27).
Statistical analysis
A descriptive analysis was performed for all the variables. The IOP and CCT values were analyzed using an analysis of variance (ANOVA) for repeated measurements. Post-hoc tests that were used were Tukey’s test and Bonferroni’s test (13). Pearson correlation test was applied to find the relationship between corneal thickness and intraocular pressure at P ≤ 0.05.
Results
Central corneal thickness
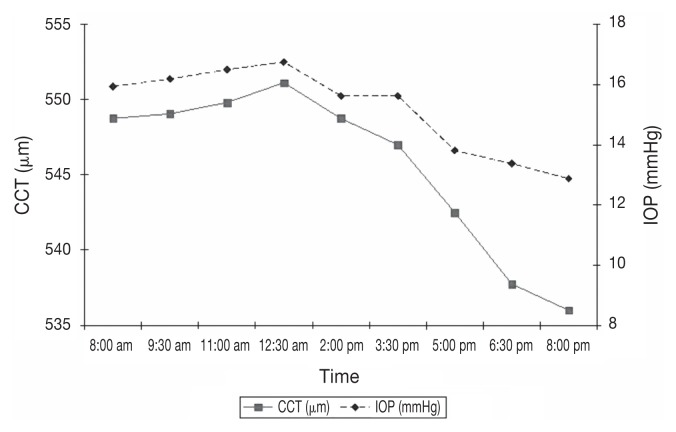
Mean CCT and standard deviation (± SD) obtained during the sampling period was 545.6 ± 21.7 μm (range: 471 to 595 μm) (Table 1). There were no significant differences between readings from 8.00 am to 5.00 pm but the readings taken at 6.30 and 8.00 pm were significantly lower (P < 0.001) than the readings at 8.00 am (Table 1; Figure 1). Mean and standard deviation (± SD) of the % DV in CCT was 7.5 ± 4.5%. There were individual changes in CCT, with diurnal variations ranging between 2.7% and 18.7% during the 12-hour sampling period (Table 2). The percentage DV ranged from 2.7% to 5.3% in 8 dogs, from 7.2% to 8.7% in 4 dogs and above 10% in the 4 others (Table 2).
Table 1.
Mean central corneal thickness (CCT) and mean intraocular pressure (IOP) readings in 16 beagle dogs measured at intervals from 8.00 am to 8.00 pm
| CCT (μm) | IOP (mmHg) | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Time | Mean ± SD | Minimum | Maximum | Mean ± SD | Minimum | Maximum |
| 8:00 am | 549 ± 24.1a | 514 | 595 | 16 ± 2.1a | 12 | 19 |
| 9:30 am | 549 ± 22.2a | 514 | 590 | 16 ± 2.0a | 12 | 19 |
| 11:00 am | 550 ± 21.2a | 519 | 590 | 17 ± 1.9a | 12 | 19 |
| 12:30 pm | 551 ± 19.6a | 516 | 586 | 17 ± 1.9a | 13 | 19 |
| 02:00 pm | 549 ± 20.4a | 514 | 589 | 16 ± 1.6a | 13 | 18 |
| 03:30 pm | 547 ± 19.9a | 499 | 577 | 16 ± 2.0a | 12 | 18 |
| 05:00 pm | 543 ± 19.8a | 485 | 565 | 14 ± 1.6b | 11 | 17 |
| 06:30 pm | 538 ± 26.3b | 471 | 574 | 13 ± 1.8b | 10 | 17 |
| 08:00 pm | 536 ± 20.1b | 494 | 568 | 13 ± 1.6b | 11 | 16 |
| Period | 545.6 ± 21.7 | 471 | 595 | 15.2 ± 2.2 | 10 | 19 |
Values with different letters are statistically significant values (P < 0.001).
SD — standard deviation.
Figure 1.
Mean ± SD diurnal central corneal thickness (CCT, μm) and intraocular pressure (IOP, mmHg) in the sampling period between 8:00 am and 8:00 pm.
Table 2.
Diurnial variations in central corneal thickness (CCT) and in intraocular pressure (IOP) in 16 beagle dogs
| CCT (μm) | IOP (mmHg) | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Dog | % SD | Minimum | Maximum | % SD | Minimum | Maximum |
| 1 | 3.7 | 534 | 554 | 50.0 | 12 | 18 |
| 2 | 5.3 | 527 | 555 | 72.7 | 11 | 19 |
| 3 | 3.1 | 540 | 557 | 60.0 | 10 | 16 |
| 4 | 3.7 | 538 | 558 | 54.5 | 11 | 17 |
| 5 | 7.2 | 515 | 552 | 35.7 | 14 | 19 |
| 6 | 7.6 | 511 | 550 | 72.7 | 11 | 19 |
| 7 | 4.9 | 531 | 557 | 38.5 | 13 | 18 |
| 8 | 4.7 | 530 | 555 | 35.7 | 14 | 19 |
| 9 | 3.3 | 549 | 567 | 38.5 | 13 | 18 |
| 10 | 2.7 | 551 | 566 | 28.6 | 14 | 18 |
| 11 | 11.9 | 505 | 565 | 38.5 | 13 | 18 |
| 12 | 18.7 | 471 | 559 | 50.0 | 12 | 18 |
| 13 | 8.7 | 515 | 560 | 36.4 | 11 | 15 |
| 14 | 15.1 | 485 | 558 | 45.5 | 11 | 16 |
| 15 | 8.6 | 548 | 595 | 35.7 | 14 | 19 |
| 16 | 10.6 | 536 | 593 | 72.7 | 11 | 19 |
| Mean | 7.5 | 524.1 | 562.6 | 47.9 | 12.2 | 17.9 |
| SD | 4.5 | 22.0 | 12.7 | 14.3 | 1.3 | 1.2 |
| Maximum | 18.7 | 551.0 | 595.0 | 72.7 | 14.0 | 19.0 |
| Minimum | 2.7 | 471.0 | 550.0 | 28.6 | 10.0 | 15.0 |
SD — standard deviation.
Intraocular pressure
Mean IOP (± SD) obtained during the sampling period was 15.2 ± 2.2 mmHg (range: 10 to 19 mmHg) (Table 1). There were no significant differences between readings from 8.00 am to 3.30 pm but the readings taken after 3.30 pm were significantly lower (P < 0.001) than the readings at 8.00 am (Table 1; Figure 1).
Mean (± SD) of the percentages of IOP diurnal variation was 47.9 ± 14.3%. High individual variations in IOP were observed, ranging between 28.6% and 72.7% during the 12-hour sampling period (Table 2). The DV was 28.6% in 1 dog, 35.7% to 38.5% in 7 dogs, 45.5% to 60% in 5 dogs, and 72.7% in 3 dogs (Table 2). Mean diurnal IOP and CCT measurements were moderately correlated in these dogs. (Pearson correlation coefficient r = 0.25, P = 0.002).
At the end of the study micropunctate fluorescein and rose Bengal staining of the cornea was done in all dogs with slight conjunctival hyperemia. Dogs were treated with preservative-free artificial tears (Oxyal; Laboratorios LLorens, Barcelona, Spain) and an antibiotic solution containing polymyxin B, neomycin, and gramicidin (Oftalmowell; UCB-pharma, Madrid, Spain). The cornea healed 3 d after treatment and all animals recovered fully.
Discussion
The CCT measurements using ultrasound pachymeter were easily obtained in all eyes studied. According to Harper et al (27), the fact that ultrasonic pachymetry necessarily involves contact with the surface of the corneal epithelium is a disadvantage compared with optical pachymetry. However, in veterinary medicine ultrasonic pachymetry has the advantages of portability, ease of use, and rapid measurements, and is well-tolerated by dogs without the need for sedation or general anesthesia.
Determination of CCT is essential for evaluating corneal rigidity and consequently represents an important factor for IOP values measured by applanation tonometry (1,2). The CCT should be considered in IOP measurements in dogs (7). In this study the CCT range (471 to 595 μm), although within normal limits (7,8), was highly variable. Variability of CCT in dogs has been attributed to differences in breeds (13), age (8,11,13), weight (8), and gender (8,13). Significantly thicker corneas have been reported in Labrador retrievers than in a beagle/briard cross (13), and in males over female dogs (8,13). However Park et al (7) failed to find differences by gender in CCT measurements. There are not many studies that address factors influencing CCT in dogs. In human ophthalmology racial differences have been widely studied, reporting CCT differences in some ethnics groups (14,28). Older age has also been associated with thinner central corneas than younger age (28). Most studies found no gender differences (14,29,30) on CCT; however, some studies reported a moderately significant association between gender and CCT (31,32).
Significant diurnal fluctuations in CCT occur in humans (18,33) and cats (16), with thick corneas after awakening, but have not previously been reported in dogs. In humans, the greater corneal thickness observed in the morning has been related to an increase in thickness during sleep, possibly due to the anaerobic metabolism which produces an osmotic gradient that attracts water in the corneal stroma (34). The CCT gradually decreased as the day progressed with the largest change in the first 3 h after awaking (18) and with a maximum decrease after 5 to 12 h (27,35). Variation may be observed between individuals, age, gender, physical activity, and environmental variables such as temperature and humidity (28,35). Despite different sleeping habits in humans and dogs, in both cases highest CCT values were observed in the morning. However in our study CCT fluctuation was not statistically significant between the first 5 measurements (from 8:00 am to 5:30 pm) and CCT progressively decreased to the last measurement at 8:00 pm. Most studies on human CCT variability considered only daytime fluctuations from 8:00 am to 8:00 pm or during waking hours (4,27,35). In 24-hour studies, Harper et al (27) and Kida et al (36) confirmed an increase in corneal thickness during sleep with a peak CCT occurring between 1:30 to 5:30 am. In cats, corneal thickness increased during periods of eye closure with a progressive decrease during periods of eye opening (16). Due to the irregular pattern of sleep of cats no diurnal or nocturnal CCT variations were observed, maintaining similar values over 24 h (16). A 24-hour study on IOP and CCT has not been reported in dogs. It would be required to provide information about the circadian fluctuations in CCT and IOP.
Mean diurnal percentage of variation (7.5%) on CCT observed in dogs of this study were comparable to those described in humans (7.2%) (27). Overall individual variability was low with 75% of dogs showing a percentage of variation less than 10%.
We have shown that significant variation occurs in IOP over a 12-hour period in healthy beagle dogs, similar to that described in humans (4,36) and dogs (19–21). IOP values were higher at the first hours in the morning, decreasing slowly during the day until 8:00 pm, which shows the same general trend as several of the previous studies in healthy beagles dogs (20,21) with the afternoon mean IOP values (5:00 pm) significantly lower than the morning means.
Mean diurnal IOP variation in this study (5.7 mmHg) was also consistent with previous studies in human ophthalmology (33). Differences between the minimum and maximum value can reach 8 mmHg as we found in 3 dogs (18.75%). It suggests that in some animals variations of IOP may be large and not recognized during clinic hours. Caution must be exercised when interpreting IOP values in terms of both diagnostics and treatment and related to the time of day when measurements must be performed because changes in IOP observed in the same patient at different clinical examinations may be due to the circadian rhythm rather than to a true change in the mean IOP (21).
Studies in humans have evaluated the diurnal correlation between CCT and IOP measurements with inconsistent results. Many of these reports found a significant positive correlation between IOP and CCT (4,18,37,38) as we have found in dogs but other investigators failed to find a temporal relationship between both (39). However, the individual IOP value is now proving to be more complex than allowing for CCT alone as tonometry is influenced by the material properties of the cornea of which CCT is but one component (40). Also it has been reported that the relation between IOP and CCT depends on the presence of corneal pathology as endothelial dystrophy. Corneal surgeries that either increase or decrease the corneal thickness represent a challenge for IOP measurement and establishment of a diagnosis of glaucoma (41).
In conclusion, IOP and CCT in beagle dogs show diurnal variations with higher values early in the morning than in the afternoon/evening and a significant correlation between both. CVJ
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Whiteacre MM, Stein RA, Hassanein K. The effect of corneal thickness on applanation tonometry. Am J Ophthalmol. 1993;115:592–596. doi: 10.1016/s0002-9394(14)71455-2. [DOI] [PubMed] [Google Scholar]
- 2.Benjumeda A, editor. Glaucomatología, para especialistas no especializados. 1st ed. Barcelona, Spain: Gráfiques Cusco; 2000. pp. 31–78. [Google Scholar]
- 3.Ko YC, Liu CJI, Hsu WM. Varying effects of corneal thickness on intraocular pressure measurements with different tonometers. Eye. 2005;19:327–332. doi: 10.1038/sj.eye.6701458. [DOI] [PubMed] [Google Scholar]
- 4.Kotecha A, Crabb DP, Spratt A, Garway-Heath DF. The relationship between diurnal variations in intraocular pressure measurements and central corneal thickness and corneal hysteresis. Inv Ophthalmol & Vis Sci. 2009;50:4229–4236. doi: 10.1167/iovs.08-2955. [DOI] [PubMed] [Google Scholar]
- 5.Burdová CM, Ferrová K, Filous A, Oskorypová K, Lezatková P, Sedlácková P. Correlation of intraocular pressure measured by applanation tonometry, noncontact tonometry and tonopen with central corneal thickness. Csek Slov Oftalmol. 2011;67:154–157. [PubMed] [Google Scholar]
- 6.Ito K, Tawara A, Kubota T, Harada Y. IOP measured by dynamic contour tonometry correlates with IOP measured by goldman applanation tonometry and non-contact tonometry in Japanese individuals. J Glaucoma. 2012;21:35–40. doi: 10.1097/IJG.0b013e31820275b4. [DOI] [PubMed] [Google Scholar]
- 7.Park YW, Jeong MB, Kim TH, et al. Effect of central corneal thickness on intraocular pressure with the rebound tonometer and the applanation tonometer in normal dogs. Vet Ophthalmol. 2011;14:169–173. doi: 10.1111/j.1463-5224.2010.00859.x. [DOI] [PubMed] [Google Scholar]
- 8.Gilger BC, Whitley RD, McLaughlin SA, Wright JC, Drane JW. Canine corneal thickness measured by ultrasonic pachymetry. Am J Vet Res. 1991;52:1570–1572. [PubMed] [Google Scholar]
- 9.Korah S, Thomas R, Muliyil J. Comparison of optical and ultrasound pachymetry. Indian J Ophthalmol. 2000;48:279–283. [PubMed] [Google Scholar]
- 10.Stapleton S, Peiffer RL., Jr Specular microscopic observations of the clinically normal canine corneal endothelium. Am J Vet Res. 1979;40:1803–1804. [PubMed] [Google Scholar]
- 11.Gwin RM, Lerner I, Warren JK, Gum G. Decrease in canine corneal endothelial cell density and increase in corneal thickness as functions of age. Invest Ophthalmol Vis Sci. 1982;22:267–271. [PubMed] [Google Scholar]
- 12.Ekesten B, Torrang I. Age-related changes in ocular distances in normal eyes of Samoyeds. Am J Vet Res. 1995;56:127–133. [PubMed] [Google Scholar]
- 13.Montiani-Ferreira F, Petersen-Jones S, Cassotis N, Ramsey DT, Gearhart P, Cardoso F. Early postnatal development of central corneal thickness in dogs. Vet Ophthalmol. 2003;6:19–22. doi: 10.1046/j.1463-5224.2003.00196.x. [DOI] [PubMed] [Google Scholar]
- 14.Aghaian E, Choe JE, Lin S, Stamper RL. Central corneal thickness of Caucasinas, Chinese, Hispanic, Filipinos, African Americans and Japanese in a glaucoma clinic. Ophthalmology. 2004;111:2211–2219. doi: 10.1016/j.ophtha.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 15.Kikkawa Y. Diurnal variation in corneal thickness. Exp Eye Res. 1973;15:1–9. doi: 10.1016/0014-4835(73)90183-8. [DOI] [PubMed] [Google Scholar]
- 16.Chang-Ling T, Efron N, Holden BA. Diurnal variation of corneal thickness in the cat. Inv Ophthalmol Vis Sci. 1985;26:102–105. [PubMed] [Google Scholar]
- 17.Madigan MC, Gillard-Crewtherm S, Kielym PM, et al. Corneal thickness changes following sleep and overnight contact lens wear in the primate (Macaca fascicularis) Curr Eye Res. 1987;6:809–815. doi: 10.3109/02713688709034848. [DOI] [PubMed] [Google Scholar]
- 18.Hamilton KE, Pye DC, Aggarwala S, Evian S, Khosla J, Perera R. Diurnal variation of central corneal thickness and goldman applanation tonometry estimates of intraocular pressure. J Glaucoma. 2007;16:29–35. doi: 10.1097/IJG.0b013e31802b350f. [DOI] [PubMed] [Google Scholar]
- 19.Gelatt KN, Gum GG, Barrie KP, et al. Diurnal variations in intra-ocular pressure in normotensive and glaucomatous Beagles. Glaucoma. 1981;3:21–24. [Google Scholar]
- 20.Giannetto C, Piccione G, Giudice E. Daytime profile of the intra-ocular pressure and tear production in normal dog. Vet Ophthalmol. 2009;12:302–205. doi: 10.1111/j.1463-5224.2009.00717.x. [DOI] [PubMed] [Google Scholar]
- 21.Piccione G, Giannetto C, Fazio F, Giudice E. Influence of different artificial lighting regimes on intraocular pressure circadian profile in the dog (Canis familiaris) Exp Anim. 2010;59:215–223. doi: 10.1538/expanim.59.215. [DOI] [PubMed] [Google Scholar]
- 22.Wilkie DA, Latimer CA. Effects of topical administration of 2.0% pilocarpine on intraocular pressure and pupil size in cats. Am J Vet Res. 1991;52:41–444. [PubMed] [Google Scholar]
- 23.Del Sole MJ, Sande PH, Bernades JM, Aba MA, Rosenstein RE. Circadian rhythm of intraocular pressure in cats. Vet Ophthalmol. 2007;10:155–161. doi: 10.1111/j.1463-5224.2007.00525.x. [DOI] [PubMed] [Google Scholar]
- 24.Katz RS, Henkind P, Weitzman ED. The circadian rhythm of the intraocular pressure in the New Zealand White rabbit. Inv Ophthalmol & Vis Sci. 1975;14:775–780. [PubMed] [Google Scholar]
- 25.McLaren JW, Brubaker RF, Fitzsimon JS. Continuous measurement of intraocular pressure in rabbits by telemetry. Inv Ophthalmol & Vis Sci. 1996;37:966–975. [PubMed] [Google Scholar]
- 26.Schnell CR, Debon C, Percicot CL. Measurement of intraocular pressure by telemetry in conscious, unrestrained rabbits. Inv Ophthalmol & Vis Sci. 1996;37:958–965. [PubMed] [Google Scholar]
- 27.Harper C, Boulton M, Bennett D, et al. Diurnal variations in human corneal thickness. Br J Ophthalmol. 1996;80:1068–1072. doi: 10.1136/bjo.80.12.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hahn S, Azen S, Ying-Lai M, Varma R Los Angeles Latino Eye Study Group. Central corneal thickness in Latinos. Invest Ophthalmol Vis Sci. 2003;44:1508–1512. doi: 10.1167/iovs.02-0641. [DOI] [PubMed] [Google Scholar]
- 29.Lifshitz T, Levy J, Rosen S, Belfair N, Levinger S. Central corneal thickness and its relationship to the patient’s origin. Eye. 2006;20:460–465. doi: 10.1038/sj.eye.6701911. [DOI] [PubMed] [Google Scholar]
- 30.Xu L, You QS, Wang YX, Jonas B. Associations between gender, ocular parameters and diseases: The Beijing eye study. Ophthalmic Res. 2011;45:197–203. doi: 10.1159/000321522. [DOI] [PubMed] [Google Scholar]
- 31.Altinok A, Sen E, Yazici A, Aksakal FN, Oncul H, Koklu G. Factors influencing central corneal thickness in a Turkish population. Curr Eye Res. 2007;32:413–419. doi: 10.1080/02713680701344361. [DOI] [PubMed] [Google Scholar]
- 32.Guttridge NM. Changes in ocular and visual variables during the menstrual cycle. Opthalmic Physiol Opt. 1994;14:38–48. doi: 10.1111/j.1475-1313.1994.tb00555.x. [DOI] [PubMed] [Google Scholar]
- 33.Chakraborty R, Read SA, Collins MJ. Diurnal variations in axial length, choroidal thickness, intraocular pressure, and ocular biometric. Inv Ophthalmol Vis Sci. 2011;52:5121–5129. doi: 10.1167/iovs.11-7364. [DOI] [PubMed] [Google Scholar]
- 34.Klyce SD. Stromal lactate accumulation can account for corneal oedema osmotically following epithelial hypoxia in the rabbit. J Physiol. 1981;321:49–64. doi: 10.1113/jphysiol.1981.sp013971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.du Toit R, Vega JA, Fonn D, Simpson T. Diurnal variation of corneal sensitivity and thickness. Cornea. 2003;22:205–209. doi: 10.1097/00003226-200304000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Kida T, Liu JHK, Weinreb RN. Effect of 24-hour corneal biomechanical changes on intraocular pressure measurement. Inv Ophthalmol Vis Sci. 2006;47:4422–4426. doi: 10.1167/iovs.06-0507. [DOI] [PubMed] [Google Scholar]
- 37.Barleon L, Hoffmann EM, Berres M, Pfeiffer N, Grus FH. Comparison of dynamic contour tonometry and Goldman applanation tonometry in glaucoma patients and healthy subjects. Am J Ophthalmol. 2006;14:583–590. doi: 10.1016/j.ajo.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 38.Realini T, Weinreb RN, Hobbs G. Contour tonometry in normal and glaucomatous eyes. J Glaucoma. 2009;18:119–123. doi: 10.1097/IJG.0b013e31817d23c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Villas-Boas FS, Morimoto L, Siqueira A, et al. Correlation between diurnal variation of intraocular pressure, ocular pulse and corneal structural properties. Arq Bras Oftalmol. 2009;72:296–301. doi: 10.1590/s0004-27492009000300004. [DOI] [PubMed] [Google Scholar]
- 40.Brandt JD, Gordon MO, Gao F, Beiser JA, Miller JP, Kass MA Ocular Hypertension Treatment Study Group. Adjusting intraocular pressure for central corneal thickness does not improve prediction models for primary open-angle glaucoma. Opthalmology. 2012;119:437–442. doi: 10.1016/j.ophtha.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al-Mahmood AM, Al-Swailem SA, Edward DP. Glaucoma and corneal transplant procedures. J Ophthalmol. 2012 doi: 10.1155/2012/576394. [DOI] [PMC free article] [PubMed] [Google Scholar]