Abstract
Rhabdomyosarcoma is a malignant tumor composed of neoplastic mesenchymal cells, with varying degrees of striated muscle cell differentiation. With most cases occurring in children younger than 10 years, it is remarkably rare in adults. Further in adults, the typical pediatric rhabdomyosarcoma variants (embryonal and alveolar sub-types) occur less frequently and exhibit predilection for viscera followed by the head and neck region. A rare case of embryonal rhabdomyosarcoma arising from the buccal mucosa in a 36-year old male patient is herewith reported. Recognition of the correct diagnosis and histological sub-type is of critical importance in the therapy of this disease, since the treatment is not uniform in the literature because of the rarity of this neoplasm in the adult population.
Keywords: Embryonal, myogenesis, oral, prognosis, rhabdomyosarcoma
INTRODUCTION
Rhabdomyosarcoma (RMS) is a malignant, soft tissue neoplasm consisting of cells derived from the primitive mesenchyme that exhibit a profound tendency to myogenesis.[1] While only 2-5% of all soft-tissue sarcomas are RMS in adults; this tumor represents approximately 60% of soft-tissue sarcomas in children.[2]
The most common sites include head and neck (35%), followed by the genitourinary tract (23%) and extremities (17%). The pre-dominant sites in the head and neck region excluding the orbit are nasopharynx, paranasal sinuses, middle ear and mastoid, and facial soft tissues. RMS of the oral cavity accounts for 10-12% of all head and neck RMS. The tongue, palate and cheek are the most common sites in the oral cavity.[3] These tumors form rapidly growing, soft swellings, which are non-descript in character.[4] Males are affected more commonly than females by a ratio of 1.3:1.0.[5]
There are three main sub-types of rhabdomyosarcoma: embryonal (ERMS), alveolar, and pleomorphic. ERMS accounts for more than 70% of rhabdomyosarcomas in children, with the alveolar rhabdomyosarcoma (ARMS) accounting for essentially all other pediatric cases. Older cases in the literature described as Pleomorphic Rhabdomyosarcoma (PRMS) in children very likely represent ERMS with anaplasia. Essentially all PRMSs, however, occur in adults.[6] Histologically, RMS is a neoplastic analogue of skeletal muscle embryogenesis.[3] Diagnosis is difficult and depends primarily on the identification of neoplastic rhabdomyoblasts. However, cells with cross striations are present only in 20-60% of cases and are mainly seen in the embryonal type.[4]
In view of its rarity, the present case of embryonal rhabdomyosarcoma arising from the buccal mucosa in a 36-year old male patient is herewith reported.
CASE REPORT
A 36-year old male patient was referred to our service for the evaluation of a painless swelling on his face that had appeared one and a half months earlier, with rapid evolution. During extra-oral examination, an extensive swelling on the right side of the face was observed, with un-defined limits. The skin overlying the swelling appeared shiny and stretched with ulceration [Figure 1a]. The swelling was associated with difficulty in mouth opening and mastication. Medical history was non-contributory to the present complaint.
Figure 1.
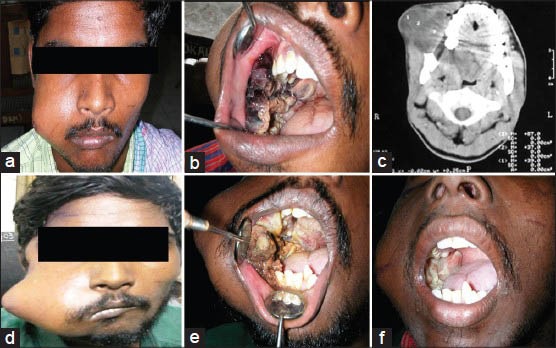
(a) Diffuse extra-oral swelling on the right side of the face, (b) Intra-oral mass with surface ulceration involving the right buccal mucosa and the posteriolateral aspect of the hard palate (c) Axial CT view depicting an expansile soft tissue lesion in the right bucco-gingival space with slight erosion of maxilla (d) Extra-oral swelling (10 days following incisional biopsy) (e) Enlargement of intra-oral mass involving entire right buccal mucosa and hard palate (f) Partial improvement noticed during the treatment's initial phase
On intra-oral examination, brownish-black colored mass was verified involving the right buccal mucosa, with necrotic changes and sloughing. The mass extended anteriorly from the right mandibular first premolar region to the retromolar region posteriorly with involvement of the posterior-lateral aspect of hard palate [Figure 1b]. On palpation, it was fibrous in consistency and non-tender. Ulceration was observed over the mass due to impingement of the teeth. No palpable cervical lymphadenopathy was present.
Orthopantomograph revealed no changes in the adjacent bone. Computerized tomography revealed a large expansile lesion with respect to right gingivo-buccal space showing slight erosion of the maxilla [Figure 1c]. Further to rule out distinct metastasis, chest radiography and ultrasonography of the abdomen were performed, that revealed no pathology.
In view of these findings, a diagnostic possibility of soft tissue sarcoma was hypothesized with differential diagnosis of Fibrosarcoma, Extra-osseous Ewing's sarcoma and Rhabdomyosarcoma. An incisional biopsy of the mass was performed and the histopathology of the specimen disclosed embryonal rhabdomyosarcoma [Figure 2a and b].
Figure 2.
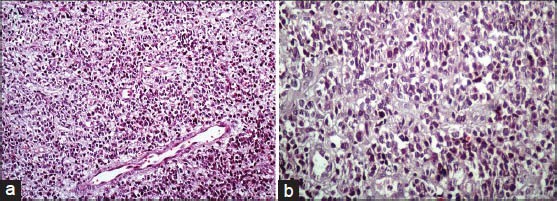
(a) Photomicrograph of the histopathologic section reveals sheets of atypical round cells having abundant eosinophilic cytoplasm with few areas showing vacuolated cells (H and E, ×200) (b) Photomicrograph demonstrates atypical rhabdomyoblasts with nuclear pleomorphism and few vacuolated cells (H and E, ×400)
Within a period of 10 days after the incisional biopsy, there was considerable increase in the size of extra-oral swelling along with an enormous increase in the intra-oral soft tissue mass involving the entire right buccal mucosa and hard palate [Figure 1d and e]. Patient was referred to an oncology centre (Madras Medical College Tamil Nadu, India) and was treated with chemotherapeutic drugs (vincristine, etoposide and ifosfamide) over a period of 32 weeks [According to Inter-group Rhabdomyosarcoma Study (IRS)-IV protocol]. Adjuvant external beam radiotherapy with a dose of 50.40 cGy in 28 fractions was given for a period of a month. Partial recovery occurred during the treatment's initial phase [Figure 1f] but with tapering of chemotherapeutic doses, there was sudden flare up in the tumor size. After that unfortunately, we lost communication with the patient for further treatment and follow up.
DISCUSSION
RMS is the most common soft tissue sarcoma in children. In contrast, RMS is rare in adults, accounting for <1% of all malignancies.[7] The present report describes a rare case of oral embryonal RMS in an adult.
Although there are no specific karyotypic abnormalities that characterize embryonal RMS, a sub-set of cases shows Loss Of Heterozygosity (LOH) at chromosome region 11p15.5, which contains several imprinted genes such as IGF2, H19 and p57. The hypothesis for the pathogenesis of ERMS is that there is LOH of the active imprinted allele.[8,9,10]
Since the time RMS was first described by Weber in 1854, it has always been a source of fascination and frustration for clinicians and pathologists because of their diverse pattern both clinically and histopathologically ranging from seemingly innocuous to pleomorphic types, frequently masquerading as an inflammatory polyp.[11] Histologically, the embryonal variety shows a mixture of spindle and un-differentiated round cells and immature striated muscle-like cells (rhabdomyoblasts) with abundant eosinophilic cytoplasm either tightly or loosely packed in a myxoid background.[3]
In the differential diagnosis with embryonal RMS, the main tumours to be considered are in the category of the so-called ‘small round blue cell tumors’ which in adults should include small cell carcinoma, merkel cell carcinoma and small cell malignant melanoma. Less commonly in this population, desmoplastic small round cell tumour (DSRCT) and Ewing sarcoma/peripheral neuroectodermal tumour (ES/PNET) may also be diagnosed.[7] Diagnosis is more accurate with newer techniques such as cytogenetic and immuno-histochemical analysis. Further, it is important that the surgeon pays attention to details such as amount of tissue and as well as location when the initial biopsy is performed for histologic and biologic studies.[3]
Recognition of the correct diagnosis and histological subtype of RMS is of critical importance in the therapy of this disease.[7] The treatment of adults with RMS is not uniform in the literature because of the rarity of the neoplasm in this population. Most series analyzing adult patients with RMS demonstrate a non-standardized multi-modality approach including surgery, chemotherapy (mostly as part of clinical trial protocols) and radiation therapy, similar to what is offered to the pediatric group.[12,13,14,15]
Comparing adult RMS with pediatric group, certain differences are apparent. There is no gender predilection with adults. The head and neck region is less commonly involved than in children, and the viscera are the most common site. The extremities are affected to a similar degree. The distribution of histologic types of rhabdomyosarcoma is similar with the exception that pleomorphic rhabdomyosarcoma is quite common. After 40 years of age, this type is the most common tumor in adults (approximately 40%).[2]
The prognosis of RMS is determined by clinical staging (TNM staging of RMS given by IRS),[5] anatomical site, histology and age of presentation.[16] On the basis of prognosis, RMS is classified into four groups:[17]
Favorable prognosis: botryoid and spindle types
Intermediate prognosis: embryonal
Poor prognosis: alveolar and undifferentiated sarcomas
Subtypes whose prognosis is not available; RMS with rhabdoid features
Considering the type i.e., embryonal, in the present case, prognosis can be considered as intermediate. Other features favouring the prognosis in the present case include localized non-invasive nature of the tumor without regional lymph node involvement or distant metastasis.
Rhabdomyosarcoma in adults is associated with a less favorable outcome and median survival is under 2 years.[13] Overall, there is a higher mortality rate in this population as compared to children, with 5 years survival averaging 35% in larger studies. The most important predictors of poor outcome common to all studies are tumour size, margin status after surgical resection, and presence of metastasis at diagnosis. Although age and histological subtype appear to be important prognostic indicators in the pediatric population, the influence of these parameters in adults is controversial.[12,13,14,15]
CONCLUSION
Overall, RMS is a rare disease in adulthood and, therefore, the clinicopathological characteristics, natural history and treatment options are not as well established in this population. But recognition of the correct diagnosis and histological sub-type of RMS is of critical importance in the therapy of this disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Franca CM, Caran EM, Alves MT, Barreto AD, Lopes NN. Rhabdomyosarcoma of the oral tissues: two new cases and literature review. Med Oral Patol Oral Cir Bucal. 2006;11:E136–40. [PubMed] [Google Scholar]
- 2.Hicks J, Flaitz C. Rhabdomyosarcoma of the head and neck in children. Oral Oncol. 2002;38:450–9. doi: 10.1016/s1368-8375(01)00105-1. [DOI] [PubMed] [Google Scholar]
- 3.Chigurupati R, Alfatooni A, Myall RW, Hawkins D, Oda D. Orofacial rhabdomyosarcoma in neonates and young children: A review of literature and management of four cases. Oral Oncol. 2002;38:508–15. doi: 10.1016/s1368-8375(01)00087-2. [DOI] [PubMed] [Google Scholar]
- 4.Cawson RA, Binnie WH, Speight P, Barrett AW, Wright JM. 5th ed. New York: Churchill Livingstone; 1998. Lucas's Pathology of Tumors of the Oral Tissues; pp. 315–7. [Google Scholar]
- 5.Enzinger FM, Weiss SW, Goldblum JR. 5th ed. St Louis, MO, USA: Mosby; 2008. Soft tissue tumors; pp. 595–631. [Google Scholar]
- 6.Gnepp DR. 2nd ed. Philadelphia: W.B. Saunders; 2009. Diagnostic Surgical Pathology of the Head and Neck; pp. 697–701. [Google Scholar]
- 7.Nascimento AF. Rhabdomyosarcomas in adults: Classification and differential diagnosis. Mini-symposium: Soft tissue tumour pathology. Diagn Histopathol. 2008;14:538–45. [Google Scholar]
- 8.Koufos A, Hansen MF, Copeland NG, Jenkins NA, Lampkin BC, Cavenee WK. Loss of heterozygosity in three embryonal tumours suggest a common pathogenic mechanism. Nature. 1985;316:330–4. doi: 10.1038/316330a0. [DOI] [PubMed] [Google Scholar]
- 9.Anderson J, Gordon A, McManus A, Shipley J, Pritchard-Jones K. Disruption of imprinted genes at chromosome region 11p15.5 in paediatric rhabdomyosarcoma. Neoplasia. 1999;1:340–8. doi: 10.1038/sj.neo.7900052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fletcher CD, Unni KK, Mertens F. Lyon: IARC Press; 2002. Pathology and Genetics of Tumours of Soft Tissue and Bone; pp. 146–9. [Google Scholar]
- 11.Stout AP. Rhabdomyosarcoma of skeletal muscles. ANN Surg. 1946;123:447–72. [PubMed] [Google Scholar]
- 12.La Quaglia MP, Heller G, Ghavimi F, Casper ES, Vlamis V, Hajdu S, et al. The effect of age at diagnosis on outcome in rhabdomyosarcoma. Cancer. 1994;73:109–17. doi: 10.1002/1097-0142(19940101)73:1<109::aid-cncr2820730120>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 13.Hawkins WG, Hoos A, Antonescu CR, Urist MJ, Leung DHY, Gold JS, et al. Clinicopathologic analysis of patients with adult rhabdomyosarcoma. Cancer. 2001;91:794–803. [PubMed] [Google Scholar]
- 14.Esnaola NF, Rubin BP, Baldini EH, Vasudevan N, Demetri GD, Fletcher CD, et al. Response to chemotherapy and predictors of survival in adult rhabdomyosarcoma. Ann Surg. 2001;234:215–23. doi: 10.1097/00000658-200108000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Little DJ, Ballo MT, Zagars GK, Pisters PW, Patel SR, El-Naggar AK, et al. Adult rhabdomyosarcoma outcome following multimodality treatment. Cancer. 2002;95:377–88. doi: 10.1002/cncr.10669. [DOI] [PubMed] [Google Scholar]
- 16.Chen SY, Thakur A, Miller A, Harwick RD. Rhabdomyosarcoma of the oral cavity: Report of four cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:192–201. doi: 10.1016/s1079-2104(05)80202-1. [DOI] [PubMed] [Google Scholar]
- 17.Al-Khateeb T, Bataineh AB. Rhabdomyosarcoma of the oral and maxillofacial region in Jordanians: a retrospective analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:580–5. doi: 10.1067/moe.2002.123860. [DOI] [PubMed] [Google Scholar]


