Abstract
Background
Rapid response teams have been adopted across hospitals to reduce the rate of inpatient cardiopulmonary arrest. Yet, data are not uniform on their effectiveness across university and community settings.
Objective
The objective of our study was to determine the impact of rapid response teams on patient outcomes in a community teaching hospital with 24/7 resident coverage.
Methods
Our retrospective chart review of preintervention-postintervention data included all patients admitted between January 2004 and April 2006. Rapid response teams were initiated in March 2005. The outcomes of interest were inpatient mortality, unexpected transfer to the intensive care unit, code blue (cardiac or pulmonary arrest) per 1000 discharges, and length of stay in the intensive care unit.
Results
Rapid response teams were activated 213 times during the intervention period. There was no statistically significant difference in inpatient mortality (3.13% preintervention versus 2.91% postintervention), code blue calls (3.09 versus 2.89 per 1000 discharges), or unexpected transfers of patients to the intensive care unit (15.8% versus 15.5%).
Conclusions
The implementation of a rapid response team did not appear to affect overall mortality and code blue calls in a community-based hospital with 24/7 resident coverage.
What is known
Rapid response teams may improve patient outcomes, yet there is inconsistent data about their effectiveness in different settings.
What is new
Retrospective chart review study with preintervention-postintervention data in a community hospital.
Limitations
Single-site study limits generalizability; lack of incidence and prevalence rates.
Bottom line
Patient outcomes are not affected by rapid response teams in a community setting with 24/7 coverage by residents.
Introduction
Rapid response teams have been recommended to help reduce the rate of inpatient cardiopulmonary arrest,1 which is typically associated with poor survival.2,3 Poor outcomes may be avoided by early detection of signs and symptoms suggesting patient deterioration, particularly cardiovascular instability.4 Rapid response teams have been studied in a variety of situations and settings.5–10 Teams typically comprise medical, nursing, and respiratory staff, who respond to predetermined changes in patient status in the inpatient, nonintensive care setting.6 The Institute for Healthcare Improvement's 100 000 lives campaign puts forth the institution of rapid response teams as 1 of 6 recommendations.1 Studies evaluating the effectiveness of rapid response teams have found mixed results, with some showing an improvement in outcomes, whereas others have shown no change in mortality and morbidity indicators.11–13 Studies conducted in academic centers show no improvement, whereas those conducted in community hospitals report improvement.3,7,9
We conducted a preintervention-postintervention study at our community-based teaching hospital to assess clinical outcomes of inpatient mortality, number of code blues (pulmonary or cardiac arrest), and unexpected transfer to the intensive care unit after instituting a rapid response team.
Methods
Setting
St Francis Hospital is a 367-bed, community-based teaching hospital in Evanston, Illinois, that sponsors an internal medicine residency program. The institution has approximately 33 000 emergency department visits and 12 000 inpatient admissions per year. It has a combined 22 beds in mixed medical-surgical intensive care units. All patients admitted to the hospital are under the care of resident teams.
Study Design and Patient Population
The design was a preintervention-postintervention trial using chart review and review of rapid response code records. Inclusion criteria were patient admissions to the medical and surgical floors during the study period. Patients with “do not resuscitate” orders were included because they were candidates for rapid response activation. Exclusion criteria were patient admissions directly to the intensive care unit from the emergency department or the operating room and patients younger than 16 years. Emergency department patients were not included in the study because no protocol has been established to activate the rapid response team in the emergency department.
The study period was from January 2004 to April 2006. The rapid response team was instituted in March 2005, and we used the period preceding implementation as the control period.
Nurse educators trained the nursing staff on the criteria for calling a rapid response. Residents were informed about the rapid response team in their morning reports as well as monthly resident meetings. The nurses had the authority to call a rapid response according to preset commonly used criteria (box).11–13
Box Criteria for Activating Rapid Response Team
Acute change in heart rate to < 40 beats/min or > 130 beats/min
Change in systolic blood pressure < 90 mm Hg
Acute change in respiratory rate < 6 breaths/min or > 30 breaths/min
Change in breathing pattern (regularity/depth)
Acute change in pulse oximetry (< 90% Spo2 on oxygen)
Acute decrease in urine output
New onset/prolonged seizures
Unexplained change in mental status
Nursing concern about patient status
Family concern regarding patient status
The rapid response team consisted of the admitting senior resident in the intensive care unit, an intensive care unit nurse, and a respiratory therapist. Team members carried a dedicated rapid response pager that was signed out before each shift. All activations of the rapid response were recorded in the rapid response log, which was signed by the senior resident and was collected and reviewed in monthly rapid response team meetings. The rapid response meetings were attended by intensive care unit staff, nursing supervisors, and resident members involved in the rapid response. The same team collected and reviewed code blue data on a frequent basis.
The possible outcomes of a rapid response included the patient staying on the floor after appropriate steps were taken by the rapid response team, transferring to the intensive care unit for closer observation, or advancing to code blue. If a patient required intensive care unit transfer, follow-up was done the next day to determine status.
Definitions and Outcomes Variables
The rapid response committee reviewed all the rapid response calls and also tracked cardiopulmonary arrests outside the intensive care units and emergency department. The timing of a rapid response was divided into daytime and off time. Daytime was defined as the time when primary teams responsible for care of the patient were required to be on site (7:00 am to 4:00 pm). The outcomes of interest were defined as inpatient mortality, unexpected transfer to the intensive care unit, code blue calls per 1000 discharges, and intensive care unit length of stay. Inpatient mortality was calculated as the total number of deaths divided by the total number of admissions to the hospital. Unexpected transfers to the intensive care unit were defined as patients who were originally admitted to the medical departments but needed to be transferred to the intensive care unit unrelated to a procedure. Code blue rates per 1000 discharges were calculated both for the entire hospital and the inpatient floors. Rates calculated for inpatient floors excluded codes in the intensive care unit and emergency department.
Sample size calculations revealed that 137 code blue events across the hospital would be required in the pretime and posttime periods each to detect a 5% decline in code blue events after introduction of rapid response teams (α = 0.05, power = 80%). To elicit a 10% decline in inpatient mortality, 350 deaths would need to be observed in both the pretime and posttime periods (α = 0.05, power = 80%). Based on historical mortality and code blue rates at our hospital, we performed our calculations for a 14-month period before and after the institution of rapid response teams to power our study to capture a 5% and 10% decline in code blue and inpatient mortality rates, respectively.
The study was approved by the St Francis Hospital Institutional Review Board.
Statistical Analysis
Linear regression was used for each outcome variable; the χ2 test was used for inpatient mortality analysis. SPSS version 16 (IBM Corp, Armonk, NY) was used for analysis.
Results
Rapid response teams were called 213 times during the 14-month intervention period. Of those, 171 calls (80.3%) were for patients admitted to medical floors, and 42 calls (19.7%) were for patients admitted to surgical specialties. The average time to respond to a rapid response by at least 1 member of the rapid response team was 3.1 minutes. Response time to acute deterioration in patient condition during the control period is not known.
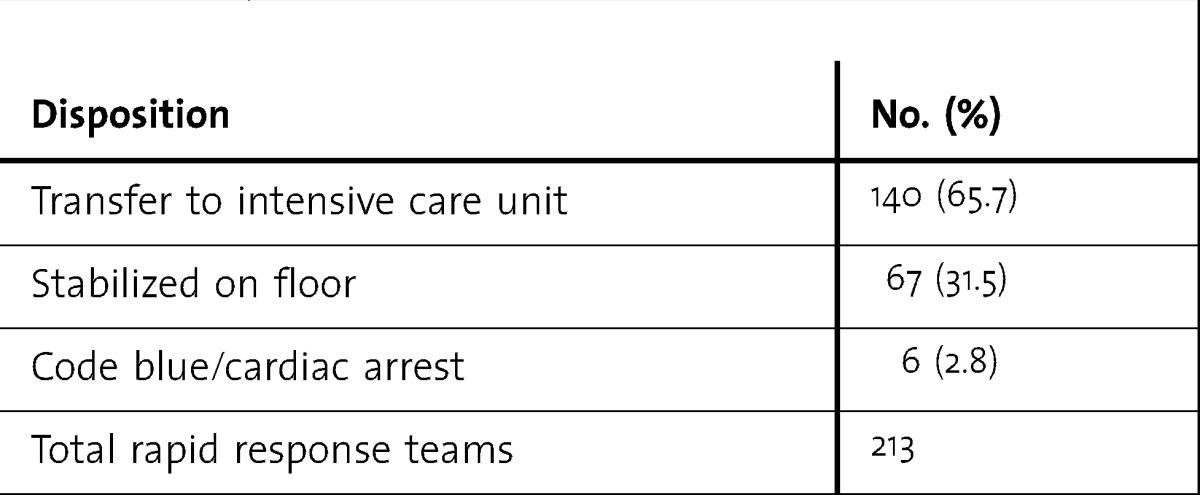
The most frequent reason to institute a rapid response was respiratory distress or respiratory-related issues (61.0%, 130 of 213; table 1). Mental status changes and multiple complaints were the next most common causes for activating the rapid response team. Most patients (65.7%, 140 of 213) were transferred to the intensive care unit for closer monitoring, and the rest (n = 73, 34.3%) were deemed stable enough to be observed on the floor (table 2). Only a few rapid response team activations (2.8%, 6 of 213) turned into cardiac arrest/code blue.
TABLE 1.
Primary Reasons to Call Rapid Response Team
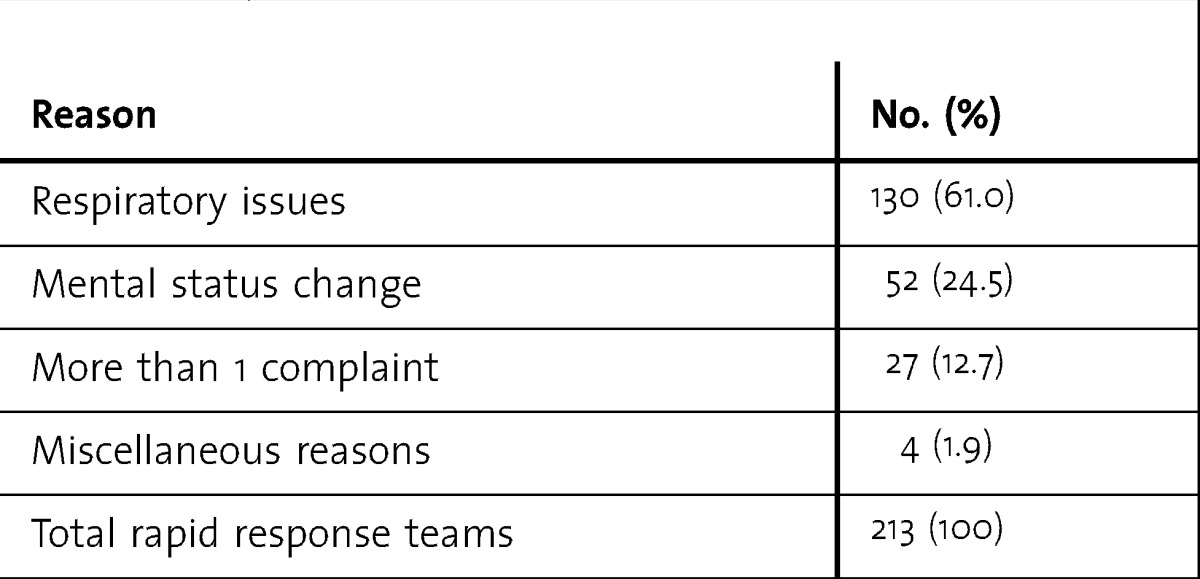
TABLE 2.
Patient Disposition After Rapid Response Team
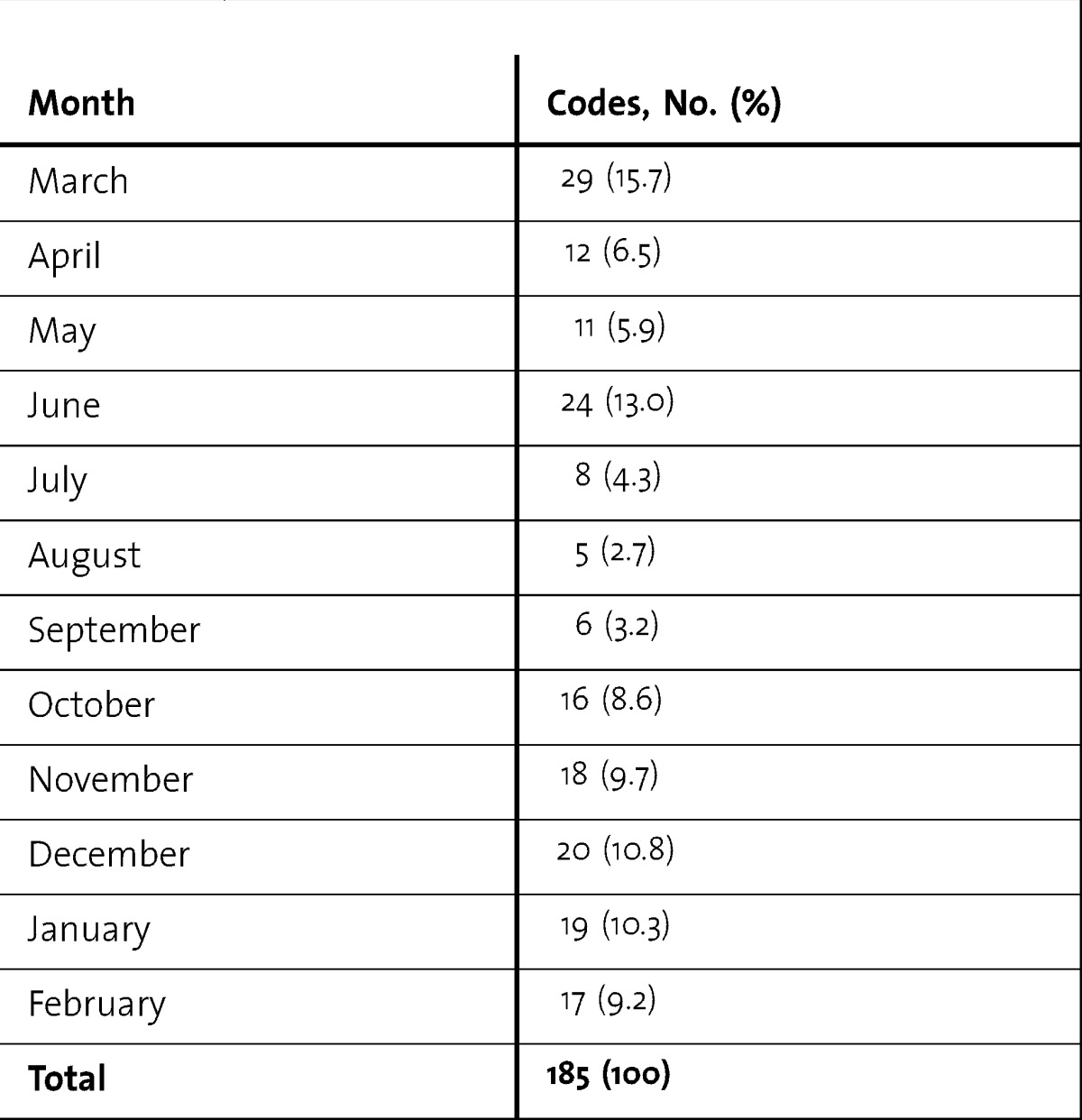
More rapid response team calls occurred during daytime (146) versus off time (67). There was no significant difference in the proportion of patients transferred to the intensive care unit at the end of a rapid response called during daytime versus off time (P = .16; table 3). When looking at the trend of codes by month, there were more codes called during the winter months (table 4). There was no statistically significant change in inpatient mortality, number of unexpected intensive care unit transfers, and code blue calls after introduction of rapid response teams. The inpatient mortality was 3.13% (439 of 14 013) in the preintervention period and decreased to 2.91% (417 of 14 333) in the postintervention period (P = .27). The number of unexpected intensive care unit transfers declined from 15.8% (295 of 1866) of intensive care unit admissions to 15.5% (258 of 1663, P = .80). The number of code blue calls on inpatient floors decreased from 3.09 per 1000 discharges per year to 2.89 per 1000 discharges per year (P = .14). The number of code blue calls in the hospital decreased from 10.59 per 1000 discharges to 10.13 per 1000 discharges (P = .21). The average length of stay in the intensive care unit increased from 3.18 days to 3.24 days.
TABLE 3.
Daytime Versus Off Timea
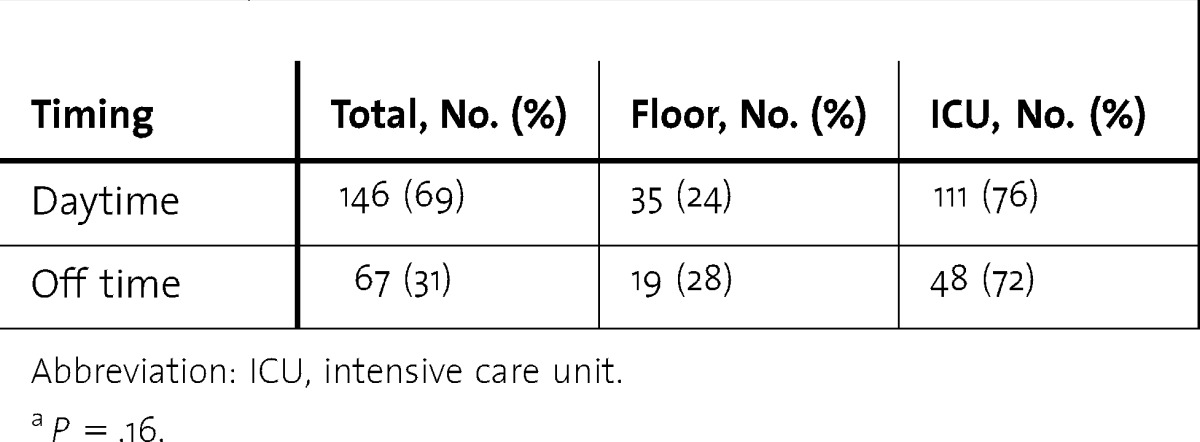
TABLE 4.
Codes Per Month
Discussion
Our findings show that the rapid response teams, while resulting in small improvements in several outcomes, did not have a statistically significant effect on inpatient mortality and the number of code blue calls in a community-based teaching hospital. These results differ from early published studies on the use of rapid response teams, which found a decrease in mortality and morbidity.4,6,7,11,14,15 A recent meta-analysis found that rapid response teams did not increase survival, but they tended to decrease out-of-intensive care unit cardiopulmonary arrests.6 Other reviews showed similar conclusions.16–18 One possible reason for the lack of effectiveness of the rapid response teams in our study could be the relative similarity in timeliness and quality of care for patients between the prerapid response and rapid response eras. The accessibility of residents when patients need to be seen remained constant, which may explain the lack of difference in mortality. One possible measure of success would be to assess the 30-day mortality or readmission rates for patients who required rapid response team activation; however, we did not have enough rapid response team calls to perform that analysis. Studies show a greater benefit in mortality among the pediatrics population,6,9 possibly because that group is more prone to rapid deterioration and may derive greater benefit from a timely intervention.
The most common reason for calling the rapid response (respiratory distress) and the interventions (nebulizers and diuretics) were consistent with prior studies.4,6,9 The rate of patients being transferred to the intensive care unit after a rapid response was higher compared with other studies. This may be because the setting was a community-based hospital, with a lack of nighttime, on-site faculty, and attending physicians may have felt more comfortable with the patients being observed in the intensive care unit after deterioration.
We did not analyze costs because the rapid response teams used scheduled members of the patient care team, and there was no substantial incremental cost associated with implementing the teams (residents, nurses, etc), so that was not an additional cost burden to the hospital. Other studies have employed midlevel providers and were able to calculate the cost of hiring and training the new staff.7
Our study has several limitations. It was conducted at a single site, limiting generalizability. We cannot calculate incidence and prevalence rates with these data, and the true prospective nature of the effect cannot be established. There was no randomization during the study. It is possible that the institution of rapid response teams might have positively affected other outcomes that we did not evaluate, such as readmission rates and nursing satisfaction. There might also have been a learning curve with implementation of a new system. Lastly, the “event rate” in our study is lower than that reported in recent studies on rapid response teams.19 This is likely due to the smaller size of our hospital and that we studied rapid response teams relatively soon after being instituted. An overall increase in familiarity with rapid response teams can potentially increase the comfort level with activating a rapid response and lead to more rapid response calls.
Conclusion
The implementation of a rapid response team did not seem to affect overall mortality and code blue calls in a community-based hospital where 24/7 coverage by residents is already in place.
Footnotes
Ankur Segon, MD, MPH, FACP, is Assistant Professor, Medical College of Wisconsin; Shahryar Ahmad, MD, is Assistant Professor, Medical College of Wisconsin; Yogita Segon, MD, is Resident Physician, Medical College of Wisconsin; Vivek Kumar, MD, is Staff Physician, Susquehana Health System; Harvey Friedman, MD, is Program Director, Internal Medicine Residency Program, Saint Francis Hospital; and Muhammad Ali, MD, is Assistant Professor, Medical College of Wisconsin.
Funding: The authors report no external funding source for this study.
References
- 1.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14 720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 2.Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98(6):1388–1392. doi: 10.1378/chest.98.6.1388. [DOI] [PubMed] [Google Scholar]
- 3.Buist MD, Jarmolowski E, Burton PR, Bernard SA, Waxman BP, Anderson J. Recognising clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care: a pilot study in a tertiary-care hospital. Med J Aust. 1999;171(1):22–25. doi: 10.5694/j.1326-5377.1999.tb123492.x. [DOI] [PubMed] [Google Scholar]
- 4.Baxter AD, Cardinal P, Hooper J, Patel R. Medical emergency teams at the Ottawa hospital: The first two years. Can J Anaesth. 2008;55(4):223–231. doi: 10.1007/BF03021506. [DOI] [PubMed] [Google Scholar]
- 5.Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med. 2010;170(1):18–26. doi: 10.1001/archinternmed.2009.424. [DOI] [PubMed] [Google Scholar]
- 6.Dacey MJ, Mirza ER, Wilcox V, Doherty M, Mello J, Boyer A, et al. The effect of a rapid response team on major clinical outcome measures in a community hospital. Crit Care Med. 2007;35(9):2076–2082. doi: 10.1097/01.ccm.0000281518.17482.ee. [DOI] [PubMed] [Google Scholar]
- 7.Jones D, Bellomo R, Bates S, Warrillow S, Goldsmith D, Hart G, et al. Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit Care. 2005;9(6):R808–R815. doi: 10.1186/cc3906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King E, Horvath R, Shulkin DJ. Establishing a rapid response team (RRT) in an academic hospital: one year's experience. J Hosp Med. 2006;1(5):296–305. doi: 10.1002/jhm.114. [DOI] [PubMed] [Google Scholar]
- 10.Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006;34(9):2463–2478. doi: 10.1097/01.CCM.0000235743.38172.6E. [DOI] [PubMed] [Google Scholar]
- 11.Berwick DM, Calkins DR, McCannon CJ, Hackbarth AD. The 100 000 lives campaign: setting a goal and a deadline for improving health care quality. JAMA. 2006;295(3):324–327. doi: 10.1001/jama.295.3.324. [DOI] [PubMed] [Google Scholar]
- 12.Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart GK, Opdam H, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003;179(6):283–287. doi: 10.5694/j.1326-5377.2003.tb05548.x. [DOI] [PubMed] [Google Scholar]
- 13.Bristow PJ, Hillman KM, Chey T, Daffurn K, Jacques TC, Norman SL, et al. Rates of in-hospital arrests, deaths and intensive care admissions: the effect of a medical emergency team. Med J Aust. 2000;173(5):236–240. doi: 10.5694/j.1326-5377.2000.tb125627.x. [DOI] [PubMed] [Google Scholar]
- 14.Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002;324(7334):387–390. doi: 10.1136/bmj.324.7334.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan PS, Khalid A, Longmore LS, Berg RA, Kosiborod M, Spertus JA. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506–2513. doi: 10.1001/jama.2008.715. [DOI] [PubMed] [Google Scholar]
- 16.Price RJ, Cuthbertson BH, Cairns CJ. The findings of the International Conference on Medical Emergency Teams are biased and misleading. Crit Care Med. 2007;35(3):992–993. doi: 10.1097/01.ccm.0000257474.01932.2f. [DOI] [PubMed] [Google Scholar]
- 17.Winters BD, Pham J, Pronovost PJ. Rapid response teams—walk, don't run. JAMA. 2006;296(13):1645–1647. doi: 10.1001/jama.296.13.1645. [DOI] [PubMed] [Google Scholar]
- 18.Price R, Cuthbertson B, Cairns C. Should hospitals have a medical emergency team. Br J Hosp Med. 2007;68(4):224. doi: 10.12968/hmed.2007.68.4.224. [DOI] [PubMed] [Google Scholar]
- 19.Shah SK, Cardenas VJ, Jr, Kuo YF, Sharma G. Rapid response team in an academic institution does it make a difference. Chest. 2011;139(6):1361–1367. doi: 10.1378/chest.10-0556. [DOI] [PubMed] [Google Scholar]


