Abstract
CHD5 was first identified because of its location on 1p36 in a region of frequent deletion in neuroblastomas. CHD5 is the fifth member of a family of chromatin remodeling proteins, and it probably functions by forming a nucleosome remodeling and deacetylation complex that regulates transcription of particular genes. CHD5 is preferentially expressed in the nervous system and testis. Based on its position, pattern of expression and function in neuroblastoma cells and xenografts, CHD5 was identified as a tumor suppressor gene (TSG). Evidence soon emerged that CHD5 also functioned as a TSG in gliomas and a variety of other tumor types, including breast, colon, lung, ovary and prostate cancers. Although one copy of CHD5 is deleted frequently, inactivating mutations of the remaining allele are rare. However, DNA methylation of the CHD5 promoter is found frequently, and this epigenetic mechanism leads to biallelic inactivation. Furthermore, low CHD5 expression is strongly associated with unfavorable clinical and biological features as well as outcome in neuroblastomas and many other tumor types. Thus, based in its likely involvement as a TSG in neuroblastomas, gliomas and many common adult tumors, CHD5 may play an important developmental role in many other tissues besides the nervous system and testis.
Keywords: CHD5, epigenetic, neuroblastoma, promoter methylation, tumor suppressor gene
CHD5: Mechanisms of Action
CHD5 is a member of the chromodomain-helicase-DNA binding (CHD) protein family
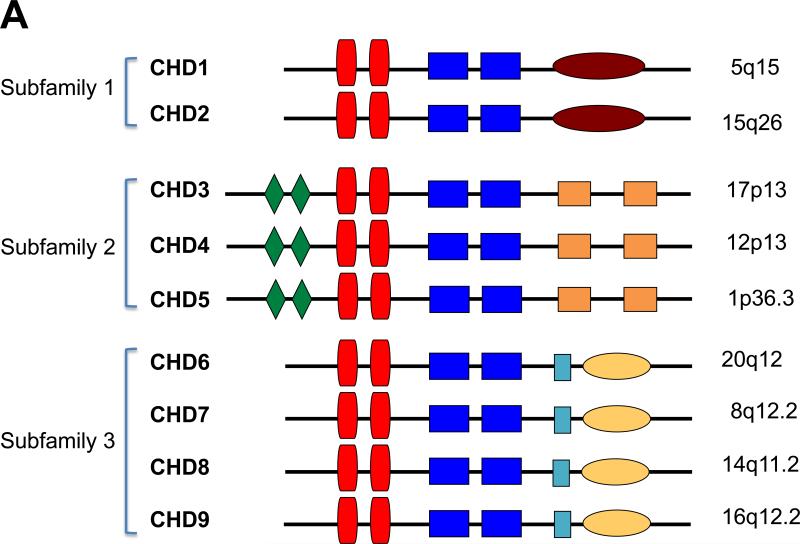
CHD5 was first identified based on its location on 1p36 in a region of frequent deletion in neuroblastomas (1). CHD5 is the fifth member of a nine-member family of CHD chromatin remodeling proteins (CHD1-CHD9) (Fig. 1A). These proteins can be classified into three subfamilies or classes, based on structural features and sequence homology— 1) CHD1 and CHD2, 2) CHD3-CHD5, and 3) CHD6-CHD9 (2-4). One report initially described CHD6 as CHD5 (5), leading to some confusion as to whether CHD5 belonged to subfamily 2 or 3 (2, 3). However, based on sequence homology, paired plant homology domain (PHD) motifs at the N-terminal region that are unique to these three members, and similar protein associations, CHD5 more appropriately belongs in the second subfamily with CHD3 and CHD4 (4).
Figure 1. CHD5 Chromatin Remodeling Protein.
A. CHD family. Shown are diagrammatic representations of the nine members of the CHD (Chromodomain-Helicase-DNA binding) family of proteins. They are divided into three subfamilies based on sequence and structural homology as well as function. The conserved motifs are shown: green diamonds = PHD finger domains; red vertical boxes = chromodomains; blue rectangular boxes = split SNF2-like helicase/ATPase domain; burgundy oval = DNA binding motif; orange boxes = domains of unknown function (DUF1, DUF2); light blue box = SANT domain; yellow oval = BRK domains. The chromosomal locations of the nine CHD family members are shown to the right.
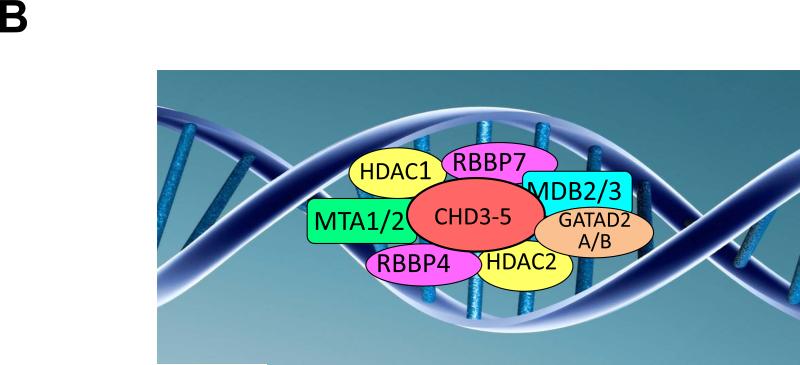
B. CHD5 NuRD complex. Shown is a diagrammatic representation of the hypothetical CHD5-NuRD complex, which is identical to a CHD4-NuRD complex. The canonical components of this complex are HDAC1 and HDAC2; MTA1 and MTA2; RBBP4 and RBBP7; GATA2DA and GATA2DB; and MDB2 and MDB3.
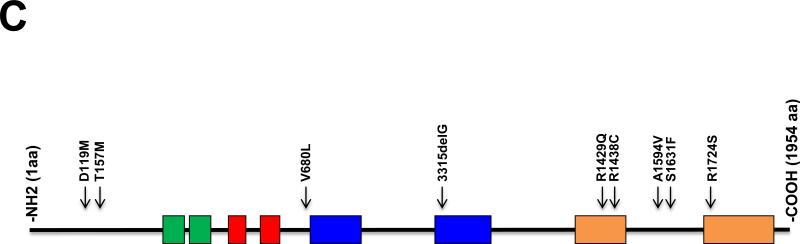
C. CHD5 mutations. Shown is a diagram of the CHD5 protein with conserved motifs, as indicated in 1A. The relative position of 9 CHD5 mutations in various cancers is listed in Table 1 and shown on this diagram. All of the mutations (8 of the 9) involved highly conserved amino acids (see Supplemental Figure 1). The G base pair deletion at nucleotide position 3315 changed the reading frame and led to a premature stop codon.
CHD5 forms a nucleosome remodeling and deacetylation (NuRD)-type chromatin remodeling complex, similar to CHD3 and CHD4
The canonical NuRD complex consists of CHD4 together with other proteins, including MTA1/2, HDAC1/2, RBBP4/7, GATAD2A/B, and MDB2/3 (6-11). This megadalton complex is presumably recruited to specific genes or DNA domains by interaction with other DNA binding proteins. We and others have evidence that CHD5 interacts with most members of a canonical NuRD complex, further supporting a similar function [(12) and unpublished] (Fig. 1B). CHD proteins in the second subfamily lack direct DNA binding motifs, so they must interact with transcription factors, cofactors, or other DNA binding proteins to regulate transcription. NuRD complexes are generally thought to be transcriptionally repressive, but they are also associated with transcriptional activation, as well as transcript elongation, termination, RNA processing, and DNA damage response (4, 13). The exact functions may depend on the cellular context, developmental stage, the proteins that form the complex, and the DNA binding proteins with which they interact (12).
CHD5 requires PHD domains for histone 3 binding and tumor suppression
Structurally, CHD5 is characterized by paired PHD domains and two tandem chromodomains at the N-terminal region, an SNF2-like helicase/ATPase domain in the central region, and a conserved, coiled-coil motif in the C-terminal region. The tandem PHD domains are zinc finger-like motifs that recognize histone tails, which also facilitate chromatin-based transcriptional regulation (14). CHD5 binds the unmodified N-terminus of H3 through its PHD domains at loci lacking H3K4me3, a mark of actively transcribed genes (14, 15). However, CHD5 can also bind to H3K27me3, a mark of inactive genes (16). Inactivating mutations in the PHD domains of CHD5 abrogate histone 3 binding, which is critical for modulation of target genes and for tumor suppression (15).
CHD5 is preferentially expressed in the nervous system and testis
Interestingly, CHD4 and CHD3 are expressed ubiquitously, whereas CHD5 is preferentially expressed in the nervous system (brain, spinal cord, adrenal medulla, sympathetic ganglia) and testis (1, 12, 16-18). Within the nervous system, CHD5 expression is restricted to neurons, and glial cells are consistently negative. Furthermore, expression is confined to the nucleus of mature neurons, consistent with its presumed role as a chromatin remodeling protein (12, 16, 17, 19). CHD5 is also required for proper spermiogenesis and chromatin condensation in sperm, and male mice with constitutional homozygous deletion of CHD5 are infertile (18). Thus, the selective pattern of CHD5 expression in the nervous system and testis suggests that CHD5 may have unique functions in these tissues. Nevertheless, CHD5 is expressed at lower levels in many other tissues, and it has been implicated as a tumor suppressor gene (TSG) in a variety of non-neural cancers, suggesting it may also play an important developmental role in other tissues.
CHD5 expression is regulated by different mechanisms
CHD5 may be transcriptionally silenced by DNA methylation of the promoter, silencing the remaining allele in some cancers with 1p deletion (see below). One study examined the methylation status of the promoter in all the CHD family genes in various cancers, and the CHD5 promoter was the most heavily methylated, (20). In addition, at least two other mechanisms of regulation have been identified. The lysine demethylase JMJD2A was identified because it cooperated with RAS activation to transform primary cells in culture, blocking cellular senescence (21). JMJD2A apparently causes transcriptional repression of CHD5, which leads to reduced p53 expression. MiRNAs can also regulate gene expression by binding to the 3’ untranslated region of mRNAs, causing translational repression or mRNA instability (22). One group analyzed the CHD5 mRNA and predicted that miR-211 bound to the CHD5 3’-UTR (23). Transfection of colon cancer cells with an miR-211 expression vector substantially decreased CHD5 expression and produced a more aggressive phenotype in vitro and in vivo, suggesting that CHD5 is a direct target of miR-211. However, transcriptional regulation by other transcription factors, miRNAs or other mechanisms is still unknown.
CHD5 functions as a TSG in part by regulating p53
We first identified CHD5 as a candidate TSG in neuroblastomas (1). Bagchi and colleagues took an independent approach using chromosome engineering to identify Chd5 as a TSG on mouse chromosome 4, a region orthologous to human 1p36 (24). They determined that Chd5 functions as a TSG that controls proliferation, apoptosis, and senescence at least in part by upregulation of p19Arf, which in turn upregulates p53 (24). CHD5 may have similar effects on p14Arf in human cells, although it is likely that its TSG function is not limited to this mechanism. Indeed, little is known about the other target genes that are regulated by CHD5 or CHD5-NuRD complexes.
CHD5 functions as a TSG in neuroblastomas and a variety of other cancers
Here we review the evidence supporting CHD5 as a bona fide TSG in neuroblastoma, a common pediatric tumor, as well as gliomas and many other adult cancers, including cancers of the breast, colon, lung, ovary, prostate, stomach, larynx, and gallbladder. In many cases, one copy of CHD5 is deleted, but the remaining allele is seldom unaltered (Fig. 1C, Table 1). Nevertheless, expression of the remaining allele (or both alleles if one is not deleted) are frequently silenced by promoter methylation. Thus, both genetic and epigenetic mechanisms are involved in silencing this novel TSG.
Table 1.
Cancers with 1p36 deletion and possible role of CHD5
| Malignancy | 1p Deletion (%) | CHD5 Mutation | CHD5 Mutation(s)+ | CHD5 Expression | Promoter Methylation* | CHD5 Growth Suppression | CHD5 Clinical Correlation | References |
|---|---|---|---|---|---|---|---|---|
| Neuroblastoma | 35% | 1/30 | V680L | Lower in HR tumors | Yes* | In vitro and in vivo | Risk factors Outcome | (32-35, 37) |
| Gliomas | 30-50% | ND | ----- | Lower in tumors | ND | ND | Outcome | (24, 40, 41) |
| Colorectal | 20-30% | ND | ----- | Lower in tumors | Yes* | In vitro and in vivo | Risk factors | (23, 42-44) |
| Breast | 61% | 2/55 | 3315delG T157M |
Lower in tumors | Yes* | In vitro and in vivo | Risk factors Outcome | (45) |
| Lung Cancer | 60% | ND | ----- | Lower in tumors | Yes | In vitro and in vivo | ND | (42) (46) |
| Ovarian | 55% | 4/123 | D119M R1429Q R1438C S1631F |
Lower in tumors | ND | ND | Outcome | (42, 47-49) |
| Gastric | 53-73% | ND | ----- | Lower in tumors | Yes* | In vitro | ND | (42) (50) (51) |
| Laryngeal SCC | ND | ND | ----- | Lower in tumors | Yes | In vitro | Risk factors | (52) |
| Gallbladder Ca. | ND | ND | ----- | Lower in tumors | ND | ND | Outcome | (53) |
| Prostate | ND | 2/8 | A1594V R1724S |
ND | ND | ND | ND | (54) |
NA = Not applicable; ND – Not done.
Nucleotide changes were converted to amino acid changes, and coding sequence positions modified based on RefSeq NM_015557.
Re-expression by 5-aza-2-deoxycytidine (5-Aza)
Role of CHD5 in Neuroblastomas
Neuroblastoma is a tumor of the sympathetic nervous system that is the most common extracranial solid tumor of childhood (25, 26). We first identified 1p deletion as a characteristic change in advanced stage neuroblastomas (27). Deletion of the short arm of chromosome 1 (1p) has been observed in 35% of primary neuroblastomas and 70-80% of neuroblastoma-derived cell lines (28-31). Deletion of 1p presumably reflects loss of one or more TSGs from this region. We refined the region of consistent deletion of 1p36 using DNA-based polymorphisms and narrowed the smallest region of consistent deletion to a ~2 Mb region on 1p36.31 (30, 32, 33). Although 23 genes mapped to this 2 Mb region, we identified CHD5 as the most likely TSG contributing to neuroblastoma pathogenesis from this region (1, 34, 35).
We first identified CHD5 as a new member of the CHD family and a candidate TSG in neuroblastomas 10 years ago (1). Indeed, subsequent studies by ourselves and others strongly support CHD5 as an important TSG in neuroblastomas, based on: 1) its function and expression profile, 2) its ability to suppress neuroblastoma growth in vitro and in vivo, and 3) the correlation of CHD5 expression with prognostic variables and outcome (17, 34-37). However, other TSGs have been identified on 1p36 that may also play important roles in neuroblastoma pathogenesis, including CAMTA1, miR-34a, KIF1Bβ, CASZ1 and ARID1A [reviewed in (38, 39)]. Most 1p deletions in neuroblastomas are quite large, so several of these other genes may be involved. However, at least for CHD5, simply deleting one copy is probably not sufficient to promote tumorigenesis, as expression the remaining allele in cases with 1p36 deletion is extremely low or undetectable (34, 37). Indeed, the remaining allele in cases with 1p deletion is seldom mutated (Table 1, Fig. 1C), suggesting that it is silenced transcriptionally by epigenetic mechanisms.
Functional analysis of CHD5 after transfection into neuroblastoma lines demonstrates that it suppresses both clonigenicity and tumorigenicity (34). High CHD5 is strongly correlated with favorable clinical and biological features as well as outcome, whereas low/absent expression is associated with unfavorable features including MYCN amplification, as well as a poor outcome (17, 37). Although one copy of CHD5 is frequently deleted, the remaining copy is rarely mutated or inactivated by DNA rearrangement. However, the CHD5 promoter is heavily methylated, especially between –780 and –450 in neuroblastoma cell lines with 1p36 deletions (34). Furthermore, CHD5 can be re-expressed by exposure to the demethylating agent 5-aza-2’-deoxycytidine (5-Aza). Thus, CHD5 is a bona fide TSG in neuroblastomas, but the remaining CHD5 allele is usually silenced by epigenetic mechanisms rather than by inactivating mutations (35).
High CHD5 expression by microarray analysis was strongly associated with favorable clinical and biological risk features as well as outcome in a panel of 101 neuroblastomas (34). Similarly, high CHD5 mRNA expression (by quantitative real-time RT-PCR) was associated with favorable risk features and outcome in a study of 814 representative primary neuroblastoma (37). CHD5 protein expression was also shown to be a strong prognostic marker in an immunohistochemical study of 90 primary neuroblastomas (17). Finally, a study of differentially expressed genes from chromosomes 1 and 17 led to an expression signature that was predictive of neuroblastoma outcome. CHD5 was identified as one of only three genes (CHD5, PAFAH1B1, NME1) that robustly classified patients into clinically relevant risk groups (36). Thus, there is strong structural and functional evidence that CHD5 is a bona fide TSG in neuroblastomas, and high CHD5 expression is strongly associated with both favorable features and outcome (and vice versa).
Role of CHD5 in Other Cancers
Gliomas (Table 1)
Law and colleagues screened 17 glioma lines for 1p deletions using fluorescence in-situ hybridization, comparative genomic hybridization and DNA polymorphisms (40). They defined a 700 kb region of consistent deletion that contained five genes and four uncharacterized transcripts; CHD5 was the most plausible TSG in this region. Bagchi and coworkers analyzed the expression of genes mapping to a 5.4 Mb region corresponding to 1p36 in 54 gliomas, and loss of CHD5 expression was significantly associated with 1p36 deletion in these tumors (24). Finally, Wang measured CHD5 expression in 128 gliomas, and down-regulation of CHD5 expression was associated with unfavorable risk features and outcome in these patients (41). These data are consistent with a role for CHD5 as a TSG in gliomas.
Colorectal cancer (Table 1)
Ragnarsson analyzed several solid tumor types for 1p allelic loss using microsatellite markers, and they identified 1p deletion in 20-30% of cases (42). Mokarram studied the methylation status of a set of cancer-related genes in 102 colon cancers from Iranian and African-American populations (51 each) (43). The methylation status of the CHD5 promoter was significantly higher in cancers from the African-American population (78%) compared to the Iranian patients (47%; p<0.002). In addition, CHD5 showed a lower level of methylation in the distal colon (43), suggesting that CHD5 may play a role in the incidence or aggressiveness of colorectal cancer in this population. Fatemi found that the CHD5 gene was repressed, either epigenetically or by chromosomal deletion, in colon adenomas compared to surrounding normal tissue (44). Cai also investigated the effect of epigenetic silencing of CHD5 on colorectal tumorigenesis (23). A colorectal cancer cell line (HCT-116) was stably transfected to overexpress miR-211, which was predicted to bind to the 3’ untranslated region of CHD5. The transfected cell line showed a 50% decrease in CHD5 protein level. In vitro and in vivo studies showed that cell proliferation, cell migration and tumor growth were significantly higher than control cells. These results suggest CHD5 is a direct target of miR-211, and epigenetic silencing of CHD5 may play a role in colorectal tumorigenesis.
Breast Cancer (Table 1)
Wu analyzed the role of CHD5 in breast cancer by screening 55 tumors for mutations, 39 tumors for promoter methylation, 90 tumors for CHD5 RNA expression, and 289 tumors for CHD5 protein expression (45). They correlated CHD5 expression changes with clinico-pathological characteristics of breast cancer. They also assessed functional effects of CHD5 on cell proliferation, invasion and tumorigenesis. Two CHD5 mutations were found out of 55 cases examined (Table 1). One was a base pair deletion leading to a premature stop codon and a truncated protein, and the other was a conserved codon at the N-terminus in a region of unknown function. CHD5 mRNA and protein expression was significantly reduced in breast cancer tissue, which was accompanied by genomic deletion and promoter methylation, and treatment with 5-Aza restored CHD5 expression. Low CHD5 mRNA expression was correlated with lymph node metastasis (p=0.026), and lack of CHD5 protein expression was correlated with higher tumor stage, ER/PR-negativity, HER2 positivity, distant metastasis and worse patient outcome (p≤0.01). Transfection of breast cancer cells with CHD5 inhibited cell proliferation and invasion in vitro, and tumorigenesis in nude mice (45). These studies suggest that decreased CHD5 expression, mediated in part by promoter methylation, contributes to the development and progression of human breast cancer.
Lung Cancer (Table 1)
Zhao studied the epigenetic modification and tumor-suppressive ability of CHD5 by measuring CHD5 mRNA and protein expression in lung cancer cell lines and tissues (46). CHD5 expression ranged from low to absent in the lung cancer lines and tissues examined, and this correlated with CHD5 promoter hypermethylation. Clonigenicity and tumor growth were abrogated in lung cancer cell lines A549 and H1299 upon restoration of CHD5 expression (46). These observations suggest that CHD5 served as a potential TSG in lung cancer.
Ovarian Cancer
Gorringe analyzed 123 primary ovarian cancers for CHD5 mutations (47). Missense mutations were identified in 3 of 123 tumors, but no inactivating mutations were found (Table 1, Fig 1C). They referred to an earlier study that identified one potentially pathogenic mutation in CHD5 out of 10 tumors examined (48) (Table 1, Fig 1C). Although none of these mutations were inactivating, all were in codons encoding conserved amino acids (Supplemental Fig. 1). Promoter methylation was seen in another 3 of 45 samples tested, and copy number loss was seen in 6 of 85 tumors. Overall, deletion, mutation or promoter methylation was seen in about 16% of cases (47). Wong compared CHD5 expression between 72 primary ovarian tumors and 12 normal ovarian tissues, and found that CHD5 expression was downregulated at least 2-fold in 32 out of 72 (41%) tumors compared to normal tissues (49). CHD5 down-regulation was associated with shorter disease-free and overall survival (p<0.05). These studies suggest a possible role for CHD5 in the pathogenesis of at least a subset of ovarian cancers.
Gastric Cancer (Table 1)
Wang examined the expression and promoter methylation status of 7 gastric cancer cell lines and 15 primary gastric tumors (50). CHD5 expression was downregulated in all gastric cancer lines. CHD5 promoter methylation was detected in all seven lines, and exposure to 5-Aza substantially restored expression levels towards that seen in normal gastric mucosa. Methylation status of the CHD5 promoter was examined in 15 primary gastric cancers, and methylation was found in 11 of 15 primary tumors. Furthermore, ectopic expression of CHD5 resulted in significant growth inhibition in colony formation assays (50). In another study, Qu conducted a study of the methylation status of cancer-related genes (including CHD5) in gastric cancer (51). The percent methylation in gastric cancers was twice that found in normal gastric mucosa. These results suggest that CHD5 play a role as TSG in gastric cancer, and expression may be downregulated by promoter hypermethylation.
Laryngeal squamous cell carcinoma (Table 1)
Wang examined CHD5 mRNA and protein expression in 65 patients with laryngeal squamous cell carcinomas (SCC) (52). Both CHD5 RNA and protein expression were significantly lower compared to normal laryngeal tissue, and the level of CHD5 expression correlated with the extent of promoter hypermethylation. Furthermore, ectopic expression of CHD5 in laryngeal SCC cells led to significant inhibition of growth and invasiveness (52). These data suggest that CHD5 acts as a TSG that is epigenetically downregulated in laryngeal SCC.
Gallbladder carcinoma (Table 1)
Du and colleagues studied CHD5 mRNA and protein expression in 120 primary gallbladder carcinomas and 20 normal gallbladder specimens (53). The expression levels of CHD5 mRNA and protein were both significantly lower in the gallbladder carcinomas than those in the normal gallbladder epithelium (mRNA: p<0.006; protein: p<0.01). Survival analysis showed that low CHD5 expression in gallbladder carcinomas was associated with shorter disease-free (p=0.01) and overall survival (p=0.008) compared to patients with high CHD5 expression in their tumors (53). Decreased expression of CHD5 is an unfavorable prognostic marker in patients with primary gallbladder carcinoma.
Prostate Cancer
Robbins conducted a comprehensive genomic survey for somatic events in metastatic prostate tumors using both high-resolution copy number analysis and targeted mutational survey of 3,508 exons from 577 cancer-related genes in eight tumors using next generation sequencing (54). Two novel missense mutations were identified in CHD5 (Table 1), but no copy number change of CHD5 was found in these tumors. However, two different missense mutations were found in two different samples (54). These studies indicate that deep genomic analysis of advanced metastatic prostate tumors can identify somatic alterations of genes that may contribute to aggressive prostate cancers, although no functional evidence was presented that CHD5 was a TSG in prostate cancer.
Conclusions
CHD5 was first identified as a new member of the CHD family and a candidate TSG deleted from 1p36 in neuroblastomas (1). Subsequent evidence showing suppression of clonigenicity and tumorigenicity, as well as correlation with risk factors and outcome, support its function as a TSG in this tumor (17, 34, 36, 37). Indeed, there is increasing evidence that CHD5 functions as a TSG in many other types of cancer, including cancers of the colon, breast, lung, and ovary, gliomas and others (Table 1). However, the pattern established in neuroblastoma is consistently seen in essentially all other tumor types, to the extent it has been studied: 1) one CHD5 allele is frequently lost by deletion; 2) the remaining CHD5 allele is rarely inactivated by mutation or structural rearrangement; 3) the CHD5 promoter is transcriptionally silenced by methylation or other epigenetic mechanisms; 4) CHD5 expression can be upregulated by exposure to demethylating agents, like 5-Aza; 5) transfection of tumor cells with a CHD5 expression inhibits tumor growth in vitro and in vivo; 6) low CHD5 expression is seen tumor tissue compared to adjacent normal tissue, and lower levels in high-risk versus low-risk tumors; 7) low CHD5 expression is associated with adverse risk factors and poor survival. Thus, CHD5 may be a master regulator, controlling cellular development, differentiation, proliferation, senescence and cell death for neuroblastomas and a variety of other tumors.
CHD5 likely functions as a part of a NuRD-type chromatin remodeling complex, but it is unknown if it has functions independent of this complex. CHD5-NuRD presumably functions predominantly as a transcriptional repressor, and it may also contribute to transcriptional activation, as well as transcript elongation, termination, RNA processing, and DNA damage response (4, 13). Nevertheless, as a nuclear protein, CHD5 may be a difficult target. Fortunately, the remaining allele in cases with 1p36 deletion is almost always intact, and it is usually silenced by promoter methylation, which is amenable to modification. The region that is methylated varies somewhat from one study to another, but the region between –400 and –800 bp from the CHD5 start site seemed most frequently involved (20, 34, 37, 46, 50, 52). Upregulation of CHD5 expression can be accomplished by exposure to 5-Aza or other demethylating agents, although there is no way to selectively target the CHD5 promoter. CHD5 expression may be repressed by transcription factors or miRNAs that may be more tractable as targets. Also, the targets of CHD5 transcriptional control are largely unknown, but they may be more easily druggable. Nevertheless, CHD5 has emerged as an important TSG that clearly plays a critical role in neuroblastomas, gliomas and a variety of other cancers.
Supplementary Material
Acknowledgments
This work was supported in part by National Institutes of Health grant CA039771, by Alex's Lemonade Stand Foundation, and the Audrey E. Evans Endowed Chair.
Abbreviations
- 5-Aza
5-aza-2’-deoxycytidine
- CHD
Chromodomain-Helicase-DNA binding
- NuRD
Nucleosome Remodeling and Deacetylation
- PHD
Plant Homology Domain
- SCC
squamous cell carcinoma
- TSG
Tumor Suppressor Gene
References
- 1.Thompson PM, Gotoh T, Kok M, White PS, Brodeur GM. CHD5, a new member of the chromodomain gene family, is preferentially expressed in the nervous system. Oncogene. 2003;22:1002–11. doi: 10.1038/sj.onc.1206211. [DOI] [PubMed] [Google Scholar]
- 2.Hall JA, Georgel PT. CHD proteins: a diverse family with strong ties. Biochemistry and cell biology = Biochimie et biologie cellulaire. 2007;85:463–76. doi: 10.1139/O07-063. [DOI] [PubMed] [Google Scholar]
- 3.Marfella CG, Imbalzano AN. The Chd family of chromatin remodelers. Mutat Res. 2007;618:30–40. doi: 10.1016/j.mrfmmm.2006.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stanley FK, Moore S, Goodarzi AA. CHD chromatin remodelling enzymes and the DNA damage response. Mutat Res. 2013 doi: 10.1016/j.mrfmmm.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Schuster EF, Stoger R. CHD5 defines a new subfamily of chromodomain-SWI2/SNF2-like helicases. Mamm Genome. 2002;13:117–9. doi: 10.1007/s00335-001-3042-6. [DOI] [PubMed] [Google Scholar]
- 6.Allen HF, Wade PA, Kutateladze TG. The NuRD architecture. Cellular and molecular life sciences : CMLS. 2013;70:3513–24. doi: 10.1007/s00018-012-1256-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai AY, Wade PA. Cancer biology and NuRD: a multifaceted chromatin remodelling complex. Nat Rev Cancer. 2011;11:588–96. doi: 10.1038/nrc3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Denslow SA, Wade PA. The human Mi-2/NuRD complex and gene regulation. Oncogene. 2007;26:5433–8. doi: 10.1038/sj.onc.1210611. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Ng HH, Erdjument-Bromage H, Tempst P, Bird A, Reinberg D. Analysis of the NuRD subunits reveals a histone deacetylase core complex and a connection with DNA methylation. Genes Dev. 1999;13:1924–35. doi: 10.1101/gad.13.15.1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xue Y, Wong J, Moreno GT, Young MK, Cote J, Wang W. NURD, a novel complex with both ATP-dependent chromatin-remodeling and histone deacetylase activities. Mol Cell. 1998;2:851–61. doi: 10.1016/s1097-2765(00)80299-3. [DOI] [PubMed] [Google Scholar]
- 11.Tong JK, Hassig CA, Schnitzler GR, Kingston RE, Schreiber SL. Chromatin deacetylation by an ATP-dependent nucleosome remodelling complex. Nature. 1998;395:917–21. doi: 10.1038/27699. [DOI] [PubMed] [Google Scholar]
- 12.Potts RC, Zhang P, Wurster AL, Precht P, Mughal MR, Wood WH, 3rd, Zhang Y, Becker KG, Mattson MP, Pazin MJ. CHD5, a Brain-Specific Paralog of Mi2 Chromatin Remodeling Enzymes, Regulates Expression of Neuronal Genes. PLoS One. 2011;6:e24515. doi: 10.1371/journal.pone.0024515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murawska M, Brehm A. CHD chromatin remodelers and the transcription cycle. Transcription. 2011;2:244–53. doi: 10.4161/trns.2.6.17840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oliver SS, Musselman CA, Srinivasan R, Svaren JP, Kutateladze TG, Denu JM. Multivalent recognition of histone tails by the PHD fingers of CHD5. Biochemistry. 2012;51:6534–44. doi: 10.1021/bi3006972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paul S, Kuo A, Schalch T, Vogel H, Joshua-Tor L, McCombie WR, Gozani O, Hammell M, Mills AA. Chd5 requires PHD-mediated histone 3 binding for tumor suppression. Cell Rep. 2013;3:92–102. doi: 10.1016/j.celrep.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Egan CM, Nyman U, Skotte J, Streubel G, Turner S, O'Connell DJ, Rraklli V, Dolan MJ, Chadderton N, Hansen K, Farrar GJ, Helin K, Holmberg J, Bracken AP. CHD5 Is Required for Neurogenesis and Has a Dual Role in Facilitating Gene Expression and Polycomb Gene Repression. Developmental cell. 2013;26:223–36. doi: 10.1016/j.devcel.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 17.Garcia I, Mayol G, Rodriguez E, Sunol M, Gershon TR, Rios J, Cheung NK, Kieran MW, George RE, Perez-Atayde AR, Casala C, Galvan P, de Torres C, Mora J, Lavarino C. Expression of the neuron-specific protein CHD5 is an independent marker of outcome in neuroblastoma. Mol Cancer. 2010;9:277. doi: 10.1186/1476-4598-9-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhuang T, Hess RA, Kolla V, Higashi M, Raabe TD, Brodeur GM. CHD5, a chromatin remodeling protein, is required for spermiogenesis and chromatin condensation. Mechanisms of Development. 2013 doi: 10.1016/j.mod.2013.10.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vestin A, Mills AA. The tumor suppressor Chd5 is induced during neuronal differentiation in the developing mouse brain. Gene expression patterns : GEP. 2013;13:482–9. doi: 10.1016/j.gep.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mulero-Navarro S, Esteller M. Chromatin remodeling factor CHD5 is silenced by promoter CpG island hypermethylation in human cancer. Epigenetics. 2008;3:210–5. doi: 10.4161/epi.3.4.6610. [DOI] [PubMed] [Google Scholar]
- 21.Mallette FA, Richard S. JMJD2A promotes cellular transformation by blocking cellular senescence through transcriptional repression of the tumor suppressor CHD5. Cell Rep. 2012;2:1233–43. doi: 10.1016/j.celrep.2012.09.033. [DOI] [PubMed] [Google Scholar]
- 22.Chen K, Rajewsky N. The evolution of gene regulation by transcription factors and microRNAs. Nature reviews Genetics. 2007;8:93–103. doi: 10.1038/nrg1990. [DOI] [PubMed] [Google Scholar]
- 23.Cai C, Ashktorab H, Pang X, Zhao Y, Sha W, Liu Y, Gu X. MicroRNA-211 expression promotes colorectal cancer cell growth in vitro and in vivo by targeting tumor suppressor CHD5. PLoS One. 2012;7:e29750. doi: 10.1371/journal.pone.0029750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bagchi A, Papazoglu C, Wu Y, Capurso D, Brodt M, Francis D, Bredel M, Vogel H, Mills AA. CHD5 is a tumor suppressor at human 1p36. Cell. 2007;128:459–75. doi: 10.1016/j.cell.2006.11.052. [DOI] [PubMed] [Google Scholar]
- 25.Brodeur GM. Neuroblastoma: biological insights into a clinical enigma. Nat Rev Cancer. 2003;3:203–16. doi: 10.1038/nrc1014. [DOI] [PubMed] [Google Scholar]
- 26.Brodeur GM, Hogarty MD, Mosse YP, Maris JM. Neuroblastoma. In: Pizzo PA, Poplack DG, editors. Principles and Practice of Pediatric Oncology. 6th ed. Lippincott, Williams and Wilkins; Philadelphia: 2011. pp. 886–922. [Google Scholar]
- 27.Brodeur GM, Sekhon G, Goldstein MN. Chromosomal aberrations in human neuroblastomas. Cancer. 1977;40:2256–63. doi: 10.1002/1097-0142(197711)40:5<2256::aid-cncr2820400536>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 28.Attiyeh EF, London WB, Mosse YP, Wang Q, Winter C, Khazi D, McGrady PW, Seeger RC, Look AT, Shimada H, Brodeur GM, Cohn SL, Matthay KK, Maris JM. Chromosome 1p and 11q deletions and outcome in neuroblastoma. N Engl J Med. 2005;353:2243–53. doi: 10.1056/NEJMoa052399. [DOI] [PubMed] [Google Scholar]
- 29.Brodeur GM, Green AA, Hayes FA, Williams KJ, Williams DL, Tsiatis AA. Cytogenetic features of human neuroblastomas and cell lines. Cancer Res. 1981;41:4678–86. [PubMed] [Google Scholar]
- 30.Fong CT, Dracopoli NC, White PS, Merrill PT, Griffith RC, Housman DE, Brodeur GM. Loss of heterozygosity for the short arm of chromosome 1 in human neuroblastomas: correlation with N-myc amplification. Proc Natl Acad Sci U S A. 1989;86:3753–7. doi: 10.1073/pnas.86.10.3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maris JM, White PS, Beltinger CP, Sulman EP, Castleberry RP, Shuster JJ, Look AT, Brodeur GM. Significance of chromosome 1p loss of heterozygosity in neuroblastoma. Cancer Res. 1995;55:4664–9. [PubMed] [Google Scholar]
- 32.White PS, Maris JM, Beltinger C, Sulman E, Marshall HN, Fujimori M, Kaufman BA, Biegel JA, Allen C, Hilliard C, et al. A region of consistent deletion in neuroblastoma maps within human chromosome 1p36.2-36.3. Proc Natl Acad Sci U S A. 1995;92:5520–4. doi: 10.1073/pnas.92.12.5520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.White PS, Thompson PM, Gotoh T, Okawa ER, Igarashi J, Kok M, Winter C, Gregory SG, Hogarty MD, Maris JM, Brodeur GM. Definition and characterization of a region of 1p36.3 consistently deleted in neuroblastoma. Oncogene. 2005;24:2684–94. doi: 10.1038/sj.onc.1208306. [DOI] [PubMed] [Google Scholar]
- 34.Fujita T, Igarashi J, Okawa ER, Gotoh T, Manne J, Kolla V, Kim J, Zhao H, Pawel BR, London WB, Maris JM, White PS, Brodeur GM. CHD5, a tumor suppressor gene deleted from 1p36.31 in neuroblastomas. J Natl Cancer Inst. 2008;100:940–9. doi: 10.1093/jnci/djn176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Okawa ER, Gotoh T, Manne J, Igarashi J, Fujita T, Silverman KA, Xhao H, Mosse YP, White PS, Brodeur GM. Expression and sequence analysis of candidates for the 1p36.31 tumor suppressor gene deleted in neuroblastomas. Oncogene. 2008;27:803–10. doi: 10.1038/sj.onc.1210675. [DOI] [PubMed] [Google Scholar]
- 36.Garcia I, Mayol G, Rios J, Domenech G, Cheung NK, Oberthuer A, Fischer M, Maris JM, Brodeur GM, Hero B, Rodriguez E, Sunol M, Galvan P, de Torres C, Mora J, Lavarino C. A three-gene expression signature model for risk stratification of patients with neuroblastoma. Clin Cancer Res. 2012;18:2012–23. doi: 10.1158/1078-0432.CCR-11-2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koyama H, Zhuang T, Light JE, Kolla V, Higashi M, McGrady PW, London WB, Brodeur GM. Mechanisms of CHD5 Inactivation in neuroblastomas. Clin Cancer Res. 2012;18:1588–97. doi: 10.1158/1078-0432.CCR-11-2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brodeur GM, Iyer R, Croucher JL, Zhuang T, Higashi M, Kolla V. Therapeutic targets in neuroblastomas. Expert Opin:Ther Targets. 2013 doi: 10.1517/14728222.2014.867946. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Henrich KO, Schwab M, Westermann F. 1p36 tumor suppression--a matter of dosage? Cancer Res. 2012;72:6079–88. doi: 10.1158/0008-5472.CAN-12-2230. [DOI] [PubMed] [Google Scholar]
- 40.Law ME, Templeton KL, Kitange G, Smith J, Misra A, Feuerstein BG, Jenkins RB. Molecular cytogenetic analysis of chromosomes 1 and 19 in glioma cell lines. Cancer Genet Cytogenet. 2005;160:1–14. doi: 10.1016/j.cancergencyto.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 41.Wang L, He S, Tu Y, Ji P, Zong J, Zhang J, Feng F, Zhao J, Gao G, Zhang Y. Downregulation of chromatin remodeling factor CHD5 is associated with a poor prognosis in human glioma. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2013;20:958–63. doi: 10.1016/j.jocn.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 42.Ragnarsson G, Eiriksdottir G, Johannsdottir JT, Jonasson JG, Egilsson V, Ingvarsson S. Loss of heterozygosity at chromosome 1p in different solid human tumours: association with survival. Br J Cancer. 1999;79:1468–74. doi: 10.1038/sj.bjc.6690234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mokarram P, Kumar K, Brim H, Naghibalhossaini F, Saberi-firoozi M, Nouraie M, Green R, Lee E, Smoot DT, Ashktorab H. Distinct high-profile methylated genes in colorectal cancer. PLoS One. 2009;4:e7012. doi: 10.1371/journal.pone.0007012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fatemi M, Paul TA, Brodeur GM, Shokrani B, Brim H, Ashktorab H. Epigenetic silencing of CHD5, a novel tumor-suppressor gene, occurs in early colorectal cancer stages. Cancer. 2013 doi: 10.1002/cncr.28316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu X, Zhu Z, Li W, Fu X, Su D, Fu L, Zhang Z, Luo A, Sun X, Fu L, Dong JT. Chromodomain helicase DNA binding protein 5 plays a tumor suppressor role in human breast cancer. Breast cancer research : BCR. 2012;14:R73. doi: 10.1186/bcr3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao R, Yan Q, Lv J, Huang H, Zheng W, Zhang B, Ma W. CHD5, a tumor suppressor that is epigenetically silenced in lung cancer. Lung Cancer. 2012;76:324–31. doi: 10.1016/j.lungcan.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 47.Gorringe KL, Choong DY, Williams LH, Ramakrishna M, Sridhar A, Qiu W, Bearfoot JL, Campbell IG. Mutation and methylation analysis of the chromodomain-helicase-DNA binding 5 gene in ovarian cancer. Neoplasia. 2008;10:1253–8. doi: 10.1593/neo.08718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sjoblom T, Jones S, Wood LD, Parsons DW, Lin J, Barber TD, Mandelker D, Leary RJ, Ptak J, Silliman N, Szabo S, Buckhaults P, Farrell C, Meeh P, Markowitz SD, Willis J, Dawson D, Willson JK, Gazdar AF, Hartigan J, Wu L, Liu C, Parmigiani G, Park BH, Bachman KE, Papadopoulos N, Vogelstein B, Kinzler KW, Velculescu VE. The consensus coding sequences of human breast and colorectal cancers. Science. 2006;314:268–74. doi: 10.1126/science.1133427. [DOI] [PubMed] [Google Scholar]
- 49.Wong RR, Chan LK, Tsang TP, Lee CW, Cheung TH, Yim SF, Siu NS, Lee SN, Yu MY, Chim SS, Wong YF, Chung TK. CHD5 Downregulation Associated with Poor Prognosis in Epithelial Ovarian Cancer. Gynecol Obstet Invest. 2011 doi: 10.1159/000323883. [DOI] [PubMed] [Google Scholar]
- 50.Wang X, Lau KK, So LK, Lam YW. CHD5 is down-regulated through promoter hypermethylation in gastric cancer. J Biomed Sci. 2009;16:95. doi: 10.1186/1423-0127-16-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Qu Y, Dang S, Hou P. Gene methylation in gastric cancer. Clin Chim Acta. 2013;424:53–65. doi: 10.1016/j.cca.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 52.Wang J, Chen H, Fu S, Xu ZM, Sun KL, Fu WN. The involvement of CHD5 hypermethylation in laryngeal squamous cell carcinoma. Oral Oncol. 2011;47:601–8. doi: 10.1016/j.oraloncology.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 53.Du X, Wu T, Lu J, Zang L, Song N, Yang T, Zhao H, Wang S. Decreased expression of chromodomain helicase DNA-binding protein 5 is an unfavorable prognostic marker in patients with primary gallbladder carcinoma. Clinical & translational oncology : official publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico. 2012 doi: 10.1007/s12094-012-0903-2. [DOI] [PubMed] [Google Scholar]
- 54.Robbins CM, Tembe WA, Baker A, Sinari S, Moses TY, Beckstrom-Sternberg S, Beckstrom-Sternberg J, Barrett M, Long J, Chinnaiyan A, Lowey J, Suh E, Pearson JV, Craig DW, Agus DB, Pienta KJ, Carpten JD. Copy number and targeted mutational analysis reveals novel somatic events in metastatic prostate tumors. Genome Res. 2011;21:47–55. doi: 10.1101/gr.107961.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.