Abstract
We examined within-individual changes in emotion dysregulation over the course of one year as a maintenance factor of borderline personality disorder (BPD) features. We evaluated the extent to which (1) BPD symptom severity at baseline predicted within-individual changes in emotion dysregulation and (2) within-individual changes in emotion dysregulation predicted four BPD features at 12-month follow-up: affective instability, identity disturbances, negative relationships, and impulsivity. The specificity of emotion dysregulation as a maintaining mechanism of BPD features was examined by controlling for a competing intervening variable, interpersonal conflict. BPD symptoms at baseline predicted overall level and increasing emotion dysregulation. Additionally, increasing emotion dysregulation predicted all four BPD features at 12-month follow-up after controlling for BPD symptoms at baseline. Further, overall level of emotion dysregulation mediated the association between BPD symptom severity at baseline and both affective instability and identity disturbance at 12-month follow-up, consistent with the notion of emotion dysregulation as a maintenance factor. Future research on the malleability of emotion dysregulation in laboratory paradigms and its effects on short-term changes in BPD features is needed to inform interventions.
Keywords: borderline personality disorder, emotion dysregulation, maintenance mechanisms
Recent findings from longitudinal studies of patients with borderline personality disorder (BPD) have challenged commonly held conceptions regarding the long-term stability and chronic nature of this illness. Specifically, findings from the Collaborative Longitudinal Personality Disorders Study (CLPS) and the McLean Study of Adult Development (MSAD) revealed that approximately 85–90% of patients with BPD experienced symptom remission within a 10-year period [1–2]. The rate of BPD relapse was quite low over this extended period as well. However, these studies have also documented sustained levels of impairment in this population, which resulted in more modest rates of full recovery [1] [3] [2]. These studies highlight the need to think longitudinally about the course of BPD and to consider factors that may facilitate or impede individuals moving across different stages of the illness, including onset, maintenance, remission, recovery, and relapse. For instance, situational changes, such as garnering more stable social support, or remissions of co-occurring Axis I disorders were shown to predict rapid and full recovery among some patients with BPD [4].
The identification of maintenance mechanisms is critical for developing and refining interventions as these are the processes that impede individuals from moving from onset to remission or from remission to recovery, for example. We posit that emotion dysregulation is one mechanism that maintains BPD features over time. Although there is no consensus on the definition of emotion dysregulation, we define emotion dysregulation as deficits in the ability to modulate the experience and expression of emotions and to maintain goal directed behavior in the presence of intense negative affect [5]. Thus, we conceptualize emotion dysregulation as distinct from negative affect or variability in affect. This conceptual distinction is important because emotion dysregulation reflects strategies and processes in the face of emotion rather than merely symptoms that define psychopathology. Emotion dysregulation has also been prospectively linked to increases in internalizing and externalizing psychopathology over a seven-month window in adolescents [6], highlighting the role of emotion dysregulation as driving increases in psychopathology over time.
Emotion dysregulation is hypothesized by several theorists to play a central role in the etiology and development of BPD [7–10], giving rise to affective instability (defined as marked intensity, reactivity, and variability of moods; [11]) as well as other symptoms of the disorder such as identity disturbance, interpersonal dysfunction, and self-harm. According to these theoretical models, transactions between an individual’s innate biological disposition toward intense emotional reactivity and invalidating environmental inputs contribute to deficits in the acquisition of effective skills for regulating these intense emotional experiences. In turn, deficits in emotion regulation capacities contribute to even more intense and variable affects (i.e., affective instability) and dysregulated cognitions, behaviors, and interpersonal relations. Given the theorized role of emotion dysregulation in the developmental psychopathology of BPD, deficits in the ability to effectively cope with and modulate affect may also serve to maintain features of the disorder over time.
From the view of emotion dysregulation as a maintenance mechanism, once BPD emerges, emotion dysregulation may sustain BPD symptoms and associated problematic behaviors, which is consistent with several studies illustrating a link between dysregulated emotion and behavior [12–14]. For instance, in a sample of college students, the relationship between BPD and dysregulated behavior (reassurance seeking, binge-eating, and alcohol use) was mediated by rumination, anger rumination, catastrophizing, and brooding, even after controlling for depression [12]. Additionally, in the natural environment, rumination and intense negative affect predicted engaging in dysregulated behavior within 2–3 hours [14]. Emerging evidence also suggests that emotion dysregulation is associated with interpersonal dysregulation. For instance, a cross-sectional study demonstrated that emotion dysregulation fully mediated the association between BPD and interpersonal problems [5]. In a recent prospective study, emotion dysregulation mediated the relationship between BPD symptoms at baseline and aggressive behavior over the course of a year.
A number of studies also support a link between emotion dysregulation and non-suicidal self-injury or suicide behaviors. Additionally, several studies have found that individuals who engage in non-suicidal self-injury report higher levels of emotion dysregulation [16–20]. Across two treatment trials, within-individual improvements in emotion regulation predicted decreases in non-suicidal self-injury over the course of 14 weeks [21], further supporting the notion that emotion dysregulation maintains non-suicidal self-injury.
Although the link between emotion dysregulation and dysregulated behaviors has been examined generally as well as for individuals with BPD, the role of emotion dysregulation in maintaining other BPD features, such as affective instability and identity problems, has not yet been examined. Additionally, most studies have relied on cross-sectional reports [8] [12] [13] or short prospective studies [14] [22]. Hence, within-individual changes, or increases in emotion dysregulation over time, as a maintenance factor for BPD features has yet to be determined. Finally, it is not clear whether emotion dysregulation has a unique association with the maintenance of BPD features or if this relationship could be accounted for by other variables that are linked to BPD and emotion dysregulation, such as interpersonal conflict [23] [15] [24].
The overall goal of this study was to examine emotion dysregulation (i.e., difficulties with emotion regulation) as a maintenance factor for BPD features over the course of one year. Specifically, we expected that the trajectory of emotion dysregulation over one year would predict BPD features even after controlling for BPD symptom severity and other emotion constructs at baseline, specifically angry rumination and depression. Additionally, we expected the relationship between within-individual changes in emotion dysregulation and BPD features to hold even after controlling for within-individual changes in interpersonal conflict over the course of the year. Our specific questions for the current study are as follows:
What are the patterns of growth (within-individual changes) in difficulties in emotion regulation over the course of one year?
Does BPD symptom severity predict growth over the course of one year in emotion dysregulation even after controlling for depression, angry rumination and demographic characteristics?
Do within-person changes in emotion dysregulation account for the maintenance of BPD features over the course of one year? That is, does growth in emotion dysregulation over one year mediate the relation between BPD symptom severity at baseline and BPD features (i.e., affective instability, identity problems, negative relationships, and self harm) one year later? Further, is mediation specific to emotion dysregulation, or can within-person changes in another core problem associated with BPD (specifically, interpersonal conflict) also mediate these associations?
Method
Sample Description
The study sample (N = 150) was comprised of individuals from both psychiatric clinics and the community representing the full range of BPD features. Patients (n = 75) were solicited from general adult outpatient psychiatric clinics and were active in treatment at the time of participation in this study. The community sample (n = 75) was recruited by telephone through the use of a random digit dialing (RDD) method coordinated by the University Center for Social and Urban Research at the University of Pittsburgh. RDD was utilized to yield a probability sample representative of demographic characteristics reflected in the U.S. census for the Pittsburgh metropolitan area with oversampling of African Americans to ensure accurate racial minority representation. Participants with psychotic disorders, organic mental disorders, mental retardation, and major medical illnesses that influence the central nervous system were excluded. At screening, participants were between the ages of 21 and 60.
To capture the full range of BPD features, potential participants were screened using the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD; [25]), a self-report questionnaire that has demonstrated good sensitivity (0.81) and specificity (.85) for BPD diagnosis [25]. We recruited participants into three strata based on the number of criteria endorsed: 0–2, 3–4, or 5 or more. The majority of participants endorsed 0–2 BPD criteria (66.7%, n=100), 16% endorsed 3–4 criteria, and 17.3% (n = 26) endorsed 5 or more criteria. Not surprisingly, the patient sample endorsed higher levels of BPD features (53.3% of patients vs. 13.3% of community participants endorsed 3 or more criteria; χ2(1) = 38.23, p < .001). Thus, we controlled for referral group status (0 = community participant, 1 = psychiatric patient participant) in analyses.
The mean age of the sample was 45 years (SD = 10.43) and 97 participants (64.7%) were female. Eighty-six participants (57.3%) identified as Caucasian, 57 (38.0%) as African American, 6 (4.0%) as more than one race, and 1 (0.7%) as Asian. Four participants (2.7%) identified their ethnicity as Hispanic. In terms of marital status, 68 participants (45.3%) were single and never married, 47 (31.4%) were married or in a long-term committed relationship, 33 (22.0%) were separated or divorced, and 2 (1.3%) were widowed. A large majority of the sample obtained education beyond high school (n = 109; 80.4% with at least some vocational or college training), but the majority of the sample was unemployed (n = 84; 56.0%).
Procedure
All participants were interviewed by trained research staff with a minimum of a master’s degree in social work or clinical psychology and at least five years of assessment/clinical experience. All interviewers were blind to the participant’s cell assignment (i.e., community or patient status and MSI-BPD score). Relevant for this study, during the baseline assessment, interviewers administered the Structured Interview for DSM-IV Personality (SIDP-IV; [26]), and the Hamilton Rating Scale for Depression (HAM-D; [27]). Participants completed self-report questionnaires at baseline and 3 month intervals for one year. All study procedures were approved by the University of Pittsburgh Institutional Review Board, and participants participated with informed, voluntary, written consent.
Measures
BPD symptoms and features
The SIDP-IV rates each DSM-IV criterion on a four-point scale (0 = absent, 1 = subthreshold, 2 = threshold, 3 = strongly present). BPD symptom severity scores were calculated by summing the 9 BPD criteria ratings from the baseline assessment. To calculate interrater reliability, 15 cases were randomly selected and rated by four judges. The internal consistency was deemed adequate (ICC = .80).
At the 12-month follow-up visit, participants completed the Personality Assessment Inventory – Borderline Features Scale (PAI-BOR; [28]), which contains 24 items rated on a four-point scale (0 = false to 3 = very true). The PAI-BOR contains four subscales that tap core features of BPD: affective instability, identity problems, negative relationships, and self harm. The self harm subscale taps impulsivity and impulsive behaviors more broadly and is not limited to self harm behaviors. Each subscale contains 6 items (e.g., “My attitude about myself changes a lot” and “My relationships have been stormy”). Elevations on these subscales have been identified as markers for a diagnosis of BPD in clinical samples [28]. In the current sample, the internal consistencies of the four subscales ranged from .77 to .84 for negative relationships and identity problems, respectively.
Emotion dysregulation
Participants completed the Difficulties in Emotion Regulation Scale (DERS; [29]) at baseline and at all follow-up appointments (3-, 6-, 9-, and 12-months). The DERS is a 36 item self-report measure that assesses difficulties relating to nonacceptance of emotional responses, difficulties engaging in goal-directed behavior due to emotional responses, impulse control difficulties due to emotional responses, lack of emotional awareness, and lack of emotional clarity in the past 3 months (e.g., “I experience my emotions as overwhelming and out of control” and “When I’m upset, it takes me a long time to feel better”). Each item is rated on a five-point scale (1 = never to 4 = most of the time). Items were summed to create a measure of emotion dysregulation. The mean at baseline was 86.83 (SD = 27.12). Across the follow-up assessments, the mean ranged from 80.69 (SD = 24.73) at the 12-month follow-up to 83.60 (SD = 27.07) at the 6-month follow-up assessment. In the current sample, the internal consistency for the DERS at each study time point was .96.
Interpersonal conflict
Participants completed the Revised Conflict Tactics Scale (CTS2; [30]), at all study time points. The CTS2 contained 40 items that assessed the frequency of aggression and victimization involving anyone (not just romantic partners) in the past five years (at baseline) and the past 3 months (at follow-up visits). The types of experiences measured included psychological aggression perpetration and victimization as well as physical assault perpetration and victimization (e.g., “Did anyone insult or swear at you?” and “Did you throw something at anyone that could have hurt?”). All items are rated on a 7-point scale (0 = 0 times to 6 = 21 or more times). Interpersonal conflict was measured by summing the frequency ratings. The mean at baseline was 27.98 (SD = 24.45). The mean at follow-ups ranged from 5.53 (SD = 8.72) at the 12-month follow-up to 6.74 (SD = 11.36) at the 9-month follow-up. In the current sample, the mean internal consistency for the CTS2 was .88, ranging from .84 to .92 for the 3-month follow-up and baseline assessment, respectively.
Emotion/mood covariates
In order to examine the specific relation between BPD features and difficulties regulating emotions, we controlled for potential confounds of this relationship at baseline. Specifically, we wanted to differentiate between constructs reflecting general negative affectivity (operationalized as depression and anger rumination) at baseline and difficulties regulating emotions as a process over time. Depression at baseline was assessed via clinician ratings on the HAM-D, which contained 20 items rated on a 5 point scale (0 = not present to 4 = very severe), including items related to depressed mood and suicide. To calculate interrater reliability, 5 cases were randomly selected and rated by five judges. The internal consistency was .93.
Anger rumination was measured at baseline by the Anger Rumination Scale (ARS; [31]). The scale contains 19 items (e.g., “I re-enact the anger episode in my mind after it has happened;” “Whenever I experience anger, I keep thinking about it for a while”) scored on a four-point scale (1 = almost never to 4 = almost always) and the mean of item responses was calculated. In the current sample, the internal consistency was .95.
Data Analytic Plan
We first examined descriptive statistics and intercorrelations between all study variables (Table 1). Next, we fit a series of unconditional latent growth curve models (LGCMs) to determine the form of growth across the year-long assessment window (i.e., 5 assessment points) in emotion dysregulation and interpersonal conflict as well as examining growth in the dual processes simultaneously. Next, we examined a conditional dual LGCM in which predictors of these trajectories were examined. These conditional models also included BPD features (i.e., affective instability, identity disturbances, negative relationships, and self harm) at the one year follow-up in order to test whether within-individual changes in emotion regulation difficulties predicted BPD features at the one-year follow-up even after controlling for within-individual change in interpersonal conflict. We tested the indirect effects of BPD symptom severity at baseline to the 12-month follow-up assessment via within-individual changes (i.e., latent intercept and slope factors) of emotion regulation difficulties and interpersonal conflict over the course of one year. The tests of indirect effects allowed us to examine whether emotion regulation difficulties were distinctive as maintenance mechanisms of BPD features over the course of one year.
Table 1.
Descriptive Statistics and Correlations Between Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | |||||||||||||
| 1. Age | |||||||||||||
| 2. Race (1=Minority) | −.04 | ||||||||||||
| 3. Gender (1=Female) | −.11 | .02 | |||||||||||
| 4. Group (1=Patient) | −.16* | .00 | .04 | ||||||||||
| 5. Depression | −.11 | .20* | .09 | .45*** | |||||||||
| 6. Angry rumination | −.10 | .12 | −.05 | .45*** | .53*** | ||||||||
| 7. BPD Symptom Severity | −.17* | .08 | .14 | .40*** | .55*** | .55*** | |||||||
| 8. Emotion Dysregulation | −.11 | −.05 | .01 | .60*** | .65*** | .73*** | .58*** | ||||||
| 9. Interpersonal Conflict | −.21*** | .05 | −.004 | .11 | .25** | .21* | .30*** | .35*** | |||||
| BPD features at 12-month follow-up | |||||||||||||
| 10. Affective instability | −.28*** | −.11 | −.02 | .49*** | .51*** | .64*** | .52*** | .67** | .35*** | ||||
| 11. Identity disturbance | −.26*** | −.06 | <.001 | .48*** | .57*** | .58*** | .57*** | .67*** | .36*** | .77*** | |||
| 12. Negative relationships | −.22** | .10 | −.10 | .37*** | .58*** | .55*** | .54*** | .58*** | .42*** | .71*** | .73*** | ||
| 13. Self harm | −.18* | .05 | −.09 | .38*** | .43*** | .38*** | .51*** | .48*** | .41*** | .55*** | .64*** | .57*** | |
|
| |||||||||||||
| Mean/% | 44.85 | 42.70% | 64.70% | 50% | 15.11 | 2.02 | 2.61 | 86.83 | 6.49 | 7.61 | 7.32 | 8.17 | 4.70 |
| Standard Deviation | 10.43 | -- | -- | -- | 8.91 | 0.67 | 3.29 | 27.12 | 8.72 | 4.27 | 4.68 | 4.13 | 3.64 |
To handle non-normal distributions of study variables we used a robust maximum likelihood estimator [32]. Missing data on dependent variables was handled through the use of the expectation maximization (EM) algorithm. We used the percentile bootstrap to test for indirect effects as this method is recommended for testing mediation with small samples, n < 500 [33]. All models were estimated with Mplus 7.0 [34]. Model fit was evaluated using the χ2 goodness of fit test, comparative fit index (CFI), Tucker-Lewis index (TLI), and root-mean-square error of approximation (RMSEA). For CFI and TLI, we used the conventional cutoff ≥.90 for acceptable fit, and ≥.95 for good fit. RMSEA values between .05–.08 represent acceptable fit, while values <.05 indicate good fit [35].
Finally, we tested interactions between demographic characteristics (i.e., gender, age, race, and group [community or clinic]) and BPD symptoms predicting within-individual changes in emotion dysregulation and interpersonal conflict over the course of one year. Additionally, we tested interactions between these demographic characteristics and BPD symptoms predicting BPD features at the 12-month follow-up visit. None of the interactions significantly predicted any of these outcomes, indicating that these characteristics do not moderate any of our findings.
Results
Question 1: Creating Latent Growth Curve Models
For emotion dysregulation and interpersonal conflict, we first fit linear models, quadratic model, and growth models with free time scores to determine the form of growth over the year-long assessment window. Since these models were not nested, we compared fit by examining the match between the model estimated growth and the observed means of scores at each assessment point as well as examining modification indices (c.f. [36]). To disentangle the overall level of emotion dysregulation from baseline measures, the intercept was fixed to the 6-month follow-up visit. The 3-month follow-up score was freed, indicating that the rate of change was not constant over all time points. Thus, the resulting mean of the slope factors for these scores can be interpreted as the rate of change for a time score change of one (rather than as the mean of the slope growth factor). No other changes to the unconditional models resulted in a change in the interpretation of the within-individual factor scores (Table 2).
Table 2.
Overall Model Fit and Growth Factors for the Unconditional Growth Models
| χ2 (df) | RMSEA (90% CI) | CFI/TLI | Intercept (6 months) | Slope (Across one year) | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean | Variance | Mean | Variance | ||||
| 1. Emotion dysregulation | 10.64 (9) | .03 (.00, .10) | 1.00/1.00 | 84.05*** | 612.22*** | −1.94*** | 20.21** |
| 2. Interpersonal conflict | 4.05 (5) | .00 (.00, .10) | 1.00/1.00 | 6.12*** | 53.86*** | −.33 | 4.59 * |
| Dual process | 23.61 (26) | .00 (.00, .06) | 1.00/1.00 | ||||
|
|
|||||||
| Process 1. | 84.07*** | 612.98*** | −1.94*** | 19.38** | |||
| Process 2. | 6.12*** | 52.62*** | −.34 | 4.27* | |||
Notes. All intercept and slope values are unstandardized. For emotion dysregulation, the 3-month time score were freely estimated so the interpretation for the slope mean is the rate of change for a time score change of one.
p ≤ .05;
p ≤ .01,
p ≤ .001.
RMSEA=Root Mean Square Error of Approximation; CFI = Comparative Fit Index; TLI=Tucker Lewis Index.
In order to test the specificity of emotion dysregulation as a maintenance factor, we also modeled the growth of interpersonal conflict. For interpersonal conflict, it was necessary for model convergence to exclude the baseline assessment from the model. This may be due to the baseline assessment representing interpersonal conflict over the past five years compared to the much shorter past three-month intervals of the remaining interpersonal conflict assessments. Again, the intercept was fixed to the 6-month follow-up. A linear growth process was retained as the final model (Table 2).
All unconditional LGCMs fit the data well (Table 2). Emotion dysregulation decreased slightly over the course of one year. However, the overall rate of change in interpersonal conflict was not significant, illustrating that, on average, these scores remained relatively constant over the course of one year. All random effects (variance components) for the intercept factors were significant, highlighting the individual variability in emotion regulation difficulties and interpersonal conflict in the overall level (intercept). Variances for both slope factors were also significant, indicating individual variability in trajectories (slope) over time for these scales.
For the dual process LGCM, the emotion dysregulation and interpersonal conflict LGCMs were simultaneously examined. The within time-point residuals across the two processes were allowed to freely co-vary (emotion dysregulation with interpersonal conflict at 6 month follow-up; emotion dysregulation with interpersonal conflict at 9 month follow-up; etc.). The final model fit the data very well (Table 2). The intercepts across the two processes were moderately correlated (r = .45, p < .001), suggesting that individuals with emotion dysregulation also have problems with interpersonal conflict. The slopes were not significantly related with each other or with intercept factors, suggesting that within-individual changes in one process were not related to changes in the other and that overall level of one process did not influence the rate of change in the other process.
Questions 2 and 3: Conditioned Latent Growth Curve Models
We examined Questions 2 and 3 simultaneously; that is, all covariates, predictors, and outcomes were simultaneously entered into the dual LGCM of emotion dysregulation and interpersonal conflict (c.f. Figure 1). By including the covariates, predictors, and outcomes simultaneously, we tested for the indirect effects (maintenance effects) of baseline BPD symptom severity on BPD features one year later via the emotion dysregulation and interpersonal conflict latent growth curve intercept and slope factors (within-individual changes). These models were adjusted for age, gender, race, group, depression, and angry rumination.
Figure 1.
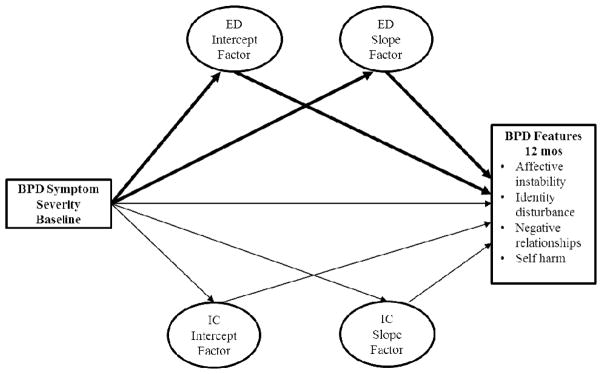
A path diagram of the conditional latent variable growth model of lack of emotion dysregulation as a unique maintenance factor of borderline personality disorder features (BPD features) from baseline to the 12-month follow-up assessment. Baseline age, race, gender, recruitment group, depression, and angry rumination were also controlled for in this model. For ease of presentation only the latent factors of the growth models are depicted. Additionally, each feature was modeled as a manifest variable (i.e., four outcome variables). The bold arrows indicate expected significant indirect paths from BPD symptom severity at baseline to the 12 month follow-up assessment via within-individual patterns of emotion dysregulation over the course of 12 months. ED = emotion dysregulation; IC = interpersonal conflict.
We examined the unique effects of age, race, gender, group, depression, angry rumination and BPD features at baseline on our latent growth factors of emotion dysregulation and interpersonal conflict (Table 3A). Age was related to the interpersonal conflict intercept factor (β = -.16, p < .05), indicating that younger individuals reported more overall difficulties with interpersonal conflict at three-month follow-up. No other predictors were related to the intercept or slope factors of interpersonal conflict.
Table 3.
Latent Growth Factors of Emotion Dysregulation as Unique Factors Predicting BPD Features
| Part 3A. Latent growth factors regressed on baseline BPD symptom severity and covariates
| ||||
|---|---|---|---|---|
| Emotion dysregulation | Interpersonal conflict | |||
|
| ||||
| Intercept | Slope | Intercept | Slope | |
| Baseline Predictors | ||||
| Age | −.01 | −.07 | −.16* | .10 |
| Race | −.20*** | −.06 | −.04 | −.01 |
| Gender | −.02 | −.05 | −.04 | −.06 |
| Group | .21*** | −.14 | −.05 | .09 |
| Depression | .28*** | −.33** | .16 | −.03 |
| Angry rumination | .40*** | −.22 | .14 | .11 |
| BPD Symptom Severity | .19** | .26* | .17 | −.16 |
| Part 3B. BPD features at one-year follow-up regressed on baseline predictors and latent growth factors
| ||||
|---|---|---|---|---|
| Affective instability | Identity disturbances | Negative relationships | Self harm | |
| Baseline Predictors | ||||
| Age | −.14** | −.13* | −.08 | −.03 |
| Race | −.10* | −.05 | .03 | .05 |
| Gender | −.01 | −.02 | −.13* | −.14* |
| Group | .11* | .08 | .03 | .16 |
| Depression | .16* | .20** | .32*** | .13 |
| Angry rumination | .31*** | .10 | .18 | −.04 |
| BPD Symptom Severity | −.06 | .06 | .10 | .19* |
| Growth factors | ||||
| Emotion Dysregulation | ||||
| Intercept | .45*** | .49*** | .18 | .24 |
| Slope | .34*** | .24** | .21* | .21* |
| Interpersonal Conflict | ||||
| Intercept | .09 | .09 | .18* | .22** |
| Slope | .01 | .07 | −.09 | −.15 |
Notes. Estimates are standardized regression coefficients (β’s).
p<.05;
p<.01;
p<.001.
Fit statistics for final model: χ2(84) = 117.02.
*** RMSEA = .05; CFI = .98; TLI = .96.
More associations were revealed between predictors and within-individual changes of emotion dysregulation. Minority race was negatively associated with the emotion dysregulation intercept factor (β = −.20, p < .001), indicating that Caucasians had higher levels of many emotion regulation difficulties at baseline. Psychiatric group status, depression, and angry rumination were positively associated with the intercept factors of emotion dysregulation (β’s = .21, .28, .40, p’s < .001, respectively), indicating that individuals in psychiatric treatment, and those with higher levels of depression and angry rumination had higher overall levels of emotion dysregulation. Out of the covariates, only depression significantly predicted the slope of emotion dysregulation, (β = −.33, p < .05), indicating that those with higher baseline depression experienced faster rates of emotion dysregulation improvement over the course of one year. Most importantly, after controlling for all covariates, BPD symptom severity at baseline was related to emotion dysregulation intercept and slope factors (β = .19, p < .01; β = 26, p < .05, respectively), indicating that those with more severe BPD symptoms at baseline experienced higher levels of emotion dysregulation as well as increases in these difficulties over the course of one year.
To examine whether within-individual changes in emotion dysregulation maintained BPD features one year later, all PAI-BOR subscales (i.e., affective instability, identity disturbances, negative relationships, and self harm) at the 12-month follow-up was regressed simultaneously on the latent variable growth factors and all covariates (Table 3B). BPD symptom severity at baseline only predicted self harm at the one-year follow-up (β = .19, p < .05). Further, emotion dysregulation factors (intercepts and slopes) predicted BPD features at the 12-month follow-up, indicating that within-individual levels and changes in emotion dysregulation are important predictors of these features. Specifically, the emotion dysregulation intercept and slope factors predicted affective instability (β = .45, p < .001 and β = .34, p < .001, respectively) and identity disturbance (β = .49, p < .001 and β = .24, p < .001, respectively), indicating that level and growth (increasing difficulties) in emotion dysregulation predict affective instability and identity problems. Only the slope factor predicted negative relationships (β = .21, p < .05) and self harm (β = .27, p < .05), indicating that increasing difficulties in emotion regulation over the course of one year, but not higher overall levels, are predictive of interpersonal difficulties and impulse control problems. In contrast, only the intercept factor of interpersonal conflict predicted negative relationships (β = .18, p < .05) and Self harm (β = .22, p < .01), indicating that overall level of interpersonal conflict, but not changes (increases) in interpersonal conflict, is predictive of interpersonal difficulties and impulse control problems.
Lastly, to test whether within-individual changes in emotion regulation difficulties uniquely maintained BPD features over the course of one year, we examined the indirect effects of BPD features at the 12 month-follow-up regressed on BPD features at baseline via the intercepts and slopes of emotion dysregulation and interpersonal conflict even after controlling for demographic features, depression, and angry rumination at baseline. There was a significant indirect effect through the emotion dysregulation intercept factor for affective instability (β = .08, p < .05; 95% CI [.02, .15]) and identity disturbance (β = .09, p < .05; 95% CI [.01, .16]), indicating that higher overall level of emotion dysregulation accounted for the stability of these BPD features over the course of one year. There were no significant indirect effects of interpersonal conflict, suggesting that within-individual changes in interpersonal conflict do not significantly maintain BPD features over the course of one year after controlling for emotion dysregulation.
Discussion
The current study examined within-individual changes in emotion dysregulation as a maintenance factor of BPD features over the course of one year in a sample enriched with BPD symptoms. Results demonstrated that, on average, emotion dysregulation decreased slightly over the course of the year. However, after controlling for demographic characteristics, depression, and angry rumination, BPD symptom severity at baseline predicted higher overall levels and increases in emotion dysregulation over time. Further, increases in emotion dysregulation over the year predicted greater BPD features (i.e., affective instability, identity problems, negative relationships, and self harm) at 12-month follow-up, even after controlling for concurrent changes in interpersonal conflict. Our analyses demonstrated the overall level of emotion dysregulation difficulties fully mediated the association between BPD symptom severity at baseline and both affective instability and identity disturbance at 12-month follow-up, suggesting that emotion dysregulation accounted for the stability of these features over the course of one year. Our results extend previous work that has found rumination and other aspects of emotion dysregulation to be related to hallmark behavioral problems in this population [20] [12] [14]. These findings also expand on our conceptualization of emotion dysregulation as an underlying factor of the disorder to a maintenance mechanism.
Although the rate of change in emotion dysregulation predicted all four categories of BPD features at follow-up (i.e., affective instability, identity disturbance, negative relationships, and self harm), the overall level of emotion dysregulation only predicted affective instability and identify disturbance. Thus, as compared to overall levels of emotion dysregulation, it appears that the chronicity and exacerbation of emotion regulation difficulties over time is predictive of a broader range of BPD features. In addition, rate of change in interpersonal conflict did not predict BPD features at follow-up. These findings demonstrate that within-individual changes in emotion dysregulation over the course of one year specifically predict BPD features. However, it was not the rate of change, but the overall level of emotion dysregulation that emerged as a maintaining mechanism for BPD features, and specifically for affective instability and identity disturbance. It is possible that difficulties regulating emotions, such as deficits in strategies for identifying and modulating affects and for controlling impulses when experiencing intense emotions, perpetuate chaotic and variable experiences with regard to mood and sense of self, thereby serving to maintain affective instability and identity problems over time.
Although increases in emotion dysregulation predicted more negative relations and self harm at follow-up, emotion dysregulation did not mediate associations between BPD symptom severity at baseline and these difficulties, suggesting that other processes might maintain problems with interpersonal relations and impulsive behavior. Interestingly, BPD symptom severity at baseline directly predicted higher self harm at 12-month follow-up, even after controlling for all other predictors. In addition, overall level of interpersonal conflict over the year predicted both negative relationships and self harm at follow-up, which is consistent with studies demonstrating associations between externalized aggression, self-injurious behavior, and suicide attempts [37]. It is possible that these difficulties may reflect greater impulsivity, which may be expressed in aggression directed at self or others [38]. These findings suggest that more severely impaired individuals who experience more chaotic interpersonal relationships are at greater risk for impulsive behavior and continued interpersonal problems a year later, even after controlling for the influence of emotion dysregulation, which serves to further exacerbate these problems.
Given that we controlled for baseline depression and anger rumination, our results are consistent with findings that the effects of emotion dysregulation on psychopathology cannot simply be accounted for by these general forms of negative affect [39]. Even though individuals with greater depression and angry rumination had higher overall levels of emotion dysregulation, depression actually predicted faster rates of improvement in emotion dysregulation over the course of the year, whereas, BPD symptom severity predicted slower rates of improvement in emotion dysregulation over time. Although speculative, it is possible that those who report more negative emotions at baseline tend to be more motivated and engaged to make changes in their lives, which may thereby influence their rate of improvement in emotion dysregulation. Alternatively, it could be that these findings represent a ceiling effect, such that an individual with higher negative emotions is restricted in terms of how much worse he/she can get over time. Additionally, changes in emotion dysregulation had strong and consistent effects across all four BPD features at 12-month follow-up, even after controlling for the influence of depression, angry rumination, and BPD symptom severity at baseline. These findings suggest that it is not merely the experiencing of intense negative affects, but also, chronic deficits in the ability to effectively identify, tolerate, and regulate these emotions that are predictive of increased BPD features over the course of one year.
Our findings with regard to patterns of change in emotion dysregulation and interpersonal conflict are similar to previous studies finding stability of BPD features over the course of one year [40–41]. The slight decrease in emotion dysregulation over the year, in comparison to the lack of significant change in interpersonal conflict during this period, is consistent with previous studies suggesting that problems in social relationships are among the most intransigent of personality disorder symptoms [42].
Strengths and Limitations
The strengths of this study are the intensive repeated assessments over the course of one year and the ability to examine within-individual changes in putative maintaining mechanisms for BPD. This time frame has practical implications as a year reflects a typical course of treatment for most randomized controlled clinical trials. Although we cannot determine the degree of change in these constructs that is due to treatment effects, the inclusion of community participants with a range of BPD symptoms in addition to patients receiving psychiatric treatment provides some perspective on naturalistic change in these constructs across these populations. Another strength of this study is the repeated assessment of interpersonal conflict over the course of the year, which enabled us to demonstrate the specificity of changes in emotion dysregulation for predicting BPD features at follow-up.
This study is not without limitations. First, we were not able to examine changes or maintenance in BPD diagnosis or DSM-IV symptoms, as these clinician-rated interview measures were not re-administered at follow-up appointments. Additionally, the measurement of emotion dysregulation, interpersonal conflict, and BPD features at 12-month follow-up relied on self-reports, which are susceptible to bias and shared method variance between these measures may have inflated associations between constructs. On a related note, our measure of emotion dysregulation may not have comprehensively assessed this complex and multidimensional construct. For instance, this measure does not general rumination tendencies. Although we controlled for angry rumination at baseline, we did not have repeated measures of this emotion-related construct and thus could not examine change in angry rumination over the year as a potential maintaining mechanism. Additionally, depression and angry rumination represent only a subset of the broader range of negative affect experiences that could be captured with a trait measure of negative affect or neuroticism. Future work may focus on emotion regulation strategies in vivo and using multiple methods of assessment, including objective measures such as observer ratings, psychophysiological assessments, neurobiological measures, and intensive repeated assessments in daily life to examine state versus trait-like experiences of negative affect. Given that we have identified within-individual variability and change in emotion dysregulation, future research on the short-term malleability of this construct and its effects on short-term changes in BPD features is needed.
Clinical Implications
These findings suggest that enhancing emotion regulation skills may lead to improvements in treatment, which is consistent with previous findings of skills targeting emotion regulation resulting in improvements in features associated with BPD [21] [43–44]. In particular, these results suggest that attention should be focused on accepting emotions, improving strategies for coping with negative emotion, and enhancing emotional clarity. Although Dialectical Behavior Therapy [9] focuses on improving emotion regulation skills explicitly, other empirically supported treatments for BPD also target emotion regulation by attending to affective processes in session, increasing the ability to recognize and label emotions, and improving patients’ awareness of emotional states as precipitants to behavior [45]. It may prove useful to carefully monitor emotion regulation capabilities throughout the course of treatment as this may be an important indicator that other BPD features may also be likely to improve over time.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gunderson JG, et al. Ten-year course of borderline personality disorder: psychopathology and function from the Collaborative Longitudinal Personality Disorders study. Arch Gen Psychiatry. 2011;68:827–837. doi: 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: A 10-year prospective follow-up study. Am J Psychiatry. 2010b;167:663–667. doi: 10.1176/appi.ajp.2009.09081130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. The 10-year course of psychosocial functioning among patients with borderline personality disorder and axis II comparison subjects. Acta Psychiatr Scand. 2010a;122:103–109. doi: 10.1111/j.1600-0447.2010.01543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gunderson JG, et al. Plausibility and possible determinants of sudden “remissions” in borderline patients. Psychiatry. 2003;66:111–119. doi: 10.1521/psyc.66.2.111.20614. [DOI] [PubMed] [Google Scholar]
- 5.Herr NR, Rosenthal MZ, Geiger PJ, Erikson K. Difficulties with emotion regulation mediate the relationship between borderline personality disorder symptom severity and interpersonal problems. Personal Ment Health. 2012 doi: 10.1002/pmh.1204. [DOI] [PubMed] [Google Scholar]
- 6.McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: a prospective study. Behav Res Ther. 2011;49:544–554. doi: 10.1016/j.brat.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crowell SE, Bauchaine TP, Linehan MM. A biosocial developmental model for borderline personality: Elaborating and extending Linehan’s theory. Psychol Bull. 2009;135:495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glenn CR, Klonsky ED. Emotion dysregulation as a core feature of borderline personality disorder. J Pers Disord. 2009;23:20–28. doi: 10.1521/pedi.2009.23.1.20. [DOI] [PubMed] [Google Scholar]
- 9.Linehan MM. Coginitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- 10.Putnam KM, Silk KR. Emotion dysregulation and the development of borderline personality disorder. Dev Psychopathol. 2005;17:899–925. doi: 10.1017/s0954579405050431. [DOI] [PubMed] [Google Scholar]
- 11.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Press; 2000. [Google Scholar]
- 12.Selby EA, Anestis MD, Bender TW, Joiner TE., Jr An exploration of the emotional cascade model in borderline personality disorder. J Abnorm Psychol. 2009;118:375–387. doi: 10.1037/a0015711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Selby EA, Anestis MD, Joiner TE. Understanding the relationship between emotional and behavioral dysregulation: Emotional cascades. Behav Res Ther 2008. 2008;46:593–611. doi: 10.1016/j.brat.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 14.Selby EA, Joiner TE. Emotional cascades as prospective predictors of dysregulated behaviors in borderline personality disorder. Personal Disord. 2012 doi: 10.1037/a0029933. [DOI] [PubMed] [Google Scholar]
- 15.Scott LN, Stepp SD, Pilkonis PA. Prospective associations between features of borderline personality disorder, emotion dysregulation, and aggression. Under review. doi: 10.1037/per0000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adrian M, Zeman J, Erdley C, Lisa L, Sim L. Emotional dysregulation and interpersonal difficulties as risk factors for nonsuicidal self-injury in adolescent girls. J Abnorm Child Psychol. 2011;39:389–400. doi: 10.1007/s10802-010-9465-3. [DOI] [PubMed] [Google Scholar]
- 17.Armey MF. Ecological momentary assessment and intervention in nonsuicidal self-injury: A novel approach to treatment. J Cogn Psychother. 2012;26:299–317. [Google Scholar]
- 18.Crowell SE, et al. Differentiating adolescent self-injury from adolescent depression: possible implications for borderline personality development. J Abnorm Child Psychol. 2012;40:45–57. doi: 10.1007/s10802-011-9578-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gratz KL, Chapman AL. The role of emotional responding and childhood maltreatment in the development and maintenance of deliberate self-harm among male undergraduates. Psychol Men Masc 2007. 2007;8:1–14. [Google Scholar]
- 20.Klonsky ED. The functions of deliberate self-injury: A review of the evidence. Clin Psychol Rev. 2007;27:226–239. doi: 10.1016/j.cpr.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Gratz KL, Levy R, Tull MT. Emotion regulation as a mechanism of change in an acceptance-based emotion regulation group therapy for deliberate self-harm among women with borderline personality pathology. J Cogn Psychother. 2012;26:365–380. [Google Scholar]
- 22.Trull TJ, et al. Affective instability: Measuring a core feature of borderline personality disorder with ecological momentary assessment. J Abnorm Psychol. 2008;117:647–661. doi: 10.1037/a0012532. [DOI] [PubMed] [Google Scholar]
- 23.Newhill CE, Eack SM, Mulvey EP. A growth curve analysis of emotion dysregulation as a mediator for violence in individuals with and without borderline personality disorder. J Pers Disord. 2012;26:452–467. doi: 10.1521/pedi.2012.26.3.452. [DOI] [PubMed] [Google Scholar]
- 24.Stepp SD, Smith TD, Morse JQ, Hallquist MN, Pilkonis PA. Prospective Associations Among Borderline Personality Disorder Symptoms, Interpersonal Problems, and Aggressive Behaviors. J Interpers Violence. 2012;27:103–124. doi: 10.1177/0886260511416468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zanarini MC, Vujanovic A, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. A screening measure for BPD: The McLean screening instrument for borderline personality disorder (MSI-BPD) J Pers Disord. 2003;17:568–573. doi: 10.1521/pedi.17.6.568.25355. [DOI] [PubMed] [Google Scholar]
- 26.Pfohl B, Blum NS, Zimmerman M. Structured interview for DSM-IV personality: SIDP-IV. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 27.Hamilton M. Rating depressive patients. J Clin Psychiatry. 1980;41:21–24. [PubMed] [Google Scholar]
- 28.Morey LC. Personality Assessment Inventory: Professional manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- 29.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26:41–54. [Google Scholar]
- 30.Strauss MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scale (CTS2): Development and preliminary psychometric data. J Fam Issues. 1996;17:283–316. [Google Scholar]
- 31.Sukhodolsky DG, Golub A, Cromwell EN. Development and validation of the anger rumination scale. Pers Individ Dif. 2001;31:689–700. [Google Scholar]
- 32.Satorra A, Bentler EM. Corrections to test statistics and standard enors in covariance structure analysis. In: von Eye A, Clogg CC, editors. Latent variables analysis: Applications for developmental research. Thousand Oaks, CA: Sage; 1994. pp. 399–419. [Google Scholar]
- 33.Fritz MS, Taylor AB, MacKinnon DP. Explanation of two anomalous results in statistical mediation analysis. Multivariate Behav Res. 2012;47:61–87. doi: 10.1080/00273171.2012.640596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2011. [Google Scholar]
- 35.McDonald RP, Ho MHR. Principles and practice in reporting structural equation analyses. Psychol Methods. 2002;7:64. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- 36.Hussong AM, Flora DB, Curran PJ, Chassin LA, Zucker RA. Defining risk heterogeneity for internalizing symptoms among children of alcoholic parents. Dev Psychopathol. 2008;20:165–193. doi: 10.1017/S0954579408000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Siever LJ. Neurobiology of aggression and violence. Am J Psychiatry. 2008;165:429–442. doi: 10.1176/appi.ajp.2008.07111774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Latalova K, Prasko J. Aggression in borderline personality disorder. Psychiatr Q. 2010;81:239–251. doi: 10.1007/s11126-010-9133-3. [DOI] [PubMed] [Google Scholar]
- 39.Bradley B, et al. Emotion dysregulation and negative affect: association with psychiatric symptoms. J Clin Psychiatry. 2011;72:685–691. doi: 10.4088/JCP.10m06409blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Trull TJ. Two-year stability of borderline personality measures. J Pers Disord. 1998;12:187–197. doi: 10.1521/pedi.1998.12.3.187. [DOI] [PubMed] [Google Scholar]
- 41.Tragesser SL, Solhan M, Schwartz-Mett R, Trull TJ. The role of affective instability and impulsivity in predicting borderline personality disorder features. J Pers Disord. 2007;21:603–614. doi: 10.1521/pedi.2007.21.6.603. [DOI] [PubMed] [Google Scholar]
- 42.Skodol AE, et al. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychol Med. 2005;35:443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Neacsiu AD, Rizvi SL, Linehan MM. Dialectical behavior therapy skills use as a mediator and outcome of treatment for borderline personality disorder. Behav Res Ther. 2010;48:832–839. doi: 10.1016/j.brat.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stepp SD, Epler AJ, Jahng S, Trull TJ. The effect of Dialectical Behavior Therapy skills use on borderline personality disorder features. J Pers Disord. 2008;22:549–563. doi: 10.1521/pedi.2008.22.6.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weinberg I, Ronningstam E, Goldblatt M, Schechter M, Maltsberger J. Common factors in empirically supported treatments of borderline personality disorder. Curr Psychiatry Rep. 2011;13:60–68. doi: 10.1007/s11920-010-0167-x. [DOI] [PubMed] [Google Scholar]


