Abstract
Objective
Negative affect precedes binge eating and purging in bulimia nervosa (BN), but little is known about factors that precipitate negative affect in relation to these behaviors. We aimed to assess the temporal relation among stressful events, negative affect, and bulimic events in the natural environment using ecological momentary assessment.
Method
A total of 133 women with current BN recorded their mood, eating behavior, and the occurrence of stressful events every day for two weeks. Multi-level structural equation mediation models evaluated the relations among Time 1 stress measures (i.e., interpersonal stressors, work/environment stressors, general daily hassles, and stress appraisal), Time 2 negative affect, and Time 2 binge eating and purging, controlling for Time 1 negative affect.
Results
Increases in negative affect from Time 1 to Time 2 significantly mediated the relations between Time 1 interpersonal stressors, work/environment stressors, general daily hassles, and stress appraisal, and Time 2 binge eating and purging. When modeled simultaneously, confidence intervals for interpersonal stressors, general daily hassles, and stress appraisal did not overlap, suggesting that each had a distinct impact on negative affect in relation to binge eating or purging.
Conclusions
Our findings indicate that stress precedes the occurrence of bulimic behaviors and that increases in negative affect following stressful events mediate this relation. Results suggest that stress and subsequent negative affect may function as maintenance factors for bulimic behaviors and should be targeted in treatment.
Keywords: bulimia nervosa, negative affect, stress, binge eating, ecological momentary assessment
Bulimia nervosa (BN) is a serious psychiatric disorder characterized by recurrent binge eating (i.e., the consumption of an unambiguously large amount of food accompanied by a sense of loss of control while eating) and inappropriate compensatory behaviors intended to counteract the effects of eating and minimize weight gain (American Psychiatric Association, 2000). BN is associated with significant physical and psychosocial health consequences, including gastrointestinal disturbances, electrolyte abnormalities, and increased rates of suicide (Crow et al., 2009; Hudson, Hiripi, Pope, & Kessler, 2007; Mitchell & Crow, 2006). Within the literature examining variables that function as potential antecedents of bulimic behaviors, there is compelling evidence suggesting that negative affect precipitates binge eating and purging in BN (Haedt-Matt & Keel, 2011). However, little is known about antecedents to those negative affective experiences that are known to function as triggers for bulimic behaviors. A better understanding of the various steps in the process by which certain events precipitate negative affect, which in turn precipitates bulimic symptoms, could inform treatment planning and the development of novel interventions for the disorder.
Negative Affect and Bulimic Behavior
Negative affect refers to a state of “subjective distress and unpleasurable engagement” that encompasses a range of adverse emotions (Watson, Clark, & Tellegen, 1988; p. 1063). Broadly, affect regulation theories posit that binge eating may be a maladaptive means of coping with negative affect (Haedt-Matt & Keel, 2011), although the different specific theories vary in terms of proposed mechanisms. For example, Heatherton and Baumeister (1991) suggested that binge eating provides an escape from aversive self-awareness by focusing attention on the immediate environment and away from distressing emotions. Alternatively, Kenardy and colleagues (1996) have suggested that binge eating enables a “trade-off” in which highly aversive emotions prior to binge eating (e.g., sadness) are replaced by more tolerable negative emotions thereafter (e.g., regret). As reviewed recently by Haedt-Matt and Keel (2011), a number of studies using various methodological approaches (e.g., traditional self-report, ecological momentary assessment [EMA], and experimental paradigms), support the notion that negative affect precipitates binge eating. EMA data have provided particularly rigorous evidence applicable to affect regulation theories, as such data are collected in the participants’ natural environment in “real time,” thus enabling investigators to establish temporal precedence with respect to affect and eating behavior while minimizing retrospective recall bias (Shiffman, Stone, & Hufford, 2008). EMA findings indicate that negative affect increases prior to bulimic behaviors (Engelberg, Steiger, Gauvin, & Wonderlich, 2007; Hilbert & Tuschen-Caffier, 2007; Smyth et al., 2007; Steiger et al., 2005), and some data suggest that these behaviors are maintained by negative reinforcement, as negative affect consequent to binge eating and purging events appears to improve (Berg et al., 2013; Engel et al., in press; Smyth et al., 2007); however, the existing literature is mixed with respect to this latter finding (Haedt-Matt & Keel, 2011; Hilbert & Tuschen-Caffier, 2007; Stein et al., 2007).
One limitation of affect regulation theories is that they do not specifically address the factors that precipitate the negative affective experiences that are viewed as important antecedents to bulimic events. An understanding of these factors would be clinically useful, particularly by contributing to theoretical models of the onset and maintenance of BN. For instance, a better understanding of the temporal sequence and process by which certain theoretical precipitants influence the occurrence of bulimic behaviors could provide multiple points of intervention (e.g., devising interventions aimed at modifying precipitants of negative affect, or the experience of negative affect itself) to interrupt the recurrence of these behaviors. Recently, Haynos and Fruzzetti (2011) applied a transactional model of emotion regulation to anorexia nervosa which describes the process by which intra-individual factors, events, cognitions, and emotions interact to influence eating disorder behaviors. This model (which could reasonably apply to other eating disorders as well) suggests that emotionally evocative events and one's appraisal of these events lead to emotional arousal, which in turn elicits eating disorder behaviors. Although several lines of evidence support aspects of this theoretical model (Haynos & Fruzzetti, 2011), to our knowledge, no studies have used momentary data to directly test this model in an eating disordered sample.
Stress and Bulimic Behavior
The term “stressor” refers to hardship or adversity, or a deviation from normality or a usual state, and “stress” to an experience in which the demands incurred by these stressors exceed one's available coping resources (Lazarus, 1993). Implicit in this model is the notion that one's appraisal of the stressor and of one's ability to cope are relevant to the experience of stress. Research suggests that eating disorders, including BN, are associated with the occurrence of stressful events (Grilo et al., 2012; Raffi, Rondini, Grandi, & Fava, 2000; Wolff, Crosby, Roberts, & Wittrock, 2000), and with abnormalities in both objective (e.g., physiological) and subjective (e.g., self-report) reactions to such events (Crowther, Sanftner, Bonifazi, & Shepherd, 2001; Koo-Loeb, Pedersen, & Girdler, 1998; Messerli-Burgy, Engesser, Lemmenmeier, Steptoe, & Laederach-Hofmann, 2010). However, the nature of the association between stressful events and eating disorder behaviors in BN, including the mechanisms by which stressful events may impact or precipitate these behaviors, remains unclear.
According to the transdiagnostic theory of eating disorders, adverse life circumstances (and particularly an adverse interpersonal environment) can contribute to both the onset and maintenance of eating disorders (Fairburn, 2008). Interpersonal theory more specifically posits that interpersonal functioning may be particularly salient in the occurrence of bulimic behaviors through the indirect mechanism of contributing to negative affect, which subsequently precipitates such behaviors (Arcelus, Haslam, Farrow, & Meyer, 2013). Interpersonal stressors (i.e., events of an interpersonal nature that are related to the experience of distress) are one construct accounted for in this theory, along with social maladjustment, social support, interpersonal problem-solving, fear of negative self-evaluation, and social comparison, among others. Consistent with this theory, recent data suggest that the relation between interpersonal problems and bulimic behaviors may be mediated by negative affect (Ansell, Grilo, & White, 2012). This model is of particular clinical relevance, given that individuals with BN and other eating disorders endorse greater interpersonal problems than controls, including difficulties with assertiveness (Hartmann, Zeeck, & Barrett, 2010; Troop, Allan, Treasure, & Katzman, 2003) and poor social support (Grissett & Norvell, 1992; Tiller et al., 1997). However, additional research using prospective, momentary data would provide a stronger test of this hypothesized mediational relationship.
In addition to research on the impact of singular, particularly impactful stressors, another body of literature on the influence of daily hassles suggests that the cumulative effects of minor stressors significantly affect mood and overall psychosocial functioning (e.g., Baker, 2006; Mroczek & Almeida, 2004; Piazza, Charles, Sliwinski, Mogle, & Almeida, 2012). The literature on daily hassles in BN is scant, as most data pertain to non-clinical samples (e.g., undergraduates or community-based individuals reporting bulimic symptoms). While the number of daily hassles may not be elevated in individuals with binge eating problems (Crowther et al., 2001; Wolff et al., 2000), evidence suggests that these individuals perceive these minor events as more stressful than controls (Crowther et al., 2001). Moreover, both the occurrence (Woods, Racine, & Klump, 2010) and the perceived impact of these minor events (Wolff et al., 2000) is associated with binge eating episodes on a daily basis. This latter finding is consistent with cognitive behavioral theory, which suggests that one's appraisal of a stressful event plays a critical role in the extent to which negative mood is experienced in response to the event (Beck, 1995).
Current Study
The current study aimed to examine the temporally-sequenced relationship among stressful events, negative affect, and bulimic behaviors in order to optimally inform both etiological and intervention research. Consistent with the transactional model of emotion dysregulation in anorexia nervosa (Haynos & Fruzzetti, 2011), we hypothesized that negative affect would mediate the relation between stressful events and subsequent binge/purge events. In addition, an exploratory aim was to examine the unique effects of different measures of stress (i.e., specific types of stressors, stress appraisal) in relation to the negative affect precipitating bulimic behaviors. Results could have important clinical implications in terms of highlighting relevant treatment foci in interventions for BN.
Method
Participants
Participants were 133 females (M age=25.3±7.6) who met DSM-IV (American Psychiatric Association, 2000) criteria for BN and were recruited for an EMA study of BN (Smyth et al., 2007). The current study, which examined antecedents to negative affect in relation to bulimic events, expands on previous studies using EMA data in this sample (e.g., Anestis et al., 2012; Berg et al., 2013; Crosby et al., 2009; Engel et al., 2007; Goldschmidt et al., 2013; Karr et al., 2013; Muehlenkamp et al., 2009; Selby et al., 2012; Zunker et al., 2011), many of which focused solely on immediate emotional antecedents to binge eating and purging, but not on factors preceding emotional antecedents to these behaviors (Berg et al., 2013; Goldschmidt et al., 2013; Karr et al., 2013; Selby et al., 2012). To be included, participants had to be female, between the ages of 18 and 55, able to read English, and medically stable with a body mass index (BMI; kg/m2) of at least 18.5 (M BMI=23.9±5.2). The sample was primarily Caucasian (n=127; 95.5%), with the majority having completed at least some college (n=107; 80.5%) and having never been married (n=85; 63.9%). Participants reported a mean age of BN symptom onset of 16.6±3.8 years, and 40.6% reported having received mental health treatment in the 6 weeks prior to assessment.
Procedure
Participants were recruited through clinic, community and campus advertising. Interested participants completed a phone screen to ascertain preliminary BN status, which consisted of assessing eating behaviors over the past month using the eating disorder module from the Structured Clinical Interview for DSM-IV Axis I Disorders/Patient Edition (SCID-I/P; First, Spitzer, Gibbon, & Williams, 1997). After study eligibility was determined, participants attended an informational session at the research facility during which they provided written informed consent and were screened for medical stability. Height and weight were measured by trained research staff using a calibrated stadiometer and scale, respectively. Participants then completed a baseline assessment battery (including the full SCID-I/P) and received thorough instructions on how to use the handheld computer (Palm 5X, Satellite Form Software) for the 2-week EMA protocol. Participants were instructed to complete EMA recordings each time they experienced an eating disorder behavior (e.g., binge eating, purging); before bedtime; and in response to 6 semi-random prompts by investigators, which occurred every 2-3 hours between 8:00 am and 10:00 pm (Wheeler & Reis, 1991). Each participant completed a two-day trial period to ensure that they understood EMA procedures; trial data were not included in the analyses. After the two-day trial, and on two additional occasions during the EMA trial, participants were scheduled to visit the research facility to receive feedback on their compliance. Participants received $200 for completing the two-week EMA trial, and were given an additional $50 for compliance rates of 85% or better on signal-contingent recordings. The study was approved by the University of North Dakota and MeritCare Hospital Institutional Review Boards.
Measures
Eating disorder symptoms
The full SCID-I/P (First et al., 1997) was administered at the informational session by trained, doctoral-level psychologists to confirm preliminary BN diagnoses established during the phone screen, as well as to assess eating disorder history and the presence of other lifetime/current psychiatric diagnoses. The SCID-I/P is a well-established measure of Axis I psychopathology with demonstrated reliability and validity in psychiatric populations (First et al., 1997; Lobbestael, Leurgans, & Arntz, 2011). Inter-rater reliability for BN diagnoses was 1.0 in the current study.
Binge eating (“I binged”) and purging (“I vomited,” “I used laxatives for weight control”) were assessed via EMA using the Eating Disorder Behavior Checklist (EDBC), which was designed for the study. Participants were instructed to record bulimic behaviors immediately after they occurred in real time, and to indicate in response to semi-random prompts whether any behaviors had occurred since the last recording. During the EMA orientation period, participants were instructed that binge eating refers to consuming “an amount of food that you consider excessive or an amount of food that other people would consider excessive, with an associated loss of control or the feeling of being driven or compelled to keep eating.” Participants were provided with personally-tailored examples of excessive amounts of food based on binge eating episodes reported on the SCID-I/P. For the current study, frequency values for vomiting and laxative misuse were summed to generate a broad purging variable.
Stressful events
Stressful events were assessed via EMA using select items from the Daily Stress Inventory (DSI; Brantley & Jones, 1989) and the Daily Experiences Survey (DES; Hokanson, Stader, Flynn, & Tate, 1992). Participants selected from a list of items the specific stressful events that had occurred since the last beep, and for each event that occurred, indicated how long ago the event happened and how stressful they found the event [from 1 (“not at all”) to 5 (“very much”)]. Reporting of stressful events was completed after the occurrence of bulimic behaviors and in response to semi-random prompts.
The DSI is a 60-item measure of daily stressful events that has good internal consistency (Brantley, Waggoner, Jones, & Rappaport, 1987) and convergent validity (Brantley, Dietz, McKnight, Jones, & Tulley, 1988). The DES is a 60-item scale designed to measure daily experiences that appears to have good internal consistency and concurrent validity (Stader & Hokanson, 1998). A total of 35 items covering a variety of stressful events were included in the EMA protocol, of which 26 were extracted from the DSI (e.g., “Had car trouble,” “Argued with a spouse/lover”), 8 were extracted from DES (e.g., “Worried about long-term goals,” “Felt stress about relationships with others”), and 1 additional item was developed based on its potential relevance to BN (i.e., “Spent time alone”). Consistent with our previous work (Smyth et al., 2009), we created three indices measuring interpersonal stressors, work/environment stressors, and daily hassles. Two independent raters assigned items to these scales using a pre-determined selection process (kappa=.782). Discrepancies were resolved by consensus with the remaining authors.
Negative affect
An abbreviated version of the Positive and Negative Affect Scale (PANAS; Watson et al., 1988) was administered via EMA to measure momentary negative affect. Participants rated their current mood at all EMA recordings (i.e., after the occurrence of bulimic behaviors, before bedtime, and in response to semi-random prompts). PANAS items were chosen based on high factor loadings and previous EMA work implicating facets of negative affect that would be clinically and/or theoretically relevant (Smyth et al., 2007). Negative affect is assessed by summing 11 items (afraid, lonely, irritable, ashamed, disgusted, nervous, dissatisfied with self, jittery, sad, distressed, angry with self), all of which are rated on a 5-point scale, with a score of “1” corresponding to “Not at all” and a score of “5” corresponding to “Extremely” for each mood state. The PANAS negative affect subscale appears to have adequate reliability (Watson et al., 1988). Cronbach's alpha in the current study was 0.92 for negative affect.
Statistical Analyses
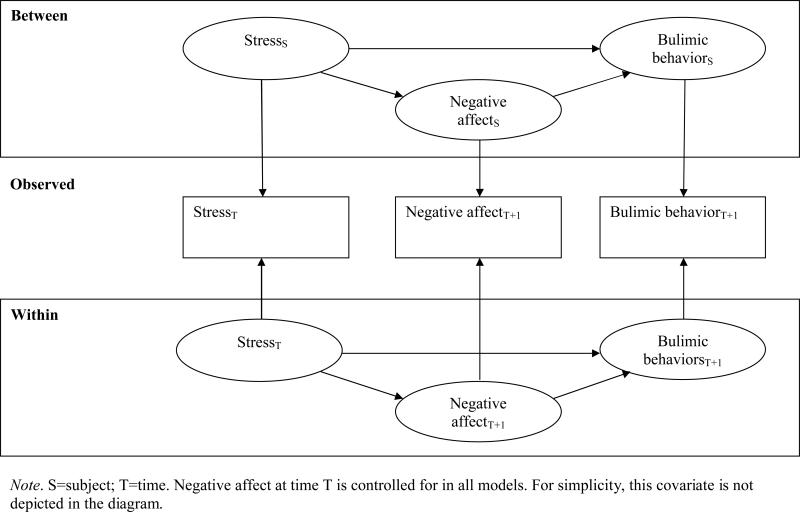
All analyses were conducted using SPSS 19.0 and Mplus 7.0. Mediation analyses were performed using a 1-1-1 (corresponding to the level of the independent variable, the mediator, and the dependent variables, respectively) multi-level structural equation model (MSEM) with fixed slopes (see Figure 1; Preacher, Zhang, & Zyphur, 2011; Preacher, Zyphur, & Zhang, 2010). MSEM uses a robust maximum likelihood estimation method, which accommodates missing data and unbalanced clusters, does not assume normality, and generates robust estimates of asymptotic parameter estimates (Preacher et al., 2010). We used MSEM for mediation analysis rather than an approach based upon multilevel modeling (MLM; e.g., Bauer, Preacher, & Gil, 2006; Kenny, Korchmaros, & Bolger, 2003) because MLM approaches combine between-subject and within-subject effects in estimating the indirect effect, thereby conflating or biasing the estimate (Preacher et al., 2010). We tested 10 independent mediation models, all of which adjusted for the presence of a current mood or anxiety disorder. In each model, the independent variable was the stress measure at Time 1, the dependent variable was bulimic behavior at Time 2, and the mediator was negative affect at Time 2, controlling for Time 1 negative affect. This sequence was designed to address the notion that increases in negative affect (rather than merely state negative affect) precede bulimic events, which is a tenet of affect regulation theories (Haedt-Matt & Keel, 2011). A total of 4 separate models were conducted to test different measures of stress as the independent variables; each of these models was run separately for binge eating and purging (i.e., a total of 8 models). The stress measures included the total count of interpersonal stressors, work/environment stressors, and general daily hassles, and the average stress appraisal across these different types of events. Two additional models were run which tested all types of stressors (interpersonal stressors, work/environment stressors, and general daily hassles) along with stress appraisal included simultaneously as independent variables to predict binge eating or purging in order to parse out the unique effects of different measures of stress. In order to assess the relative importance of each type of stress measure in relation to participants’ negative affect and bulimic behaviors, we examined the confidence intervals of the odds ratios (overlapping versus not). Because we were primarily interested in the temporal relations among stress constructs, negative affect, and bulimic events, our main focus was on within-subjects effects (which would describe the process by which these events are related in time; e.g., whether the presence of a greater number of stressful events is related to greater increases in subsequent negative affect and hence a greater likelihood of associated bulimic events) as opposed to between-subjects effects (which would describe relations among varying degrees of these constructs averaged across subjects; e.g., whether a participant who experienced a greater number of stressful events also experienced greater negative affect and more frequent occurrence of bulimic events within the 2-week sampling period).
Figure 1.
Illustration of the mediation model for stress, negative affect, and bulimic behaviors
Results
Descriptive Information
Participants responded to an average of 86% of semi-random prompts, and 75% of participants responded to at least 83% of the prompts. Approximately 75% of semi-random prompt recordings were made within 20 minutes. Bedtime recordings were completed on approximately 84% of all possible occasions. Participants reported an average of 7.8±6.5 binges and 11.1±9.6 purges during the 2-week EMA protocol. Participants reported an average of 108.5±85.1 stressful events over the course of the protocol, including 50.0±39.9 interpersonal stressors; 32.0±32.0 work/environment hassles; and 26.6±22.9 general daily hassles. Stressful events were recorded during 39.1% of EMA recordings. The average stress appraisal rating across reported stressful events was 2.3±1.1. Participants reported a higher average stress appraisal for work/environment stressors than either interpersonal stressors or general daily hassles, which did not differ from one another [F(2, 9902)=357.89; p<.001]. An average of 2.5±1.2 hours lapsed between Time 1 EMA recordings and Time 2 binge eating, and an average of 2.5±1.1 hours lapsed between Time 1 recordings and Time 2 purging. There were small but significant correlations among the different types of stressors (see Table 1).
Table 1.
Correlations among Time 1 stress variables, Time 2 negative affect, and Time 2 bulimic events
| Time 1 | Time 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Interpersonal stressors | Work/environment stressors | General daily hassles | Stress appraisal | Negative affect | Binge eating | Purging | ||
| Time 1 | Interpersonal stressors | --- | .29* | .23* | .12* | .22* | .11* | .07* |
| Work/environment stressors | --- | --- | .20* | .30* | .27* | .09* | .06* | |
| General daily hassles | --- | --- | --- | -.04* | .11* | .003 | .004 | |
| Stress appraisal | --- | --- | --- | --- | .11* | .08* | .09* | |
| Time 2 | Negative affect | --- | --- | --- | --- | --- | .15* | .14* |
| Binge eating | --- | --- | --- | --- | --- | --- | .56* | |
| Purging | --- | --- | --- | --- | --- | --- | --- | |
p<.01
Within-Subjects Predictors of Binge Eating and Purging
When the independent variables (i.e., stress variables) were modeled separately within subjects, change in negative affect from Time 1 to Time 2 mediated the relation between Time 1 interpersonal stressors, work/environment stressors, general daily hassles, and stress appraisal, and Time 2 binge eating and (separately) purging (ps<.05; see Table 2).
Table 2.
Summary of within-subjects mediation results for stress constructs modeled individually
| Independent variable (IV) | Mediating variable (MV) | Dependent variable (DV) | Effect of IV on MV (a) | Effect of MV on DV (b) | Direct effect (c') | Indirect effect (a*b) | Confidence Intervals |
|---|---|---|---|---|---|---|---|
| T1 interpersonal stress | T2 negative affect | T2 binge eating | 0.228** (S.E.=0.026) | 0.010** (S.E.=0.001) | −0.008** (S.E.=0.001) | 0.002** (S.E.=0.000) | .002-.003 |
| T1 work/environment stress | T2 negative affect | T2 binge eating | 0.198** (S.E.=0.026) | 0.010** (S.E.=0.001) | −0.009** (S.E.=0.001) | 0.002** (S.E.=0.000) | .001-.002 |
| T1 general daily hassles | T2 negative affect | T2 binge eating | 0.154** (S.E.=0.025) | 0.010** (S.E.=0.001) | −0.008** (S.E.=0.001) | 0.001** (S.E.=0.000) | .001-.002 |
| T1 stress appraisal | T2 negative affect | T2 binge eating | 1.452** (S.E.=0.136) | 0.010** (S.E.=0.001) | −0.014** (S.E.=0.004) | 0.014** (S.E.=0.002) | .012-.017 |
| T1 interpersonal stress | T2 negative affect | T2 purging | 0.228** (S.E.=0.026) | 0.010** (S.E.=0.001) | −0.010** (S.E.=0.002) | 0.002** (S.E.=0.000) | .002-.003 |
| T1 work/environment stress | T2 negative affect | T2 purging | 0.197** (S.E.=0.026) | 0.010** (S.E.=0.001) | −0.010** (S.E.=0.001) | 0.002** (S.E.=0.000) | .002-.003 |
| T1 general daily hassles | T2 negative affect | T2 purging | 0.153** (S.E.=0.025) | 0.010** (S.E.=0.001) | −0.010** (S.E.=0.001) | 0.002** (S.E.=0.000) | .001-.002 |
| T1 stress appraisal | T2 negative affect | T2 purging | 1.442** (S.E.=0.136) | 0.010** (S.E.=0.001) | −0.012* (S.E.=0.004) | 0.015** (S.E.=0.002) | .012-.018 |
p<.01;
p≤.001
When Time 1 stress variables (interpersonal stressors, work/environment stressors, general daily hassles, and stress appraisal) were modeled simultaneously within subjects, change in negative affect from Time 1 to Time 2 mediated the relation between interpersonal stressors (indirect effect estimate=0.006; 95% CI=0.004 to 0.007), general daily hassles (indirect effect estimate=-0.005; 95% CI=-0.007 to -0.003), and stress appraisal (indirect effect estimate=0.013; 95% CI=0.011 to 0.016) and Time 2 binge eating as well as purging (interpersonal stressors indirect effect estimate=0.006; 95% CI=0.004 to 0.008; general daily hassles indirect effect estimate=-.005; 95% CI=-0.007 to -0.003; stress appraisal indirect effect estimate=0.014; 95% CI=0.011 to 0.017). The effect for work/environment stressors was not significant for either binge eating or purging (ps≥.21). The non-overlapping confidence intervals for interpersonal stressors, general daily hassles, and stress appraisal suggest that each had a unique impact on participants’ change in negative affect in relation to binge eating and purging.
Between-Subjects Predictors of Binge Eating and Purging
The mediation models for stress variables modeled separately between subjects were non-significant for binge eating (ps≥.68) and purging (ps≥.06), with one exception: Time 2 negative affect significantly mediated the relationship between Time 1 stress appraisal and Time 2 binge eating, after controlling for Time 1 negative affect (p=.03; see Table 3).
Table 3.
Summary of between-subjects mediation results for stress constructs modeled individually
| Independent variable (IV) | Mediating variable (MV) | Dependent variable (DV) | Effect of IV on MV (a) | Effect of MV on DV (b) | Direct effect (c') | Indirect effect (a*b) | Confidence Intervals |
|---|---|---|---|---|---|---|---|
| T1 interpersonal stress | T2 negative affect | T2 binge eating | 5.828*** (S.E.=1.421) | 0.000 (S.E.=0.001) | 0.052*** (S.E.=0.012) | 0.001 (S.E. =0.004) | −.006-.009 |
| T1 work/environment stress | T2 negative affect | T2 binge eating | 6.633*** (S.E.=1.468) | 0.000 (S.E.=0.001) | 0.068*** (S.E.=0.014) | −0.002 (S.E. =0.006) | −.012-.007 |
| T1 general daily hassles | T2 negative affect | T2 binge eating | 5.956** (S.E.=1.958) | 0.000 (S.E.=0.001) | 0.073*** (S.E.=0.020) | .002 (S.E.=0.005) | −.006-.010 |
| T1 stress appraisal | T2 negative affect | T2 binge eating | 6.271*** (S.E.=0.963) | 0.002 (S.E.=0.001)* | 0.003 (S.E.=0.010) | 0.011* (S.E.=0.005) | .003-.020 |
| T1 interpersonal stress | T2 negative affect | T2 purging | 5.885*** (S.E.=1.434) | 0.001 (S.E.=0.001) | 0.057** (S.E.=0.019) | .005 (S.E.=0.009) | −.009-.020 |
| T1 work/environment stress | T2 negative affect | T2 purging | 6.709*** (S.E.=1.482) | 0.000 (S.E.=0.002) | 0.072** (S.E.=0.022) | 0.002 (S.E.=0.010) | −.015-.019 |
| T1 general daily hassles | T2 negative affect | T2 purging | 6.068** (S.E.=1.992) | 0.001 (S.E.=0.001) | 0.098** (S.E.=0.030) | 0.004 (S.E.=0.009) | −.010-.018 |
| T1 stress appraisal | T2 negative affect | T2 purging | 6.264*** (S.E.=0.962) | 0.003* (S.E.=0.002) | −0.007 (S.E.=0.014) | 0.020 (S.E.=0.011) | .002-.037 |
p<.05;
p<.01
p<.001
When Time 1 interpersonal stressors, work/environment stressors, general daily hassles, and stress appraisal were modeled simultaneously between subjects, mediation effects for these variables were non-significant for binge eating (ps≥.63) and purging (ps≥.09).
Discussion
The purpose of the current study was to characterize the associations among stressful events, negative affect, and bulimic behaviors in women with BN using data collected via EMA, which allowed for the variables to be temporally sequenced. Although the extant theoretical and empirical literature supports an indirect relation between various types of stress and eating disorder behaviors that is mediated by negative affect (e.g., Ansell et al., 2012; Haynos & Fruzzetti, 2011), no studies to date have utilized momentary, prospective data to substantiate this model. In the current study, we found that stress, operationalized both as the number of stressors and as one's appraisal of stressful events, temporally preceded the occurrence of binge eating and purging behaviors, and that increases in negative affect related to the occurrence of binge eating and purging behaviors mediated this relationship. Interpersonal stressors, general daily hassles, and stress appraisal (but not work/environment stressors) were each uniquely predictive of increases in negative affect associated with binge eating and purging when tested simultaneously against one another, which provides support for interpersonal theory, the general daily hassles literature, and cognitive behavioral models of eating disorders, respectively. Moreover, there was limited support for a between-subjects model whereby individuals who experienced a greater number of stressful events or had more negative stress appraisals also experienced higher levels of negative affect linked to higher rates of bulimic behaviors; one exception is that those with higher stress appraisal experienced greater negative affect related to binge eating, providing additional support for the cognitive behavioral model. Overall, our data suggest that on occasions in which women with BN experience a greater number of stressful events or more stressful appraisals of these events, they are more likely to experience subsequent increases in negative affect that are associated with binge eating and purging behaviors. That these results applied to our full sample, rather than just a subset of women with BN who experienced greater numbers of stressful events or higher stress appraisal, has strong relevance for treatments designed to target the general BN population.
Our results have important implications in terms of understanding the process by which bulimic events occur in the natural environment and should be used to maximize the efficacy of existing interventions for BN. First, our data provide insight into factors that precipitate negative affect in relation to BN symptoms. Although previous studies have shown that stressful events are related to bulimic behaviors, none to date have specified to mechanisms by which this association unfolds in real time. For example, while prior studies have shown that life stressors and a generally stressful interpersonal environment may be related to the onset or maintenance of eating disorder symptoms (Raffi et al., 2000; Woods et al., 2010) and that negative affect mediates this relationship (Ansell et al., 2012; Elliott et al., 2010), few have established temporal precedence in this relationship (Grilo et al., 2012; Smyth, Heron, Wonderlich, Crosby, & Thompson, 2008), and none have used data collected in a momentary fashion in naturalistic settings.
Second, our data provide support for the cognitive behavioral model of binge eating, which presumes that one's negatively-valenced interpretation of events contributes to adverse emotional reactions that then promote the occurrence of dysfunctional behaviors (Beck, 1995). Cognitive behavior therapy (CBT) for BN addresses problematic eating patterns and involves modifying beliefs surrounding eating, shape, and weight (Fairburn, Marcus, & Wilson, 1993). More recent iterations of CBT for BN address events and moods that contribute to the occurrence of bulimic behaviors through the use of problem-solving and mood modulation skills (Fairburn, 2008). The current results suggest that a focus on cognitions and appraisals related to stressful events may also be appropriate and helpful in reducing affectively-driven binge eating episodes, and future studies should assess changes in temporal relations among stress, negative affect, and bulimic behaviors among individuals who have received CBT in order to better understand the mechanisms by which it results in symptom reduction. It should be noted that the current study did not specifically assess whether participants’ appraisals of events as more or less stressful were related to their cognitive interpretations of these events; future EMA studies should seek to further understand processes involved in these stress appraisals.
Our data also support one aspect of the interpersonal model of binge eating, namely, that acute interpersonal stressors perpetuate adverse emotional experiences which in turn trigger bulimic behaviors (Arcelus et al., 2013). This may partially explain the positive impact of interpersonal psychotherapy on binge eating and purging in BN (Murphy, Straebler, Basden, Cooper, & Fairburn, 2012), as IPT aims to improve varying aspects of interpersonal functioning in order to reduce negative affect related to bulimic symptoms. Because our measure of interpersonal stressors was quite broad in nature, future EMA studies should seek to identify specific interpersonal constructs that may be more or less relevant to the momentary experience of negative affect and related bulimic behaviors, such as social comparison or lack of adequate social support.
Work/environment stressors were rated as most subjectively stressful by participants, but these stressors did not uniquely predict increases in negative affect related to binge eating and purging when directly compared to other types of stress measures. One interpretation might be that although women with BN experience these stressors as more stressful, they are better able to cope with these stressors than with other types of stress. Alternatively, interpersonal stressors, general daily hassles, and stress appraisal may be more salient and enduring aspects of stress than that elicited by work/environment stressors. In accordance with interpersonal theory (Arcelus et al., 2013) and the daily hassles literature (e.g., Baker, 2006; Mroczek & Almeida, 2004; Piazza et al., 2012), events that impact self-evaluation or lead to a cumulative build-up of distress, respectively, may be more acutely impactful than events that may be perceived as relatively innocuous or time-limited.
Overall, the current study was marked by several strengths, including the large, community-based sample and the use of EMA to assess the associations among stressful events, negative affect, and bulimic behaviors. In particular, EMA allowed us to temporally establish the relationship among these constructs in the natural environment, which would be difficult using other study designs; however, it should be noted that in our mediation models, negative affect and bulimic events were assessed during the same EMA recording in order to maximize the amount of useable data, which makes it difficult to definitively infer that increases in negative affect led to the occurrence of bulimic events. Moreover, our stress measures allowed us to examine the unique contributions of both stressful events (i.e., objective construct) and the consequent experience of stress (i.e., subjective construct) in relation to negative affect and bulimic behaviors. Finally, all models controlled for the presence of current mood and anxiety disorders, indicating that the relations among stress, negative affect, and bulimic behaviors could not be attributed to current psychopathology.
However, several limitations should also be noted. First, although previous EMA studies have not demonstrated reactivity effects (Stein & Corte, 2003), carrying the handheld computer and making frequent recordings may have altered participants’ appraisals of events, mood, and behavior patterns. Indeed, a comparison of week 1 and week 2 reporting of the these variables revealed no significant differences, with the exception of negative affect, for which week 1 reporting was slightly but significantly higher (M=25.0 vs. 24.1; p<.001). Thus, reactivity in the current study appeared to be minimal. Further, this study did not assess all types of eating disorder behaviors because of the low base rates of some of these behaviors (e.g., fasting). Future studies should consider assessing the relationships among stressful events, negative affect, and other types of bulimic behaviors. There may have been overlap between the some of the stressful events (e.g., “felt stress about relationships with others”; “worried about long-term goals”) and negative affect items (e.g., “distressed”), although correlations between stressful events and negative affect were small (r range=.11-.27), indicating that these are likely distinct constructs. It should also be noted that the correlation between the PANAS with and without including the “distressed” item was very high (r=.997), which further allays concerns about construct overlap. Finally, because assessing subtypes of women with BN for whom certain aspects of stress are more salient than others was beyond the scope of the current study, future research should address the possibility that the associations among stress, negative affect, and bulimic events may be moderated by individual traits (e.g., affective lability; Anestis et al., 2009).
In summary, the results of the current study suggest that stressful events and their interpretation play a prominent role in the well-established association between negative affect and bulimic behaviors. Results substantiate several models of eating disorders using momentary, ecologically valid data, and help elucidate the process by which bulimic events occur in the natural environment. Future studies should clarify individual or subgroup characteristics that may be relevant to further understanding this relationship. Taken together, the current data should be used improve existing interventions for BN and related eating disorders, and to guide the development of new approaches to managing these serious psychiatric disorders.
Acknowledgements
This work was supported by NIH grants R01-MH59674, P30-DK50456, and T32-MH082761.
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, text revision. 4th ed. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Anestis MD, Peterson CB, Bardone-Cone AM, Klein MH, Mitchell JE, Crosby RD, Joiner TE. Affective lability and impulsivity in a clinical sample of women with bulimia nervosa: The role of affect in severely dysregulated behavior. International Journal of Eating Disorders. 2009;42:259–266. doi: 10.1002/eat.20606. doi:10.1002/eat.20606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anestis MD, Silva C, Lavender JM, Crosby RD, Wonderlich SA, Engel SG, Joiner TE. Predicting nonsuicidal self-injury episodes over a discrete period of time in a sample of women diagnosed with bulimia nervosa: An analysis of self-reported trait and ecological momentary assessment based affective lability and previous suicide attempts. International Journal of Eating Disorders. 2012;45:808–811. doi: 10.1002/eat.20947. doi:10.1002/eat.20947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansell EB, Grilo CM, White MA. Examining the interpersonal model of binge eating and loss of control over eating in women. International Journal of Eating Disorders. 2012;45:43–50. doi: 10.1002/eat.20897. doi:10.1002/eat.20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcelus J, Haslam M, Farrow C, Meyer C. The role of interpersonal functioning in the maintenance of eating psychopathology: A systematic review and testable model. Clinical Psychology Review. 2013;33:156–167. doi: 10.1016/j.cpr.2012.10.009. doi:10.1016/j.cpr.2012.10.009. [DOI] [PubMed] [Google Scholar]
- Baker SR. Towards an idiothetic understanding of the role of social problem solving in daily event, mood and health experiences: A prospective daily diary approach. British Journal of Health Psychology. 2006;11:513–531. doi: 10.1348/135910705X57647. doi:10.1348/135910705x57647. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Preacher KJ, Gil KM. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychological Methods. 2006;11:142–163. doi: 10.1037/1082-989X.11.2.142. doi:10.1037/1082-989x.11.2.142. [DOI] [PubMed] [Google Scholar]
- Beck JS. Cognitive therapy: Basics and beyond. Guilford Press; New York, NY: 1995. [Google Scholar]
- Berg KC, Crosby RD, Cao L, Peterson CB, Engel SG, Mitchell JE, Wonderlich SA. Facets of negative affect prior to and following binge-only, purge-only, and binge/purge events in women with bulimia nervosa. Journal of Abnormal Psychology. 2013;122:111–118. doi: 10.1037/a0029703. doi:10.1037/a0029703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brantley P, Jones G. Daily Stress Inventory: Professional Manual. Psychological Assessment Resources, Inc.; Odessa, FL: 1989. [Google Scholar]
- Brantley PJ, Dietz LS, McKnight GT, Jones GN, Tulley R. Convergence between the Daily Stress Inventory and endocrine measures of stress. Journal of Consulting and Clinical Psychology. 1988;56:549–551. doi: 10.1037//0022-006x.56.4.549. doi:10.1037/0022-006x.56.4.549. [DOI] [PubMed] [Google Scholar]
- Brantley PJ, Waggoner CD, Jones GN, Rappaport NB. A Daily Stress Inventory: Development, reliability, and validity. Journal of Behavioral Medicine. 1987;10:61–74. doi: 10.1007/BF00845128. doi:10.1007/bf00845128. [DOI] [PubMed] [Google Scholar]
- Crosby RD, Wonderlich SA, Engel SG, Simonich H, Smyth J, Mitchell JE. Daily mood patterns and bulimic behaviors in the natural environment. Behaviour Research and Therapy. 2009;47:181–188. doi: 10.1016/j.brat.2008.11.006. doi:S0005-7967(08)00238-6 [pii] 10.1016/j.brat.2008.11.006 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, Mitchell JE. Increased mortality in bulimia nervosa and other eating disorders. American Journal of Psychiatry. 2009;166:1342–1346. doi: 10.1176/appi.ajp.2009.09020247. doi:10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- Crowther JH, Sanftner J, Bonifazi DZ, Shepherd KL. The role of daily hassles in binge eating. International Journal of Eating Disorders. 2001;29:449–454. doi: 10.1002/eat.1041. doi:doi:10.1002/eat.1041. [DOI] [PubMed] [Google Scholar]
- Elliott CA, Tanofsky-Kraff M, Shomaker LB, Columbo KM, Wolkoff LE, Ranzenhofer LM, Yanovski JA. An examination of the interpersonal model of loss of control eating in children and adolescents. Behaviour Research and Therapy. 2010;48:424–428. doi: 10.1016/j.brat.2009.12.012. doi:10.1016/j.brat.2009.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel SG, Boseck JJ, Crosby RD, Wonderlich SA, Mitchell JE, Smyth J, Steiger H. The relationship of momentary anger and impulsivity to bulimic behavior. Behaviour Research and Therapy. 2007;45:437–447. doi: 10.1016/j.brat.2006.03.014. doi:10.1016/j.brat.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Engel SG, Wonderlich SA, Crosby RD, Mitchell JE, Crow S, Peterson CB, Gordon KH. The role of affect in the maintenance of anorexia nervosa: Evidence from a naturalistic assessment of momentary behaviors and emotion. Journal of Abnormal Psychology. doi: 10.1037/a0034010. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelberg MJ, Steiger H, Gauvin L, Wonderlich SA. Binge antecedents in bulimic syndromes: An examination of dissociation and negative affect. International Journal of Eating Disorders. 2007;40:531–536. doi: 10.1002/eat.20399. doi:10.1002/eat.20399. [DOI] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive behavior therapy and eating disorders. Guilford Press; New York: 2008. [Google Scholar]
- Fairburn CG, Marcus MD, Wilson GT. Cognitive-behavioral therapy for binge eating and bulimia nervosa: A comprehensive treatment manual. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. Guilford Press; New York: 1993. pp. 317–360. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition With Psychotic Screen. Biometrics Research, New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- Goldschmidt AB, Peterson CB, Wonderlich SA, Crosby RD, Engel SG, Mitchell JE, Berg KC. Trait-level and momentary correlates of bulimia nervosa with a history of anorexia nervosa. International Journal of Eating Disorders. 2013;46:140–146. doi: 10.1002/eat.22054. doi:doi:10.1002/eat.22054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Pagano ME, Stout RL, Markowitz JC, Ansell EB, Pinto A, Skodol AE. Stressful life events predict eating disorder relapse following remission: Six-year prospective outcomes. International Journal of Eating Disorders. 2012;45:185–192. doi: 10.1002/eat.20909. doi:doi:10.1002/eat.20909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grissett NI, Norvell NK. Perceived social support, social skills, and quality of relationships in bulimic women. Journal of Consulting and Clinical Psychology. 1992;60:293–299. doi: 10.1037//0022-006x.60.2.293. doi:doi:10.1037/0022-006X.60.2.293. [DOI] [PubMed] [Google Scholar]
- Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137:660–681. doi: 10.1037/a0023660. doi:10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann A, Zeeck A, Barrett MS. Interpersonal problems in eating disorders. International Journal of Eating Disorders. 2010;43:619–627. doi: 10.1002/eat.20747. doi:10.1002/eat.20747. [DOI] [PubMed] [Google Scholar]
- Haynos AF, Fruzzetti AE. Anorexia nervosa as a disorder of emotion dysregulation: Evidence and treatment implications. Clinical Psychology: Science and Practice. 2011;18:183–202. doi:doi:10.1111/j.1468-2850.2011.01250.x. [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. doi:10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Hilbert A, Tuschen-Caffier B. Maintenance of binge eating through negative mood: A naturalistic comparison of binge eating disorder and bulimia nervosa. International Journal of Eating Disorders. 2007;40:521–530. doi: 10.1002/eat.20401. doi:10.1002/eat.20401. [DOI] [PubMed] [Google Scholar]
- Hokanson JE, Stader SR, Flynn HA, Tate RL. The daily experiences survey: An instrument for daily recordings of multiple variables associated with psychopathology. Florida State University; 1992. Unpublished manuscript. [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr., Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. doi:10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karr TM, Crosby RD, Cao L, Engel SG, Mitchell JE, Simonich H, Wonderlich SA. Posttraumatic stress disorder as a moderator of the association between negative affect and bulimic symptoms: An ecological momentary assessment study. Comprehensive Psychiatry. 2013;54:61–69. doi: 10.1016/j.comppsych.2012.05.011. doi:10.1016/j.comppsych.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenardy J, Arnow B, Agras WS. The aversiveness of specific emotional states associated with binge-eating in obese subjects. Australian and New Zealand Journal of Psychiatry. 1996;30:839–844. doi: 10.3109/00048679609065053. doi:10.3109/00048679609065053. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Korchmaros JD, Bolger N. Lower level mediation in multilevel models. Psychological Methods. 2003;8:115–128. doi: 10.1037/1082-989x.8.2.115. doi:doi:10.1037/1082-989X.8.2.115. [DOI] [PubMed] [Google Scholar]
- Koo-Loeb JH, Pedersen C, Girdler SS. Blunted cardiovascular and catecholamine stress reactivity in women with bulimia nervosa. Psychiatry Research. 1998;80:13–27. doi: 10.1016/s0165-1781(98)00057-2. doi:doi:10.1016/S0165-1781(98)00057-2. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. From psychological stress to the emotions: A history of changing outlooks. Annual Review of Psychology. 1993;44:1–21. doi: 10.1146/annurev.ps.44.020193.000245. doi:10.1146/annurev.ps.44.020193.000245. [DOI] [PubMed] [Google Scholar]
- Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II). Clinical Psychology and Psychotherapy. 2011;18:75–79. doi: 10.1002/cpp.693. doi:10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- Messerli-Burgy N, Engesser C, Lemmenmeier E, Steptoe A, Laederach-Hofmann K. Cardiovascular stress reactivity and recovery in bulimia nervosa and binge eating disorder. International Journal of Psychophysiology. 2010 doi: 10.1016/j.ijpsycho.2010.07.005. doi:10.1016/j.ijpsycho.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Current Opinion in Psychiatry. 2006;19:438–443. doi: 10.1097/01.yco.0000228768.79097.3e. doi:10.1097/01.yco.0000228768.79097.3e. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Almeida DM. The effect of daily stress, personality, and age on daily negative affect. Journal of Personality. 2004;72:355–378. doi: 10.1111/j.0022-3506.2004.00265.x. doi:doi:10.1111/j.0022-3506.2004.00265.x. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Engel SG, Wadeson A, Crosby RD, Wonderlich SA, Simonich H, Mitchell JE. Emotional states preceding and following acts of non-suicidal self-injury in bulimia nervosa patients. Behaviour Research and Therapy. 2009;47:83–87. doi: 10.1016/j.brat.2008.10.011. doi:10.1016/j.brat.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy R, Straebler S, Basden S, Cooper Z, Fairburn CG. Interpersonal psychotherapy for eating disorders. Clinical Psychology and Psychotherapy. 2012;19:150–158. doi: 10.1002/cpp.1780. doi:10.1002/cpp.1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza JR, Charles ST, Sliwinski MJ, Mogle J, Almeida DM. Affective reactivity to daily stressors and long-term risk of reporting a chronic physical health condition. Annals of Behavioral Medicine. 2012 doi: 10.1007/s12160-012-9423-0. doi:10.1007/s12160-012-9423-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Zhang Z, Zyphur MJ. Alternative methods for assessing mediation in multilevel data: The advantages of multilevel SEM. Structural Equation Modeling: A Multidisciplinary Journal. 2011;18:161–182. doi:10.1080/10705511.2011.557329. [Google Scholar]
- Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychological Methods. 2010;15:209–233. doi: 10.1037/a0020141. doi:10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- Raffi AR, Rondini M, Grandi S, Fava GA. Life events and prodromal symptoms in bulimia nervosa. Psychological Medicine. 2000;30:727–731. doi: 10.1017/s0033291799002019. [DOI] [PubMed] [Google Scholar]
- Selby EA, Doyle P, Crosby RD, Wonderlich SA, Engel SG, Mitchell JD, Le Grange D. Momentary emotion surrounding bulimic behaviors in women with bulimia nervosa and borderline personality disorder. Journal of Psychiatric Research. 2012;46:1492–1500. doi: 10.1016/j.jpsychires.2012.08.014. doi:10.1016/j.jpsychires.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. doi:doi:10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Heron KE, Wonderlich SA, Crosby RD, Thompson KM. The influence of reported trauma and adverse events on eating disturbance in young adults. International Journal of Eating Disorders. 2008;41:195–202. doi: 10.1002/eat.20490. doi:10.1002/eat.20490. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. doi:10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Sliwinski MJ, Crosby RD, Engel SG, Mitchell JE, Calogero RM. Ecological momentary assessment of affect, stress, and binge-purge behaviors: Day of week and time of day effects in the natural environment. International Journal of Eating Disorders. 2009;42:429–436. doi: 10.1002/eat.20623. doi:10.1002/eat.20623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stader SR, Hokanson JE. Psychosocial antecedents of depressive symptoms: An evaluation using daily experiences methodology. Journal of Abnormal Psychology. 1998;107:17–26. doi: 10.1037//0021-843x.107.1.17. [DOI] [PubMed] [Google Scholar]
- Steiger H, Gauvin L, Engelberg MJ, Ying Kin NM, Israel M, Wonderlich SA, Richardson J. Mood- and restraint-based antecedents to binge episodes in bulimia nervosa: Possible influences of the serotonin system. Psychological Medicine. 2005;35:1553–1562. doi: 10.1017/S0033291705005817. doi:10.1017/s0033291705005817. [DOI] [PubMed] [Google Scholar]
- Stein KF, Corte CM. Ecologic momentary assessment of eating-disordered behaviors. International Journal of Eating Disorders. 2003;34:349–360. doi: 10.1002/eat.10194. doi:10.1002/eat.10194. [DOI] [PubMed] [Google Scholar]
- Stein RI, Kenardy J, Wiseman CV, Dounchis JZ, Arnow BA, Wilfley DE. What's driving the binge in binge eating disorder?: A prospective examination of precursors and consequences. International Journal of Eating Disorders. 2007;40:195–203. doi: 10.1002/eat.20352. doi:10.1002/eat.20352. [DOI] [PubMed] [Google Scholar]
- Tiller JM, Sloane G, Schmidt U, Troop N, Power M, Treasure JL. Social support in patients with anorexia nervosa and bulimia nervosa. International Journal of Eating Disorders. 1997;21:31–38. doi: 10.1002/(sici)1098-108x(199701)21:1<31::aid-eat4>3.0.co;2-4. doi:doi:10.1002/(SICI)1098-108X(199701)21:1<31::AID-EAT4>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- Troop NA, Allan S, Treasure JL, Katzman M. Social comparison and submissive behaviour in eating disorder patients. Psychology and Psychotherapy. 2003;76:237–249. doi: 10.1348/147608303322362479. doi:10.1348/147608303322362479. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. doi:doi:10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wheeler L, Reis HT. Self-recording of everyday life events: Origins, types, and uses. Journal of Personality. 1991;59:339–354. [Google Scholar]
- Wolff GE, Crosby RD, Roberts JA, Wittrock DA. Differences in daily stress, mood, coping, and eating behavior in binge eating and nonbinge eating college women. Addictive Behaviors. 2000;25:205–216. doi: 10.1016/s0306-4603(99)00049-0. doi:doi:10.1016/S0306-4603(99)00049-0. [DOI] [PubMed] [Google Scholar]
- Woods AM, Racine SE, Klump KL. Examining the relationship between dietary restraint and binge eating: Differential effects of major and minor stressors. Eating Behaviors. 2010;11:276–280. doi: 10.1016/j.eatbeh.2010.08.001. doi:10.1016/j.eatbeh.2010.08.001. [DOI] [PubMed] [Google Scholar]
- Zunker C, Peterson CB, Crosby RD, Cao L, Engel SG, Mitchell JE, Wonderlich SA. Ecological momentary assessment of bulimia nervosa: Does dietary restriction predict binge eating? Behaviour Research and Therapy. 2011;49:714–717. doi: 10.1016/j.brat.2011.06.006. doi:10.1016/j.brat.2011.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]