Abstract
Activating the immune system for therapeutic benefit in cancer has long been a dream of some immunologists, and even a few oncologists. After decades of disappointment, the tide has finally changed due to the success of recent proof-of-concept clinical trials. Most notable has been the ability of the anti-CTLA4 antibody ipilimumab to achieve significant increases in survival of patients with metastatic melanoma, an indication where conventional therapies have failed. Viewed in the context of advances in understanding of how tolerance, immunity, and immunosuppression regulate anti-tumor immune responses together with the advent of targeted therapies, these successes suggest that active immunotherapy represents a path forward to obtaining durable, long-lasting responses in cancer patients.
The passive transfer of anti-cancer monoclonal antibodies and donor T cells in the context of allogeneic bone marrow transplantation are effective treatments for a variety of hematologic and solid malignancies 1. Although not always thought of as “immunotherapy”, the success of these biotherapeutics likely reflects the ability of the donor cells or antibodies to induce an immediate immune reaction against cancer, bypassing a requirement to activate endogenous immunity. These immune treatments have been well established in oncology for several decades, and continued advances in antibody and T cell engineering should further enhance their clinical impact in the years to come (Box 1).
Box 1. Established immune treatments.
Nine monoclonal antibodies targeting six cancer-associated proteins (Her2/neu, EGFR, VEGF, CD20, CD52, and CD33) are approved for the treatment of solid and hematologic malignancies. In addition to antagonizing oncogenic pathways, these biotherapeutics may act by opsonizing tumor cells and triggering their death or removal by antibody-dependent cellular cytotoxity or phagocytosis 94. Ongoing investigations in murine models and patients raise the possibility that they may also stimulate adaptive immune responses in some settings 95. Recently, the successful conjugation of toxins to antibodies has been achieved, and these have induced clinical responses in patients refractory to the naked antibody 96. The concurrent administration of immunostimulatory cytokines such as IL-2 and GM-CSF may also enhance the efficacy of antibody therapy.
Allogeneic bone marrow transplantation and the infusion of donor lymphocytes can be highly effective therapy for some leukemias and lymphomas 24. The graft-versus-leukemia effects involve direct killing of tumor cells by donor lymphocytes, together with the subsequent induction of broader innate and adaptive reactions. Based on these clinical benefits, many groups are exploring the use of adoptive T cell therapy in the autologous setting. Promising strategies include the use of lymphodepletion prior to T cell infusion, and the engineering of new T cell specificities with chimeric antigen receptors 97.
Other immune treatments that have received FDA approval include recombinant cytokines, such as interleukin-2 (IL-2, Proleukin®), which is used for melanoma and renal cell cancer (RCC). Response rates are low (~15%) and the significant risk of serious systemic inflammation requires administration as an in-patient. Interferon-alpha is another agent that gained approval for “immunologic cancers” (ie melanoma, RCC). Although also associated with low response rates and high dose toxicity, a small subset of melanoma patients who are also pre-disposed to autoimmunity has been shown to exhibit impressive responses in survival 98. It has been difficult to pre-identify these patients, however, limiting the utility of the approach. Yet, when seen, responses are durable, suggesting they reflect active anti-tumor immunity.
In contrast to these passive immunotherapy strategies, the active stimulation of specific and durable anti-tumor immunity has proved elusive. In 1891, a young New York surgeon named William Coley began intratumoral injections of live or inactivated Streptococcus pyrogenes and Serratia marscescens in an effort to reproduce the spontaneous remissions of sarcomas observed in rare cancer patients who had developed erysipelas 2. Given Elie Metchnikoff’s contemporaneous work demonstrating the immune system’s ability to cause inflammation and destroy invading bacteria, “Coley’s toxins” made sense by acting to stimulate anti-bacterial phagocytes that might also kill bystander tumor cells. Some significant responses were recorded over the ensuing 40 years, but successes were sporadic, difficult to reproduce, and not obtained in a scientifically rigorous fashion. One notable exception was in superficial bladder cancer, where the intravesical injection of live bacilli Calmette-Guérin (BCG) after surgical resection was shown to prolong patient survival 3. Other than this particular clinical setting, the approach was never embraced by oncologists who, instead, continued to rely on surgery and increasingly on effective new methods such as radiation therapy and ultimately chemotherapy. Coley’s strategy was further discounted due to the very real risks associated with the administration of infectious or at least pyrogenic agents to already weakened cancer patients, ironic given the trauma associated with the treatments that did come into common use. Thus began the history of cancer immunotherapy. Before continuing with the story, however, it will be useful to summarize what must happen to elicit protective immune responses to cancer, and why overcoming these barriers has been so difficult.
Generating anti-cancer immunity: a multi-step challenge
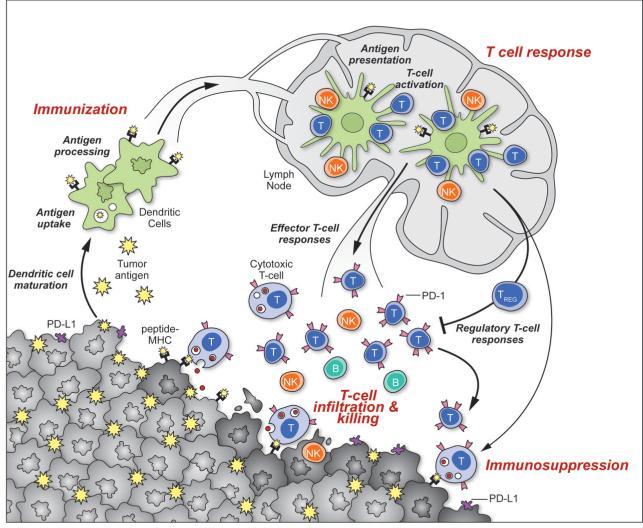
Based on our current understanding of the immune response, one can identify three distinct steps that must be achieved, either spontaneously or therapeutically, in order to mount effective anti-tumor immunity (Fig. 1). To initiate immunity, dendritic cells (DCs) must sample antigens derived from the tumor, which can be ingested in situ or delivered exogenously as part of a therapeutic vaccine. These antigens might reflect one or more of the many mutated proteins typical of cancer, the products of non-mutated genes that are preferentially expressed by cancer cells (eg cancer-testis antigens), or differentiation antigens associated with the cancer’s tissue of origin but against which thymic or peripheral tolerance has been incompletely established (eg melanosome-associated proteins in melanoma) 4,5. Upon antigen encounter, the DCs would also have to receive a suitable activation (“maturation”) signal, allowing them to differentiate extensively to promote immunity as opposed to tolerance including enhanced processing and presentation of tumor antigen-derived peptides 6,7. Activation signals could be therapeutically supplied exogenously (eg Toll-like receptor ligands, agonist antibodies against activating receptors such as CD40) or endogenously: dying or necrotic tumor cells release factors (eg high mobility group proteins, ATP) thought to result in the immunogenic maturation of DCs. In addition, tumor cells appear to ectopically express ER proteins on the plasma membrane (eg calreticulin) that promote their phagocytosis, possibly enabling presentation of tumor antigens on MHC class I and class II molecules. Some forms of chemotherapy or targeted therapy may promote a more immunogenic phenotype 8.
Figure 1. Generation and regulation of anti-tumor immunity.
Understanding the events in generating and regulating anti-tumor immunity suggests at least three sites for therapeutic intervention: promoting the antigen presentation functions of DCs, promoting the production of protective T cell responses, and overcoming immunosuppression in the tumor bed. Anti-tumor immune responses must begin with the capture of tumor-associated antigens by DCs, either delivered exogenously or captured from dead or dying tumor cells. The DCs process the captured antigen for presentation or cross-presentation on MHC class II and class I molecules (respectively) and migrate to draining lymph nodes. If capture and presentation occurred in the presence of an immunogenic maturation stimulus, DCs will elicit anti-cancer effector T cell responses in the lymph node; if no such stimulus was received, DCs will instead induce tolerance leading to T cell deletion, anergy, or the production of Tregs. In the lymph node, antigen presentation to T cells will elicit responses depending on the type of DC maturation stimulus received and on the interaction of T-cell costimulatory molecules with their surface receptors on DCs. Thus, interaction of CD28 or OX40 with CD80/86 or OX40L will promote potentially protective T cell responses, while interaction of CTLA4 with CD80/86 or PD-1 with PD-L1/PD-L2 will suppress T cell responses, and possibly promote Treg formation. Antigen-educated T cells (along with B cells and NK cells) will exit the lymph node and enter the tumor bed, where a host of immunosuppressive defense mechanisms can be produced by tumors (or infiltrating myeloid cells) that oppose effector T cell function. These include the upregulation of PD-L1/L2 on the cancer cell surface, release of PGE2, arginase and IDO (all T cell suppressors), and the release of VEGF (triggered in part by intratumoral hypoxia), which inhibits T cell diapedesis from the vasculature and thus infiltration into the tumor bed.
Next, in lymphoid organs, tumor antigen-loaded DCs must generate protective T cell responses 9. The precise type of T cell responses needed is unknown, but certainly they must include the production of CD8+ effector T cells with cytotoxic potential. DCs may also trigger antibody and NK/NKT cell responses, which may contribute to tumor immunity. The lymph node is a second potential site for therapeutic intervention, providing agents that may help guide the T cell response. However, the DCs are again key players as they must have been matured by a stimulatory adjuvant in order to have a chance at eliciting the desired T cells. Presentation of antigens by DCs at the steady state (i.e. DCs that have not received an immunogenic maturation signal) promotes tolerance by regulatory T cell (Treg) production 10-13, which would oppose an anti-tumor response.
Finally, cancer-specific T cells must enter the tumor bed to perform their function. Here, there is the challenge of immune suppression (Box 2). Tumors may, presumably by skewing DC maturation, prevent immunizaton, trigger the “wrong” immune response, or enable the local accumulation or expansion of Tregs that would oppose the activity of effector T cells. Indeed, infiltration of Tregs correlates with poor prognosis in a variety of epithelial tumor types 14,15. Tumors may downregulate their expression of MHC class I molecules or their expression of target tumor antigens and can also produce a variety of surface molecules (eg PD-L1, -L2) that engage receptors on the surfaces of activated T cells (PD-1), causing T cell anergy or exhaustion 16,17. Expression of such suppressive ligands can be associated with oncogenic mutations seen in many cancers (eg PTEN loss) 18. Additionally, tumors can release immunosuppressive molecules, such as indoleamine 2,3-dioxygenase (IDO) which consumes tryptophan and limits T cell function 19,20. Myeloid-derived suppressor cells can also be recruited into the tumor, and release additional T cell suppressors such as arginase and nitrous oxide synthase 21. Hypoxia in the tumor microenvironment may promote the generation of adenosine, which similarly inhibits effector T cell function 22. Hypoxia can also lead to the production of CCL28, which attracts immigration of Tregs 23. Finally, tumor stroma cells can also suppress the function of effector lymphocytes. For example, mesenchymal stem cells block proliferation and function of effector T cells 24, while tumor vascular cells can suppress T cell adhesion (to tumor endothelium) and prevent homing to tumors, an effect in part mediated by vascular endothelial growth factor (VEGF) 25 as well as by the endothelin-B receptor (ETBR, also known as EDNRB)26.
Box 2.
Tumors escape immune attack by a variety of complementary mechanisms of immunosuppression, many of which operate in parallel. Among paracrine mediators, adenosine, prostaglandin E2, TGF-β, and VEGF-A exert multiple direct and indirect immunosuppressive activities. These mediators may function in the suppression of DCs, indirectly inhibiting T cell penetration into the tumor bed, or directly suppressing effector T cell activation while enhancing the function of Tregs. For example, adenosine, released by tumour cells under hypoxia, contributes to the suppression T cell activation, and Treg expansion. VEGF-A can also suppress proper T cell development and function: VEGF-A treatment of mouse splenocytes during T cell stimulation was shown to induce IL-10 production from T cells while suppressing IFN-γ production 99. Tumor cells can also directly escape T cell recognition by downregulating MHC class I or by disabling other components of the antigen processing machinery. Shedding of soluble NKG2D ligands such as MIC-A or MIC-B can severely compromise the ability of effector T cells to function in the tumor microenvironment. In addition, tumor cells may upregulate surface ligands, which mediate T cell anergy (or exhaustion), including PD-L1 and other ligands to inhibitory T cell receptors. A variety of leukocyte subsets infiltrating tumors are able to suppress T cell function as well. In addition to Tregs, accumulation of which in tumors correlate with a poor prognostic outcome14, other suppressive lymphocyte subsets have been reported including IL-10 producing B cells and B regulatory cells, type II NKT cells, NK cells and γδ T cells. Myeloid lineage cells also promote immune suppression in tumours. Chief among them are the poorly understood myeloid-derived suppressor cells or MDSCs100. Their characterization is ultimately based on their ability to suppress T and NK cell activation, likely through several mechanisms including nitric oxide (NO), reactive oxidative species (ROS), arginase, interleukin 10 (IL-10) and transforming growth factor beta (TGF-β); there are also reports that MDSCs may specifically induce the expansion of Tregs. Finally, tumor stroma cells play important immune modulatory role. The so-called cancer-associated fibroblasts (CAFs) can promote the recruitment and function of immunosuppressive cells through the secretion of CCL2 and CXCL12. In addition, they can suppress T effector cells through secretion of TGF-β. Finally, myeloid-derived mesenchymal stem cells exert important immunosuppressive functions by blocking proliferation and function of T effector cells. Further study is needed to determine which of these mechanisms are most important in general, and which determine the immune status in individual patients.
Thus, the deck appears stacked against the success of immunotherapy. Any approach would have to overcome several significant barriers: the fact that tumor-associated antigens are typically closely related or identical to self antigens, that it will be very difficult to separate therapeutic responses from pathological autoimmune responses, that both central and peripheral tolerance would have conspired to deplete or inactivate the relevant T cell repertoire, and that the tumor microenvironment is inherent immunosuppressive. Yet, there now appears to be a path to clinical success.
Cancer vaccines are finally showing early signals of activity
Vaccines come in two formats: prophylactic and therapeutic 9. Prophylactic (or preventative) vaccines have been used with considerable success in preventing cancers of viral origin, such as HBV and HPV, where the etiologic agent is known. In contrast, the development of therapeutic vaccines to treat existing disease has proved problematic. The long history of failure has tainted the entire strategy of immunotherapy in the eyes of many oncologists.
The idea of a therapeutic cancer vaccine originated with the discovery that patients can harbor CD8+ and CD4+ T cells specific for cancer-testis or differentiation antigens expressed in their tumors 4. Vaccination might reasonably be expected to amplify the frequency and strength of these pre-existing responses or perhaps induce some de novo reactions. Additionally, clinico-pathologic studies have demonstrated a strong association between prolonged patient survival and the presence of intra-tumoral CD3+ or CD8+ cytotoxic T cells and an interferon-gamma (IFN-γ) gene signature 27,28. Thus, if vaccination could trigger these types of T cell responses, then clinical benefit might be expected.
Unfortunately, the many initial attempts were compromised by a poor understanding of the mechanism of immunization, specifically the role of DCs. Mostly conducted by academic groups, thousands of patients were treated with vaccines consisting of short peptides, often without an effective DC-activating adjuvant 29. Free peptides likely have poor pharmacokinetic properties and may be rapidly cleared before being loaded onto DCs, where their half-life may also be short. Without an adjuvant, the DCs might well remain in the steady state and promote tolerance as much as immunity. As a result, there typically was poor immunization, infrequent responses to the selected tumor antigens (assuming they were even the correct ones), and minimal therapeutic benefits. Recently, however, the co-administration of IL-2 as an immune stimulant with a short peptide derived from gp100, a melanocyte differentiation antigen, was shown under some conditions to augment tumor responses and prolong progression-free survival compared to IL-2 alone in advanced melanoma patients 30. These findings suggest that increasing immune activation with peptide vaccines is a critical step for improving therapeutic efficacy.
Since the importance and function of DCs in stimulating T cell responses is now well known, current vaccine trials are more rationally designed. One potentially promising approach involves the use of peptides (~20-mer) that are somewhat longer than bind to MHC class I molecules (10-12-mer). In the presence of a suitable DC-activating adjuvant, these peptides are thought to be more efficient at generating effector T cells, perhaps because some processing may be required. A recent study of peptides derived from the HPV-16 E6 and E7 viral oncoproteins administered in incomplete Freund’s adjuvant showed clinical responses in 15 of 19 women with vulvar intraepithelial neoplasia 31. Tumor regressions were associated with the generation of HPV specific, IFN-γ producing CD4+ and CD8+ T cells. These favorable results might reflect in part the selection of viral gene products for immunization, since these proteins might be more readily recognized as foreign by the host. Indeed, a small trial of long peptides derived from p53, a tumor suppressor often mutated in cancer, delivered in Montanide (an emulsion-adjuvant) induced a weaker IFN-γ producing T cell response and no tumor regressions in advanced ovarian cancer patients, indicating the need to further optimize these formulations or that p53 is simply not sufficiently immunogenic in this setting; in contrast to viral antigens, p53 might also have to break pre-existing tolerance to self 32.
Full-length proteins are also being explored as targets for cancer vaccinations, as they contain a broader profile of epitopes that might be presented by DCs. Among these approaches, GlaxoSmithKline (GSK) is currently conducting a massive (>2500 patients) randomized Phase III trial using a recombinant fusion protein encoding a single cancer-testis antigen (MAGE-A3) in HLA-A2-positive NSCLC patients, together with their ASO2B adjuvant consisting of a saponin/lipid-A emulsion combined with TLR4 and TLR9 agonists. Initial read-outs from a Phase II trial (180 patients) showed some survival response (27%) but this was not sufficient to reach statistical significance 33. Objective T cell responses were not reported, nor were data on the level or homogeneity of MAGE-A3 expression in the study group; this latter parameter might be especially important, since immune attack on subpopulations of lung cancer cells that lack MAGE-A3 would require diversification of the T cell response to additional cancer antigens.
Another target that has attracted some attention is the antigen receptor on B cell lymphomas (idiotype), which is an example of a clonally expressed tumor-specific antigen. Three randomized Phase III trials testing recombinant idiotypes (prepared individually for each patient) administered with GM-CSF (to attract DCs) were undertaken. One trial in which eligibility was restricted to subjects who first achieved a complete response to cytotoxic chemotherapy suggested that vaccination might prolong progression-free survival. However, the two other studies failed to reveal a clinical benefit, which might reflect differences in patient populations, vaccine manufacturing methods, or that the approach is not sufficiently robust 34.
Viral vectors encoding tumor antigens are another vaccine platform undergoing evaluation. These strategies exploit the strong immune responses directed against viral components to enhance reactivity against the cancer antigen. One such 125-patient Phase II trial, conducted by Bavarian-Nordic and the US National Cancer Institute, involved an initial inoculation of a recombinant vaccinia virus encoding prostate specific antigen (PSA) and the adhesion molecules B7.1, ICAM-1, and LFA-3; a similarly configured fowlpox vector was administered subsequently in a prime-boost strategy, and GM-CSF was administered with the vectors for further immune stimulation (the entire vaccine product is termed PROSTVAC). In addition to reactivity against the pox viral gene products, the introduction of the adhesion molecules in the infected cells was intended to have them serve as surrogate DCs, although the specializations of DCs for T cell stimulation extend well beyond these three adhesion molecules. While there was no impact of vaccination on progression-free survival, there was an overall survival benefit: 25.1 months vs 16.6 months in the control group (patients treated with empty vector plus saline) 35. A larger Phase III trial is planned using vector alone, vector plus GM-CSF (as a DC adjuvant or attractant), or empty vector plus GM-CSF.
A variety of earlier stage trials are also in progress, using defined antigens that are delivered to DCs by coupling to DC-targeted monoclonal antibodies (eg DEC-205) or further peptide and viral vector trials, in conjunction with various adjuvants. The ability of these approaches to facilitate durable anti-cancer immune responses particularly on their own, however, remains to be demonstrated.
Another strategy for vaccine therapy involves the use of cell-based approaches. One of the ideas underlying this strategy is that an actual cancer cell would already harbor a wide range of tumor-associated antigens (including mutant proteins), so that if used as a vaccine the problem of antigen selection would be reduced. A meta-analysis of 173 published peer-reviewed immunotherapy trials in various solid tumor types revealed that patients immunized with whole tumor antigen had low but significantly higher rates of objective clinical response (8.1%) than patients immunized with molecularly defined tumor antigens (3.6%) 36. Although autologous tumor cells are the best choice of immunogen for this approach, the complexities of vaccine manufacture for individual patients led to the application of allogeneic tumor cell lines. Among these strategies, the one that progressed farthest into clinical development was GVAX® for prostate cancer, advanced by the now-defunct Cell Genesys. The vaccine product was comprised of two prostate cancer cell lines that were stably engineered to secrete GM-CSF. After promising early hints, GVAX® failed in Phase III trials due to lack of clinical efficacy 37; this failure might reflect a lack of sufficient immunogenicity of the approach, alterations in preparation of the vaccine product necessitated by commercial scale-up, or the inability of allogeneic tumor cell lines to represent adequately the spectrum of antigens characteristic of individual prostate cancers in patients.
There has also been considerable interest, particularly among academic groups, in developing DC-based vaccines. In this approach, DCs are isolated from a cancer patient, loaded with antigens (peptides or even tumor cell lysates) ex vivo, activated, and then re- infused back into the patient 9,38. Although there have been some promising hints of efficacy and responses, as yet no clearly positive studies have been reported and the approach has not gained broad support from the biotech-pharmaceutical industry, given the complexities of cell isolation, ex vivo manipulation, and re-infusion. There is one notable exception, however, as will be discussed shortly.
In general, the barriers to success, or at least to quantifying the success, of cancer vaccines administered as “single agents” are many. First, the criteria for defining optimal tumor antigens remain to be fully defined 39,40. Mere expression in the target tumor population may be inadequate for predicting the ability to generate protective T cell responses. Identification of peptides bound to MHC class I on the tumor by mass spectroscopy can identify those antigens that yield potential targets 41, but these peptide-MHCI complexes might still not be sufficiently immunogenic rejection antigens (ie able to generate effective T cell responses). Moreover, antigen expression within a tumor bed can be heterogeneous. Even the allogeneic tumor cell line based approaches are limited by the fact that a given patient’s tumor is likely to harbor mutations that are not found in the vaccine product. Second, the optimal adjuvant for producing anti-tumor CD8+ T cell responses that can be used safely and effectively in humans is not yet clear. The desired adjuvant (or adjuvant combination) will be one capable of triggering the maturation of DCs to a state where they can facilitate the generation of tumor-reactive, CD8+ cytotoxic T cells. Finally, although it is likely that conditions for immunization will eventually be optimized, the effectiveness of a tumor- specific T cell population may still be limited by the multiple mechanisms of immunosuppression used by tumors to guard against T cell killing. These are not reasons to eliminate a vaccine arm from consideration as part of an immunotherapy, but rather to highlight some of the difficulties in assessing success in the absence of other immunomodulatory agents. Like with all forms of targeted therapy in cancer, the discovery and application of predictive biomarkers or diagnostics, which could identify those patients most likely to benefit from a given vaccine, will be an important challenge for future development.
Provenge®: an efficacious cell-based vaccine for prostate cancer, but how does it work?
Questions of mechanism notwithstanding, a fact of drug development is that performance in the clinic is the final arbiter of success. The first validation of active immunotherapy as a viable approach to cancer treatment was the FDA approval in April 2010 of Provenge® (sipuleucel-T) for advanced prostate cancer. What is Provenge®? Originally assumed to be an autologous DC-based vaccine 42 (it was developed by the eponymously named company, Dendreon), Provenge® actually comprises an incompletely characterized, complex mixture of peripheral blood mononuclear cells (PBMC) supplemented with a cytokine and tumor-derived differentiation antigen. In the pivotal Phase III trial 43, total PBMC were collected from patients by leukopheresis at weeks 0, 2, and 4 and then cultured for 36-44 hr at 37°C in medium containing a fusion protein composed of prostatic acid phosphatase (PAP; a tumor-associated differentiation antigen) and GM-CSF prior to reinfusion. This was compared against a placebo that was prepared by incubating one-third of the leukopheresis product for 36-44 hr at 2°C-8°C without exposure to the fusion protein (the remaining two-thirds were cryopreserved to allow for subsequent vaccine manufacture in a salvage protocol). Thus, the control not only lacked the presumptive immunizing antigen but was also processed somewhat differently.
The clinical results showed little evidence of tumor shrinkage or delay in disease progression. By standard RECIST criteria, only 1 of the 341 patients in the active arm exhibited a partial response. 2.6% showed at least a 50% reduction in PSA levels on at least two visits, vs 1.3% in the placebo group. Nevertheless, a 4.1 month improvement in median survival was achieved (25.8 vs 21.7 months), deemed significant by the FDA in a patient population that has few if any other effective therapeutic options.
While Provenge® is clearly a cell-based therapy, how does it work? Although a majority (66%) of the survivors exhibited an antibody response to the fusion protein, the fraction of patients producing antibodies that recognized endogenous PAP was much lower (28.5%). Moreover, T cell responses to either the fusion protein or PAP were not associated with survival. These discrepancies might reflect a limitation of monitoring anti-tumor immune responses in the peripheral blood, as compared to the tumor microenvironment. However, they also raise the possibility that other undefined factors in the cellular product may play an important role. Further studies are required to understand the therapeutic mechanism of Provenge®, and to define the impact of the different cell processing procedures on the placebo product.
The lack of tumor shrinkage, long the sine qua non for gauging cancer therapy, in the face of a survival benefit is surprising but perhaps not unexpected for immunotherapy. As seen pre-clinically, an effect on pre-existing tumors due to immune manipulations can be delayed while an immune response develops 44,45. Furthermore, biopsies of metastases after vaccination in some clinical trials revealed the presence of immune infiltrates that mediate tumor destruction in association with extensive edema, which may be followed by fibrosis 46. These histopathologic findings suggest that monitoring tumor size alone may be inadequate for assessing the overall therapeutic effects of vaccination. As discussed below, these considerations apply to the evaluation of CTLA-4 antibody blockade, highlighting the need to modify tumor response criteria in light of new insights into the biology of immunotherapy 44.
Adoptive lymphocyte therapy: A panacea?
Adoptive transfer of lymphocytes with tumoricidal properties can, in theory, bypass the daunting task of breaking tolerance to tumor antigens and generating a high frequency of high avidity effector T cells. The discovery that host lymphodepletion facilitates engraftment of adoptively transferred T cells has enabled the successful transfer of ex vivo expanded TILs from patients with melanoma, with dramatic clinical responses, some of which are complete and durable 47,48.
Advances in T cell culturing methods and T cell engineering through retroviral vectors carrying cloned T cell receptors (TCRs) or chimeric antigen receptors (CARs) enriched by costimulatory signaling domains has expanded the opportunities for adoptive T cell therapy beyond patients with resectable tumors harboring reactive T cells to a larger population with solid tumors expressing the cognate target(s) 49. The advent of CARs bypasses also the need for tumor cells to possess a functional antigen processing machinery and express antigen through MHC class I or II molecules, as transduced T cells can recognize the intact surface protein through the affinity domain (usually a scFv antibody) of the artificial CAR. Early clinical results appear very promising 50,51 . However, safety issues surrounding the selection of the target, the paucity of such targets, manufacturing complexities and costs, and the lack of durable responses in many patients indicates that additional interventions are required to properly direct and activate T cells in the tumor microenvironment.
A far more convenient approach to the same end may be the therapeutic use of bispecific antibodies that engage both the TCR and an antigen on the tumor cell surface. In B cell lymphoma and leukemia, this approach has been applied with impressive success in the clinic by MicroMet 52. However, the platform has a number of liabilities including neurotoxicity and the necessity for continuous pump-mediated infusion due to the very rapid clearance of the antibody fragment. Nevertheless, such bispecific antibodies further emphasize that it may prove possible to repurpose T cell specificity for therapeutic benefit.
Ipilimumab: from vaccination to immune modulation to effective therapy
The most important development for cancer immunotherapy, and hopefully for the benefit of many cancer patients, was the recent readout of the ipilimumab Phase III trials in late stage metastatic melanoma. Not only was a clear survival advantage observed for a patient group with no other therapeutic options, but it was achieved with an agent whose mechanism of action is virtually certain to involve the modulation of endogenous T cell responses. The results were deemed significant enough that in March of 2011, the FDA granted broad approval for patients with metastatic melanoma, either as initial therapy or after relapse.
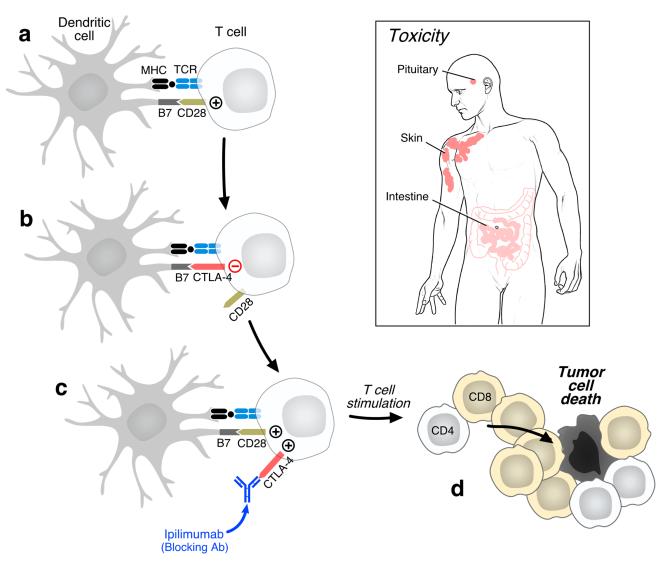
Ipilimumab is a monoclonal antibody to CTLA4, whose role in regulating T cell function has been well studied for many years by a number of groups, notably that of James Allison and colleagues 53. CTLA4 is a key negative regulator, being recruited to the plasma membrane upon T cell activation where it binds to members of the B7 family of accessory molecules expressed by DCs and other antigen presenting cells (Fig. 2). CTLA4 ligation effectively inhibits further activation and expansion, thereby controlling the progress of an immune response and attenuating the chances for chronic autoimmune inflammation. The negative regulation is overcome by use of a blocking antibody. The fundamental importance of CTLA4 to controlling T cell function is well illustrated by the phenotype of CTLA4-/- mice, which die of an aggressive lymphoproliferative disorder at a young age 54,55. Interestingly, CTLA4 ligation is also important for the immune suppressive function of Tregs, further assisting to dampen T cell responses 56. Treg function is thus also thought to be blocked by anti-CTLA4.
Figure 2. Biologic activities of CTLA-4 antibody blockade.
Upon encountering a dendritic cell presenting a cognate tumor antigen-derived peptide epitope and expressing B7 costimulatory molecules (CD80, CD86), specific anti-tumor T cells become activated through TCR and CD28 signaling. CTLA-4 is subsequently upregulated and preferentially engages B7 to attenuate T cell responses. Ipilimumab blocks CTLA-4 function, thereby allowing for enhanced T cell stimulation and more potent anti-tumor reactions. Ipilimumab may also antagonize CTLA-4 on regulatory T cells to limit their ability to suppress anti-tumor T cell effector responses (not shown). CTLA-4 antibody blockade compromises tolerance to some normal tissue antigens, provoking inflammatory toxicities that can especially impact the skin, pituitary gland, and intestine in human patients.
The rationale for using anti-CTLA4 in cancer therapy was to unrestrain pre-existing anti-cancer T cell responses and possibly trigger new responses. Indeed, it is well known for melanoma (and other diseases) that tumor-infiltrating lymphocytes (TILs) exist, and that they can bear specificity for tumor antigens 4,57-59. Pre-clinical studies using mouse models were promising, leading two companies (Pfizer and BMS/Medarex) to put two different anti-CTLA4 antibodies into the clinic. Phase II trials failed to reach their endpoints of tumor regressions, but BMS/Medarex felt there was sufficient potential for a long term benefit that a lengthy randomized Phase III trial was initiated in relapsed-refractory metastatic melanoma patients to determine overall survival. Their antibody, ipilimumab, was given to one arm, antibody plus a short peptide (gp100) for a melanoma differentiation antigen to a second arm, and the control arm received the short peptide alone. Although the Kaplan-Meier plots of survival were inseparable for the first several months, a two-fold survival benefit was detected at 12-15 months in both antibody arms, which was durable out >2.5 years and included some complete responses (cures?) 60.
In a second BMS/Medarex randomized trial involving 502 patients with previously untreated metastatic melanoma, the addition of ipilimumab to the standard therapy of dacarbazine was shown to improve overall survival compared to dacarbazine alone (11.2 months versus 9.1 months); the combination treatment also significantly increased the proportion of surviving patients with at least three years of follow-up (20.8% versus 12.2%) 61. Although only a relatively small fraction of patients derived clinical benefit, these studies clearly establish ipilimumab as an active agent, which offers patients at what is normally the terminal stage of this disease, clinically meaningful benefits and the possibility for long-term survival. Furthermore, the results validate the idea that activating the T cell compartment can on its own provide significant therapeutic effect.
The use of ipilimumab does present some clinical and scientific challenges. First is the rather significant rate of on-target toxicities observed. Up to 23% of the ipilimumab-treated patients developed serious (grade 3-4) adverse events including colitis and hypophysitis due to induced inflammation (possibly autoimmune in nature), and in conjunction with dacarbazine, ~20% showed significant elevations of liver function tests. Toxicity does not accurately predict positive therapeutic outcome, however, indicating that many patients will experience inflammatory pathology without benefiting from an anti-tumor effect. These toxicities might be expected given the fact that the removal of CTLA4 from mice leads to virulent inflammatory disease, as mentioned earlier. The different spectrum of toxicities with ipilimumab compared to standard cancer treatments also means that practicing oncologists will need to acquire additional expertise in the management of inflammatory disorders.
A second clinical challenge with ipilimumab relates to the kinetics of the anti-tumor response. In contrast to conventional cytotoxic therapies that may trigger rapid tumor shrinkage due to direct killing of cancer cells, the stimulation of T cell responses with ipilimumab may take several months to occur. Tumors may increase in size during this period, and some component of this growth may reflect the consequences of an evolving inflammatory reaction. Indeed, as many as 10% of patients treated with ipilimumab who were scored with progressive disease using the modified WHO criteria for tumor size were shown to achieve disease stabilization and prolonged survival 44,60. This unusual pattern of treatment response has led to the proposal of new immune-related criteria that may aid clinical decision-making regarding continuation of therapy 62. [Box 3]
Box 3. Clinical assessment of immunotherapy.
Oncologists traditionally evaluate the activity of cancer therapies through measurements of tumor area or volume. These standard metrics include the Response Evaluation in Solid Tumors (RECIST) and modified World Health Organization (mWHO) criteria. Clinical responses to cytotoxic treatments such as chemotherapy, radiation therapy, and some targeted agents usually occur quickly (within a few weeks to months) because their presumed mechanism of action involves a direct effect on tumor cells. Moreover, these treatments generally result in a reduction in tumor size, as cancer cells undergo apoptosis or other modes of programmed cell death. Although tumor regressions indicate a beneficial impact of therapy, this may not always translate into improvements in survival due to the potential emergence of lethal, drug resistant cells. Immunotherapy induced tumor destruction, in contrast, may be delayed or even preceded by a period of apparent tumor growth. In clinical trials of ipilimumab, 10-20% of patients showed an increase in tumor size when evaluated three months after starting treatment, but subsequently achieved prolonged tumor control or regression without any additional intervention. These subjects demonstrated comparable long-term survival as those with more rapid tumor regressions. The mechanisms underlying the delayed responses are not yet well understood, but might include the effects of immune infiltrates in tumors or just the long period of time required to generate sufficient T cells to accomplish tumor killing. This distinctive biology has led to the proposal of immune-related response criteria (irRC)40, which allow for greater flexibility in following increases in tumor size during immunotherapy prior to declaring treatment failure.
The rationale of ipilimumab monotherapy is that its use thus far assumes that tumor protective T cells exist in the patient prior to therapy, and that these cells will exert anti-tumor activity if CTLA4 is blocked. The above clinical studies were carried out without concomitant effective immunization. An uncoupled peptide to the melanoma differentiation antigen epitope was included in some arms, but dosed without adjuvant or DC maturation agent. Although CTLA4 would be expected to be induced on tumor-reactive T cells only after immunization, clinical responses observed in the absence of prior exogenous vaccination indicates that tumor reactive TILs expressing CTLA4 are responsive to checkpoint blockade and acquire effective tumor rejecting functions. The notion of exogenous versus endogenous vaccination will be further discussed below.
Despite these limitations, ipilimumab provides realistic hope for melanoma patients, particularly those with late stage disease who otherwise had little if any hope at all. More broadly, it provides clear clinical validation for cancer immunotherapy in general. The results will also intensify the search for predictive biomarkers for positive responders. Other applications of ipilimumab are already being vigorously pursued and, indeed, the door has been opened for the development and investigation of a host of other potential immunotherapeutic strategies, some of which may prove both more effective and safer than targeting CTLA4. At long last, there is now also the prospect for combining with other immunotherapeutic regimens, such as effective vaccination, which arguably should have been considered much earlier in the >10 year clinical study history of anti-CTLA4.
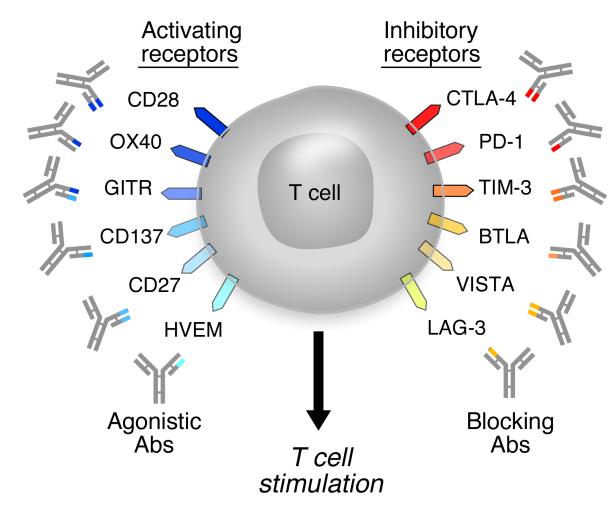
Next generation T cell immunomodulators
The success of anti-CTLA4 in melanoma should create interest in evaluating other antibodies that can be used to activate T cell responses. There are a number of known receptors that could serve as targets for agonist antibodies, including 4-1BB, OX40, GITR, CD27, and CD28 (Fig. 3). The latter, however, also introduces a cautionary note since in an early clinical trial of an agonist anti-CD28 (TGN1412), severe toxicities and even deaths resulted from unexpected cytokine release 63. These serious events emphasize the power of the immune system and the need for extreme care and a conservative trial design when employing any immune activator. The use of agents that clear more rapidly from the circulation than intact IgG’s may help mitigate the potential for such toxicities, or at least enable the more rapid removal of the inducing drug. The same consideration may apply to anti-CTLA4 therapy, where alternative dosing strategies may serve to increase its therapeutic index.
Figure 3. T cell targets for immunoregulatory antibody therapy.
In addition to specific antigen recognition through the TCR, T cell activation is regulated through a balance of positive and negative signals provided by costimulatory receptors. These surface proteins are typically members of either the TNF receptor or B7 superfamilies. Agonistic antibodies directed against activating costimulatory molecules and blocking antibodies against negative costimulatory molecules may enhance T cell stimulation to promote tumor destruction.
LAG-3 is another T cell receptor that, like CTLA4, is largely suppressive. Less well studied than CTLA4, LAG-3 appears similar in that it acts to limit the activity of CD4+ and CD8+ T cells, and augment the activity of Tregs 64,65. There is also a significant intracellular pool of LAG-3, like CTLA4 66. However, the functional consequences of its deletion are far less dramatic in that it may have to work in concert with other regulatory molecules (eg, PD-L1) 67. This situation suggests, however that antagonizing LAG-3 may provide an alternative to antagonizing CTLA4, and perhaps with a better safety profile.
Another attractive approach that is also beginning to receive some clinical validation is targeting immunosuppression in the tumor bed. Even if a vaccine or T cell modulation therapy is successful, the ability of tumors to counteract immune effectors may act to limit clinical benefit. Of current clinical interest is the PD-1/PD-L1(-L2) axis. PD-1 is expressed by T cells, particularly activated T cells, and binds to its ligands PD-L1/L2 that can be expressed by potential target cells, thereby rendering the T cell unresponsive or “exhausted” 68. This axis is well characterized as limiting T cell responses in chronic virus infection 69, but increasingly it is thought to play a role in limiting immune responses in cancer as well 70. A variety of tumors, including melanoma, ovarian, renal, hepatocellular, and glioblastoma, have been found to express PD-L1 (and occasionally PD-L2). Indeed, PD-L1 expression has been found to correlate with poor prognosis 71,72, and also to be increased upon activation of the oncogenic PI3K pathway (eg, by PTEN deletion) 18. Antibodies to PD-1 have reached the clinic, and in early Phase I trials they have displayed good activity in a variety of cancer types, and at least thus far, with a toxicity profile that appears safer than ipilimumab 73. The reduced toxicity is consistent with the generally milder autoimmune phenotype seen in PD-1−/− mice 68 as compared to CTLA4−/− mice. However, the lung inflammation and cardiomyopathy observed in mice 74,75 may prove to be a concern in the clinic. An important biologic and clinical question is whether the effector function of tumor reactive TILs coexpressing multiple inhibitory receptors can be fully recovered by targeting a single receptor or whether combinatorial checkpoint blockade is required for sustained tumor protection.
Other potential approaches to T cell immunosuppression would include targeting Tregs for inactivation or depletion, since in many tumor beds, the infiltration of Tregs may act to oppose effector T cell function as much as the presence of negative regulatory molecules on the surface of effector cells (eg PD-1). While no specific surface marker of Tregs has yet been identified, some proteins such as GITR and OX40 may be transiently expressed, possibly enabling them as targets (although they are also expressed by activated effector T cells in humans) 76,77. Anti-CD25 antibodies may preferentially deplete Treg, at least following shortterm therapy, and may help increase the efficacy of active immunization 78. Finally, low dose cyclophosphamide may preferentially target Treg and allow for attenuation of Treg in the context of immunization protocols 79,80.
As mentioned earlier, tumor beds can produce a number of soluble mediators that counteract T cell function such as IDO, arginase, and PGE2 81. To the extent that these agents can be diagnostically demonstrated as predictive biomarkers, efforts to inhibit their activities with either small molecule or antibody antagonists might also be useful additions to a portfolio of cancer immunotherapeutics. Further, as knowledge on the immunoregulatory function of tumor vasculature increases, therapeutic maneuvers “normalizing” the tumor vessels appear interesting to combine with immunotherapy. Indeed, VEGF blockade has resulted in increased T cell homing to tumors 82 and has enhanced the efficacy of immunotherapy in the mouse 83. Lastly, the importance of tumor-promoting inflammatory pathways such as STAT3 and NF-κB signaling, and cytokines including IL-6, IL-17, IL-23, and TNF-α has been demonstrated 84. Inhibition of these circuits might not only antagonize tumor progression, but also enhance the activity of immunotherapy.
Combination immunotherapy
The use of combinations of chemotherapeutic drugs has traditionally been a mainstay of oncology. Even in the relatively recent age of molecularly targeted therapies, the development of combinations is proving to be of benefit to broaden responses as well as to treat resistance. The difference is that, in theory, combinations of targeted agents can be combined rationally, in a scientifically guided fashion. There is no reason to believe that the same will not hold true for immunotherapy.
In melanoma, there has been another recent success in the small molecule realm. For patients bearing the V600E activating mutation of B-Raf, the Roche inhibitor vemurafenib has been shown to yield dramatic responses in up >50% of patients 85. Yet, resistance develops rapidly (<1 year) creating the necessity for an additional therapy. Although one likely effective approach is to add a second small molecule inhibitor to MEK, to prevent the tumor from activating a compensatory pathway, one might predict the tumor will circumvent this strategy as well. Therefore, the prospect of generating long-lasting protective immunity during the remission period is intensely attractive and trials combining ipilimumab with vemurafinib are in the planning stages. Since the vemurafinib-induced death of the tumors can be expected to release endogenous tumor antigens, it is possible that the small molecule and immunotherapeutic approaches may synergize, with B-Raf inhibition acting to help prime de novo T cell responses that can then be facilitated by the anti-CTLA4. Success, however, makes the assumption that the B-Raf inhibitor is not suppressive of immune responses under the conditions that the two agents would be combined in the clinic.
In this and all other instances where immunotherapeutics are to be combined with targeted or chemotherapeutic agents, it will be critical to assess the potential interactions of the combination(s). Small molecule inhibitors, and cytotoxic chemotherapy alike, may act on cells of the immune system to block DC or T cell function, or modify the tumor or tumor microenvironment in a fashion that will antagonize the development of immunity. Alternatively, conditions may be found where such inhibitors or cytotoxic drugs may be immunostimulatory to T cells, as recently suggested for an IAP antagonist 86 or surprisingly for the mTORC1 inhibitor rapamycin, which is normally used as an immunosuppressive agent in the transplant setting 87. Similarly, although conventional wisdom viewed the effects of chemotherapy as obligatorily deleterious to immune mechanisms, such effects are rather drug-, dose- and/or schedule-dependent. Since the same agent may prove inhibitory, benign, or even stimulatory depending on the stage of immune response being targeted, and dose/schedule used 88,89, great care must be exercised when designing clinical protocols lest an efficacious drug be dismissed due to negative interactions or sub-optimal dosing schedules.
The effects of conventional chemotherapeutics on the immune system may be more nuanced than previously believed. Evidence is emerging that tumor cells can die in multiple ways, with some forms of (apoptotic) death actually leading to the enhancement of an immune response to the tumor 90. So-called immunogenic cell death is characterized in part by the release of ATP and high mobility group protein B1, which could activate local infiltrating myeloid cells and DCs via a purinergic receptor or TLR4, respectively. Cytotoxic agents that elicit this death fingerprint may have the ability to help induce anti-tumor immune responses and therefore be better candidates for combination therapy with immunologically active agents. Again, great care must be exercised to use such agents at doses and schedules that do not suppress effector CTLs.
Finally, the prospect of combining immunotherapeutic agents themselves must also be considered. To do this rationally, one must return again to the various steps of the immune response that need to be addressed in order to generate anti-cancer immunity (Fig. 1), consider the step(s) under the control of each agent, and assess the potential for overlapping or synergistic toxicity that would decrease rather than increase therapeutic index. For example, combining anti-CTLA4 with anti-PD1 makes sense biologically, as the two agents remove the brakes from T cell activation at two distinct stages: proliferation (CTLA4) and effector function (PD1). Yet, both might be expected to exhibit similar adverse events, underscoring the need to define carefully the potential for serious toxicity.
Vaccines: there and back again.
Agents that act at the effector stage (eg anti-PD1, inhibitors of immunosuppression) can act only be re-energizing the pre-existing T cells. Agents that act at the proliferation/activation stage (eg ipilimumab) can probably enhance not only pre-existing responses but also de novo responses. Thus, either could work well in conjunction with a vaccine approach, the place where immunotherapy in cancer got its start. But would endogenous or exogenous vaccines be preferable for this purpose?
Exogenous vaccines involve introducing pre-selected antigens on antibody delivery vehicles targeted to DCs, encoded in viral vectors, or administered as peptides or proteins in a suitable adjuvant and carrier. The approach has been highly effective in generating prophylaxis and protective immunity against infectious agents 9. In fact, such vaccines represent some of medicine’s greatest successes. That vaccines have been far less impressive in cancer could reflect the use of poor platforms that fail to elicit optimal antigen processing or presentation by DCs, sub-optimal adjuvants, or the absence of co-administered agents that facilitate T cell responses or overcome immunosuppression in the tumor bed. In addition, the antigens selected may have been poorly chosen, unable to generate protective T cells with high affinity T cell receptors because the tolerance barrier was just too high or unable to generate a sufficient quantity of T cell receptor ligands (peptide-MHC class I complexes) at the tumor cell surface.
Endogenous vaccines involve mobilizing antigens from a patient’s own tumor, in situ. This would have to be accomplished by inducing tumor cell death under conditions that favor the ability of endogenous DCs to capture, process, and present tumor-derived antigens. Although less controllable than the exogenous approach, endogenous vaccines have the distinct advantage of potentially allowing the presentation of the dozens – or hundreds – of mutations harbored by cancer cells 5. If even only a fraction of these can form MHC binding peptides that serve as T cell epitopes, as neo-antigens they would certainly not have been subject to suppression by central tolerance. Whether chemotherapy alone is sufficient to induce such in situ vaccination however is unknown. Because of the powerful immunosuppressive circuitries operating in the tumor microenvironment, additional signals are likely required to properly polarize the tumor-infiltrating antigen presenting cells, which can be now achieved by pathogen-derived signals or other DC maturation agents.
A recent attempt at endogenous vaccination involves the intratumoral injection of replication conditional Herpes simplex viruses engineered to secrete GM-CSF. These oncolytic viruses (OncoVex), which have entered Phase III testing in melanoma, cause lysis of tumor cells upon infection, whereupon GM-CSF release may enhance DC function in the tumor microenvironment to stimulate responses against autologous cancer antigens 91. A second attractive approach involves the combination of cytotoxic therapies in conjunction with agonistic antibodies to CD40. While this strategy might be predicted to augment DC priming of anti-tumor T cells, an important role for macrophage-mediated killing was instead implicated 92. Lastly, combinations of chemotherapy with Toll-like receptor (TLR) agonists could provide the right ingredients of tumor antigen release and tumor APC activation.
Perspectives
Despite its long if not always distinguished history, these are early days for a new science, and clinical practice, of cancer immunotherapy. Nevertheless, as an exciting therapeutic strategy that merits serious consideration by the biopharmaceutical industry and clinical oncology community alike, recent results have indeed allowed cancer immunotherapy finally to come of age. This transition coincides with another in the development of cancer immunology as a field. In much of the 20th century, the focus was on cancer “immunosurveillance” given the prominent view that the immune system plays a homeostatic role in controlling cancer. Basically, when oncogenic or other mutations occurred, the immune system was theorized to respond, thereby preventing the development of a tumor, at least when the system was operating normally. This concept was refined by “immunoediting”, which recognizes the complex and dynamic cross-talk between the tumor and host throughout all stages of disease development, including the possibility of tolerance 93. In the 21st century, however, we believe that the emerging pre-clinical and clinical data has turned attention directly towards the primary role of “tolerance and immune suppression”. Leaving aside the issue of whether the immune response plays a homeostatic function in prevention, cancer develops and escapes control either because tumor cells are too similar to their normal counterparts and therefore do not elicit sufficient immunity or because they are famously adept at inducing peripheral tolerance. While ipilimumab might work either to induce de novo responses or enhance pre-existing ones, the clinical activity of anti-PD1 antibodies seems more closely associated with overcoming tolerance than with generating an anti-cancer T cell repertoire.
Cancer immunotherapy has come of age at just the right time. The advent of a cohort of inhibitors that target oncogenic pathways with ever greater specificity is starting to reveal significant and sometimes spectacular responses in several indications. Yet, even in diagnostically defined populations, these responses can be transient or require continued dosing. If such drug regimens can be matched to appropriate immunotherapies, activating a patient’s immune system during a time of tumor reduction and remission may be the best way to ensure that responses are converted to long-term, durable benefit. In addition to the development of additional agents to prime and guide the immune response, appropriate pharmacodynamic biomarkers will have to be implemented to determine if a given immunotherapy is having the desired effect and appropriate diagnostics used to identify which strategy to apply to which patient. Finally, scientists, drug developers, and oncologists will have to work together to implement new metrics for evaluating the effectiveness of immunotherapies. Their mechanism of action is so distinct, both mechanistically and temporally, as compared to conventional cytotoxic drugs that they cannot be expected to perform according to standards developed a generation ago, even though the result may ultimately be curative.
Acknowledgment
This article is dedicated to the memory of our mentor, friend, and inspiration Ralph Steinman, whose scientific life was dedicated to advancing the field of immunology in general and cancer immunotherapy in particular. Just before learning of his Nobel Prize, Ralph fell victim to the disease that we hope will be more effectively treated by the development of immunotherapeutic approaches based on the pioneering work reviewed here. We and many others will dedicate ourselves to this effort on Ralph’s behalf, and on behalf of cancer patients throughout the world.
References
- 1.Dougan M, Dranoff G. Immune therapy for cancer. Annu Rev Immunol. 2009;27:83–117. doi: 10.1146/annurev.immunol.021908.132544. doi:10.1146/annurev.immunol.021908.132544. [DOI] [PubMed] [Google Scholar]
- 2.Hall SS. A commotion in the blood: life, death, and the immune system. Henry Holt; 1997. [Google Scholar]
- 3.Sylvester RJ. Bacillus Calmette-Guerin treatment of non-muscle invasive bladder cancer. Int J Urol. 2011;18:113–120. doi: 10.1111/j.1442-2042.2010.02678.x. doi:10.1111/j.1442-2042.2010.02678.x. [DOI] [PubMed] [Google Scholar]
- 4.Boon T, Coulie PG, Van den Eynde BJ, van der Bruggen P. Human T cell responses against melanoma. Annu Rev Immunol. 2006;24:175–208. doi: 10.1146/annurev.immunol.24.021605.090733. doi:10.1146/annurev.immunol.24.021605.090733. [DOI] [PubMed] [Google Scholar]
- 5.Segal NH, et al. Epitope landscape in breast and colorectal cancer. Cancer Res. 2008;68:889–892. doi: 10.1158/0008-5472.CAN-07-3095. doi:10.1158/0008-5472.CAN-07-3095. [DOI] [PubMed] [Google Scholar]
- 6.Mellman I, Steinman RM. Dendritic cells: specialized and regulated antigen processing machines. Cell. 2001;106:255–258. doi: 10.1016/s0092-8674(01)00449-4. [DOI] [PubMed] [Google Scholar]
- 7.Trombetta ES, Mellman I. Cell biology of antigen processing in vitro and in vivo. Annu Rev Immunol. 2005;23:975–1028. doi: 10.1146/annurev.immunol.22.012703.104538. doi:10.1146/annurev.immunol.22.012703.104538. [DOI] [PubMed] [Google Scholar]
- 8.Zitvogel L, Kroemer G. Anticancer immunochemotherapy using adjuvants with direct cytotoxic effects. J Clin Invest. 2009;119:2127–2130. doi: 10.1172/JCI39991. doi:10.1172/JCI39991. This paper reviews the argument for certain forms of apoptotic cell death as enhancing anti-tumor immune responses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palucka K, Banchereau J, Mellman I. Designing vaccines based on biology of human dendritic cell subsets. Immunity. 2010;33:464–478. doi: 10.1016/j.immuni.2010.10.007. doi:10.1016/j.immuni.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Darrasse-Jeze G, et al. Feedback control of regulatory T cell homeostasis by dendritic cells in vivo. J Exp Med. 2009;206:1853–1862. doi: 10.1084/jem.20090746. doi:10.1084/jem.20090746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang A, et al. Disruption of E-cadherin-mediated adhesion induces a functionally distinct pathway of dendritic cell maturation. Immunity. 2007;27:610–624. doi: 10.1016/j.immuni.2007.08.015. doi:10.1016/j.immuni.2007.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steinman RM, Turley S, Mellman I, Inaba K. The induction of tolerance by dendritic cells that have captured apoptotic cells. J Exp Med. 2000;191:411–416. doi: 10.1084/jem.191.3.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steinman RM, Hawiger D, Nussenzweig MC. Tolerogenic dendritic cells. Annu Rev Immunol. 2003;21:685–711. doi: 10.1146/annurev.immunol.21.120601.141040. doi:10.1146/annurev.immunol.21.120601.141040. [DOI] [PubMed] [Google Scholar]
- 14.Curiel TJ, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. 2004;10:942–949. doi: 10.1038/nm1093. Nat Med. [DOI] [PubMed] [Google Scholar]
- 15.Kono K, et al. CD4(+)CD25high regulatory T cells increase with tumor stage in patients with gastric and esophageal cancers. Cancer Immunol Immunother. 2006;55:1064–1071. doi: 10.1007/s00262-005-0092-8. doi:10.1007/s00262-005-0092-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kooi S, et al. HLA class I expression on human ovarian carcinoma cells correlates with T-cell infiltration in vivo and T-cell expansion in vitro in low concentrations of recombinant interleukin-2. Cell Immunol. 1996;174:116–128. doi: 10.1006/cimm.1996.0301. [DOI] [PubMed] [Google Scholar]
- 17.Hamanishi J, et al. Programmed cell death 1 ligand 1 and tumor-infiltrating CD8+ T lymphocytes are prognostic factors of human ovarian cancer. Proc Natl Acad Sci U S A. 2007;104:3360–3365. doi: 10.1073/pnas.0611533104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parsa AT, et al. Loss of tumor suppressor PTEN function increases B7-H1 expression and immunoresistance in glioma. Nat Med. 2007;13:84–88. doi: 10.1038/nm1517. doi:10.1038/nm1517. [DOI] [PubMed] [Google Scholar]
- 19.Mellor AL, Munn DH. IDO expression by dendritic cells: tolerance and tryptophan catabolism. Nat Rev Immunol. 2004;4:762–774. doi: 10.1038/nri1457. doi:10.1038/nri1457. [DOI] [PubMed] [Google Scholar]
- 20.Munn DH, Mellor AL. IDO and tolerance to tumors. Trends Mol Med. 2004;10:15–18. doi: 10.1016/j.molmed.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Marigo I, Dolcetti L, Serafini P, Zanovello P, Bronte V. Tumor-induced tolerance and immune suppression by myeloid derived suppressor cells. Immunol Rev. 2008;222:162–179. doi: 10.1111/j.1600-065X.2008.00602.x. doi:10.1111/j.1600-065X.2008.00602.x. [DOI] [PubMed] [Google Scholar]
- 22.Ohta A, et al. A2A adenosine receptor protects tumors from antitumor T cells. Proc Natl Acad Sci U S A. 2006;103:13132–13137. doi: 10.1073/pnas.0605251103. doi:0605251103 [pii] 10.1073/pnas.0605251103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Facciabene A, et al. Tumour hypoxia promotes tolerance and angiogenesis via CCL28 and T(reg) cells. Nature. 2011;475:226–230. doi: 10.1038/nature10169. doi:10.1038/nature10169 nature10169 [pii] [DOI] [PubMed] [Google Scholar]
- 24.Aggarwal S, Pittenger MF. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood. 2005;105:1815–1822. doi: 10.1182/blood-2004-04-1559. doi:2004-04-1559 [pii] 10.1182/blood-2004-04-1559. [DOI] [PubMed] [Google Scholar]
- 25.Bouzin C, Brouet A, De Vriese J, Dewever J, Feron O. Effects of vascular endothelial growth factor on the lymphocyte-endothelium interactions: identification of caveolin-1 and nitric oxide as control points of endothelial cell anergy. J Immunol. 2007;178:1505–1511. doi: 10.4049/jimmunol.178.3.1505. [DOI] [PubMed] [Google Scholar]
- 26.Buckanovich RJ, et al. Endothelin B receptor mediates the endothelial barrier to T cell homing to tumors and disables immune therapy. Nat Med. 2008;14:28–36. doi: 10.1038/nm1699. [DOI] [PubMed] [Google Scholar]
- 27.Zhang L, et al. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med. 2003;348:203–213. doi: 10.1056/NEJMoa020177. [DOI] [PubMed] [Google Scholar]
- 28.Galon J, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313:1960–1964. doi: 10.1126/science.1129139. [DOI] [PubMed] [Google Scholar]
- 29.Rosenberg SA, Yang JC, Restifo NP. Cancer immunotherapy: moving beyond current vaccines. Nat Med. 2004;10:909–915. doi: 10.1038/nm1100. doi:10.1038/nm1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwartzentruber DJ, et al. gp100 peptide vaccine and interleukin-2 in patients with advanced melanoma. N Engl J Med. 2011;364:2119–2127. doi: 10.1056/NEJMoa1012863. doi:10.1056/NEJMoa1012863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kenter GG, et al. Vaccination against HPV-16 oncoproteins for vulvar intraepithelial neoplasia. N Engl J Med. 2009;361:1838–1847. doi: 10.1056/NEJMoa0810097. doi:10.1056/NEJMoa0810097. [DOI] [PubMed] [Google Scholar]
- 32.Leffers N, et al. Immunization with a P53 synthetic long peptide vaccine induces P53-specific immune responses in ovarian cancer patients, a phase II trial. Int J Cancer. 2009;125:2104–2113. doi: 10.1002/ijc.24597. doi:10.1002/ijc.24597. [DOI] [PubMed] [Google Scholar]
- 33.Vansteenkiste J, et al. Final results of a multi-center, double-blind, randomized, placebo-controlled phase II study to assess the efficacy of MAGE-A3 immunotherapeutic as adjuvant therapy in stage IB/II non-small cell lung cancer (NSCLC) Journal of clinical oncology. 2007;25 (18S), abstract, 7554. [Google Scholar]
- 34.Freedman A, et al. Placebo-controlled phase III trial of patient-specific immunotherapy with mitumprotimut-T and granulocyte-macrophage colony-stimulating factor after rituximab in patients with follicular lymphoma. J Clin Oncol. 2009;27:3036–3043. doi: 10.1200/JCO.2008.19.8903. doi:10.1200/JCO.2008.19.8903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kantoff PW, et al. Overall Survival Analysis of a Phase II Randomized Controlled Trial of a Poxviral-Based PSA-Targeted Immunotherapy in Metastatic Castration-Resistant Prostate Cancer. J Clin Oncol. 2010;28:1099–1105. doi: 10.1200/JCO.2009.25.0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Neller MA, López JA, Schmidt CW. Antigens for cancer immunotherapy. Seminars in Immunology. 2008;20:286–295. doi: 10.1016/j.smim.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 37.Copier J, Dalgleish Whole-cell vaccines: A failure or a success waiting to happen? Curr Opin Mol Ther. 2010;12:14–20. [PubMed] [Google Scholar]
- 38.Schuler G. Dendritic cells in cancer immunotherapy. Eur J Immunol. 2010;40:2123–2130. doi: 10.1002/eji.201040630. doi:10.1002/eji.201040630. The authors summarizes the current state of the art in the use of autologous dendritic cell vaccines. [DOI] [PubMed] [Google Scholar]
- 39.Neller MA, Lopez JA, Schmidt CW. Antigens for cancer immunotherapy. Semin Immunol. 2008;20:286–295. doi: 10.1016/j.smim.2008.09.006. doi:S1044-5323(08)00098-5 [pii] 10.1016/j.smim.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 40.Cheever MA, et al. Translational Research Working Group developmental pathway for immune response modifiers. Clin Cancer Res. 2008;14:5692–5699. doi: 10.1158/1078-0432.CCR-08-1266. doi:10.1158/1078-0432.CCR-08-1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rammensee HG, Weinschenk T, Gouttefangeas C, Stevanovic S. Towards patient-specific tumor antigen selection for vaccination. Immunol Rev. 2002;188:164–176. doi: 10.1034/j.1600-065x.2002.18815.x. [DOI] [PubMed] [Google Scholar]
- 42.Small EJ, et al. Immunotherapy of hormone-refractory prostate cancer with antigen-loaded dendritic cells. J Clin Oncol. 2000;18:3894–3903. doi: 10.1200/JCO.2000.18.23.3894. [DOI] [PubMed] [Google Scholar]
- 43.Kantoff PW, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–422. doi: 10.1056/NEJMoa1001294. doi:10.1056/NEJMoa1001294. This paper describes the clinical trial results that led to the FDA approval of Provenge for prostate cancer. [DOI] [PubMed] [Google Scholar]
- 44.Wolchok JD, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15:7412–7420. doi: 10.1158/1078-0432.CCR-09-1624. doi:10.1158/1078-0432.CCR-09-1624. The authors summarize the argument for using a different set of criteria to evaluate the efficacy of immunotherapies given the mechanistic differences from conventional anti-cancer drugs. [DOI] [PubMed] [Google Scholar]
- 45.Leach DR, Krummel MF, Allison JP. Enhancement of antitumor immunity by CTLA-4 blockade. Science. 1996;271:1734–1736. doi: 10.1126/science.271.5256.1734. [DOI] [PubMed] [Google Scholar]
- 46.Hodi FS, et al. Immunologic and clinical effects of antibody blockade of cytotoxic T lymphocyte-associated antigen 4 in previously vaccinated cancer patients. Proc Natl Acad Sci U S A. 2008;105:3005–3010. doi: 10.1073/pnas.0712237105. doi:10.1073/pnas.0712237105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dudley ME, et al. Cancer regression and autoimmunity in patients after clonal repopulation with antitumor lymphocytes. Science. 2002;298:850–854. doi: 10.1126/science.1076514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rosenberg SA, Restifo NP, Yang JC, Morgan RA, Dudley ME. Adoptive cell transfer: a clinical path to effective cancer immunotherapy. Nat Rev Cancer. 2008;8:299–308. doi: 10.1038/nrc2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.June CH. Principles of adoptive T cell cancer therapy. J Clin Invest. 2007;117:1204–1212. doi: 10.1172/JCI31446. doi:10.1172/JCI31446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Robbins PF, et al. Tumor regression in patients with metastatic synovial cell sarcoma and melanoma using genetically engineered lymphocytes reactive with NY-ESO-1. J Clin Oncol. 2011;29:917–924. doi: 10.1200/JCO.2010.32.2537. doi:JCO.2010.32.2537 [pii] 10.1200/JCO.2010.32.2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kalos M, et al. T cells with chimeric antigen receptors have potent antitumor effects and can establish memory in patients with advanced leukemia. Sci Transl Med. 2011;3:95ra73. doi: 10.1126/scitranslmed.3002842. doi:3/95/95ra73 [pii] 10.1126/scitranslmed.3002842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Topp MS, et al. Targeted therapy with the T-cell-engaging antibody blinatumomab of chemotherapy-refractory minimal residual disease in B-lineage acute lymphoblastic leukemia patients results in high response rate and prolonged leukemia-free survival. J Clin Oncol. 2011;29:2493–2498. doi: 10.1200/JCO.2010.32.7270. doi:JCO.2010.32.7270 [pii] 10.1200/JCO.2010.32.7270. This paper describes the clinical results for an intriguing approach to tumor targeting of T cells using bispecific antibodies. [DOI] [PubMed] [Google Scholar]
- 53.Chambers CA, Kuhns MS, Egen JG, Allison JP. CTLA-4-mediated inhibition in regulation of T cell responses: mechanisms and manipulation in tumor immunotherapy. Annu Rev Immunol. 2001;19:565–594. doi: 10.1146/annurev.immunol.19.1.565. doi:10.1146/annurev.immunol.19.1.565. A recent review describing current understanding of the mechanism of action of CTLA-4. [DOI] [PubMed] [Google Scholar]
- 54.Waterhouse P, et al. Lymphoproliferative disorders with early lethality in mice deficient in Ctla-4. Science. 1995;270:985–988. doi: 10.1126/science.270.5238.985. [DOI] [PubMed] [Google Scholar]
- 55.Tivol EA, et al. Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity. 1995;3:541–547. doi: 10.1016/1074-7613(95)90125-6. [DOI] [PubMed] [Google Scholar]
- 56.Wing K, et al. CTLA-4 control over Foxp3+ regulatory T cell function. Science. 2008;322:271–275. doi: 10.1126/science.1160062. doi:10.1126/science.1160062. [DOI] [PubMed] [Google Scholar]
- 57.Cipponi A, Wieers G, van Baren N, Coulie PG. Tumor-infiltrating lymphocytes: apparently good for melanoma patients. But why? 2011;60:1153–1160. doi: 10.1007/s00262-011-1026-2. Cancer Immunol Immunother. doi:10.1007/s00262-011-1026-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Disis ML, et al. High-titer HER-2/neu protein-specific antibody can be detected in patients with early-stage breast cancer. J Clin Oncol. 1997;15:3363–3367. doi: 10.1200/JCO.1997.15.11.3363. [DOI] [PubMed] [Google Scholar]
- 59.Novellino L, Castelli C, Parmiani G. A listing of human tumor antigens recognized by T cells: March 2004 update. Cancer Immunol Immunother. 2005;54:187–207. doi: 10.1007/s00262-004-0560-6. doi:10.1007/s00262-004-0560-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hodi FS, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. doi:10.1056/NEJMoa1003466. This paper reports the pivotal clinical trial data that shortly thereafter led to the FDA approval of anti-CTLA4 for the treatment of metastatic melanoma. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Robert C, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–2526. doi: 10.1056/NEJMoa1104621. doi:10.1056/NEJMoa1104621. [DOI] [PubMed] [Google Scholar]
- 62.Hoos A, et al. Improved endpoints for cancer immunotherapy trials. J Natl Cancer Inst. 2010;102:1388–1397. doi: 10.1093/jnci/djq310. doi:10.1093/jnci/djq310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Suntharalingam G, et al. Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med. 2006;355:1018–1028. doi: 10.1056/NEJMoa063842. doi:10.1056/NEJMoa063842. [DOI] [PubMed] [Google Scholar]
- 64.Workman CJ, Vignali DA. Negative regulation of T cell homeostasis by lymphocyte activation gene-3 (CD223) J Immunol. 2005;174:688–695. doi: 10.4049/jimmunol.174.2.688. [DOI] [PubMed] [Google Scholar]
- 65.Huang CT, et al. Role of LAG-3 in regulatory T cells. Immunity. 2004;21:503–513. doi: 10.1016/j.immuni.2004.08.010. doi:10.1016/j.immuni.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 66.Woo SR, et al. Differential subcellular localization of the regulatory T-cell protein LAG-3 and the coreceptor CD4. Eur J Immunol. 2010;40:1768–1777. doi: 10.1002/eji.200939874. doi:10.1002/eji.200939874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Okazaki T, et al. PD-1 and LAG-3 inhibitory co-receptors act synergistically to prevent autoimmunity in mice. J Exp Med. 2011;208:395–407. doi: 10.1084/jem.20100466. doi:10.1084/jem.20100466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol. 2008;26:677–704. doi: 10.1146/annurev.immunol.26.021607.090331. doi:10.1146/annurev.immunol.26.021607.090331. This article reviews the evidence for immunosuppression by the induction of T cell exhaustion via activation of PD1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Watanabe T, Bertoletti A, Tanoto TA. PD-1/PD-L1 pathway and T-cell exhaustion in chronic hepatitis virus infection. J Viral Hepat. 2010;17:453–458. doi: 10.1111/j.1365-2893.2010.01313.x. doi:10.1111/j.1365-2893.2010.01313.x. [DOI] [PubMed] [Google Scholar]
- 70.Sakuishi K, et al. Targeting Tim-3 and PD-1 pathways to reverse T cell exhaustion and restore anti-tumor immunity. J Exp Med. 2010;207:2187–2194. doi: 10.1084/jem.20100643. doi:10.1084/jem.20100643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gadiot J, et al. Overall survival and PD-L1 expression in metastasized malignant melanoma. Cancer. 2011;117:2192–2201. doi: 10.1002/cncr.25747. doi:10.1002/cncr.25747. [DOI] [PubMed] [Google Scholar]
- 72.Gao Q, et al. Overexpression of PD-L1 significantly associates with tumor aggressiveness and postoperative recurrence in human hepatocellular carcinoma. Clin Cancer Res. 2009;15:971–979. doi: 10.1158/1078-0432.CCR-08-1608. doi:10.1158/1078-0432.CCR-08-1608. [DOI] [PubMed] [Google Scholar]
- 73.Brahmer JR, et al. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol. 2010;28:3167–3175. doi: 10.1200/JCO.2009.26.7609. doi:10.1200/JCO.2009.26.7609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nishimura H, Nose M, Hiai H, Minato N, Honjo T. Development of lupus-like autoimmune diseases by disruption of the PD-1 gene encoding an ITIM motif-carrying immunoreceptor. Immunity. 1999;11:141–151. doi: 10.1016/s1074-7613(00)80089-8. [DOI] [PubMed] [Google Scholar]
- 75.Nishimura H, et al. Autoimmune dilated cardiomyopathy in PD-1 receptor-deficient mice. Science. 2001;291:319–322. doi: 10.1126/science.291.5502.319. doi:10.1126/science.291.5502.319. [DOI] [PubMed] [Google Scholar]
- 76.Ito T, et al. OX40 ligand shuts down IL-10-producing regulatory T cells. Proc Natl Acad Sci U S A. 2006;103:13138–13143. doi: 10.1073/pnas.0603107103. doi:10.1073/pnas.0603107103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cohen AD, et al. Agonist anti-GITR monoclonal antibody induces melanoma tumor immunity in mice by altering regulatory T cell stability and intra-tumor accumulation. PLoS One. 2010;5:e10436. doi: 10.1371/journal.pone.0010436. doi:10.1371/journal.pone.0010436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Golovina TN, Vonderheide RH. Regulatory T cells: overcoming suppression of T-cell immunity. Cancer J. 2010;16:342–347. doi: 10.1097/PPO.0b013e3181eb336d. doi:10.1097/PPO.0b013e3181eb336d 00130404-201007000-00009 [pii] [DOI] [PubMed] [Google Scholar]
- 79.Emens LA, et al. Timed sequential treatment with cyclophosphamide, doxorubicin, and an allogeneic granulocyte-macrophage colony-stimulating factor-secreting breast tumor vaccine: a chemotherapy dose-ranging factorial study of safety and immune activation. J Clin Oncol. 2009;27:5911–5918. doi: 10.1200/JCO.2009.23.3494. doi:JCO.2009.23.3494 [pii] 10.1200/JCO.2009.23.3494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ghiringhelli F, et al. Metronomic cyclophosphamide regimen selectively depletes CD4+CD25+ regulatory T cells and restores T and NK effector functions in end stage cancer patients. Cancer Immunol Immunother. 2007;56:641–648. doi: 10.1007/s00262-006-0225-8. doi:10.1007/s00262-006-0225-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Muller AJ, Scherle PA. Targeting the mechanisms of tumoral immune tolerance with small-molecule inhibitors. Nat Rev Cancer. 2006;6:613–625. doi: 10.1038/nrc1929. doi:10.1038/nrc1929. [DOI] [PubMed] [Google Scholar]
- 82.Manning EA, et al. A vascular endothelial growth factor receptor-2 inhibitor enhances antitumor immunity through an immune-based mechanism. Clin Cancer Res. 2007;13:3951–3959. doi: 10.1158/1078-0432.CCR-07-0374. doi:13/13/3951 [pii] 10.1158/1078-0432.CCR-07-0374. [DOI] [PubMed] [Google Scholar]
- 83.Shrimali RK, et al. Antiangiogenic agents can increase lymphocyte infiltration into tumor and enhance the effectiveness of adoptive immunotherapy of cancer. Cancer Res. 2010;70:6171–6180. doi: 10.1158/0008-5472.CAN-10-0153. doi:0008-5472.CAN-10-0153 [pii] 10.1158/0008-5472.CAN-10-0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang L, et al. IL-17 can promote tumor growth through an IL-6-Stat3 signaling pathway. J Exp Med. 2009;206:1457–1464. doi: 10.1084/jem.20090207. doi:10.1084/jem.20090207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chapman PB, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507–2516. doi: 10.1056/NEJMoa1103782. doi:10.1056/NEJMoa1103782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dougan M, et al. IAP inhibitors enhance co-stimulation to promote tumor immunity. J Exp Med. 2010;207:2195–2206. doi: 10.1084/jem.20101123. doi:10.1084/jem.20101123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ferrer IR, et al. Cutting edge: Rapamycin augments pathogen-specific but not graft-reactive CD8+ T cell responses. J Immunol. 2010;185:2004–2008. doi: 10.4049/jimmunol.1001176. doi:10.4049/jimmunol.1001176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Machiels JP, et al. Cyclophosphamide, doxorubicin, and paclitaxel enhance the antitumor immune response of granulocyte/macrophage-colony stimulating factor-secreting whole-cell vaccines in HER-2/neu tolerized mice. Cancer Res. 2001;61:3689–3697. [PubMed] [Google Scholar]
- 89.Alagkiozidis I, et al. Time-dependent cytotoxic drugs selectively cooperate with IL-18 for cancer chemo-immunotherapy. J Transl Med. 2011;9:77. doi: 10.1186/1479-5876-9-77. doi:1479-5876-9-77 [pii] 10.1186/1479-5876-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Obeid M, et al. Calreticulin exposure dictates the immunogenicity of cancer cell death. Nat Med. 2007;13:54–61. doi: 10.1038/nm1523. [DOI] [PubMed] [Google Scholar]
- 91.Senzer NN, et al. Phase II clinical trial of a granulocyte-macrophage colony-stimulating factor-encoding, second-generation oncolytic herpesvirus in patients with unresectable metastatic melanoma. J Clin Oncol. 2009;27:5763–5771. doi: 10.1200/JCO.2009.24.3675. doi:10.1200/JCO.2009.24.3675. [DOI] [PubMed] [Google Scholar]
- 92.Beatty GL, et al. CD40 agonists alter tumor stroma and show efficacy against pancreatic carcinoma in mice and humans. Science. 2011;331:1612–1616. doi: 10.1126/science.1198443. doi:10.1126/science.1198443. Although it is unclear if activation of CD40 works by activating innate or adaptive immunity, the results reported in this paper are impressive. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity's roles in cancer suppression and promotion. Science. 2011;331:1565–1570. doi: 10.1126/science.1203486. doi:10.1126/science.1203486. [DOI] [PubMed] [Google Scholar]
- 94.Nahta R, Esteva FJ. Herceptin: mechanisms of action and resistance. Cancer Lett. 2006;232:123–138. doi: 10.1016/j.canlet.2005.01.041. doi:10.1016/j.canlet.2005.01.041. [DOI] [PubMed] [Google Scholar]
- 95.Taylor C, et al. Augmented HER-2 specific immunity during treatment with trastuzumab and chemotherapy. Clin Cancer Res. 2007;13:5133–5143. doi: 10.1158/1078-0432.CCR-07-0507. doi:10.1158/1078-0432.CCR-07-0507. [DOI] [PubMed] [Google Scholar]
- 96.Lewis Phillips GD, et al. Targeting HER2-positive breast cancer with trastuzumab-DM1, an antibody-cytotoxic drug conjugate. Cancer Res. 2008;68:9280–9290. doi: 10.1158/0008-5472.CAN-08-1776. doi:10.1158/0008-5472.CAN-08-1776. [DOI] [PubMed] [Google Scholar]
- 97.Porter DL, Levine BL, Kalos M, Bagg A, June CH. Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia. N Engl J Med. 2011;365:725–733. doi: 10.1056/NEJMoa1103849. doi:10.1056/NEJMoa1103849. A recent and clinically impressive attempt at adoptive T cell therapy using genetically altered, patient-derived T cells. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gogas H, et al. Prognostic significance of autoimmunity during treatment of melanoma with interferon. N Engl J Med. 2006;354:709–718. doi: 10.1056/NEJMoa053007. doi:10.1056/NEJMoa053007. [DOI] [PubMed] [Google Scholar]
- 99.Shin JY, Yoon IH, Kim JS, Kim B, Park CG. Vascular endothelial growth factor-induced chemotaxis and IL-10 from T cells. Cell Immunol. 2009;256:72–78. doi: 10.1016/j.cellimm.2009.01.006. doi:10.1016/j.cellimm.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 100.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–174. doi: 10.1038/nri2506. doi:nri2506 [pii] 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]