Abstract
Significance: Functional stem cell decline has been postulated to result in loss of maintenance of tissue homeostasis leading to organismal decline and diseases of aging. Recent Advances: Recent findings implicate redox metabolism in the control of stem cell pool and stem cell aging. Although reactive oxygen species (ROS) are better known for their damaging properties to DNA, proteins and lipids, recent findings suggest that ROS may also be an integral physiological mediator of cellular signaling in primary cells. Critical Issues: Here we review recent published work on major signaling pathways and transcription factors that are regulated by ROS and mediate ROS regulation of stem cell fate. We will specifically focus on how alterations in this regulation may be implicated in disease and particularly in diseases of stem cell aging. In general, based on the work described here we propose a model in which ROS function as stem cell rheostat. Future Directions: Future work in elucidating how ROS control stem cell cycling, apoptotic machinery, and lineage determination should shed light on mechanisms whereby ROS may control stem cell aging. Antioxid. Redox Signal. 20, 1902–1916.
Introduction
Stem cells maintain tissue homeostasis over time by regularly replacing damaged or lost cells. Tissues with high turnover rate, such as blood and skin are maintained by resident stem cells that compensate for the loss of differentiated or damaged cells. Stem cells share two defining properties—pluripotency and self-renewal. Stem cells are pluripotent in that they give rise to all cells within a given tissue (or to all cells within the body). Stem cells also have the capacity to generate with each division, another cell with the stem cell program. This stem cell property is known as self-renewal and enables the organism to maintain a stem cell pool throughout its lifetime. The function of stem cells is known to decline with age, a process that may be implicated in the loss of maintenance of tissue homeostasis leading to organ failure and diseases of aging (Fig. 1) (38).
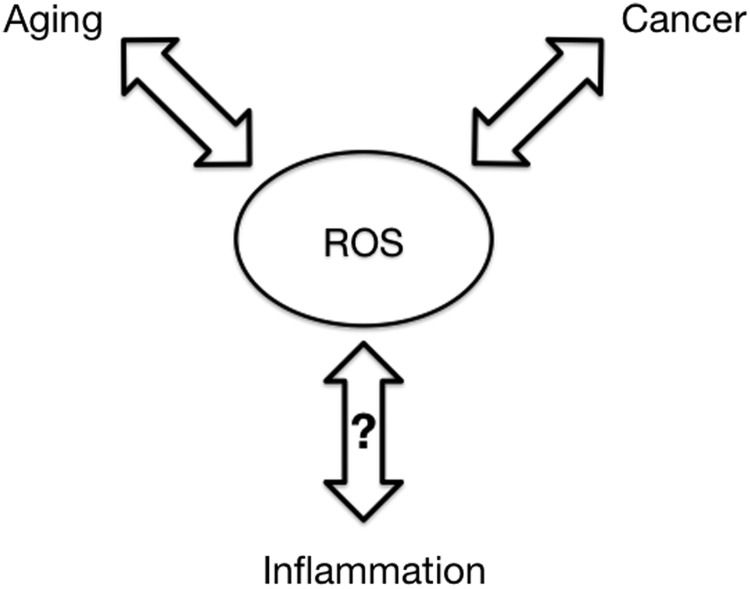
FIG. 1.
Contribution of ROS to disease in stem cells. Oxidative stress and aberrant ROS signaling are associated with aging-related diseases including cancer. In turn, these diseases can lead to further dysregulation of ROS signaling and increased oxidative stress. ROS damage is also known to contribute to inflammation; however, the cross-talk between ROS and the inflammatory response in stem cells is unclear.
Adult stem cells are known to be mostly quiescent and to rarely enter cell cycle (38). The few exceptions, such as intestinal stem cells (97), are the subject of debate (72, 87). It has been postulated that quiescence protects stem cells from incurring damage during cell division and plays a necessary role in their lifetime maintenance. Nonetheless, when faced with major tissue loss or damage, stem cells exit their quiescent state and enter the cell cycle to proliferate and generate large numbers of differentiated progenies. These properties may be shared by cancer stem cells (91). Efforts aimed at elucidating the source of the potential of stem cells to regenerate in response to damaged or lost tissues has been the focus of much research in the past over 50 years. Although such studies have reached new heights within the past decade, the basis for the ability of deeply quiescent cells to proliferate on demand is not known. Several recent publications point to metabolism as a potential source for resolving this enigma (35, 110, 129).
Reactive Oxygen Species as Stem Cell Rheostat
Cellular respiration, a process necessary for the survival of all aerobic organisms, involves the oxygen dependent process of oxidative phosphorylation to produce adenosine triphosphate (ATP). The energy released from the hydrolysis of ATP drives essential chemical reactions within the cell. While some ATP production can occur through the anaerobic process of glycolysis, most ATP is synthesized in the mitochondria through oxidative phosphorylation; however, the production of ATP within the mitochondria can lead to the release of harmful reactive oxygen species (ROS) as a byproduct. ROS can adversely react with DNA, lipids, and proteins and the cumulative effects of this damage are thought to contribute to the physiological effects of aging (82). On the other hand, ROS are also considered to be essential components in multiple biological processes as second messengers (21). Emerging evidence increasingly suggests that ROS may not only be a byproduct of metabolic oxidative phosphorylation, but intimately implicated in the physiological regulation of signaling pathways. Alterations in the redox milieu, that is, ROS production versus scavenging, may lead to disease as a result of too much ROS damage, but also perhaps, by means of redox-mediated enhancement (or inhibition) of an otherwise physiologically ROS-regulated signaling protein/pathway (Fig. 1).
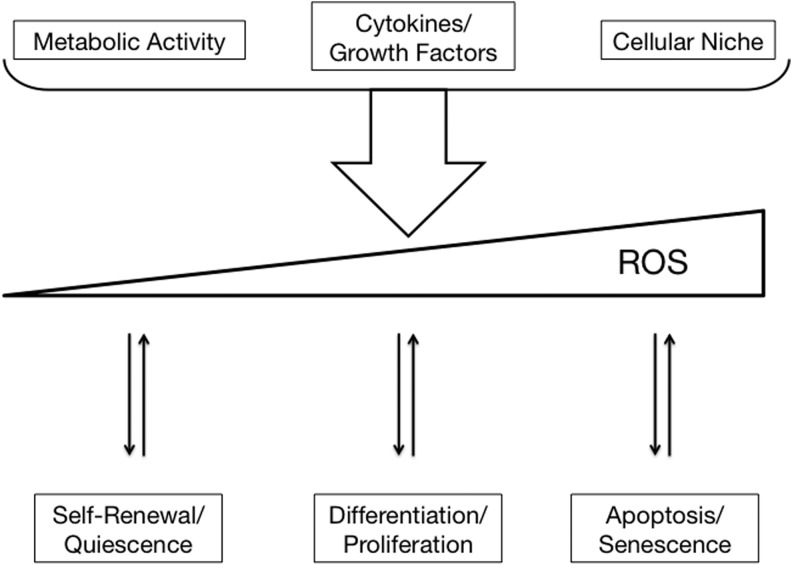
ROS are being increasingly implicated in the physiological regulation of critical developmental processes, including the emergence of embryonic blood stem cells (33, 35, 89). A potential model may be that ROS function as a stem cell rheostat by sensing and translating environmental cues into a cellular response to balance cellular output (function) with cellular input (e.g., nutrients, cytokines). Stem cells, in particular, may take advantage of redox regulation to coordinate cell cycle with differentiation as a means of holding their stem cell fate in check, while ensuring homeostasis. Understanding the possible mechanisms by which ROS influence stem cells' fate may provide insights into how the aging of stem cells may be implicated in diseases of aging, as slight variations in ROS content may have profound effects on stem cell fate (Fig. 2).
FIG. 2.
ROS as stem cell rheostat. Various stem cell intrinsic and extrinsic factors can alter the cellular redox state through the generation of ROS. The cell can sense a gradient of ROS concentrations with multiple proteins in various pathways and respond accordingly. ROS, reactive oxygen species.
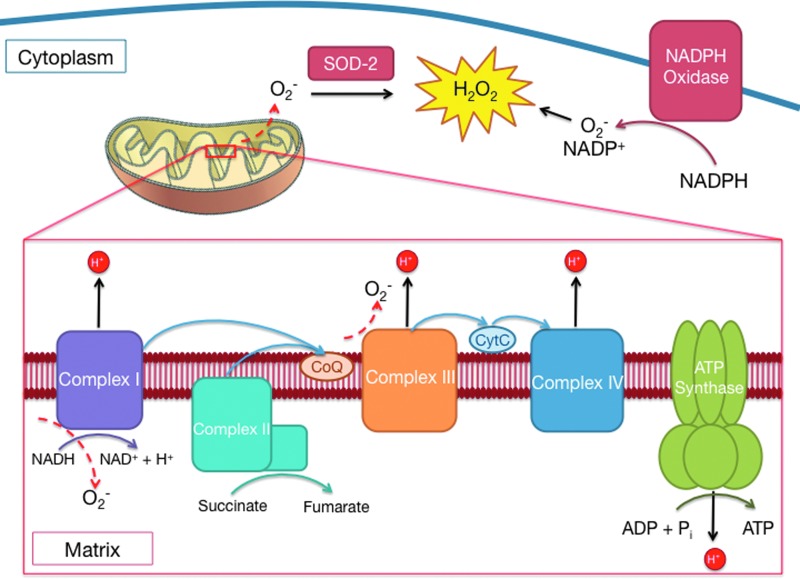
Source of ROS in Stem Cells
Mitochondria produce almost 90% of ROS in all cells (3). The function of mitochondria in stem cells is an area of active investigation; however, it remains to be determined whether mitochondria are the sole or the major source of ROS in stem cells (Fig. 3). The NADPH Nox family of oxidases is another major source of ROS (8). The primary function of the NADPH Nox family of oxidases is the production of ROS (8). NADPH oxidases are found in phagocytic and nonphagocytic cells, and preferentially use NADPH rather than NADH as substrate. Nox2 and 4 are expressed in human CD34+ hematopoietic stem cells (HSCs) and progenitors (85). The contribution of Nox signaling to the biology of stem cells remains to be seen. It is, however, likely that Nox proteins are involved in the regulation of ROS in stem cells (22, 84, 85). Importantly, the relative contribution of different sources of ROS to the maintenance of tissue homeostasis remains unclear.
FIG. 3.
Sources of ROS. A majority of ROS is produced by the mitochondria mainly through the aberrant reduction of O2 at complexes I and III during oxidative phosphorylation. The highly reactive and unstable superoxide anion (O2−) is scavenged by SOD-1 to form H2O2, also a type of ROS. H2O2 is more stable and is responsible for direct protein modifications. Another source of intracellular ROS is NADPH oxidase, which produces O2- through the oxidation of NADPH. SOD, superoxide dehydrogenase; H2O2, hydrogen peroxide. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/ars
ROS in the Regulation of Signaling Pathways
ROS are generated as a consequence of activity by oncoproteins and several cytokine and growth factor stimuli [(45, 46, 74, 98, 106, 111, 117, 134) reviewed in Thannickal and Fanburg (113)]. While the exact mechanism by which cytokine receptor signaling generates ROS in nonphagocytic cells is not fully understood, it is proposed that ROS modulate protein function by oxidization of reactive cysteine residues in signaling proteins [reviewed in Pervaiz et al. (82) and Thannickal and Fanburg (113)]. Stimulation of growth factor receptors, such as epidermal growth factor, platelet-derived growth factor (PDGF), and insulin signaling is associated with a transient burst of ROS production that ultimately participates in cellular signaling. This is partly achieved by transient phosphorylation and inhibition of local detoxification enzymes, such as peroxiredoxin I (122). Transient accumulation of ROS around locally concentrated membrane signaling proteins enables ROS to function as signaling messengers (122). ROS impact cellular signaling through protein modifications, such as intramolecular disulfide bridges, sulfonyl-amide bond formation, direct activation of tyrosine kinases by Cys oxidation, or by inhibition of phosphatases [reviewed in Thannickal and Fanburg (113)]. In turn, the catalytic activity of antioxidant enzymes, such as peroxiredoxins, catalase, and glutathione peroxidase is modified by signaling molecules [reviewed in Rhee et al. (92)] suggesting a dynamic balance between cellular signaling and regulation of oxidative stress. Many protein tyrosine phosphatases are reversibly oxidized and inactivated by ROS providing a mechanism for ROS-induced mitogenesis (5, 6, 39, 69). In particular, ROS are known to inhibit the function of phosphatase and tensin homology (PTEN), protein tyrosine phosphatase 1B (PTP1B), and CDC25 (68, 69, 99, 101), and inhibit expression of genes such as the one encoding for the adaptor protein Lnk, a negative regulator of cytokine receptor signaling (126). More recently, ROS have been implicated as mediators of a newly discovered nonapoptotic form of cell death termed ferroptosis, which requires mainly iron (19). Importantly, ROS directly regulate the function of a number of proteins implicated in stress response and metabolism (see Table 1). Recent findings describe a physiological function for ROS in the control of disease and developmental processes (33, 35, 78, 89) further supporting a key function for ROS in cellular signaling in vivo.
Table 1.
Direct ROS Modification of Key Proteins Regulating Stem Cell Function
| Protein | Residue | Modification | Experimental system | Effect | Description | Reference |
|---|---|---|---|---|---|---|
| ATM | C2991 | Disulfide Bond | Primary human fibroblasts, AT1-ABR | Activating | Oxidation of CYS-2991 activates dimer form of ATM through covalent linkage of two ATM monomers and changes substrate specificity from that of only DNA damage repair proteins to downstream effectors of oxidative stress regulation. However, many downstream proteins regulated by oxidized ATM overlap with those regulated by phosphorylated ATM (induced by double stranded DNA breaks). | (27, 28) |
| AKT | C297, C311 | Disulfide Bond | H9C9, mouse ventral midbrain | Varied | Oxidation of CYS-297 and CYS-311 causes formation of an intramolecular disulfide bond leading to inactivation of AKT through improved association w/PP2A, modification can be reversed by glutaredoxin. | (56, 73, 102) |
| FOXO | C477-FoxO4 | Disulfide Bond | HEK293T, DLD1, MEF | Varied | Dansen et al. demonstrate ROS oxidation of CYS-477 on FoxO4 causes association with CBP/p300 through a disulfide bond and subsequent acetylation leading to differential targeting by FoxO4. | (15) |
| mTORC1 | Unknown | Unknown | HEK293T | Activating | Treatment of mTOR with cysteine oxidizers prevents binding of Raptor and enhances kinase activity of mTOR specifically on S6K1. However, treatment with antimycin A, normally causing increased ROS production by mitochondria, had contrasting effects seen with increased association with Raptor and inhibition of S6K1 phosphorylation. Yoshida et al. show cysteine oxidizers regulating Rheb, leading to active mTORC1. (No direct modification of mTOR by H2O2) | (95, 128) |
| p53 | C141, Y327 | Glutathionylation, Nitration | U87MG, HCT116, MCF7, SAOS-2 | Varied | Glutathionylation of CYS-141 induced by H2O2, inactivates p53 by preventing its dimerization and DNA binding ability. Nitric oxide-mediated nitration of tyr327 enhances p53 nuclear localization and DNA binding activity by increasing oligomerization of p53. | (119, 125) |
| PTEN | C124, C71 | Disulfide Bond | HELA, U87MG, HEK293T, 3T3 | Inhibitory | Oxidation of the catalytic cysteine CYS-124 triggers disulfide bond formation with CYS71 and leads to loss of enzymatic activity. | (59, 62, 101) |
| SIRT | C67-SIRT1 | S-Glutathiolation | HEK293T, BAEC | Indirect Inhibition | Oxidation of CYS-67 by S-nitrosoglutathione (GSNO, a product of nitric oxide and glutathione) prevents SIRT1 activation by resveratrol though leading to nitrosylation and subsequent covalent addition of glutathione. Basal activity levels are unaffected. | (131) |
PTEN, phosphatase and tensin homology; mTOR, mammalian target of rapamycin; ATM, ataxia telangiectasia mutated; H2O2, hydrogen peroxide.
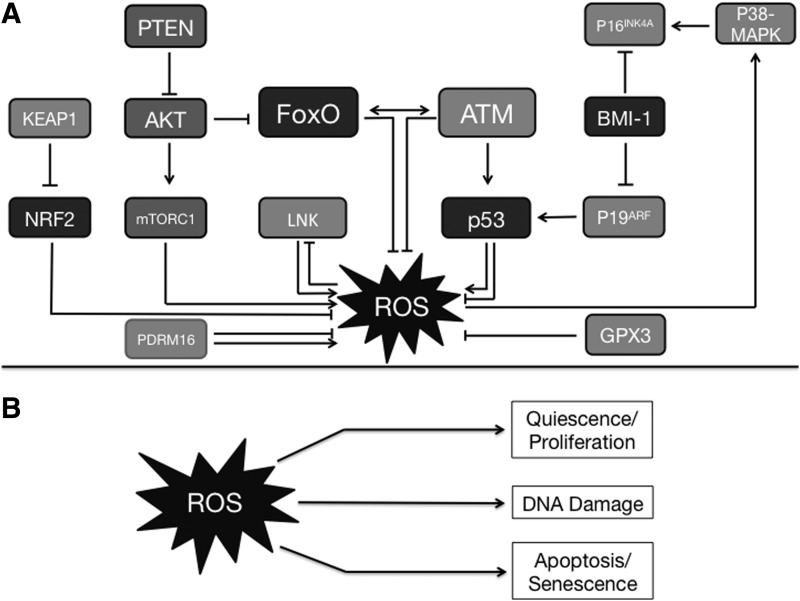
ROS in the Regulation of Stem and Progenitor Cells
The few number of adult stem cells and the lack of easy access to these cells limits to a large extent biochemical and molecular approaches that are routinely used in studies of somatic cells or cultured lines. Nonetheless, work in the past decade has remarkably improved our understanding of ROS regulation of stem cells. ROS are emerging as critical physiological regulators of stem and progenitor cells (Fig. 4). While HSCs have low levels of ROS as compared to their more mature progenies (49), neural stem cells (NSCs) (58) accumulate high levels of ROS that control their proliferation and self-renewal. When bone marrow regions are divided according to their levels of ROS, all long-term HSCs capable of generating more than 20% chimerism 20 weeks after transplantation into lethally irradiated mice are found within the bone marrow compartment with relatively low levels of ROS (49). Specifically, HSCs with lower ROS levels engraft irradiated recipients better than do HSCs with higher ROS content (49). A higher percentage of cells with low ROS levels were in G0 indicating their low cycling status. These cells express high levels of Notch1, cdkn1a (p21), N-cadherin, and CaR and low levels of p16 and mammalian target of rapamycin (mTOR) as compared to ROS high cells enriched for hematopoietic progenitors. In these studies, the low but detectable levels of p53 in ROS low cells were significantly higher than levels found in ROS high cells. These studies also indicated that in vitro treatment with either N-acetylcysteine (NAC), a generator of glutathione in scavenging ROS, or inhibitors of p38 mitogen-activated protein kinase (MAPK), or mTOR all led to full recovery of hematopoietic cell activity in culture. Although these latter experiments were not conducted in vivo, they suggest that at least some of the ROS-mediated effects on multipotent progenitors are reversible. They also indicate that a connective network of ROS-p38MAPK and mTOR participate in the control of the hematopoietic stem/progenitor cell pool (Fig. 4). Indeed, ROS regulation of p38MAPK has been implicated in the loss of self-renewal of HSC during serial transplantation—a classic unexplained observation regarding HSCs (48). ROS also regulate mTOR directly by controlling the interaction of mTOR with mTOR regulator raptor (95, 128). In turn, activation of mTOR leads to increased oxidative stress in HSCs and loss of HSC function (13).
FIG. 4.
ROS regulation of signaling pathways in stem cells. (A) In stem cells, a variety of proteins that respond to ROS can determine cellular outcomes, such as whether to enter the cell cycle or remain quiescent. Proteins, including transcription factors p53, PDRM16, FoxO, and NRF2 can, in turn, regulate levels of ROS. (B) A schematic of effects of ROS in stem cells. ATM, ataxia telangiectasia mutated
In agreement with the notion that endogenous ROS regulate fundamental properties of HSC and are implicated in diseases of HSC, several models of ROS-mediated HSC deficiencies provide an explanation for the physiological function of ROS in the control of HSC. Two prominent models are mice deficient in ataxia telangiectasia mutated (ATM) and mice deficient in FoxO3 (or triple FoxO). ATM serine threonine protein kinase is a critical enzyme in the regulation of stress response to DNA damage, specifically double strand DNA break (7). Loss of function mutations in ATM is associated with ataxia telangiectasia that is an autosomal disorder characterized by neuronal degeneration, immunodeficiencies, genomic instability, predisposition to lymphomas and other malignancies, and extreme sensitivity to ionizing radiation (4). While ROS are found accumulated in several cell types and tissues of ataxia telangiectasic patients (52) and antioxidant enzymes are either upregulated or downregulated in ATM mutant cells, the mechanism of ATM regulation of ROS is not clear (7, 83). ATM-deficient HSC accumulate ROS, and exhibit a ROS-mediated compromise in their maintenance and repopulation ability. ROS accumulation induces upregulation of the cell cycle regulators cyclin-dependent kinase inhibitors p16INK4a and p19ARF in ATM mutant HSC. p16INK4a and p19ARF tumor suppressors (47) are generated from alternative open reading frames of the INK4a locus. p16INK4a and p19ARF inhibit cell cycle progression through inhibition of inhibitors (therefore activation) of retinoblastoma and p53 proteins respectively. Ectopic expression of the polycomb protein Bmi-1, which represses both p16INK4a and p19ARF, restores the defective stem cell function in ATM−/− mice. Subsequent experiments using E6 or E7 human papilloma viral protein expression demonstrated that upregulation of p16INK4a but not p19ARF mediates the HSC defects in ATM knockout mice. Upregulation of p16INK4a in HSCs is an indicator of aging. These studies imply that ROS-mediated upregulation of p16INK4a induces senescence in ATM−/− HSC leading to their functional impairment.
Accumulation of ROS in FoxO- (or FoxO3)-deficient HSC (70, 114, 126), similar to ATM-deficient HSC (47), has been implicated in the loss of HSC quiescence (although, in this case, ROS regulation of FoxO-deficient or FoxO3-deficient HSC self-renewal is yet to be formally demonstrated). FoxO transcription factors exhibit many tumor suppressor functions, such as inhibition of cell cycle, induction of apoptosis and repair of damaged DNA. FoxO have emerged as key regulators of stem cell pluripotency in adult hematopoietic and neural system (FoxO3) (70, 79, 90, 114, 126), as well as in embryonic cells (FoxO1 and FoxO3 in mouse embryonic stem cells (mESC) and FoxO1 in human ESC) (133). In addition, FoxO3 is essential for the maintenance of oocyte pool (11). Interestingly, FoxO (in particular FoxO3) are essential for the maintenance of leukemic stem cells (40, 75, 107). It is not understood how FoxO3 requirement for maintaining leukemic stem cells is compatible with its function as a tumor suppressor.
Loss of FoxO3 alone recapitulates most of the phenotype observed in triple FoxO (FoxO1, −3 and −4)-deleted mice, albeit with less severity (16, 63, 70, 80, 127). Aging exacerbates the defective FoxO3−/− HSC function (70). FoxO3 may control HSC aging via an intrinsic mechanism. It is also conceivable that, by contributing to tissue oxygenation, FoxO3 regulation of red blood cell lifespan (66) may protect HSC from premature aging. FoxO- and FoxO3- deficient HSC exhibit loss of quiescence, while FoxO-deficient HSC are highly cycling, the cycling of FoxO3- deficient HSC is impaired in that they accumulate in the G2/M phase of cell cycle. It is not known exactly how ROS signaling controls HSC quiescence versus cycling; however, p19ARF/p53 and p16INK4a/Rb have been implicated. As in ATM−/− HSC, p16INK4a, that is a critical regulator of HSC activity and senescence (50), was upregulated in FoxO3−/− HSC (127). However, in contrast to ATM−/− HSC, upregulation of p16INK4a in FoxO3−/− HSC was not mediated by ROS. While p19ARF was not significantly modulated in FoxO3 mutant HSC, upregulation of the p53/p21 axis was found to be mediated by the accumulation of ROS (127). In addition, ATM expression is modulated in a ROS-independent manner by FoxO3 in HSC suggesting that FoxO3 is required for ATM transcription (127). In agreement with the notion that FoxO3 and ATM are part of the same network, FoxO3 also regulates the kinase activity of ATM protein (116). These findings together suggest that both ATM and FoxO3 constitute an important node in the regulation of oxidative stress in HSC. Notably, both FoxO and ATM are redox sensors in that their activity is directly regulated by ROS (24, 28).
Similar to the bone marrow niche, ROS levels were used to subdivide the subventricular zone, a NSC containing niche. High ROS brain cells more closely resembled NSCs based on their ability to form neurospheres in culture. Conversely, cells sorted from the subventricular zone based on known NSC markers exhibit higher levels of ROS compared to nonenriched cells. In these cells, the ROS generating protein NOX is responsible for this increase. It was shown that NOX activation in response to growth factors stimulated the PI3K/AKT pathway through inhibition of PTEN (58). Although, in vivo knockdown of NOX or its inhibition significantly decreased proliferation, self-renewal was not affected and more BrdU label retaining cells were present in the subventricular zone. FoxO are also essential for the regulation of NSCs (79, 90). In FoxO3 (as well as in FoxO1, 3, 4) null cells, a redox-mediated gene expression profile has implicated ROS in the loss of NSC function (90). Similar to HSCs, loss of FoxO in NSCs led to loss of quiescence, increased cycling, decreased self-renewal capacity, and also an increase in ROS) (79, 90). Furthermore, treatment with the antioxidant NAC was able to partially rescue the self-renewal defects, but not the increased cycling in FoxO null NSCs (79). Taken together, proliferation of NSCs requires NOX activation and subsequent ROS signaling through the PI3K/AKT pathway, while FoxO may regulate the transition from quiescence to proliferation that leads to either self-renewal or differentiation, partially through reducing ROS levels.
Similar to the regulation of adult stem cells, FoxO proteins regulate the pluripotency of ESC (133). While only FoxO1 (but not FoxO3) is essential for the expression of master regulators of pluripotency, Oct4 and Sox2, in human ESC, FoxO1 and FoxO3 both are implicated in the control of mESC pluripotency. Although it is clear that FoxO1 regulation of pluripotency in human ESC is not mediated by ROS, whether there is any relationship between FoxO and oxidative stress in the regulation of pluripotency in ESC remains unknown.
AKT serine/threonine protein kinases are upstream negative regulators of FoxO that by phosphorylating FoxO promote their cytosolic localization. AKT exists in three isoforms, and their knockout mouse models exhibit distinct phenotypes. Loss of AKT1 or AKT2 alone has only mild effects on HSC (51). Loss of AKT1 and AKT2 together result in increased quiescence of HSC, which remain in G0 and compete poorly against wild-type HSC in reconstitution of lethally irradiated recipients. This is associated with enhanced maintenance of HSC function through serial transplantation and decreased levels of ROS (51). Together, these studies suggest that potential inhibition of FoxO by AKT is functionally important in the control of HSC. Additional work should clarify whether ROS are involved in the regulation of AKT and FoxO3 in HSC.
The p53 tumor suppressor has also been implicated in the control of HSC (65, 112). In contrast to FoxO and ATM, loss of p53 results in increased quiescence of long-term repopulating HSC and is associated with an increased ability to promote competitive repopulation (65, 112) suggesting that maintenance of HSC homeostasis may involve a balance of FoxO, ATM with p53. Interestingly, the increased HSC function seen in p53-null mice is associated with death if the recipient mice are lethally irradiated. Indeed, irradiated mice transplanted with p53−/− HSC succumb to lymphomas within 4 months after transplantation (65, 112).
p53 regulates a number of ROS-inducing genes (p53-induced genes) that modulate apoptosis via control of mitochondria in tumor cells (86). Interestingly, p53, like ATM and FoxO, is also a redox sensor (81). Although p53 has been recently implicated in the control of ROS in postnatal bone marrow (1), it is unclear whether p53 regulation of ROS has any function in postnatal or adult HSC.
The polycomb repressor Bmi-1 is another potential regulator of redox status in HSC. Bmi-1 is essential for the regulation of HSC self-renewal via its control of the Ink4a/Arf locus. Bmi-1 was recently found to be essential for the control of mitochondrial function in thymocytes. Increased ROS levels are associated with a decrease in oxygen consumption and ATP production in thymocytes, and increased ROS levels mediate abnormal thymic function and activation of the DNA damage response in thymocytes. Although ROS levels were also elevated in Bmi-1−/− hematopoietic long-term repopulating cells, the contribution of high ROS levels to the abnormal function of these cells in Bmi-1−/− mice is not known (64). These findings suggest that Bmi-1 (and perhaps other critical regulators of HSC self-renewal) may have important functions in controlling mitochondria and/or controlling the DNA damage response in HSC.
Another redox regulator of stem cells is the PR domain containing 16 (PRDM16) transcription factor (2, 14). PRDM16 is a regulator of human leukemogenesis and brown fat. PRDM16 also regulates redox status in neuronal and HSCs (14). Loss of PRDM16 results in abnormal cycling and significantly increased cell death in stem cells. However, while ROS are increased in PRDM16−/− NSCs and mediate some of the neural stem progenitor defects in PRDM16−/− mice, the levels of ROS in PRDM16−/− HSCs are decreased (14).
In Drosophila, ROS are involved in the control of hematopoietic stem/progenitor cell differentiation, as well as homeostasis of intestinal stem cells. Endogenous ROS signaling regulates blood stem cells via FoxO and JNK activation (78). The regulation of intestinal stem cells in Drosophila is through the Keap-nuclear factor-erythroid-2-related factor 2 (Nrf2) antioxidant axis (42). It was shown that Nrf2 is constitutively active in ISC. Nrf2 belongs to the cap-n-collar subfamily of the basic leucine zipper (b-Zip) transcription factors and is ubiquitously expressed as a master regulator in the antioxidant response pathway. Loss of Nrf2 in ISCs causes accumulation of ROS and accelerates age-related degeneration of the intestinal epithelium. These findings establish that Keap1 and Nrf2 comprise a critical redox management system that regulates stem cell function, and raise the question as to whether these regulators are involved in other high-turnover tissue stem cells (42). Interestingly, it was recently shown that loss of Nrf2 results in loss of quiescence of HSCs, expansion and hematopoietic stem and progenitors and alterations in cell migration and bone marrow retention suggesting a critical function in the regulation of HSC (115).
Many of the proteins discussed here, such as ATM, p53, FoxO, mTORC1, AKT, and PTEN (15, 24, 27, 28, 56, 59, 62, 73, 95, 101, 102, 119, 125, 128) all of which have important functions in the control of stem cells, are redox sensors, in that their activity is directly modulated by ROS (Table 1). This common property raises the possibility that ROS have a key function in coordinating the interactions of the PTEN/AKT/mTOR/FoxO pathway with ATM and p53. It is also tempting to speculate that mechanisms that control ROS in stem cells are directly implicated in the control of stem cell fate. It remains to be seen whether redox state is implicated in the regulation of these proteins in stem cells.
The gradual loss of function through serial transplantations or in long-term suspension cultures are well recognized features of HSC (36, 37). ROS are recognized as potential mediators of the loss of HSC function in these settings as antioxidant treatment improves (almost normalizes) HSC function throughout serial transplantation and in long-term in vitro culture (48). ROS activation of p38-MAPK is implicated in limiting HSC function both in vivo and in vitro (48). Exactly how ROS control HSC function is not known. One potential mechanism is through the regulation of the response to DNA damage or through regulation of DNA repair. In support of this, there is recently reported evidence that accumulation of oxidative DNA damage restricts the self-renewal capacity of human HSCs (124).
ROS, Aging, and Malignancy
Aging is associated with reduced tissue regeneration leading to increased degenerative disease and cancer. Stem cells regenerate many adult tissues and are implicated in the development of cancer. It is therefore, thought that age-related changes in stem cells may contribute to age-related disease. Consistent with this, stem cell function declines with age in numerous tissues as result of accumulation of DNA damage, mitochondrial damage, epigenetic and environmental modulations, etc. Whether and to what extent ROS contribute to the aging of stem cells is an active area of research. Excessive ROS concentrations lead to abnormal proliferation, growth, and malignancies (47, 77). This has been particularly illustrated in peroxiredoxin 1-deleted mice, which exhibit severe ROS-mediated hemolytic anemias and tumor formation (lymphomas, carcinomas and sarcomas) (77) later in life, and in superoxide dismutase 2-deleted mice, which exhibit oxidative stress mediated hematopoietic abnormalities (23, 67).
Aged HSC are compromised in their regeneration and tissue repair capacity. Aging is associated with HSC expansion, compromise of their homing, gradual loss of their function, HSC myeloid biased-differentiation, and onset of anemia (20, 93, 103). Studies in the past decade suggest redox pathways contribute to the HSC aging. Specifically, alterations in the regulation of ROS by FoxO3 and ATM with age contribute to HSC aging (47, 48, 70). However, underlying mechanisms remain unknown. The importance of the PTEN/AKT/mTOR/FoxO signaling pathway in the control of ROS in stem cells, as well as its involvement in the control of cellular aging, raises the possibility that the regulation of ROS may be implicated in the rate of stem cell aging.
Myeloproliferative neoplasms (MPN) encompass a number of preleukemic blood stem cell disorders that occur with increasing frequency with age and result in the expansion of a myeloid lineage. FoxO-triple mutant and FoxO3−/− mice exhibit myeloproliferative activity reminiscent of human MPN (114, 126). The myeloproliferation in FoxO3−/− mice is characterized by over accumulation of ROS, which are the principal mediator of amplification of the FoxO3−/− hematopoietic progenitor pool and of myeloproliferative-like syndrome in mice (126). ROS activation of the AKT/mTOR signaling pathway as part of a feedback loop has been implicated in the myeloproliferation. Consistent with these findings, constitutive activation of AKT (a negative regulator of FoxO) in mouse HSCs leads to a myeloproliferative disease associated with lymphoblastic thymic T cell lymphoma. A small but significant percentage of these mice develop acute myeloid leukemias (AML) without pre-existing MPN, although AML is not seen in FoxO3−/− or triple FoxO-deleted mice. The AKT-driven disorders in this model are not redox sensitive, but treatment with rapamycin to inhibit mTOR signaling was found to partially improve the T cell lymphoma (54). In contrast, the MPN (or AML) in this model (in contrast to MPN in FoxO3−/− mice) was not sensitive to rapamycin. Nonetheless, in other models, AML seems to be sensitive to rapamycin (132).
The analysis of myeloproliferation in FoxO3−/− mice also suggests that ROS-mediated regulation of SH2B3 (Lnk) adaptor protein expression significantly enhances the sensitivity of cytokine signaling to changes in physiological ROS, and leads to increased cycling and expansion of FoxO3 mutant hematopoietic progenitor cells. Lnk is a negative regulator of cytokine receptor signaling (108, 118) that binds to JAK2 protein tyrosine kinase (and thrombopoietin receptor) and downregulates thrombopoietin receptor signals that are essential for supporting HSC. In Drosophila, dFoxO represses Lnk expression directly. Also, in Drosophila, Lnk negatively regulates lifespan via control of oxidative stress (105). Overall, Lnk is a negative regulator of HSC (10). Lnk−/− HSC are increasingly quiescent and exhibit enhanced self-renewal (10). Loss of Lnk may contribute to protecting HSC from aging (9). Consistent with the model of ROS as a stem cell rheostat, the levels of ROS are lower in Lnk−/− HSC than in wild type controls (Bigarella, Liang and Ghaffari, unpublished findings). These findings raise the possibility that modulations of ROS are highly connected to HSC function and aging, and to longevity of the whole organism, the point where the stem cell theory of aging and the oxygen radical theory of aging may intersect.
Sirtuins, a family of NAD-dependent deacetylases (with seven members in mammals), are implicated in the regulation of aging, oxidative stress, and metabolism. SIRT1 controls apoptosis of mouse embryonic stem cells (mESC) by regulating nuclear versus mitochondrial localization of p53 in response to endogenous oxidative stress (34) (Fig. 5). SIRT1 is further implicated in the regulation of mitochondrial biogenesis in skeletal muscle (88). Whether SIRT1 has any function in the redox regulation of adult stem cells remains unknown (131). Interestingly, recent findings suggest that SIRT3, another member of the sirtuin family, which has a critical function in the maintenance of mitochondria and metabolism (55), is essential for the control of ROS during aging of HSC. SIRT3 was shown to enhance the function of old HSC, suggesting that aging of stem cells may be reversible. As old HSC are implicated in blood malignancies, such as leukemias, MPNs, and myelodysplasia, the possibility that SIRT3 plays a role in the initiation or maintenance of these disorders requires further investigations. Similarly, it will be interesting to determine if polymorphism in SIRT3 expression (or modulation of SIRT3 deacetylase activity) is associated with longevity, as has been proposed for FoxO3 (120, 121).
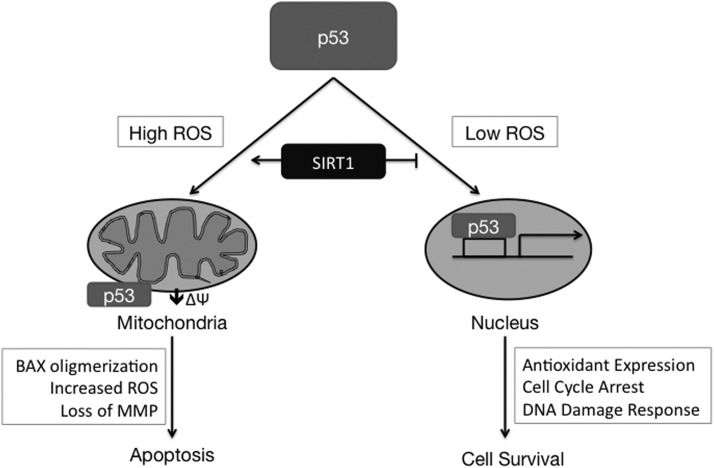
FIG. 5.
SIRT1 mediated apoptosis in mESCs [adapted from Gurumurthy et al. (29)]. In response to ROS, p53 can either induce apoptosis, under high ROS concentrations, or initiate events that promote cell survival, under low ROS conditions. Deacetylation of p53 by SIRT1 prevents nuclear translocation and promotes the proapoptotic response elicited by cytosolic p53. mESC, mouse embryonic stem cells.
HSC and Mitochondria
Studies of liver kinase B1 (LKB1) knockout mice have revealed important functions for mitochondria in stem cells (94). Loss of LKB1 (25, 29, 76), an evolutionarily conserved regulator of cellular energy metabolism, leads to pancytopenia, loss of HSC reserves, decreased mitochondrial biogenesis, reduced energy production, reduced mitochondrial membrane potential, and reduced ATP levels. LKB1 is an upstream kinase acting on adenine monophosphate-activated protein kinase (AMPK) (Fig. 6). By phosphorylating tuberous sclerosis complex, AMPK negatively regulates mTORC1. Although loss of LKB1 leads to the activation of mTORC1, ROS levels are not altered in LKB1−/− or AMPK−/− HSC (or any other hematopoietic cell examined), and the LKB1 HSC phenotype seems to be mTOR-independent. Loss of AMPK function leads to mitochondrial defects and mildly altered HSC function and decreased long-term multilineage reconstitution but does not phenocopy the effects of LKB1. A critical outcome of these studies is that the regulation and function of LKB1/AMPK/mTORC1 seems to be specific to HSC and distinct from their function in more committed hematopoietic progenitors. Loss of LKB1 leads to defective centrosomes and mitotic spindles with consequent aneuploidy. These studies illustrate the complex and specific function of metabolic pathways and mitochondria in the control of HSC cycling and dormancy; the results suggest that tight regulation of energy metabolism is critically involved in the control of mitosis in stem cells.
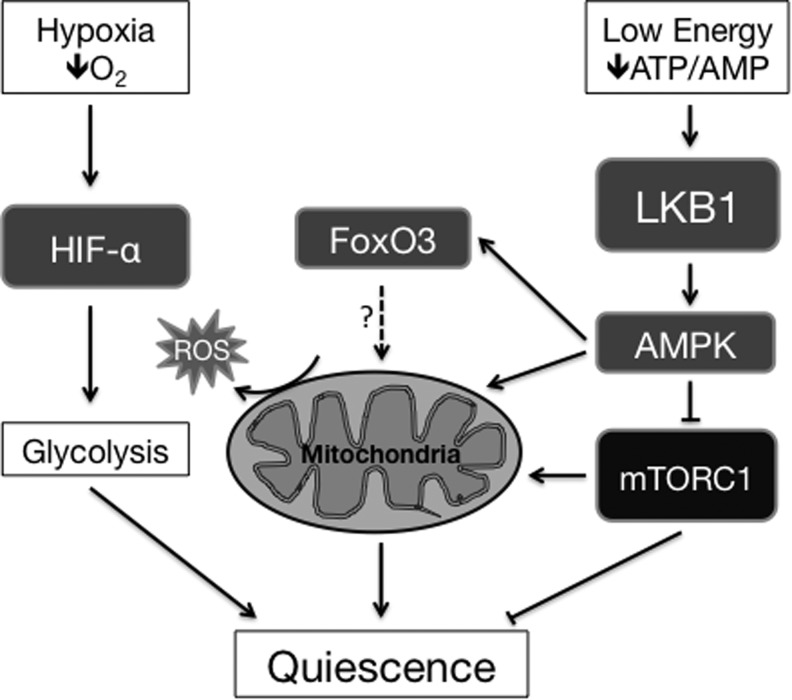
FIG. 6.
Mitochondrial and metabolic control of HSC quiescence. While glycolytic metabolism is crucial for maintenance of HSCs in quiescence, functional mitochondria are also necessary. LKB1 and AMPK can be activated upon low energy conditions to regulate mitochondrial function and biogenesis, partially through the inhibition of anabolic processes mediated by mTORC1. FoxO3 may also have a potential role in regulating mitochondrial function. HSC, hematopoietic stem cells; AMPK, adenine monophosphate-activated protein kinase; LKB1, liver kinase B1.
Signaling by mTOR protein kinase has also been implicated in the control of mitochondria. mTOR is a critical regulator of normal hematopoietic and leukemic stem cells. Loss of Tsc1, an upstream inhibitor of mTOR, leads to mTORC1 activation, loss of HSC quiescence, enhanced mitochondrial biogenesis, and ROS accumulation leading to HSC activation and progressive loss of the HSC pool (13). Loss of HSC activity is partially restored by scavenging ROS via administration of NAC in vivo. As mTOR signaling is increasingly implicated in the regulation of longevity, it will be interesting to determine if mTOR regulation of stem cells and aging are interrelated.
HIF-1 Mediated Hypoxic Response
The hypoxic response occurs at cellular O2 levels ranging from 0.3% to 3%, and is regulated by the master transcriptional regulator of hypoxic response (hypoxia-inducible factor [HIF]). To maintain oxygen homeostasis at normoxic levels, the response to hypoxia is two-fold. First, the cell decreases oxygen consumption by inhibiting ATP intensive processes and switching to glycolytic metabolism. Second, the tissue increases the local oxygen supply through angiogenesis and erythropoiesis (60). The hypoxic response is critical for stem cell maintenance (61, 104). The HIF-1 complex, a heterodimer of a HIF-α subunit and a HIF-1β subunit, activates most of the genes that induce angiogenesis, erythropoiesis, and glycolysis, including vascular endothelial growth factor, erythropoietin, and various glycolytic enzymes. HIF-α has three isoforms, HIF-1α, HIF-2α, and HIF-3α, which exhibit differing tissue specificities and regulate different genes. Both HIF-α and HIF-β subunits are expressed constitutively, but HIF-α stability is dependent on oxygen availability. Under normoxia, HIF-α is hydroxylated at proline residues within its oxygen dependent domain by prolyl hydroxylases (PHD) (Fig. 7). PHD function is dependent on oxygen as a substrate and requires the cofactors α-ketoglutarate and iron (100). After hydroxylation, HIF-α becomes a target of the Von Hippel-Lindau protein (pVHL) E3 ubiquitin ligase. Ubiquitination of HIF-α allows for recognition and subsequent proteasomal degradation (53). Under hypoxia, PHD loses the ability to modify HIF-α leading to its stabilization and heterodimerization with HIF-1β.
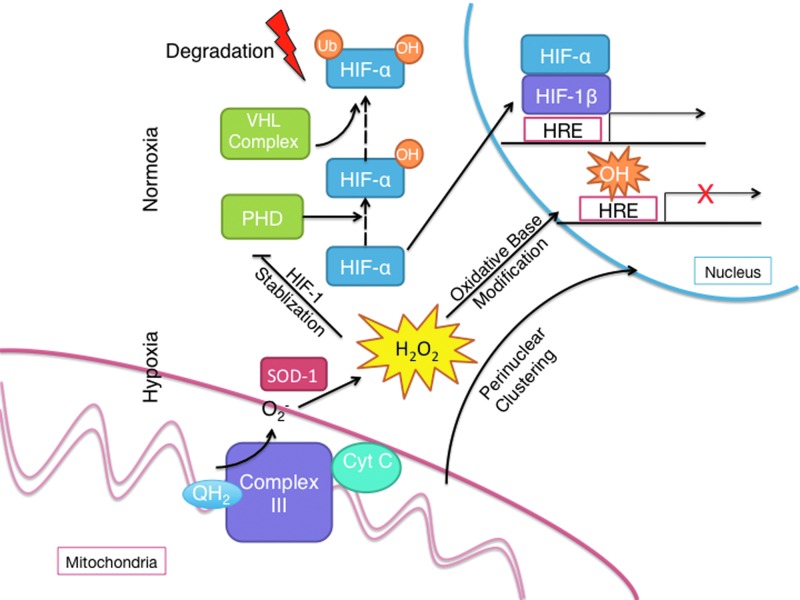
FIG. 7.
ROS mediated HIF response. Under normoxia, HIF-1α and HIF-2α are hydoxylated by prolyl hydroxylases, allowing them to be recognized by the VHL complex. The VHL complex polyubiquinates HIF-α leads to proteosomal degradation. Under hypoxia, mitochondrial complex III increases generation of cytosolic superoxide, which is quickly dismutated into hydrogen peroxide. The rise in hydrogen peroxide activates HIF-α by preventing PHD mediated HIF-α hydroxylation. Furthermore, it elicits perinuclear clustering of mitochondria and oxidative base modifications that are associated with transcriptional activation at HREs. HIF, hypoxia-inducible factor; HRE, hypoxic response elements. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/ars
Unexpectedly, multiple in vitro studies have shown that an increase in ROS production stimulates the hypoxic response to low cellular oxygen (1.5% O2) (12, 32). Details of the pathway have yet to be elucidated, but complex III of the mitochondrial electron transport chain is a probable source of the enhanced generation of ROS that have been linked to stabilization of HIF1a. There are also several reports that hypoxia-generated ROS oxidize specific residues in hypoxia response elements (HREs) of hypoxia-inducible genes. On the basis of multiple lines of indirect evidence, it has been speculated that hypoxia-induced base modifications might contribute to transcriptional regulation (see Fig. 7). However, isolated mitochondria actually produce lower amounts of ROS as concentrations of oxygen decrease. This suggests that a decrease in oxygen concentration alone is not sufficient to increase ROS production, and upstream factors that increase superoxide generation by complex III are necessary. Importantly, hypoxia-induced ROS are required for activation of the hypoxic response (12, 130). The contradictory roles of mitochondrial ROS raise the question as to whether ROS generation results from inefficiencies within the electron transport chain or is a tightly regulated process. The debate as to whether mitochondrial ROS are required for HIF signaling is specifically of interest to stem cell biologists, as localization of adult stem cells in hypoxic niches is critical to the maintenance of the stem cell pool, and HIF1α is critical for the maintenance of stem cells (109). Although ROS levels measured by MitoTracker Orange (CM-H2TMRos) are increased in HIF-1α-deleted HSC, the potential function of ROS in this context in stem cells has not been evaluated (109).
Cancer Stem Cells
The cancer stem cell hypothesis postulates that most tumors are highly heterogeneous in their cellular components and only a small subset of cells within the tumor that have self-renewing potential maintain the disease. Although the molecular bases of cancer stem cell self-renewal are unknown, it is hypothesized that many cancer stem cells share many of the same regulatory mechanisms as normal adult stem cells (91). The levels of ROS prove to be of importance in cancer stem cells, the self-renewing and tumorigenic subpopulation within a tumor. Cancer stem cells have been functionally characterized in multiple types of cancers through their ability to generate a tumor after transplantation into a new animal and can be distinguished by their cell surface markers. Diehn and Majeti show ROS levels are significantly lower in CSCs derived from murine and human solid tumors when compared to nontumorigenic cells from matched tumor masses when measured by dichlorofluorescein diacetate (DCF-DA), a marker of H2O2 (17, 18). However, when murine CSCs are sorted according to ROS concentration based on DCF-DA intensity, both low and high ROS populations are able to establish tumors in recipient mice, which suggest ROS levels alone do not determine tumorigenicity. Nevertheless, the lower levels of ROS in cancer stem cells are attributed to an upregulation of antioxidant genes that functionally results in increased resistance to free radical damage induced by ionizing radiation. DNA damage assays demonstrate that CSCs incur less DNA damage compared to the nontumorigenic cells after irradiation. Furthermore, inhibition of ROS scavenging by CSCs sensitizes them to irradiation, and conversely, addition of antioxidants to nontumorigenic tumor cells provides protection against irradiation.
Like adult stem cells, cancer stem cells exhibit low accumulation of ROS as compared to their normal tissue counterparts. They are exquisitely sensitive to ROS, equipped with a strong antioxidant and DNA damage repair arsenal and are highly sensitive to antioxidant depletion (17, 18). Evidence from studies of parthenolide, a naturally occurring molecule, in human AMLs suggests that ROS production preferentially targets leukemic cells and induces apoptosis (30, 31). The set of genes enriched for in CSC's mainly involve glutathione metabolism, a protein required for H2O2 scavenging. A similar phenomenon is seen in leukemic stem cells (LSC), which overexpress glutathione peroxidase 3 (GPx3) relative to normal leukemic cells (41). GPx3 is an enzyme that catalyzes the oxidation of glutathione by H2O2 to prevent it from forming more toxic intermediates. The high levels of GPx3 lead to low levels of ROS within LSCs and provide them with a greater proliferative capacity shown by comparison with GPx3 knock down LSCs in a competitive repopulation assay. Additionally, mRNA levels of GPx3 correlate well with clinical severity of AML. In summary, CSCs gain various methods of scavenging ROS through increased expression of antioxidant genes, which in turn increase their self-renewal potential and protect against irradiation. These findings indicate that interfering with ROS management may provide a potential target for therapy of cancer. More recently, low levels of ROS have been associated with leukemic stem cell properties of human AML providing an opportunity to target these cells directly (57). Directly comparing the high ROS to the low ROS AML cell population, instead of segregating leukemic stem cells based on established cell surface markers, revealed that the low ROS fraction possess a lower metabolic rate dependent on oxidative phosphorylation. Disruption of mitochondrial energy production by targeting BCL-2, a gene found highly upregulated in the low ROS population, selectively induced an increase in ROS and apoptosis in low ROS cells (57). Intriguingly, addition of antioxidants could not rescue BCL-2 inhibited low ROS containing AML cells, suggesting the mechanism of killing is not through increased ROS. Whether directly targeting the antioxidant machinery of the low ROS fraction could also eradicate them, was untested. Nevertheless, cancer stem cells appear to contain low levels of ROS that are associated with functional benefits, such as radioresistance and self-renewal potential, which makes targeting this population crucial in eliminating the tumor.
Along the same lines, targeting proteins that regulate ROS levels could potentially be an effective way of killing CSCs. Using a histone deacetylase inhibitor (HDACi) against leukemia cell lines demonstrates this effect, seen through the induction of cell death as a result of increased ROS levels (44). HDACi stimulates activity of NADPH oxidase, one of the main sources of cellular ROS, while subsequently causing nuclear translocation of NRF2, a transcription factor controlling many of the genes responsible for antioxidant activity. Furthermore, a synergistic relationship as measured by cell death is observed when cells are treated with a drug that depletes glutathione, β-phenylethyl isothiocyanate after treatment by an HDACi. The same combinatorial treatment can also overcome HDACI resistance, which arises due to the transcriptional upregulation of antioxidant genes by NRF2. The cytotoxicity of the drugs can be inhibited through pretreatment with NAC, a molecule, which enhances glutathione synthesis. Although these experiments do not distinguish between CSCs and the rest of the leukemic cell population, modulating ROS levels proves to be an effective way of targeting leukemia.
ROS may participate in the events that initiate leukemia and be a potential contributor to leukemic transformation. Experimental evidence show ROS promoting growth factor independent proliferation, an initial step of tumorgenesis, in hematopoietic progenitors induced by ectopic expression of constitutively active RAS (43). RAS activation leads to ROS production by NADPH oxidase, which together with RAS increases proliferation of transfected hematopoietic progenitors cultured in serum and growth factor free media. It is important to note that although proliferation increases, survival is diminished in cells transfected with oncogenic RAS as an effect of increased ROS demonstrated by the increase in percent cell viability of transfected cells when treating with antioxidants.
Stem Cells in the Clinic
One of the most promising applications of stem cells is to utilize the self-renewal and multipotent nature of stem cells as a therapy to replenish various cell types and tissues destroyed by disease. However, because stem cells samples are precious and not easy to acquire, storage of samples remains an important objective. Research into the role of ROS in stem cells can lead to more efficient methods of cryopreservation, which allows for the long-term storage of cells so they can be used at later time points for therapeutic or research uses. The technique employs slowly freezing cells to a temperature of −196°C in the presence of dimethylsulfoxide, both elements that reduce the formation of damaging ice crystals (96). Although most mammalian cell types can be cryopreserved and recovered with standard protocols, efficient recovery of cryopreserved stem cells is much more challenging. The reason being that after freezing and thawing there is a significant increase in ROS, which stem cells are uniquely sensitive to. The increase in ROS after cryopreservation was shown to induce apoptosis in human embryonic stem cells and contribute to the poor recovery rate (123). In subsequent studies, incorporating methods that minimize ROS levels over the whole cryopreservation process led to increased viability and cell recovery (71, 96).
Concluding Remarks
Regulation of ROS is clearly of critical importance to adult stem cells. Less is known about ROS regulation of embryonic stem cells. Although key transcription factors and signaling proteins have been identified, the exact mechanism by which ROS control stem cell transcriptional network is unknown. Future studies on how ROS interconnect cell cycle and apoptotic machinery, whether ROS impact the stem cell epigenome as well as whether and how ROS influence stem cell fate determination, stem cell transformation and aging should clarify the details, as well as the importance, of the ROS regulated network in adult and embryonic stem cell biology.
Abbreviations Used
- AML
acute myeloid leukemia
- AMPK
adenine monophosphate-activated protein kinase
- ATM
ataxia telangiectasia mutated
- ATP
adenosine triphosphate
- DCF-DA
dichlorofluorescein diacetate
- ESC
embryonic stem cells
- GPx3
glutathione peroxidase 3
- H2O2
hydrogen peroxide
- HDACi
histone deacetylase inhibitor
- HIF
hypoxia-inducible factor
- HRE
hypoxic response elements
- HSC
hematopoietic stem cells
- LKB1
liver kinase B1
- MAPK
mitogen-activated protein kinase
- mESC
mouse embryonic stem cells
- MPN
myeloproliferative neoplasms
- mTOR
mammalian target of rapamycin
- NAC
N-acetylcysteine
- Nrf2
nuclear factor-erythroid-2-related factor 2
- NSC
neural-stem cell
- PRDM16
PR domain containing 16
- PTEN
phosphatase and tensin homology
- ROS
reactive oxygen species
- SOD
superoxide dehydrogenase
Acknowledgments
This work was supported in part by National Institutes of Health grants RO1 DK077174, New York State Stem Cell Science (NYSTEM) award (CO24408), Irma Hirschl/Weill-Caulier Trust Research Award and MPN Research Foundation (to S.G.), and RO1 RHL116365A (S.G., CoPI). R.L. is supported by GM008553 NIH T32 training grant.
References
- 1.Abbas HA, Maccio DR, Coskun S, Jackson JG, Hazen AL, Sills TM, You MJ, Hirschi KK, and Lozano G. Mdm2 is required for survival of hematopoietic stem cells/progenitors via dampening of ROS-induced p53 activity. Cell Stem Cell 7: 606–617, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aguilo F, Avagyan S, Labar A, Sevilla A, Lee DF, Kumar P, Lemischka IR, Zhou BY, and Snoeck HW. Prdm16 is a physiologic regulator of hematopoietic stem cells. Blood 117: 5057–5066, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balaban RS, Nemoto S, and Finkel T. Mitochondria, oxidants, and aging. Cell 120: 483–495, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Barlow C, Hirotsune S, Paylor R, Liyanage M, Eckhaus M, Collins F, Shiloh Y, Crawley JN, Ried T, Tagle D, and Wynshaw-Boris A. Atm-deficient mice: a paradigm of ataxia telangiectasia. Cell 86: 159–171, 1996 [DOI] [PubMed] [Google Scholar]
- 5.Barrett WC, DeGnore JP, Keng YF, Zhang ZY, Yim MB, and Chock PB. Roles of superoxide radical anion in signal transduction mediated by reversible regulation of protein-tyrosine phosphatase 1B. J Biol Chem 274: 34543–34546, 1999 [DOI] [PubMed] [Google Scholar]
- 6.Barrett WC, DeGnore JP, Konig S, Fales HM, Keng YF, Zhang ZY, Yim MB, and Chock PB. Regulation of PTP1B via glutathionylation of the active site cysteine 215. Biochemistry 38: 6699–6705, 1999 [DOI] [PubMed] [Google Scholar]
- 7.Barzilai A, Rotman G, and Shiloh Y. ATM deficiency and oxidative stress: a new dimension of defective response to DNA damage. DNA Repair (Amst) 1: 3–25, 2002 [DOI] [PubMed] [Google Scholar]
- 8.Bedard K. and Krause KH. The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev 87: 245–313, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Bersenev A, Rozenova K, Balcerek J, Jiang J, Wu C, and Tong W. Lnk deficiency partially mitigates hematopoietic stem cell aging. Aging Cell 11: 949–959, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bersenev A, Wu C, Balcerek J, and Tong W. Lnk controls mouse hematopoietic stem cell self-renewal and quiescence through direct interactions with JAK2. J Clin Invest 118: 2832–2844, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castrillon DH, Miao L, Kollipara R, Horner JW, and DePinho RA. Suppression of ovarian follicle activation in mice by the transcription factor Foxo3a. Science 301: 215–218, 2003 [DOI] [PubMed] [Google Scholar]
- 12.Chandel NS, Maltepe E, Goldwasser E, Mathieu CE, Simon MC, and Schumacker PT. Mitochondrial reactive oxygen species trigger hypoxia-induced transcription. Proc Natl Acad Sci U S A 95: 11715–11720, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen C, Liu Y, Liu R, Ikenoue T, Guan KL, and Zheng P. TSC-mTOR maintains quiescence and function of hematopoietic stem cells by repressing mitochondrial biogenesis and reactive oxygen species. J Exp Med 205: 2397–2408, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chuikov S, Levi BP, Smith ML, and Morrison SJ. Prdm16 promotes stem cell maintenance in multiple tissues, partly by regulating oxidative stress. Nat Cell Biol 12: 999–1006, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dansen TB, Smits LM, van Triest MH, de Keizer PL, van Leenen D, Koerkamp MG, Szypowska A, Meppelink A, Brenkman AB, Yodoi J, Holstege FC, and Burgering BM. Redox-sensitive cysteines bridge p300/CBP-mediated acetylation and FoxO4 activity. Nat Chem Biol 5: 664–672, 2009 [DOI] [PubMed] [Google Scholar]
- 16.Dejean AS, Beisner DR, Ch'en IL, Kerdiles YM, Babour A, Arden KC, Castrillon DH, DePinho RA, and Hedrick SM. Transcription factor Foxo3 controls the magnitude of T cell immune responses by modulating the function of dendritic cells. Nat Immunol 10: 504–513, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diehn M, Cho RW, Lobo NA, Kalisky T, Dorie MJ, Kulp AN, Qian D, Lam JS, Ailles LE, Wong M, Joshua B, Kaplan MJ, Wapnir I, Dirbas FM, Somlo G, Garberoglio C, Paz B, Shen J, Lau SK, Quake SR, Brown JM, Weissman IL, and Clarke MF. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature 458: 780–783, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diehn M. and Majeti R. Metastatic cancer stem cells: an opportunity for improving cancer treatment? Cell Stem Cell 6: 502–503, 2010 [DOI] [PubMed] [Google Scholar]
- 19.Dixon SJ, Lemberg KM, Lamprecht MR, Skouta R, Zaitsev EM, Gleason CE, Patel DN, Bauer AJ, Cantley AM, Yang WS, Morrison B, 3rd, and Stockwell BR. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 149: 1060–1072, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dykstra B, Olthof S, Schreuder J, Ritsema M, and de Haan G. Clonal analysis reveals multiple functional defects of aged murine hematopoietic stem cells. J Exp Med 208: 2691–2703, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finkel T. Signal transduction by reactive oxygen species. J Cell Biol 194: 7–15, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frassanito MC, Piccoli C, Capozzi V, Boffoli D, Tabilio A, and Capitanio N. Topological organization of NADPH-oxidase in haematopoietic stem cell membrane: preliminary study by fluorescence near-field optical microscopy. J Microsc 229: 517–524, 2008 [DOI] [PubMed] [Google Scholar]
- 23.Friedman JS, Rebel VI, Derby R, Bell K, Huang TT, Kuypers FA, Epstein CJ, and Burakoff SJ. Absence of mitochondrial superoxide dismutase results in a murine hemolytic anemia responsive to therapy with a catalytic antioxidant. J Exp Med 193: 925–934, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fukuoka M, Daitoku H, Hatta M, Matsuzaki H, Umemura S, and Fukamizu A. Negative regulation of forkhead transcription factor AFX (Foxo4) by CBP-induced acetylation. Int J Mol Med 12: 503–508, 2003 [PubMed] [Google Scholar]
- 25.Gan B, Hu J, Jiang S, Liu Y, Sahin E, Zhuang L, Fletcher-Sananikone E, Colla S, Wang YA, Chin L, and Depinho RA. Lkb1 regulates quiescence and metabolic homeostasis of haematopoietic stem cells. Nature 468: 701–704, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghaffari S. Oxidative stress in the regulation of normal and neoplastic hematopoiesis. Antioxid Redox Signal 10: 1923–1940, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guo Z, Deshpande R, and Paull TT. ATM activation in the presence of oxidative stress. Cell Cycle 9: 4805–4811, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guo Z, Kozlov S, Lavin MF, Person MD, and Paull TT. ATM activation by oxidative stress. Science 330: 517–521, 2010 [DOI] [PubMed] [Google Scholar]
- 29.Gurumurthy S, Xie SZ, Alagesan B, Kim J, Yusuf RZ, Saez B, Tzatsos A, Ozsolak F, Milos P, Ferrari F, Park PJ, Shirihai OS, Scadden DT, and Bardeesy N. The Lkb1 metabolic sensor maintains haematopoietic stem cell survival. Nature 468: 659–663, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guzman ML, Rossi RM, Karnischky L, Li X, Peterson DR, Howard DS, and Jordan CT. The sesquiterpene lactone parthenolide induces apoptosis of human acute myelogenous leukemia stem and progenitor cells. Blood 105: 4163–4169, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guzman ML, Rossi RM, Neelakantan S, Li X, Corbett CA, Hassane DC, Becker MW, Bennett JM, Sullivan E, Lachowicz JL, Vaughan A, Sweeney CJ, Matthews W, Carroll M, Liesveld JL, Crooks PA, and Jordan CT. An orally bioavailable parthenolide analog selectively eradicates acute myelogenous leukemia stem and progenitor cells. Blood 110: 4427–4435, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guzy RD. and Schumacker PT. Oxygen sensing by mitochondria at complex III: the paradox of increased reactive oxygen species during hypoxia. Exp Physiol 91: 807–819, 2006 [DOI] [PubMed] [Google Scholar]
- 33.Hamanaka RB, Glasauer A, Hoover P, Yang S, Blatt H, Mullen AR, Getsios S, Gottardi CJ, Deberardinis RJ, Lavker RM, and Chandel NS. Mitochondrial reactive oxygen species promote epidermal differentiation and hair follicle development. Sci Signal 6: ra8, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Han MK, Song EK, Guo Y, Ou X, Mantel C, and Broxmeyer HE. SIRT1 regulates apoptosis and Nanog expression in mouse embryonic stem cells by controlling p53 subcellular localization. Cell Stem Cell 2: 241–251, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harris JM, Esain V, Frechette GM, Harris LJ, Cox AG, Cortes M, Garnaas MK, Carroll KJ, Cutting CC, Khan T, Elks PM, Renshaw SA, Dickinson BC, Chang CJ, Murphy MP, Paw BH, Vander Heiden MG, Goessling W, and North TE. Glucose metabolism impacts the spatio-temporal onset and magnitude of HSC induction in vivo. Blood 121: 2483–2493, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harrison DE. and Astle CM. Loss of stem cell repopulating ability upon transplantation. Effects of donor age, cell number, and transplantation procedure. J Exp Med 156: 1767–1779, 1982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harrison DE, Astle CM, and Delaittre JA. Loss of proliferative capacity in immunohemopoietic stem cells caused by serial transplantation rather than aging. J Exp Med 147: 1526–1531, 1978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He S, Nakada D, and Morrison SJ. Mechanisms of stem cell self-renewal. Annu Rev Cell Dev Biol 25: 377–406, 2009 [DOI] [PubMed] [Google Scholar]
- 39.Hecht D. and Zick Y. Selective inhibition of protein tyrosine phosphatase activities by H2O2 and vanadate in vitro. Biochem Biophys Res Commun 188: 773–779, 1992 [DOI] [PubMed] [Google Scholar]
- 40.Helgason GV, Young GA, and Holyoake TL. Targeting chronic myeloid leukemia stem cells. Curr Hematol Malig Rep 5: 81–87, 2010 [DOI] [PubMed] [Google Scholar]
- 41.Herault O, Hope KJ, Deneault E, Mayotte N, Chagraoui J, Wilhelm BT, Cellot S, Sauvageau M, Andrade-Navarro MA, Hebert J, and Sauvageau G. A role for GPx3 in activity of normal and leukemia stem cells. J Exp Med 209: 895–901, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hochmuth CE, Biteau B, Bohmann D, and Jasper H. Redox regulation by Keap1 and Nrf2 controls intestinal stem cell proliferation in Drosophila. Cell Stem Cell 8: 188–199, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hole PS, Pearn L, Tonks AJ, James PE, Burnett AK, Darley RL, and Tonks A. Ras-induced reactive oxygen species promote growth factor-independent proliferation in human CD34+ hematopoietic progenitor cells. Blood 115: 1238–1246, 2010 [DOI] [PubMed] [Google Scholar]
- 44.Hu Y, Lu W, Chen G, Zhang H, Jia Y, Wei Y, Yang H, Zhang W, Fiskus W, Bhalla K, Keating M, Huang P, and Garcia-Manero G. Overcoming resistance to histone deacetylase inhibitors in human leukemia with the redox modulating compound beta-phenylethyl isothiocyanate. Blood 116: 2732–2741, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Iiyama M, Kakihana K, Kurosu T, and Miura O. Reactive oxygen species generated by hematopoietic cytokines play roles in activation of receptor-mediated signaling and in cell cycle progression. Cell Signal 18: 174–182, 2006 [DOI] [PubMed] [Google Scholar]
- 46.Irani K, Xia Y, Zweier JL, Sollott SJ, Der CJ, Fearon ER, Sundaresan M, Finkel T, and Goldschmidt-Clermont PJ. Mitogenic signaling mediated by oxidants in Ras-transformed fibroblasts. Science 275: 1649–1652, 1997 [DOI] [PubMed] [Google Scholar]
- 47.Ito K, Hirao A, Arai F, Matsuoka S, Takubo K, Hamaguchi I, Nomiyama K, Hosokawa K, Sakurada K, Nakagata N, Ikeda Y, Mak TW, and Suda T. Regulation of oxidative stress by ATM is required for self-renewal of haematopoietic stem cells. Nature 431: 997–1002, 2004 [DOI] [PubMed] [Google Scholar]
- 48.Ito K, Hirao A, Arai F, Takubo K, Matsuoka S, Miyamoto K, Ohmura M, Naka K, Hosokawa K, Ikeda Y, and Suda T. Reactive oxygen species act through p38 MAPK to limit the lifespan of hematopoietic stem cells. Nat Med 12: 446–451, 2006 [DOI] [PubMed] [Google Scholar]
- 49.Jang YY. and Sharkis SJ. A low level of reactive oxygen species selects for primitive hematopoietic stem cells that may reside in the low-oxygenic niche. Blood 110: 3056–3063, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Janzen V, Forkert R, Fleming HE, Saito Y, Waring MT, Dombkowski DM, Cheng T, DePinho RA, Sharpless NE, and Scadden DT. Stem-cell ageing modified by the cyclin-dependent kinase inhibitor p16INK4a. Nature 443: 421–426, 2006 [DOI] [PubMed] [Google Scholar]
- 51.Juntilla MM, Patil VD, Calamito M, Joshi RP, Birnbaum MJ, and Koretzky GA. AKT1 and AKT2 maintain hematopoietic stem cell function by regulating reactive oxygen species. Blood 115: 4030–4038, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kamsler A, Daily D, Hochman A, Stern N, Shiloh Y, Rotman G, and Barzilai A. Increased oxidative stress in ataxia telangiectasia evidenced by alterations in redox state of brains from Atm-deficient mice. Cancer Res 61: 1849–1854, 2001 [PubMed] [Google Scholar]
- 53.Kamura T, Koepp DM, Conrad MN, Skowyra D, Moreland RJ, Iliopoulos O, Lane WS, Kaelin WG, Jr., Elledge SJ, Conaway RC, Harper JW, and Conaway JW. Rbx1, a component of the VHL tumor suppressor complex and SCF ubiquitin ligase. Science 284: 657–661, 1999 [DOI] [PubMed] [Google Scholar]
- 54.Kharas MG, Okabe R, Ganis JJ, Gozo M, Khandan T, Paktinat M, Gilliland DG, and Gritsman K. Constitutively active AKT depletes hematopoietic stem cells and induces leukemia in mice. Blood 115: 1406–1415, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim HS, Patel K, Muldoon-Jacobs K, Bisht KS, Aykin-Burns N, Pennington JD, van der Meer R, Nguyen P, Savage J, Owens KM, Vassilopoulos A, Ozden O, Park SH, Singh KK, Abdulkadir SA, Spitz DR, Deng CX, and Gius D. SIRT3 is a mitochondria-localized tumor suppressor required for maintenance of mitochondrial integrity and metabolism during stress. Cancer Cell 17: 41–52, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Konishi H, Fujiyoshi T, Fukui Y, Matsuzaki H, Yamamoto T, Ono Y, Andjelkovic M, Hemmings BA, and Kikkawa U. Activation of protein kinase B induced by H(2)O(2) and heat shock through distinct mechanisms dependent and independent of phosphatidylinositol 3-kinase. J Biochem 126: 1136–1143, 1999 [DOI] [PubMed] [Google Scholar]
- 57.Lagadinou ED, Sach A, Callahan K, Rossi RM, Neering SJ, Minhajuddin M, Ashton JM, Pei S, Grose V, O'Dwyer KM, Liesveld JL, Brookes PS, Becker MW, and Jordan CT. BCL-2 inhibition targets oxidative phosphorylation and selectively eradicates quiescent human leukemia stem cells. Cell Stem Cell 12: 329–341, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Le Belle JE, Orozco NM, Paucar AA, Saxe JP, Mottahedeh J, Pyle AD, Wu H, and Kornblum HI. Proliferative neural stem cells have high endogenous ROS levels that regulate self-renewal and neurogenesis in a PI3K/Akt-dependant manner. Cell Stem Cell 8: 59–71, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee SR, Yang KS, Kwon J, Lee C, Jeong W, and Rhee SG. Reversible inactivation of the tumor suppressor PTEN by H2O2. J Biol Chem 277: 20336–20342, 2002 [DOI] [PubMed] [Google Scholar]
- 60.Lendahl U, Lee KL, Yang H, and Poellinger L. Generating specificity and diversity in the transcriptional response to hypoxia. Nat Rev Genet 10: 821–832, 2009 [DOI] [PubMed] [Google Scholar]
- 61.Leontieva OV. and Blagosklonny MV. Hypoxia and gerosuppression: the mTOR saga continues. Cell Cycle 11: 3926–3931, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Leslie NR, Bennett D, Lindsay YE, Stewart H, Gray A, and Downes CP. Redox regulation of PI 3-kinase signalling via inactivation of PTEN. EMBO J 22: 5501–5510, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lin L, Hron JD, and Peng SL. Regulation of NF-kappaB, Th activation, and autoinflammation by the forkhead transcription factor Foxo3a. Immunity 21: 203–213, 2004 [DOI] [PubMed] [Google Scholar]
- 64.Liu J, Cao L, Chen J, Song S, Lee IH, Quijano C, Liu H, Keyvanfar K, Chen H, Cao LY, Ahn BH, Kumar NG, Rovira II, Xu XL, van Lohuizen M, Motoyama N, Deng CX, and Finkel T. Bmi1 regulates mitochondrial function and the DNA damage response pathway. Nature 459: 387–392, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu Y, Elf SE, Miyata Y, Sashida G, Huang G, Di Giandomenico S, Lee JM, Deblasio A, Menendez S, Antipin J, Reva B, Koff A, and Nimer SD. p53 regulates hematopoietic stem cell quiescence. Cell Stem Cell 4: 37–48, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Marinkovic D, Zhang X, Yalcin S, Luciano JP, Brugnara C, Huber T, and Ghaffari S. Foxo3 is required for the regulation of oxidative stress in erythropoiesis. J Clin Invest 117: 2133–2144, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Melov S, Coskun P, Patel M, Tuinstra R, Cottrell B, Jun AS, Zastawny TH, Dizdaroglu M, Goodman SI, Huang TT, Miziorko H, Epstein CJ, and Wallace DC. Mitochondrial disease in superoxide dismutase 2 mutant mice. Proc Natl Acad Sci U S A 96: 846–851, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Meng TC, Buckley DA, Galic S, Tiganis T, and Tonks NK. Regulation of insulin signaling through reversible oxidation of the protein-tyrosine phosphatases TC45 and PTP1B. J Biol Chem 279: 37716–37725, 2004 [DOI] [PubMed] [Google Scholar]
- 69.Meng TC, Fukada T, and Tonks NK. Reversible oxidation and inactivation of protein tyrosine phosphatases in vivo. Mol Cell 9: 387–399, 2002 [DOI] [PubMed] [Google Scholar]
- 70.Miyamoto K, Araki KY, Naka K, Arai F, Takubo K, Yamazaki S, Matsuoka S, Miyamoto T, Ito K, Ohmura M, Chen C, Hosokawa K, Nakauchi H, Nakayama K, Nakayama KI, Harada M, Motoyama N, Suda T, and Hirao A. Foxo3a is essential for maintenance of the hematopoietic stem cell pool. Cell Stem Cell 1: 101–112, 2007 [DOI] [PubMed] [Google Scholar]
- 71.Motta JP, Gomes BE, Bouzas LF, Paraguassu-Braga FH, and Porto LC. Evaluations of bioantioxidants in cryopreservation of umbilical cord blood using natural cryoprotectants and low concentrations of dimethylsulfoxide. Cryobiology 60: 301–307, 2010 [DOI] [PubMed] [Google Scholar]
- 72.Munoz J, Stange DE, Schepers AG, van de Wetering M, Koo BK, Itzkovitz S, Volckmann R, Kung KS, Koster J, Radulescu S, Myant K, Versteeg R, Sansom OJ, van Es JH, Barker N, van Oudenaarden A, Mohammed S, Heck AJ, and Clevers H. The Lgr5 intestinal stem cell signature: robust expression of proposed quiescent ‘;+4’ cell markers. EMBO J 31: 3079–3091, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murata H, Ihara Y, Nakamura H, Yodoi J, Sumikawa K, and Kondo T. Glutaredoxin exerts an antiapoptotic effect by regulating the redox state of Akt. J Biol Chem 278: 50226–50233, 2003 [DOI] [PubMed] [Google Scholar]
- 74.Nagayasu H, Hamada J, Kawano T, Konaka S, Nakata D, Shibata T, Arisue M, Hosokawa M, Takeichi N, and Moriuchi T. Inhibitory effects of malotilate on invasion and metastasis of rat mammary carcinoma cells by modifying the functions of vascular endothelial cells. Br J Cancer 77: 1371–1377, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Naka K, Hoshii T, Muraguchi T, Tadokoro Y, Ooshio T, Kondo Y, Nakao S, Motoyama N, and Hirao A. TGF-beta-FOXO signalling maintains leukaemia-initiating cells in chronic myeloid leukaemia. Nature 463: 676–680, 2010 [DOI] [PubMed] [Google Scholar]
- 76.Nakada D, Saunders TL, and Morrison SJ. Lkb1 regulates cell cycle and energy metabolism in haematopoietic stem cells. Nature 468: 653–658, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Neumann CA, Krause DS, Carman CV, Das S, Dubey DP, Abraham JL, Bronson RT, Fujiwara Y, Orkin SH, and Van Etten RA. Essential role for the peroxiredoxin Prdx1 in erythrocyte antioxidant defence and tumour suppression. Nature 424: 561–565, 2003 [DOI] [PubMed] [Google Scholar]
- 78.Owusu-Ansah E. and Banerjee U. Reactive oxygen species prime Drosophila haematopoietic progenitors for differentiation. Nature 461: 537–541, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Paik JH, Ding Z, Narurkar R, Ramkissoon S, Muller F, Kamoun WS, Chae SS, Zheng H, Ying H, Mahoney J, Hiller D, Jiang S, Protopopov A, Wong WH, Chin L, Ligon KL, and DePinho RA. FoxOs cooperatively regulate diverse pathways governing neural stem cell homeostasis. Cell Stem Cell 5: 540–553, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Paik JH, Kollipara R, Chu G, Ji H, Xiao Y, Ding Z, Miao L, Tothova Z, Horner JW, Carrasco DR, Jiang S, Gilliland DG, Chin L, Wong WH, Castrillon DH, and DePinho RA. FoxOs are lineage-restricted redundant tumor suppressors and regulate endothelial cell homeostasis. Cell 128: 309–323, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Parks D, Bolinger R, and Mann K. Redox state regulates binding of p53 to sequence-specific DNA, but not to non-specific or mismatched DNA. Nucleic Acids Res 25: 1289–1295, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pervaiz S, Taneja R, and Ghaffari S. Oxidative stress regulation of stem and progenitor cells. Antioxid Redox Signal 11: 2777–2789, 2009 [DOI] [PubMed] [Google Scholar]
- 83.Peter Y, Rotman G, Lotem J, Elson A, Shiloh Y, and Groner Y. Elevated Cu/Zn-SOD exacerbates radiation sensitivity and hematopoietic abnormalities of Atm-deficient mice. EMBO J 20: 1538–1546, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Piccoli C, D'Aprile A, Ripoli M, Scrima R, Lecce L, Boffoli D, Tabilio A, and Capitanio N. Bone- marrow derived hematopoietic stem/progenitor cells express multiple isoforms of NADPH oxidase and produce constitutively reactive oxygen species. Biochem Biophys Res Commun 353: 965–972, 2007 [DOI] [PubMed] [Google Scholar]
- 85.Piccoli C, Ria R, Scrima R, Cela O, D'Aprile A, Boffoli D, Falzetti F, Tabilio A, and Capitanio N. Characterization of mitochondrial and extra-mitochondrial oxygen consuming reactions in human hematopoietic stem cells. Novel evidence of the occurrence of NAD(P)H oxidase activity. J Biol Chem 280: 26467–26476, 2005 [DOI] [PubMed] [Google Scholar]
- 86.Polyak K, Xia Y, Zweier JL, Kinzler KW, and Vogelstein B. A model for p53-induced apoptosis. Nature 389: 300–305, 1997 [DOI] [PubMed] [Google Scholar]
- 87.Powell AE, Wang Y, Li Y, Poulin EJ, Means AL, Washington MK, Higginbotham JN, Juchheim A, Prasad N, Levy SE, Guo Y, Shyr Y, Aronow BJ, Haigis KM, Franklin JL, and Coffey RJ. The pan-ErbB negative regulator Lrig1 is an intestinal stem cell marker that functions as a tumor suppressor. Cell 149: 146–158, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Price NL, Gomes AP, Ling AJ, Duarte FV, Martin-Montalvo A, North BJ, Agarwal B, Ye L, Ramadori G, Teodoro JS, Hubbard BP, Varela AT, Davis JG, Varamini B, Hafner A, Moaddel R, Rolo AP, Coppari R, Palmeira CM, de Cabo R, Baur JA, and Sinclair DA. SIRT1 is required for AMPK activation and the beneficial effects of resveratrol on mitochondrial function. Cell Metab 15: 675–690, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Raimundo N, Song L, Shutt TE, McKay SE, Cotney J, Guan MX, Gilliland TC, Hohuan D, Santos- Sacchi J, and Shadel GS. Mitochondrial stress engages E2F1 apoptotic signaling to cause deafness. Cell 148: 716–726, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Renault VM, Rafalski VA, Morgan AA, Salih DA, Brett JO, Webb AE, Villeda SA, Thekkat PU, Guillerey C, Denko NC, Palmer TD, Butte AJ, and Brunet A. FoxO3 regulates neural stem cell homeostasis. Cell Stem Cell 5: 527–539, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Reya T, Morrison SJ, Clarke MF, and Weissman IL. Stem cells, cancer, and cancer stem cells. Nature 414: 105–111, 2001 [DOI] [PubMed] [Google Scholar]
- 92.Rhee SG, Yang KS, Kang SW, Woo HA, and Chang TS. Controlled elimination of intracellular H(2)O(2): regulation of peroxiredoxin, catalase, and glutathione peroxidase via post-translational modification. Antioxid Redox Signal 7: 619–626, 2005 [DOI] [PubMed] [Google Scholar]
- 93.Rossi DJ, Bryder D, and Weissman IL. Hematopoietic stem cell aging: mechanism and consequence. Exp Gerontol 42: 385–390, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sahin E. and Depinho RA. Linking functional decline of telomeres, mitochondria and stem cells during ageing. Nature 464: 520–528, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sarbassov DD. and Sabatini DM. Redox regulation of the nutrient-sensitive raptor-mTOR pathway and complex. J Biol Chem 280: 39505–39509, 2005 [DOI] [PubMed] [Google Scholar]
- 96.Sart S, Ma T, and Li Y. Cryopreservation of pluripotent stem cell aggregates in defined protein-free formulation. Biotechnol Prog 29: 143–153, 2013 [DOI] [PubMed] [Google Scholar]
- 97.Sato T, Vries RG, Snippert HJ, van de Wetering M, Barker N, Stange DE, van Es JH, Abo A, Kujala P, Peters PJ, and Clevers H. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 459: 262–265, 2009 [DOI] [PubMed] [Google Scholar]
- 98.Sattler M, Winkler T, Verma S, Byrne CH, Shrikhande G, Salgia R, and Griffin JD. Hematopoietic growth factors signal through the formation of reactive oxygen species. Blood 93: 2928–2935, 1999 [PubMed] [Google Scholar]
- 99.Savitsky PA. and Finkel T. Redox regulation of Cdc25C. J Biol Chem 277: 20535–20540, 2002 [DOI] [PubMed] [Google Scholar]
- 100.Schofield CJ. and Ratcliffe PJ. Oxygen sensing by HIF hydroxylases. Nat Rev Mol Cell Biol 5: 343–354, 2004 [DOI] [PubMed] [Google Scholar]
- 101.Seo JH, Ahn Y, Lee SR, Yeol Yeo C, and Chung Hur K. The major target of the endogenously generated reactive oxygen species in response to insulin stimulation is phosphatase and tensin homolog and not phosphoinositide-3 kinase (PI-3 kinase) in the PI-3 kinase/Akt pathway. Mol Biol Cell 16: 348–357, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Shaw M, Cohen P, and Alessi DR. The activation of protein kinase B by H2O2 or heat shock is mediated by phosphoinositide 3-kinase and not by mitogen-activated protein kinase-activated protein kinase-2. Biochem J 336 (Pt 1): 241–246, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Signer RA. and Morrison SJ. Mechanisms that regulate stem cell aging and life span. Cell Stem Cell 12: 152–165, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Simon MP, Tournaire R, and Pouyssegur J. The angiopoietin-2 gene of endothelial cells is up-regulated in hypoxia by a HIF binding site located in its first intron and by the central factors GATA-2 and Ets-1. J Cell Physiol 217: 809–818, 2008 [DOI] [PubMed] [Google Scholar]
- 105.Slack C, Werz C, Wieser D, Alic N, Foley A, Stocker H, Withers DJ, Thornton JM, Hafen E, and Partridge L. Regulation of lifespan, metabolism, and stress responses by the Drosophila SH2B protein, Lnk. PLoS Genet 6: e1000881, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sundaresan M, Yu ZX, Ferrans VJ, Irani K, and Finkel T. Requirement for generation of H2O2 for platelet-derived growth factor signal transduction. Science 270: 296–299, 1995 [DOI] [PubMed] [Google Scholar]
- 107.Sykes SM, Lane SW, Bullinger L, Kalaitzidis D, Yusuf R, Saez B, Ferraro F, Mercier F, Singh H, Brumme KM, Acharya SS, Scholl C, Tothova Z, Attar EC, Frohling S, Depinho RA, Armstrong SA, Gilliland DG, and Scadden DT. AKT/FOXO signaling enforces reversible differentiation blockade in myeloid leukemias. Cell 146: 697–708, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Takaki S, Morita H, Tezuka Y, and Takatsu K. Enhanced hematopoiesis by hematopoietic progenitor cells lacking intracellular adaptor protein, Lnk. J Exp Med 195: 151–160, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Takubo K, Goda N, Yamada W, Iriuchishima H, Ikeda E, Kubota Y, Shima H, Johnson RS, Hirao A, Suematsu M, and Suda T. Regulation of the HIF-1alpha level is essential for hematopoietic stem cells. Cell Stem Cell 7: 391–402, 2010 [DOI] [PubMed] [Google Scholar]
- 110.Takubo K, Nagamatsu G, Kobayashi CI, Nakamura-Ishizu A, Kobayashi H, Ikeda E, Goda N, Rahimi Y, Johnson RS, Soga T, Hirao A, Suematsu M, and Suda T. Regulation of glycolysis by pdk functions as a metabolic checkpoint for cell cycle quiescence in hematopoietic stem cells. Cell Stem Cell 12: 49–61, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tanaka H, Matsumura I, Ezoe S, Satoh Y, Sakamaki T, Albanese C, Machii T, Pestell RG, and Kanakura Y. E2F1 and c-Myc potentiate apoptosis through inhibition of NF-kappaB activity that facilitates MnSOD-mediated ROS elimination. Mol Cell 9: 1017–1029, 2002 [DOI] [PubMed] [Google Scholar]
- 112.TeKippe M, Harrison DE, and Chen J. Expansion of hematopoietic stem cell phenotype and activity in Trp53-null mice. Exp Hematol 31: 521–527, 2003 [DOI] [PubMed] [Google Scholar]
- 113.Thannickal VJ. and Fanburg BL. Reactive oxygen species in cell signaling. Am J Physiol Lung Cell Mol Physiol 279: L1005–1028, 2000 [DOI] [PubMed] [Google Scholar]
- 114.Tothova Z, Kollipara R, Huntly BJ, Lee BH, Castrillon DH, Cullen DE, McDowell EP, Lazo- Kallanian S, Williams IR, Sears C, Armstrong SA, Passegue E, DePinho RA, and Gilliland DG. FoxOs are critical mediators of hematopoietic stem cell resistance to physiologic oxidative stress. Cell 128: 325–339, 2007 [DOI] [PubMed] [Google Scholar]
- 115.Tsai JJ, Dudakov JA, Takahashi K, Shieh JH, Velardi E, Holland AM, Singer NV, West ML, Smith OM, Young LF, Shono Y, Ghosh A, Hanash AM, Tran HT, Moore MA, and van den Brink MR. Nrf2 regulates haematopoietic stem cell function. Nat Cell Biol 15: 309–316, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tsai WB, Chung YM, Takahashi Y, Xu Z, and Hu MC. Functional interaction between FOXO3a and ATM regulates DNA damage response. Nat Cell Biol 10: 460–467, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Vafa O, Wade M, Kern S, Beeche M, Pandita TK, Hampton GM, and Wahl GM. c-Myc can induce DNA damage, increase reactive oxygen species, and mitigate p53 function: a mechanism for oncogene-induced genetic instability. Mol Cell 9: 1031–1044, 2002 [DOI] [PubMed] [Google Scholar]
- 118.Velazquez L, Cheng AM, Fleming HE, Furlonger C, Vesely S, Bernstein A, Paige CJ, and Pawson T. Cytokine signaling and hematopoietic homeostasis are disrupted in Lnk-deficient mice. J Exp Med 195: 1599–1611, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Velu CS, Niture SK, Doneanu CE, Pattabiraman N, and Srivenugopal KS. Human p53 is inhibited by glutathionylation of cysteines present in the proximal DNA-binding domain during oxidative stress. Biochemistry 46: 7765–7780, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Willcox BJ, Donlon TA, He Q, Chen R, Grove JS, Yano K, Masaki KH, Willcox DC, Rodriguez B, and Curb JD. FOXO3A genotype is strongly associated with human longevity. Proc Natl Acad Sci U S A 105: 13987–13992, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Willcox BJ, He Q, Chen R, Yano K, Masaki KH, Grove JS, Donlon TA, Willcox DC, and Curb JD. Midlife risk factors and healthy survival in men. JAMA 296: 2343–2350, 2006 [DOI] [PubMed] [Google Scholar]
- 122.Woo HA, Yim SH, Shin DH, Kang D, Yu DY, and Rhee SG. Inactivation of peroxiredoxin I by phosphorylation allows localized H(2)O(2) accumulation for cell signaling. Cell 140: 517–528, 2010 [DOI] [PubMed] [Google Scholar]
- 123.Xu X, Cowley S, Flaim CJ, James W, Seymour L, and Cui Z. The roles of apoptotic pathways in the low recovery rate after cryopreservation of dissociated human embryonic stem cells. Biotechnol Progr 26: 827–837, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yahata T, Takanashi T, Muguruma Y, Ibrahim AA, Matsuzawa H, Uno T, Sheng Y, Onizuka M, Ito M, Kato S, and Ando K. Accumulation of oxidative DNA damage restricts the self-renewal capacity of human hematopoietic stem cells. Blood 118: 2941–2950, 2011 [DOI] [PubMed] [Google Scholar]
- 125.Yakovlev VA, Bayden AS, Graves PR, Kellogg GE, and Mikkelsen RB. Nitration of the tumor suppressor protein p53 at tyrosine 327 promotes p53 oligomerization and activation. Biochemistry 49: 5331–5339, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Yalcin S, Marinkovic D, Mungamuri SK, Zhang X, Tong W, Sellers R, and Ghaffari S. ROS- mediated amplification of AKT/mTOR signalling pathway leads to myeloproliferative syndrome in Foxo3(−/−) mice. EMBO J 29: 4118–4131, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yalcin S, Zhang X, Luciano JP, Mungamuri SK, Marinkovic D, Vercherat C, Sarkar A, Grisotto M, Taneja R, and Ghaffari S. Foxo3 is essential for the regulation of ataxia telangiectasia mutated and oxidative stress-mediated homeostasis of hematopoietic stem cells. J Biol Chem 283: 25692–25705, 2008 [DOI] [PubMed] [Google Scholar]
- 128.Yoshida S, Hong S, Suzuki T, Nada S, Mannan AM, Wang J, Okada M, Guan KL, and Inoki K. Redox regulates mammalian target of rapamycin complex 1 (mTORC1) activity by modulating the TSC1/TSC2- Rheb GTPase pathway. J Biol Chem 286: 32651–32660, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yu WM, Liu X, Shen J, Jovanovic O, Pohl EE, Gerson SL, Finkel T, Broxmeyer HE, and Qu CK. Metabolic regulation by the mitochondrial phosphatase PTPMT1 is required for hematopoietic stem cell differentiation. Cell Stem Cell 12: 62–74, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yuan Y, Hilliard G, Ferguson T, and Millhorn DE. Cobalt inhibits the interaction between hypoxia- inducible factor-alpha and von Hippel-Lindau protein by direct binding to hypoxia-inducible factor-alpha. J Biol Chem 278: 15911–15916, 2003 [DOI] [PubMed] [Google Scholar]
- 131.Zee RS, Yoo CB, Pimentel DR, Perlman DH, Burgoyne JR, Hou X, McComb ME, Costello CE, Cohen RA, and Bachschmid MM. Redox regulation of sirtuin-1 by S-glutathiolation. Antioxid Redox Signal 13: 1023–1032, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zeng Z, Sarbassov dos D, Samudio IJ, Yee KW, Munsell MF, Ellen Jackson C, Giles FJ, Sabatini DM, Andreeff M, and Konopleva M. Rapamycin derivatives reduce mTORC2 signaling and inhibit AKT activation in AML. Blood 109: 3509–3512, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhang X, Yalcin S, Lee DF, Yeh TY, Lee SM, Su J, Mungamuri SK, Rimmele P, Kennedy M, Sellers R, Landthaler M, Tuschl T, Chi NW, Lemischka I, Keller G, and Ghaffari S. FOXO1 is an essential regulator of pluripotency in human embryonic stem cells. Nat Cell Biol 13: 1092–1099, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhu QS, Xia L, Mills GB, Lowell CA, Touw IP, and Corey SJ. G-CSF induced reactive oxygen species involves Lyn-PI3-kinase-Akt and contributes to myeloid cell growth. Blood 107: 1847–1856, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]