Immune thrombocytopenia (ITP) is a common bleeding disorder characterized by autoantibody-mediated platelet destruction. Antibodies predominantly target platelet glycoproteins GPIIb/IIIa (70–80%) and GPIb/IX (20–40%), with some patients having both. In animal models, anti-GPIb/IX but not anti-GPIIb/IIIa antibodies are associated with Fc-independent platelet clearance and resistance to intravenous immunoglobulin G (IVIG) therapy.1,2 In humans, anti-GPIb/IX-mediated ITP is associated with inferior responses to both IVIG and corticosteroids.3–5 The mechanism behind anti-GPIb/IX-mediated Fc-independent platelet clearance has not been adequately addressed.6,7 We recently found in murine models of ITP that anti-GPIb/IX antibodies trigger platelet activation and neuraminidase translocation to the cell membrane, causing platelet desialylation (removal of sialic acid residues) and Fc-independent hepatic platelet clearance (Li J et al., submitted manuscript).8 Here we report the first clinical evidence of antibody-mediated platelet desialylation utilizing ITP sera from a fatal case. In addition, we show antibody specificity was exclusively targeting GPIb/IX and not GPIIb/IIIa. Our findings introduce an Fc-independent mechanism of platelet destruction that may explain the differences in response to therapy between anti-GPIb/IX and anti-GPIIb/IIIa-mediated ITP.
The patient was a 63-year old male with a 7-year history of Evan’s syndrome with severe thrombocytopenia, mucocutaneous bleeding, and gastrointestinal hemorrhage. He had presented seven years previously with autoimmune hemolytic anemia (AIHA). He was treated with corticosteroids, intravenous immunoglobulin (IVIG), and red cell transfusions and experienced a complete response with no further recurrences of AIHA. He presented with ITP five years before the current admission with a platelet count of 16×109/L but no bleeding manifestations. He was treated with corticosteroids with complete response. He experienced 3 additional episodes of thrombocytopenia four, two, and one year before the current admission (platelet count nadirs were 35×109/L, 13×109/L, and 1×109/L, respectively), each treated with corticosteroids as an outpatient with normal platelet counts between relapses. Relapses were not associated with hemorrhagic symptoms other than petechiae.
Seven days before the current admission, the patient developed petechiae. Platelet count was 58×109/L (hemoglobin 134 g/L with no evidence of hemolysis). The following day he noted oral purpura and his platelet count fell to 4×109/L. He was started on oral dexamethasone 40 mg daily for four days as an outpatient. Platelet counts three and five days later were unchanged. On Day 5, due to new onset of melena, he was admitted to hospital (platelet count 2×109/L). Over Days 5 to 7 he was administered intravenous steroids, intravenous immunoglobulin (IVIG), tranexamic acid, 5 units of red blood cells, and 4 platelet pools with continued gastrointestinal hemorrhage. No increments in platelet count were seen post platelet transfusion. On Day 7, he developed progressive shortness of breath, hemoptysis, and patchy airspace disease (Online Supplementary Figure S1). Despite intravenous and endotracheal tranexamic acid and recombinant factor VIIa, he had progressive respiratory failure due to pulmonary hemorrhage and died. Sera was obtained from the patient prior to death and laboratory testing with monoclonal antibody-specific immobilization of platelet antigen (MAIPA) revealed a strikingly high level of anti-GPIb/IX antibodies, with no detectable anti-GPIIb/IIIa antibodies (Figure 1A). To evaluate whether the anti-GPIb/IX antibodies had an effect on the hemostatic function of platelets, we incubated the patient’s sera with normal human platelets and stimulated aggregation in vitro using ristocetin (an agonist specifically inducing GPIb-VWF interaction). The patient’s anti-GPIb/IX antibodies were found to interfere with normal platelet function as shown by inhibition of GPIb-VWF-mediated platelet aggregation (Figure 1B). Aggregation may have been impaired due to competitive inhibition of the GPIb receptor by the anti-GPIb antibodies, which likely further enhanced the severity of the patient’s hemorrhage.
Figure 1.
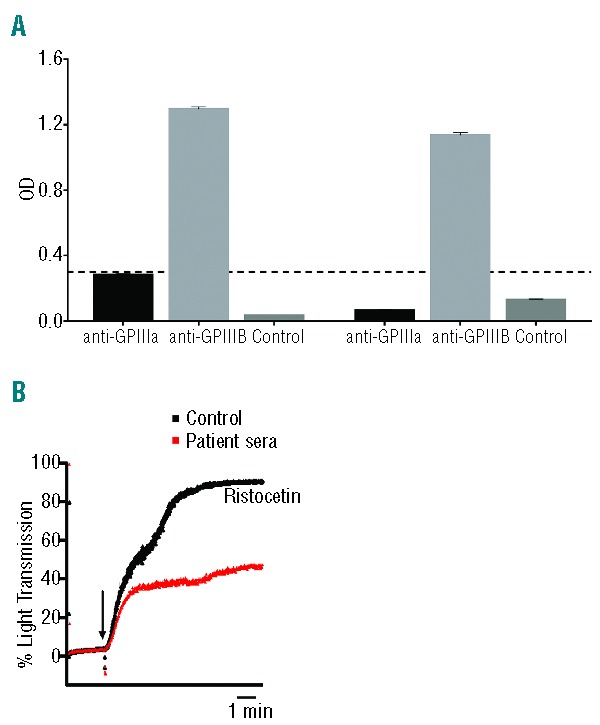
(A) GPIb/IX specificity as detected by MAIPA in two independent assays (OD: optical density). No anti-β3 (i.e. anti-GPIIIa) antibodies were detected (black bars, below the dotted black line). Only anti-GPIb antibodies were detected (light gray bars, above dotted black line). Control was normal human sera. (B) Ristocetin-induced (i.e. GPIb-VWF-mediated) platelet aggregation was inhibited by patient sera (5× dilution). Control was normal human sera.
The most interesting finding was that incubation of the patient’s sera with normal human platelets resulted in platelet activation and marked platelet desialylation (Figure 2A and B). Platelet activation was detected by P-selectin staining.9,10 Desialylation was detected by flow cytometry with fluorescein-conjugated Ricinus Communis Agglutinin I (RCA-1), which binds to underlying galactose residues. Neuraminidase-1 (NEU1) is a mammalian sialidase with narrow substrate specificity with preference for glycoproteins. NEU1 can be found in abundance in platelet granules and can be clearly observed via immunofluorescence of permeabilized platelets (Online Supplementary Figure S2). Platelet NEU1 has been shown to translocate to the platelet surface to mediate platelet desialylation during cold storage. We found that incubation of normal human non-permeabilized platelets with this patient’s sera induced surface expression of NEU1 (Figure 2C), which likely mediated the observed desialylation. We, therefore, propose that the antibody specificity and severe desialylation observed affected not only platelet number, but also platelet function and response to treatment, resulting in fatal refractory hemorrhage. A change in antibody specificity may explain why previous relapses occurred without hemorrhage in this patient. Physicians should be aware that even within the same individual, each ITP relapse may differ in bleeding severity and response to treatment, possibly due to changes in antibody specificity. Thus, we strongly recommend that screening for antibody specificity become standard practice for ITP at the first presentation and at every relapse.
Figure 2.
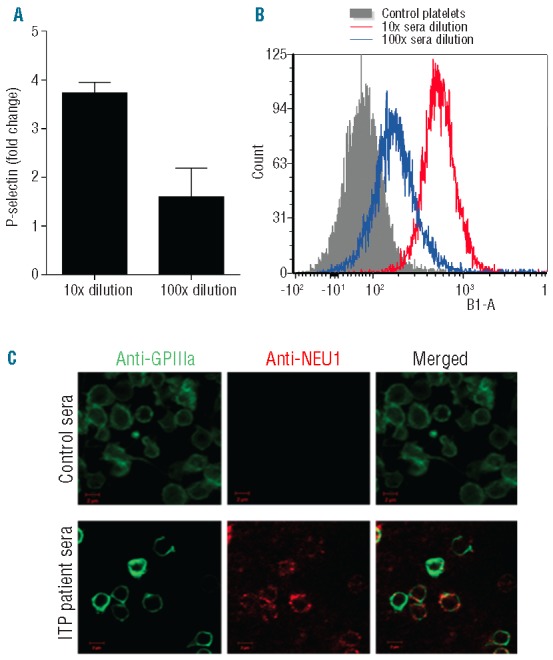
(A) P-selectin expression after incubation with patient sera in serial dilutions, expressed as fold change from control sera. (B) Platelet desialylation after incubation with patient sera in serial dilutions. B1-A represents desialylation as measured by flow cytometry detection of fluorescein-conjugated Ricinus Communis Agglutinin I (RCA-1) bound to exposed desialylated galactose residues. (C) Neurominidase (NEU1, red) translocation to the platelet surface (GPIIIa, green) after incubation with patient sera. Platelets were non-permeabilized. Scale bar represents 2 μm.
Our proposal is supported by our very recent discovery in animal models of ITP. Previously, we and others have found that anti-GPIbα antibodies cause platelet activation and apoptosis.12,13 We further found in a murine model of anti-GPIb/IX-mediated ITP that anti-GPIb/IX antibodies trigger platelet activation and degranulation, which likely was accompanied by neuraminidase translocation to the cell membrane, causing platelet desialylation.8 Through engagement with Ashwell Morell receptors on hepatocytes, in vivo evidence suggested that these desialylated platelets may be cleared by the liver in addition to the spleen.8 Importantly, this Fc-independent thrombocytopenia was successfully treated with sialidase inhibition in animal models of anti-GPIb/IX-mediated ITP.8 Notably, a previous case report described an ITP patient who was treated with a neuraminidase inhibitor (TamifluTM) for H1N1 influenza and had a complete resolution of her thrombocytopenia after five days. Therefore, it is likely that the severe platelet desialylation observed in our case contributed to the pathogenesis of ITP. This study establishes the clinical relevance of the desialylation pathway and presents its potential as an important biomarker and therapeutic target for refractory ITP.
Acknowledgments
The authors would also like to thank Alexandra H. Marshall for editorial assistance and intellectual input.
Footnotes
Funding: this study was funded by the Canadian Institutes of Health Research (MOP #97918).
The online version of this article has a Supplementary Appendix.
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Nieswandt B, Bergmeier W, Rackebrandt K, Gessner JE, Zirngibl H. Identification of critical antigen-specific mechanisms in the development of immune thrombocytopenic purpura in mice. Blood. 2000;96(7):2520–7 [PubMed] [Google Scholar]
- 2.Webster ML, Sayeh E, Crow M, Chen P, Nieswandt B, Freedman J, et al. Relative efficacy of intravenous immunoglobulin G in ameliorating thrombocytopenia induced by antiplatelet GPIIbIIIa versus GPIbalpha antibodies. Blood. 2006;108(3):943–6 [DOI] [PubMed] [Google Scholar]
- 3.Zeng Q, Zhu L, Tao L, Bao J, Yang M, Simpson EK, et al. Relative efficacy of steroid therapy in immune thrombocytopenia mediated by anti-platelet GPIIbIIIa versus GPIbalpha antibodies. Am J Hematol. 2012;87(2):206–8 [DOI] [PubMed] [Google Scholar]
- 4.Go RS, Johnston KL, Bruden KC. The association between platelet autoantibody specificity and response to intravenous immunoglobulin G in the treatment of patients with immune thrombocytopenia. Haematologica. 2007;92(2):283–4 [DOI] [PubMed] [Google Scholar]
- 5.Peng J, Ma S-H, Liu J, Hou Y, Liu X-M, Niu T, et al. Association of autoantibody specificity and response to intravenous immunoglobulin G therapy in immune thrombocytopenia: a multicentre cohort study. J Throm Haem. 2014;[epub ahead of print] 10.1111/jth.12524 [DOI] [PubMed] [Google Scholar]
- 6.Li J, van der Wal DE, Zhu L, Vadasz B, Simpson EK, Li C, et al. Fc-independent phagocytosis: implications for IVIG and other therapies in immune-mediated thrombocytopenia. Cardiovasc Hematol Disord Drug Targets. 2013;13(1):50–8 [DOI] [PubMed] [Google Scholar]
- 7.Li C, Li J, Li Y, Lang S, Yougbare I, Zhu G, et al. Crosstalk between Platelets and the Immune System: Old Systems with New Discoveries. Adv Hematol. 2012;2012:384685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Der Wal DE, Zhu G, Li J, Vadasz B, Yougbare I, Lang S, et al. Desialylation: A Novel Platelet Clearance Mechanism and a Potential New Therapeutic Target in Anti-GPIb Antibody Mediated Thrombocytopenia. 54th ASH Annual Meeting and Exposition, 2012:Abstract 265 [Google Scholar]
- 9.Yang H, Lang S, Zhai Z, Li L, Kahr WH, Chen P, et al. Fibrinogen is required for maintenance of platelet intracellular and cell-surface P-selectin expression. Blood. 2009;114(2):425–36 [DOI] [PubMed] [Google Scholar]
- 10.Yang Y, Shi Z, Reheman A, Jin JW, Li C, Wang Y, et al. Plant food delphinidin-3-glucoside significantly inhibits platelet activation and thrombosis: novel protective roles against cardiovascular diseases. PloS One. 2012;7(5):e37323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jansen AJ, Josefsson EC, Rumjantseva V, Liu QP, Falet H, Bergmeier W, et al. Desialylation accelerates platelet clearance after refrigeration and initiates GPIbalpha metalloproteinase-mediated cleavage in mice. Blood. 2012;119(5):1263–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Urbanus RT, van der Wal DE, Koekman CA, Huisman A, van den Heuvel DJ, Gerritsen HC, et al. Patient autoantibodies induce platelet destruction signals via raft-associated glycoprotein Ibalpha and Fc RIIa in immune thrombocytopenia. Haematologica. 2013;98(7):e70–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li C, Piran S, Chen P, Lang S, Zarpellon A, Jin JW, et al. The maternal immune response to fetal platelet GPIbalpha causes frequent miscarriage in mice that can be prevented by intravenous IgG and anti-FcRn therapies. J Clin Invest. 2011;121(11):4537–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alioglu B, Tasar A, Ozen C, Selver B, Dallar Y. An experience of oseltamivir phosphate (tamiflu) in a pediatric patient with chronic idiopathic thrombocytopenic purpura: a case report. Pathophysiol Haemost Thromb. 2010;37(2–4):55–8 [DOI] [PubMed] [Google Scholar]


