Abstract
Exploring the relationships among PTSD, alcohol misuse, and women's use of intimate partner violence (IPV) is vital to develop our understanding of the etiologies of women's use of IPV, which can serve to maximize intervention efforts for women. This study examined the extent to which posttraumatic stress disorder (PTSD) symptom clusters are directly and indirectly related to women's use of IPV through pathways involving alcohol misuse while controlling for severity of women's IPV victimization. The sample was comprised of substance using, low socioeconomic status community women (n = 143) currently experiencing IPV victimization. The majority of the sample was African American (n = 115, 80.42%). This sample had a mean annual household income of $14,368.68 (SD = $12,800.68) and the equivalent of a high school education (11.94 years, SD = 1.32). Path analyses indicated that the strongest statistical relationship emerged between women's use of IPV and women's IPV victimization. PTSD re-experiencing and numbing symptom severity were related to women's use of psychological, minor physical, and severe physical IPV, however these relationships were indirect through alcohol misuse. Findings lend preliminary support for the application of the self-medication hypothesis to the study of PTSD, alcohol misuse, and IPV among women.
Keywords: Traumatic stress, alcohol use, physical abuse, psychological abuse, women's aggression
Despite substantial literature indicating that women's use of intimate partner violence (IPV) is highly prevalent and has deleterious health effects for both men and women, research examining its precursors and correlates is scant (Hines & Douglas, 2010; Swan, Gambone, Caldwell, Sullivan, & Snow, 2008). However, literature examining the precursors and correlates of men's use of IPV is abundant and consistent: Posttraumatic stress disorder (PTSD) and alcohol misuse are strongly associated with men's use of IPV (Bell & Orcutt, 2009; Foran & O'Leary, 2008). The extent to which PTSD and alcohol misuse are associated with women's use of IPV is understudied; addressing this question is imperative to inform community interventions and mental health treatment planning for women (Babcock, Roseman, Green, & Ross, 2008; Johnson, Zlotnick, & Perez, 2011). Therefore, the present study examined whether the severity of PTSD symptom clusters and alcohol misuse are related to the use of psychological and physical IPV among women who experienced IPV victimization in their current relationships.
Few studies have examined the link between women's PTSD and use of IPV. Those studies found that women's PTSD symptom severity was indirectly related to their use of IPV through anger and poor relationship adjustment (Swan, Gambone, Fields, Sullivan, & Snow, 2005; Taft, Monson, Hebenstreit, King, & King, 2009a).These findings also indicate that women's IPV victimization is strongly related to their use of IPV. However, these studies’ clinical implications are limited because PTSD and IPV were examined as single constructs: PTSD as a total severity score or diagnosis and IPV as a total score rather than as the severity of specific types (e.g., psychological and physical). Researchers have emphasized the importance of applying a more nuanced framework to research on PTSD to remain consistent with the Diagnostic and Statistical Manual of Mental Disorders-V. This study addresses these limitations by applying an empirically supported four-factor structure of PTSD representing re-experiencing, avoidance, numbing, and hyperarousal symptoms (King, Leskin, King, & Weathers, 1998; Yufik & Simms, 2010) and by examining three distinct types of IPV: psychological, minor physical, and severe physical.
Differential relationships between PTSD symptom clusters and the use of aggressive behavior (including but not limited to IPV) have been documented among men from community, Veteran, and treatment seeking samples. Consistently, the PTSD hyperarousal symptom cluster is most strongly, and directly, related to men's use of aggression (Hellmuth, Stappenbeck, Hoerster, & Jakupcak, 2012; Taft, Vogt, Marshall, Panuzio, & Niles, 2007b); In one Taft and colleagues (2007a) study, PTSD hyperarousal symptoms also were indirectly related to IPV through alcohol problems among male Veterans. Re-experiencing, avoidance, and numbing symptoms have been directly and indirectly related to men's use of aggression through alcohol misuse (Taft et al., 2007a; Taft et al., 2009b).
The influence of PTSD on alcohol misuse among both genders has often been explained by the tension reduction hypothesis (Conger, 1956) which suggests a bidirectional causal relationship between alcohol misuse and stress. A primary motivating factor for alcohol misuse across populations is the desire to manage stress and negative emotion (see Sher & Grekin, 2007, for review). When applied to women who experience IPV victimization and PTSD symptoms, drive reduction theory together with the self-medication hypothesis suggest that women may (mis)use alcohol to cope with the distress associated with their IPV victimization and PTSD symptoms (Sullivan & Holt, 2008; Todd, Armeli, & Tennen, 2009).
Two theoretical frameworks explain why alcohol misuse and use of IPV are strongly related. First, alcohol myopia theory suggests that alcohol misuse leads to perceptual bias in social cognition, such that a person experiences heightened sensitivity to perceived threat (Clements & Schumacher, 2010; Steele & Josephs, 1990). Second, proximal effects theories suggest that alcohol misuse leads to a person to experience behavioral disinhibition (Foran & O'Leary, 2008). In turn, heightened sensitivity and behavioral disinhibition are theorized to precipitate the use of IPV (Clements & Schumacher, 2010; Foran & O'Leary, 2008). However, findings of recent research suggest that alcohol use plays less of a role in women's use of IPV than in men's (Foran & O'Leary, 2008; Testa et al., 2012). This may be due to the functional use of IPV among women as a means of self defense against IPV victimization (Caldwell, Swan, Allen, Sullivan, & Snow, 2009; Swan et al., 2008). These motivations to use IPV may lessen the likelihood that alcohol misuse will explain the link between some PTSD symptoms and use of IPV among women. Despite the fact that IPV victimization, PTSD symptoms, and alcohol misuse frequently co-occur among women (Sullivan, Cavanaugh, Buckner, & Edmondson, 2009), no studies have examined the roles that PTSD and alcohol misuse might play in women's use of IPV. Advancing our knowledge in this area may help mental health treatment providers develop and implement more safe and effective clinical interventions for women (Feeny, Zoellner, Mavissakalian, & Roy-Byrne, 2009; Fontana, Rosenheck, & Desai, 2010).
Using a sample of women who experienced IPV victimization in their current relationships, we examined the extent to which the severity of women's PTSD symptom clusters was directly related to their use of psychological and physical IPV and indirectly related through alcohol misuse. Given the strong association of women's IPV victimization to their use of IPV (Swan et al., 2005; Taft et al., 2009b), our analyses controlled for the severity of women's psychological and physical IPV victimization. Based on the aforementioned literature, we hypothesized that: 1) the severity of hyperarousal symptoms would be directly related to women's use of IPV, and 2) the severity of re-experiencing, avoidance, and numbing symptoms would be directly related to women's use of IPV and indirectly related through alcohol misuse.
Method
Procedures
All study procedures were approved by the Institutional Review Board of the primary investigator's institution. Recruitment flyers advertising the Women's Relationship Study were posted in grocery stores, government agencies, nail salons, and two primary care clinics in an urban New England community. The current study was conducted using data from the baseline assessment portion of a larger study, which focused on micro-longitudinal data collection (i.e., daily data collection for 90 days). In this larger study, daily data were not collected on PTSD. To be eligible, a woman must have experienced at least one act of physical victimization by her current male intimate partner in the past 30 days, as measured via phone screen using selected items from the Conflict Tactics Scale-2 (CTS-2; Straus, Hamby, & Warren, 2003). Additional eligibility criteria included: (a) age 18 years or older, (b) current involvement in a heterosexual intimate relationship of at least six months with contact at least twice per week, and (c) use of drugs or alcohol at least one time in the 30 days prior to study entry. Exclusion criteria included inpatient psychiatric hospitalization during the previous year and current residence in a shelter or group home. Of the 1,120 women who were screened, 198 met inclusion criteria. The final sample consisted of the 143 women who met eligibility criteria, attended the scheduled interview, and agreed to participate.
Participants completed a semi-structured, computer-assisted interview administered face-to-face by trained master or doctoral-level female research associates. Only female research associates conducted interviews in an effort to maximize participants’ comfort and minimize potential distress associated with disclosing sensitive information, and thus, to follow the ethical guidelines of our profession. During the informed consent procedure, interviewers asked each participant if her participation would put her at risk. No participant reported safety concerns. At the conclusion of the interview, participants were debriefed, compensated $45, and provided with a list of community resources. Interviewers provided assistance with access to resources as needed.
Participants
On average, participants were 38.09 years old (SD = 10.65). The majority of the sample was African American (n = 115, 80.42%), 9.09% were White, 6.29% were Latina, 2.10% were American Indian or Alaska Native, and 1.40% identified themselves as bi- or multi-racial. The majority of participants were unemployed (n = 104, 27.27%). Most participants had children (n=122, 85.52%) and nearly half had children under 18 leaving with them (45.45%). Participants had a mean annual household income of $14,368.68 (SD = $12,800.68) and the equivalent of a high school education (M = 11.94 years, SD = 1.32). Participants reported average current intimate relationship length of 6.41 years (SD = 5.97) and more than half were married or cohabitating (n = 85; 59.44%). Twelve percent of the sample had utilized at least one service related to their mental health, IPV victimization, or substance use (e.g., AA meetings, outpatient treatment) in the three months preceding study participation.
Measures
Posttraumatic stress symptom severity
PTSD symptom cluster severity for the three month period prior to study entry was measured using the 49-item Posttraumatic Stress Diagnostic Scale (PDS; Foa, 1995) To the extent possible, symptom severity was assessed in relation to current IPV exposure. We separated the avoidance and numbing symptom clusters consistent with symptom structures outlined by studies demonstrating empirical support for this four factor structure (King et al., 1998; Yufik & Simms, 2010). Symptom severity scores were calculated for each of the four PTSD clusters by summing their respective responses; 0 (not at all, or only one time), 1 (once a week or less, or once in a while), 2 (2 to 4 times a week, or half the time), 3 (5 or more times a week, or almost always). A total symptom severity score of 0 indicates no symptoms, 1-10 is mild, 11-20 is moderate, 21-35 is moderate to severe, and 36 and above are severe. Cronbach's α = .82 for the five re-experiencing symptoms, α = .74 for the 5 numbing symptoms, and α = .80 for the five hyperarousal symptoms; The inter-item correlation was .53 for the two avoidance symptoms.
Women's use of IPV against a current partner
Use of psychological and physical IPV was measured over a reference period of three months with the 78-item Revised Conflict Tactics Scale (CTS-2; Straus et al., 2003). Response categories that comprised a range of values were recoded (Straus et al., 2003) [i.e., 3-5 times (recoded to 4), 6-10 times (recoded to 8), 11-20 times (recoded to 15), and more than 20 times (recoded to 25)]. Severity scores were calculated for each of the three subscales by summing the respective responses; Cronbach's α = .82 for the five minor physical IPV items (e.g., pushing, slapping), Cronbach's α = .73 for the seven severe physical IPV items (e.g., kicking, choking, beating up, using a weapon), and Cronbach's α = .81 for the eight psychological IPV items (e.g. shouted or yelled at a partner, called partner fat or ugly).
Women's IPV victimization by a current partner
Physical and psychological IPV victimization was measured with the 78-item CTS-2. The three month assessment period and coding scheme were identical to that of use of IPV described above. Because of the small sample size and to preserve statistical power, women's physical IPV victimization was operationalized as one variable rather than examining minor and severe physical victimization separately. Cronbach's α = .91 for the 12 physical IPV victimization items, and Cronbach's α = .81 for the eight psychological IPV victimization items.
Alcohol Misuse
The Alcohol Use Disorders Identification Test (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993) was used to assess severity of women's alcohol misuse during the past three months. The AUDIT is a 10-item screening measure developed by the World Health Organization to assess alcohol consumption, drinking behavior, adverse reactions, and problems related to alcohol use. Each item is scored from 0-4 (0 = never, 1 = less than monthly, 2 = montly, 3 = weekly, and 4 = daily or almost daily), and total scores range from 0-40 with higher scores indicative of greater alcohol misuse severity. Total scores ≥ 8 typically indicate alcohol problems (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001) however, cut scores ≥ 6 are more accurate for community women (Reinert & Allen, 2007; Selin, 2003). Cronbach's α = .89.
Data analysis
Study variables were assessed for normality. To produce normal distributions, each IPV variable was log10 transformed (Tabachnick & Fidell, 2007). Raw scores are presented in Table 1. Demographic variables including age, education, race, and income were not significantly correlated with outcome variables and thus, were not controlled for in these analyses. Relationships among women's use of IPV, IPV victimization, and alcohol misuse were analyzed using path analytic techniques in AMOS® 19.0 (Arbuckle, 2010; Kline, 2011). Full information maximum likelihood estimation was used to generate standardized parameter estimates (Peters & Enders, 2002). Exogenous variables measuring women's IPV victimization and PTSD symptom severity were correlated and the three variables measuring women's use of IPV were correlated. Model testing and respecification were conducted according to Kenny's (1999) three-step procedure. First, empirically informed direct and indirect paths were chosen to produce a theory-driven initial model consistent with the aforementioned hypotheses. Second, to prevent specification error (e.g., omitting significant and theoretically relevant relationships among existing variables), we tested whether any additional significant (p < .05) paths existed among the variables of our model. No significant paths were found; no paths were added to the initial model. Standard measures including chi-square, normed fit index (NFI), Tucker-Lewis index (TLI), comparative fit index (CFI), and root mean square error of approximation (RMSEA) were used to assess model fit. A non-significant chi-square, values of NFI, TLI, and CFI ≥ .90, and lower RMSEA values (particularly those less than .05), are considered indicators of good model fit (Browne & Cudeck, 1992; Hu, 1999; Lei & Wu, 2007).
Table 1.
Descriptive Statistics and Correlations Among PTSD Symptoms Clusters, Alcohol Misuse, use of IPV, and IPV victimization.
| Observed Range | Mean | Standard Deviation | Correlations | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | |||
| PTSD symptom severity | 0-47 | 15.13 | 10.17 | |||||||||
| PTSD cluster severity | ||||||||||||
| Re-experiencing | 0 – 15 | 3.80 | 3.28 | – | ||||||||
| Avoidance | 0 – 6 | 2.05 | 1.94 | .61** | – | |||||||
| Numbing | 0 – 14 | 3.90 | 3.36 | .55** | .56** | – | ||||||
| Hyperarousal | 0 – 15 | 5.38 | 3.77 | .55** | .43** | .64** | – | |||||
| Alcohol misuse | 1 – 40 | 10.99 | 8.76 | .45** | .36** | .42** | .45** | – | ||||
| Psychological IPV | 1 – 200 | 56.81 | 43.55 | .30** | .22** | .27** | .28** | .32** | – | |||
| Minor Physical IPV | 0 – 125 | 16.39 | 22.56 | .26** | .24** | .31** | .28** | .45** | .56** | – | ||
| Severe Physical IPV | 0 – 105 | 7.34 | 15.65 | .40** | .26** | .35** | .31** | .43** | .55** | .70** | – | |
| Psychological Victimization | 1 – 200 | 54.97 | 41.55 | .49** | .34** | .39** | .38** | .34** | .74** | .39** | .47** | – |
| Physical Victimization | 1 – 250 | 25.95 | 42.07 | .59** | .39** | .40** | .38** | .37** | .32** | .43** | .60** | .58** |
Note. IPV = intimate partner violence; PTSD = posttraumatic stress disorder. Means and standard deviations calculated using non-transformed values.
Pearson r correlations were calculated using log 10 transformed values.
p < .01.
Bootstrapping procedures in AMOS® were used to estimate the significance of indirect effects. Bootstrapping is a preferred method for estimating and testing hypotheses compared to other methods (e.g., the Sobel test) as it does not rely on the assumption that the indirect effect is normally distributed (Kline, 2011; Preacher & Hayes, 2008). Bootstrapping was done with 2,000 random samples generated from the observed covariance matrix to estimate bias-corrected 95% confidence intervals and significance values for the standardized indirect effects in the final model.
Results
Means and standard deviations for women's PTSD symptom cluster severity, alcohol misuse, use of IPV, and IPV victimization are presented in Table 1. Twenty-seven women (18.9%) met full diagnostic screening criteria for PTSD. Regarding PDS symptom severity scores, seven women (4.9%) reported none, 45 (31.5%) reported mild, 52 (36.4%) reported moderate, 34 (23.8%) reported moderate to severe, and five (3.5%) reported severe PTSD symptoms. Bivariate correlations are presented in Table 2. The strongest correlations were found among the four PTSD symptom clusters, between use of IPV and IPV victimization, and between the PTSD symptom clusters and IPV victimization. In their current relationships, all women used and were victimized by psychological IPV. One hundred twenty-eight (89.5%) and 141 (98.6%) women used and were victimized by minor physical IPV, respectively. Ninety one (63.6%) and 100 (69.9%) women used and were victimized by severe physical IPV, respectively.
Table 2.
Standardized Regression Weights for the Final Model of PTSD Symptom Clusters, Alcohol Misuse, IPV Victimization, and use of IPV.
| Alcohol Misuse | Psychological IPV | Minor Physical IPV | Severe Physical IPV | |
|---|---|---|---|---|
| PTSD Re-experiencing severity | 0.29** | −0.07 | −0.18 | −0.05 |
| PTSD Avoidance severity | 0.05 | – | – | – |
| PTSD Numbing severity | 0.24* | – | – | – |
| PTSD Hyperarousal severity | – | 0.02 | 0.06 | 0.01 |
| Alcohol Misuse | – | 0.12* | 0.34*** | 0.23** |
| Psychological Victimization | – | 0.83*** | 0.18* | 0.15 |
| Physical Victimization | – | −0.18* | 0.29** | 0.47*** |
Note. PTSD = posttraumatic stress disorder. Betas and standard errors were calculated using log 10 transformed values.
– represent paths that were not hypothesized, nor significant in the initial model and thus not examined in the final model.
p < .05.
p < .01.
p < .001.
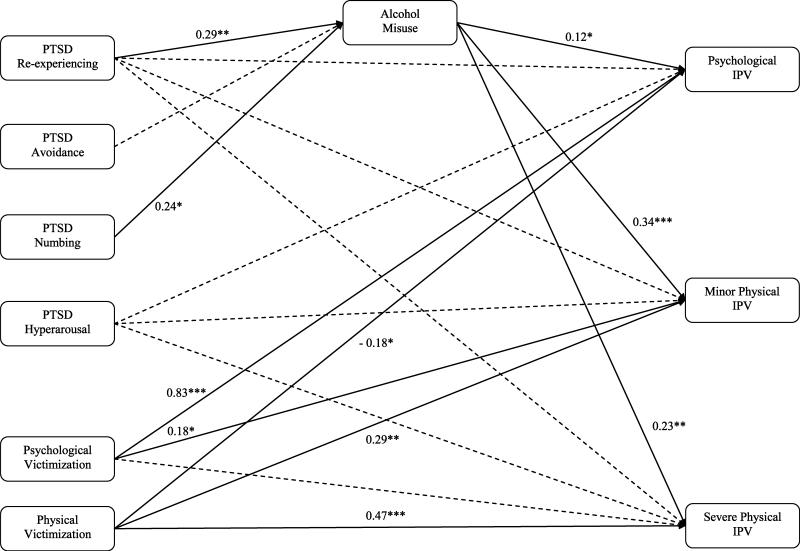
The model (Figure 1) provided excellent fit to the data, χ2 (9) = 11.33, p = .25, χ2 / df = 1.26, NFI = .99, TLI = .98; CFI = 1.00, RMSEA = .04 [CI = .00-.11]. As presented in Table 3, the severity of PTSD symptom clusters was not directly related to women's use of IPV. However, indirect relationships emerged via alcohol misuse. Most relationships that emerged were of moderate strength. Exceptions include a modest relationship between alcohol misuse and use of psychological IPV, and between physical IPV victimization and use of psychological IPV. A stronger relationship emerged between psychological IPV victimization and use of psychological IPV. As presented in Table 4, PTSD re-experiencing and numbing symptom severity were positively related to alcohol misuse which, in turn, was related to greater levels of women's use of psychological, minor physical, and severe physical IPV. PTSD re-experiencing symptom severity had significant indirect effects on the use of psychological IPV (β = .04, p<.05), minor physical IPV (β = .10, p<.05) and severe physical IPV (β = .07, p<.05). PTSD numbing symptom severity had significant indirect effects on the use of minor physical IPV (β = .08, p<.05) and severe physical IPV (β = .05, p<.05). Women's psychological IPV victimization severity was directly related to their use of psychological and minor physical IPV. Women's physical IPV victimization severity was directly related to their use of psychological, minor, and severe physical IPV.
Figure 1. Final model for PTSD cluster, victimization, alcohol misuse and use of aggression.
Note. Only weights for significant paths are reported in the figures using standardized estimates. Dashed lines indicate nonsignificant paths. *p < .05 **p < .01 *** p ≤ .001
Table 3.
Bootstrap Analyses for Indirect Effects of PTSD Symptom Severity to Use of IPV Through Alcohol Misuse
| Bootstrap estimates | ||||
|---|---|---|---|---|
| Predictor | Criterion | Standardized indirect effect | SE for standardized indirect effect | 95% CI for standardized indirect effect (lower, upper) |
| PTSD Re-experiencing severity | Psychological IPV | .04 | .02 | [0.003, 0.105]* |
| Minor Physical IPV | .10 | .04 | [0.026, 0.196]* | |
| Severe Physical IPV | .07 | .04 | [0.012, 0.165]* | |
| PTSD Avoidance severity | Psychological IPV | .01 | .01 | [–0.011, 0.058] |
| Minor Physical IPV | .02 | .03 | [–0.038, 0.095] | |
| Severe Physical IPV | .01 | .02 | [–0.025, 0.080] | |
| PTSD Numbing severity | Psychological IPV | .03 | .03 | [–0.002, 0.106] |
| Minor Physical IPV | .08 | .05 | [0.012, 0.194]* | |
| Severe Physical IPV | .05 | .04 | [0.005, 0.158]* | |
Note. PTSD = Posttraumatic stress disorder; IPV= Intimate partner violence; CI = confidence interval; SE = bias-corrected standard error.
Confidence intervals excluding zero are significant (i.e., p < .05).
Discussion
This investigation was the first to examine relationships among PTSD symptom clusters, alcohol misuse, and use of IPV in a sample of women experiencing IPV in their current relationships. Greater severity of PTSD re-experiencing symptoms was indirectly related to the use of psychological, minor physical, and severe physical IPV through alcohol misuse. Similarly, greater severity of PTSD numbing symptoms was indirectly related to women's use of minor and severe physical IPV through alcohol misuse. Women's use of IPV was most strongly related to the severity of women's IPV victimization, highlighting the central role that women's IPV victimization plays in their use of IPV. Our results illuminate a great need for future research to disentangle these related constructs. Addressing these questions may facilitate more informed and clinically applicable conclusions about the individual and contextual etiologies of women's use of IPV, particularly among women who also experience IPV victimization.
Similar to studies conducted among other populations, our findings highlight the significant role that PTSD re-experiencing and numbing symptoms play in distress and impaired functioning compared to hyperarousal and avoidance. While re-experiencing and avoidance symptoms are considered by some to be hallmarks of PTSD, numbing symptoms often result in great distress and impairment, indicating that the impact of this symptom cluster should not be overlooked (Hellmuth et al., 2012; Lunney & Schnurr, 2007). The fact that re-experiencing and numbing, but not hyperarousal or avoidance, were indirectly and not directly related to women's use of IPV in this sample may be explained by the application of tension reduction theory and the self-medication hypothesis. This theory suggests that because these clusters produce the most distress, their presence may have produced the greatest amount of motivation to misuse alcohol, which was also related to women's use of IPV. This literature would be enhanced by studies designed to explicitly test these theories among IPV-victimized women.
Whereas some literature has suggested that addressing PTSD symptoms among men may reduce their use of IPV or aggressive behaviors (Bell & Orcutt, 2009), pathways to intervention for women experiencing PTSD, bidirectional IPV, and alcohol misuse remain unclear due to several factors unique to this population. First, much of the literature examining the link between PTSD and men's use of aggression was based upon studies of male veterans, a group with unprecedented access to mental health care if they choose to pursue it. However, many low income community women such as those in our sample do not have adequate access to mental health treatment or IPV services (Goodman, Smyth, Borges, & Singer, 2009). Recent evidence suggests that despite active help-seeking by low-income community women experiencing IPV, the mental health care needs of IPV-victimized community women frequently go unmet (Hien & Ruglass, 2009). This literature suggests that low income women who experience concurrent IPV victimization and use of IPV, substance use, and mental health problems experience both a great need for intervention and extensive barriers to treatment. Further, the critical role that alcohol misuse played in our model suggests that addressing mental health and alcohol misuse problems concurrently may be prove more effective to reduce women's use of IPV compared to mental health treatment alone. Therefore, ameliorating women's use of IPV may not be accomplished efficiently through traditional vehicles for delivering mental health treatment. Future research should explore the extent to which women in health care treatment facilities, the criminal justice system, and shelters benefit from having a thorough assessment of their use of IPV, IPV victimization, mental health and substance use. Without this information, providers may overlook intervention opportunities or inadvertently engage women in a course of treatment that could exacerbate their risk for IPV victimization, use of IPV, and their negative consequences.
If replicated, our findings also provide a platform to expand on two critical areas of research. First, the existing literature indicates that IPV is often bidirectional, and that some men experience severe forms of IPV victimization (Hines & Douglas, 2009). Therefore, our findings emphasize the need for future studies to examine additional pathways leading to men's use of IPV in the context of PTSD, such as the influence of men's IPV victimization on the relationships between PTSD symptoms, alcohol misuse, and use of IPV. Second, our findings provide a preliminary empirical basis for developing and testing new hypotheses.
Limitations
Several factors limit the generalizability of this study's findings. This is a study of IPV-victimized women only and their PTSD symptoms are assessed referent to IPV. Therefore, it remains unclear whether the novel findings presented here are due to gender as opposed to differences in the origin of PTSD. Further, this study focused specifically on women in relationships with men as it is based on theories of IPV that have been developed in the context of heterosexual relationships; the dynamics of IPV in same-sex-relationships are unique and therefore, these theories may not apply (Johnson & Ferraro, 2000). Data regarding sexual orientation and the gender of participants’ past partners was not collected in the current study. Future studies should aim to assess this information. Given the skewed nature of our data prior to transformation, an alternative data analytic approach for future studies is to dichotomize similarly skewed violence related outcome variables. The small sample size utilized in this study suggests that findings should be interpreted with caution and must be replicated using larger samples. Because PTSD has different emotional and behavioral correlates depending on the type and chronicity of criterion A stressor (Forbes et al., 2011; Kelley, Weathers, McDevitt-Murphy, Eakin, & Flood, 2009), perhaps PTSD-related use of IPV has distinct etiologies from non PTSD-related use of IPV (Bell & Orcutt, 2009). Additional research is needed with other populations of women (e.g., treatment seeking women, women Veterans, and community women with non-IPV related PTSD) to specify the influences of gender and origin of PTSD on the use of IPV. Use of IPV, IPV victimization, and alcohol misuse commonly co-occur with other influential factors such as drug use, non-IPV related trauma, family of origin violence, social support, comorbid psychiatric diagnoses, and individual coping styles not examined in the current study. Given the preliminary, hypothesis-generating focus of the present study, future research investigating these factors among a larger sample to increase statistical power and detect small effect sizes is needed. All data in this study were collected via self-report and therefore, are subject to self-report bias. This study also utilized a cross-sectional design, prohibiting us from making causal inferences about our findings. Future studies should utilize larger sample sizes, longitudinal and micro-longitudinal designs and dyadic data. Doing so would maximize statistical power, allow researchers to develop more comprehensive conceptual models, and make causal inferences about the etiologies of IPV. Future research may also improve upon our design by examining if IPV victimization subtypes are differentially related to substance use and use of IPV on a daily basis.
Conclusions
In this sample of IPV-victimized women, the severity of PTSD re-experiencing and numbing symptom clusters are related to the use of psychological and minor and severe physical IPV through pathways involving alcohol misuse. These results emphasize the need for future research to investigate women's use of IPV related to PTSD and the need for mental health providers to thoroughly screen their adult female patients for use of IPV, IPV victimization, and alcohol misuse. Future research is necessary to delineate the effects of gender, alcohol misuse, and IPV victimization on women's use of IPV.
Acknowledgments
This manuscript is the result of work supported, in part, by resources from the National Institutes on Drug Abuse (K23 DA019561, T32DA019426, and R25 DA020515) and the Swiss National Science Foundation (PBLAP1-131842 and PBLAP1-140055).
References
- Arbuckle JL. Amos (Version 19.0) SPSS Inc.; Chicago, IL: 2010. [Google Scholar]
- Babcock JC, Roseman A, Green CE, Ross JM. Intimate partner abuse and PTSD symptomatology: examining mediators and moderators of the abuse-trauma link. Journal of Family Psychology. 2008;22(6):809–818. doi: 10.1037/a0013808. doi: 10.1037/a0013808. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test. World Health Organization; Geneva, Switzerland: 2001. [Google Scholar]
- Bell KM, Orcutt HK. Posttraumatic stress disorder and male-perpetrated intimate partner violence. Journal of the American Medical Association. 2009;302(5):562–564. doi: 10.1001/jama.2009.1126. doi: 10.1001/jama.2009.1126. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative Ways of Assessing Model Fit. Sociological Methods & Research. 1992;21(2):230–258. doi: 10.1177/0049124192021002005. [Google Scholar]
- Caldwell JE, Swan SC, Allen CT, Sullivan TP, Snow DL. Why I Hit Him: Women's Reasons for Intimate Partner Violence. Journal of Aggression, Maltreatment & Trauma. 2009;18(7):672–697. doi: 10.1080/10926770903231783. doi: 10.1080/10926770903231783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements K, Schumacher JA. Perceptual biases in social cognition as potential moderators of the relationship between alcohol and intimate partner violence: A review. Aggression and Violent Behavior. 2010;15(5):357–368. doi: 10.1016/j.avb.2010.06.004. [Google Scholar]
- Conger JJ. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Feeny NC, Zoellner LA, Mavissakalian MR, Roy-Byrne PP. What would you choose? Sertraline or prolonged exposure in community and PTSD treatment seeking women. Depression & Anxiety. 2009;26(8):724–731. doi: 10.1002/da.20588. doi: 10.1002/da.20588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB. Posttraumatic stress diagnostic scale manual. National Computer Systems Pearson, Inc.; Minneapolis, MN: 1995. [Google Scholar]
- Fontana A, Rosenheck R, Desai R. Female Veterans of Iraq and Afghanistan seeking care from VA specialized PTSD Programs: comparison with male veterans and female war zone veterans of previous eras. Journal of Womens Health. 2010;19(4):751–757. doi: 10.1089/jwh.2009.1389. doi: 10.1089/jwh.2009.1389. [DOI] [PubMed] [Google Scholar]
- Foran HM, O'Leary KD. Alcohol and intimate partner violence: a meta-analytic review. Clinical Psychology Review. 2008;28(7):1222–1234. doi: 10.1016/j.cpr.2008.05.001. doi: 10.1016/j.cpr.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Forbes D, Fletcher S, Parslow R, Phelps A, O'Donnell M, Bryant RA, Creamer M. Trauma at the hands of another: longitudinal study of differences in the posttraumatic stress disorder symptom profile following interpersonal compared with noninterpersonal trauma. J Clin Psychiatry. 2011 doi: 10.4088/JCP.10m06640. doi: 10.4088/JCP.10m06640. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Smyth KF, Borges AM, Singer R. When Crises Collide. Trauma, Violence, & Abuse. 2009;10(4):306–329. doi: 10.1177/1524838009339754. doi: 10.1177/1524838009339754. [DOI] [PubMed] [Google Scholar]
- Hellmuth JC, Stappenbeck CA, Hoerster KD, Jakupcak M. Modeling PTSD Symptom Clusters, Alcohol Misuse, Anger, and Depression as They Relate to Aggression and Suicidality in Returning U.S. Veterans. Journal of Traumatic Stress. 2012;25(5):527–534. doi: 10.1002/jts.21732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien D, Ruglass L. Interpersonal partner violence and women in the United States: an overview of prevalence rates, psychiatric correlates and consequences and barriers to help seeking. International journal of law and psychiatry. 2009;32(1):48–55. doi: 10.1016/j.ijlp.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines DA, Douglas EM. Women's Use of Intimate Partner Violence against Men: Prevalence, Implications, and Consequences. Journal of Aggression, Maltreatment & Trauma. 2009;18(6):572–586. doi: 10.1080/10926770903103099. [Google Scholar]
- Hines DA, Douglas EM. Intimate terrorism by women towards men: does it exist? Journal of Aggression, Conflict and Peace Research. 2010;2(3):36–56. doi: 10.5042/jacpr.2010.0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [Google Scholar]
- Johnson DM, Zlotnick C, Perez S. Cognitive behavioral treatment of PTSD in residents of battered women's shelters: results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2011;79(4):542–551. doi: 10.1037/a0023822. doi: 10.1037/a0023822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MP, Ferraro KJ. Research on domestic violence in the 1990s: The discovery of difference. Journal of Marriage and the Family. 2000;57(283-294) [Google Scholar]
- Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE, Flood AM. A comparison of PTSD symptom patterns in three types of civilian trauma. [Article]. Journal of Traumatic Stress. 2009;22(3):227–235. doi: 10.1002/jts.20406. [DOI] [PubMed] [Google Scholar]
- Kenny DA. [May 16, 2011];Respecification of latent variable models. 1999 from http://davidakenny.net/cm/respec.htm.
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the clinician-administered PTSD scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10(2):90–96. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3rd ed. Guilford Press; New York: 2011. [Google Scholar]
- Lei P-W, Wu Q. Introduction to Structural Equation Modeling: Issues and Practical Considerations. Educational Measurement: Issues and Practice. 2007;26(3):33–43. doi: 10.1111/j.1745-3992.2007.00099.x. [Google Scholar]
- Lunney CA, Schnurr PP. Domains of quality of life and symptoms in male veterans treated for posttraumatic stress disorder. Journal of Traumatic Stress. 2007;20(6):955–964. doi: 10.1002/jts.20269. doi: 10.1002/jts.20269. [DOI] [PubMed] [Google Scholar]
- Peters CLO, Enders C. A primer for the estimation of structural equation models in the presence of missing data: Maximum likelihood algorithms. Journal of Targeting, Measurement & Analysis for Marketing. 2002;11(1):81–95. [Google Scholar]
- Preacher K, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test: An Update of Research Findings. Alcoholism: Clinical and Experimental Research. 2007;31(2):185–199. doi: 10.1111/j.1530-0277.2006.00295.x. doi: 10.1111/j.1530-0277.2006.00295.x. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Selin KH. Test-Retest Reliability of the Alcohol Use Disorder Identification Test in a General Population Sample. Alcoholism: Clinical and Experimental Research. 2003;27(9):1428–1435. doi: 10.1097/01.ALC.0000085633.23230.4A. doi: 10.1097/01.alc.0000085633.23230.4a. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Grekin ER. Alcohol and Affect Regulation. In: Gross JJ, editor. Handbook of Emotion Regulation. Guilford Press; New York, NY: 2007. p. 654. [Google Scholar]
- Steele CM, Josephs RA. Alcohol myopia: Its prized and dangerous effects. American Psychologist. 1990;45(8):921–933. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Warren WL. The Conflict Tactics Scales Handbook: Revised Conflict Tactics Scale (CTS2) and CTS: Parent-Child Version (CTSPC) Western Psychological Services; Los Angeles, CA, USA: 2003. [Google Scholar]
- Sullivan TP, Cavanaugh CE, Buckner JD, Edmondson D. Testing posttraumatic stress as a mediator of physical, sexual, and psychological intimate partner violence and substance problems among women. Journal of Traumatic Stress. 2009;22(6):575–584. doi: 10.1002/jts.20474. doi: 10.1002/jts.20474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan TP, Holt LJ. PTSD symptom clusters are differentially related to substance use among community women exposed to intimate partner violence. Journal of Traumatic Stress. 2008;21(2):173–180. doi: 10.1002/jts.20318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan SC, Gambone LJ, Caldwell JE, Sullivan TP, Snow DL. A review of research on women's use of violence with male intimate partners. Violence and Victims. 2008;23(3):301–314. doi: 10.1891/0886-6708.23.3.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan SC, Gambone LJ, Fields AM, Sullivan TP, Snow DL. Women who use violence in intimate relationships: the role of anger, victimization, and symptoms of posttraumatic stress and depression. Violence & Victims. 2005;20(3):267–285. doi: 10.1891/vivi.20.3.267. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. HarperCollins College Publishers; New York: 2007. [Google Scholar]
- Taft CT, Kaloupek DG, Schumm JA, Marshall AD, Panuzio J, King DW, Keane TM. Posttraumatic stress disorder symptoms, physiological reactivity, alcohol problems, and aggression among military veterans. Journal of Abnormal Psychology. 2007a;116(3):498–507. doi: 10.1037/0021-843X.116.3.498. doi: 10.1037/0021-843X.116.3.498. [DOI] [PubMed] [Google Scholar]
- Taft CT, Monson CM, Hebenstreit CL, King DW, King LA. Examining the correlates of aggression among male and female Vietnam veterans. Violence & Victims. 2009a;24(5):639–652. doi: 10.1891/0886-6708.24.5.639. [DOI] [PubMed] [Google Scholar]
- Taft CT, Vogt DS, Marshall AD, Panuzio J, Niles BL. Aggression among combat veterans: relationships with combat exposure and symptoms of posttraumatic stress disorder, dysphoria, and anxiety. Journal of Traumatic Stress. 2007b;20(2):135–145. doi: 10.1002/jts.20197. doi: 10.1002/jts.20197. [DOI] [PubMed] [Google Scholar]
- Taft CT, Weatherill RP, Woodward HE, Pinto LA, Watkins LE, Miller MW, Dekel R. Intimate partner and general aggression perpetration among combat veterans presenting to a posttraumatic stress disorder clinic. American Journal of Orthopsychiatry. 2009b;79(4):461–468. doi: 10.1037/a0016657. doi: 10.1037/a0016657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa M, Kubiak A, Quigley BM, Houston RJ, Derrick JL, Levitt A, Leonard KE. Husband and wife alcohol use as independent or interactive predictors of intimate partner violence. J Stud Alcohol Drugs. 2012;73(2):268–276. doi: 10.15288/jsad.2012.73.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd M, Armeli S, Tennen H. Interpersonal problems and negative mood as predictors of within-day time to drinking. Psychology of Addictive Behaviors. 2009;23(2):205–215. doi: 10.1037/a0014792. doi: 10.1037/a0014792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yufik T, Simms LJ. A meta-analytic investigation of the structure of posttraumatic stress disorder symptoms. Journal of Abnormal Psychology. 2010;119(4):764–776. doi: 10.1037/a0020981. doi: 10.1037/a0020981. [DOI] [PMC free article] [PubMed] [Google Scholar]