Abstract
The US Institute of Medicine and healthcare experts have called for new approaches to manage healthcare quality problems. In this chapter, we focus on macroergonomics, a branch of human factors and ergonomics that is based on the systems approach and considers the organizational and sociotechnical context of work activities and processes. Selected macroergonomic approaches to healthcare quality and patient safety are described such as the SEIPS model of work system and patient safety and the model of healthcare professional performance. Focused reviews on job stress and burnout, workload, interruptions, patient-centered care, health IT and medical devices, violations, and care coordination provide examples of macroergonomics contributions to healthcare quality and patient safety. Healthcare systems and processes clearly need to be systematically redesigned; examples of macroergonomic approaches, principles and methods for healthcare system redesign are described. Further research linking macroergonomics and care processes/patient outcomes is needed. Other needs for macroergonomics research are highlighted, including understanding the link between worker outcomes (e.g., safety and well-being) and patient outcomes (e.g., patient safety), and macroergonomics of patient-centered care and care coordination.
Keywords: macroergonomics, work system, sociotechnical system, organizational context, SEIPS model, healthcare quality, patient safety, patient-centered care, care coordination, job stress, workload, interruptions, system design, mixed methods research
1. INTRODUCTION
Multiple reports by the US Institute of Medicine (IOM) describe the major challenges experienced by the healthcare system (2001, 2004, 2006). The 1999 IOM report on “To Err is Human: Building a Safer Health System” (Kohn, Corrigan, & Donaldson, 1999) indicates that between 44,000 and 98,000 people die every year of preventable medical errors. The IOM reports and numerous healthcare experts called on new approaches, including human factors and ergonomics (HFE), to tackle these problems. The IOM report on health information technology (IT) and patient safety (2012) directly calls for greater involvement of and consideration for HFE in the areas of quality and risk management processes used by health IT vendors and in research on the design and use of health IT. The HFE discipline is increasingly recognized as a major scientific contributor to healthcare quality and patient safety (Carayon, Xie, & Kianfar, 2013).
In this chapter, we focus on macroergonomics, a branch of HFE that advocates the systems approach and considers the larger organizational and sociotechnical context of work activities and processes (Hendrick & Kleiner, 2001). Macroergonomics needs to be further integrated in healthcare research and practice in order to develop, implement and sustain solutions for improving healthcare quality and patient safety.
1.1 Healthcare Quality Aims
The IOM report on “Crossing the Quality Chasm” (2001) describes six dimensions of quality: (1) safety, (2) effectiveness, (3) patient-centered care, (4) timeliness, (5) efficiency, and (6) equity. A safe healthcare system prevents or mitigates iatrogenic patient injuries. Healthcare effectiveness refers to “services based on scientific knowledge to all who could benefit, and refraining from providing services to those not likely to benefit” (IOM, 2001, p.6). Patient-centered care is “care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions” (IOM, 2001, p.6). Timeliness can be considered one component of efficiency of care as it focuses on reduction in care delays and patient waits; efficiency of care is concerned with issues of waste, including waste of equipment, supplies, ideas and energy. Equitable care is care “that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socio-economic status” (IOM, 2001, p.6). It is important for HFE practitioners and researchers to be familiar with these quality aims. Research and practical initiatives in HFE should target outcomes of importance to health care, i.e. any of the six quality aims (Carayon et al., 2011a).
1.2 Focus on Macroergonomics
According to the International Ergonomics Association (IEA) (2000), HFE is “the scientific discipline concerned with the understanding of the interactions among humans and other elements of a system, and the profession that applies theoretical principles, data and methods to design in order to optimize human well-being and overall system performance.” Recently, Dul et al. (2012) emphasized the three core elements of the IEA definition for HFE: (1) systems approach, (2) design driven, and (3) joint optimization of performance and well-being. The IEA also defines organizational ergonomics or macroergonomics (one of three specialized domains of HFE): “Organizational ergonomics is concerned with the optimization of sociotechnical systems, including their organizational structures, policies, and processes.” Table 1 summarizes the key elements of macroergonomics and examples of macroergonomic applications to healthcare quality and patient safety.
Table 1.
Key Elements of Macroergonomics for Healthcare Quality and Patient Safety
| Key Elements of Macroergonomics | Examples of Macroergonomic Applications to Healthcare Quality and Patient Safety |
|---|---|
| Systems approach |
|
| Joint optimization of performance and well-being |
|
| Consideration of organizational and sociotechnical context |
|
| System interactions and levels (e.g., relationship between micro- and macro-ergonomic elements) |
|
| Implementation process |
|
Pasmore (1988) and Trist (1981) developed early models of sociotechnical work systems that included three components: the social system, the technical system and the environment. Each component represents a key aspect of the work system and interacts with the other components. Historically, sociotechnical systems theory applied to HFE problems has been called macroergonomics, and derives from the Human Factors and Ergonomics Society sub-discipline of Organizational Design and Management (ODAM) (Kleiner, 2008). Macroergonomists have long recognized the importance of a systems approach to improve well-being and performance (Hendrick, 2008; M. J. Smith & Carayon-Sainfort, 1989). They use their knowledge about microergonomics to improve system design while acknowledging (Zink, 2000) and attending “to the larger system factors that will ultimately support or negate interface-level implementations or interventions” (Kleiner, 2008, p. 462). As indicated in Table 1, consideration of the organizational and sociotechnical context is a key element of macroergonomics. Because macroergonomics is anchored within HFE, it is important for macroergonomists to understand the multi-level relationships and interactions between microergonomic variables (e.g., usability of health IT) and the organizational context (e.g., participatory process for selecting usable and useful health IT); considering system interactions and levels is another unique element of macroergonomics (see Table 1). Because of their consideration of the organizational context and their interest in system interactions, macroergonomists also develop theories and models for supporting and facilitating the implementation of HFE changes (for example, participatory ergonomics; see Table 1).
Because of its attention to the larger organizational context and entire sociotechnical systems, macroergonomics is an important approach to enhancing healthcare quality and patient and employee safety. Healthcare researchers and professionals recognize the importance of the ‘context’ in which patient safety practices and quality improvement initiatives are implemented (Ovretveit et al., 2011; Shekelle et al., 2011; Shekelle, Pronovost, & Wachter, 2010). This context is similar to the work system or sociotechnical system concept of macroergonomics.
Like other domains of HFE, macroergonomics aims to optimize both well-being and system performance (Dul et al., 2012). In the domain of health care, human well-being refers to satisfaction, worker health and safety, stress and burnout, learning and personal development at the individual and team levels, whereas system performance refers to patient safety, quality and operational efficiency. This double objective of macroergonomics is emphasized in the macroergonomic models of healthcare quality and patient safety reviewed in section 2.
Macroergonomics has a lot in common with other systems engineering approaches, such as cognitive systems engineering and resilience engineering (Dainoff, 2009; Hoffman & Militello, 2009). For instance, macroergonomists and cognitive systems engineers ask similar questions about strengths and limitations of work complexity, optimal configurations of teamwork and unintended consequences of technology (Carayon, 2006; Clegg, 2000; Woods & Hollnagel, 2006). Macroergonomics and resilience engineering share common interests in the organizational aspects of safety (Hollnagel, Woods, & Leveson, 2006). However, as described by Hoffman and Militello (2009), macroergonomics goes beyond the focus of cognitive systems engineering, which tends to be on the design of technologies for tasks, and addresses issues of organizational design (Carayon & Hoonakker, 2013). Whereas resilience engineering is focused on safety (Hollnagel, Woods, & Leveson, 2006), macroergonomics has a broader interest in a range of system performance and worker outcomes (see the element of ‘joint optimization of performance and well-being’ in Table 1). In addition, macroergonomics considers not only the cognitive aspects of work, but also the psychosocial aspects of work that are important for job satisfaction, worker motivation and job stress (Carayon, 2009; M. J. Smith & Carayon-Sainfort, 1989); see section 3.1 on Healthcare Job Design. For additional discussion about the relationship between different approaches to work system design, including macroergonomics and cognitive systems engineering, see Hoffman and Militello (2009) and Dainoff (2009).
1.3 Role of Macroergonomics in Healthcare Quality and Patient Safety
Macroergonomics has much to offer health care to improve the quality of patient care. The Agency for Healthcare Research and Quality (AHRQ) is charged with annual reporting of progress made in advancing the quality of US care (2012) based on the six IOM quality dimensions. Timeliness of care is a major issue. Wait times to see a physician in the Emergency Department (ED) are increasing and relate to ED crowding and inefficient patient flow throughout the organization (Hing & Bhuiya, 2012). While the percent of heart attack patients receiving treatment within the recommended time window has increased from 44% to 91% between 2005 to 2010 (Krumholz et al., 2011), significant delays exist before the patient presents to the facility that can deliver care, related to referral center transportation issues, ED delays, and delays in diagnosis (Miedema et al., 2011). A macroergonomics approach to this problem would focus on assessing work system characteristics in various organizational settings (e.g., EMS, emergency room, hospital cardiology services) that contribute positively or negatively to the timeliness of treatment.
Many reports have documented gaps in care provided. The DHHS Office of the Inspector General Report on hospital care received by patients on Medicare (2012) found that 1.5% of hospitalized elderly patients experience iatrogenic harm during their stay that contributes to their death (about 15,000 patients per month). The Centers for Disease Control and Prevention (CDC) reported that in 2002 over 1.7 million people developed healthcare-associated infections (HAIs – the most common hospital complication) related to urinary and intravenous (IV) catheters and other devices and treatments that patients receive; 99,000 of these patients died (Klevens et al., 2007). Whereas it was previously believed that HAIs were not preventable, the science now exists to prevent HAIs through macroergonomic-based interventions (AHRQ, 2012; Kleiner & Lewis, 2012; Pronovost et al., 2006). See section 6.1 for examples of macroergonomic studies on HAIs.
With respect to effectiveness, a US study of adult-recommended care for thirty acute and chronic medical conditions and preventive care found that patients receive only 55% of the recommended care and 11% of patients received care that is not recommended and potentially harmful (McGlynn et al., 2003). Inefficiencies in providing recommended care contribute to waste in healthcare; 30% of the $2.3 trillion dollars spent on health care annually is waste and can be eliminated from the system while still achieving the same or better patient outcomes (Delaune & Everett, 2008). Other examples of waste and inefficiencies include poor patient adherence to prescribed medications, underuse and overuse of medications, and ED visits by patients with non-urgent complaints (Delaune & Everett, 2008). A macroergonomics approach to patient adherence to prescribed medications would include considerations for micro-ergonomic aspects (e.g., design of medication box or reminder system) as well as the organizational and sociotechnical context (e.g., involvement of caregivers in helping patients take medications).
Disparities in healthcare provision by race, ethnicity, socioeconomic status and age are narrowing but continue to be common in the US. Racially and ethnically diverse patients receive worse care than Whites and non-Hispanics for 30–41% of measures, and low-income people had worse access to care than high-income people (89% of measures) (AHRQ, 2012). Macroergonomics research in this domain has begun to examine cultural aspects of trust in the healthcare system, in particular healthcare technologies (Montague & Lee, 2012; Montague, Winchester, & Kleiner, 2010).
The final IOM domain of quality is patient-centered care. A report by the Commonwealth Fund reveals that 33% of sick patients report leaving their doctor’s office without answers to important questions, 33–50% of patients report that their doctors sometimes, rarely, or never tell them about treatment options or involve them in decision making and over 60% of sicker US adults report difficulty getting needed care on nights, weekends and holidays without going to the ED (Shaller, 2007). See section 3.2 for additional information about macroergonomics and patient-centered care.
The discipline of HFE, and more specifically macroergonomics, can make significant contributions to all six healthcare quality aims (see Table 2 for examples). It is important to recognize that the six aims may interact and conflict with each other. Some may be considered acute or short-term goals (effectiveness, timeliness and efficiency) whereas other quality aims (safety, patient-centered care and equity) reflect chronic or long-term goals (Woods, 2006). As healthcare organizations may be more likely to pay attention to short-term goals at the expense of long-term goals, it is necessary to understand how to balance trade-offs between the various quality aims (Carayon, 2009; Woods, 2006). Balance between goals can be achieved by examining the broad organizational context in which goals at different levels are embedded (Rasmussen, 1997; Waterson, 2009).
Table 2.
Examples of Macroergonomic Issues for the Healthcare Quality Aims
| IOM Quality Aims | Examples of Macroergonomic Issues |
|---|---|
| Safety | Role of information flow between multiple clinicians and healthcare organizations in medication safety. |
| Effectiveness | Design and implementation of clinical decision support for recommended care. |
| Patient-centered care * | Designing improved patient experiences and clinician workflows that facilitate patient participation. |
| Timeliness | Impact of patient volume on time pressure and delays in care. |
| Efficiency | Impact of supply chain management on nursing work. |
| Equity | Design of personal health records for diverse patient populations. |
For further discussion of macroergonomics of patient-centered care, see section 3.2.
Macroergonomics also focuses on maximizing clinician health and well-being. Indeed, many patient outcomes like satisfaction with care and adherence to treatment plan have been linked to physician outcomes such as job satisfaction (DiMatteo et al., 1993; Peltier, Dahl, & Mulhern, 2009). There is growing concern about the impact of physician burnout on quality and safety of care delivery (Shanafelt et al., 2010; Shanafelt et al., 2012; Thomas, 2004). Health care also experiences among the highest number of nonfatal occupational-related injuries and illnesses across all US industries (CDC, 2012). Although nonfatal, these can be more costly. They include preventable injuries and illnesses, such as needlestick injuries, infections (e.g., influenza) transmitted from patients or other healthcare workers and musculoskeletal injuries. Healthcare needs innovative work redesign solutions for both patient and clinician health, such as those proposed by macroergonomics.
1.4 The Importance of a Macroergonomic Approach
A case adapted from research observations in a primary care clinic illustrates the importance of macroergonomics in understanding performance in complex work systems (Box 1).
Box 1. Case description of a primary care visit.
An elderly woman, Mrs. Smith, and her granddaughter Melody visit Dr. Jones, a family physician, at a primary care clinic. Dr. Jones enters the room carrying a laptop computer and paperwork. Mrs. Smith describes her problems with seasonal allergies and Dr. Jones asks questions, examines her and tells her that he can prescribe something for her symptoms. During the visit, Dr. Jones asks what medications Mrs. Smith is taking. “I can tell you,” she says, and recites a long list of medications from memory, some by name, some by what she thinks it is for (“my heart pill … oh yeah, I forgot to take that yesterday, should I take two today?”) and some by color (“I take that purple pill at nighttime”). Melody helps match the medication name to what it is for but did not bring a list with her. Dr. Jones sighs that, even though this is Mrs. Smith’s third visit, he still does not have an accurate medication list. Dr. Jones mentions Mrs. Smith’s blood pressure, sparking a conversation about her blood pressure history. Dr. Jones offers to show Mrs. Smith the blood pressure history graphed on the computer but she cannot make out the tiny numbers graphed on the laptop screen. She does not say anything, but makes a mental note to bring her reading glasses next time.
“As long as we’re on the computer, let’s order your blood pressure medicine prescription refill,” says Dr. Jones. He begins to navigate the order entry software while Mrs. Smith and Melody wait. “Doctor…” Mrs. Smith says, as a question comes to mind, but then, reconsidering, “I’ll let you finish with the computer, first.” The order entry is taking too long. “Why can’t I click on this?” mutters Dr. Jones. After several attempts, he restarts the process, while Mrs. Smith waits. This time it works and he closes the laptop and begins packing up. “You’ll also want to get an over-the-counter medicine called for your allergies called loratidine…” Dr. Jones starts, but Mrs. Smith interrupts. “Can’t you just write a prescription so it’s cheaper?” she asks. “Yeah,” he says, glancing at his watch and then at his closed laptop, “Yeah, I’ll put it in, but I don’t know if it’s covered by your insurance, so if it’s not, give us a call.” Mrs. Smith remembers her question as Dr. Jones is leaving the room. “Can you take a look at this mole on my arm?” Dr. Jones checks the clock. He is already running 30 minutes behind and his nurse has added two urgent care patients to his already packed patient schedule. “Come back in 1 month to recheck your blood pressure and allergies and I’ll check the mole then.”
Dr. Jones exits the room and comments to a passing-by medical assistant, “Remind me to put in an order for Mrs. Smith if I forget.” There is no time to enter orders or document the visit before his next appointment. He hurries to the next patient, wishing he could flip through the paper patient chart – a relic from the days before electronic medical records – on his way down the hall. After the day’s visits, Dr. Jones returns to his office, plugs in his laptop, and arranges his notes while waiting for it to boot up (the battery ran out during the last visit). Using a combination of notes and memory, Dr. Jones types his notes for his patient visits, in reverse order so that he can get the most recent visit down while it is fresh in his mind. It is a slow process; he is not a fast typist and he has not had the time to figure out how to use the electronic health record features that the organization’s information technology specialist showed him a few months ago to speed up documentation. As he is putting on his coat to go home, he realizes he forgot to order Mrs. Smith’s medication; he makes a mental note to do this first thing when he gets to his home computer.
An analysis of this scenario could identify several important microergonomic problems related to individual performance (overreliance on memory) or person-technology interaction (vision-impaired acuity of a display). Microergonomic problems are conducive to microergonomic solutions such as new tools (e.g., checklists) or user interface redesign. A macroergonomic analysis acknowledges these microergonomic problems and situates them in a broader organizational context. Macroergonomics extracts clues of higher-level influence on lower-level phenomena (Karsh & Brown, 2010): the patient’s memory of her medications is supplemented by her granddaughter, a team-level strategy; the doctor’s ability to remember to order a medication depends on organization-level constraints such as how busy his schedule is, whether he is running behind or on time, the choice to have physicians carry portable laptop computers that take time to power-up rather than provide computers in each exam room and whether there is time in between patient visits to enter orders and document patient visits.
Macroergonomics’ broad scope helps to see not only the many elements at multiple levels that relate to individual performance but also how cross-sections of performance are pieced together over time to form workflows, coordinated activity and communication patterns. Indeed, a macroergonomic view of the primary care physician’s activities shows not only discrete episodes of single-task performance but also how work accumulates; how tasks are assigned, rearranged, and prioritized over the course of a day; and even how computer-based work is distributed between the home and the workplace. These considerations illustrate macroergonomics’ concern for not only patients and the quality of their care but also for the health, safety and well-being of clinicians. Macroergonomics often orients us to phenomena that fall outside the core expertise of microergonomics, including for example, power dynamics, organizational/safety culture and social norms, the social implications of computer use during a person-to-person encounter, the trade-off between the effectiveness and affordability of medical therapies, the incorporation of insurance coverage and medication formulary considerations into treatment plans, and teamwork or joint decision-making between patients and clinicians. Fittingly, macroergonomic solutions are typically multi-level. For example, an effective microergonomic redesign in a primary care clinic might be introducing a usable software tool for displaying graphs, whereas a macroergonomic redesign might accompany the new tool with office space redesign to accommodate a large monitor for displaying performance dashboard information to patients and just-in-time training to support clinician effective adaptation to the new tool.
2. MACROERGONOMIC APPROACHES TO HEALTHCARE QUALITY AND PATIENT SAFETY
In a macroergonomics approach, the entire system must be considered; not just the system elements, but also interactions among the system elements and relationships between various systems. This emphasis on system interactions is similar to the Interacting Systems Model of Ergonomics outlined by Wilson (2000). In this section, we review three macroergonomic models and describe system elements that can influence healthcare quality and patient safety. We first describe two macroergonomic models developed by researchers at the University of Wisconsin-Madison and then one model developed in the UK. The section ends with a description of additional macroergonomic issues of importance to healthcare quality and patient safety.
2.1 SEIPS Model of Work System and Patient Safety
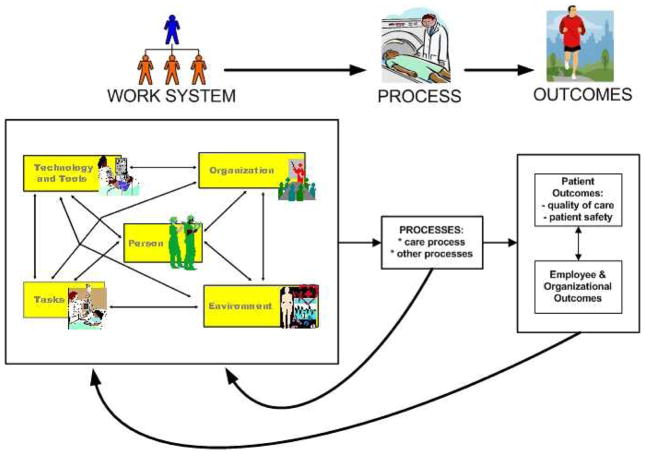
The SEIPS (Systems Engineering Initiative for Patient Safety) model of work system and patient safety (Carayon et al., 2006) integrates the macroergonomic work system model of Smith and Carayon (Carayon & Smith, 2000; M. J. Smith & Carayon-Sainfort, 1989; M. J. Smith & Carayon, 2001) and the Structure-Process-Outcome model of Donabedian (1978). According to the SEIPS model (see Figure 1), patient safety and, more generally healthcare quality, are influenced by work systems and processes. For instance, HAIs are influenced by various processes, such as hand hygiene, patient room cleaning and other infection control guidelines. The design of work systems influences the performance of processes that are known to prevent or mitigate HAIs (Alvarado, 2012; Alvarado, Wood, & Carayon, 2006; Gurses et al., 2008). Lack of easy access to hand hygiene products may hinder clinicians’ ability to comply with hand hygiene practices. Work organization in intensive care units (e.g., frequent interruptions) may affect physician performance of central line placement and, therefore, compliance with sterile field procedures (Alvarado, 2012; Carayon et al., 2006).
Figure 1.
SEIPS Model of Work System and Patient Safety (Carayon et al., 2006)
According to Donabedian (1988), a care process is “what is actually done in giving and receiving care” (p. 1745), and is, therefore, influenced by all work system elements. The SEIPS model expands Donabedian’s model by including not only care processes, but also other processes (e.g., supply chain management, housekeeping, purchasing) that can influence outcomes.
Another important aspect of the SEIPS model is the relationship between patient outcomes (e.g., patient safety) and employee and organizational outcomes (e.g., clinician quality of working life). For instance, a nurse who is experiencing back pain may not have all of the physical (strength) and cognitive (attention) abilities needed to lift a patient out of bed; this situation may increase the risk for patient falls. Research has explored the link between patient outcomes and employee and organizational outcomes (Williams et al., 2012). Physicians who experience high burnout are more likely to perceive problems with quality of care (Shanafelt et al., 2010; Shanafelt et al., 2012; Thomas, 2004). Taylor et al. (2012) found a negative association between two dimensions of safety climate (i.e. perceptions of organizational commitment to safety and quality of collaboration), and a patient outcome (i.e. decubitus ulcer) and nurse injury. Worker outcomes may mediate the impact of working conditions on patient outcomes (Hickam et al., 2003; Laschinger & Leiter, 2006; Lundstrom, Pugliese, Bartley, Cox, & Guither, 2002; Williams et al., 2012). Further research is needed to examine the relationship between worker outcomes and patient outcomes.
The SEIPS model also defines feedback loops between processes and the work system, and between outcomes and the work system. These feedback loops represent triggers for work system redesign: data on process deficiencies and outcomes may help to identify needs for changes in the work system. When the work system is redesigned according to HFE principles, process performance should be enhanced and improvements in patient outcomes and employee and organizational outcomes are more likely to occur.
The SEIPS model has been used by researchers to address a variety of patient safety and healthcare quality problems (Carayon, 2012a), such as medication safety (Wetterneck et al., 2006; Wetterneck et al., 2011), medication management process failures (Faye et al., 2010), and hospital readmissions and ED visits for patients with chronic diseases (Carayon et al., 2012). The SEIPS model can also be used by healthcare professionals (1) to identify factors contributing to patient safety events, (2) to anticipate systemic impact of work system changes such as implementation of health IT, and (3) to evaluate the macroergonomic aspects of interventions.
With respect to macroergonomics research, the SEIPS model can be used as an overall framework to guide data collection on the various work system factors that influence a particular care process or a specific healthcare quality or patient safety problem. This data collection often relies on multiple qualitative and quantitative methods; see section 5.3 for examples of macroergonomic studies that use multiple data collection methods. The SEIPS model can also be used to quantitatively model and test how interactions of work system factors contribute to outcomes, such as perceived workload, patient safety problems and job stress; see, for example, the studies on ICU nursing workload by Gurses and Carayon (Gurses & Carayon, 2007a, 2009a; Gurses, Carayon, & Wall, 2009). The SEIPS model has also been used as the underlying framework for a range of methodologies for work system analysis; see section 5.2 for examples. For additional information on the SEIPS model and its research and practical applications, see Carayon et al. (2013).
2.2 Karsh and Colleagues’ Model of Healthcare Professional Performance
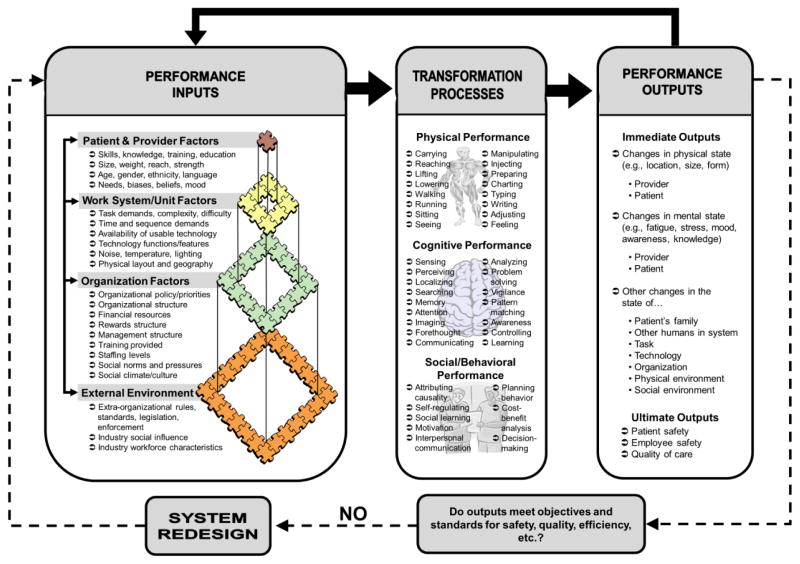
Prior to Karsh et al. (2006) the major patient safety paradigms focused on either reducing healthcare professional (HCP) errors, reducing patient harm, or improving the use of evidence-based medicine. The paradigms acknowledged systems change as a lever for patient safety improvements but none provided details about which system changes were needed and how changes would actually affect target outcomes (errors, injuries, quality) (Holden, 2011a). Karsh et al. (2006) recognized this gap and developed a new HFE paradigm for patient safety that promotes achieving patient safety through the (re)design of healthcare systems to support HCP performance and the elimination or control of hazards.
The model of healthcare professional performance adopts a sociotechnical systems model inspired by open systems theory1 (Katz & Kahn, 1966) and the SEIPS model (Carayon et al., 2006) (see Figure 2). HCP performance is treated as the transformation process in the cyclical input-transformation-output chain. Performance is defined as the physical (e.g., walking, carrying, reaching), cognitive (e.g., perceiving, analyzing, communicating), and social/behavioral (e.g., self-evaluating, decision making, cost-benefit) activities carried out by HCPs toward some (usually patient-related) goal (Figure 2, middle). The inputs into performance come from a multilevel work system (Figure 2, left side). At the work system center are people and performance-relevant factors such as skills, knowledge, age, and beliefs. People are nested in units nested in organizations and therefore influence and are influenced by unit- and organization-level factors such as tasks and goals, the physical and social environments, and organizational policies and routines. Organizations in turn operate in an external environment including industry practices, legislation, and societal conditions. Performance phenomena and any resultant outcomes are products of multifactorial interactions within and between systems and the quality of performance fluctuates depending on the degree of fit between system factors (Karsh, Escoto, Beasley, & Holden, 2006; Karsh et al., 2009). The performance outputs are immediate outputs such as changes in physical and mental state of the HCP and patient and more downstream outputs such as patient and employee safety, and quality of care (Figure 2, right side). Another important aspect of this paradigm is the notion of feedback; system outputs are evaluated against objectives and the work system is redesigned or adapted accordingly (Holden et al., 2011a; Novak, Holden, Anders, Hong, & Karsh, forthcoming).
Figure 2.
Model of Healthcare Professional Performance (Karsh, Holden, Alper, & Or, 2006)
When work system inputs may adversely create performance risk, they are called hazards. Karsh and colleagues therefore promoted the systematic proactive analysis of work systems to identify hazards as well as the retroactive analysis of performance problems as insight into possible hazards (Carayon, Faye, Hundt, Karsh, & Wetterneck, 2011; Holden, Rivera-Rodriguez, Faye, Scanlon, & Karsh, 2012, in press; Karsh, Holden, Alper, & Or, 2006). The inclusion of social/behavioral performance mechanisms in the model of healthcare professional performance underlines one of the unique contributions of macroergonomics that integrates considerations for psychosocial aspects of work.
The model of healthcare professional performance has proven useful in framing patient safety generally (DeBourgh & Prion, 2012) and especially in positing the performance mechanism that mediates between work system interventions (input) and safety outcomes (output) (Holden, 2011a; Holden et al., 2011a). The model has also been applied to conceptualize how multiple factors across levels interact to produce safety (Karsh & Brown, 2005, 2010), error reporting (Holden & Karsh, 2007), and behavioral outcomes such as HCP use of technology (Holden & Karsh, 2007, 2009). The model is also at the heart of the campaign to make the goal of healthcare technology design to support HCP performance (Holden, 2011a; Karsh, 2009; Karsh, Weinger, Abbott, & Wears, 2010; Stead & Lin, 2009).
2.3 Vincent and Colleagues’ Framework for Patient Safety Incidents
Vincent and colleagues (1998) developed a framework for analyzing patient safety incidents that includes seven types of system factors: (1) patient factors, (2) task and technology factors, (3) individual (staff) factors), (4) team factors, (5) work environmental factors, (6) organizational and management factors, and (7) institutional context factors. These system factors influence clinical practice and may contribute to patient safety incidents; they are similar to the latent failures in Reason’s (2004) model. The framework was adapted to specifically examine patient safety and quality of surgery (Vincent, Moorthy, Sarker, Chang, & Darzi, 2004). Three groups of factors explained surgical complications and adverse surgical outcomes: (1) patient risk factors (e.g., presence of comorbidity), (2) surgical skills (e.g., technical skills) and (3) operation profile (which includes the system factors listed above). The primary focus of Vincent and colleagues’ framework is to understand and analyze patient safety incidents and accidents. The SEIPS model and Karsh and colleagues’ model of healthcare professional performance complement this framework by providing additional insights for improving healthcare systems and processes (Vincent, 2010). The SEIPS model describes care processes as being influenced by the work system and influencing outcomes. Therefore, in comparison to Karsh and colleagues’ model and the framework of Vincent and colleagues, the SEIPS model can be more easily adopted by healthcare professionals who focus on care process improvement and redesign. The focus of Karsh and colleagues’ model on performance of healthcare professionals provides additional insights regarding how to support performance and subsequently healthcare quality. In contrast to the framework of Vincent and colleagues that focuses specifically on patient safety incidents and accidents, the SEIPS model and the model of Karsh and colleagues emphasize both worker and patient outcomes; this is in line with the double objective of HFE (Dul et al., 2012).
All three models, the SEIPS model, the model of healthcare professional performance and Vincent et al. framework for patient safety incidents, highlight the importance of systems approach to healthcare quality and patient safety. The framework by Vincent et al. focuses on analyzing patient safety incidents, whereas the SEIPS model and the model of healthcare professional performance go beyond analysis and provide frameworks, mechanisms and feedback loops to support healthcare work system redesign. The system factors in the three models are slightly different, but are conceptually similar and exhaustive. The model of healthcare professional performance emphasizes the multi-level nature of system design in a manner similar to other models, such as Rasmussen’s (1997) hierarchical system design model.
2.4 Other Macroergonomic Issues in Healthcare Quality and Patient Safety
Waterson (2009) conducted a review of systems approaches to patient safety; the following characteristics were used to identify human factors systems approaches: (1) input-output-processes, (2) whole-part relationships and (3) interactions among system elements. Most studies reviewed focused on medical errors (e.g., reporting of errors) and perceptions of safety problems and examined a limited number of factors. Few studies actually assessed relationships among system factors, including interactions between different system levels. This review highlights the need for additional research on macroergonomics in healthcare quality and patient safety, in particular understanding system levels and the connections between the levels.
3. FOCUSED REVIEWS ON MACROERGONOMICS TOPICS IN HEALTHCARE QUALITY AND PATIENT SAFETY
In this section, we focus our review on the macroergonomics of (1) healthcare job design (job stress, workload and interruptions), (2) patient-centered care, (3) health IT and medical devices, (4) violations and (5) care coordination. These topics were chosen because they are core issues in healthcare quality and patient safety that are often debated in the healthcare literature and that can benefit from macroergonomics.
3.1 Healthcare Job Design
This section reviews three key areas of research: job stress and burnout, workload, and interruptions, which have been targeted by macroergonomic healthcare researchers with the aim to improve job design and implement job redesign interventions.
3.1.1 Job Stress and Burnout
As described above, macroergonomics aims at jointly optimizing system performance and well-being. Therefore, macroergonomists are concerned with all aspects of work, i.e. cognitive, physical and psychosocial. In this section, we briefly review research on job stress and burnout in healthcare, including a description of psychosocial work factors that contribute to job stress and burnout. Given the extensive literature on job stress and burnout in healthcare, we refer the readers to Williams et al. (2012) and Schaufeli (2007) for additional information on this domain.
Based on a systematic literature review of over 100 articles in the scientific literature, Hickam et al. (2003) examined the effects of personal, professional, and social aspects of healthcare work on patient safety. The personal aspects included stress, burnout, dissatisfaction, motivation and autonomy. Hickam et al. found that overall there is no evidence (NE) or not sufficient evidence (NSE) to conclude that healthcare worker stress (1) causes increased adverse patient outcomes (NSE), (2) affects the rate of medical errors (NSE), (3) affects the rate of recognition after errors occur (NSE), (4) affects the probability that adverse events will occur following detected or undetected medical errors (NE), and (5) that the complexity of the care plans affects whether stress affects patient outcomes (NE). Jones et al. (1988) examined the relationship between stress and malpractice risks of 91 departments in five hospitals in the US. High malpractice risk departments had significantly higher scores on organizational stress (employees’ perceptions of well-being of their department and organization) and job stress (mental, emotional and psychosomatic stress reactions that employees attribute to their work) but not on personal stress (stressful life events experienced in the past year) as compared to low malpractice risk departments.
More recently, Williams et al. (2012) reviewed studies that examine the relationship between stress and burnout with quality of care; they found a less consistent relationship when researchers use objective measures of care quality as compared to patient perceptions of healthcare quality. Challenges in operationalizing stress contribute to the difficulty in establishing a direct relationship between stress and quality of care and patient safety (Williams et al., 2012). Further macroergonomic research is needed to understand the common work system antecedents for worker outcomes such as job stress and burnout, and patient outcomes.
3.1.2 Workload
Clinician workload is high in health care and has been shown to negatively affect quality of working life and the quality of care (Kiekkas et al., 2008; Pronovost et al., 2002; Michtalik et al., 2013). The conceptualization and measurement of workload in health care has focused on staffing ratios with research showing that as the nurse to patient ratio decreases, quality of care deteriorates (Lang, Hodge, Olson, Romano, & Kravitz, 2004; Shekelle, 2013). Macroergonomists advocate measures of workload at multiple system levels. Carayon and Gurses (2005) identified four levels of measures for clinician workload2: (1) unit-level measures (e.g., number of clinicians per patient), (2) job-level measures of workload as a job characteristic, (3) patient-level measures (e.g., based on the patient’s clinical condition), and (4) situation-level measures (e.g., specific work system demands on individual clinicians). Similarly, Holden and colleagues distinguished between unit-, job- and task-level measures3 (Holden et al., 2010; Holden et al., 2011b). They measured perceived workload at each level using a standardized, cross-sectional survey of nursing and pharmacy workers at two academic, freestanding pediatric hospitals in the US. A multilevel statistical (logit) model of 176 registered nurses showed that self-reported unit-level workload was significantly associated with higher self-reported dissatisfaction and burnout (unstandardized partial regression coefficient, γ = 0.31 and 0.45, respectively), whereas task-level mental workload was significantly associated with the self-reported likelihood of medication error (γ = 1.04) and burnout (γ = 0.25) (Holden et al., 2011b). Additional statistical modeling furthered highlighted the importance of considering workload measurement at different levels. For example, in a multiple linear regression analysis of 48 pharmacists and 31 pharmacy technicians, greater job dissatisfaction was significantly associated with higher “external” mental workload (interruptions, divided attention, and rushing during medication tasks; standardized regression coefficient, β = 0.31) but significantly associated with lower “internal” mental workload (concentration, effort, β = −0.27) (Holden et al., 2010). In other words, two workload measures had opposite effects on self-reported worker well-being.
Each workload conceptualization and measure has strengths and weaknesses and may affect clinician and patient outcomes. For example, unit-level measures such as the number of patients per nurses can be useful to measure the overall workload in a unit at a macro-level and can be used to compare performance and outcomes across units. However, workload measures at the situation- and task-levels are needed to provide insight and direction about how to redesign the work environment to improve clinician quality of working life and clinical outcomes (Gurses, Carayon, & Wall, 2009; Holden et al., 2011b; Hoonakker et al., 2011a). Given the current and expected shortage of clinicians and aging of the population (General Accounting Office (GAO), 2001; Colwill, Cultice, & Kruse, 2008), research on how to reduce workload by redesigning the work system using a macroergonomics approach has paramount importance. For instance, redesigning the work system may involve implementing a technology that takes blood pressure and pulse vital signs and sends the values automatically to the EHR so nurses do not have to spend time documenting.
3.1.3 Interruptions
Interruptions became a topic of interest to many healthcare researchers after the IOM stated that interruptions were likely contributors to errors (Institute of Medicine, 2000). In the healthcare literature, “interruption” is often used synonymously for distractions, breaks-in-task, disruptions or operational failures. Despite the varying terms, researchers are concerned about a clinician’s performance being affected when his/her attention to a primary task is interrupted. Rivera-Rodriguez and Karsh (2010) conducted a systematic literature review of interruptions across healthcare settings. They found only three studies that actually linked interruptions to medical errors (Flynn et al., 1999; Westbrook, Woods, Rob, Dunsmuir, & Day, 2010; Wiegmann, ElBardissi, Dearani, Daly, & Sundt, 2007). Three additional studies tested interventions to eliminate or reduce interruptions, either during medication administration by nurses or during a physician-patient visit (Pape, 2003; Pape et al., 2005; Peleg et al., 2000), two of which were successful (Pape, 2003; Pape et al., 2005). However, from a macroergonomic viewpoint that considers the broad organizational context, elimination of interruptions is not practical for the healthcare environment, as interruptions are built into the system with phones, pagers, patient call lights; in addition, patient emergencies that would take precedence over the interrupted task are not uncommon. Also, the research on interruptions had taken a microergonomic approach by only focusing on the person being interrupted. For example, Grundgeiger et al. (2010) studied the impact of interruptions on ICU nurses’ cognitive demands and the strategies they use to resume activities. This research is important to identify the cognitive impact of interruptions, but does not consider the larger organizational context in which interruptions occur.
Rivera-Rodriguez (2012) studied interruptions from a macroergonomics perspective and conducted research on interruptions that goes beyond the narrow focus on the interruptee. By understanding the viewpoint of the interrupter, she can proactively study interruptions prior to their occurrence to understand why, when, and how nurses interrupted each other. She studied expert nurses in a Neuroscience Surgical Intensive Care Unit (NSICU) at a non-profit, 440-bed tertiary care hospital in the Midwest of the United States. To understand nurses’ decisions surrounding interruptions, she conducted open-ended interviews with ten nurses. During the interviews, nurses described their experiences with interruptions, their work environment with regards to interruptions, and the decisions they made about interrupting. The interviews were analyzed in the NVivo9© qualitative data analysis software, using dimensional analysis as a guide (Caron & Bowers, 2000; Kools, McCarthy, Durham, & Robrecht, 1996; Schatzman, 1991). Rivera-Rodriguez found that nurses used specific cues to determine the interruptibility of another nurse; and nurses often completed quick cost-benefit analyses to determine if the information they were about to interrupt with was more important than 1) the primary task of the other nurse, or 2) the potential consequence of the interruption. She also found that many of the interruptions were team-based: nurses interrupted each other to help one another with patient care tasks. More interruption research needs take the macroergonomic or sociotechnical systems perspective used by Rivera-Rodriguez. Studies also need to distinguish between value-added versus non-value added interruptions. Then, interruption interventions can be designed to target non-value added interruptions, which will make the interventions more compatible with the reality of healthcare delivery and clinician workflow (Rivera-Rodriguez, 2012).
3.2 Macroergonomics of Patient-Centered Care
The majority of macroergonomics research and practice in health care attempts to understand and support the performance of healthcare workers. Patient safety efforts, for example, tend to focus on the design of a clinician’s work system with the idea that better design will result in better outcomes for patients (DeLucia, Ott, & Palmieri, 2009; Karsh, Holden, Alper, & Or, 2006; Vincent, 2010). A similar assumption is made in research on improving patients’ experiences through clinical process redesign or improving the quality of care by addressing healthcare professionals’ workplace stress and well-being (Holden, 2011b; Rutledge et al., 2009; Sexton, Thomas, & Helmreich, 2000; Williams, McMurray, Baier-Manwell, Schwartz, & Linzer, 2007). In worker-centered macroergonomic analyses, the patient and the patient’s family are often viewed as a component of the worker’s broader work system. For example, Gurses and Carayon’s (2007b) study of performance obstacles in critical care nursing discusses patient-related obstacles as part of nurses’ “tasks” (“dealing with family needs” reported by 35% of the 265 ICU nurses participating in the survey) and their “environment” (“distractions from family members” reported by 42% of ICU nurses, and “phone calls from family members” reported by 23% of ICU nurses).
However, the paradigm of patient and family involvement is changing. The IOM (2001) identified patient-centeredness as a critical component of healthcare quality to draw attention to the patient, otherwise excluded from healthcare design and process decisions. This recognizes that in health care patients are not only the customers of the work system, but their characteristics and activities are inputs to and products of the work system.4 Even in settings where they are not synchronously involved (e.g., the patient is unconscious, non-communicative, not of decision-making capacity or not present), for example, in the inpatient pharmacy, trauma resuscitation, the neonatal intensive care unit, or during surgery (Holden et al., 2010; Xiao, Seagull, Mackenzie, & Klein, 2004), a patient’s needs and goals are encoded in advanced directive documents, prior communications with clinicians or family, and patient advocates or other representatives. Furthermore, macroergonomics research is increasingly conducted in settings where the patient or family is or can be an active performer of care-related “work” activities (see Table 3). It is imperative to understand and design the macroergonomic system of patients and family members in order to support their performance (Carayon et al., 2011b; Henriksen, Joseph, & Zayas-Cabán, 2009; Montague, Winchester, & Kleiner, 2010; Zayas-Cabán & Brennan, 2007) (see Table 4). This means both: (1) helping the patient or family work in concert with clinicians within a team-based model of care such as family-centered rounds (Hoonakker et al., 2011a; Muething, Kotagal, Schoettker, Gonzalez del Rey, & DeWitt, 2007) or joint care-planning models like the patient-centered medical home (Berenson et al., 2008), and (2) supporting patients and families in the “care work” they do at home or in the community, such as understanding their health (Altman Klein & Meininger, 2004) or managing their medications (Altman Klein & Meininger, 2004; Morrow et al., 2005).
Table 3.
Examples of Care-related “Work” Performed by Patients and Family Members, Alone, or in Concert with Clinicians
| Examples of Patient/Family “Work” Performance to be Supported |
|---|
|
Table 4.
Macroergonomic System Factors Shaping Patient’s or Family’s “Work” Performance
| Work System Elements | Examples of System Elements Shaping Patient’s or Family’s “Work” Performance |
|---|---|
| People | Given what they are asked to or want to do, do patients or families have adequate knowledge, skills, and abilities? How motivated are they? What are their goals and how well do they align with the goals of clinicians or the healthcare system? |
| Tasks | How difficult or complex are the tasks relative to patients’ or families’ abilities? How many tasks are to be done and how are tasks allocated to patients, families, and health care clinicians? How do these tasks align with the perceived or desired roles of those individuals? |
| Tools/technologies | Do patients or families have the information they need or the means for obtaining the information? Do they have technology to track or communicate information? Do they have the medical equipment needed for self-monitoring and therapy? Is the technology they have compatible with planned interventions, such as e-mail reminders or informational websites? |
| Organization | Are patients and families recognized as partners in their health and care? What rights do they have? Do their schedules align with those of the health system’s? |
| Environment | Do patients or families have a place to do their work? Is it free of noise and distractions? Is there adequate lighting, privacy, space, and utilities? Are their living arrangements conducive to healthy behaviors? Do surrounding social, political, legal, and educational systems facilitate or impede patients’ or families’ activities? |
3.3 Macroergonomics of Health Information Technology (IT) and Medical Devices
Health IT implementation is expanding significantly due to varied incentives by the federal government and organizations interested in improving the quality of health care in the US (Blumenthal & Tavenner, 2010; Gold, McLaughlin, Devers, Berenson, & Bovbjerg, 2012). Examples of health IT include electronic health records (EHRs), computerized provider order entry (CPOE), patient portal, personal health records (PHRs), electronic prescribing, smart infusion pump and barcoded medication dispensing and administration technologies. A major hazard in health care that contributes to poor care across all IOM domains of quality is information chaos, or a clinician not having the information he/she needs at the time that they need it to provide the best care possible (Beasley et al., 2011; Elder et al., 2006; Schultz, Carayon, Hundt, & Springman, 2007). If designed and implemented appropriately, health IT such as EHRs makes patient information readily accessible. For instance, patient information can be shared across health systems through health information exchanges (HIEs). But the implementation of health IT does not come without its issues, such as lack of support to clinician cognitive work and misfit with clinician workflows (Karsh, Weinger, Abbot, & Wears, 2010; Stead & Lin, 2009). Patient privacy concerns add complexity to the sharing of information through HIEs, especially across state lines, and many EHRs have limited, if any, ability for patients to access their own information and communicate with their healthcare team. Patient portals, PHRs and other consumer health IT applications have the potential to provide patients (and consumers) access to health information and services and to support patient-centered care, but need greater HFE input (Agarwal, Anderson, Crowley, & Kannan, 2011; Morrow & Chin, 2013; NRC Committee on the Role of Human Factors in Home Health Care, 2011; Zayas-Caban & Dixon, 2010).
The concept that the usability of health IT affects the safety of care is slowly being accepted by the healthcare community and vendors of health IT (McDonnell, Werner, & Wendel, 2010; Middleton et al., 2013). There are few rules to guide the design of health IT, no mandates for the use of HFE principles in design and implementation5, and no testing is required to demonstrate that the design of the health IT supports clinicians’ cognitive work (e.g., providing adequate situation awareness for patient care while minimizing mental workload and maximizing efficiency). This is in contrast to medical devices that have strict regulations and controls imposed by the Food and Drug Administration (ANSI/AAMI HE75:2009ANSI/AAMI HE75:2009; Weinger, Wiklund, & Gardner-Bonneau, 2011). Not surprisingly then, health IT, while improving the quality and safety of patient care, has also introduced new sources of error that are directly related to design and implementation deficits (Koppel et al., 2005; Magrabi, Ong, Runciman, & Coiera, 2010; Wetterneck et al., 2011) that could be proactively identified and solved by a macroergonomics approach.
Macroergonomic approaches to the design and implementation of health IT can address many of the challenges and problems described above. Macroergonomic principles for implementation are discussed in section 4.1; here we focus on macroergonomic design of health IT. First, it is important to understand the diversity of technology users. For instance, a smart IV pump is used by anesthesiologists who administer medications during surgery, by nurses who administer IV medications to patients in the unit and by biomedical engineers who maintain and fix the pumps. Our research has shown different HFE challenges experienced by anesthesiologists and nurses in their use of smart IV pump technology (Carayon, Hundt, & Wetterneck, 2010; Carayon et al., 2005; Schroeder, Wolman, Wetterneck, & Carayon, 2006). For instance, a design flaw of the smart IV pump led to a medication overdose when used by an anesthesiologist in the high time-pressure environment of the operating room (Schroeder, Wolman, Wetterneck, & Carayon, 2006). On the other hand, nurses were primarily affected by the efficiency problems associated with that same smart IV pump technology (Carayon, Hundt, & Wetterneck, 2010). The different users—who will also sometimes include patients or families (Or & Karsh, 2009)—have different expectations and needs, and work in very different work systems that may affect technology use. Another example is tools used to document patient encounters in the EHR. Pre-designed templates can speed documentation; however, these templates need to be customized to the physician specialty and patient appointment type (e.g. consultation, yearly physical exam, or progress notes). Some clinicians may not type well and need to supplement manual documentation with dictation.
Second, patient care involves multiple individuals who often collaborate to make decisions regarding treatment. Therefore, from a macroergonomic viewpoint, health IT needs to be designed to fit the needs of individual users as well as the needs of teams (IOM, 2012; Reddy, Gorman, & Bardram, 2011; Wears, 2008). This is especially important in primary care with the emphasis on patient-centered medical homes (Nutting et al., 2009). The medical home model calls for health IT to support the work of physician-led teams in clinics that include physicians, mid-level providers, nurses, medical assistants, receptionists and social workers. The health IT should allow multiple team members to safely access the patient record at the same time, allow for easy information sharing and electronic communication between team members and the patient, and also have tools for the team to care for populations of patients to monitor the quality of care delivered.
Third, the technology needs to be integrated in the workflow both temporally and spatially, and at multiple levels (Carayon et al., 2010). Work flows through patient visits between the physician and the patient (intra-visit). Work flows between specialists at different clinics or from the hospital setting to the primary care clinic (inter-organizational). Work flows between members of a clinic team, for example, in the patient-centered medical home described above (microsystem/intra-clinic flow). Work also flows in the mind of clinicians, for example, while assessing a patient complaint and determining the diagnosis and course of action (cognitive workflow). All of these workflows must be supported by the design and implementation of health IT (Hoonakker, Khunlertkit, Tattersall, Keevil, & Smith, 2012; Horsky, Kaufman, Oppenheim, & Patel, 2003).
3.4 Violations and Patient Safety
HFE has contributed to patient safety efforts in many ways (Carayon, Xie, & Kianfar, 2013), particularly in the quantification and understanding of medical errors and their contribut ing factors (Flin, Winter, Sarac, & Raduma, 2009; Gosbee, 2002; Reason, 2000). Far less attention has been paid to the occurrence and causes of intentional safety violations that affect patient safety largely independent of unintended errors (Amalberti, Vincent, Auroy, & de Saint Maurice, 2006). In the context of patient safety, safety violations (or workarounds) have been defined as deliberate acts that deviate from “rules and standards” (Amalberti, Vincent, Auroy, & de Saint Maurice, 2006, p. i66) or “established protocols of practice” (Phipps et al., 2008, p. 1626), or acts that break “rules, policies, protocols or procedures” (Alper et al., 2012, p. 408). Some note that safety “rules” in health care are incredibly varied, ranging from broad or contested guidelines, to exact and widespread procedures, to institution-specific policies and informal norms, to diagnostic or therapeutic “orders” (Amalberti, Vincent, Auroy, & de Saint Maurice, 2006; de Saint Maurice, Auroy, Vincent, & Amalberti, 2010; Phipps et al., 2008). Whether safety violations refer to rules that are intended to promote safety or actually do promote safety is also unclear. Therefore, in addition to safety rule violations that resemble those in other industries (e.g., the use of personal protective equipment), macroergonomics research in health care has explored guideline (non)compliance (Gurses et al., 2008), deviation from written procedures and the overriding or working around of alarms, alerts and safety technologies (Hoonakker, Wetterneck, Carayon, Cartmill, & Walker, 2011; Koppel, Wetterneck, Telles, & Karsh, 2008; Schultz, Carayon, Hundt, & Springman, 2007).
A key finding emerging from early work on patient safety violations is that, like errors, violations are shaped by an array of interacting “latent” factors representing many aspects and levels of the sociotechnical work system (Alper & Karsh, 2009; Lawton et al., 2012; Phipps et al., 2008). For example, studies in anesthesiology (Beatty & Beatty, 2004; de Saint Maurice, Auroy, Vincent, & Amalberti, 2010; Phipps et al., 2008) reveal reasons for safety violations related to the violated rule, the worker, including worker perceptions (Phipps, Parker, Meakin, & Beatty, 2010), and various organizational factors including time pressure, goal conflict, resources and equipment design. These studies, as well as studies in surgery (R. McDonald, Waring, & Harrison, 2006), intensive care nursing (Drews, Wallace, Benuzillo, Markewitz, & Samore, 2012), and pediatric nursing (Alper et al., 2012) also demonstrate that various factors interact to promote violations. For example, a survey of 199 nurses in two pediatric hospitals showed that medication administration process violations depended on a combination of the situation (routine vs. emergency), setting (medical/surgical vs. oncology unit) and task (checking patient identification vs. documenting administration) (Alper et al., 2012). Violation reports were highest for emergency situations, rather than for routine operations, highest by hematology-oncology-transplant unit nurses, followed by PICU nurses and then medical/surgical unit nurses, and highest during patient identification checking, followed by matching a medication to a medication administration record, and then documenting an administration.
Several studies also highlight the multifactorial and often combinatorial effect of macroergonomic factors such as policy-workflow incompatibility, inadequate staffing, and the physical environment (noise, layout) on violations of the policy for the use of barcoded medication administration technology (Koppel, Wetterneck, Telles, & Karsh, 2008; Schultz, Carayon, Hundt, & Springman, 2007). Violations – including the overriding or disabling of alerts and alarms – are commonly reported across settings and technologies and appear to be shaped by a combination of macroergonomic factors (Karsh, 2009; Miller, Fortier, & Garrison, 2011; Niazkhani, Pirnejad, van der Sijs, & Aarts, 2011; Saleem et al., 2011; Trbovich, Pinkney, Cafazzo, & Easty, 2010). See section 5.3 for the description of a study of CPOE drug alert overrides that led to duplicate medication ordering errors and the work system factors that contributed to the overrides and the ordering errors (Wetterneck et al., 2011).
One of the crucial questions facing healthcare violations researchers and healthcare organizations is the extent to which all rules are “good” and violations are “bad.” Although violations may increase risk (Reason, Parker, & Lawton, 1998) and sometimes become implicated in high-profile medical incidents (e.g., Smetzer, Baker, Byrne, & Cohen, 2010), studies demonstrate that some violations are necessary or are seen as necessary at the time to the healthcare worker to accomplish the work to be done (Halbesleben, Wakefield, & Wakefield, 2008; Phipps et al., 2008); and that some rules are well-intentioned but may not have a net positive impact on patient safety (Dierks, Christian, & Roth, 2004). In coming decades, the focus on error reduction will probably show greater interest in both adaptation/resilience (Patterson et al., 2006; Reason, 2008) and standardization/rule enforcement (Runciman, Merry, & Walton, 2007), two seemingly contradictory approaches that may need to be carefully balanced (Cook & Rasmussen, 2005; Lawton & Parker, 1999).
3.5 Care Coordination Across the Continuum of Care
Transitions of care occur within a healthcare organization (e.g., shift change, transition from ICU to general care unit) and between healthcare organizations (e.g., transfer of care from hospital to primary care setting), and are a particularly vulnerable time period for patient safety (Jencks, Williams, & Coleman, 2009; K. M. McDonald et al., 2010; van Walraven et al., 2011). Poor communication is a major cause of transition safety problems, and interventions to support communication, such as checklists or use of different handover communication tools (e.g., SBAR, structured discharge summaries), have been remedial to some extent (Hesselink et al., 2012; McCulloch, Rathbone, & Catchpole, 2011; Morey et al., 2002). However, by using a macroergonomics approach, it becomes clear that improving communication is necessary but not sufficient to improve safety of care transitions; many other work system factors also play a role (Patterson & Wears, 2010). For example, a study investigating patient handoffs from cardiac operating rooms (ORs) to intensive care units using a macroergonomics approach identified many work system factors that are potentially responsible for unsafe care transitions (Gurses et al., 2012):
physical environment: narrow hallways from ORs to the ICU made it hard to maneuver the patient bed
tasks: incorrect task prioritization by the receiving ICU nurse who performed non-urgent tasks during the handoff report
tools/technologies: the use of different brands of infusion pumps in ORs and ICUs led to a complete changeover of medications and the pump as part of the care transition
organization: anesthesiologists prepared their own medications while nurses used only pharmacy-prepared medications, leading to drug waste and increased potential for medication errors during care transitions
individual: a receiving intensivist who insisted on sitting in front of a computer rather than coming near the bedside to hear the full handoff report.
A macroergonomic viewpoint on transitions of care examines both positive and negative contributions to patient safety. Whereas emphasis has been put on the hazardous nature of care transitions (Arora et al., 2009), care transitions can also be opportunities for re-evaluation of care decisions, review of patient care and discussion among clinicians, and another ‘pair of eyes’ providing a different perspective (Cooper, Long, Newbower, & Philip, 1982; Perry, 2004; Wears et al., 2003). This macroergonomic systems approach to care transitions can enhance interventions aimed at improving care coordination.
4. MACROERGONOMICS IN HEALTHCARE SYSTEM DESIGN
This section addresses the question of how to implement macroergonomics in health care and how to use macroergonomics to improve system design. According to Emery and Trist (1965), work system design must be compatible with the workers in the system and the external environment in a way that results in optimal outcomes (worker well-being and system performance). Hendrick (1991), through a longitudinal assessment of organizations, identified three organizational pitfalls that translated into criteria for effective work system design. One criterion relates to joint design, i.e. the work system design must be human-centered, and therefore jointly optimized between human and technological systems (Cherns, 1976). The second criterion addresses a humanistic approach to task allocation where the designers should first consider whether or not it is necessary for a human to perform a task before assigning the task to a human or technology (Cherns, 1976). The final criterion emphasizes the sociotechnical system; the designer should use a systematic methodology to analyze the sociotechnical system and integrate the findings into the work system’s design (Cherns, 1976).
4.1 Healthcare System Design and Redesign
An increasing body of research addresses healthcare system redesign. Healthcare system redesign consists of a series of inter-related steps (Carayon, 2003): (1) analysis of work system design, (2) implementation of redesigned work system, and (3) operation and continuous improvement of redesigned work system. In this section, we focus on implementation and continuous improvement; examples of tools for analyzing work systems are described in section 5.2.
Knowledge exists about characteristics of work systems and processes that affect patient safety and healthcare quality and that can be used in healthcare system redesign. However, such knowledge is not systematically applied. This underlies the need for translational research and research on the implementation and dissemination of healthcare interventions (Woolf, 2008). Macroergonomics has long addressed similar concerns regarding implementation and dissemination (see Table 1 for implementation as a key element of macroergonomics).
Participatory ergonomics is one approach developed to facilitate the implementation of HFE interventions or system changes (Noro & Imada, 1991; Wilson, 1991). Participatory ergonomics allows users of ergonomics (e.g., nurses, patients) to take an active role in the identification and analysis of ergonomic risk factors as well as the design and implementation of ergonomic solutions. Participatory ergonomics can be used in conjunction with other macroergonomic methods such as MEAD (MacroErgonomic Analysis and Design) and MAS (Macroergonomics Analysis of Structure) (Kleiner, 2007) (see section 5.2). Evanoff and colleagues have conducted one of the few projects on participatory ergonomics in healthcare (Bohr, Evanoff, & Wolf, 1997; Evanoff et al., 1999). One study examined the implementation of three participatory ergonomics teams in a medical center: a group of orderlies from the dispatch department, a group of ICU nurses, and a group of laboratory workers. Overall, the dispatch and laboratory team members were satisfied with the participatory ergonomics process, and these perceptions improved over time. However, the ICU team members expressed more negative perceptions of the participatory process because of the lack of time and the time pressures of clinical demands. The studies by Evanoff and colleagues demonstrate the feasibility of implementing participatory ergonomics in healthcare, and highlight the difficulty of the approach in a high-stress, high-pressure environment, such as an ICU.
At the stage of healthcare system implementation, it is important to consider evidence-based principles for implementation of sociotechnical change (see Table 5) (Karsh, 2004).
Table 5.
Macroergonomic Principles for Implementation (Karsh, 2004)
| Implementation Design Principles | Reason for Importance |
|---|---|
| Top management commitment | Enables additional design principles. |
| Responsibility/accountability | Effective in promoting success because it shows the importance of the change and lets end users know who to go to with ideas or concerns |
| Structured program | Provides end users with a “road map” which can reduce uncertainty and promote feelings of control. Reduces many of the fears associated with new system: end users will know why the change is coming, what to expect, when to expect it, where to expect it to happen and who will be in charge. |
| Training | Targets self-efficacy, ease of use, and usefulness explicitly. Reduces uncertainty and fear and promotes control because users gain knowledge and skills. |
| Pilot testing | Involves users with the new system and creates a test bed to uncover and solve problems. Promotes an understanding of integration needs. |
| Communication | Early and clear communication about intentions begins to reduce uncertainty and promotes perceptions of procedural justice. Clear and open communication channels are needed between prospective end users, decision makers and technical support. |
| Feedback | Feedback on end user concerns and ideas must be provided quickly so that they know they are being taken seriously, e.g., staffing a help desk with knowledgeable staff at all times when people are engaged in using the new system. |
| Simulation | Use before, during, and after an implementation promotes predictions, self-efficacy, usefulness, intervention validation, ease of use and control while reducing the variety of fears that can exist. |
| End user participation | Enhances perceptions of justice, self-efficacy and control, reduces a variety of fears and uncertainty. May have both cognitive and motivational components. |
The last stage of healthcare system (re)design involves a continuous system adaptation and improvement process (Carayon, 2006) that relies on several principles, including active participation of clinicians and patients in system design and redesign activities (e.g., participatory ergonomics), individual and organizational learning (see section 4.3), and sense-making6 of on-going system changes and their impact on care processes and outcomes.
4.2 Usability in the Organizational Context
ISO 9241 defines usability as “the extent to which a product can be used by specified users to achieve specified goals with effectiveness, efficiency and satisfaction in a specified context of use” (International Standards Organization, 1998). One must keep in mind that “products” are not restricted to a device or technology as is frequently the focus. User manuals (Ginsburg, 2005) and other documents and tools designed to aid users are all too frequently overlooked during the design and development phases and negatively affect users due to poor usability.
Usability in health care is rapidly gaining attention (Middleton et al., 2013). Karsh (2004) states that macroergonomics offers an additional perspective on usability and proposes incorporating usability with the science of technology design and implementation. Although Nielsen’s (1993) facets of usability – learnability, memorability, efficiency, satisfaction and freedom from error – should not be overlooked in the design of devices and technology, usability also plays a significant role in the continuous implementation process described in the previous section (Carayon, 2006) due to its longitudinal impact on workflow (Carayon, 2009) and user satisfaction (Murff & Kannry, 2001). For instance, even one to three years after BCMA (Bar Coding Medication Administration) technology implementation, usability issues emerged that affected safe use of the technology by nurses (Carayon et al., 2007). A series of 62 direct observations of medication administration by nurses using BCMA technology in one hospital identified a range of technology problems (e.g., automation surprises) as well as working conditions (e.g., interruptions) that could potentially affect the safety of medication administration.
Health IT implementations have often failed, in large part because of the lack of sufficient attention to the facets of health IT usability and a poorly planned implementation process (Connolly, 2005). Likewise there are documented compromises in patient safety related to health IT (Institute of Medicine, 2012). A macroergonomics perspective provides a framework for performing usability evaluations throughout an implementation. In the context of planning for the introduction of a health IT and assessing its impact on workflow assessment, usability should be incorporated in every step of the design life cycle (Yen & Bakken, 2012):
from identifying and describing system requirements,
to procurement (Ginsburg, 2005),
throughout the system development process (including iterative design, workflow analysis and the development of training systems),
to post-implementation evaluation of the design on error, user satisfaction and efficiency (both the short- and long-term).
By incorporating usability assessments in the pre-implementation phases, the costs of redesign associated with outright costs to a vendor as well as costs associated with time and dissatisfaction can be significantly reduced (Schumacher, Webb, & Johnson, 2009). Usability should also be incorporated with the continuous improvement/technology implementation processes as errors and inefficiencies associated with a technology may be addressed and mitigated once they are carefully evaluated. Outputs of usability assessments can provide valuable information for redesigning and improving workflows and systems.
Usability can also be incorporated in a macroergonomic proactive risk assessment (Carayon, Faye, Hundt, Karsh, & Wetterneck, 2011; Faye et al., 2010). Since workflow assessment is one component in many common risk assessment methods, including Failure Mode and Effects Analysis (FMEA), it is logical to incorporate a technology’s design – and an evaluation of its usability – in the risk assessment (Wetterneck et al., 2006). Recommendations for changes that require modifications to workflows, technology design and training programs addressing the use of the technology can all occur as a result of a macroergonomic risk assessment (Hundt et al., 2013).
4.3 Organizational Learning and Resilience
In this section we describe how two macroergonomic approaches complement each other. One, organizational learning, provides a foundation, and the other, resilience, expands our understanding of the worker’s role and adaptive ability to contribute to safe work systems. Better understanding these concepts should facilitate macroergonomic system design and redesign efforts in healthcare.
Organizational learning occurs when what has been learned from experience – both within and outside an organization – is applied to current and future actions and decisions (Argyris & Schon, 1978). This may happen at a macro- or micro-system level but what is important is that, by applying learning, the system is capable of creating safer systems and avoiding or responding to safety incidents and errors constructively, rather than reactively (Hundt, 2012). This can then contribute to resilience in a system where people are recognized as being capable of and then allowed to adapt to deviation from the norm regardless of whether or not the deviation was foreseen (Hollnagel, 2011). People acknowledge and meet sociotechnical system demands by applying experience, policies and procedures and human capacity associated with adaptability to varying situations. They are proactive and detect events before they occur; or promptly respond to and correct events without extreme disruption to the system (Hollnagel, Woods, & Leveson, 2006). Both hindsight and foresight are necessary for resilience in systems (Woods & Cook, 2001) where humans are seen as assets that serve as the primary contributors to system resilience. Resilience also focuses on positive outcomes occurring despite known or inherent weaknesses in system design (Hollnagel, Woods, & Leveson, 2006).
Healthcare provides a work system that is highly dependent on the expertise, judgment and vigilance of the workers, including the clinicians providing care and the patients receiving it. In healthcare, organizational learning can lead to resilience in areas such as error recovery systems. Healthcare workers are aware of the potential for errors and can recognize and recover from such errors either before harm occurs or immediately afterwards when they rescue the system, including the patient, from worse harm. Much like how resilience builds upon our understanding of organizational learning, error recovery systems complement and go beyond policies and procedures that organizations put into place to prevent errors from occurring (Wetterneck, 2012).
As described by Hundt et al. (2006), the continuous implementation of a smart IV pump demonstrated many characteristics of resilience and learning. After a serious event occurred (Schroeder, Wolman, Wetterneck, & Carayon, 2006), and was effectively managed in the short term due to the quick actions of clinicians, the FMEA team that had identified potential pump vulnerabilities prior to the pump’s implementation (Wetterneck et al., 2006) took on the role of leading the incident analysis and effectively managed the event for the long-term by working with the manufacturer to redesign the IV pump (Carayon, Wetterneck, Hundt, Rough, & Schroeder, 2008). Ongoing training programs and feedback to clinical staff who used the pumps emphasized staff vigilance and resilience. Not only did the organization learn from the incident but, through publications and reporting to the Food and Drug Administration MAUDE (Manufacturer and User Facility Device Experience) database, other organizations also had the opportunity to learn from the event. Further examples of using macroergonomic risk assessment to promote organizational learning are reviewed elsewhere (Carayon, Faye, Hundt, Karsh, & Wetterneck, 2011; Hundt, 2012). Applying macroergonomic concepts to promote organizational learning and resilience offers significant promise for continued efforts to increase patient safety and quality at all levels of care.
5. IMPLICATIONS FOR METHODOLOGY AND PRACTICE
This section describes three major implications of macroergonomics for healthcare quality and patient safety: (1) the roles of macroergonomic practitioners in healthcare organizations, (2) macroergonomic methodologies that can be used in healthcare practice, and (3) macroergonomic research approaches and the importance of mixed methods research.
5.1 Macroergonomic Practitioners for Healthcare
Macroergonomic practitioners can play important roles in improving healthcare quality and safety (Carayon, 2005). Macroergonomic practitioners could be either HFE consultants or employees of healthcare organizations. Table 6 provides specific examples of hospital departments or areas that macroergonomic practitioners can contribute to with their unique set of skills and knowledge.
Table 6.
Examples of Macroergonomic Practitioners’ Roles in a Hospital
| Departments/Areas | Expertise | Project Examples |
|---|---|---|
| Risk management | Medical accident investigation | Work system analysis to identify all system factors that played a role in the accident |
| Risk management | Proactive risk assessment | Proactive risk assessment of hospital discharge process to reduce readmissions |
| Information Technology | Health IT design, implementation and evaluation | Managing the implementation of and evaluation of the impact of EHR systems on the entire work system |
| Clinical engineering | Proactive assessment of medical device, impact of procurement decisions on the work system | Proactive evaluation of smart IV pump technology implementation |
| Quality and patient safety | Large-scale change, safety culture | Safety culture evaluation and improvement efforts, use of participatory ergonomics approach |
| Infection control and prevention | (Re)designing work system to improve compliance with evidence based guidelines | Redesigning the work system (e.g. location of sinks and alcohol gel, increasing awareness, individualized feedback mechanisms) to improve compliance with hand hygiene guidelines |
| Facility management | Physical ergonomics; layout design; participatory ergonomics | Renovation of a clinical unit |
| Various clinical units | HFE; change management | Support to local change efforts, such as interdisciplinary rounds or hand hygiene |
Healthcare macroergonomic practitioners need graduate-level education in HFE with a specialization in macroergonomics. Ideally, during their formal education they will be exposed to varied healthcare settings, work on projects and/or conduct their thesis research in the domain of healthcare and gain further experience in healthcare after completing graduate school. Depending on their interests, macroergonomic practitioners may want to gain additional training in epidemiology, public health, medical informatics and/or health services research through short courses or certificate programs. In addition to broad HFE knowledge, they should develop knowledge of healthcare context and culture (e.g., evidence-based medicine), skills in multidisciplinary teamwork, ability to deal with uncertainty and ambiguity, communication skills, in particular communication with top management, and knowledge and skills in leadership and change management (Carayon, 2010; Carayon & Xie, 2011). Healthcare macroergonomic practitioners can also benefit from education and/or experience in other domains; this could add to their broad and deep understanding of the fundamental work system issues that impact system performance and worker well-being.
Barriers exist to increasing the recruitment of macroergonomic, and more generally HFE, practitioners in healthcare, including the organizational culture and awareness of the healthcare community. Clinicians should, but do not always, recognize that improving quality and safety requires input and expertise of various disciplines, and that a single discipline will not be able to solve the complex and challenging problems in healthcare. Integration of macroergonomics (and more generally HFE) in healthcare organizations requires a deep understanding of commonly held values and beliefs in health care (Carayon & Xie, 2011). The healthcare culture can be characterized on the following dimensions: scientific inquiry or evidence-based medicine, individual responsibility for care, autonomy and excellence (Carroll & Quijada, 2007; M. A. Smith & Bartell, 2007). Three scenarios emerge when examining the fit between these cultural values and macroergonomics values (Carayon & Xie, 2011) including: (1) some values fit with each other, (2) some values conflict with each other and (3) some values need to be adapted. For instance, the systems approach is key to macroergonomics (see Table 1 and models in section 2). This may conflict with the healthcare value of individual (i.e., physician) responsibility for care. If an error occurs, those in health care are likely to look for the person responsible for the error, whereas the macroergonomist will look for the system factors that contributed to the error. The drive for excellence in health care can help support macroergonomic interventions aimed at improving work systems, processes and outcomes; this would represent a benefit of the commonly held value of excellence for encouraging work system redesign. Macroergonomic practitioners in health care should be aware of the cultural differences and similarities between healthcare and macroergonomics.
5.2 Macroergonomic Systems Approach in Healthcare Practice
To implement the work system design process, tools and methods need to be used for each of the different steps (Carayon, 2012b; Carayon, Alvarado, & Hundt, 2003; Carayon, Alvarado, & Hundt, 2007). In the analysis phase several HFE methods can be used, such as macroergonomic proactive risk assessment (Carayon, Faye, Hundt, Karsh, & Wetterneck, 2011), work sampling (Carayon, Smith, Hundt, Kuruchittham, & Li, 2009), process analysis (Schultz, Carayon, Hundt, & Springman, 2007), variance analysis (Hallock, Alper, & Karsh, 2006; Hamilton-Escoto, Hallock, Wagner, & Karsh, 2004), and analysis of work system barriers and facilitators (Gurses & Carayon, 2007a). Many of these methods can also be applied to identify solutions for work redesign. Other HFE tools can be used to design solutions, such as task allocation methods and simulation (Carayon, 2012b). MEAD (MacroErgonomic Analysis and Design) and MAS (Macroergonomics Analysis of Structure) (Kleiner, 2007) are macroergonomic methods that cover multiple steps of the work system design process. More information on general macroergonomic methods can be found in Stanton et al. (2004).
Macroergonomists rely on a range of analytic tools and methods to analyze work systems, and adapt them to ensure that all work system elements, including the organizational and sociotechnical context, are considered. For instance, various methods such as FMEA have been developed to analyze vulnerabilities of high-risk processes. Macroergonomists have adapted these proactive risk assessment methods to analyze system vulnerabilities in IV medication administration (Wetterneck et al., 2006), medication management by ICU nurses (Faye et al., 2010) and patient transfer from operating room to ICU (Hundt et al., 2013). These adaptations are based on the SEIPS model (see Figure 1) (Carayon et al., 2006), rely on various data collection methods (e.g., observation, archival data analysis) to identify and characterize process vulnerabilities, and use a participatory process to ensure stakeholder representation in the analysis and redesign of the process (Carayon, Faye, Hundt, Karsh, & Wetterneck, 2011).
In order to analyze and (re)design a work system, all work system components and processes have to be considered (see Figures 1 and 2). The Macroergonomic Analysis and design of a work system’s Structure (MAS) proposes to analyze the three major sociotechnical system components separately: (1) the technological subsystem, (2) the personnel subsystem and (3) the external environmental characteristics. Technological subsystem analysis determines task variability (the number of exceptions encountered in one’s work) and the task analyzability (the procedures one has available for responding to task exceptions) (Perrow, 1967). Personnel subsystem analysis determines the professionalism and psycho-social characteristics of the workforce. External environment analysis determines the organization’s ability to adapt to the external environment, such as standards, legislation, and characteristics of the healthcare workforce. The separate analyses of the organization’s subsystems provide guidance about the structural design for the work system. In general, healthcare systems can be characterized by a technological subsystem with high analyzability and variability; by a personnel subsystem with a highly educated and trained workforce, which will allow for employee discretion; and by an external environment that is characterized by high complexity and uncertainty, which requires the work system to have relatively low vertical differentiation, decentralized decision making, low formalization and a high level of professionalism among its work groups.
At the core of the sociotechnical or macroergonomic work system analysis is variance analysis (Pasmore, 1988). The goal of the variance analysis is to determine the causes of the difference (variance) between the ideal state of an organization and its actual state (reality) and the work system factors that affect the variance. A variance analysis of the diagnostic testing process was conducted in a healthcare organization with 30 outpatient clinics (Hallock, Alper, & Karsh, 2006). Data were collected using a series of 38 interviews of physicians, clinic managers, medical assistants and other staff in six of the 30 clinics. The data collection was iterative: concurrent data analysis identified the need to collect data from additional clinics or people. The following tools were used to analyze the data: process flowcharts, variance matrices, key variance control tables and a process comparison chart. A total of 36 variances was identified that occurred across or influenced various stages of the process. For instance, lack of availability of the patient chart affected visit preparation as the results were not available. Most variances occurred at the interfaces between systems (e.g., clinic-laboratory interface) and were related to poor or absent feedback structures (e.g., lack of physician notification about test result). This variance analysis produced multiple system redesign recommendations to improve the timeliness of the diagnostic testing process and, therefore, patient safety. Variance analysis is one type of macroergonomic work system analysis tools. It is often used in the context of a larger analysis process, such as MEAD.
The MacroErgonomic Analysis and Design (MEAD) framework (Hendrick & Kleiner, 2001, 2002) is a method adapted from sociotechnical system analysis methodology (Emery & Trist, (1978) and is used to assess work processes. MEAD is characterized by 10 phases, including variance matrix analysis, role network analysis and function allocation and joint design. Each MEAD phase is defined by several steps. For example, the Initial Scanning phase is performed in 4 steps: (1) mission, vision, principles (MVP) analysis; (2) system scan; (3) environmental scan; and (4) initial organizational design dimensions specifications. The goal of these 4 steps is to analyze the variance between what the organization professes as its defining characteristics and its identity as shown in actual behavior. For example, analysis of the MVP of a nursing home can indicate that it focuses on patient care, but due to understaffing, the nurse-patient ratio may be well below the required rate (Kleiner, 2011, p. 83). A healthcare application of MEAD in a nursing home can be found in Kleiner (2007). MEAD has similarities with other design processes such as the 12-step ergonomics design process (Wilson, 1995), the structured work redesign process with 8 phases (Parker & Wall, 1998) and the 10-step work system analysis (Karsh & Alper, 2005). Most work system design processes are characterized by an analysis phase, synthesis phase, evaluation phase and feedback/continuous improvement.
5.3 Macroergonomics Research Approach in Healthcare Quality and Patient Safety
Using a macroergonomics approach to address problems in healthcare delivery requires multiple research methods to fully evaluate the work system and its impact on care processes and outcomes (Carayon et al., 2006). This takes into consideration the complex, dynamic nature of the healthcare system and the understanding that change in any one part of the healthcare system will impact all parts of the system. Interventions to improve healthcare tend to be multi-faceted and multi-targeted (Campbell et al., 2000; Shcherbatykh, Holbrook, Thabane, & Dolovich, 2008). Change management principles highlight the importance of a holistic, systems approach to implementing and evaluating change, and the need to pay attention to all system levels (Holden, Or, Alper, Rivera-Rodriguez, & Karsh, 2008; Karsh & Brown, 2010) (see Table 5). Understanding the full effect of a macroergonomic intervention requires the evaluation of the intervention outcome, the context (i.e. work system) in which it was implemented and the process used to implement it (see Figure 1). The importance of using multiple methods in research and best practices for doing so has also been emphasized by the National Institutes of Health in its recent report on mixed methods research (Creswell, Klassen, Plano Clark, & Smith, 2011). Therefore, the use of multiple methods in macroergonomics research is in line with current recommendations for healthcare research.
Mixed methods research is defined as, “research in which the investigator collects, analyzes, mixes and draws inferences from both quantitative and qualitative data in a single study or a program of inquiry” (Tashakkori & Creswell, 2007, p.4). Qualitative methods, such as patient and clinician interviews (e.g., Carayon et al., 2011b; Holden, 2011), clinician focus groups (e.g., Faye et al., 2010), and qualitative observations of tasks (Carayon et al., 2007; Gurses et al., 2012), can help us develop a better understanding of work systems and processes, create research hypotheses, and better inform researchers to further explore the context or setting in which an intervention takes place. Quantitative methods, including clinician surveys (e.g., Hoonakker, Cartmill, Carayon, & Walker, 2011), quantitative observations such as time study (e.g., Douglas et al., 2012) or experiments such as a randomized controlled trial to improve patient outcomes, allow us to test hypotheses and state whether an intervention “worked” based on the desired outcomes. Importantly, using multiple methods allows triangulation of research findings and the integration of the results of the investigations, emphasizing the strengths of each method to inform and answer research questions (Newman & Benz, 1998).
Multiple macroergonomic studies have used mixed methods research. Gurses and Carayon (2009b) used interviews to identify the work system performance obstacles and facilitators experienced by 15 ICU nurses. The qualitative interview data were analyzed using content analysis and served as input to construct a questionnaire, which was then distributed to nurses in 17 ICUs in Wisconsin (Gurses & Carayon, 2007a). The survey of 265 ICU nurses helped to quantify performance obstacles and assess their impact on ICU nurses’ workload, stress and perceptions of quality and safety of care (Gurses, Carayon, & Wall, 2009). Using structural equation modeling, we showed that perceived workload mediated the impact of performance obstacles (e.g., poor physical environment, dealing with many family-related issues), with the exception of equipment-related issues, on perceived quality and safety of care and fatigue and stress.
To evaluate why duplicate medication ordering errors increased after implementation of a CPOE system with clinical decision support, Wetterneck et al. (2011) triangulated data from physician and nurse task analyses, clinician surveys, analysis of meeting minutes, a heuristic evaluation of the computer interface and medication error reports. Using the SEIPS model (see Figure 1), researchers identified a range of work system factors that contributed to the increase in duplicate medication ordering errors. For instance, survey data showed that ordering providers were neutral about the usefulness of duplicate medication alerts for identifying problems with medication orders and for helping them correct a problem with a medication order. Medication error reports provided data on how the organization of ICU rounds contributed to duplicate medication orders; 23% of the duplicate orders were entered during patient rounds. Our direct observations confirmed that, during rounds post CPOE implementation, multiple providers were working on various tasks simultaneously in a loosely coordinated manner on different computers.
As these examples demonstrate, by using multiple data collection methods and various mixed methods research designs (e.g., sequential design with interviews providing input in a survey, triangulation of data from multiple methods), macroergonomists are able to systematically assess work systems in health care. This understanding includes recognition of the challenges and opportunities a system functions under and greatly enhances the identification of means for improving the system.
6. IMPLICATIONS FOR THEORY
Research in macroergonomics in healthcare quality and patient safety needs to clearly demonstrate its value, i.e. its impact on the IOM quality aims (see section 1.1). Therefore, the next section describes some of the mechanisms for linking macroergonomics to care processes and patient outcomes. In the final section, we highlight promising areas of research for macroergonomics in healthcare quality and patient safety.
6.1 Research Linking Macroergonomics and Care Processes/Patient Outcomes
While conducting macroergonomics research in health care, it is important to keep in mind that the ultimate goals are to improve care processes and well-being and performance outcomes [patient, family, clinician and organizational outcomes] (Carayon et al., 2006). Macroergonomics research should have a clear link to care processes and outcomes. This will increase acceptance of and attention to macroergonomics, and accelerate its adoption within health care.
There are only a limited number of studies of what can be defined as “macroergonomics interventions” to improve patient outcomes. One of these, the Central Line Associated Bloodstream Infections (CLABSI) Project, used a collaborative, participatory research approach to reduce CLABSIs initially in one ICU (Berenholtz et al., 2004). A multi-component intervention was designed to address several factors in the ICU work system: (1) education about central line insertion and maintenance, (2) creating a central line insertion cart to make it easy for care physicians to access all the needed supplies, (3) implementing a central line insertion checklist to be completed by a nurse while the line is inserted, (4) empowering nurses to stop the procedure if there is a violation in guideline compliance, and (5) daily assessment of whether a central line can be removed. Next, 108 Michigan ICUs implemented a further developed version of the intervention including the 5 original interventions and additional work system interventions such as implementing a comprehensive unit-based safety program to improve the safety culture, training ICU team leaders on the basics of HFE and safety science, and providing monthly and quarterly feedback to each participating site on CLABSI rates (Pronovost et al., 2006). This study reduced the CLABSI rates to a median of zero in 108 Michigan ICUs (Pronovost et al., 2006). When studying the components of this initiative, it becomes obvious that the principles of macroergonomics have been incorporated in the methods used and interventions developed and implemented in this collaborative. Another example of macroergonomic intervention study is the use of MEAD to reduce HAIs in dialysis procedures (Kleiner & Lewis, 2012).
In addition to studies that provide support for the importance of a macroergonomics approach in designing interventions aimed at improving clinical outcomes, there is a considerable need for high-quality studies describing the relationships among work system factors, care processes and outcomes using a macroergonomics approach. We need to build this knowledge base so that appropriate and effective work system interventions and quality improvement efforts are designed and implemented. For example, Gurses and colleagues (2008) investigated compliance with evidence-based guidelines in ICUs using a macroergonomics approach. Their qualitative research found that reducing ambiguity in work systems (ambiguities in responsibilities, tasks, methods, expectations, exceptions) can be an effective strategy in improving compliance with evidence-based guidelines. Another example is the qualitative work conducted in 5 tele-ICUs by macroergonomists to identify aspects of the tele-ICU that affect processes and outcomes of care (Hoonakker et al., 2011; Khunlertkit & Carayon, 2012). Using semi-structured interviews of tele-ICU nurses, physicians and managers, they found that the tele-ICU contributed to care processes and patient outcomes through multiple work system pathways, such as the tele-ICU technology facilitating availability of extra resources for patient care (Khunlertkit & Carayon, 2012). This research describes the potential linkages and mechanisms between the tele-ICU work system and ICU care processes and patient outcomes. Future research could quantitatively assess and compare the contributions of various tele-ICU work system factors to ICU care processes and patient outcomes.
Theoretical development is needed to clarify and specify the specific mechanisms that link work system factors to care processes and patient outcomes (i.e. healthcare quality and patient safety). Initial work has been done to identify some of these mechanisms, such as the mediating roles of workload, efficiency and role optimization (Carayon, Alvarado, & Hundt, 2007). Further conceptualization will enhance the specificity of the SEIPS model and the ‘arrows’ linking the various elements.
Although the methods and principles of macroergonomics are crucial to improve health care processes and outcomes, they are only part of the solution. Healthcare problems are complex and require input and expertise from other disciplines and groups, including clinicians, health services researchers, epidemiologists, sociologists, organizational researchers, and informaticians. Hence, there is an urgent need to expand collaborations between macroergonomics and other disciplines in order to develop effective, efficient and sustainable solutions informed by the wisdom of interdisciplinary groups of researchers, and clinical and non-clinical practitioners (Gurses, Ozok, & Pronovost, 2012).
6.2 Promising Theoretical Developments in Macroergonomics in Healthcare Quality and Patient Safety
Given the breadth of healthcare quality problems, it can be challenging to identify promising areas for future macroergonomics research. This chapter has highlighted numerous research needs in macroergonomics in healthcare quality and patient safety that are summarized in Table 7.
Table 7.
Research Needs in Macroergonomics in Healthcare Quality and Patient Safety
| Relationship between worker outcomes and healthcare quality and patient safety, and the work system factors contributing to outcomes |
| Redesigning the healthcare work system to decrease job stress and workload and tosupport interruption management |
| Macroergonomic interventions and their impact on care processes and patient outcomes |
| Macroergonomics of patient-centered care |
| Balancing autonomy and resilience, and standardization and rule prescription |
| Macroergonomics of care coordination |
Further research on the relationship between worker outcomes (e.g., well-being, occupational safety and health) and healthcare quality/patient safety is clearly needed. We need to further understand the work system factors (or combination of work system factors) that contribute simultaneously to improving both worker and patient outcomes. We also need to understand potential conflicts between healthcare quality and worker outcomes. For example, redesigning the work system for increased efficiency (e.g., more effective supply chain management) may benefit healthcare workers: having easier access to supplies and equipment may decrease healthcare professionals’ workload and frustration and improve their job satisfaction. But, increasing efficiency in a care process may heighten work pressure experienced by healthcare workers. Further theoretical developments are necessary to understand the role of job stress in both worker outcomes and patient outcomes; this research will help to develop work system redesign interventions that can improve both worker and patient outcomes. Further research is also needed to link macroergonomic work system interventions to healthcare quality and patient safety (see section 6.1).
As suggested in section 3.2, there is little macroergonomics (and more generally HFE) research on the “work” of patients and family members. Understanding the system surrounding patients and the contribution of various system factors in helping patients manage their health and illness is an important research area.
Standardization has been proposed as a major principle for improving healthcare quality and patient safety (IOM, 2001). We need to consider the macroergonomic aspects of standardization, in particular what is standardized and how standardization is implemented (Carayon, Alyousef, & Xie, 2012). Standardization of patient rooms may help to support clinician performance to reduce cognitive effort needed to adapt to varying physical layouts (Reiling & Chernos, 2007). However, standardization may produce rules and policies that do not fit clinical workflow, therefore leading to violations (see section 3.4). Theoretical development is needed in this area, especially as standardization is strongly advocated as a systems engineering approach by the IOM (2001) and healthcare experts.
Finally macroergonomics research needs to examine the numerous challenges of care coordination (section 3.5). This is a particularly interesting theoretical area as care coordination problems occur across multiple healthcare organizations and at different system levels. Because of the multiple organizational structures and processes involved in care coordination, a macroergonomics approach that considers the broad organizational and sociotechnical context to healthcare quality and patient safety problems is particularly relevant. The macroergonomics research on care coordination will also contribute to our understanding of system levels and system interactions (Karsh & Brown, 2010; Waterson, 2009).
7. CONCLUSION
Macroergonomics has made significant contributions to healthcare quality and patient safety. Macroergonomic models of healthcare quality and patient safety are well-accepted by the healthcare community (Carayon, Xie, & Kianfar, 2013). Healthcare professionals and researchers are increasingly interested in learning about macroergonomics. Therefore, the potential impact of macroergonomics on improving care processes and patient outcomes is significant.
The macroergonomic lens on healthcare quality and patient safety provides major opportunities for the entire HFE discipline to make contributions to specific areas. Macroergonomics helps to put microergonomic issues in the larger organizational and sociotechnical context. Approaching healthcare quality and patient safety problems from a macroergonomic viewpoint can also increase the likelihood of HFE adoption by healthcare organizations, professionals and researchers (Carayon, 2010). If HFE is considered as an innovation (Greenhalgh, Robert, MacFarlane, Bate, & Kyriakidou, 2004), then macroergonomists, and more generally HFE practitioners and researchers, need to be aware of the factors that either hinder or facilitate the adoption and use of HFE by health care (Carayon, 2010).
Acknowledgments
This chapter is dedicated to Bentzi Karsh, a leader in macroergonomics research in health care. Bentzi contributed significantly to this chapter by influencing its focus and content. The work also reflects many of the insights Bentzi shared throughout his research career with us, his friends, colleagues and advisees. Sadly he passed away on August 18, 2012, shortly before we finished this chapter.
The manuscript was partially supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Rich Holden is supported by NCATS grant 2KL2TR000446–06 through the Vanderbilt Institute for Clinical and Translational Research (VICTR).
Biographies
Pascale Carayon, PhD, is Procter & Gamble Bascom Professor in Total Quality in the Department of Industrial and Systems Engineering and the Director of the Center for Quality and Productivity Improvement (CQPI) at the University of Wisconsin-Madison. She leads the Systems Engineering Initiative for Patient Safety (SEIPS) at the University of Wisconsin-Madison (http://cqpi.engr.wisc.edu/seips_home). She received her Engineer diploma from the Ecole Centrale de Paris, France, in 1984 and her Ph.D. in Industrial Engineering from the University of Wisconsin-Madison in 1988. Professor Carayon’s research focuses on macroergonomics, in particular in healthcare quality and patient safety, and aims at modeling, assessing and improving work systems (i.e. the system of tasks performed by individuals using various technologies in a physical and organizational environment) in order to improve system performance and worker well-being. Her research has been funded by the Agency for Healthcare Research and Quality, the National Science Foundation, the National Institutes for Health, the National Institute for Occupational Safety and Health, the Department of Defense, various foundations and private industry. Professor Carayon is a Fellow of the Human Factors and Ergonomics Society and a Fellow of the International Ergonomics Association. She is the Recipient of the International Ergonomics Association Triennial Distinguished Service Award (2012).
Ben-Tzion (Bentzi) Karsh, PhD, was professor of Industrial and Systems Engineering at the University of Wisconsin-Madison. He passed away on August 18, 2012, in Madison, Wisconsin after a courageous battle with cancer. He earned his Bachelor’s degree in Psychology, and a Master’s degree and doctorate degree in Industrial Engineering from the University of Wisconsin-Madison. In the Industrial Engineering Department he studied and worked with many faculty, including his Ph.D. advisor, Michael J. Smith. His research focused on macroergonomics in healthcare delivery systems, in particular optimizing human interaction with technology in healthcare settings and understanding the relationship between the work system and patient safety in vulnerable populations such as children and the elderly. His research had significant academic and practical impact. He published more than 60 journal papers. Professor Karsh was extremely active and successful in securing research funding, with multiple grants from the Agency for Healthcare Research and Quality and the National Institutes for Health. He was known as one of the leading thinkers in applying human factors to healthcare systems.
Ayse P. Gurses, PhD, is an associate professor in School of Medicine and Bloomberg School of Public Health at the Johns Hopkins University. She obtained her PhD in Industrial Engineering at the University of Wisconsin-Madison in 2005 and completed her postdoctoral training at the University of Maryland-Baltimore in 2006. Her areas of expertise include human factors engineering and patient safety. Her current research focus includes improving patient safety in the cardiac operating room, transitions of care, care coordination, providers’ compliance with evidence-based guidelines, and nursing working conditions. She has extensive experience with working in interdisciplinary research environments and collaborating with clinicians on human-factors related projects. Her work has been funded by the Agency for Health Care Research and Quality, the National Patient Safety Foundation, the National Science Foundation, the Society of Cardiac Anesthesiologists, and the Robert Wood Johnson Foundation. Dr. Gurses has published in a variety of journals including Applied Ergonomics, Journal of the American Medical Informatics Association, Journal of Biomedical Informatics, Health Services Research, Quality and Safety in Health Care, Joint Commission Journal on Quality and Patient Safety, and Critical Care. She is the associate editor of the IIE Transactions on Healthcare Systems Engineering Socio-Technical System Analysis Department.
Richard J. Holden, PhD, is an assistant professor of Medicine and Biomedical Informatics at Vanderbilt University and a faculty member of the Center for Research and Innovation in Systems Safety in the Vanderbilt University Medical Center. He received a joint PhD in Industrial Engineering and Psychology at the University of Wisconsin-Madison in 2009. His work applies human factors to the design and evaluation of sociotechnical interventions toward improving health and healthcare. He is especially interested in health information technology (HIT) and is the principal investigator of a National Institutes of Health (NIH)-sponsored career development award to develop and evaluate patient-facing HIT to support chronic disease self-care. Dr. Holden has also served as an investigator on grants funded by the Agency for Healthcare Research and Quality, the National Institute of Standards and Technology, the Patient Centered Outcomes Research Institute, and the Swedish Council for Working Life and Social Research.
Peter Hoonakker, Ph.D., is a Research Scientist and the Associate Director of Research in the Center for Quality and Productivity Improvement at the University of Wisconsin-Madison, USA. He obtained his Ph.D. in psychology from the University of Vienna, Austria. During the past 20 years he has conducted research on the relation between job and organizational characteristics, quality of working life and various outcome measures such as health, productivity, safety, absenteeism, and turnover. Throughout his career, he has worked on research projects in The Netherlands and the USA, and on international research projects in collaboration with researchers in other countries, in various branches of industry, such as construction industry, manufacturing industry, the information technology sector, educational institutions, the public sector, mental health institutions, and most recently in health care. He has published over 70 technical reports and nearly 150 book chapters, conference papers, and journal articles in the American Journal of Industrial Medicine, Applied Ergonomics, Behaviour and Information Technology, Human Factors and Ergonomics in Manufacturing, IIE Transactions on Healthcare Systems, International Journal of Medical Informatics, Journal of the American Medical Informatics Association, Social Science & Medicine, and the Cochrane Database of Systematical Reviews.
Ann Schoofs Hundt, PhD, is a Research Scientist and the Associate Director for Education at the University of Wisconsin-Madison Center for Quality and Productivity Improvement and has been part of the Systems Engineering Initiative for Patient Safety since its inception in 2001. She received her PhD in Industrial Engineering from the University of Wisconsin-Madison. Her undergraduate degree and initial 10 years of work experience were in health information services and quality assurance at a large academic medical center. Her research interests are in the areas of macroergonomics and patient safety. She has co-authored numerous publications in various health care, informatics and human factors journals. Research she participates in has primarily been funded by the Agency for Healthcare Research and Quality and the National Institutes for Health.
Enid Montague, PhD, is an assistant professor in the Feinburg School of Medicine at Northwestern University. She obtained her PhD in Industrial and Systems Engineering at Virginia Polytechnic Institute and State University in 2008. Her areas of expertise include human factors and ergonomics engineering in health care systems and in the design of consumer products. Her current research focus is on technology-mediated collaboration in health care contexts, specifically on understanding patient and provider trust in technologies, organizations and in collaborative relationships.
A. Joy Rodriguez, PhD, is an assistant professor in the Department of Industrial Engineering at Clemson University. She obtained her PhD in Industrial and Systems Engineering at the University of Wisconsin-Madison in 2011. Her area of expertise is in human factors engineering and sociotechnical systems theory as applied to the domain of healthcare. Her specific research interests lie in understanding how healthcare professions interact with one another to communicate, make decisions, work as teams, problem solve, and recover from system failures such as poor technology design. She has held key roles on grants funded by the Agency for Healthcare Research and Quality and the Robert Wood Johnson Foundation.
Tosha Wetterneck, MD, MS, is Associate Professor of Medicine at the University of Wisconsin School of Medicine and Public Health. Dr. Wetterneck received her medical degree from the Medical College of Wisconsin. She completed an Internal Medicine residency and chief residency at the University of Wisconsin Hospital and Clinics (UWHC) in Madison, WI, where she currently practices as an Academic Hospitalist. She is a member of the Systems Engineering Initiative for Patient Safety (SEIPS) at UW-Madison and affiliate faculty in the Department of Industrial and Systems Engineering at UW. Dr. Wetterneck has performed patient safety research at the Center for Quality and Productivity Improvement since 2003. Dr. Wetterneck’s research focuses on the design and implementation of tools, including health information technology, to promote clinician situation awareness, the delivery of high quality of care, medication safety and error recovery.
Footnotes
Open systems theory emphasizes the environment in which organizations exist and describes various interactions between organizations and their environment, e.g., customers, competitors, labor unions and government agencies. For more information on open systems theory, see Katz and Kahn (1966).
These measures of workload are often referred as task, job or work demands in the HFE literature.
The task-level measures of Holden and colleagues (2010, 2011) are one example of the situation-level measures described by Carayon and Gurses (2005).
Another chapter in this Review of Human Factors and Ergonomics addresses the issue of health self-management and describes implications for technology (Mitzner, McBride, Barg-Walkow, & Rogers, 2013).
Various federal efforts are underway to support the use of HFE in health IT design; see, for example, activities by NIST on EHR usability (Lowry et al., 2012; Schumacher & Lowry, 2010).
Sense-making is the process by which organizational members ascribe meaning to their experience and can developed a shared awareness and understanding of different individuals’ perspectives (Weick, 2001).
References
- Agarwal R, Anderson C, Crowley K, Kannan PK. Improving Consumer Health IT Application Development: Lessons From Other Industries - Background Report. Rockville, MD: AHRQ; 2011. [Google Scholar]
- Agency for Healthcare Research and Quality. National Healthcare Quality Report 2011. Rockville, MD: Agency for Healthcare Research and Quality; 2012. [Google Scholar]
- Alper SJ, Holden RJ, Scanlon MC, Patel NR, Kaushal R, Skibinski K, Karsh B-T. Self-reported violations during medication administration in two pediatric hospitals. British Medical Journal Quality & Safety. 2012;21:408–415. doi: 10.1136/bmjqs-2011-000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alper SJ, Karsh B-T. A systematic review of safety violations in industry. Accident Analysis & Prevention. 2009;41(4):739–754. doi: 10.1016/j.aap.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Altman Klein H, Meininger AR. Self management of medication and diabetes: Cognitive control. IEEE Transactions on Systems, Man, and Cybernetics--Part A: Systems and Humans. 2004;34(6):718–725. [Google Scholar]
- Alvarado CJ. Human factors and ergonomics in infection prevention. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2. Boca Raton, FL: Taylor & Francis Group; 2012. pp. 793–802. [Google Scholar]
- Alvarado CJ, Wood KE, Carayon P. Human factors and ergonomics task analysis in ultrasonic guidance and infection control for CVC cannulation. In: Pikaar RN, Koningsveld EAP, Settels PJM, editors. Proceedings of the IEA2006 Congress. Elsevier; 2006. [Google Scholar]
- Amalberti R, Vincent C, Auroy Y, de Saint Maurice G. Violations and migrations in health care: A framework for understanding and management. Quality & Safety in Health Care. 2006;15:66–71. doi: 10.1136/qshc.2005.015982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ANSI/AAMI HE75:2009. Human factors engineering: Design of medical devices 2009 [Google Scholar]
- Argyris C, Schon DA. Organizational Learning: A Theory of Action Perspective. Reading: MA: Addison-Wesley Publishing Company; 1978. [Google Scholar]
- Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, Kripalani S. Hospitalist handoffs: A systematic review and task force recommendations. Journal of Hospital Medicine. 2009;4(7):433–440. doi: 10.1002/jhm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beasley JW, Wetterneck TB, Temte J, Lapin JA, Smith P, Rivera-Rodriguez AJ, Karsh B-T. Information chaos in primary care: Implications for physician performance and patient safety. Journal of the American Board of Family Medicine. 2011;24(6):745–751. doi: 10.3122/jabfm.2011.06.100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beatty PCW, Beatty SF. Anaesthetists’ intentions to violate safety guidelines. Anaesthesia. 2004;59:528–540. doi: 10.1111/j.1365-2044.2004.03741.x. [DOI] [PubMed] [Google Scholar]
- Berenholtz SM, Pronovost P, Lipsett PA, Hobson D, Earsing K, Farley JE, Perl TM. Eliminating catheter-related bloodstream infections in the intensive care unit. Critical Care Medicine. 2004;32(10):2014–2020. doi: 10.1097/01.ccm.0000142399.70913.2f. [DOI] [PubMed] [Google Scholar]
- Berenson RA, Hammons T, Gans DN, Zuckerman S, Merrell K, Underwood WS, Williams AF. A house is not a home: Keeping patients at the center of practice redesign. Health Affairs. 2008;27(5):1219–1230. doi: 10.1377/hlthaff.27.5.1219. [DOI] [PubMed] [Google Scholar]
- Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. New England Journal of Medicine. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- Bohr PC, Evanoff BA, Wolf L. Implementing participatory ergonomics teams among health care workers. American Journal of Industrial Medicine. 1997;32(3):190–196. doi: 10.1002/(sici)1097-0274(199709)32:3<190::aid-ajim2>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock D, Spiegelhalter D, Tyrer P. Framework for design and evaluation of complex interventions to improve health. British Medical Journal. 2000;321(7262):694–696. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P. Macroergonomics in quality of care and patient safety. In: Luczak H, Zink KJ, editors. Human Factors in Organizational Design and Management. Santa Monica, CA: IEA Press; 2003. pp. 21–35. [Google Scholar]
- Carayon P. Top management’s view on human factors and patient safety: Do they see it? In: Tartaglia R, Bagnara S, Bellandi T, Albolino S, editors. Healthcare Systems Ergonomics and Patient Safety. Florence, Italy: Taylor & Francis; 2005. pp. 38–42. [Google Scholar]
- Carayon P. Human factors of complex sociotechnical systems. Applied Ergonomics. 2006;37:525–535. doi: 10.1016/j.apergo.2006.04.011. [DOI] [PubMed] [Google Scholar]
- Carayon P. The Balance Theory and the work system model... Twenty years later. International Journal of Human-Computer Interaction. 2009;25(5):313–327. [Google Scholar]
- Carayon P. Human factors in patient safety as an innovation. Applied Ergonomics. 2010;41(5):657–665. doi: 10.1016/j.apergo.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P. Sociotechnical systems approach to healthcare quality and patient safety. Work: A Journal of Prevention, Assessment and Rehabilitation. 2012a;41(0):3850–3854. doi: 10.3233/WOR-2012-0091-3850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Boca Raton, CA: Taylor & Francis; 2012b. [Google Scholar]
- Carayon P, Alvarado CJ, Hundt AS. Reducing Workload and Increasing Patient Safety Through Work and Workspace Design. Washington, DC: Institute of Medicine; 2003. [Google Scholar]
- Carayon P, Alvarado CJ, Hundt AS. Work design and patient safety. Theoretical Issues in Ergonomics Science. 2007;8(5):395–428. [Google Scholar]
- Carayon P, Alvarado CJ, Hundt AS. Work design and patient safety. TIES-Theoretical Issues in Ergonomics Science. 2007;8(5):395–428. [Google Scholar]
- Carayon P, Alyousef B, Hoonakker P, Hundt AS, Cartmill R, Tomcavage J, Walker J. Challenges to care coordination posed by the use of multiple health IT applications. Work: A Journal of Prevention, Assessment and Rehabilitation. 2012;41(0):4468–4473. doi: 10.3233/WOR-2012-0746-4468. [DOI] [PubMed] [Google Scholar]
- Carayon P, Alyousef B, Xie A. Human factors and ergonomics in health care. In: Salvendy G, editor. Handbook of Human Factors and Ergonomics. 4. New York, NY: John Wiley & Sons; 2012. pp. 1574–1595. [Google Scholar]
- Carayon P, Bass E, Bellandi T, Gurses AP, Hallbeck SM, Mollo V. Sociotechnical systems analysis in health care: A research agenda. IIE Transactions on Healthcare Systems Engineering. 2011a;1(3):145–160. doi: 10.1080/19488300.2011.619158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, DuBenske LL, McCabe BC, Shaw B, Gaines ME, Kelly MM, Cox ED. Work system barriers and facilitators to family engagement in rounds in a pediatric hospital. In: Albolino S, Bagnara S, Bellandi T, Llaneza J, Rosal G, Tartaglia R, editors. Healthcare Systems Ergonomics and Patient Safety. Boca Raton, FL: CRC Press; 2011b. pp. 81–85. [Google Scholar]
- Carayon P, Faye H, Hundt AS, Karsh B-T, Wetterneck TB. Patient safety and proactive risk assessment. In: Yuehwern Y, editor. Handbook of Healthcare Delivery Systems. Boca Raton, FL: Taylor & Francis; 2011. pp. 12–11. [Google Scholar]
- Carayon P, Hoonakker P. Organizational design and cognitive work. In: Lee JD, Kirlik A, editors. The Oxford Handbook of Cognitive Engineering. New York, NY: Oxford University Press; 2013. pp. 216–225. [Google Scholar]
- Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, Brennan PF. Work system design for patient safety: The SEIPS model. Quality & Safety in Health Care. 2006;15(Supplement I):i50–i58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Hundt AS, Wetterneck TB. Nurses’ acceptance of Smart IV pump technology. International Journal of Medical Informatics. 2010;79:401–411. doi: 10.1016/j.ijmedinf.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Karsh B-T, Cartmill R, Hoonakker P, Hundt AS, Krueger D, Wetterneck TB. Incorporating Health Information Technology into Workflow Redesign-Summary Report. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- Carayon P, Smith MJ. Work organization and ergonomics. Applied Ergonomics. 2000;31:649–662. doi: 10.1016/s0003-6870(00)00040-5. [DOI] [PubMed] [Google Scholar]
- Carayon P, Smith P, Hundt AS, Kuruchittham V, Li Q. Implementation of an Electronic Health Records system in a small clinic. Behaviour and Information Technology. 2009;28(1):5–20. [Google Scholar]
- Carayon P, Wetterneck TB, Hundt AS, Ozkaynac M, Ram P, DeSilvey J, Sobande S. Observing nurse interaction with infusion pump technologies. In: Henriksen K, Battles JB, Marks E, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation. Vol. 2. Rockville, MD: Agency for Healthcare Research and Quality; 2005. pp. 349–364. [PubMed] [Google Scholar]
- Carayon P, Wetterneck TB, Hundt AS, Ozkaynak M, DeSilvey J, Ludwig B, Rough SS. Evaluation of nurse interaction with bar code medication administration technology in the work environment. Journal of Patient Safety. 2007;3(1):34–42. [Google Scholar]
- Carayon P, Wetterneck TB, Hundt AS, Rough S, Schroeder M. Continuous technology implementation in health care: The case of advanced IV infusion pump technology. In: Zink K, editor. Corporate Sustainability as a Challenge for Comprehensive Management. New York: Springer; 2008. pp. 139–151. [Google Scholar]
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden RJ, Gurses AP. Human factors systems approach to healthcare quality and patient safety. Applied Ergonomics. 2013 doi: 10.1016/j.apergo.2013.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Xie A. Decision making in healthcare system design: When human factors engineering meets health care. In: Proctor RW, Nof SY, Yih Y, editors. Cultural Factors in Decision Making and Action. Taylor & Francis; 2011. [Google Scholar]
- Carayon P, Xie A, Kianfar S. Human Factors and Ergonomics. In: Shekelle PG, Wachter R, Pronovost P, Schoelles K, McDonald K, Dy S, Shojania K, Reston J, Berger Z, Johnsen B, Larkin J, Lucas S, Martinez K, Motala A, Newberry S, Noble M, Pfoh E, Ranji S, Rennke S, Schmidt E, Shanman R, Sullivan N, Sun F, Tipton K, Treadwell J, Tsou A, Vaiana M, Weaver S, Wilson R, Winters B, editors. Making Health Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices. Comparative Effectiveness Review No. 211. Rockville, MD: Agency for Healthcare Research and Quality; 2013. pp. 325–350. AHRQ Publication No.13-E001-EF. [Google Scholar]
- Caron CD, Bowers BJ. Methods and application of dimensional analysis: A contribution to concept and knowledge development in nursing. In: Rodgers BL, Knafl KA, editors. Concept development in nursing: Foundations, techniques, and applications. 2. Philadelphia: Saunders; 2000. pp. 285–319. [Google Scholar]
- Carroll JS, Quijada MA. Tilting the culture in health care: Using cultural strengths to transform organizations. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Mahwah, NJ: Lawrence Erlbaum Associates, Publishers; 2007. pp. 823–832. [Google Scholar]
- Centers for Disease Control and Prevention. Workplace safety and health topics: Healthcare workers. 2012. 2012 from http://www.cdc.gov/niosh/topics/healthcare/
- Cherns A. The principles of sociotechnical design. Human Relations. 1976;29(8):783–792. [Google Scholar]
- Clegg CW. Sociotechnical principles for system design. Applied Ergonomics. 2000;31:463–477. doi: 10.1016/s0003-6870(00)00009-0. [DOI] [PubMed] [Google Scholar]
- Connolly C. Cedars-Sinai doctors cling to pen and paper. Washington Post 2005 Mar; [Google Scholar]
- Cook R, Rasmussen J. “Going solid”: A model of system dynamics and consequences for patient safety. Quality & Safety in Health Care. 2005;14(2):130–134. doi: 10.1136/qshc.2003.009530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper JB, Long CD, Newbower RS, Philip JH. Critical incidents associated with intraoperative exchanges of anesthesia personnel. Anesthesiology. 1982;56(6):456–461. doi: 10.1097/00000542-198206000-00010. [DOI] [PubMed] [Google Scholar]
- Creswell JW, Klassen AC, Plano Clark VL, Smith KC. Best practices for mixed methods research in the health sciences. National Institutes of Health; 2011. [Google Scholar]
- Dainoff MJ. Can’t we all just get along? Some alternative views of the knowledge worker in complex HCI systems. International Journal of Human-Computer Interaction. 2009;25(5):328–347. [Google Scholar]
- de Saint Maurice G, Auroy Y, Vincent C, Amalberti R. The natural lifespan of a safety policy: Violations and system migrations in anaesthesia. Quality & Safety in Health Care. 2010;19(4):327–331. doi: 10.1136/qshc.2008.029959. [DOI] [PubMed] [Google Scholar]
- DeBourgh GA, Prion SK. Patient safety manifesto: A professional imperative for prelicensure nursing education. Journal of Professional Nursing. 2012;28:110–118. doi: 10.1016/j.profnurs.2011.05.001. [DOI] [PubMed] [Google Scholar]
- Delaune J, Everett W. Clinical care: A comprehensive analysis in support of systemwide improvements. In: Everett W, King N, editors. Waste and inefficiency in the U.S. health care system. New England, MA: New England Health Care Institute; 2008. pp. 1–68. [Google Scholar]
- DeLucia PR, Ott TE, Palmieri PA. Performance in nursing. Reviews of Human Factors and Ergonomics. 2009;5(1):1–40. [Google Scholar]
- Dierks MM, Christian CK, Roth EM. Healthcare safety: The impact of disabling “safety” protocols. IEEE Transactions on Systems, Man, and Cybernetics--Part A: Systems and Humans. 2004;34(6):693–698. [Google Scholar]
- DiMatteo MR, Sherbourne CD, Hays RD, Ordway L, Kravitz RL, McGlynn EA, Rogers WH. Physicians’ characteristics influence patients’ adherence to medical treatment: Results from the Medical Outcomes Study. Health Psychology. 1993;12(2):93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- Donabedian A. The quality of medical care. Science. 1978;200:856–864. doi: 10.1126/science.417400. [DOI] [PubMed] [Google Scholar]
- Donabedian A. The quality of care. How can it be assessed? Journal of the American Medical Association. 1988;260(12):1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Douglas S, Cartmill R, Brown R, Hoonakker P, Slagle J, Van Roy KS, Carayon P. The work of adult and pediatric intensive care unit nurses. Nursing Research. 2012;62(1):50–58. doi: 10.1097/NNR.0b013e318270714b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drews FA, Wallace J, Benuzillo J, Markewitz B, Samore M. Protocol adherence in the intensive care unit. Human Factors and Ergonomics in Manufacturing & Service Industries. 2012;22(1):21–31. [Google Scholar]
- Dul J, Bruder R, Buckle P, Carayon P, Falzon P, Marras WS, van der Doelen B. A strategy for human factors/ergonomics: Developing the discipline and profession. Ergonomics. 2012;55(4):377–395. doi: 10.1080/00140139.2012.661087. [DOI] [PubMed] [Google Scholar]
- Elder NC, Graham D, Brandt E, Dovey S, Phillips R, Ledwith J, Hickner J. The testing process in family medicine: problems, solutions, and barriers as seen by physicians and their staff: A study of the American Academy of Family Physicians’ Research Network. Journal of Patient Safety. 2006;2(1):25–32. [Google Scholar]
- Emery F, Trist E. The causal texture of organizational environments. Human Relations. 1965;18:21–31. [Google Scholar]
- Emery FE, Trist EL. The causal texture of organizational environments. In: Pasmore WA, Sherwood JJ, editors. Sociotechnical Systems: A Sourcebook. San Diego, CA: University Associates; 1978. [Google Scholar]
- Evanoff VA, Bohr PC, Wolf L. Effects of a participatory ergonomics team among hospital orderlies. American Journal of Industrial Medicine. 1999;35:358–365. doi: 10.1002/(sici)1097-0274(199904)35:4<358::aid-ajim6>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Faye H, Rivera-Rodriguez AJ, Karsh B-T, Hundt AS, Baker C, Carayon P. Involving intensive care unit nurses in a proactive risk assessment of the medication management process. The Joint Commission Journal on Quality and Patient Safety. 2010;36(8):376–384. doi: 10.1016/s1553-7250(10)36056-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flin R, Winter J, Sarac C, Raduma M. Report for Methods and Measures Working Group of WHO Patient Safety. Geneva: World Health Organization; 2009. Human Factors in Patient Safety: Review of Topics and Tools. [Google Scholar]
- Flynn EA, Barker KN, Gibson JT, Pearson RE, Berger BA, Smith LA. Impact of interruptions and distractions on dispensing errors in an ambulatory care pharmacy. American Journal of Health-System Pharmacy. 1999;56(13):1319–1325. doi: 10.1093/ajhp/56.13.1319. [DOI] [PubMed] [Google Scholar]
- Ginsburg G. Human factors engineering: A tool for medical device evaluation in hospital procurement decision-making. Journal of Biomedical Informatics. 2005;38:213–219. doi: 10.1016/j.jbi.2004.11.008. [DOI] [PubMed] [Google Scholar]
- Gold MR, McLaughlin CG, Devers KJ, Berenson RA, Bovbjerg RR. Obtaining providers’ ‘buy-in’ and establishing effective means of information exchange will be critical to HITECH’s success. Health Affairs. 2012;31(3):514–526. doi: 10.1377/hlthaff.2011.0753. [DOI] [PubMed] [Google Scholar]
- Gosbee J. Human factors engineering and patient safety. Quality & Safety in Health Care. 2002;11(4):352–354. doi: 10.1136/qhc.11.4.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T, Robert G, MacFarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: Systematic review and recommendations. The Milbank Quarterly. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundgeiger T, Sanderson P, MacDougall HG, Venkatesh B. Interruption management in the intensive care unit: Predicting resumption times and assessing distributed support. Journal of Experimental Psychology: Applied. 2010;16(4):317–334. doi: 10.1037/a0021912. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Carayon P. Performance obstacles of intensive care nurses. Nursing Research. 2007a;56(3):185–194. doi: 10.1097/01.NNR.0000270028.75112.00. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Carayon P. Exploring performance obstacles of intensive care nurses. Applied Ergonomics. 2009a;40(3):509–518. doi: 10.1016/j.apergo.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Carayon P. A qualitative study of performance obstacles and facilitators among ICU nurses. Applied Ergonomics. 2009b;40(3):509–518. doi: 10.1016/j.apergo.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Carayon P, Wall M. Impact of performance obstacles on intensive care nurses workload, perceived quality and safety of care, and quality of working life. Health Services Research. 2009;44(2):422–443. doi: 10.1111/j.1475-6773.2008.00934.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurses AP, Kim G, Martinez EA, Marsteller J, Bauer L, Lubomski LH, Thompson D. Identifying and categorizing patient safety hazards in cardiovascular operating rooms using an interdisciplinary approach: A multisite study. British Medical Journal Quality & Safety. 2012 doi: 10.1136/bmjqs-2011-000625. accepted. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Ozok AA, Pronovost P. Time to accelerate integration of human factors and ergonomics in patient safety. British Medical Journal Quality & Safety. 2012;21(4):347–351. doi: 10.1136/bmjqs-2011-000421. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Seidl KL, Vaidya V, Bochicchio G, Harris AD, Hebden J, Xiao Y. Systems ambiguity and guideline compliance: A qualitative study of how intensive care units follow evidence-based guidelines to reduce healthcare-associated infections. Quality & Safety in Health Care. 2008;17(5):351–359. doi: 10.1136/qshc.2006.021709. [DOI] [PubMed] [Google Scholar]
- Halbesleben JRB, Wakefield DS, Wakefield BJ. Work-arounds in health care settings: Literature review and research agenda. Health Care Management Review. 2008;33:2–12. doi: 10.1097/01.HMR.0000304495.95522.ca. [DOI] [PubMed] [Google Scholar]
- Hallock ML, Alper SJ, Karsh B-T. A macroergonomic work system analysis of the diagnostic testing process in an outpatient health care facility for process improvement and patient safety. Ergonomics. 2006;49(5–6):544–566. doi: 10.1080/00140130600568832. [DOI] [PubMed] [Google Scholar]
- Hamilton-Escoto K, Hallock M, Wagner J, Karsh B-T. Using variance analysis to detect hazards in a bar-code assisted medication preparation process. Joint Commission Journal on Quality and Safety. 2004;30(11):622–628. doi: 10.1016/s1549-3741(04)30073-0. [DOI] [PubMed] [Google Scholar]
- Hendrick HW. Human factors in organizational design and management. Ergonomics. 1991;34:743–756. [Google Scholar]
- Hendrick HW. Applying ergonomics to systems: Some documented “lessons learned”. Applied Ergonomics. 2008;39(4):418–426. doi: 10.1016/j.apergo.2008.02.006. [DOI] [PubMed] [Google Scholar]
- Hendrick HW, Kleiner BM. Macroergonomics: An Introduction to Work System Design. Santa Monica, CA: Human Factors and Ergonomics Society; 2001. [Google Scholar]
- Hendrick HW, Kleiner BM. Macroergonomics: Theory, Methods and Applications. Mahwah, NJ: Lawrence Erlbaum Associates; 2002. [Google Scholar]
- Henriksen K, Joseph A, Zayas-Cabán T. The human factors of home health care: A conceptual model for examining safety and quality concerns. Journal of Patient Safety. 2009;5:229–236. doi: 10.1097/PTS.0b013e3181bd1c2a. [DOI] [PubMed] [Google Scholar]
- Hesselink G, Schoonhoven L, Barach P, Spijker A, Gademan P, Kalkman C, Wollersheim H. Improving patient handovers from hospital to primary care: A systematic review. Annals of Internal Medicine. 2012;157(6):417–428. doi: 10.7326/0003-4819-157-6-201209180-00006. [DOI] [PubMed] [Google Scholar]
- Hickam DH, Severance S, Feldstein A, Ray L, Gorman P, Schuldheis S, Helfand M. The Effect of Health Care Working Conditions on Patient Safety. Rockville, MD: Agency for Healthcare Research and Quality; 2003. [PMC free article] [PubMed] [Google Scholar]
- Hing E, Bhuiya F. Wait Time for Treatment in Hospital Emergency Departments: 2009. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- Hoffman RR, Militello LG. Perspectives on Cognitive Task Analysis. New York: Psychology Press; 2009. [Google Scholar]
- Holden RJ. Cognitive performance-altering effects of electronic medical records: An application of the human factors paradigm for patient safety. Cognition, Technology & Work. 2011a;13:11–29. doi: 10.1007/s10111-010-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ. Lean thinking in emergency departments: A critical review. Annals of Emergency Medicine. 2011b;57:265–278. doi: 10.1016/j.annemergmed.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Brown RL, Alper SJ, Scanlon MC, Patel NR, Karsh B-T. That’s nice, but what does IT do? Evaluating the impact of bar coded medication administration by measuring changes in the process of care. International Journal of Industrial Ergonomics. 2011;41:370–379. doi: 10.1016/j.ergon.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Karsh B-T. A review of medical error reporting system design considerations and a proposed cross-level system research framework. Human Factors. 2007;49:257–276. doi: 10.1518/001872007X312487. [DOI] [PubMed] [Google Scholar]
- Holden RJ, Karsh B-T. A theoretical model of health information technology usage behaviour with implications for patient safety. Behaviour & Information Technology. 2009;28:21–38. [Google Scholar]
- Holden RJ, Or CKL, Alper SJ, Rivera-Rodriguez AJ, Karsh B-T. A change management framework for macroergonomic field research. Applied Ergonomics. 2008;39(4):459–474. doi: 10.1016/j.apergo.2008.02.016. [DOI] [PubMed] [Google Scholar]
- Holden RJ, Patel NR, Scanlon MC, Shalaby TM, Arnold JM, Karsh B-T. Effects of mental demands during dispensing on perceived medication safety and employee well being: A study of workload in pediatric hospital pharmacies. Research in Social & Administrative Pharmacy. 2010;6:293–306. doi: 10.1016/j.sapharm.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Rivera-Rodriguez AJ, Faye H, Scanlon MC, Karsh B-T. Automation and adaptation: Nurses’ problem-solving behavior following the implementation of bar coded medication administration technology. Cognition, Technology & Work. 2012 doi: 10.1007/s10111-012-0229-4. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Scanlon MC, Patel NR, Kaushal R, Escoto KH, Brown RL, Karsh B-T. A human factors framework and study of the effect of nursing workload on patient safety and employee quality of working life. British Medical Journal Quality & Safety. 2011;20:15–24. doi: 10.1136/bmjqs.2008.028381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ. Cognitive performance-altering effects of electronic medical records: An application of the human factors paradigm for patient safety. Cognition, Technology & Work. 2011;13(1):11–29. doi: 10.1007/s10111-010-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollnagel E. Prologue: The scope of resilience engineering. In: Hollnagel E, Paries J, Woods D, Wreathall J, editors. Resilience Engineering in Practice - A Guidebook. Burlington, VT: Ashgate Studies in Resilience Engineering; 2011. pp. xxix–xxxix. [Google Scholar]
- Hollnagel E, Woods DD, Leveson N, editors. Resilience Engineering - Concepts and Precepts. Burlington, VT: Ashgate; 2006. [Google Scholar]
- Hoonakker P, Carayon P, Gurses AP, Brown R, Khunlertkit A, McGuire K, Walker JM. Measuring workload of ICU nurses with a questionnaire survey: The NASA Task Load Index (TLX) IIE Transactions on Healthcare Systems Engineering. 2011;1(2):131–143. doi: 10.1080/19488300.2011.609524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoonakker P, Cartmill R, Carayon P, Walker JM. Development and psychometric qualities of the SEIPS survey to evaluate CPOE/EHR implementation in ICUs. International Journal of Healthcare Information Systems and Informatics. 2011;6(1):51–69. doi: 10.4018/jhisi.2011010104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoonakker P, Khunlertkit A, McGuire K, Carayon P, Wiegmann D, Wood K. A day in life of a tele-Intensive Care Unit nurse. In: Albolino S, Bagnara S, Bellandi T, Llaneza J, Rosal G, Tartaglia R, editors. Healthcare Systems Ergonomics and Patient Safety. Boca Raton, FL: CRC Press; 2011. [Google Scholar]
- Hoonakker P, Khunlertkit A, Tattersall M, Keevil J, Smith PD. Computer decision support tools in primary care. Work: A Journal of Prevention, Assessment and Rehabilitation. 2012;41:4474–4478. doi: 10.3233/WOR-2012-0747-4474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoonakker P, Wetterneck TB, Carayon P, Cartmill R, Walker JM. Drug alerts override from a human factors perspective. In: Albolino S, Bagnara S, Bellandi T, Llaneza J, Rosal G, Tartaglia R, editors. Healthcare Systems Ergonomics and Patient Safety 2011. Boca Raton, FL: CRC Press; 2011. pp. 367–371. [Google Scholar]
- Horsky J, Kaufman DR, Oppenheim MI, Patel VL. A framework for analyzing the cognitive complexity of computer-assisted clinical ordering. Journal of Biomedical Informatics. 2003;36:4–22. doi: 10.1016/s1532-0464(03)00062-5. [DOI] [PubMed] [Google Scholar]
- Hundt AS. Organizational learning in health care. In: Carayon P, editor. Human Factors and Ergonomics in Health Care and Patient Safety. 2. Boca Raton, FL: CRC Press; 2012. pp. 97–108. [Google Scholar]
- Hundt AS, Adams JA, Schmid A, Musser LM, Walker JM, Wetterneck TB, Carayon P. Conducting an efficient proactive risk assessment prior to CPOE implementation. International Journal of Medical Informatics. 2013;82:25–38. doi: 10.1016/j.ijmedinf.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- Institute of Medicine. Keeping Patients Safe: Transforming the Work Environment of Nurses. Washington, D.C: The National Academies Press; 2004. [PubMed] [Google Scholar]
- Institute of Medicine. Preventing Medication Errors. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- Institute of Medicine. Health IT and Patient Safety: Building Safer Systems for Better Care. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- International Ergonomics Association. The Discipline of Ergonomics. 2000 Retrieved August 22, 2004. [Google Scholar]
- International Standards Organization. International Standards Organization (ISO) 9241–11: Guidance on Usability. Geneva: 1998. [Google Scholar]
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Jones JW, Barge BN, Steffy BD, Fay L, Kunz L, Wuebker L. Stress and medical malpractice: Organizational risk assessment and intervention. Journal of Applied Psychology. 1988;73(4):727–735. doi: 10.1037/0021-9010.73.4.727. [DOI] [PubMed] [Google Scholar]
- Karsh B-T. Beyond usability: Designing effective technology implementation systems to promote patient safety. Quality & Safety in Health Care. 2004;13:388–394. doi: 10.1136/qshc.2004.010322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karsh B-T. Clinical practice improvement and redesign: How change in workflow can be supported by clinical decision support. Rockville, MD: Agency for Healthcare Research and Quality; 2009. [Google Scholar]
- Karsh B-T, Alper SJ. Work system analysis: The key to understanding health care systems. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation (Vol. 2: Concepts and Methodology) Rockville, MD: AHRQ; 2005. [PubMed] [Google Scholar]
- Karsh B-T, Brown R. The impact of organizational hierarchies on the design and analysis of medical error research. In: Carayon P, Robertson M, Kleiner BM, Hoonakker P, editors. Human Factors in Organizational Design and Management – VII. Santa Monica, CA: IEA Press; 2005. pp. 293–298. [Google Scholar]
- Karsh B-T, Brown R. Macroergonomics and patient safety: The impact of levels on theory, measurement, analysis and intervention in patient safety research. Applied Ergonomics. 2010;41(5):674–681. doi: 10.1016/j.apergo.2009.12.007. [DOI] [PubMed] [Google Scholar]
- Karsh B-T, Escoto KH, Beasley JW, Holden RJ. Toward a theoretical approach to medical error reporting system research and design. Applied Ergonomics. 2006;37:283–295. doi: 10.1016/j.apergo.2005.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karsh B-T, Holden RJ, Alper SJ, Or CKL. A human factors engineering paradigm for patient safety: Designing to support the performance of the healthcare professional. Quality & Safety in Health Care. 2006;15(i6):i59–i65. doi: 10.1136/qshc.2005.015974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karsh B-T, Holden RJ, Escoto KH, Alper SJ, Scanlon MC, Arnold J, Brown RL. Do beliefs about hospital technologies predict nurses’ perceptions of quality of care? A study of task-technology fit in two pediatric hospitals. International Journal of Human-Computer Interaction. 2009;25:374–389. [Google Scholar]
- Karsh B-T, Weinger MB, Abbott PA, Wears RL. Health information technology: Fallacies and sober realities. Journal of the American Medical Informatics Association. 2010;17:617–623. doi: 10.1136/jamia.2010.005637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz D, Kahn RL. Common characteristics of open systems. In: Katz D, Kahn RL, editors. The Social Psychology of Organizations. New York: John Wiley & Sons; 1966. pp. 14–29. [Google Scholar]
- Khunlertkit A, Carayon P. Contributions of the tele-ICU technology to quality of care and patient safety. 2012 doi: 10.1016/j.jcrc.2012.10.005. under review. [DOI] [PubMed] [Google Scholar]
- Kiekkas P, Sakellaropoulos GC, Brokalaki H, Manolis E, Samios A, Skartsani C, Baltopoulos GI. Association between nursing workload and mortality of intensive care unit patients. Journal of Nursing Scholarship. 2008;40(4):385–390. doi: 10.1111/j.1547-5069.2008.00254.x. [DOI] [PubMed] [Google Scholar]
- Kleiner BM. Sociotechnical system design in health care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Mahwah, NJ: Lawrence Erlbaum Associates; 2007. pp. 79–94. [Google Scholar]
- Kleiner BM. Macroegonomics: Work system analysis and design. Human Factors. 2008;50(3):461–467. doi: 10.1518/001872008X288501. [DOI] [PubMed] [Google Scholar]
- Kleiner BM. Sociotechnical system design in healthcare. In: CP, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2. Mahwah, NJ: Lawrence Erlbaum Associates; 2011. [Google Scholar]
- Kleiner BM, Lewis V. Human dimensions of information and communication technologies in health services systems: Macroergonomics in healthcare: Using MEAD to analyze and improve health systems. Paper presented at the International Conference on Applied Human Factors and Ergonomics; San Francisco, CA. 2012. [Google Scholar]
- Klevens RM, Edwards JR, Richards CL, Jr, Horan TC, Gaynes RP, Pollock DA, Cardo DM. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Reports. 2007;122(2):160–166. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington, D.C: National Academy Press; 1999. [PubMed] [Google Scholar]
- Kools S, McCarthy M, Durham R, Robrecht L. Dimensional analysis: Broadening the conception of grounded theory. Qualitative Health Research. 1996;6(3):312–330. [Google Scholar]
- Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, Strom BL. Role of computerized physician order entry systems in facilitating medications errors. Journal of the American Medical Association. 2005;293(10):1197–1203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- Koppel R, Wetterneck TB, Telles JL, Karsh B-T. Workarounds to barcode medication administration systems: Their occurrences, causes, and threats to patient safety. Journal of the American Medical Informatics Association. 2008;15:408–423. doi: 10.1197/jamia.M2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Curtis JP. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011;124(9):1038–1045. doi: 10.1161/CIRCULATIONAHA.111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang TA, Hodge M, Olson V, Romano PS, Kravitz RL. Nurse-patient ratios: A systematic review on the effects of nurse staffing on patient, nurse employee, and hospital outcomes. Journal of Nursing Administration. 2004;34(7–8):326–337. doi: 10.1097/00005110-200407000-00005. [DOI] [PubMed] [Google Scholar]
- Laschinger HKS, Leiter MP. The impact of nursing work environments on patient safety outcomes. Journal of Nursing Administration. 2006;36(5):259–267. doi: 10.1097/00005110-200605000-00019. [DOI] [PubMed] [Google Scholar]
- Lawton R, McEachan RRC, Giles SJ, Sirriyeh R, Watt IS, Wright J. Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: A systematic review. British Medical Journal Quality & Safety. 2012;21:369–380. doi: 10.1136/bmjqs-2011-000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton R, Parker D. Procedures and the professional: The case of the British NHS. Social Science & Medicine. 1999;48:353–361. doi: 10.1016/s0277-9536(98)00345-1. [DOI] [PubMed] [Google Scholar]
- Lowry SZ, Quinn MT, Ramaiah M, Brick D, Patterson ES, Zhang J, Gibbons MC. A Human Factors Guide to Enhance EHR Usability of Critical User Interactions when Supporting Pediatric Patient Care. NIST; 2012. [Google Scholar]
- Lundstrom T, Pugliese G, Bartley J, Cox J, Guither C. Organizational and environmental factors that affect worker health and safety and patient outcomes. American Journal of Infection Control. 2002;30(2):93–106. doi: 10.1067/mic.2002.119820. [DOI] [PubMed] [Google Scholar]
- Magrabi F, Ong MS, Runciman W, Coiera E. An analysis of computer-related patient safety incidents to inform the development of a classification. Journal of the American Medical Informatics Association. 2010;17(6):663–670. doi: 10.1136/jamia.2009.002444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCulloch P, Rathbone J, Catchpole K. Interventions to improve teamwork and communications among healthcare staff. British Journal of Surgery. 2011;98(4):469–479. doi: 10.1002/bjs.7434. [DOI] [PubMed] [Google Scholar]
- McDonald KM, Schultz E, Albin L, Pineda N, Lonhart J, Sundaram V, Malcolm E. Care Coordination Measures Atlas. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- McDonald R, Waring J, Harrison S. Rules, safety and the narrativisation of identity: A hospital operating theatre case study. Sociology of Health & Illness. 2006;28(2):178–202. doi: 10.1111/j.1467-9566.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- McDonnell C, Werner K, Wendel K. Electronic Health Record Usability: Vendor Practices and Perspectives. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- McGlynn EA, Asch SM, Adams JA, Keesey J, Hicks J, DeCristofaro A, Kerr E. The quality of health care delivered to adults in the United States. New England Journal of Medicine. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- Michtalik HJ, Yeh HC, Pronovost PJ, Brotman DJ. Impact of attending physician workload on patient care: A survey of hospitalists. JAMA Internal Medicine. 2013;173(5):375–377. doi: 10.1001/jamainternmed.2013.1864. [DOI] [PubMed] [Google Scholar]
- Middleton B, Bloomrosen M, Dente MA, Hashmat B, Koppel R, Overhage MJ, Zhang J. Enhancing patient safety and quality of care by improving the usability of electronic health record systems: recommendations from AMIA. Journal of the American Medical Informatics Association. 2013 doi: 10.1136/amiajnl-2012-001458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miedema MD, Newell MC, Duval S, Garberich RF, Handran CB, Larson DM, Henry TD. Causes of delay and associated mortality in patients transferred with ST-segment-elevation myocardial infarction. Circulation. 2011;124(15):1636–1644. doi: 10.1161/CIRCULATIONAHA.111.033118. [DOI] [PubMed] [Google Scholar]
- Miller DF, Fortier CR, Garrison KL. Bar code medication administration technology: Characterization of high-alert medication triggers and clinician workarounds. Annals of Pharmacotherapy. 2011;45:162–168. doi: 10.1345/aph.1P262. [DOI] [PubMed] [Google Scholar]
- Mitzner TL, McBride SE, Barg-Walkow LH, Rogers WA. Self-management of wellness and illness in an aging population. Reviews of Human Factors and Ergonomics 2013 [Google Scholar]
- Montague E, Lee JD. Trust in health technologies. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2. Boca Raton, FL: Taylor & Francis Group; 2012. pp. 281–291. [Google Scholar]
- Montague E, Winchester WW, Kleiner BM. Trust in medical technology by patients and healthcare providers in obstetric work systems. Behaviour & Information Technology. 2010;29(5):541–554. doi: 10.1080/01449291003752914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey JC, Simon R, Jay GD, Wears RL, Salisbury M, Dukes KA, Berns SD. Error reduction and performance improvement in the emergency department through formal teamwork training: Evaluation results of the MedTeams project. Health Services Research. 2002;37(6):1553–1581. doi: 10.1111/1475-6773.01104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow DG, Chin J. Technology as a bridge between health care systems and older adults. In: Zheng RZ, Hill RD, Gardner MK, editors. Engaging Older Adults with Modern Technology: Internet Use and Information Access Needs. Hershey, PA: Information Science Reference; 2013. pp. 59–79. [Google Scholar]
- Morrow DG, Weiner M, Young J, Steinley D, Deer M, Murray MD. Improving medication knowledge among older adults with heart failure: A patient-centered approach to instruction design. Gerontologist. 2005;45(4):545–552. doi: 10.1093/geront/45.4.545. [DOI] [PubMed] [Google Scholar]
- Muething SE, Kotagal UR, Schoettker PJ, Gonzalez del Rey J, DeWitt TG. Family-centered bedside rounds: A new approach to patient care and teaching. Pediatrics. 2007;119(4):829–832. doi: 10.1542/peds.2006-2528. [DOI] [PubMed] [Google Scholar]
- Murff HJ, Kannry J. Physician satisfaction with two order entry systems. Journal of the American Medical Informatics Association. 2001;8(5):499–509. doi: 10.1136/jamia.2001.0080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman I, Benz CR. Qualitative-Quantitative Research Methodology. Carbondale, Il: Southern Illinois University Press; 1998. [Google Scholar]
- Niazkhani Z, Pirnejad H, van der Sijs H, Aarts J. Evaluating the medication process in the context of CPOE use: The significance of working around the system. International Journal of Medical Informatics. 2011;80:490–506. doi: 10.1016/j.ijmedinf.2011.03.009. [DOI] [PubMed] [Google Scholar]
- Nielsen J. Usability Engineering. Morgan Kaufmann; Amsterdam, The Netherlands: 1993. [Google Scholar]
- Noro K, Imada A. Participatory Ergonomics. London: Taylor & Francis; 1991. [Google Scholar]
- Novak LL, Holden RJ, Anders SH, Hong JY, Karsh B-T. Using a sociotechnical framework to understand adaptations in health IT implementation. International Journal of Medical Informatics. doi: 10.1016/j.ijmedinf.2013.01.009. forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NRC Committee on the Role of Human Factors in Home Health Care. Consumer Health Information Technology in the Home: A Guide for Human Factors Design Considerations. Washington, DC: National Academies Press; 2011. [Google Scholar]
- Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. The Annals of Family Medicine. 2009;7(3):254–260. doi: 10.1370/afm.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Or CKL, Karsh B-T. A systematic review of patient acceptance of consumer health information technology. Journal of the American Medical Informatics Association. 2009;16:550–560. doi: 10.1197/jamia.M2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ovretveit JC, Shekelle PG, Dy SM, McDonald KM, Hempel S, Pronovost P, Wachter RM. How does context affect interventions to improve patient safety? An assessment of evidence from studies of five patient safety practices and proposals for research. British Medical Journal Quality & Safety. 2011;20(7):604–610. doi: 10.1136/bmjqs.2010.047035. [DOI] [PubMed] [Google Scholar]
- Pape TM. Applying airline safety practices to medication administration. MEDSURG Nursing. 2003;12(2):77–94. [PubMed] [Google Scholar]
- Pape TM, Guerra DM, Muzquiz M, Bryant JB, Ingram M, Schranner B, Welker J. Innovative approaches to reducing nurses’ distractions during medication administration. Journal of Continuing Education in Nursing. 2005;36(3):108–116. doi: 10.3928/0022-0124-20050501-08. quiz 141–102. [DOI] [PubMed] [Google Scholar]
- Parker S, Wall T. Job and Work Design. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Pasmore WA. Designing Effective Organizations: The Sociotechnical Systems Perspective. New York: John Wiley & Sons; 1988. [Google Scholar]
- Patterson ES, Wears RL. Patient handoffs: Standardized and reliable measurement tools remain elusive. The Joint Commission Journal on Quality and Patient Safety. 2010;36(2):52–61. doi: 10.1016/s1553-7250(10)36011-9. [DOI] [PubMed] [Google Scholar]
- Patterson ES, Woods DD, Roth EM, Cook RI, Wears RL, Render ML. Three key levers for achieving resilience in medication delivery with information technology. Journal of Patient Safety. 2006;2:33–38. [Google Scholar]
- Peleg R, Froimovici M, Peleg A, Milrad V, Ohana G, Fitoussi S, Shvartzman P. Interruptions to the physician-patient encounter: An intervention program. Israel Medical Association Journal. 2000;2(7):520–522. [PubMed] [Google Scholar]
- Peltier J, Dahl A, Mulhern F. The Forum: Business Results Through People. Vol. 2012. Northwestern University; Evanston, IL: 2009. The Relationship Between Employee Satisfaction and Hospital Patient Experiences. The Forum. [Google Scholar]
- Perrow C. A framework for the comparative analysis of organizations. American Sociological Review. 1967;32:194–208. [Google Scholar]
- Perry S. Transitions in care: Studying safety in emergency department signovers. Focus on Patient Safety. 2004;7(2):1–3. [Google Scholar]
- Phipps DL, Parker D, Meakin GH, Beatty PCW. Determinants of intention to deviate from clinical practice guidelines. Ergonomics. 2010;53(3):393–403. doi: 10.1080/00140130903428650. [DOI] [PubMed] [Google Scholar]
- Phipps DL, Parker D, Pals EJM, Meakin GH, Nsoedo C, Beatty PCW. Identifying violation-provoking conditions in healthcare setting. Ergonomics. 2008;51(11):1625–1642. doi: 10.1080/00140130802331617. [DOI] [PubMed] [Google Scholar]
- Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients. Journal of the American Medical Association. 2002;288(17):2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- Pronovost P, Needham D, Berenholtz SM, Sinopoli D, Chu H, Cosgrove S, Goeschel C. An intervention to decrease catheter-related bloodstream infections in the ICU. New England Journal of Medicine. 2006;355(26):2725–2732. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- Rasmussen J. Risk management in a dynamic society: A modelling problem. Safety Science. 1997;27(2/3):183–213. [Google Scholar]
- Reason J. Human error: Models and management. British Medical Journal. 2000;320:768–770. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reason J. Beyond the organisational accident: The need for “error wisdom” on the frontline. Quality & Safety in Health Care. 2004;13(Suppl II):ii28–ii33. doi: 10.1136/qshc.2003.009548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reason J. The Human Contribution: Unsafe Acts, Accidents, and Heroic Recoveries. Burlington, VT: Ashgate Publishing Company; 2008. [Google Scholar]
- Reason J, Parker D, Lawton R. Organizational controls and safety: The varieties of rule-related behavior. Journal of Occupational and Organizational Psychology. 1998;71:289–304. [Google Scholar]
- Reddy MC, Gorman P, Bardram J. Special issue on Supporting collaboration in healthcare settings: the role of informatics. International Journal of Medical Informatics. 2011;80:541–543. doi: 10.1016/j.ijmedinf.2011.05.001. [DOI] [PubMed] [Google Scholar]
- Reiling J, Chernos S. Human factors in hospital safety design. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Mahwah, NJ: Lawrence Erlbaum Associates; 2007. pp. 275–286. [Google Scholar]
- Rivera-Rodriguez AJ. Interruptions in healthcare: A qualitative study from the interrupter’s perspective. The University of Wisconsin-Madison; 2012. [Google Scholar]
- Rivera-Rodriguez AJ, Karsh B-T. Interruptions and distractions in healthcare: Review and reappraisal. Quality & Safety in Health Care. 2010;19(4):304. doi: 10.1136/qshc.2009.033282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runciman B, Merry A, Walton M. Safety and Ethics in Healthcare: A Guide to Getting it Right. Aldershot, UK: Ashgate; 2007. [Google Scholar]
- Rutledge T, Stucky E, Dollarhide A, Shively M, Jain S, Wolfson T, Dresselhaus T. A real-time assessment of work stress in physicians and nurses. Health Psychology. 2009;28(2):194–200. doi: 10.1037/a0013145. [DOI] [PubMed] [Google Scholar]
- Saleem JJ, Russ AL, Neddo A, Blades PT, Doebbeling BN, Foresman BH. Paper persistence, workarounds, and communication breakdowns in computerized consultation management. International journal of medical informatics. 2011;80(7):466–479. doi: 10.1016/j.ijmedinf.2011.03.016. [DOI] [PubMed] [Google Scholar]
- Schatzman L. Dimensional analysis: Notes on an alternative approach to the grounding of theory in qualitative research. In: Maines DR, editor. Social organization and social process: Essays in honor of Anselm Strauss. New York: Aldine De Gruyter; 1991. pp. 303–314. [Google Scholar]
- Schaufeli WB. Burnout in health care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Mahwah, NJ: Lawrence Erlbaum Associates; 2007. pp. 217–232. [Google Scholar]
- Schroeder ME, Wolman RL, Wetterneck TB, Carayon P. Tubing misload allows free flow event with Smart intravenous infusion pump. Anesthesiology. 2006;105(2):434–435. doi: 10.1097/00000542-200608000-00038. [DOI] [PubMed] [Google Scholar]
- Schultz K, Carayon P, Hundt AS, Springman S. Care transitions in the outpatient surgery preoperative process: Facilitators and obstacles to information flow and their consequences. Cognition, Technology & Work. 2007;9(4):219–231. [Google Scholar]
- Schumacher RM, Lowry SZ. NIST Guide to the Processes Approach for Improving the Usability of Electronic Health Records. NIST; 2010. [Google Scholar]
- Schumacher RM, Webb JM, Johnson KR. How to select an electronic health record system that healthcare professionals can use. Oakbrook Terrace, IL: User Centric, Inc; 2009. [Google Scholar]
- Sexton JB, Thomas EJ, Helmreich RL. Error, stress, and teamwork in medicine and aviation: Cross sectional surveys. British Medical Journal. 2000;320(745):745–749. doi: 10.1136/bmj.320.7237.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaller D. Patient-centered care: What does it take? The Common Wealth Fund; 2007. pp. 1–34. [Google Scholar]
- Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, Freischlag J. Burnout and medical errors among American surgeons. Annals of Surgery. 2010;251(6):995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, Oreskovich MR. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine. 2012:1–9. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- Shcherbatykh I, Holbrook A, Thabane L, Dolovich L. Methodologic issues in health informatics trials: The complexities of complex interventions. Journal of the American Medical Informatics Association. 2008;15(5):575–580. doi: 10.1197/jamia.M2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shekelle PG. Nurse–patient ratios as a patient safety strategy: A systematic review. Annals of Internal Medicine. 2013;158(5_Part_2):404–409. doi: 10.7326/0003-4819-158-5-201303051-00007. [DOI] [PubMed] [Google Scholar]
- Shekelle PG, Pronovost PJ, Wachter RM, Taylor SL, Dy SM, Foy R, Walshe K. Advancing the science of patient safety. Annals of Internal Medicine. 2011;154(10):693–696. doi: 10.7326/0003-4819-154-10-201105170-00011. [DOI] [PubMed] [Google Scholar]
- Shekelle PG, Pronovost P, Wachter R. Assessing the Evidence for Context-Sensitive Effectiveness and Safety of Patient Safety Practices: Developing Criteria. Rockville, MS: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- Smetzer J, Baker C, Byrne FD, Cohen MR. Shaping systems for better behavioral choices: Lessons learned from a fatal medication error. The Joint Commission Journal on Quality and Patient Safety. 2010;36(4):152–163. doi: 10.1016/s1553-7250(10)36027-2. [DOI] [PubMed] [Google Scholar]
- Smith MA, Bartell JM. The relationship between physician professionalism and health care systems change. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. Mahwah, NJ: Lawrence Erlbaum Associates; 2007. pp. 139–146. [Google Scholar]
- Smith MJ, Carayon-Sainfort P. A balance theory of job design for stress reduction. International Journal of Industrial Ergonomics. 1989;4(1):67–79. [Google Scholar]
- Smith MJ, Carayon P. Balance theory of job design. In: Karwowski W, editor. International Encyclopedia of Ergonomics and Human Factors. London: Taylor & Francis; 2001. pp. 1181–1184. [Google Scholar]
- Stanton N, Hedge A, Brookhuis K, Salas E, Hendrick HW, editors. Handbook of Human Factors and Ergonomics Methods. Boca Raton, FL: CRC Press; 2004. [Google Scholar]
- Stead WW, Lin HS, editors. Computational Technology for Effective Health Care: Immediate Steps and Strategic Directions. Washington, D.C: National Academies Press; 2009. [PubMed] [Google Scholar]
- Tashakkori A, Creswell J. Exploring the nature of research questions in mixed methods research. Journal of Mixed Methods Research. 2007;1(3):207–211. [Google Scholar]
- Taylor JA, Dominici F, Agnew J, Gerwin D, Morlock L, Miller MR. Do nurse and patient injuries share common antecedents? An analysis of associations with safety climate and working conditions. British Medical Journal Quality & Safety. 2012;21(2):101–111. doi: 10.1136/bmjqs-2011-000082. [DOI] [PubMed] [Google Scholar]
- Thomas NK. Resident burnout. Journal of the American Medical Association. 2004;292(23):2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- Trbovich PL, Pinkney S, Cafazzo JA, Easty AC. The impact of traditional and smart pump infusion technology on nurse medication administration performance in a simulated inpatient unit. Quality & Safety in Health Care. 2010;19:430–434. doi: 10.1136/qshc.2009.032839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trist E. The Evolution of Socio-technical Systems. Toronto: Quality of Working Life Center; 1981. [Google Scholar]
- U.S. Department of Health Care and Human Services Office of Inspector General. Adverse events in hospitals: National incidence in medicare beneficiaries. U.S. Department of Health Care and Human Services; 2012. [Google Scholar]
- van Walraven C, Jennings A, Taljaard M, Dhalla I, English S, Mulpuru S, Forster AJ. Incidence of potentially avoidable urgent readmissions and their relation to all-cause urgent readmissions. Canadian Medical Association Journal. 2011;183(14):E1067–1072. doi: 10.1503/cmaj.110400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent C. Patient Safety. Chichester, UK: Wiley-Blackwell; 2010. [Google Scholar]
- Vincent C, Moorthy K, Sarker SK, Chang A, Darzi AW. Systems approaches to surgical quality and safety: From concept to measurement. Annals of Surgery. 2004;239(4):475–482. doi: 10.1097/01.sla.0000118753.22830.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. British Medical Journal. 1998;316(7138):1154–1157. doi: 10.1136/bmj.316.7138.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waterson P. A critical review of the systems approach within patient safety research. Ergonomics. 2009;52(10):1185–1195. doi: 10.1080/00140130903042782. [DOI] [PubMed] [Google Scholar]
- Wears RL. The chart is dead: Long live the chart. Annals of Emergency Medicine. 2008;52(4):390–391. doi: 10.1016/j.annemergmed.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Wears RL, Perry SJ, Shapiro M, Beach C, Croskerry P, Behara R. The Human Factors and Ergonomics Society, editor. Proceedings of the Human Factors and Ergonomics Society 47th Annual Meeting. Santa Monica, CA: The Human Factors and Ergonomics Society; 2003. Shift changes among emergency physicians: Best of times, worst of times; pp. 1420–1423. c ed. [Google Scholar]
- Weick KE. Making Sense of the Organization. Oxford, UK: Blackwell Publishers; 2001. [Google Scholar]
- Weinger MB, Wiklund M, Gardner-Bonneau D, editors. Handbook of Human Factors in Medical Device Design. Boca Raton, FL: CRC Press; 2011. [Google Scholar]
- Westbrook JI, Woods A, Rob MI, Dunsmuir W, Day RO. Association of interruptions with an increased risk and severity of medication administration errors. Archives of Internal Medicine. 2010;170(8):683–690. doi: 10.1001/archinternmed.2010.65. [DOI] [PubMed] [Google Scholar]
- Wetterneck TB. Error recovery in health care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2. Boca Raton, FL: Taylor & Francis; 2012. pp. 763–774. [Google Scholar]
- Wetterneck TB, Skibinski KA, Roberts TL, Kleppin SM, Schroeder ME, Enloe M, Carayon P. Using failure mode and effects analysis to plan implementation of smart i.v. pump technology. American Journal of Health-System Pharmacy. 2006;63(16):1528–1538. doi: 10.2146/ajhp050515. [DOI] [PubMed] [Google Scholar]
- Wetterneck TB, Walker JM, Blosky MA, Cartmill RS, Hoonakker P, Johnson MA, Carayon P. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. Journal of the American Medical Informatics Association. 2011;18(6):774–782. doi: 10.1136/amiajnl-2011-000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM., 3rd Disruptions in surgical flow and their relationship to surgical errors: An exploratory investigation. Surgery. 2007;142(5):658–665. doi: 10.1016/j.surg.2007.07.034. [DOI] [PubMed] [Google Scholar]
- Williams ES, Halbesleben JRB, Manwell LB, McMurray JE, Rabatin J, Rashid A, Linzer M. The effect of workplace health care worker stress and burnout on patient outcomes. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2. Boca Raton, FL: Taylor & Francis Group; 2012. pp. 119–131. [Google Scholar]
- Williams ES, McMurray J, Baier-Manwell L, Schwartz MD, Linzer M. Effect of workplace stress on patient outcomes. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Patient Safety. Mahwah, NJ: Lawrence Erlbaum; 2007. pp. 181–197. [Google Scholar]
- Williams ES, Halbesleben, Jonathon RB, Manwell Linda Baier, McMurray Julia E, Rabatin Joseph, Rashid Ayesha, Linzer Mark. The effect of workplace health care worker stress and burnout on patient outcomes. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2. Boca Raton, FL: Taylor & Francis Group; 2012. pp. 119–131. [Google Scholar]
- Wilson JR. Participation: A framework and a foundation for ergonomics? Journal of Occupational Psychology. 1991;64:67–80. [Google Scholar]
- Wilson JR. A framework and a context for ergonomics methodology. In: Wilson JR, Corlett EN, editors. Evaluation of Human Work - A Practical Ergonomics Methodology. 2. London: Taylor & Francis; 1995. pp. 1–39. [Google Scholar]
- Wilson JR. Fundamentals of ergonomics in theory and practice. Applied Ergonomics. 2000;31(6):557–567. doi: 10.1016/s0003-6870(00)00034-x. [DOI] [PubMed] [Google Scholar]
- Woods DD. Essential characteristics of resilience. In: Hollnagel E, Woods DD, Leveson N, editors. Resilience Engineering - Concepts and Precepts. Burlington, Vermont: Ashgate; 2006. pp. 21–34. [Google Scholar]
- Woods DD, Cook R. From counting failures to anticipating risk: Possible futures for patient safety. In: Zipperer L, Cushman S, editors. Lessons in Patient Safety. Chicago, IL: National Patient Safety Foundation; 2001. pp. 89–97. [Google Scholar]
- Woods DD, Hollnagel E. Joint Cognitive Systems: Patterns in Cognitive Systems Engineering. Boca Raton, FL: CRC Press; 2006. [Google Scholar]
- Woolf SH. The meaning of translational research and why it matters. Journal of the American Medical Association. 2008;299(2):211–213. doi: 10.1001/jama.2007.26. [DOI] [PubMed] [Google Scholar]
- Xiao Y, Seagull FJ, Mackenzie CF, Klein K. Adaptive leadership in trauma resuscitation teams: A grounded theory approach to video analysis. Cognition, Technology & Work. 2004;6:158–164. [Google Scholar]
- Yen PY, Bakken S. Review of health information technology usability study methodologies. Journal of the American Medical Informatics Association. 2012;19(3):413–422. doi: 10.1136/amiajnl-2010-000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayas-Cabán T, Brennan PF. Human factors in home care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Patient Safety. Mahwah, NJ: Lawrence Erlbaum; 2007. pp. 883–897. [Google Scholar]
- Zayas-Caban T, Dixon BE. Considerations for the design of safe and effective consumer health IT applications in the home. Quality & safety in health care. 2010;19(Suppl 3):i61–67. doi: 10.1136/qshc.2010.041897. [DOI] [PubMed] [Google Scholar]
- Zink K. Ergonomics in the past and the future: From a German perspective to an international one. Ergonomics. 2000;43(7):920–930. doi: 10.1080/001401300409116. [DOI] [PubMed] [Google Scholar]