Abstract
Background:
Rapid response team (RRT) has been implemented in developed countries with the aim of early recognition and response to critical care triggers for the better patient outcome. However, the data concerning their efficacy is hardly available until date from Indian subcontinent.
Aims:
To evaluate the impact of RRT implementation on patient outcome during medical emergencies.
Settings and Design:
Retrospective observational study of RRT records of in-bed patients of super specialty academic teaching hospital.
Materials and Methods:
RRT record forms during the first half of the year from January 2012 to June 2012 were included for all inpatients and out-patients irrespective of their age, gender and diseases profile after their inclusion in the system. Outcomes such as patient stayed in the room, patient transfer to intensive care unit (ICU), patient discharge and generation of code blue event, mortality and length of stay in hospital/ICU were measured.
Statistical Analysis:
Descriptive analysis was performed with the help of statistical software STATA 9.0 and R 2.13.2 (StataCorp LP, Lakeway Drive College Station, Texas, USA).
Results:
Analysis of 41 RRT calls showed decreased code blue calls by 2.44% and decrease in mortality by 4.88%. Average length of stay in ICU and hospital post RRT assistance for patients was 2.55 and 6.95 days respectively. Conversely percentage of patients requiring a higher level of care was more (75.61%) than those who stayed in their rooms/wards (24.39%).
Conclusion:
Implementation of RRT in this hospital was associated with reduced code blue events and its attendant mortality outside the ICU settings. However, more number of patient requiring higher levels of care delineates the need for a larger evidence based medicine study.
Keywords: Code blue events, evidence based medicine, medical emergency team, rapid response team, rationale therapeutics, serious adverse events
INTRODUCTION
The rate of serious adverse events in hospitalized patients ranges from 2.9%-17% of cases.[1,2] In another study, fourth to sixth the most common cause of deaths have been ascribed to the drug related problems.[3] Many of such presentation may not be related to the patient's original diagnosis, underlying medical conditions or drug related problems including the serious adverse events. However, outcome of such events may result in prolongation of existing hospitalization, permanent disability and death. Incomplete assessment of such unexpected events may result in increased fatalities.
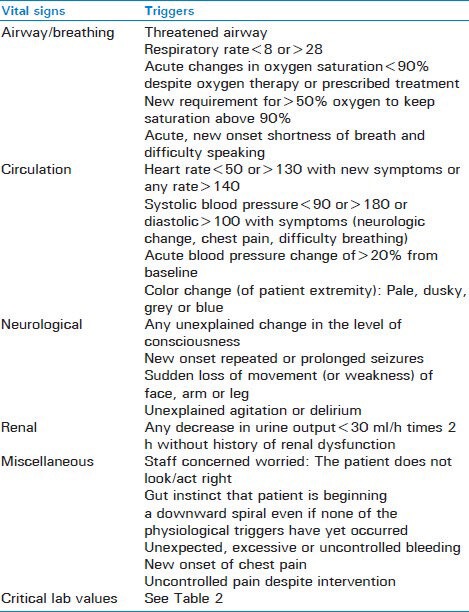
Incomplete assessments of patients, breakdowns in communication (i.e., between patients and nurses, between nurses and physicians), insufficiencies in therapies and lack of adequate follow-up of patients after an intervention not only contribute to failure to rescue, but also lead to suboptimal patient care. Several studies show that abnormal vital signs [Table 1] can help identify clinical deterioration in patients minutes to hours before a serious adverse event occurs.[4,5] Most of the conditions eventually lead to organ failure and can culminate into cardiopulmonary arrests.
Table 1.
Abnormal vital sign triggers for activating rapid response team
Cardiopulmonary arrests and its attendant mortality in patients coming to or admitted in hospitals are common and their delayed intervention is associated with lower survival rate and poor neurological outcome.[6] It has been observed that almost half of the cases of cardiopulmonary arrests are preceded by deterioration in vital signs or other clinical indices 6-8 h prior to arrest.[7,8,9,10] Therefore, early recognition of activating triggers and generating codes may provide a window of opportunity for averting cardiopulmonary arrest and its attendant mortality.[11]
The codes are used in hospitals world-wide to alert staff to various emergencies. “Code blue” is generally used to indicate a patient requiring resuscitation most often as the result of a cardiac arrest. Until date, Indian hospitals are dependent on code blue team for any medical emergency. These code blue teams double up as rapid response teams (RRT) in many developed countries as well as where personnel trained in critical care is limited resource.
The growing understanding into unexpected clinical deterioration and increased cardiopulmonary arrest cases advocate the need of RRTs that is also known as a medical emergency teams in some regions. Unanticipated clinical deterioration is often the precursor of cardiac arrest and death.[12] Hence, it has been considered that, earlier the clinical deterioration detected and treated the better is the likelihood of a favorable outcome.[10]
RRTs have gained interest all over the world as a means of providing medical care of the highest quality and process of getting improvement in patient outcome. Moreover, implementation of RRT program has been considered as a solution to inappropriate and/or inadequate treatment of patients.[13,14,15,16,17,18] In an initiative, known as “100,000 Lives Campaign” promoted by the institute for health-care improvement, one out of six recommended strategies was the recommendation of instituting RRT to reduce the number of preventable in-patient deaths in the United States between the period of 2004-2006.[19] However, this trend has not been percolated in the developing countries like India where still a framed process is not in vogue.
RRT is a group of health-care professionals involving an intensivist on call such as physician/respiratory therapist and a registered nurse. RRT team members must be available 24 h for a day and 7 days a week for evaluation of those patients who are not in the intensive care unit (ICU) but develop signs and symptoms of clinical deterioration[20] so as to deliver critical care expertise in an attempt to avoid further clinical deterioration and cardiopulmonary arrests and codes.[21] Hence RRT is activated when a patient begins to deteriorate and before the patient experiences a cardiac or pulmonary arrest.
Because there was no proper system of evaluation of emergencies in this part of the world, this pilot study was planned to evaluate the outcome of the recently introduced RRT activation in an Indian tertiary care corporate academic hospital set up.
MATERIALS AND METHODS
The study was carried out after the approval both form scientific committee and Institutional Ethics Committee of the Max, Super Specialty Hospital, Saket, New Delhi, India. Since it was a retrospective study, requirement for informed consent was waived. It involved evaluation of the effect of RRT activation on patient outcome in medical emergencies. We conducted a retrospective analysis of the RRT data of patients available for the period of January 2012 to June 2012 at a tertiary care corporate academic hospital in South Delhi.
The RRT in this tertiary care hospital consisted of mainly five members namely a critical care consultant on duty as team leader, junior consultant/ICU senior resident internal medicine and a nursing supervisor. It can be activated by assigned nurse or floor/duty doctor or by any other staff (first responder) by dialing a two digit number at the designated call center of the hospital. Once an activation call is made, the RRT team is expected to reach at the spot within 5 min to assess the patient and assign the intervention required to stabilize the condition of the patients. In addition, the RRT would discuss management with the patient's primary physician and determine the need for additional intensive monitoring. Because different hospitals have different facilities, RRT team differs accordingly for each block at our hospital as well. RRT record forms [Figure 1] of all in-patients and out-patients, irrespective of their age, gender and disease, were included. Forms, which were not filled properly or were unclear, excluded from the study.
Figure 1.
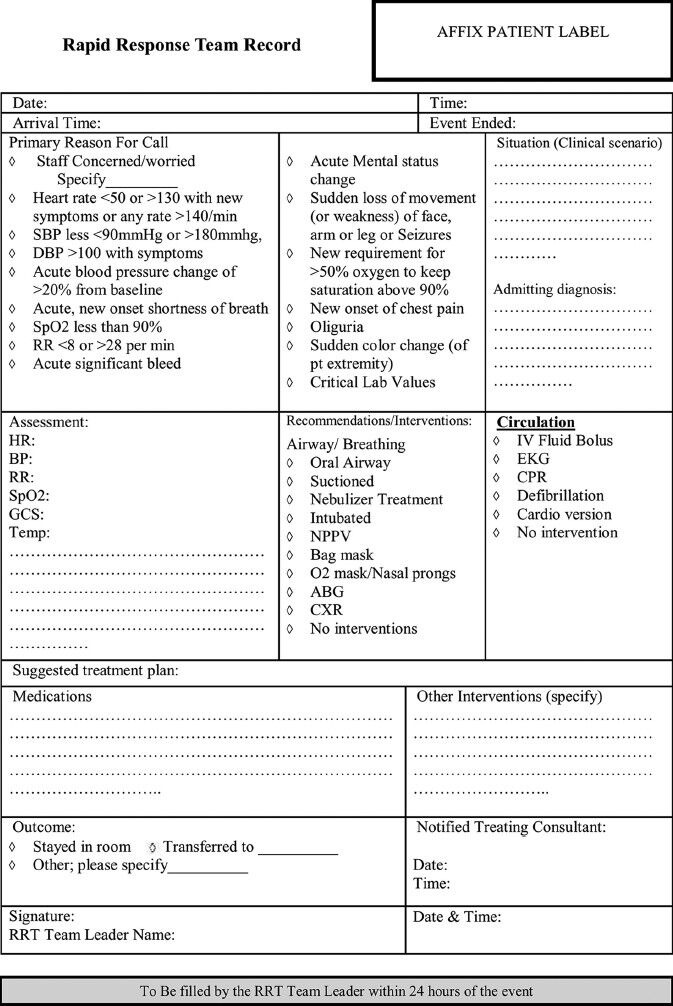
Rapid response team record form
Outcome measures
Primary outcome measures evaluated for the purpose of study included: Patient stayed in the room and was shifted to ICU, occurrence of code blue event, mortality, patient discharged and length of stay of patient in ICU or hospital.
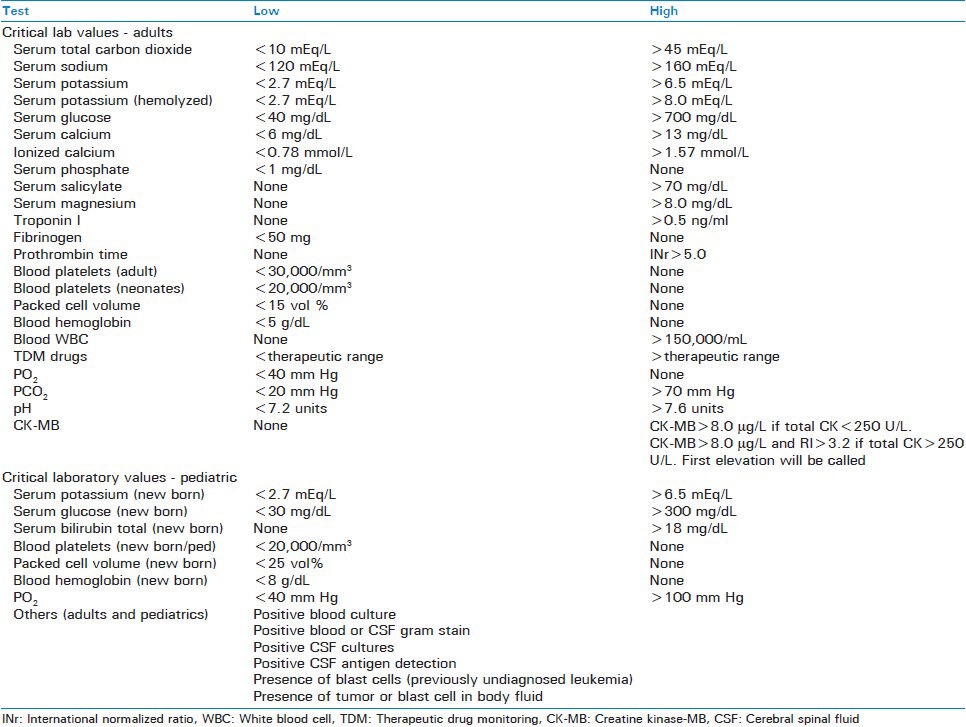
As a part of the study protocol, RRT records were also assessed for determining the primary reasons for RRT activation (staff concerned/worried, altered heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure, respiratory rate (RR) and SpO2, acute blood pressure change, new onset shortness of breath, acute significant bleed, acute mental status change, sudden loss of movement, new requirement of O2 to keep saturation above 90%, new onset of chest pain, critical lab values [Table 2]), activation occurring per month, age profile of patients, gender profile of patients and activation for patients in different diseased condition.
Table 2.
Critical laboratory values
Statistical analysis
The evaluation of the impact of RRT activation in medical emergencies on patient outcome from the respective RRT data was carried out by descriptive analysis. Descriptive analysis such as the number of subjects (n), mean, median, standard deviation, minimum and maximum for continuous data and frequencies and percentages for categorical data was used.
For patients who stayed in the room and for those who were transferred to a higher level of care i.e., transfer to ICU, percentage was calculated out of the total RRT activation. Similarly, percentage was calculated for other factors, which included occurrence of code blue event and mortality. Since all RRT activation occurred for in-patients, none of them was discharged immediately after the RRT assistance. For the length of stay of patients either in a hospital or in ICU, mean was calculated to get a rough estimate of stay of patients in hospital/ICU after RRT assistance.
Primary reasons for activation, disease profile and gender profile of patients were all calculated in terms of percentage. However, the age of patients requiring RRT assistance was calculated in terms of mean. Final analysis of the data was performed on STATA 9.0 and R 2.13.2 statistical software.
RESULTS
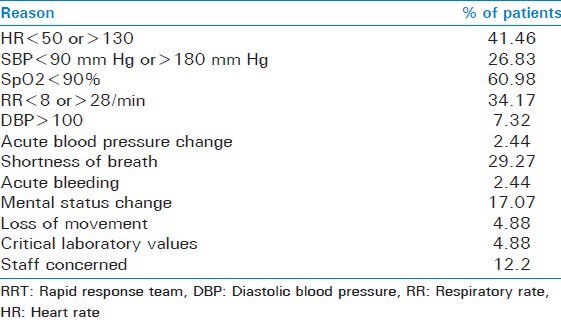
Since our primary objective was to evaluate the impact of RRT assistance on patient outcome, we didn't intend to calculate the RRT dose (i.e., RRT generated per 1000 patients admitted or discharged) or total number of patients coming to or admitted in the hospital. Hence we concentrated only on those patients for whom RRT was activated in emergency situations and the primary reasons [Table 3].
Table 3.
Primary reasons for RRT activation
For the period of January 2012 to June 2012, a total of 51 RRT calls were activated in west block of our hospital where mainly cancer patients admitted. However, out of the total, 10 records were excluded from the study as they met exclusion criteria.
For cases requiring RRT assistance majority of patients were transferred to a higher level of care (75.68%) and relatively low number of patients stayed in the room (19.51%). There was just a single conversion to code blue event (2.44%) while the number of deaths were 2 (4.88%) out of the total cases. Since all RRT activations were for in-patients, patients either stayed in the room or they were returned to their rooms from ICU after stabilization. Survival to discharge post RRT assistance for the patients was found to be 95.12%. Mean length of stay for patients in hospital and in ICU was found to be 6.95 and 2.55 days respectively. A change in readings of oxygen saturation pressure, HR and RR were the most frequent triggerss that lead to RRT activation. Change in SpO2 constituted more than 50% of cases. Shortness of breath was obsereved in 29% of cases followed by 27% of cases with altered SBP. Nearly, 17% of the total cases reflected a change in the mental status of patients that lead to RRT trigger. 12% of the RRT activation occured because staff had a strong feeling that something is grossly wrong with the patient, which can not be pointed out. RRT was activated mostly (41%) for the cancer patients. Cardiac and respiratory triggers constituted second largest fraction (22% each). Neurological triggers constituted 7.32% cases followed by cardiopulmonary diseases 4.88% and gastrointestinal tract triggers 2.44%. Mean age of patients requiring RRT assistance was 59.80 years. The incidence of emergencies requiring RRT assistance was higher in males (65.85%) than in females (34.15%).
DISCUSSION
This study was conducted retrospectively to evaluate the effect of RRT at a corporate tertiary care academic hospital on patient outcome. To our knowledge this is the first of its kind study conducted, documenting the need and efficacy of RRT in an Indian hospital. Earlier when there was no RRT in our hospital there had been the high rate of patients being admitted to ICU through wards. Many of these were urgent transfers after a code blue. Code blue team was doubling up as RRT in the present set up. For non-code situations, the process for ICU transfer was complex. The situation in the ward was perplexed regarding calling criteria for a non-cardiac arrest scenario and the response team. The response to such emergencies was not always urgent and protocol based. The hospital was in dire need of a protocol based system like RRT. Consequently RRT was implemented for the management of hospital emergencies. Implementation of RRT may be associated with reduction of code blue and a trend toward reduced mortality. However, despite a decrease in code blue events fair fraction of patients required a higher level of care i.e., there were more numbers of transfers to ICU. It was considerably higher than those who stayed in the room. Reason for this may be attributed to the fact that either there was a delay in RRT activation or it was due to more critical subset of the patients admitted in hospital wards.
Our study, though, underpowered (due to shorter duration and comparatively smaller sample size) to detect a decrease in the hospital mortality corresponding to the observed 17% and 33.8% decrease in cardiopulmonary arrests, but is a rise up initiative.[11,17] The evidence on RRT world-wide is overwhelming and this just serve as a primer for our health-care settings. A larger study may provide data for the generalization to other hospitals or RRT programs.
As a part of the primary outcome measures we also calculated the average length of stay of the patients post RRT assistance both for ICU (2.55 days) and for the hospital (6.95 days). Due to lack of previous studies in the same hospital or anywhere else for this particular outcome measure, it was difficult to predict whether the values obtained for the length of stay in ICU/hospital were significant.
Among the primary reasons for activation, change in SpO2, HR and RR were the most frequent triggers. Out of all, change in SpO2 constituted 61% cases that lead to RRT activation. In 17% of all the cases analyzed, RRT was called because there was change in the mental status of the patients. It was an interesting finding since these patients were not admitted because of any neurological or behavioral problem. Such patients who are hospitalized on non-behavioral health units can be difficult to address by staff members. Thus, pressing the need for specialized staff like behavior emergency response team[22] to be instituted in future. In this study, it was found that maximum RRT activation were in oncology patients (41.46%) followed by cardiac and respiratory triggers (21.95% each). Most of the seriously ill older patients required long-term critical care support.
The minimum age of the patient requiring RRT assistance was 27 while maximum was 85. Present study indicated a direct relation between the advancing age and requirement for RRT activation since patients with age of 60 years or above required critical care activation most. Mean age was found to be 59.80 years. Interestingly cases of RRT activation were found to be higher in males than in females. A longer duration of such study is required to be performed to know whether this finding is consistent or not. In this hospital, an average of 6.9 RRT activations per month occurred during the period of 6 month with most RRT activation occurring in the first 3 month.
CONCLUSION
Implementation of RRT in our hospital was found to be associated with reduced code blue events and its attendant mortality. For the purpose of evaluating the impact of RRT up to a satisfactory level, randomized controlled trial with sufficiently longer duration should be considered to rigorously evaluate the need and efficacy of RRT.
Training of RRT team members should be considered as one of the most important assets to successful implementation and working of RRT. Calling criteria should be followed strictly and there should be a change in the documentation of RRT to assess its efficacy accurately. For this real time documentation can be looked for integration to hospital information system.
RRT augmentation is particularly effective in long-term ill patients who often require urgent critical interventions. We need to develop objective and subjective criteria to trigger RRT. Implementation and resource allocation of an effective RRT program is paramount to improve critical care in non-designated areas. These programs will set new milestones in clinical quality and safety of ward patients. Critical care is a level of care and expertise that seriously ill patients require.
ACKNOWLEDGMENT
The authors would like to thank Prof. Mushtaq Ahmed Shah, Head of the Department, Department of Pharmacology, SGT Medical Institute, Hospital and Research, Gurgaon, Haryana, India.
Footnotes
Source of Support: Nil
Conflict of Interest: No.
REFERENCES
- 1.Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38:261–71. doi: 10.1097/00005650-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Vincent C, Neale G, Woloshynowych M. Adverse events in British Hospitals: Preliminary retrospective record review. BMJ. 2001;322:517–9. doi: 10.1136/bmj.322.7285.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: A meta-analysis of prospective studies. JAMA. 1998;279:1200–5. doi: 10.1001/jama.279.15.1200. [DOI] [PubMed] [Google Scholar]
- 4.Buist MD, Jarmolowski E, Burton PR, Bernard SA, Waxman BP, Anderson J. Recognising clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care. A pilot study in a tertiary-care hospital. Med J Aust. 1999;171:22–5. doi: 10.5694/j.1326-5377.1999.tb123492.x. [DOI] [PubMed] [Google Scholar]
- 5.Hillman KM, Bristow PJ, Chey T, Daffurn K, Jacques T, Norman SL, et al. Antecedents to hospital deaths. Intern Med J. 2001;31:343–8. doi: 10.1046/j.1445-5994.2001.00077.x. [DOI] [PubMed] [Google Scholar]
- 6.Chan PS, Krumholz HM, Nichol G, Nallamothu BK American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 7.Franklin C, Mathew J. Developing strategies to prevent inhospital cardiac arrest: Analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22:244–7. [PubMed] [Google Scholar]
- 8.Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98:1388–92. doi: 10.1378/chest.98.6.1388. [DOI] [PubMed] [Google Scholar]
- 9.Bedell SE, Deitz DC, Leeman D, Delbanco TL. Incidence and characteristics of preventable iatrogenic cardiac arrests. JAMA. 1991;265:2815–20. [PubMed] [Google Scholar]
- 10.Smith AF, Wood J. Can some in-hospital cardio-respiratory arrests be prevented? A prospective survey. Resuscitation. 1998;37:133–7. doi: 10.1016/s0300-9572(98)00056-2. [DOI] [PubMed] [Google Scholar]
- 11.Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: A systematic review and meta-analysis. Arch Intern Med. 2010;170:18–26. doi: 10.1001/archinternmed.2009.424. [DOI] [PubMed] [Google Scholar]
- 12.Adelstein BA, Piza MA, Nayyar V, Mudaliar Y, Klineberg PL, Rubin G. Rapid response systems: A prospective study of response times. J Crit Care. 2011;26:635.e11–8. doi: 10.1016/j.jcrc.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 13.Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: Preliminary study. BMJ. 2002;324:387–90. doi: 10.1136/bmj.324.7334.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hourihan F, Bishop G, Hillman K, Daffurn K, Lee A. The medical emergency team: A new strategy to identify and intervene in high-risk patients. Clin Intensive Care. 1995;6:269–72. [Google Scholar]
- 15.Repasky TM, Pfeil C. Experienced critical care nurse-led rapid response teams rescue patients on in-patient units. J Emerg Nurs. 2005;31:376–9. doi: 10.1016/j.jen.2005.06.025. [DOI] [PubMed] [Google Scholar]
- 16.Seckel MA, Johnson K. Ask the experts. Rapid response team. Crit Care Nurse. 2005;25:52–5. [PubMed] [Google Scholar]
- 17.DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL, et al. Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care. 2004;13:251–4. doi: 10.1136/qshc.2003.006585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Institute for healthcare improvement. Building rapid response teams. [Cited on 2013 Jan 6]. Available from: http://www.ihi.org/IHI//Topics/CriticalCare/ImprovementStories/BuildingRapidResponseTeams.htm .
- 19.Berwick DM, Calkins DR, McCannon CJ, Hackbarth AD. The 100,000 lives campaign: Setting a goal and a deadline for improving health care quality. JAMA. 2006;295:324–7. doi: 10.1001/jama.295.3.324. [DOI] [PubMed] [Google Scholar]
- 20.Sharek PJ, Parast LM, Leong K, Coombs J, Earnest K, Sullivan J, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a Children's Hospital. JAMA. 2007;298:2267–74. doi: 10.1001/jama.298.19.2267. [DOI] [PubMed] [Google Scholar]
- 21.Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart G, Opdam H, et al. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med. 2004;32:916–21. doi: 10.1097/01.ccm.0000119428.02968.9e. [DOI] [PubMed] [Google Scholar]
- 22.Loucks J, Rutledge DN, Hatch B, Morrison V. Rapid response team for behavioral emergencies. J Am Psychiatr Nurses Assoc. 2010;16:93–100. doi: 10.1177/1078390310363023. [DOI] [PubMed] [Google Scholar]


