Abstract
Using a consensus epitope prediction approach, three rotavirus (RV) peptides that induce cytokine secretion by CD4 T cells from healthy volunteers were identified. The peptides were shown to bind HLA-DRB1*0101 and then used to generate MHC II tetramers. RV specific T cell lines specific for one of the three peptides studied were restricted by MHC class II molecules and contained T cells that bound the tetramer and secreted cytokines upon activation with the peptide. The majority of RV and Flu tetramer+ CD4 T cells in healthy volunteers expressed markers of antigen experienced T cells, but only RV specific CD4 T cells expressed intestinal homing receptors. CD4 T cells from children that received a RV vaccine, but not placebo recipients, were stained with the RV-VP6 tetramer and also expressed intestinal homing receptors. Circulating RV-specific CD4 T cells represent a unique subset that expresses intestinal homing receptors.
Keywords: Rotavirus (RV), T cells, intestinal homing receptors, MHC class II tetramers
INTRODUCTION
Rotavirus (RV) is the leading worldwide cause of severe gastroenteritis in children under the age of 5 years (Tate et al., 2012). Two vaccines (Rotarix™ and Rotateq™) have been included in national immunization programs in many countries (Glass et al., 2012), but their efficacy is relatively low in some African and Asian countries, where they are most needed (Angel et al., 2012). Thus, improvement of current vaccines or generation of new RV vaccines is desirable; however, an important drawback to this end is the lack of optimal immune correlates of protection after vaccination (Angel et al., 2012).
The protective immune response to RV in humans and animals is mediated by intestinal IgA (Blutt et al., 2012; Franco et al., 2006), which is, at least partially, T cell dependent: on the one hand, in the murine model the CD4 T cells are essential for the development of RV-specific intestinal IgA (Franco and Greenberg, 1997). On the other hand, children with T and/or B immunodeficiencies get chronically infected with RV, suggesting that both arms of the immune system are important in clearance of RV infection (Gilger et al., 1992). Our group has observed that higher frequencies of RV-specific CD8 and CD4 T cells secreting IFN-γ circulate in symptomatically infected adults and RV-exposed laboratory workers, compared with healthy volunteers. (Jaimes et al., 2002). In contrast, children with RV diarrhea had low or below detection levels of RV-specific CD8 and CD4 T cells secreting IFN-γ (Jaimes et al., 2002; Mesa et al., 2010; Rojas et al., 2003). Consequently, monitoring of RV-specific CD4 T cells responses after vaccination may require a direct and highly sensitive assay.
The expression of tissue-homing receptors defines subsets of memory T cells that preferentially home to the skin or gut (Butcher and Picker, 1996; Sallusto and Lanzavecchia, 2009). These receptors are imprinted by dendritic cells in developing T cells and promote trafficking properties based on the site-specific expression of their ligands (Sigmundsdottir and Butcher, 2008). Gastrointestinal associated lymphoid tissue dendritic cells metabolize food-vitamin A into retinoic acid, which induces the T cells to express high levels of the gut-homing receptors α4β7 and CCR9, predisposing the migration of the recent activated T cells from the blood to the effector sites in the gut mucosa (Mavigner et al., 2012). The natural ligand of the α4β7 integrin is the mucosal addressing cell adhesion molecule-1 (MAdCAM-1), which is expressed by endothelial cells of the lamina propria along the entire intestine. Whereas, CCL25, the ligand of CCR9, is only expressed by small intestine endothelial and epithelial cells (Mavigner et al., 2012). Thus, T cells that express both markers are conditioned to home to the small intestine.
RV predominantly replicates in mature enterocytes of the small intestine, but also has a systemic dissemination (Blutt et al., 2003) and, consequently, both intestinally and systemically primed T cells are expected to be generated (Franco et al., 2006). Using purified subsets of peripheral blood mononuclear cells (PBMC) that express the intestinal homing receptor α4β7, we found that RV-specific CD4 T cells secreting IFN-γ from adult volunteers preferentially express this receptor (Rojas et al., 2003). With similar studies other investigators have shown that in healthy adults circulating CD4 T cells that proliferate in vitro in response to RV also express α4β7 (Rott et al., 1997). All of these studies have the drawback that subsets of T cells expressing the homing receptor have to be purified before their identification in the functional studies, which may change their phenotype. Moreover, no studies have assessed the expression of CCR9 on human RV-specific T cells.
Recently, the use of MHC class II tetramers for characterization of CD4 T cells populations (Vollers and Stern, 2008) has appeared as a new important tool to characterize antigen-specific T cells against different viruses (Nastke et al., 2012; Nepom, 2012). Also, tetramers have been used to examine the CD4 T cells responses after vaccination against influenza (Flu) (Danke and Kwok, 2003) and anthrax (Laughlin et al., 2007). The tetramers permit the ex vivo quantification and phenotypic characterization of T cells without T cell activation. In the present study, we identified the first HLA-DR1-restricted human RV-specific CD4 T cell epitope, and used MHC class II tetramers to characterize the phenotype of the T cells specific to this epitope. T cells specific for the RV peptide tetramer, but not for a Flu virus peptide-tetramer, expressed intestinal homing receptors. Moreover, antigen experienced CD4 T cells from children that received a RV vaccine, but not from placebo recipients, were stained with the RV tetramer and expressed intestinal homing receptors.
METHODS
Epitope prediction and peptides synthesis
To predict HLA-DR1 (DRB1*0101) binding epitopes, we used the sequences of the RV strain KU G1P[8] form the NCBI genome databases (BAA84966, BAA84967, Q82050.1, BAA84969, BAA84970, AAK15270.1, BAA84962, BAA84963, BAA84964, P13842, BAA84965, BAA03847). Each potential 9-mer binding frame was evaluated using two independent prediction algorithms: P9 (Calvo-Calle et al., 2007; Hammer et al., 1994; Nastke et al., 2012; Sturniolo et al., 1999) and SYFPEITHI (Schuler et al., 2007), as previously described (Calvo-Calle et al., 2007; Nastke et al., 2012). Potential epitopes were selected using cutoff scores of ≥1.5 for P9 and ≥29 for SYFPEITHI. Overall, 1,440 possible 9-mer minimal epitopes were evaluated and 39 potential epitopes, scoring highly for both algorithms, were selected (Supplementary table 1), extended by six residues on each side, and synthesized (Sigma-Aldrich PEPscreen®) with an acetylated N-terminal and amidated C-terminal.
Subjects
After written informed consent was signed, blood samples were obtained from 52 healthy volunteers, 23 to 52 years old that, as expected, had serum antibodies against RV. Frozen PBMC from 35 RV IgA seropositive vaccinated children and 24 RV seronegative placebo recipient children (samples from a previous study (Rojas et al., 2007)), in whom the informed consent authorized further studies, were also assessed. This was a double-blind randomized controlled study, in which children received two doses of either placebo (n = 160) or 106.7 focus-forming units of the attenuated RIX4414 human RV vaccine (precursor of the Rotarix™ vaccine, n = 159). The first and second doses were administered at 2 and 4 months of age, respectively, and children were bled 14–16 days after each dose. Studies were approved by the Ethics Committee of the San Ignacio Hospital and Pontificia Universidad Javeriana.
Human haplotype determination
DNA was obtained from blood samples using Illustra blood genomicPrep Mini Spin Kit (G/E healthcare, UK Buckinghamshire), according to manufacturer’s instructions. The HLA class II haplotype was determined using All set Gold-SSP HLA DRDQ low resolution Kit (Invitrogen Corporation, Wisconsin USA), PCR-based protocols, according to manufacturer’s instructions. All samples identified as a DRB1*01 in low resolution were analyzed for high-resolution using the All set Gold-SSP HLA DRB1*01 high-resolution Kit (Invitrogen Corporation, Wisconsin USA), according to manufacturer’s instructions. (Supplementary table 2).
Antigen stimulation of PBMC and intracellular cytokine staining (ICS)
PBMC were purified from heparinized whole-blood samples by Ficoll-Hypaque gradients (Lympho Separation Medium, MP Biomedicals). The cells were washed twice with RPMI containing 20 mM HEPES, 100 U of penicillin/ml, and 100 mg of streptomycin/ml plus 10% fetal bovine serum (FBS) (all from GIBCO, Carlsbad, CA, USA) (complete medium) and re-suspended in 1ml of AIM-V® medium (life technologies, Carlsbad, CA, USA). PBMC (1×106 cells in a final volume of 1 ml) were stimulated with the supernatant of MA104 cells infected with RRV (Rhesus RV, MOI:7), the supernatant of mock-infected MA104 cells (negative control), the superantigen staphylococcal enterotoxin B (SEB; Sigma, St Louis, Mo, USA), peptides pools (5 peptides per pool at 1 µg/ml each) or individual peptides at different concentrations. Anti-CD28 (0.5 µg/ml) and anti-CD49d (0.5 µg/ml) (Both from BD Biosciences, San Jose, CA) monoclonal antibodies were added to each sample as co-stimulators (Waldrop et al., 1998; Waldrop et al., 1997). Antigen stimulation was done in 15 ml polystyrene tubes (Becton Dickinson Falcon Labware, Franklin Lakes, N.J., USA) incubated with a 5° slant for 10 h at 37°C with 5% CO2. The last 5 h of the incubation included brefeldin A (10 µg/ml; Sigma) to block the secretion of cytokines. At the end of the incubation, the cells were washed once with PBS–0.5% bovine serum albumin (Merck, Darmstadt, Germany) 0.02% sodium azide (Mallinckrodt Chemicals, Paris, Ky.) (Staining Buffer). Then, a 2 mM final concentration of EDTA (GIBCO, N.Y. USA) in PBS was added for 10 min to detach plastic-adherent cells, and the samples were washed once more with Staining Buffer. PBMC were stained with Aqua viability reagent (Invitrogen Molecular Probes, Eugene, OR) in PBS for 10 min at room temperature (RT), and the cells were stained with monoclonal antibodies (Mabs) against CD14-V500 and CD19-V500, as a dump channel, CD3-pacific blue, CD4-PerCP-Cy5.5, and CD8-APC-H7 for 20 min at RT (all from BD Biosciences, San Jose, CA). After two wash steps with Staining Buffer, cells were treated with Citofix/Citoperm solution (BD Biosciences, San Jose, CA) for 30 min at 4°C and washed twice with 1 ml of Perm/Wash solution (BD Bioscience, San Jose, CA). Then, Mabs against IL-2-FITC, IFN-γ-PE-Cy7 and TNF-α-APC (all from BD Biosciences) were added and incubated for 20 min at RT. Production of IL-2 and IFN-γ by RV stimulated T cells was observed in our previous work; TNF-α secretion was also evaluated to make a more comprehensive analysis of multifunctional T cells (Gattinoni et al., 2011). Finally, the cells were washed twice with Perm/Wash, resuspended in 250 µl of Perm/Wash, acquired in a FACSAria flow cytometer (BD Biosciences, San Jose, CA) and analyzed with FlowJo software v.9.3.2.
Peptide binding assays
Peptide binding to DR1 and DR4 was analyzed using an ELISA-based competition assay, as previously described (Parra-López et al., 2006). Purified HLA-DR1 or DR4 molecules (0.05 µM) were diluted with freshly prepared binding buffer (100 mM citrate/phosphate buffer [pH 5.4], 0.15 mM NaCl, 4mM EDTA, 4% NP-40, 4 mM PMSF, and 40 µg/ml for each of the following protease inhibitors: soybean trypsin inhibitor, antipain, leupeptin and chymostatin) containing 0.025 µM biotin-labeled hemagglutinin HA306–318, a well described binding peptide from Flu hemagglutinin (PKYVKQNTLKLAT) (Roche and Cresswell, 1990), and various concentrations of unlabeled competitor peptide (HA306–318, NSP2-3 (SGNVIDFNLLDQRIIWQNWYA), VP3-4 (YNALIYYRYNYAFDLKRWIYL) and VP6-7 (DTIRLLFQLMRPPNMTPAVNA)) in a total volume of 120 µl. Peptides were diluted from stock solutions in binding buffer. After 48h of incubation at RT, 100 µl were transferred to 96-well ELISA microtiter plates (Immuno Modules MaxiSorp, Nunc, Denmark), which had been previously coated overnight with a 10 µg/ml anti-HLA-DR Mab LB3.1, washed, and subsequently blocked with PBS containing 3% bovine serum albumin. After 2 hours of incubation at RT, plates were washed with PBS, 0.05% Tween-20 and incubated for 1h with phosphatase-labeled streptavidin (KPL, Maryland, USA). Captured biotin-labeled peptide/DR complexes were revealed with 4-nitrophenylphosphate substrate (KPL, Maryland, USA). For determining peptide binding to HLA-DR molecules a Ultramark ELISA plate reader (Bio-Rad, CA, USA) with a 405 nm filter was used. Results at each concentration are expressed normalized with respect to the maximum observed binding, and used to calculate IC50 values.
Carboxyfluorescein succinimidyl ester (CFSE) proliferation assay
Proliferation of cells was evaluated by CFSE staining as reported by Quah (Quah and Parish, 2010; Quah et al., 2007), with some modifications. Briefly, 4–10×106 fresh PBMC were resuspended in 1 ml of PBS 1×, placed in a 15 ml conical tube, and stained with CFDA-SE (CellTrace™ CFSE Cell Proliferation Kit). The cells were incubated 5 min at RT, protected from light, and then washed 3 times with 10 ml of PBS 1X-FBS 5% at RT. Finally, the cells were diluted in 1 ml of RPMI supplemented with 10% AB+ human serum (Multicell, human serum AB, Wisent INC, Canada). After CFSE staining, PBMC were stimulated with SEB and three RV peptides (NSP2-3, VP3-4, and VP6-7) for 5 days at 37°C with 5% CO2. Then, cells were harvested, washed twice with PBS 1×, and stained with Violet viability reagent (Invitrogen Molecular Probes, Eugene, OR) in PBS for 10 min; CD3-PE, CD4-PerCP-Cy5.5 and CD8-APC-H7 were added and incubated for 30 min at RT. Finally, the cells were resuspended in 250 µl of PBS, acquired in a FACSAria flow cytometer (BD Biosciences, San Jose, CA) and analyzed with FlowJo software v.9.3.2.
T cell lines
T cell lines were generated from PBMC. 1–2×106 PBMC per well were incubated in 24-well plates in 1 ml of RPMI 1640 supplemented with AB+ human serum 10% (Multicell), 100 U/ml penicillin, 100 µg/ml streptomycin, 1 mM sodium pyruvate, 2 mM L-glutamine, and 1 mM nonessential amino acids. Antigen-specific populations were expanded by culture in the presence of NSP2-3, VP3-4 or VP6-7 peptides (10 µg/ml) or RRV infected MA104 cell lysate (MOI:7). After 48h of incubation at 37°C with 5% CO2, fresh T cell medium supplemented with 100 U/ml IL-2r (Proleukin; Chiron Corporation, Emeryville, CA) was added. This last step was repeated every 2 days until the culture completed 12 days. Then, autologous non-irradiated PBMC (ratio 2:1), pulsed with or without peptide (10 µg/ml) for 1h, were used as source of antigen-presenting cells to stimulate the T cell lines. Finally, T cell lines were evaluated by ICS, as described above. In some cases, the cells were stained as described below with the class II tetramer.
Class II tetramer staining of PBMC from adults and children
Biotinylated HLA-DR1-peptide complexes were prepared using proteins produced in insect cells, as previously described (Cameron et al., 2002). Class II tetramers with different peptides (HA306–318, a transferrin [TRF] control peptide [RVEYHFLSPYVSRKESP (Chicz et al., 1992)], NSP2-3, VP3-4 or VP6-7) were prepared with streptavidin-PE (Invitrogen, MD, USA) from a stock solution at a final concentration of 1 µg diluted in 50 µl of PBS 1×. Fresh PBMC obtained from 8 DR1 healthy adults were washed twice in PBS 1× and distributed in 5 ml polystyrene tubes (5×106 cells/50µl per tube). Frozen PBMC of 3 vaccinated or 3 placebo recipient HLA-DR1 children were thawed at 37°C and washed twice with a 5 ml BenzonaseR (Novagen, San Diego, CA) solution pre-heated at 37°C. Then, the cells were distributed in 5 ml polystyrene tubes. 50 µl of Dasatinib® (Bristol-Myers Squibb Company Princeton, NJ 08543 USA) solution (100 µM) was added to each tube and incubated for 30 min at 37°C (Lissina et al., 2009). Later, 10 µl of AB+ human serum was mixed with the cells just before tetramer solution (1 µg) was added and incubated for 120 min at RT. Unlabeled mouse anti-CCR9 Mab was added and incubated for 20 min at RT, then the cells were washed once with PBS 1×, followed by addition of goat anti-mouse antibodies (AF-488 or Pacific Blue [Invitrogen Corporation, Wisconsin USA]) and incubated for 20 min at RT. The cells were washed once with PBS 1×, then Aqua reagent was added and incubated for 10 min at RT; subsequently, Mabs against CD14-V500 and CD19-V500, as a dump channel, CD3 (Pacific Blue or AF-700), CD4-PerCP-Cy5.5, CD8-APC-H7, CD45RA (FITC or PE-Cy7), CD62L-V450 or CCR7-PE-Cy7, and α4β7-APC (ACT-1) were added and incubated for 20 min at RT. Cells were washed and resuspended in 400 µl of PBS-BSA-sodium azide, acquired in a FACSAria flow cytometer (BD Biosciences, San Jose, CA) and analyzed with FlowJo software v.9.3.2.
ELISA for RV-specific IgA in plasma
For detection of RV-specific IgA, 96-well vinyl micro titer plates were coated with 70 µl of a 1:10 dilution (in PBS, pH 7.4) of supernatant from RF (bovine RV) virus-infected MA104 cells or the supernatant of mock-infected MA104 cells (negative control) and incubated overnight at 4°C. The wells were then blocked with 150 µl of 5% nonfat powdered milk plus 0.1% Tween-20 in PBS (5% BLOTTO) and the plates were incubated at 37°C for 1 h. Then, the BLOTTO was discarded, and 70 µl of serial plasma dilutions in 2.5% BLOTTO were deposited in each well. After 2h of incubation at 37°C, the plates were washed three times with PBS-Tween-20, and 70 µl of biotin-labeled goat anti-human IgA (Kirkegaard & Perry Laboratories, Gaithersburg, Md.) diluted (1:1000) in 2.5% BLOTTO was added to the plates. The plates were then incubated for 1h at 37°C. After three washes with PBS-Tween-20, 70 µl of streptavidin-peroxidase (Kirkegaard & Perry Laboratories, Gaithersburg, Md.) diluted (1:1000) in 2.5% BLOTTO was added, and the plates were incubated for 1h at 37°C. After three washes with PBS-Tween-20, the plates were developed using 70 µl of tetramethyl benzidine substrate (TMB; Sigma, St. Louis, Mo.). The reaction was stopped by the addition of 17.5 µl of sulfuric acid (2 M). Absorbance was read at 450 nm wavelength on an ELISA plate reader (Multiskan EK, Thermolab Systems). Samples were considered positive if optical density (OD) in the well was >0.1 OD units and were two times higher than the OD of the negative control (Rojas et al., 2007).
Statistical analyses
Analysis was performed with GraphPad Prism version 6. Differences between groups were evaluated with the nonparametric Wilcoxon test.
RESULTS
Prediction of RV epitopes
We used a consensus approach that combined P9 binding and SYFPEITHI presentation algorithms to predict HLA-DR1-restricted T cell epitopes (Calvo-Calle et al., 2007) from the KU strain of RV (Table S1). Thirty-nine 9-mer sequences with high scores were selected: 11 were derived from non-structural proteins and the remaining 28 were derived from structural proteins (Table S1). Peptides were synthesized as 21-mers, containing the 9-mer sequence of interest flanked by 6 aa residues on each side.
Screening of peptide pools and identification of individual peptides recognized by CD4 T cells from healthy adults
The 39 peptides were organized in 8 pools of 5 peptides each (pool 8 only had 4 peptides) according to the algorithm score; the 5 peptides with the lowest scores were arranged in pool 1, and the 4 peptides with highest scores were joined in the pool 8. We expected that HLA-DR1-peptides selected would be recognized by CD4 T cells from individuals of other MHC haplotypes, because of the broadly specific “promiscuous” peptide binding motifs characteristic of most human MHC class II protein, that give rise to the concept of “MHC class II supertypes” (Greenbaum et al., 2011). For this reason, all 18 volunteers selected for our screening experiments expressed MHC haplotypes belonging to the DR-1 supertype (Table S2) (Greenbaum et al., 2011).
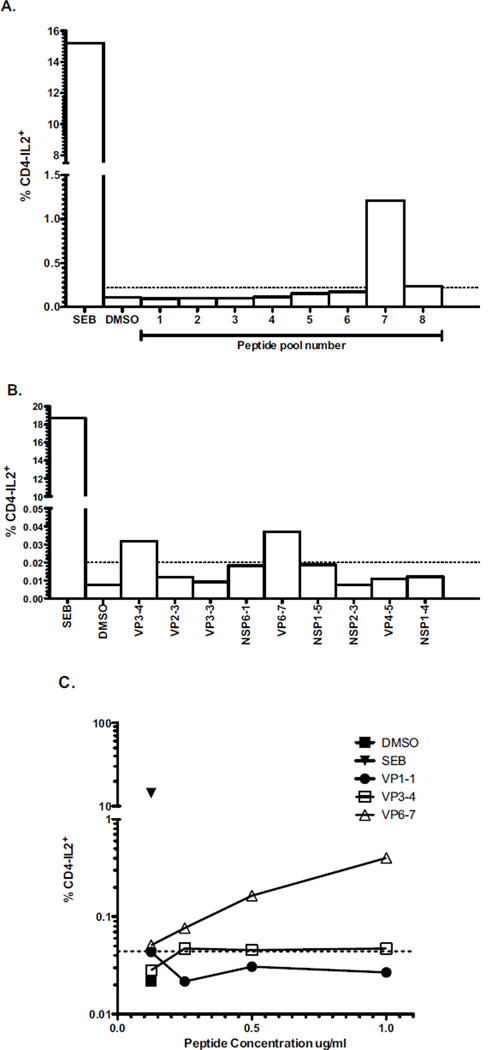
PBMC of 18 healthy volunteers were obtained and CD4 T cell responses to pools of peptides were evaluated by ex-vivo ICS of IFN-γ and IL-2. CD4 T cells from 4 volunteers (HA-02; HA-04; HA-05 and HA-06) responded against the peptide pools: cells from volunteer HA-06 recognized pools 7 and 8 (Fig. 1A), cells from volunteer HA-05 recognized pool 5 (CD4 IL-2+: 0,0232%), and cells from volunteers HA-02 (CD4 IL-2+: 0,0208%) and HA-04 (CD4 IL-2+: 1,284%) recognized pool 7 (data not shown). Positive pools were deconvoluted to individual peptides using the same assay. Fig. 1B shows the frequency of cells from volunteer HA-06 producing IL-2 in response to peptides from pools 7 and 8. Three peptides (VP6-7, NSP2-3, and VP3-4) were found to induce IL-2 production by CD4 T cells from the HLA-DR1-volunteers: VP6-7 induced IL-2 production in cells from volunteers HA-06 (Fig. 1B), HA-02, and HA-04; and also IFN-γ production in cells from HA-06 (data not shown). In addition, VP3-4 induced IL-2 production in cells from volunteer HA-06 (Fig. 1B), and NSP2-3 in cells from HA-04 (data not shown). No response was seen to individual peptides of pool 5 from volunteer HA-05 (data not shown).
Fig. 1. CD4 T cells from one healthy adult recognize peptide pools and individual RV peptides.
PBMC from HA-06 were stimulated with peptide pools (A), or individual peptides (B), at a concentration of 1 µg/ml or with different doses (C) during 10h at 37°C and for the last 5h, 1 µg/ml of brefeldin A was added. The frequencies of T cells producing IL-2 and IFN-γ were evaluated by intracellular cytokine staining. SEB was used as a positive control. Responses were considered positive if the number of IL-2 or IFN-γ-producing CD4 T cells was at least twice that of the DMSO control and above 0.02% (dashed lines). In the experiments shown T cells did not produce IFN-γ.
The percentage of cells producing IL-2 in response to VP6-7 peptide used to stimulate PBMC from the volunteers HA-06 (Fig. 1C), HA-02, and HA-04 (data not shown) was dose dependent. A similar result was obtained stimulating cells from volunteer HA-06 with VP3-4 peptide (Fig. 1C), but no dose effect was observed with cells from volunteer HA-04 stimulated with NSP2-3 (data not shown).
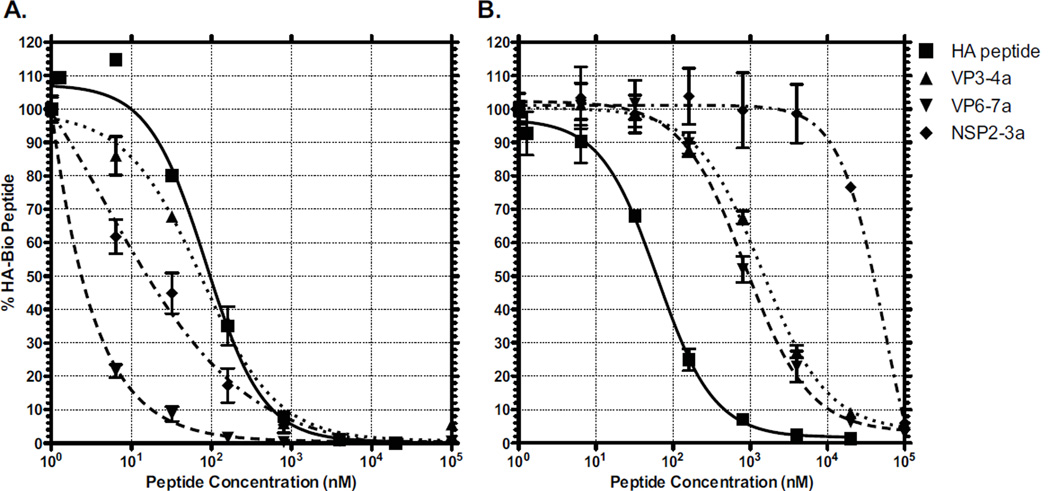
RV peptides bind HLA-DR1 molecules
To evaluate if the initial 9-mer sequences defined using prediction algorithms bind to recombinant DR1 and DR4 MHC molecules, the 9 aa core of the peptides NSP2-3, VP3-4 and VP6-7, with 1aa addition at both ends, were synthetized and tested for HLA-DR1 and HLA-DR4 binding in a competition binding assay with a biotinylated high affinity DR1- and DR4-binding peptide from Flu haemagglutinin HA306–318 (Fig. 2). Compared to HA peptide (IC50 96 nM), VP6-7 (IC50 2 nM) and NSP2-3 (IC50 15 nM) peptides bound to the HLA-DR1 molecules with relatively higher affinity and VP3-4 peptide bound with similar affinity (IC50 73 nM). In contrast, all RV peptides show low affinity binding to the HLA-DR4 molecules (IC50 from 0.8 µM to 55 µM) (Fig. 2). Based on these results, DR1 tetramers were synthetized with the RV peptides NSP2-3, VP3-4, and VP6-7.
Fig. 2. RV peptides bind HLA-DR1 but not HLA-DR4.
Competition binding assays for RV (NSP2-3, VP3-4, and VP6-7) and Flu (HA306–318) peptides were performed. The graphics show inhibition of binding of the biotinylated HA306–318 peptide to HLA-DR1 (A) and HLA-DR4 (B) by increasing amounts of RV and flu peptides. Results were analyzed using GraphPad Prism Software version 6.
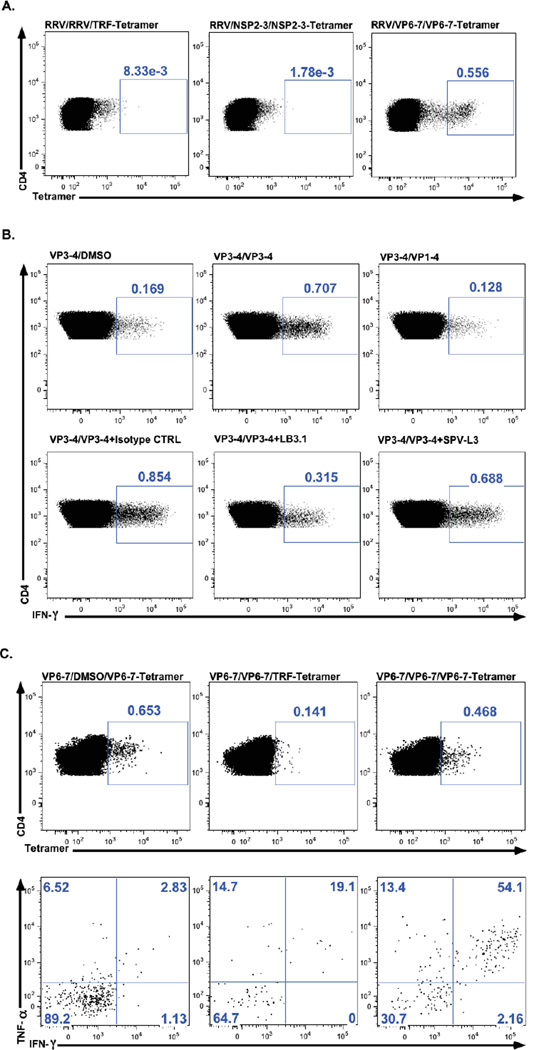
RV peptide VP6-7 is recognized by RRV specific T cell lines
To evaluate if the selected peptides were processed and presented after viral infection, RRV-T cell lines were derived from two HLA-DR1 healthy volunteers (HA-02 and HA-41) and stained with the three RV DR1-tetramers. RRV-T cell lines derived from both volunteers only stained with VP6-7-tetramers (Fig. 3A and data not shown). In addition, after restimulation of RRV-T cell lines from volunteers HA-02 and HA-52 with RRV and VP6-7 peptide, CD4 T cells producing TNF-α and/or IFN-γ were identified in both cases (data not shown). Only one of these cell lines produced cytokines after restimulation with NSP2-3 and neither of them after restimulation with the VP3-4 peptide (data not shown).
Fig. 3. Response of RRV and peptide specific T cell lines.
(A) A RRV-T cell line was obtained from a healthy adult (HA-02), then restimulated with RRV, NSP2-3, VP3-4 or VP6-7, and finally stained with the TFR-tetramer or the corresponding RV-tetramers. Left panel: RRV-T cell line restimulated with RRV and stained with the TRF-tetramer. Middle panel: RRV-T cell line restimulated with NSP2-3 peptide and stained with the NSP2-3-tetramer. Right panel: RRV-T cell line restimulated with VP6-7 peptide and stained with the VP6-7-tetramer. This T cell line only recognizes the VP6-7 tetramer. (B). A VP3-4 specific T cell line from HA-02 was restimulated with DMSO (upper left panel), VP1-4 as a control peptide (upper right panel), or VP3-4 in the absence (upper center panel) or in the presence of an isotype control antibody (lower left panel), LB3.1 (lower center panel), or SPV-L3 (lower right panel) antibodies, which are directed against HLA-DR or HLA-DQ molecules, respectively, and the frequencies of cells producing IFN-γ were evaluated by intracellular cytokine staining. (C) A VP6-7 specific T cell line from HA-02 was stimulated with DMSO (left panels) or VP6-7 (middle and right panels) for 6h at 37°C and stained with the VP6-7-tetramer (upper right and left panels) or TRF-tetramer (upper center panels). Tetramer+ cells were evaluated by ICS for TNF-α and IFN-γ production (lower panels). Numbers inside all graphics represent percentages of populations. Responses were considered positive if the frecuency of TNF-α and/or IFN-γ-producing CD4 T cells was at least twice that of the DMSO control stimulated cells.
RV peptides are presented to CD4 T cells in the context of HLA-DR molecules
To determine if the three RV peptides were presented in the context of HLA-DR molecules, peptide specific T cell lines from two individuals (HA-02 [DRB1*01:01] and HA-06 [DRB1*01:02]) were restimulated with the corresponding or control peptides in the absence or presence of LB3.1 or SPV-L3 antibodies (directed against HLA-DR or HLA-DQ molecules, respectively) and IFN-γ production was evaluated by intracellular cytokine staining. The frequency of CD4 T cells specific for VP6-7, NSP2-3 and VP3-4 producing IFN-γ decreased in the presence of LB3.1, but not in the presence of SPV-L3 (Fig. 3B and data not shown): IFN-γ production of VP3-4-T cell line from HA-02 volunteer was reduced approximately 55% in the presence of LB3.1 and only 6% in the presence of SPV-L3 (Fig. 3B). From volunteer HA-06, only a VP6-7 specific T cell line was obtained and the response of these cells was also specifically inhibited by LB3.1 (data not shown). These results provide additional evidence that RV peptides are presented in the context of HLA-DR molecules, as indicated by tetramer staining.
VP6-7-MHC class II tetramers recognize functional peptide-specific CD4 T cells in T cell lines
To provide additional evidence that VP6-7-tetramers recognize functional VP6-7-specific CD4 T cells, T cell lines from two volunteers (HA-02 and HA-19) were stained with tetramers (TRF or VP6-7) and restimulated with VP6-7 peptide or DMSO (as negative control), and the production of IFN-γ and TNF-α was evaluated by intracellular cytokine staining. When the VP6-7-T cell line from HA-02 was restimulated with VP6-7 peptide almost 70% of the VP6-7-tetramer positive CD4 T cells produced cytokines (TNF-α and/or IFN-γ), whereas in the control stimulated T cell line only a low number (10%) of tetramer positive cells produced cytokines (Fig. 3C). Similar results were obtained with a VP6-7- T cell line derived from HA-19 volunteer (data not shown).
CD4 T cells from DR1 healthy adults proliferate and produce cytokines after stimulation with RV peptides
Fresh PBMC from eight DRB1*0101 (HA-02, HA-15, HA-19, HA-23, HA-25, HA-41, HA-51 and HA-52) and two DRB1*0102 healthy volunteers (HA-04 and HA-06) were stimulated with the three RV peptides and evaluated 10h later by intracellular cytokine staining (IL-2, TNF-α and IFN-γ), and 5 days later for proliferation using CFSE staining. Five DRB1*0101 (HA-15, HA-19, HA-29, HA-51 and HA-52) and one DRB1*0102 (HA-04) healthy adults had detectable levels of cytokine producing CD4 T cells (Table 1). CD4 T cells from HA-15 and HA-19 produced IL-2 after stimulation with VP6-7. CD4 T cells from HA-51 and HA-52 produced TNF-α after stimulation with VP6-7. Cells from HA-29 responded to VP3-4 stimulation producing TNF-α and cells from HA-04 responded to VP3-4 producing TNF-α and to VP6-7 producing IFN-γ (Table 1). CD4 T cells of HA-02 proliferated in response to the three RV peptides (NSP2-3, VP3-4, and VP6-7), whereas CD4 T cells obtained from HA-19 and HA-23 only proliferated to NSP2-3 stimulus. Thus, although approximately 60% of DR1 individuals have peptide-specific T cells detectable by intracellular cytokine staining or proliferation, these responses do not seem to occur simultaneously.
Table 1.
Cytokine production and proliferation of CD4 T cells after stimulation with RV peptides.
| Healthy Adult | Peptide Stimulus |
CD4 T cytokine production |
CD4 T proliferation |
|---|---|---|---|
| HA-02 | NSP2-3 | − | + |
| VP3-4 | − | + | |
| VP6-7 | − | + | |
| HA-15 | NSP2-3 | − | − |
| VP3-4 | − | − | |
| VP6-7 | IL-2(+) | − | |
| HA-19 | NSP2-3 | − | + |
| VP3-4 | − | − | |
| VP6-7 | IL-2(+) | − | |
| HA-23 | NSP2-3 | − | + |
| VP3-4 | − | − | |
| VP6-7 | − | − | |
| HA-29 | NSP2-3 | − | − |
| VP3-4 | TNF-α(+) | − | |
| VP6-7 | − | − | |
| HA-41 | NSP2-3 | − | − |
| VP3-4 | − | − | |
| VP6-7 | − | − | |
| HA-51 | NSP2-3 | − | N.D. |
| VP3-4 | − | N.D. | |
| VP6-7 | TNF-α(+) | N.D. | |
| HA-52 | NSP2-3 | − | N.D. |
| VP3-4 | − | N.D. | |
| VP6-7 | TNF-α(+) | N.D. | |
| HA-04* | NSP2-3 | − | N.D. |
| VP3-4 | TNF-α(+) | N.D. | |
| VP6-7 | IFN-γ(+) | N.D. | |
| HA-06* | NSP2-3 | − | − |
| VP3-4 | − | − | |
| VP6-7 | − | − |
HLA DRB1 0102 Healthy volunteer. N.D. Not Done.
+, at least two-times background values.
Antigen experienced CD4 T cells of healthy volunteers stained with VP6-7-tetramer are enriched in the populations expressing the intestinal homing receptors
Fresh PBMC from the same eight DRB1*0101 healthy donors described above were stimulated with the three RV peptides in order to generate specific T cell lines. Specific T cell lines for VP6-7 were obtained in all eight individuals and specific T cell lines for NSP2-3 and VP3-4 each in four individuals (Table 2). T cell lines from three volunteers (HA-02, HA-51 and HA-52) were expanded with three peptides; T cell lines from two volunteers (HA-15 and HA-19) were expanded with two peptides and T cell lines from three volunteers only recognized VP6-7 (Table 2).
Table 2.
Ex vivo phenotyping of Tetramer+ CD4 T cells of DRB1*0101 healthy adults with RV peptide specific TCLs.
| Healthy Adult | Peptide Tetramer |
#Tet+/6.0×105 CD4+ T cells |
% Antigen experienced T cells* |
% α4β7(+) CCR9(−)# |
% α4β7(+) CCR9(+)# |
% α4β7(−) CCR9(−)# |
% α4β7(−) CCR9(+)# |
|---|---|---|---|---|---|---|---|
| HA-02 | TRF | 8 | 54.5 | 33.3 | 33.3 | 33.3 | 0 |
| FLU | 36 | 68.4 | 42.3 | 7.69 | 50 | 0 | |
| NSP2-3 | 10 | 53.8 | 85.7 | 14.3 | 0 | 0 | |
| VP3-4 | 16 | 61.1 | 54.5 | 9.09 | 27.3 | 9.09 | |
| VP6-7 | 28 | 85.7 | 63.3 | 26.7 | 3.33 | 6.67 | |
| HA-15 | TRF | 4 | 0 | ¥ | ¥ | ¥ | ¥ |
| FLU | 30 | 83.3 | 25 | 12.5 | 62.5 | 0 | |
| VP3-4 | 16 | 23.1 | 50 | 0 | 50 | 0 | |
| VP6-7 | 22 | 63.2 | 63.6 | 27.3 | 9.09 | 0 | |
| HA-19 | TRF | 10 | 85.7 | 8.33 | 33.3 | 33.3 | 25 |
| FLU | 24 | 65.7 | 21.7 | 0 | 78.3 | 0 | |
| NSP2-3 | 18 | 48.1 | 30.8 | 7.69 | 61.5 | 0 | |
| VP6-7 | 26 | 64.1 | 28 | 4 | 64 | 4 | |
| HA-23 | TRF | 8 | 57.1 | 25 | 25 | 50 | 0 |
| FLU | 60 | 91.2 | 32.7 | 3.85 | 61.5 | 1.92 | |
| VP6-7 | 24 | 87 | 75 | 15 | 10 | 0 | |
| HA-29 | TRF | 14 | 50 | 0 | 50 | 50 | 0 |
| FLU | 48 | 59.3 | 6.25 | 12.5 | 81.2 | 0 | |
| VP6-7 | 32 | 38.9 | 57.1 | 14.3 | 28.6 | 0 | |
| HA-41 | TRF | 3 | 100 | 33.3 | 0 | 66.7 | 0 |
| FLU | 42 | 97.1 | 3.03 | 0 | 90.9 | 6.06 | |
| VP6-7 | 25 | 67.3 | 50 | 0 | 50 | 0 | |
| HA-51 | TRF | 98 | 36.7 | 44.8 | 20.7 | 27.6 | 6.9 |
| FLU | 155 | 40.6 | 50.7 | 15.5 | 31 | 2.82 | |
| NSP2-3 | 63 | 31.7 | 34.6 | 30.8 | 26.9 | 7.69 | |
| VP3-4 | 54 | 37.5 | 45.8 | 12.5 | 29.2 | 8.33 | |
| VP6-7 | 50 | 41.5 | 58.8 | 23.5 | 5.88 | 11.8 | |
| HA-52 | TRF | 72 | 27.3 | 66.7 | 0 | 33.3 | 0 |
| FLU | 284 | 25.4 | 40.3 | 8.06 | 50 | 1.61 | |
| NSP2-3 | 140 | 17 | 55.6 | 11.1 | 27.8 | 5.56 | |
| VP3-4 | 149 | 22.6 | 35.7 | 0 | 57.1 | 7.14 | |
| VP6-7 | 134 | 16.5 | 31.2 | 25 | 43.7 | 0 |
Antigen experienced cells are CD62L−,CD45RA+/− and CD62L+ CD45RA− (Figure 4B).
Percentages correspond to antigen experienced cells.
, No antigen experienced cells were identified.
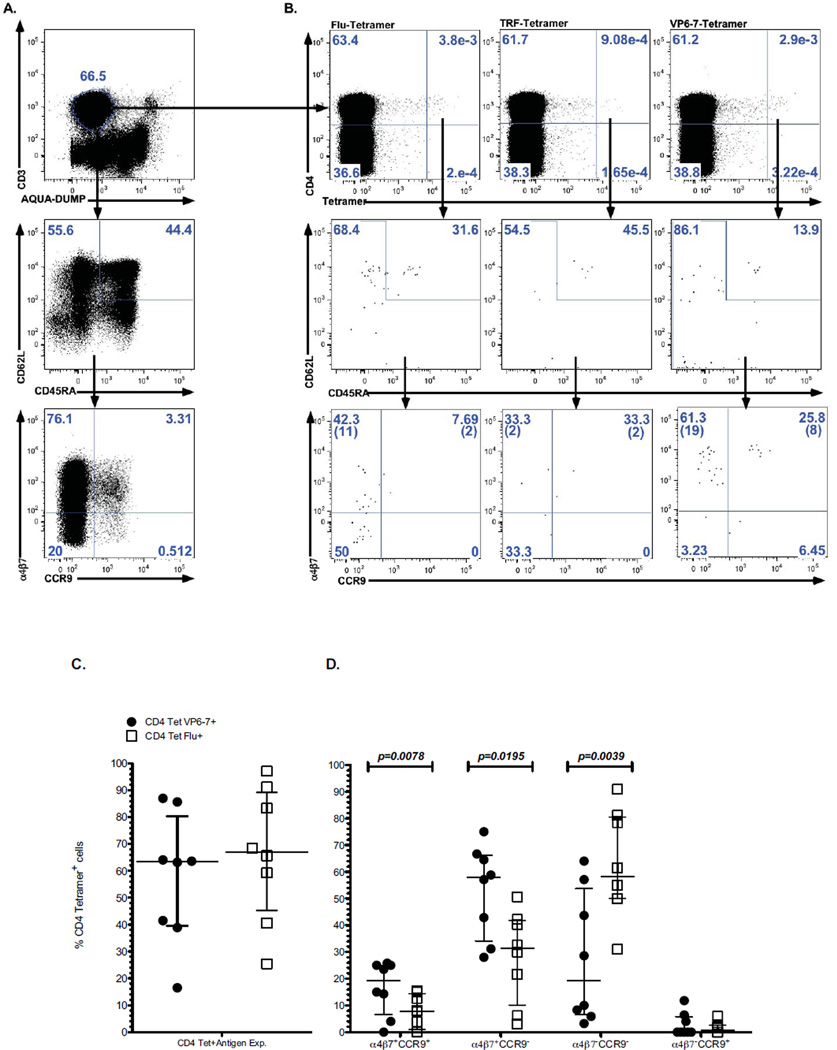
To compare the phenotype of RV- and Flu-specific T cells of the volunteers in which T cell lines were expanded, PBMC were stained with the TRF-, Flu-, and the corresponding RV-peptide tetramers (Figs 4A and 4B). The relative numbers of the CD4 T cells that stained with the tetramers VP6-7 and Flu (medians of 27/6.0×105 and 45/6.0×105 CD4 T cells, respectively) were higher than those stained with the TRF-tetramer (median of 9/6.0×105 CD4 T cells) (Wilcoxon test p=0.011 and p=0.003, respectively). Most of the CD4 T cells stained with VP6-7- and Flu-tetramers (medians of 63.5% and 67.05%, respectively) showed a phenotype of antigen experienced cells (CD62L−CD45RA+/− and CD62L+CD45RA−) and no statistical differences were observed in the frequencies of these cells (Table 2, Fig. 4C). Antigen experienced CD4 T cells stained with VP6-7-tetramer were enriched in the populations expressing the intestinal homing receptors: α4β7+CCR9+ and α4β7+CCR9− (Table 2, Figs 4B and 4D). In contrast, antigen experienced CD4 T cells stained with Flu-tetramer were enriched in the α4β7−CCR9− population (Table 2, Figs 4B and 4D).
Fig. 4. Phenotype and expression of homing receptors of CD4 tetramer+ T cells of healthy adults.
Fresh PBMC were obtained from HLA-DRB1*0101 healthy adults and stained with the Flu-tetramer (left panels), the TRF-tetramer (center panels) or the VP6-7-tetramer (right panels) and antibodies against differentiation markers and intestinal homing receptors. After gating on live CD3 T cells, total (A) or tetramer+ (B) CD4 T cells (top panels) were analyzed to identify antigen experienced T cells CD62L−CD45RA+/− and CD62L+CD45RA− (middle panels). The expression of α4β7 and CCR9 intestinal homing receptors was evaluated in antigen experienced cells (lower panels). Numbers in parenthesis in the lower row dot plots indicate number of events. Results from the eight volunteers for antigen experienced T cells VP6-7-tetramer+ and Flu-tetramer+ cells (C) and the expression of intestinal homing receptors (D) are summarized. Statistically significant differences determined with the Wilcoxon test are shown.
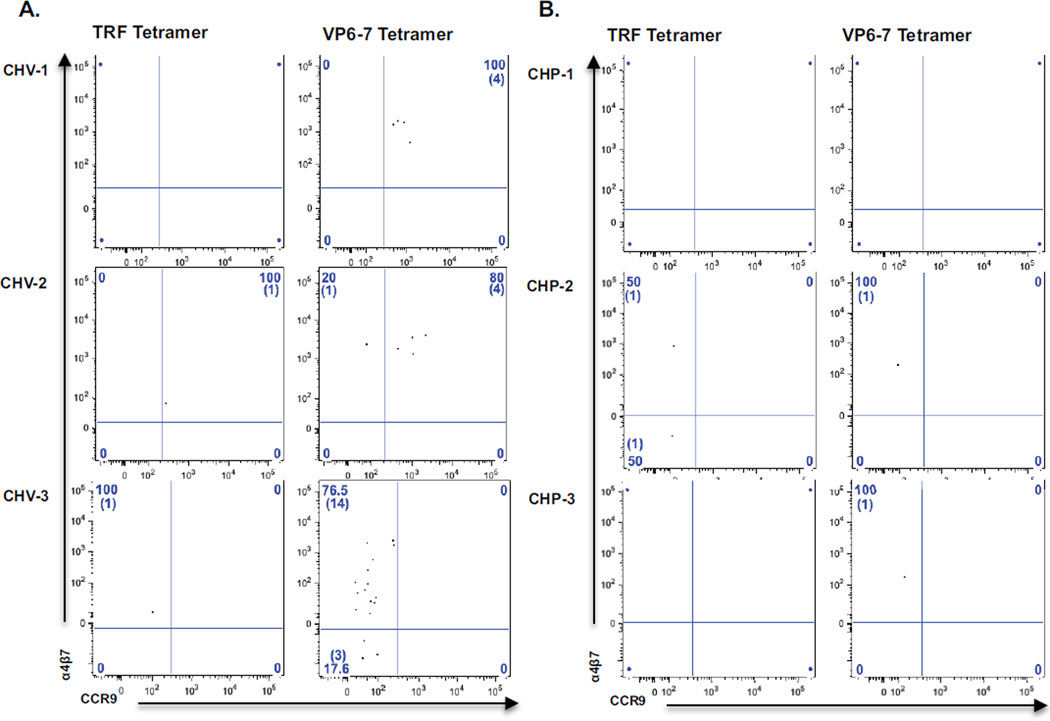
RV-tetramer+ CD4 T cells in vaccinated children are enriched in the populations expressing the intestinal homing receptors
To evaluate if RV vaccination induced the expansion of RV-CD4 T cells of children, PBMC from three HLA-DR1-vaccinated and three HLA-DR1-placebo recipient children, obtained two weeks after the second dose of the RIX4414 human attenuated RV vaccine or placebo (Rojas et al., 2007), were stained with the VP6-7- or control TRF-tetramers, and the same panel of markers previously used in adults. Because of the limited amount of sample available from vaccinated children only direct PBMC staining and not T cell line experiments were performed. The vaccinated, but not placebo recipient children, had detectable serum levels of RV-specific IgA after two doses of RV vaccine (data not shown). In vaccinated children and placebo recipient children from 40–71% and 0–8%, respectively, of VP6-7-tetramer+ cells had the phenotype of antigen-experienced cells (data not shown). In both groups of children the CD4 T cells stained with the TRF-tetramer only 0–30% of cells had this phenotype (data not shown). In vaccinated children, VP6-7 antigen experienced CD4 T cells were detected at low frequencies (0.001–0.1%). In all 3 cases, most of the antigen experienced CD4 tetramer+ T cells expressed α4β7, and in two children (Fig. 5A, two top panels), most cells expressed both, α4β7 and CCR9, homing receptors. In vaccinated children the TRF-tetramer (Fig. 5A, left panels) stained from 4 to 10 times less antigen experienced cells than the VP6-7-tetramer (from <0.0001–0.01%). In placebo recipients (Fig. 5B), VP6-7- and TRF-tetramers detected antigen experienced CD4 T cells at similar low levels (<0.0001–0.003%).
Fig. 5. Expression of homing receptors on antigen experienced (CD62L−CD45RA+/− and CD62L+CD45RA−) CD4 T cells from RV vaccinated and placebo recipient children.
Frozen PBMC from HLA-DRB1*0101 RV vaccinated (A) or placebo recipient children (B) were stained as in Fig. 4 with the TRF-tetramer (left panels) and VP6-7-tetramer (right panels). Dot plots show the expression of α4β7 and CCR9 intestinal homing receptors of CD4-tetramer+ antigen experienced cells from individual children. Numbers in parenthesis in the dot plots indicate number of events.
DISCUSSION
We have identified a RV CD4 T cell epitope (VP6-7) and shown that HLA-DR1 tetramers loaded with this peptide, but not a Flu peptide, expressed intestinal homing receptors (Fig. 4). Moreover, studies with a low number of vaccinated children showed that this type of reagent might be useful to monitor the RV CD4 T cell response in vaccine trials (Fig. 5).
Of 39 predicted epitopes, three peptides were identified by screening of PBMC from healthy adults by intracellular cytokine staining; all of them also bound to HLA-DRB1*0101 molecules (Figs. 1 and 2). The VP6-7 peptide is probably processed and presented after RV infection, since it was recognized by a rotavirus-T cell line (Fig. 3A). Moreover, peptide specific T cell lines were DR-MHC restricted (Fig. 3B) and VP6-7-tetramers were recognized by cells of vaccinated but not placebo recipient children (Fig. 5), characterizing this peptide as a RV epitope. This epitope overlaps totally with one previously found in mice (Baños et al., 1997) and partially with a VP6 epitope found in Rhesus macaques (Zhao et al., 2008), which suggests that this region is particularly prone to be recognized by CD4 T cells. Although a RV specific class II restricted human T cell epitope had been previously described (Honeyman et al., 2010), our studies are the first to characterize epitope specific CD4 T cells with tetramers.
HLA supertypes are defined as a set of HLA (class I or II) associated with largely overlapping peptide/binding repertoires. Recently, three different class II DR supertypes were classified (main DR, DR4 and DRB3) (Greenbaum et al., 2011), and all of the healthy adults volunteers for our screening experiments were selected for having the main DR supertype, which includes HLA-DR1 and many other class II molecules. Contrary to our expectations, only HLA-DR1 healthy adults recognized three peptides. However, in one DRB1*0102 individual VP6-7 T cell line were generated and their stimulation was inhibited by an anti-DR monoclonal antibody, suggesting that at this level promiscuity for HLA binding exists. The levels of promiscuity of viral epitopes varies between studies from low (Kwok et al., 2008; Nepom, 2012) to moderate (Roti et al., 2008). Further studies are necessary to clarify the reasons for these differences.
Ex vivo tetramer staining of PBMC from healthy adults showed that CD4 T cells specific for the VP6-7 peptide expressed intestinal homing receptors. This result is in agreement with our previous report, in which we observed that RV-specific IFN-γ secreting CD4 T cells from adult volunteers preferentially express the intestinal homing receptor α4β7 (Rojas et al., 2003). The present findings extend these results by showing that RV-tetramer+ antigen experienced (CD62L−CD45RA+/− and CD62L+CD45RA−) CD4 T cells express both α4β7 and CCR9 and, thus, are prone to home to the small intestine. Compared to total non-antigen specific T cells, VP6-7 specific T cells are enriched approximately 10 times in CCR9 expressing cells (Figs 4A and 4B), indicating that this is indeed a unique subset. Further studies are necessary to determine if these circulating dual α4β7 and CCR9 expressing RV-specific T cells have a unique TCR repertoire.
The generation of RRV- or RV peptide-specific T cell lines support the results obtained with ex vivo tetramer staining. Characterization of T cell lines expanded with RRV showed that VP6-7 and NSP2-3 are processed and presented by infected cells (Fig. 3A and data not shown). However, peptide-specific T cell lines were obtained after stimulation of PBMC with all three peptides (Table 1). Moreover, responses of T cell lines specific for the three peptides generated from PBMC obtained from an HLA-DRB1*0101 healthy adult were significantly blocked with an antibody against DR and poorly against an antibody to DQ molecules (Fig. 3B and data not shown), suggesting that the VP6-7 epitope and the two candidate RV-epitopes (NSP2-3 and VP3-4) were presented in the context of HLA-DR molecules. T cell lines expanded with virus lysate preparations might select clonotypes associated with immunodominant peptides over low frequency and/or slowly growing clonotypes (Nastke et al., 2012). Thus, in some of the experiments with the RRV-T cell lines the responses to the NSP2-3 and VP3-4 candidate epitopes might have been masked.
The simultaneous staining of the majority of cytokine secreting cells from a VP6-7 T cell line with the VP6-7 tetramer (Fig. 3C) supports the specificity of the tetramer staining. Moreover, they show that most cells stained with the tetramer are functional. A correlation between cells staining with the tetramer and those producing cytokines ex vivo is difficult to establish, because of the low or inexistent level of cytokine secreting cells specific for the RV peptides (Table 1). However, the capacity of the tetramers to identify specific T cells ex vivo seems more sensitive than the intracellular cytokine staining and proliferation assays (Table 1) and, thus, more suited to vaccine studies in children. Nonetheless, it is possible that some of the cells stained with the tetramer might be secreting cytokines not evaluated.
Staining of cells from vaccinated and placebo recipient children with the VP6-7 tetramer showed that VP6-7-specific CD4 T cells could be expanded after RV vaccination. Although the numbers of cells observed in the vaccinated children were low (Fig. 5A), they were all, as expected, α4β7 and in two cases they also expressed CCR9. The cells used in the present study had been frozen over seven years (Rojas et al., 2007), and it is expected that studies with fresh cells may permit to obtain more cells to study an increase in the sensitivity of the assay. Further studies are necessary to confirm that CD4 T cells from HLA-DR1 vaccinated children recognize the RV epitope we have identified.
In conclusion, we have shown that CD4 T cells specific for a RV epitope express intestinal homing receptors, which supports the hypothesis that cells primed in peripheral compartments may constitute a separate lineage (Sallusto and Lanzavecchia, 2009). We also describe MHC tetramers that could be used to analyze RV-specific CD4 T cell responses in vaccine studies. Similar studies in the context of other MHC haplotypes are needed to expand the number of tetramers available to monitor the CD4 T cell response to RV vaccines and, hopefully, develop better correlates of protection.
Supplementary Material
Research Highlights.
A DR1 restricted epitope derived from the rotavirus VP6 protein was identified.
CD4 T cells specific for this epitope were characterized using class II tetramers.
CD4 T cells specific for the rotavirus epitope but not specific for an influenza epitope expressed intestinal homing receptors.
ACKNOWLEDGMENTS
This work was financed by grants from Colciencias 1203-408-20481 and the Pontificia Universidad Javeriana (ID5195). LJS and JMCC received support from NIH grant U19-AI057319 and EB funding from R37-AI047822 and RC1-AI087257 also from the NIH, which funded Ab production. Miguel Parra was funded by a scholarship from Colciencias.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Angel J, Franco MA, Greenberg HB. Rotavirus immune responses and correlates of protection. Curr Opin in Virol. 2012;2:419–425. doi: 10.1016/j.coviro.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baños DM, Lopez S, Arias CF, Esquivel FR. Identification of a T-helper cell epitope on the rotavirus VP6 protein. J Virol. 1997;71:419–426. doi: 10.1128/jvi.71.1.419-426.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blutt SE, Kirkwood CD, Parreno V, Warfield KL, Ciarlet M, Estes MK, Bok K, Bishop RF, Conner ME. Rotavirus antigenaemia and viraemia: a common event? Lancet. 2003;362:1445–1449. doi: 10.1016/S0140-6736(03)14687-9. [DOI] [PubMed] [Google Scholar]
- Blutt SE, Miller AD, Salmon SL, Metzger DW, Conner ME. IgA is important for clearance and critical for protection from rotavirus infection. Mucosal Immunol. 2012;5:712–719. doi: 10.1038/mi.2012.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butcher EC, Picker LJ. Lymphocyte homing and homeostasis. Science. 1996;272:60–66. doi: 10.1126/science.272.5258.60. [DOI] [PubMed] [Google Scholar]
- Calvo-Calle JM, Strug I, Nastke M-D, Baker SP, Stern LJ. Human CD4+ T cell epitopes from vaccinia virus induced by vaccination or infection. PLoS Pathog. 2007;3:1511–1529. doi: 10.1371/journal.ppat.0030144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron TO, Norris PJ, Patel A, Moulon C, Rosenberg ES, Mellins ED, Wedderburn LR, Stern LJ. Labeling antigen-specific CD4(+) T cells with class II MHC oligomers. J Immunol Methods. 2002;268:51–69. doi: 10.1016/s0022-1759(02)00200-4. [DOI] [PubMed] [Google Scholar]
- Chicz RM, Urban RG, Lane WS, Gorga JC, Stern LJ, Vignali DA, Strominger JL. Predominant naturally processed peptides bound to HLA-DR1 are derived from MHC-related molecules and are heterogeneous in size. Nature. 1992;358:764–768. doi: 10.1038/358764a0. [DOI] [PubMed] [Google Scholar]
- Danke NA, Kwok WW. HLA class II-restricted CD4+ T cell responses directed against influenza viral antigens postinfluenza vaccination. J Immunol. 2003;171:3163–3169. doi: 10.4049/jimmunol.171.6.3163. [DOI] [PubMed] [Google Scholar]
- Franco MA, Angel J, Greenberg HB. Immunity and correlates of protection for rotavirus vaccines. Vaccine. 2006;24:2718–2731. doi: 10.1016/j.vaccine.2005.12.048. [DOI] [PubMed] [Google Scholar]
- Franco MA, Greenberg HB. Immunity to rotavirus in T cell deficient mice. Virology. 1997;238:169–179. doi: 10.1006/viro.1997.8843. [DOI] [PubMed] [Google Scholar]
- Gattinoni L, Lugli E, Ji Y, Pos Z, Paulos CM, Quigley MF, Almeida JR, Gostick E, Yu Z, Carpenito C, Wang E, Douek DC, Price DA, June CH, Marincola FM, Roederer M, Restifo NP. A human memory T cell subset with stem cell-like properties. Nature Medicine. 2011;17:1290–1297. doi: 10.1038/nm.2446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilger MA, Matson DO, Conner ME, Rosenblatt HM, Finegold MJ, Estes MK. Extraintestinal rotavirus infections in children with immunodeficiency. J Pediatr. 1992;120:912–917. doi: 10.1016/s0022-3476(05)81959-6. [DOI] [PubMed] [Google Scholar]
- Glass RI, Parashar U, Patel M, Tate J, Jiang B, Gentsch J. The control of rotavirus gastroenteritis in the United States. Trans Am Clin Climatol Assoc. 2012;123:36–53. [PMC free article] [PubMed] [Google Scholar]
- Greenbaum J, Sidney J, Chung J, Brander C, Peters B, Sette A. Functional classification of class II human leukocyte antigen (HLA) molecules reveals seven different supertypes and a surprising degree of repertoire sharing across supertypes. Immunogenetics. 2011;63:325–335. doi: 10.1007/s00251-011-0513-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer J, Bono E, Gallazzi F, Belunis C, Nagy Z, Sinigaglia F. Precise prediction of major histocompatibility complex class II-peptide interaction based on peptide side chain scanning. J Exp Med. 1994;180:2353–2358. doi: 10.1084/jem.180.6.2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honeyman MC, Stone NL, Falk BA, Nepom G, Harrison LC. Evidence for Molecular Mimicry between Human T Cell Epitopes in Rotavirus and Pancreatic Islet Autoantigens. J Immunol. 2010;184:2204–2210. doi: 10.4049/jimmunol.0900709. [DOI] [PubMed] [Google Scholar]
- Jaimes MC, Rojas OL, González AM, Cajiao I, Charpilienne A, Pothier P, Kohli E, Greenberg HB, Franco MA, Angel J. Frequencies of virus-specific CD4(+) and CD8(+) T lymphocytes secreting gamma interferon after acute natural rotavirus infection in children and adults. J Virol. 2002;76:4741–4749. doi: 10.1128/JVI.76.10.4741-4749.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok WW, Yang J, James E, Bui J, Huston L, Wiesen AR, Roti M. The anthrax vaccine adsorbed vaccine generates protective antigen (PA)-Specific CD4+ T cells with a phenotype distinct from that of naive PA T cells. Infect Immun. 2008;76:4538–4545. doi: 10.1128/IAI.00324-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laughlin EM, Miller JD, James E, Fillos D, Ibegbu CC, Mittler RS, Akondy R, Kwok W, Ahmed R, Nepom G. Antigen-specific CD4+ T cells recognize epitopes of protective antigen following vaccination with an anthrax vaccine. Infect Immun. 2007;75:1852–1860. doi: 10.1128/IAI.01814-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lissina A, Ladell K, Skowera A, Clement M, Edwards E, Seggewiss R, van den Berg HA, Gostick E, Gallagher K, Jones E, Melenhorst JJ, Godkin AJ, Peakman M, Price DA, Sewell AK, Wooldridge L. Protein kinase inhibitors substantially improve the physical detection of T-cells with peptide-MHC tetramers. J Immunol Methods. 2009;340:11–24. doi: 10.1016/j.jim.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mavigner M, Cazabat M, Dubois M, L’faqihi F-E, Requena M, Pasquier C, Klopp P, Amar J, Alric L, Barange K, Vinel J-P, Marchou B, Massip P, Izopet J, Delobel P. Altered CD4+ T cell homing to the gut impairs mucosal immune reconstitution in treated HIV-infected individuals. J. Clin. Invest. 2012;122:62–69. doi: 10.1172/JCI59011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesa MC, Gutiérrez L, Duarte-Rey C, Angel J, Franco MA. A TGF-beta mediated regulatory mechanism modulates the T cell immune response to rotavirus in adults but not in children. Virology. 2010;399:77–86. doi: 10.1016/j.virol.2009.12.016. [DOI] [PubMed] [Google Scholar]
- Nastke M-D, Becerra A, Yin L, Dominguez-Amorocho O, Gibson L, Stern LJ, Calvo-Calle JM. Human CD4+ T Cell Response to Human Herpesvirus 6. J Virol. 2012;86:4776–4792. doi: 10.1128/JVI.06573-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nepom GT. MHC Class II Tetramers. J Immunol. 2012;188:2477–2482. doi: 10.4049/jimmunol.1102398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra-López C, Calvo-Calle JM, Cameron TO, Vargas LE, Salazar LM, Patarroyo ME, Nardin E, Stern LJ. Major histocompatibility complex and T cell interactions of a universal T cell epitope from Plasmodium falciparum circumsporozoite protein. J Biol Chem. 2006;281:14907–14917. doi: 10.1074/jbc.M511571200. [DOI] [PubMed] [Google Scholar]
- Quah BJC, Parish CR. The use of carboxyfluorescein diacetate succinimidyl ester (CFSE) to monitor lymphocyte proliferation. JoVE. 2010 doi: 10.3791/2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quah BJC, Warren HS, Parish CR. Monitoring lymphocyte proliferation in vitro and in vivo with the intracellular fluorescent dye carboxyfluorescein diacetate succinimidyl ester. Nat Protoc. 2007;2:2049–2056. doi: 10.1038/nprot.2007.296. [DOI] [PubMed] [Google Scholar]
- Roche PA, Cresswell P. High-affinity binding of an influenza hemagglutinin-derived peptide to purified HLA-DR. J Immunol. 1990;144:1849–1856. [PubMed] [Google Scholar]
- Rojas OL, Caicedo L, Guzmán C, Rodríguez L-S, Castañeda J, Uribe L, Andrade Y, Pinzón R, Narváez CF, Lozano JM, De Vos B, Franco MA, Angel J. Evaluation of circulating intestinally committed memory B cells in children vaccinated with attenuated human rotavirus vaccine. Viral Immunol. 2007;20:300–311. doi: 10.1089/vim.2006.0105. [DOI] [PubMed] [Google Scholar]
- Rojas OL, González AM, González R, Pérez-Schael I, Greenberg HB, Franco MA, Angel J. Human rotavirus specific T cells: quantification by ELISPOT and expression of homing receptors on CD4+ T cells. Virology. 2003;314:671–679. doi: 10.1016/s0042-6822(03)00507-5. [DOI] [PubMed] [Google Scholar]
- Roti M, Yang J, Berger D, Huston L, James EA, Kwok WW. Healthy human subjects have CD4+ T cells directed against H5N1 influenza virus. J Immunol. 2008;180:1758–1768. doi: 10.4049/jimmunol.180.3.1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rott LS, Rosé JR, Bass D, Williams MB, Greenberg HB, Butcher EC. Expression of mucosal homing receptor alpha4beta7 by circulating CD4+ cells with memory for intestinal rotavirus. J Clin Invest. 1997;100:1204–1208. doi: 10.1172/JCI119633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallusto F, Lanzavecchia A. Heterogeneity of CD4+ memory T cells: functional modules for tailored immunity. Eur. J. Immunol. 2009;39:2076–2082. doi: 10.1002/eji.200939722. [DOI] [PubMed] [Google Scholar]
- Schuler MM, Nastke M-D, Stevanovikć S. SYFPEITHI: database for searching and T-cell epitope prediction. Methods Mol Biol. 2007;409:75–93. doi: 10.1007/978-1-60327-118-9_5. [DOI] [PubMed] [Google Scholar]
- Sigmundsdottir H, Butcher EC. Environmental cues, dendritic cells and the programming of tissue-selective lymphocyte trafficking. Nat Immunol. 2008;9:981–987. doi: 10.1038/ni.f.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturniolo T, Bono E, Ding J, Raddrizzani L, Tuereci O, Sahin U, Braxenthaler M, Gallazzi F, Protti MP, Sinigaglia F, Hammer J. Generation of tissue-specific and promiscuous HLA ligand databases using DNA microarrays and virtual HLA class II matrices. Nat Biotechnol. 1999;17:555–561. doi: 10.1038/9858. [DOI] [PubMed] [Google Scholar]
- Tate JE, Burton AH, Boschi-Pinto C, Steele AD, Duque J, Parashar UD. 2008 estimate of worldwide rotavirus-associated mortality in children younger than 5 years before the introduction of universal rotavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:136–141. doi: 10.1016/S1473-3099(11)70253-5. [DOI] [PubMed] [Google Scholar]
- Vollers SS, Stern LJ. Class II major histocompatibility complex tetramer staining: progress, problems, and prospects. Immunology. 2008;123:305–313. doi: 10.1111/j.1365-2567.2007.02801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldrop SL, Davis KA, Maino VC, Picker LJ. Normal human CD4+ memory T cells display broad heterogeneity in their activation threshold for cytokine synthesis. J Immunol. 1998;161:5284–5295. [PubMed] [Google Scholar]
- Waldrop SL, Pitcher CJ, Peterson DM, Maino VC, Picker LJ. Determination of antigen-specific memory/effector CD4+ T cell frequencies by flow cytometry: evidence for a novel, antigen-specific homeostatic mechanism in HIV-associated immunodeficiency. J Clin Invest. 1997;99:1739–1750. doi: 10.1172/JCI119338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao W, Pahar B, Sestak K. Identification of Rotavirus VP6-Specific CD4+ T Cell Epitopes in a G1P[8] Human Rotavirus-Infected Rhesus Macaque. Virology (Auckl) 2008;1:9–15. doi: 10.4137/vrt.s563. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.