Abstract
Vitamin D (vit-D) is essential for bone health, although many osteoporosis patients have low levels of 25-hydroxy-vit-D [25(OH)D]. This randomized, open-label study compared the effects of once weekly alendronate 70 mg containing 5600 IU vit-D3 (ALN/D5600) to alendronate 70 mg without additional vit-D (ALN) on the percent of patients with vit-D insufficiency [25(OH)D <15 ng/mL, primary endpoint] and serum parathyroid hormone (PTH, secondary endpoint) levels in postmenopausal, osteoporotic Korean women. Neuromuscular function was also measured. A total of 268 subjects were randomized. Overall, 35% of patients had vit-D insufficiency at baseline. After 16-weeks, there were fewer patients with vit-D insufficiency in the ALN/D5600 group (1.47%) than in the ALN group (41.67%) (p<0.001). Patients receiving ALN/D5600 compared with ALN were at a significantly decreased risk of vit-D insufficiency [odds ratio=0.02, 95% confidence interval (CI) 0.00-0.08]. In the ALN/D5600 group, significant increases in serum 25(OH)D were observed at weeks 8 (9.60 ng/mL) and 16 (11.41 ng/mL), where as a significant decrease was recorded in the ALN group at week 16 (-1.61 ng/mL). By multiple regression analysis, major determinants of increases in serum 25(OH)D were ALN/D5600 administration, seasonal variation, and baseline 25(OH)D. The least squares mean percent change from baseline in serum PTH in the ALN/D5600 group (8.17%) was lower than that in the ALN group (29.98%) (p=0.0091). There was no significant difference between treatment groups in neuromuscular function. Overall safety was similar between groups. In conclusion, the administration of 5600 IU vit-D in the ALN/D5600 group improved vit-D status and reduced the magnitude of PTH increase without significant side-effects after 16 weeks in Korean osteoporotic patients.
Keywords: Alendronate, vitamin-D, vitamin-D insufficiency, osteoporosis, parathyroid hormone
INTRODUCTION
Osteoporosis, the most common bone disorder in postmenopausal women, is characterized by reduced bone density, increased bone turnover, and micro-structural abnormalities that lead to increased fracture risk morbidity and mortality.1,2 Approximately 75 million people worldwide have osteoporosis, including one-third of postmenopausal women and the great majority of the elderly,2 and the prevalence of osteoporosis and its socio-economic burden are expected to increase due to increasing average life expectancy.3 The disease burden of osteoporosis is a growing concern in many countries, including Korea,4,5,6 where among women 40-79 years of age, the prevalence of osteoporosis is approximately 30%.7
Vitamin D is an important component of osteoporosis treatment,8 both for its direct effects on bone and the fact that optimal vitamin D nutrition appears to maximize the response to anti-resorptive agents in vitamin D insufficient patients.9,10 In addition to its effects on bone, vitamin D deficiency is also associated with insulin resistance, metabolic syndrome, vitamin D supplementation improved muscle strength, physical performance and decreased risk of falls.11,12,13 Vitamin D is synthesized upon exposure to sunlight, and is absorbed from food. However, its synthesis is frequently insufficient and intake from un-supplemented food may be inadequate.8,14 Supplementation with cholecalciferol (vitamin D3) is a practical and effective method of improving vitamin D status. Unfortunately, even though such doses of vitamin D are recommended to osteoporotic women, many patients being treated for osteoporosis do not receive sufficient levels of vitamin D.12,13 According to a recent study in Korea, the average serum 25-hydroxy-vitamin D [25(OH)D] level of Korean postmenopausal women was 17 ng/mL (values less than 15 ng/mL were considered insufficient when the current study was designed).15,16
Combination therapy with a drug and a vitamin supplement is a useful method for treating vitamin insufficient osteoporotic patients. A single-tablet, once weekly formulation of alendronate 70 mg plus vitamin D3 2800 IU (ALN/D2800) was introduced to provide vitamin D3 to osteoporotic patients. In a previous study, ALN/D2800 reduced the proportion of patients with 25(OH)D below 15 ng/mL by 64% after 15 weeks of treatment.17 Subsequently, a higher 5600 IU weekly dose of vitamin D3, (corresponding to 800 IU daily) was recommended for some groups, including patients with osteoporosis or a sedentary life style and institutionalized elderly.18,19
This 16-week, open-labeled, randomized, active controlled study was conducted to directly compare the efficacy of the higher 5600 IU dose of vitamin D3 combined with weekly alendronate 70 mg to weekly alendronate 70 mg alone (without vitamin D3 supplements). Calcium carbonate (500 mg/day) was also administered. The primary objective of this study was to evaluate the effects of treatment on vitamin D status as assessed by serum 25(OH)D levels, with the goal of reducing the risk of vitamin D insufficiency. Examining the effect of treatment on parathyroid hormone (PTH) levels was a secondary objective, and assessment of the effects on neuromuscular function was an exploratory objective of the study.
MATERIALS AND METHODS
Study subjects and design
This study was a prospective, 16-week, randomized, open-labeled, active controlled trial conducted across 17 investigational centers in Korea. Patients were recruited for the study beginning in March 2008, and by April 2009 the study was completed. Vitamin D insufficiency and vitamin D deficiency were defined as serum 25(OH)D level <15 ng/mL and 25(OH)D <9 ng/mL, respectively.
Inclusion in the study required satisfactory general health; being postmenopausal (≥6 months beyond the final menstrual period); serum 25(OH)D ≥9 ng/mL; presence of osteoporosis [defined as one of the following: lumbar spine or femoral neck T-score ≤-2.5, T-score ≤-2.0 with any lumbar spine fracture, or two or more fractures in lumbar spine regardless of bone mineral density (BMD)]; no contraindication to oral bisphosphonates; spine or hip anatomy suitable for dual-energy X-ray absorptiometry (DXA); willingness to limit direct sunlight exposure to <1 hour/day with sunscreen; and avoidance of other vitamin D supplements during the 16-week study. Patients with serum 25(OH)D levels <15 ng/mL but ≥9 ng/mL were required to have serum PTH and total alkaline phosphatase within reference ranges.
Reasons for exclusion included vitamin D deficiency [25(OH)D <9 ng/mL], abnormalities of the esophagus that delay esophageal emptying (e.g., stenosis or achalasia), certain malignancies, active systemic diseases that could pose an added risk to the patient or the patient's ability to complete the study, other disorders of bone or mineral metabolism, or recent treatment with agents that affect bone or calcium metabolism. Patients who could not sit or stand for at least 30 minutes and patients with a history of alcohol or drug abuse were also excluded.
Patients were evaluated for eligibility at a screening visit (day -14--day -1), followed by a randomization visit (week 0); two additional clinic visits (weeks 8 and 16), during which compliance and adverse experiences were assessed; and one follow up visit or telephone contact (week 18) to assess adverse experiences. Patients were allocated to treatment groups using a computer-generated randomized allocation schedule created by the study's statistician. Numbered containers were used to implement allocation, and each patient was assigned the next number in the sequence upon being enrolled.
Treatment
Patients were randomly assigned to receive once-weekly tablets containing either ALN/D5600 or ALN, both manufactured by Merck & Co., Inc., Whitehouse Station, NJ, USA. Patients were instructed to take tablets in a fasting state upon waking up in the morning a half-hour before the first food, beverage (except water), or other medication. They were also told to stay upright until consuming the first food of the day. Patients recorded doses of study medication taken or missed in a diary that was brought to each clinic visit. Both ALN/D5600- and ALN-treated groups were given 500 mg/day of calcium carbonate (200 mg of elemental calcium), to be taken at least 30 minutes after ingestion of the ALN/D5600 or ALN tablet. If a subject showed poor tolerance to the calcium carbonate, calcium citrate could be prescribed. The subject was not withdrawn from the study if he or she stopped taking calcium due to poor tolerance. If a patient's 25(OH)D declined to <9 ng/mL, the central laboratory notified the study site and the patient was withdrawn from the study drug and treated with cholecalciferol within 2 weeks of the date of sample acquisition. Patients were not permitted to take supplemental vitamin D or calcium other than what was provided. The study was conducted in accordance with principles of Good Clinical Practice and was approved by the appropriate Institutional Review Boards and regulatory agencies. Written informed consent was obtained from all patients before performing any study procedure.
Efficacy
The efficacy of the study drug was evaluated in patients who received at least one dose of investigational product and underwent baseline and at least one efficacy measurement. The primary endpoint was serum 25(OH)D level, with the primary efficacy variable defined as the percentage of subjects with vitamin D insufficiency [serum 25(OH)D level <15 ng/mL]. Serum 25(OH)D (mean of duplicate measures) was measured prior to randomization and at weeks 8 and 16. The secondary efficacy variable was percentage change from baseline in serum PTH. Serum PTH (mean of duplicate measures) was measured prior to randomization, and at week 16. For assessment of the exploratory endpoint, neuromuscular function was evaluated at five of the 17 investigational sites using tests of standing balance (examining ability to stand with the feet together in the side-by-side, semi-tandem, and tandem positions), gait speed (8-foot walk test; the time of the faster of two trials was used for scoring), and time to rise from a chair five times (sit-to-stand test). Higher scores represent better function. The physical performance tests used in this study were previously described in detail.20,21
Safety
Clinical evaluations and laboratory measurements, including serum chemistry and hematology were performed at selected visits. All clinical and laboratory adverse experiences and concomitant medication use were recorded. The investigators evaluated and recorded all adverse experiences (AEs) based on predefined criteria regarding intensity, seriousness, duration, action taken, and causal relationship with the investigational drug.
Safety and tolerance were evaluated by reviewing all safety variables including clinical adverse experiences, laboratory test results, and vital signs. Serious AEs were immediately reported to MSD Korea regardless of the investigator's assessment of a causal relationship to study drug, and were recorded for each subject.
Clinical measurements
Serum 25(OH)D was analyzed by radioimmunoassay (RIA) (DiaSorin Inc., Stillwater, MN, USA; the company citing a 2× standard deviation range in their reference group of 9.0-37.6 ng/mL). Serum PTH was analyzed by immunoradiometric assay using ELSA-PTH (CIS Bio International, Sorgues, France, the normal reference range cited by the manufacturer being 8-76 pg/mL). Serum calcium, phosphorus, blood urea nitrogen, creatinine, alkaline phosphatase, aspartate aminotransferase, and alanine aminotransferase were assessed at each site.
BMD of the spine (L1, L2, L3, and L4) and femur (femoral neck and femur total) was assessed by DXA (Hologic-Hologic Corporation, Waltham, MA, USA or GE Lunar-GE Healthcare Lunar, Madison, WI, USA).
Statistical analysis
Patients were stratified according to baseline 25(OH)D: a vitamin D insufficient group [25(OH)D <15 ng/mL] and a vitamin D sufficient group [25(OH)D ≥15 ng/mL]. The type I error was 0.025 (one-sided) and the power was 90% to detect a 0.375 odds ratio of vitamin D insufficiency between ALN/D5600 and ALN groups with 175 patients randomized into each treatment group. This calculation was based on an overall dropout rate of 20% from the beginning of the study (i.e., n=140 per group).
The differences in the ratios between treatment groups for the analysis of primary efficacy evaluation variables and 95% confidence intervals (CI) were calculated using the weighted average of Cochran-Mantel-Haenszel in which pre-treatment vitamin D level was adjusted. The secondary efficacy evaluation variable, % change of PTH at 16 weeks, was analyzed by analysis of covariance, with baseline serum PTH level as the covariate. Treatment effects on neuromuscular function were evaluated by the chi-square or Fisher's exact test.
Missing data for the efficacy evaluation were imputed by the last observation carried forward technique.
RESULTS
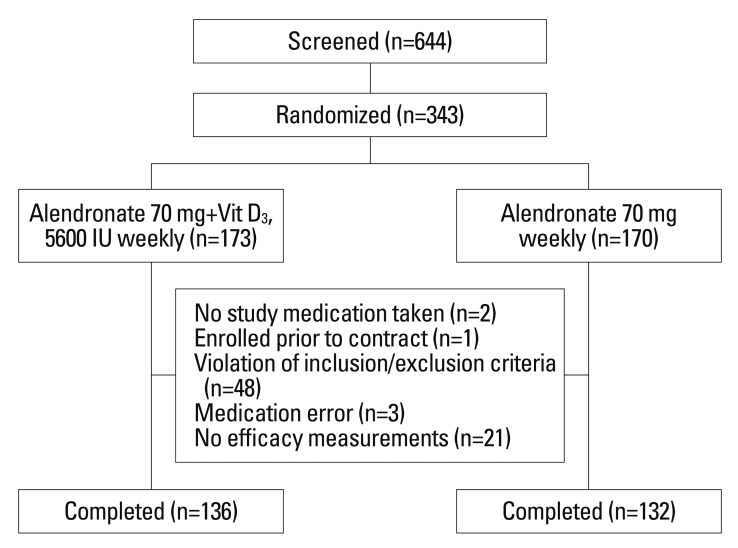
A total of 343 subjects who met eligibility criteria were randomly allocated (173 in the ALN/D5600 group and 170 in the ALN group). Patient disposition is shown in Fig. 1. The Modified Intend-to-treat set for efficacy evaluation consisted of 268 (136 in ALN/D5600 group and 132 in ALN group) subjects who received at least one dose of investigational product and who underwent efficacy assessment of a pre-treatment value and at least one value after the start of treatment. Subject data were analyzed based on the allocated treatment group at randomization regardless of the drugs administered during the trial. The safety evaluation utilized the all patients as treated set for 341 subjects (171 for ALN/D5600 and 170 for ALN) who received drugs at least once after randomization. They were analyzed according to the drugs actually administered.
Fig. 1.
Summary of patient disposition.
Demographic and other baseline characteristics
There were no clinically meaningful differences between the groups at baseline (Table 1). In both treatment groups, the largest age group was between 60 and 69 years. The mean elapsed time since diagnosis of osteoporosis was approximately 2 years for each treatment group, although most patients were not previously treated for osteoporosis (Table 1). The number of subjects who had ever taken vitamin D was similar between the two groups and was not statistically significant (n=7 in ALN/D5600 vs. n=3 in ALN group). The proportion of subjects with vitamin D insufficiency in the treatment groups was not significantly different at baseline (Table 2).
Table 1.
Baseline Characteristics of Patients by Treatment Group
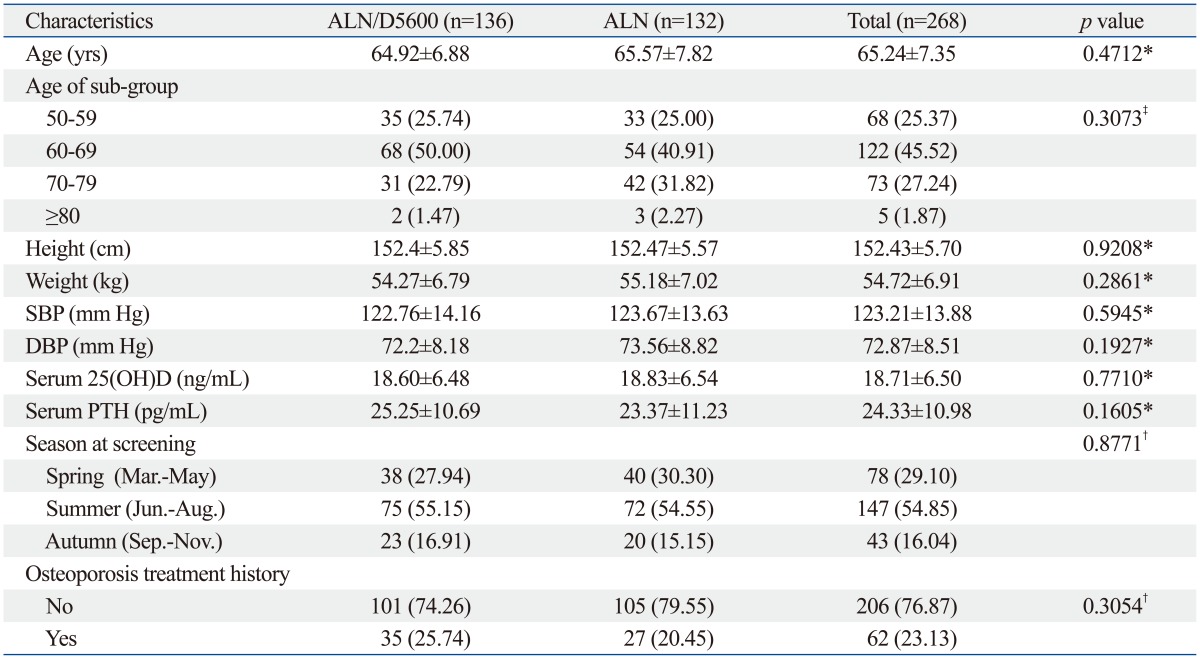
ALN/D5600, alendronate containing 5600 IU of vitamin D3; ALN, alendronate; SBP, systolic blood pressure; DBP, diastolic blood pressure; 25(OH)D, serum 25-hydroxy-vitamin D; PTH, parathyroid hormone.
Data are expressed as number (percentage) or as mean±SD. Missing in control group (N): height (2), weight (2), SBP (1), DBP (1).
*Unpaired t-test.
†Chi-square test.
‡Fisher's exact test.
Table 2.
Mean Values of 25(OH)D
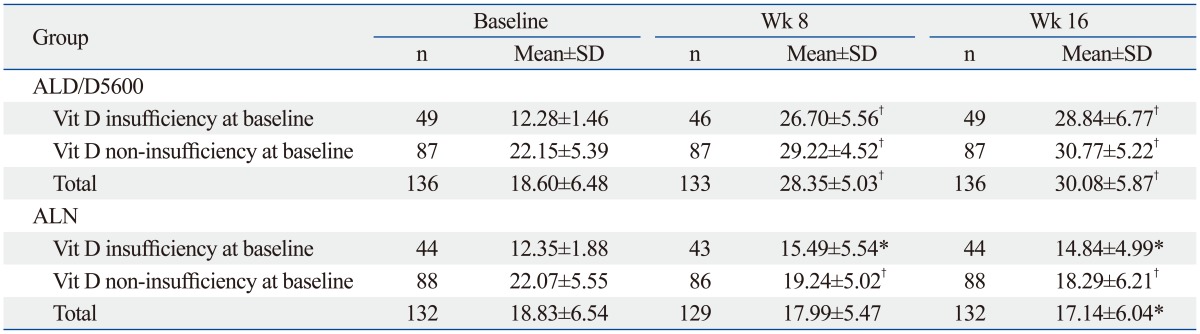
ALN/D5600, alendronate containing 5600 IU of vitamin D3; ALN, alendronate; Vit D, vitamin D.
Vitamin D insufficiency [Yes: 25(OH)D <15 ng/mL, No: 25(OH)D ≥15 ng/mL].
*p<0.01, †p<0.0001 compared to values of baseline.
Measurements of treatment compliance
The mean compliance of study drug treatment was 98.44±7.64% in the ALD/D5600 group and 98.86±4.93% in the ALN group. The two groups did not show a statistically significant difference in treatment compliance (p=0.589).
Primary endpoint: serum 25-hydroxyvitamin D
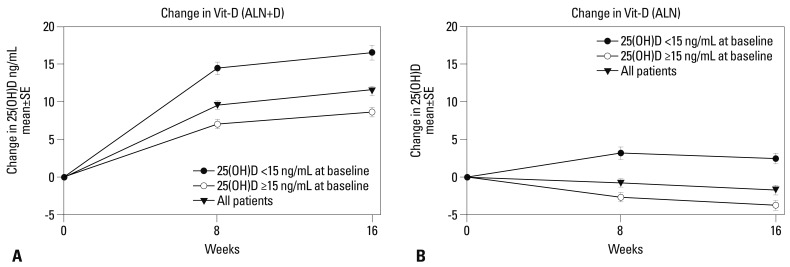
As shown in Table 2, mean serum 25(OH)D increased at weeks 8 and 16 from baseline in the ALN/D5600 group (p<0.001). However, in the ALN group, mean values of serum 25(OH)D decreased from baseline at weeks 8 and 16, with the decline reaching significance at week 16 (p<0.01). The mean change in serum 25(OH)D [adjusted for baseline serum 25(OH)D] at week 8 was 9.60 ng/mL in the ALN/D5600 group, but was -0.81 ng/mL in the ALN group, a significant difference between the groups (p<0.001). The mean change from baseline in serum 25(OH)D at 16 weeks was 11.41 ng/mL in the ALN/D5600 group, while it was -1.61 ng/mL in the ALN group (p<0.001 between groups). Increases in serum 25(OH)D were much higher in subgroups that were vitamin D-insufficient at baseline, compared with those vitamin D-sufficient at baseline, in both treatment groups (Fig. 2).
Fig. 2.
Mean change of 25-hydroxyvitamin D according to baseline 25-hydroxyvitamin D status. (A) Mean change of 25-hydroxyvitamin D in patients receiving alendronate containing 5600 IU of vitamin D3. (B) Mean change of 25-hydroxyvitamin D in patients receiving alendronate. ALN, alendronate.
Table 3 describes the proportion of subjects with vitamin D <15 ng/mL at week 8 and week 16 in each treatment group. The percentage of subjects with vitamin D insufficiency at week 8 was 0.75% (n=1/133) in the ALN/D5600 group and 28.68% (n=37/129) in the ALN group, and the difference between the groups was statistically significant (p<0.001). At week 16, the percentage with vitamin D insufficiency was 1.47% (n=2/136) in the ALN/D5600 group and 41.67% (n=55/132) in the ALN group (p<0.001). The odds ratio of vitamin D insufficiency in the ALN/D5600 group was significantly lower than that in the ALN group after 8 (odds ratio=0.01, 95% CI 0.00-0.08) and 16 weeks of treatment (odds ratio=0.02, 95% CI 0.00-0.08).
Table 3.
Proportion of Patients with Vitamin D Insufficiency at Baseline, Week 8 and Week 16
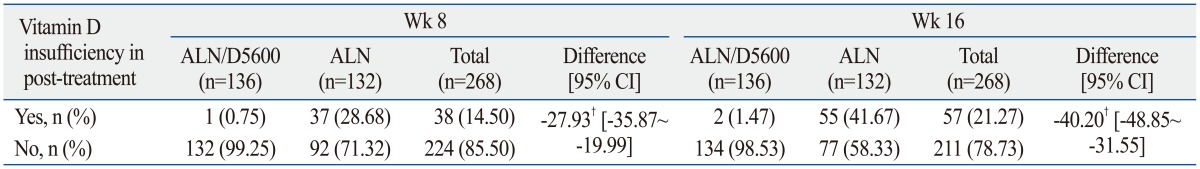
ALN/D5600, alendronate containing 5600 IU of vitamin D3; ALN, alendronate; CI, confidence interval.
Vitamin D insufficiency [Yes: 25(OH)D <15 ng/mL, No: 25(OH)D ≥15 ng/mL]. Cochran-Mantel-Haenszel test using covariate as vitamin D deficiency at baseline. Missing data at week 8-ALN/D5600 (3 subjects), ALN (3 subjects).
†p<0.0001.
Among patients with 25(OH)D levels <15 ng/mL at baseline, the proportions of persisting insufficiency were 2.17% (n=1/46) at week 8 and 4.08% (n=2/49) at week 16 in the ALN/D5600 group. However, they were 53.49% (n=23/43) at week 8 and 52.27% (n=23/44) at week 16 in the ALN group. In the ALN/D5600 group, there was no incidence of newly developed vitamin D insufficiency in patients with vitamin D sufficiency at baseline either at week 8 or week 16. In contrast, 36.36% (n=32/88) of subjects in the ALN group with vitamin D sufficiency at baseline developed vitamin D insufficiency at week 16 (Supplementary Table 1, only online).
In multiple regression analysis, major determinants of delta increment of serum 25(OH)D were ALN/D5600 administration, basal 25(OH)D level, and seasonal variation (Supplementary Table 2, only online).
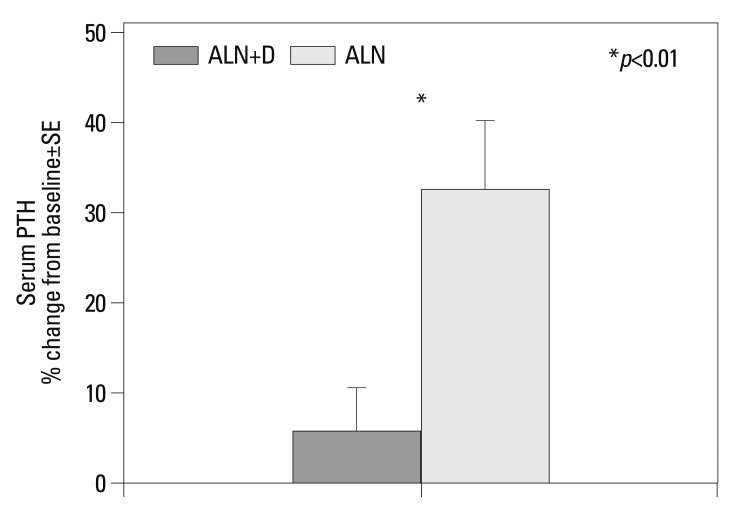
Secondary endpoint: PTH
The percent change from baseline in serum PTH at week 16 was analyzed as a secondary endpoint (Supplementary Table 3, only online) (Fig. 3). In the ALN/D5600 group, a small and non-significant increase from baseline to week 16 was observed, whereas a significant increase (p<0.001) was observed in the ALN group. The least squares mean percent change from baseline of serum PTH in the ALN/D5600 group was significantly lower than that in the ALN group (8.17% vs. 29.98%, respectively, p<0.01).
Fig. 3.
Percent change from baseline in serum PTH at 16 weeks. *p<0.01 between treatments. PTH, parathyroid hormone; ALN, alendronate.
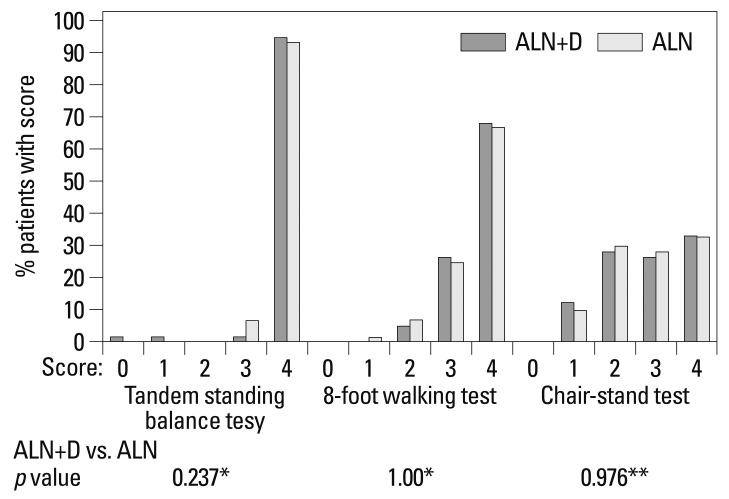
Exploratory endpoint: neuromuscular function
There were no significant differences in test results of neuromuscular function between the treatment groups (Fig. 4).
Fig. 4.
Neuromuscular Function Tests at 16 Weeks. *Fisher's exact test, **Chi-square test. ALN, alendronate.
Safety and adverse events evaluation
A similar percentage of participants reported clinical AEs (included regardless of the investigator's assessment of causal relationship to study drug): 37.43% (n=64/171, 105 cases) in the ALN/D5600 group and 32.35% (n=55/170, 87 cases) in the ALN group (Table 4). Serious AEs reported during the study period comprised 4.09% (n=7/171, 10 cases) in the ALN/D5600 group and 0.59% (n=1/170, 1 case) in the ALN group. Among 10 cases in the ALN/D5600 group (lung abscess, uterine prolapse, cystocele, gastric tumor, stroke, flu-like symptom, otitis media, and herpes zoster), only 1 case (flu-like symptom) was considered a drug related adverse event. The severity of the serious adverse drug reactions was mild, not life-threatening, and did not require hospitalization. AEs determined by the investigator to be related to study drug comprised 15.20% (n=26/171, 34 cases) in the ALN/D5600 group and 14.71% (n=25/170, 33 cases) in the ALN group. There were no statistically significant differences in incidence of adverse events and adverse drug reactions between the groups.
Table 4.
Clinical Adverse Experiences (Regardless of Investigator's Assessment of Causal Relationship to Study Drug) Classified by System Organ Class (APaT Set); Preferred Term with Incidence ≥1% Are Included
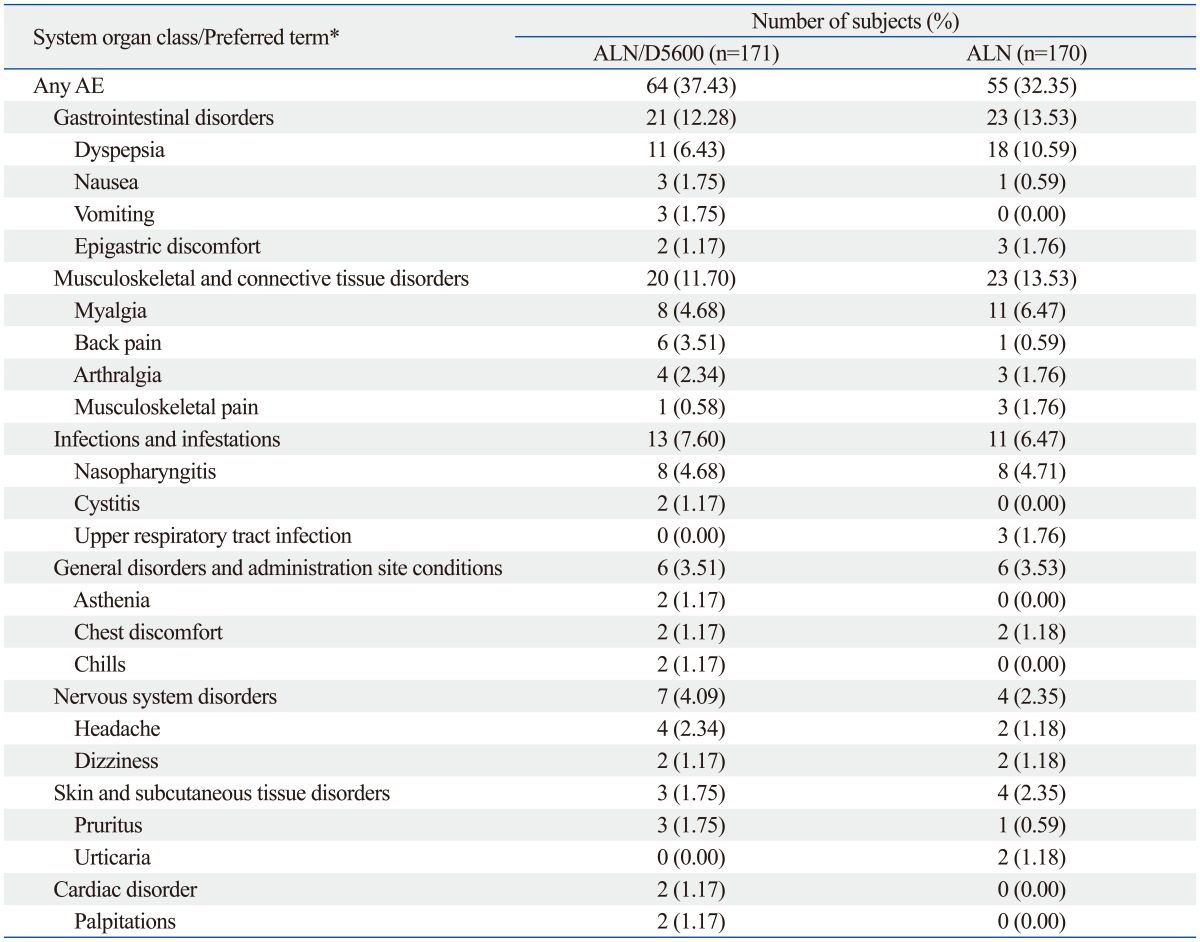
APaT, all patients as treated; ALN/D5600, alendronate containing 5600 IU of vitamin D3; ALN, alendronate.
*Overlap count.
DISCUSSION
This is the first study to evaluate a fixed dose combination of alendronate 70 mg with and without cholecalciferol 5600 IU in Korean postmenopausal women with osteoporosis. This study showed that, compared with ALN alone, once-weekly ALN/D5600 provided superior efficacy for increasing serum 25(OH)D levels, reduced the risk of vitamin D insufficiency, and reduced the magnitude of the PTH increase significantly in patients with osteoporosis. The relative safety and tolerability of the 5600 IU vitamin D present in alendronate plus D 5600 were also demonstrated in this study.
In osteoporosis treatment, vitamin D is an essential component in maintaining bone mass and reducing fracture risk. Without adequate vitamin D, the body cannot produce the active hormone calcitriol (1,25-dihydroxyvitamin D), whose principal action is to enhance intestinal calcium and phosphate absorption. Therefore, disorders of bone formation and resorption (i.e., osteomalacia and osteoporosis) may be associated with lack of vitamin D. In addition, vitamin D is also involved in other aspects of bone formation and resorption. The vitamin D receptor is expressed in endocrine cells, muscle cells, and immune cells, including macrophages and bone cells,22,23,24 and vitamin D deficiency may also be associated with some non-bone effects, including hypertension, and chronic infections such as tuberculosis.8,14 Vitamin D insufficiency is a worldwide problem.17 Recent meta-analysis revealed that vitamin D intake less than 700 IU/day was not sufficient for prevention of fractures.11,12
A total of 343 volunteers participated in this randomized clinical trial, and the average basal serum 25(OH)D concentration was 18.7 ng/mL, a value comparable to previously reported values in Korean population.15 As expected, compared to ALN once weekly alone, the addition of 5600 units of vitamin D3 in ALN/D5600 once weekly for 16 weeks significantly increased serum 25(OH)D concentration (ALN/D5600 once weekly: 18.6 to 30.1 ng/mL vs. ALN alone: 18.8 to 17.1 ng/mL). In fact, serum 25(OH)D concentrations obtained at 8 weeks after ALN/D5600 once weekly administration reached approximately 94% of the level at 16 weeks. Just 8 weeks of treatment with ALN/D5600 was enough to increase the mean serum 25(OH)D level close to a level that has been argued by some to be optimal (>30 ng/mL).13
To evaluate the effect of ALN/D5600 on serum 25(OH)D concentration according to basal serum 25(OH)D levels, subjects were grouped according to baseline 25(OH) levels with a cutoff value of 15 ng/mL. Interestingly, compared to the vitamin D-sufficient group, increases in serum 25(OH)D were greater in the vitamin D-insufficient group after therapy (16.5 ng/mL vs. 8.6 ng/mL). We obtained similar results even after adjusting the cutoff value of vitamin D insufficiency to 10 ng/mL or 20 ng/mL (data not shown). A previous study reported that larger increases in 25(OH)D were typically observed in patients with very low baseline 25(OH)D, probably due to the fact that production of 25(OH)D is regulated with greater expression of 25-hydroxylase at low 25(OH)D levels and more conversion of 25(OH)D to 24,25(OH)2D at higher levels of 25(OH)D.25
In our multiple regression analysis, basal 25(OH)D, seasonal variation, and ALN/D5600 once weekly were identified as the most important factors influencing the observed increases in 25(OH)D level. Similar numbers of subjects in both groups were recruited in the spring and summer (45/113 vs. 40/112). We did not find any effects of age regardless of the basal 25(OH)D levels (data not shown).
ALN is a powerful anti-resorptive agent, and it inhibits the bone resorbing activity of osteoclasts by competitively inhibiting farnesyl pyrophosphatase; it also induces apoptosis of osteoclasts in very high doses, but the drug produces a reversible inhibition of osteoclast function at doses typically used to treat osteoporosis.26,27 Previous studies reported that ALN treatment increases serum PTH by reducing bone resorption and slightly reducing serum calcium.27 Continuous elevation of serum PTH is reported to be detrimental to non-osseous tissues and may promote catabolic effects on bone.28,29 On the other hand, ALN/D5600 once weekly increased serum 25(OH)D without any meaningful increase in serum PTH. This observation may answer the question why PTH increases when bisphosphonates are started. While the primary effect on PTH is from reduction of calcium loss from the skeleton, vitamin D insufficiency appears to play a role as well.
As the exploratory objective of this study, we evaluated treatment effects of ALN/D5600 on the neuromuscular system through neuromuscular function tests. However, we did not observe any beneficial effects of ALN/D5600 on lower-extremity function. The reason for this is not clear. The trial's short duration, the fact that there were only 4 subjects in this study with serum 25(OH)D less than 10 ng/mL, or the fitness of the subjects at baseline might each have influenced the results of this exploratory endpoint.
The overall safety of ALN/D5600 once weekly was similar to that of ALN once weekly. There were only a few incidents of flu-like symptoms, such as myalgia, arthralgia, back pain, and dyspepsia, which are recognized adverse drug reactions to bisphosphonates, including alendronate, and not to vitamin D supplements. ALN/D5600 once weekly demonstrated comparable upper gastrointestinal tolerability, and the most commonly reported upper-GI AEs were dyspepsia (ALN/5800, 6.43%; ALN alone 10.59%, respectively), vomiting, and epigastric discomfort. Neither treatment was associated with hypercalcemia. As a result of the safety evaluation, it is reasonable to conclude that there were no clinically significant differences between treatment groups; accordingly, we ascertained that ALN/D5600 generally has a safety level similar to ALN. The limitations of this study are that we did not study the effects of ALN/D5600 on hypercalciuria and the change of bone turnover markers.
In conclusion, ALN/D5600 once weekly for 16 weeks provided enough vitamin D to reach target serum 25(OH)D levels (>15 ng/mL) in >98% of patients. Furthermore, it showed superior efficacy to that of ALN without vitamin D supplementation. The combination tablet of ALN/D5600 once weekly not only significantly increased serum 25(OH)D but greatly reduced increases in PTH, compared to ALN. Moreover, the safety and tolerability of ALN with or without vitamin D3 were comparable.
ACKNOWLEDGEMENTS
All authors listed above received research grants for VALUE study from MSD Korea Ltd., for patient care and administrative services.
Yong Soo Kim is an employee of MSD Korea Ltd.
Yong-Ki Min, Yoon-Sok Chung, Dong-Won Byun, In Joo Kim, Dong Jin Chung, and Sung-Kil Lim are editorial board members for MD faculty of MSD Korea.
We thank Elizabeth Rosenberg, PhD., Global Scientific and Medical Publications, Merck, and Hye Kyung Kim of Yonsei University Medical Library, for their help in the preparation of this article.
This study was sponsored by MSD Korea Ltd.
Footnotes
The authors have no financial conflicts of interest.
Supplementary Material
Proportion of Patients with Vitamin D Insufficiency
Multiple Regression Analysis for Increment of Serum 25(OH)D
Serum PTH
References
- 1.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 2.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 3.Shi N, Foley K, Lenhart G, Badamgarav E. Direct healthcare costs of hip, vertebral, and non-hip, non-vertebral fractures. Bone. 2009;45:1084–1090. doi: 10.1016/j.bone.2009.07.086. [DOI] [PubMed] [Google Scholar]
- 4.Jang SN, Choi YH, Choi MG, Kang SH, Jeong JY, Choi YJ, et al. [Prevalence and associated factors of osteoporosis among postmenopausal women in Chuncheon: Hallym Aging Study (HAS)] J Prev Med Public Health. 2006;39:389–396. [PubMed] [Google Scholar]
- 5.Jung JK, Kim HJ, Lee HK, Kim SS, Shin CS, Kim JT. Fracture incidence and risk of osteoporosis in female type 2 diabetic patients in Korea. Diabetes Metab J. 2012;36:144–150. doi: 10.4093/dmj.2012.36.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee SH, Lee TJ, Cho KJ, Shin SH, Moon KH. Subsequent hip fracture in osteoporotic hip fracture patients. Yonsei Med J. 2012;53:1005–1009. doi: 10.3349/ymj.2012.53.5.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shin CS, Choi HJ, Kim MJ, Kim JT, Yu SH, Koo BK, et al. Prevalence and risk factors of osteoporosis in Korea: a community-based cohort study with lumbar spine and hip bone mineral density. Bone. 2010;47:378–387. doi: 10.1016/j.bone.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 8.Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87:1080S–1086S. doi: 10.1093/ajcn/87.4.1080S. [DOI] [PubMed] [Google Scholar]
- 9.Adami S, Giannini S, Bianchi G, Sinigaglia L, Di Munno O, Fiore CE, et al. Vitamin D status and response to treatment in post-menopausal osteoporosis. Osteoporos Int. 2009;20:239–244. doi: 10.1007/s00198-008-0650-y. [DOI] [PubMed] [Google Scholar]
- 10.Koo JH, Kim HK, Kim IS, Kim EK, Chung YS. The effects of combined treatment of alendronate plus active or plain vitamin D on the vitamin D metabolism and bone turnover markers in patients with osteoporosis. Endocrinol Metab. 2010;25:305–309. [Google Scholar]
- 11.Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA. 2005;293:2257–2264. doi: 10.1001/jama.293.18.2257. [DOI] [PubMed] [Google Scholar]
- 12.Pfeifer M, Begerow B, Minne HW. Vitamin D and muscle function. Osteoporos Int. 2002;13:187–194. doi: 10.1007/s001980200012. [DOI] [PubMed] [Google Scholar]
- 13.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 14.Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. 2004;80(6 Suppl):1678S–1688S. doi: 10.1093/ajcn/80.6.1678S. [DOI] [PubMed] [Google Scholar]
- 15.Lim SK, Kung AW, Sompongse S, Soontrapa S, Tsai KS. Vitamin D inadequacy in postmenopausal women in Eastern Asia. Curr Med Res Opin. 2008;24:99–106. doi: 10.1185/030079908x253429. [DOI] [PubMed] [Google Scholar]
- 16.Rizzoli R, Eisman JA, Norquist J, Ljunggren O, Krishnarajah G, Lim SK, et al. Risk factors for vitamin D inadequacy among women with osteoporosis: an international epidemiological study. Int J Clin Pract. 2006;60:1013–1019. doi: 10.1111/j.1742-1241.2006.01066.x. [DOI] [PubMed] [Google Scholar]
- 17.Recker R, Lips P, Felsenberg D, Lippuner K, Benhamou L, Hawkins F, et al. Alendronate with and without cholecalciferol for osteoporosis: results of a 15-week randomized controlled trial. Curr Med Res Opin. 2006;22:1745–1755. doi: 10.1185/030079906x120913. [DOI] [PubMed] [Google Scholar]
- 18.National Osteoporosis Foundation, American Academy of Orthopaedic Surgeons. Physician's guide to prevention and treatment of osteoporosis. 2nd ed. Washington, D.C.: National Osteoporosis Foundation; 2003. [Google Scholar]
- 19.Institute of Medicine (U.S.); Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Institute of Medicine (U.S.); Subcommittee on Upper Reference Levels of Nutrients, Institute of Medicine (U.S.); Subcommittee on Interpretation, Uses of Dietary Reference Intakes. Dietary reference intakes. a report of the Subcommittee on Interpretation and Uses of Dietary Reference Intakes and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine. Applications in dietary assessment. Washington, D.C.: National Academy Press; 2001. [Google Scholar]
- 20.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 22.DeLuca HF. Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr. 2004;80(6 Suppl):1689S–1696S. doi: 10.1093/ajcn/80.6.1689S. [DOI] [PubMed] [Google Scholar]
- 23.Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353–373. doi: 10.4065/81.3.353. [DOI] [PubMed] [Google Scholar]
- 24.van Etten E, Decallonne B, Mathieu C. 1,25-dihydroxycholecalciferol: endocrinology meets the immune system. Proc Nutr Soc. 2002;61:375–380. doi: 10.1079/PNS2002170. [DOI] [PubMed] [Google Scholar]
- 25.Lips P, Wiersinga A, van Ginkel FC, Jongen MJ, Netelenbos JC, Hackeng WH, et al. The effect of vitamin D supplementation on vitamin D status and parathyroid function in elderly subjects. J Clin Endocrinol Metab. 1988;67:644–650. doi: 10.1210/jcem-67-4-644. [DOI] [PubMed] [Google Scholar]
- 26.Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc. 2008;83:1032–1045. doi: 10.4065/83.9.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vasikaran SD. Bisphosphonates: an overview with special reference to alendronate. Ann Clin Biochem. 2001;38(Pt 6):608–623. doi: 10.1258/0004563011901037. [DOI] [PubMed] [Google Scholar]
- 28.Horwitz MJ, Tedesco MB, Sereika SM, Syed MA, Garcia-Ocaña A, Bisello A, et al. Continuous PTH and PTHrP infusion causes suppression of bone formation and discordant effects on 1,25(OH)2 vitamin D. J Bone Miner Res. 2005;20:1792–1803. doi: 10.1359/JBMR.050602. [DOI] [PubMed] [Google Scholar]
- 29.Wang YH, Liu Y, Buhl K, Rowe DW. Comparison of the action of transient and continuous PTH on primary osteoblast cultures expressing differentiation stage-specific GFP. J Bone Miner Res. 2005;20:5–14. doi: 10.1359/JBMR.041016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Proportion of Patients with Vitamin D Insufficiency
Multiple Regression Analysis for Increment of Serum 25(OH)D
Serum PTH