Abstract
Objective
To determine whether a 1-day behavioral intervention, aimed at enhancing psychological flexibility, improves headache outcomes of migraine patients with comorbid depression.
Background
Migraine is often comorbid with depression, with each disorder increasing the risk for onset and exacerbation of the other. Managing psychological triggers, such as stress and depression, may result in greater success of headache management.
Method
Sixty patients with comorbid migraine and depression were assigned to a 1-day Acceptance and Commitment Training plus Migraine Education workshop (ACT-ED; N=38) or to Treatment as Usual (TAU; N=22). Patients completed a daily headache diary prior to, and for 3 months following, the intervention. Clinical variables examined included headache frequency/severity, medication use, disability, and visit to a healthcare professional. Comparisons were made between baseline findings and findings at the 3-month follow-up.
Results
Participants assigned to the ACT-ED condition exhibited significant improvements in headache frequency, headache severity, medication use, and headache-related disability. In contrast, the TAU group did not exhibit improvements. The difference in headache outcomes between ACT-ED and TAU was not statistically significant over time (i.e., the treatment by time interaction was non-significant). These results complement those of a previous report showing effects of ACT-ED verus TAU on depression and disability (1).
Conclusion
A 1-day ACT-ED workshop targeting psychological flexibility may convey benefit for patients with comorbid migraine and depression. These pilot study findings merit further investigation using a more rigorously designed large-scale trial.
Keywords: Acceptance and Commitment Therapy (ACT), Illness Management, Migraine, Headache Diaries, Treatment Outcome
Introduction
Psychiatric disorders are highly prevalent in patients with migraine (2–5). Depression, in particular, is three to five times more common among migraineurs than in the general population (6–8). This comorbidity is a major health concern as it results in decreased quality of life, poorer response to headache treatment, and overall worse prognosis (3, 9, 10). It is also associated with increased risk for suicidality, medication overuse, and disability (9–13). Prospective studies suggest that the depression-migraine relationship is bidirectional, with each disorder increasing the risk for onset and/or exacerbation of the other (6). Of concern, these epidemiological findings have not yet resulted in improved treatments for patients with both migraine and depression. For example, there have been no studies that actively recruit patients with both disorders and examine the impact of a behavioral intervention on both migraine and depression. Given the bidirectional relationship between depression and migraine, it is likely that addressing both disorders in treatment may result in better overall outcomes.
Psychological treatments of depression often share similar goals to those of migraine and thus may offer promise for addressing both conditions simultaneously (14). A growing body of work indicates that Acceptance and Commitment Therapy (ACT) may provide a unified approach to the treatment of both depression and migraine. ACT aims to target core psychological processes that are related to diverse problematic behaviors. ACT attempts to cultivate acceptance (versus experiential avoidance) and mindfulness and to encourage behavioral engagement in meaningful life activities (15, 16).. In the mental health domain, higher levels of avoidance have been associated with higher levels of general psychopathology, including depression, anxiety, and stress (17–20). In the chronic pain literature, avoidance of pain is significantly associated with greater disability and poor quality of life (17–20). Conversely, acceptance of pain is associated with reduced psychopathology, enhanced physical and social functioning, and greater pain tolerance in patients (21–23). In a recent review on headache trigger avoidance, Martin and Macleod (24) challenge the conventional wisdom that avoidance of headache triggers is optimal for functioning in the long run and instead advocates “coping with triggers.” Together, these lines of work suggest that an intervention aimed at minimizing avoidance and optimizing acceptance-based coping in patients with comorbid depression and migraine may improve both conditions.
ACT is listed by the American Psychological Association as an evidence-based treatment for disorders as varied as depression, chronic pain, mixed anxiety, obsessive-compulsive disorder, and psychosis (25). A recent treatment trial of patients with chronic headache found that an 8-session ACT group intervention resulted in significantly decreased disability and distress compared to treatment as usual (26). Importantly, even when presented as a brief intervention, ACT has resulted in positive long-term outcomes in patients with diabetes, pain, obesity, seizures, and psychosis (27) (28) (29–31).
In a previously reported successful controlled trial (1), a one-day ACT plus migraine education (ACT-ED) group workshop was compared to a Treatment As Usual (TAU) on outcomes of depression and general functioning. The ACT-ED condition resulted in significant improvements in depressive symptom levels and in general functioning relative to TAU (1). The one-day group format was chosen to ensure treatment adherence and completion, which is one of the greatest obstacles to the effective delivery of mental health services (32); for ease of implementation in primary care settings; and to allow broader access and more unitary comprehensive care for comorbid depression and migraine (33). This format is also cost-effective (34), and is more accessible and feasible than weekly treatments particularly for patients who live in rural communities or suffer other barriers to accessing care (35).
The data being presented in this manuscript come from the aforementioned treatment outcome study (1). The current manuscript, however, explores the impact of this one-day ACTED treatment on headache-specific outcomes. Thus, these data do not overlap with those presented in the previous report focused on depression and general functioning outcomes. We hypothesized that the participants in the ACT-ED condition would demonstrate more improvements in headache-related outcomes than the TAU group at the 3-month follow-up period.
Methods
Participants
Participants were 60 individuals who enrolled in the treatment study (ACT-ED N=38; TAU N=22) after meeting the following screening and inclusion criteria at intake: 1) self-reported diagnosis of migraine from a physician1; 2) scored ≥ 2 on the ID Migraine, a self-administered highly-sensitive 3-item screen for migraine (36); 3) reported 4–12 migraine days over the previous month; 4) diagnosis of current major depressive episode (MDE) on the Structured Clinical Interview (SCID-IV)(37); and 5) score of > 17 on the Hamilton Rating Scale for Depression, which suggests moderate to severe symptoms of depression (HRSD) (38, 39). Participants were excluded if they reported a history of brain injury, schizophrenia, bipolar disorder, current substance abuse, endorsed current imminent suicidality, or had begun a new medication in the previous four weeks. Eligible participants who were available on dates set for the workshop were assigned to the ACT-ED condition. Otherwise, they were assigned to TAU. A 2:1 ACT-ED to TAU assignment ratio was used in order to increase the number of patients with active treatment for estimating the within (treatment) group effect size, while still maintaining adequate power. All study procedures were approved by the university institutional review board.
Treatment Groups
Participants assigned to ACT-ED (N = 38) completed a 5-hour workshop based on ACT and migraine education. Each ACT-ED workshop included 5–8 patients and emphasized three topics. The migraine education component (one hour), implemented by a neurologist specialized in Headache Medicine (author A.R.), involved education about the pathology of migraine, risks for migraine chronification, migraine triggers, treatment of migraines, medication overuse migraine, and lifestyle factors contributing to migraine. The ACT component (four hours) was implemented by two psychologists (authors L.D. and J.M.) with extensive training in ACT. A manual was developed (by authors L.D. and J.M.) for the treatment and all workshop administrations followed the protocol closely. The workshop included training in acceptance and values-based committed action. The acceptance portion emphasized new ways of managing troubling thoughts, feelings, and pain sensations (e.g., learning how to recognize, and develop cognitive distance from, unhelpful thoughts such as “I can’t take this pain anymore” or “I am not good enough”) and learning how to willingly face experiences that cannot be changed. Training in values-based committed action involved teaching patients how to recognize ineffective patterns of behavior and habits, exploring and setting life goals and those related to health, and promoting effective and committed actions to achieve these goals despite the urge to do otherwise.
As noted above, the processes targeted in ACT are applicable to a broad range of human problems, including depression and pain. Thus, the workshop aimed at teaching these processes using examples relevant to both migraine and depression. For example, migraine involves both noxious physical experiences (e.g., physical sensations of throbbing, nausea, etc) and the reactions to them, which include thoughts (e.g., this is awful, I can’t bear this, not again), feelings (e.g., shame, worthlessness, hopelessness), and behaviors (e.g., avoidance of activities). The ACT-ED intervention did not focus directly on the noxious experiences but, instead, on the reactions to them and the effect that these reactions have had on mental health and functioning. This was done by teaching new ways to respond to thoughts and feelings related to pain – acceptance and mindfulness – and encouraging behavioral (re)commitment in meaningful life activities.
Patients in the TAU (N = 22) group completed the same clinical assessments as the ACT-ED group. Participants in both groups continued to take any medications they had been taking at entry to the study. As noted above, if participants had been on a stable dose of medication for four weeks or more, they were not excluded from the trial.
Headache Diary
All participants were asked to fill out headache diaries on a daily basis prior to the intervention (2–4 weeks) and for 3 months following the intervention. More specifically, participants recorded whether they had experienced a headache (Yes/No); if yes, they also reported headache severity (Mild, Moderate, or Severe), whether abortive medication was taken for the headache (Yes/No), whether the headache resulted in Work or Leisure Disability (Minimal, Mild, Moderate, or Severe disability), and whether the headache resulted in seeing a healthcare provider (Yes/No).
As noted above, measures of depression and general functioning were also obtained and are described in a previously published report of this study (1).
Data Analyses
Independent samples 2-tailed t-test was used to compare the ACT-ED and TAU groups on initial demographic and clinical characteristics. Generalized linear mixed (GLM) model was used to compare the probability of experiencing an event (headache, moderate to severe headache, medication use for headache, work and leisure disability) on any day during the baseline month and at the 1-, 2-, and 3-months of follow-up. This corresponds to the mean percent of days per month that an event was reported. The fixed effects in the model included treatment group, time, and treatment by time interaction. The test for treatment by time interaction compares the change over time between the ACT-ED and TAU group. From this fitted model, tests of mean contrast were performed to examine changes over time within each group and compare groups at each time point. The p-values for these tests were adjusted using Bonferroni’s method to account for the number of tests performed. The GLM is a procedure that allows us to fit a model even when there are missing data. Using maximum likelihood estimation methods, under the assumption of missing data at random, this method provides valid estimates and valid results of statistical tests. All these analyses were conducted using SAS statistical software version 9.3. The number of participants who visited a health care professional during any given month during the entire study period was small, rendering multivariate analyses not feasible. Thus, simple comparisons of rates of health care use between the two groups will be provided.
Results
Patient Characteristics
Table 1 presents demographic and clinical characteristics of the 60 study participants who enrolled in the treatment trial. Almost all participants were white and tended to be well educated, which is generally consistent with the population from which participants were recruited. Participants were mostly female, consistent with higher rates of both migraine and depression in females. Almost all participants were taking acute medications (prescribed or over-the-counter) for their migraine-related pain. Only 34% of those in the ACTED and 32% in the TAU condition were taking preventive migraine medications – consistent with findings from the American Migraine Prevalence and Prevention Study (40). Of note, the ACT-ED and TAU groups exhibited similar baseline values on the critical variables of interest.
Table 1.
Demographic Variables
| Variable | ACT-ED (n=38) | TAU (n=22) | P-value |
|---|---|---|---|
| Age (mean/SD) | 32.5 (12.6) | 29.6 (11.7) | .56 |
| Gender, % female | 95 | 91 | .28 |
| Ethnicity, % Caucasian | 90 | 82 | .40 |
| Education, % with > 12 years education | 92 | 91 | .87 |
| Working or in school, % yes | 94 | 82 | .11 |
| Age of onset of Migraines (mean/SD) | 19 (9.6) | 17 (10.3) | .99 |
| Number of migraine attacks during month prior to baseline visit (mean/SD) | 6.7 (3.3) | 7.4 (3.8) | .37 |
| Currently taking as needed acute medications for migraine (% yes) | 97 | 95 | .90 |
| Currently taking preventive medications for migraine (% yes) | 34 | 32 | .85 |
| Currently on an antidepressant medication (% yes) | 47 | 45 | .89 |
Note. ACT-ED = Acceptance and Commitment Training plus Migraine Education; TAU = Treatment as Usual.
Headache
There were 36/38 (95%) participants total in the ACT-ED group and 14/22 (64%) in the TAU group who had at least one month data consisting of 14 days or more of headache diary entries. The following represent the number of participants with data at each time point: Baseline: 25 ACT-ED, 9 TAU; One-Month Follow-Up: 33 ACT-ED, 13 TAU; Two-Month Follow-Up: 33 ACT-ED, 14 TAU; Three-Month Follow-Up: 32 ACT-ED, 12 TAU. We also examined the number of time points per participant: 21 participants in ACT-ED and 7 in TAU had data from all 4 time points; 12 participants in ACT-ED and 6 in TAU had data from 3 time points; 1 participant from TAU had data from 2 time points; 3 participants from ACT-ED had data from 1 time point.
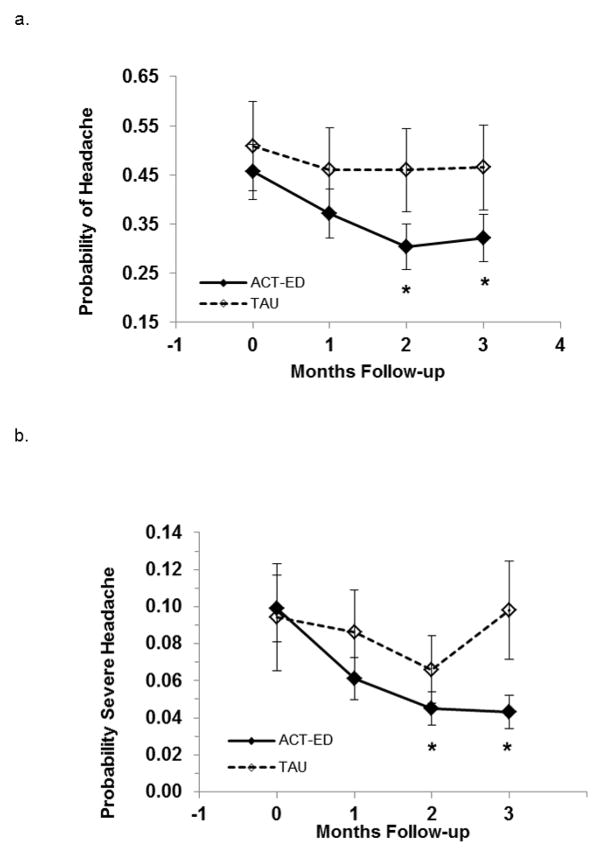
Headache Occurrence & Headache Severity
There was a significant change from baseline through the 3 follow-up months in the probability of reporting a headache on any day in the ACT-ED group (p=0.002). More specifically, the probability of a headache dropped from 45.6%±5.6% at baseline to 32.2%±4.8% at the 3 month follow-up in the ACT-ED group (Odds Ratio = .57; 95% CI = .36 –.90). In contrast, no significant change was seen in the TAU group, with probability of 50.8%%±9.1% at baseline and 46.5%±8.7% at the 3 month follow-up (p>0.90; Odds Ratio = .84; 95% CI= .41–1.7) (See Figure 1a). However, the statistical test comparing the change over time did not detect a difference between the groups (treatment*time interaction p=0.40).
Figure 1.
a. Probability of reporting a headache for the ACT-ED and TAU groups at baseline and over the 3-month follow-up period.
*significant difference within ACT-ED group from baseline to 2-months (p < .01) and to 3-months (p<.01). All other between group and within group differences were non-significant.
b. Probability of experiencing moderate to severe pain for the ACT-ED and TAU groups at baseline and over the 3-month follow-up period.
*significant difference within ACT-ED group from baseline to 2 months (p<.01) and to 3 months (p < .01). All other between group and within group differences were non-significant.
Similar findings were seen for headache severity (rating of pain as moderate or severe). The probability of experiencing a moderate to severe headache dropped from 10%± 1.8% at baseline to 4.3 %±1.0% at the 3 month follow-up in the ACT-ED group (p=.004). This difference is expressed as an odds ratio of .41 (95% CI: .22–.77). In contrast, no significant change was seen in the TAU group, where probability of experiencing a moderate to severe headache was 9.4%%±9.1% at baseline and 9.8%±2.7% at the 3 month follow-up (p>.90; Odds Ratio = 1.0; 95% CI: .41 – 2.7) (See Figure 1b). However, the statistical test comparing the change over time was not able to detect a difference between the groups (treatment*time interaction p=0.20).
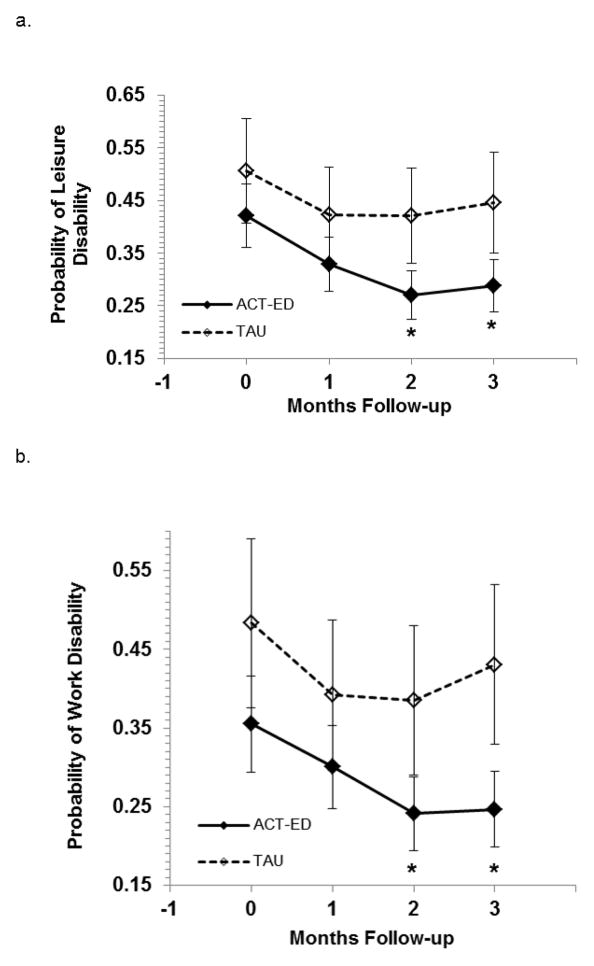
Leisure and Work Disability
The probability of experiencing disability for leisure activities dropped from 42.1%±6.0% at baseline to 28.8%±4.9% at the 3 month follow-up in the ACT-ED group (p=0.016) but did not significantly change in the TAU group (p>0.90; 50.6%±10.0% at baseline and 44.6%±9.5% at the 3 month follow-up) (See Figure 2a). The odds ratio for leisure disability at 3-month follow-up relative to baseline is .56 (95% CI=.32–.97) in the ACT-ED group and .78 (95% CI = .33 – 1.9) in the TAU group. The overall treatment by time interaction was not significant (p=.70).
Figure 2.
a. Probability of experiencing leisure disability for the ACT-ED and TAU groups at baseline and over the 3-month follow-up period.
*significant difference within ACT-ED group from baseline to 2 months (p<.01) and to 3 months (p = .02). All other between group and within group differences were non-significant.
b. Probability of experiencing work disability for the ACT-ED and TAU groups at baseline and over the 3-month follow-up period.
*significant difference within ACT-ED group from baseline to 2 months (p<.05) and to 3 months (p < .05). All other between group and within group differences were non-significant.
As shown in Figure 2b, the probability of experiencing work disability dropped from 35.5%±6.1% at baseline to 24.6%±4.8% at the 3 month follow-up in the ACT-ED group (p=.04; Odds Ratio=1.0, 95% CI: .33–1.1). In contrast, the TAU group did not exhibit a significant change in work disability between baseline (48%±10.7%) and the 3-month follow-up (43.1%±10.2%; odds ratio = 1.8, 95% CI: .32–2.1; p>.90). The overall treatment by time interaction was not significant (p=.66).
Use of Acute Medication for Headache
Findings for use of acute headache medication was consistent with that of headache occurrence and severity (see Figure 3). There was a significant decrease (p=0.048) in medication use in the ACT-ED group from baseline (23.6%±3.8%) to the 3-month post-intervention follow-up (16.4%±2.8%). This difference is expressed as an odds ratio of .64 (95% CI: .37–1.1). In contrast, the TAU group did not exhibit a significant change in medication use from baseline (28.0%±6.8%) to the 3 month follow-up (27.3%±6.1%) (Odds Ratio= .97; 95% CI: .42–2.2; p>0.90). The overall treatment by time interaction was not significant (p=.50).
Figure 3.
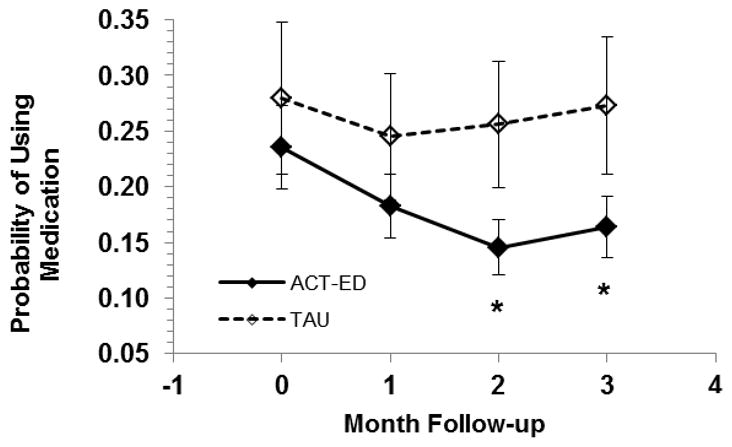
Probability of taking medication during acute attack for the ACT-ED and TAU groups at baseline and over the 3-Month Follow-up Period.
*significant difference within ACT-ED group from baseline to 2 months (p<.01) and to 3 months (p < .05). All other between group and within group differences were non-significant.
Visit to Health Care Professional
Finally, we examined the number of participants who visited a health care professional during the study period. In the month prior to the intervention, 20% (5/25) participants in the ACT-ED group and 22% (2/9) in the TAU group reported seeing a health professional. At the 3-month follow-up, this rate dropped to 3% (1/32) for the ACT-ED group but increased to 33% (4/12) in the TAU group.
Overall, the difference in headache outcomes between ACT-ED and TAU was not statistically significant over time (i.e., the treatment by time interaction was non-significant). However, at the three-month follow-up assessment, patients in the ACT-ED condition reported fewer headache days, decreased headache pain severity, less disability and use of medications, and decreased visits to a healthcare professional compared to baseline. In contrast, the TAU group did not exhibit significant improvements in these areas from baseline to the three-month follow-up.
Medication Changes and Involvement in Psychotherapy
Preventive Migraine Medication
Three of thirty six participants in the ACT-ED group (8%) and 3/14 in the WL/TAU group (21%) started or increased their dose of a preventive migraine medication during the follow-up period. A Fisher’s Exact test indicated this difference was not significant (p =.3). None of the participants in ACT-ED and 1/14 (7%) in the WL/TAU had either reduced or discontinued a migraine preventive medicine. This difference also was not significant (Fisher’s Exact Test: p =.28).
Antidepressant Use
Nine of thirty six participants in the ACT-ED group (25%) and 5/14 in the WL/TAU group (36%) started, or increased their dose of, an antidepressant during the follow-up period. A Fisher’s Exact Test indicated this difference was not significant (p =.50). Two of thirty-six participants in ACT-ED (6%) and 2/14 (14%) in the WL/TAU had either reduced or discontinued an antidepressant (p =.31).
Psychotherapy
Three of thirty six participants in the ACT-ED group (8%) and 2/14 in the WL/TAU group (14%) began psychotherapy or counseling during the three month follow-up period (Fishers Exact Test: p =.61).
Discussion
This pilot study suggests that a 1-day group workshop is feasible and acceptable for patients with comorbid depression and migraine. Thus, it can be considered as alternative to the regularly prescribed weekly behavioral treatments. It also demonstrates that patients in the ACT-ED intervention exhibited significant reductions in headache frequency, pain severity, disability, and medication use. In contrast, the TAU group did not exhibit improvements. Of note, however, the treatment by time interaction effects across headache outcomes were not significant. It will be important to test this intervention in a more rigorously designed and larger-scale clinical trial with randomized assignment. Doing so would clarify whether the null treatment by time interaction effect in the pilot was due to inadequate power or whether the ACT-ED treatment effect was not strong enough to show a difference between groups over time.
A larger trial would also allow for examination of possible mediators and moderators of treatment response. Understanding the specific mechanisms or processes that mediate clinical improvement in headache outcomes allows for intervention optimization by refining and emphasizing the components responsible for change and eliminating non-active ingredients. Increased understanding of the active processes that underlie therapeutic improvement will also increase prospects for understanding and addressing impediments and failures in treatment. If ACT-ED proves to be efficacious, it would have important implications for patients suffering from comorbid migraine and depression – namely that that they can be treated for both of their conditions using a unified approach.
The extremely high proportion of outpatients who drop out of treatment prematurely presents one of the greatest obstacles to the effective delivery of mental health services. A brief intervention ensures treatment adherence and completion, and is more feasible for patients who live in rural communities or suffer other barriers to accessing care. Relatively large effects for brief ACT interventions that are maintained through several months of follow-up have been shown in controlled trials of patients with health problems (27–30). However, this is the first study to assess the impact of a one-day workshop on headache outcomes in a population with comorbid psychiatric and medical problems. These promising initial findings merit further study and replication with a more rigorous design.
Despite extensive epidemiological research documenting the high prevalence of depression in patients with migraine and the negative effects this comorbidity has on outcomes, there is a striking paucity of clinical studies addressing this comorbidity (9, 14, 41, 42). This was the first study utilizing an ACT approach to improve the emotional and physical functioning of patients with comorbid depression and migraine (1). The goal of ACT is to help patients flexibly respond to life events in ways that do not exacerbate difficulties and do not restrict their engagement in meaningful life activities. In this group of depressed migraineurs specifically, patients were taught to notice the differences between the physical sensations of the migraine (i.e., noxious physical experiences such as physical sensations of throbbing pain, nausea, and enhanced sensitivity to sensory stimulation) and their reactions to them, which may include thoughts (e.g., I can’t bear this, this is awful), feelings (e.g., shame, worthlessness, hopelessness), and behaviors (e.g., avoidance of activities) that exacerbate the migraine.
Viewing the migraine pain as “unacceptable” not only exacerbates the headache pain, but also leads to avoidance of situations that may elicit pain, sometimes with significant costs to quality of life. From an ACT theoretical perspective, decreased engagement in meaningful activities leads to greater feelings of isolation, depression, and reduced functioning. Thus, patients are taught how to acknowledge their pain without struggling with it, to examine whether their avoidance strategies are actually helping with their pain in the long run, to recognize the effect this avoidance is having on life engagement and vitality, and are encouraged to re-engage in their life in meaningful and valuable ways.
There is preliminary data showing that Pain Acceptance and Values-based Actions are positively associated with better physical functioning and negatively associated with depression and disability in migraine patients (43). An important next step would be to empirically assess whether these processes did in fact mediate the changes observed in headaches. In chronic pain patients, changes in acceptance during treatment have been found to be related to improvements in functioning and quality of life (18, 19, 27, 28, 44–46).
Limitations and Future Directions
The intervention implemented in this study included both ACT and education about migraine. Thus, it is impossible to assess the separate contribution of these different elements. Future studies should compare the efficacy of ACT separately from migraine education and should include assessments of putative change processes. Future studies should also assess treatment integrity across workshop administrations and the influence this has on treatment response.
To date, there are no studies that assess the effects of treating psychiatric comorbidity on migraine symptoms. Given the bidirectional influence of depression and migraine, an improvement in one disorder should result in improvement in the other. It is difficult to determine from this study whether improvements in depression and functioning led to improvements in headache or whether the reverse is true.
Future studies should also ensure random treatment assignment. In the current study, participant assignment to ACT-ED or TAU was based on availability. It is possible that the participants in the two groups differ in important ways, such as motivation. Furthermore, the 3-month follow-up period in this study is relatively short. Future studies should examine whether the positive treatment effects obtained here persist over longer periods of time or if they begin to wear off at certain times. This could provide important information about timing for booster sessions.
A greater number of participants in the ACT-ED condition completed headache diaries throughout the study period compared to the TAU condition (95% versus 64%, respectively). It is unclear how this may have affected the results of this study and we currently do not have the ability to elucidate reasons for these differences. It is possible, however, that participants in the ACT-ED group felt a greater sense of commitment to the study because of their involvement in the treatment arm. It is also possible that patients experiencing worsening of symptoms are less likely to complete diaries, in which case effect sizes would be larger for the ACT-ED condition. Alternatively, if participants who are experiencing improvements in symptoms are less likely to complete diaries, the effect size for ACT-ED would be attenuated. Future studies should address this issue by providing better guidance to patients on the importance of completing the headache diaries and perhaps providing incentives for doing so.
Finally, migraine diagnosis in this study was not based on a clinical assessment; it was based on the ID-Migraine, patient’s report that his/her physician had diagnosed a migraine, and verification of diagnosis of migraine in medical charts for nearly two-thirds of the patients. Although misdiagnosis is possible, the ID-Migraine has been demonstrated to have high sensitivity and specificity (36). In addition, a study by Martin and colleagues examining the predictive value of migraine diagnostic criteria found that the three ID-Migraine items can effectively predict migraine in diverse clinical settings (47). Nonetheless, future studies should obtain formal migraine diagnoses of participants.
Acknowledgments
This work was made possible by grants number KL2RR024980 and UL1RR024979 to the first author from the National Center for Research Resources (NCRR), a part of the National Institutes of Health (NIH); and grant number K08 NS066087-05 to the second author. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CTSA or NIH.
Abbreviations
- ACT
Acceptance and Commitment Therapy
- TAU
Treatment as Usual
Footnotes
58% the participants had medical files in our hospital and we were able to confirm the diagnosis of migraine by a physician through chart review.
The authors declare that there are no conflicts of interest in this study
References
- 1.Dindo L, Recober A, Marchman JN, Turvey C, O’Hara MW. One-day behavioral treatment for patients with comorbid depression and migraine: A pilot study. Behav Res Ther. 2012;50(9):537–43. doi: 10.1016/j.brat.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jette N, Patten S, Williams J, Becker W, Wiebe S. Comorbidity of migraine and psychiatric disorders--a national population-based study. Headache. 2008;48(4):501–16. doi: 10.1111/j.1526-4610.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- 3.Pompili M, Di Cosimo D, Innamorati M, Lester D, Tatarelli R, Martelletti P. Psychiatric comorbidity in patients with chronic daily headache and migraine: a selective overview including personality traits and suicide risk. J Headache Pain. 2009;10(4):283–90. doi: 10.1007/s10194-009-0134-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radat F, Swendsen J. Psychiatric comorbidity in migraine: a review. Cephalalgia. 2005;25(3):165–78. doi: 10.1111/j.1468-2982.2004.00839.x. [DOI] [PubMed] [Google Scholar]
- 5.Sheftell FD, Atlas SJ. Migraine and psychiatric comorbidity: from theory and hypotheses to clinical application. Headache. 2002;42(9):934–44. doi: 10.1046/j.1526-4610.2002.02217.x. [DOI] [PubMed] [Google Scholar]
- 6.Breslau N, Lipton RB, Stewart WF, Schultz LR, Welch KM. Comorbidity of migraine and depression: investigating potential etiology and prognosis. Neurology. 2003;60(8):1308–12. doi: 10.1212/01.wnl.0000058907.41080.54. [DOI] [PubMed] [Google Scholar]
- 7.Hamelsky SW, Lipton RB. Psychiatric comorbidity of migraine. Headache. 2006;46(9):1327–33. doi: 10.1111/j.1526-4610.2006.00576.x. [DOI] [PubMed] [Google Scholar]
- 8.Lake AE, 3rd, Rains JC, Penzien DB, Lipchik GL. Headache and psychiatric comorbidity: historical context, clinical implications, and research relevance. Headache. 2005;45(5):493–506. doi: 10.1111/j.1526-4610.2005.05101.x. [DOI] [PubMed] [Google Scholar]
- 9.Buse DC, Andrasik F. Behavioral medicine for migraine. Neurol Clin. 2009;27(2):445–65. doi: 10.1016/j.ncl.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Cahill CM, Murphy KC. Migraine: another headache for psychiatrists? Br J Psychiatry. 2004;185:191–3. doi: 10.1192/bjp.185.3.191. [DOI] [PubMed] [Google Scholar]
- 11.Smitherman TA, McDermott MJ, Buchanan EM. Negative impact of episodic migraine on a university population: quality of life, functional impairment, and comorbid psychiatric symptoms. Headache. 2011;51(4):581–9. doi: 10.1111/j.1526-4610.2011.01857.x. [DOI] [PubMed] [Google Scholar]
- 12.Lake AE., 3rd Medication overuse headache: biobehavioral issues and solutions. Headache. 2006;46 (Suppl 3):S88–97. doi: 10.1111/j.1526-4610.2006.00560.x. [DOI] [PubMed] [Google Scholar]
- 13.Bigal ME, Lipton RB. Modifiable risk factors for migraine progression. Headache. 2006;46(9):1334–43. doi: 10.1111/j.1526-4610.2006.00577.x. [DOI] [PubMed] [Google Scholar]
- 14.Baskin SM, Smitherman TA. Comorbidity between migraine and depression: update on traditional and alternative treatments. Neurol Sci. 2011;32 (Suppl 1):S9–13. doi: 10.1007/s10072-011-0549-9. [DOI] [PubMed] [Google Scholar]
- 15.Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behav Ther. 2004;35(4):639–65. doi: 10.1016/j.beth.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Hayes SC, Strosahl K, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. New York City: Guilford Press; 1999. [Google Scholar]
- 17.McCracken LM, Vowles KE, Eccleston C. Acceptance-based treatment for persons with complex, long standing chronic pain: a preliminary analysis of treatment outcome in comparison to a waiting phase. Behav Res Ther. 2005;43(10):1335–46. doi: 10.1016/j.brat.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Vowles KE, McCracken LM, Eccleston C. Processes of change in treatment for chronic pain: the contributions of pain, acceptance, and catastrophizing. Eur J Pain. 2007;11(7):779–87. doi: 10.1016/j.ejpain.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 19.Vowles KE, Wetherell JL, Sorrell JT. Targeting Acceptance, Mindfulness, and Values-Based Action in Chronic Pain: Findings of Two Preliminary Trials of an Outpatient Group-Based Intervention. Cognitive and Behavioral Practice. 2009;16(1):49–58. [Google Scholar]
- 20.Buse DC, Rupnow MF, Lipton RB. Assessing and managing all aspects of migraine: migraine attacks, migraine-related functional impairment, common comorbidities, and quality of life. Mayo Clin Proc. 2009;84(5):422–35. doi: 10.1016/S0025-6196(11)60561-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCracken LM, Vowles KE. Acceptance of chronic pain. Curr Pain Headache Rep. 2006;10(2):90–4. doi: 10.1007/s11916-006-0018-y. [DOI] [PubMed] [Google Scholar]
- 22.Viane I, Crombez G, Eccleston C, Devulder J, De Corte W. Acceptance of the unpleasant reality of chronic pain: effects upon attention to pain and engagement with daily activities. Pain. 2004;112(3):282–8. doi: 10.1016/j.pain.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 23.Vowles KE, McNeil DW, Gross RT, McDaniel ML, Mouse A, Bates M, et al. Effects of pain acceptance and pain control strategies on physical impairment in individuals with chronic low back pain. Behav Ther. 2007;38(4):412–25. doi: 10.1016/j.beth.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Martin PR, MacLeod C. Behavioral management of headache triggers: Avoidance of triggers is an inadequate strategy. Clin Psychol Rev. 2009;29(6):483–95. doi: 10.1016/j.cpr.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 25.http://www.div12.org/PsychologicalTreatments/treatments.html.
- 26.Mo’tamedi H, Rezaiemaram P, Tavallaie A. The effectiveness of a group-based acceptance and commitment additive therapy on rehabilitation of female outpatients with chronic headache: preliminary findings reducing 3 dimensions of headache impact. Headache. 2012;52(7):1106–19. doi: 10.1111/j.1526-4610.2012.02192.x. [DOI] [PubMed] [Google Scholar]
- 27.Gregg JA, Callaghan GM, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: a randomized controlled trial. J Consult Clin Psychol. 2007;75(2):336–43. doi: 10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- 28.Dahl J, Wilson KG, Nilsson A. Acceptance and commitment therapy and the treatment of persons at risk for long-term disability resulting from stress and pain symptoms: A preliminary randomized trial. Behav Ther. 2004;35(4):785–801. [Google Scholar]
- 29.Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann Behav Med. 2009;37(1):58–69. doi: 10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]
- 30.Lundgren T, Dahl J, Melin L, Kies B. Evaluation of acceptance and commitment therapy for drug refractory epilepsy: a randomized controlled trial in South Africa--a pilot study. Epilepsia. 2006;47(12):2173–9. doi: 10.1111/j.1528-1167.2006.00892.x. [DOI] [PubMed] [Google Scholar]
- 31.Bach P, Hayes SC. The use of acceptance and commitment therapy to prevent the rehospitalization of psychotic patients: a randomized controlled trial. J Consult Clin Psychol. 2002;70(5):1129–39. doi: 10.1037//0022-006x.70.5.1129. [DOI] [PubMed] [Google Scholar]
- 32.Wierzbicki M, Pekarik G. Professional Psychology: Research and Practice. 1993. A Meta-Analysis of Psychotherapy Dropout. [Google Scholar]
- 33.Cummings NA, Cummings JL, Johnson JN, Baker NJ. Behavioral health in primary care: a guide for clinical integration. Madison: Psychosocial Press; 1997. [Google Scholar]
- 34.Robinson P, Gregg J, Dahl J, Lundgren T. ACT in medical settings. In: Hayes SC, Strosahl K, editors. A practical guide to acceptance and commitment therapy. Springer; 2004. pp. 295–314. [Google Scholar]
- 35.Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res. 2005;40(1):135–55. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lipton RB, Dodick D, Sadovsky R, Kolodner K, Endicott J, Hettiarachchi J, et al. A self-administered screener for migraine in primary care: The ID Migraine validation study. Neurology. 2003;61(3):375–82. doi: 10.1212/01.wnl.0000078940.53438.83. [DOI] [PubMed] [Google Scholar]
- 37.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–9. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 38.Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry. 1988;45(8):742–7. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- 39.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6(4):278–96. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 40.Diamond S, Bigal ME, Silberstein S, Loder E, Reed M, Lipton RB. Patterns of diagnosis and acute and preventive treatment for migraine in the United States: results from the American Migraine Prevalence and Prevention study. Headache. 2007;47(3):355–63. doi: 10.1111/j.1526-4610.2006.00631.x. [DOI] [PubMed] [Google Scholar]
- 41.Maizels M, Smitherman TA, Penzien DB. A review of screening tools for psychiatric comorbidity in headache patients. Headache. 2006;46 (Suppl 3):S98–109. doi: 10.1111/j.1526-4610.2006.00561.x. [DOI] [PubMed] [Google Scholar]
- 42.Evans RW, Rosen N. Expert opinion: migraine, psychiatric comorbidities, and treatment. Headache. 2008;48(6):952–8. doi: 10.1111/j.1526-4610.2008.01074.x. [DOI] [PubMed] [Google Scholar]
- 43.Dindo L, Recober A, Marchman J, O’Hara M, Turvey C. Depression and Disability in Migraine: The Role of Pain-Acceptance and Values-Based Action. Under Review. [DOI] [PubMed] [Google Scholar]
- 44.Wicksell RK, Melin L, Lekander M, Olsson GL. Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quality of life in longstanding pediatric pain--a randomized controlled trial. Pain. 2009;141(3):248–57. doi: 10.1016/j.pain.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 45.Vowles KE, McCracken LM. Comparing the role of psychological flexibility and traditional pain management coping strategies in chronic pain treatment outcomes. Behav Res Ther. 2010;48(2):141–6. doi: 10.1016/j.brat.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 46.McCracken LM, Gutierrez-Martinez O. Processes of change in psychological flexibility in an interdisciplinary group-based treatment for chronic pain based on Acceptance and Commitment Therapy. Behav Res Ther. 2011;49(4):267–74. doi: 10.1016/j.brat.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 47.Martin VT, Penzien DB, Houle TT, Andrew ME, Lofland KR. The predictive value of abbreviated migraine diagnostic criteria. Headache. 2005;45(9):1102–12. doi: 10.1111/j.1526-4610.2005.00234.x. [DOI] [PubMed] [Google Scholar]