Abstract
Although antifungal prophylaxis is frequently administered to patients with acute myeloid leukemia (AML) during remission-induction chemotherapy (RIC), its impact on reducing invasive fungal infections (IFIs) outside clinical trials is rarely reported. We performed a retrospective observational study to identify risk factors for development of IFIs (definite or probable, using revised European Organization for Research and Treatment of Cancer [EORTC] criteria) and all-cause mortality in a cohort of 152 AML patients receiving RIC (2009 to 2011). We also compared rates of IFI and mortality in patients who received echinocandin versus anti-Aspergillus azole (voriconazole or posaconazole) prophylaxis during the first 120 days of RIC. In multivariate analysis, clofarabine-based RIC (hazard ratio [HR], 3.5; 95% confidence interval [CI], 1.5 to 8.3; P = 0.004) and echinocandin prophylaxis (HR, 4.6; 95% CI, 1.8 to 11.9; P = 0.002) were independently associated with higher rates of IFI rates during RIC. Subsequent analysis failed to identify any malignancy- or chemotherapy-related covariates linked to echinocandin prophylaxis that accounted for the higher rates of breakthrough IFI. Although the possibility of other confounding variables cannot be excluded, our findings suggest that echinocandin-based prophylaxis during RIC for AML may be associated with a higher risk of breakthrough IFI.
INTRODUCTION
Patients with acute myeloid leukemia (AML) undergoing remission-induction chemotherapy (RIC) are among those in the highest risk group for developing invasive fungal infections (IFIs), especially mold infections (1–3). However, the optimal strategy for using antifungal prophylaxis in this population (i.e., which drug should be administered and whether it should be a broad- or narrow-spectrum drug) continues to be debated and often differs from one treatment center to the next (4–7).
Recently we reported on the incidence density of documented IFIs (definite or probable; revised European Organization for Research and Treatment of Cancer [EORTC] and Mycoses Study Group [MSG] criteria) (8) in a contemporary cohort of patients with newly diagnosed AML who received primary antifungal prophylaxis (PAP) during RIC (3). Despite the frequent use of voriconazole or posaconazole prophylaxis (72% of evaluated cases), the incidence density of documented IFIs was 2.0 infections per 1,000 prophylaxis days, and the majority of breakthrough infections were caused by invasive molds (3). Importantly, in this epidemiological study we also observed a higher incidence density of breakthrough IFI among patients receiving an echinocandin as primary antifungal prophylaxis. As several confounding variables may influence the risk for breakthrough IFI independently of the type of prophylaxis selected, we examined whether specific patient risk factors that are independent of echinocandin use may explain the higher rates of breakthrough IFI documented among AML patients undergoing RIC.
MATERIALS AND METHODS
Study designs and patients.
We performed a retrospective, observational study to investigate predictive factors for documented IFIs and death within 120 days of starting remission induction chemotherapy (RIC) in a cohort of 152 adult (18 years of age and older) patients with newly diagnosed AML. The study population was drawn from consecutive unselected patients at the University of Texas MD Anderson Cancer Center who were admitted during 2009 to 2011 for RIC. All patients were prescribed antifungal prophylaxis during their treatment (3). We excluded patients with a history of prior stem cell transplantation (SCT) or patients who received transplantation within 120 days of the first admission. Details concerning the study population and variable definitions have been previously reported (3) and are summarized as supplemental information (see File S1 in the supplemental material). This observational study was approved by the MD Anderson Institutional Review Board Committee.
Two analyses were performed to evaluate risk factors associated with the development of IFI and, as a secondary endpoint, all-cause mortality following initiation of RIC. First, we compared malignancy-, chemotherapy-, and infection-related risk factors in patients who developed IFIs versus patients who were IFI free at 120 days following the initiation of RIC. We then compared risk factors for mortality at 120 days. Patients were excluded from the analysis if they did not complete RIC in the hospital (n = 6) or received only fluconazole prophylaxis (n = 12). The drug, dose, and duration of primary antifungal prophylaxis were determined by the treating hematologist and were not standardized per an institutional prophylaxis protocol for AML patients.
After screening disease- and chemotherapy-related covariates associated with breakthrough IFI and all-cause mortality, we then compared risk factors for IFI in patients who received anti-Aspergillus triazoles (voriconazole or posaconazole) versus echinocandin prophylaxis. For the purposes of this analysis, patients must have received the anti-Aspergillus triazole or echinocandin for more than two consecutive days before switching to another antifungal agent. Patients were not included in the analysis if they had received multiple Aspergillus-active therapies or fluconazole-only prophylaxis or had not been hospitalized during the first 42 days of RIC. We did not exclude patients if they had a period of overlapping fluconazole prophylaxis with either a mold-active triazole or an echinocandin.
Data collection.
Data were extracted from patients' electronic medical records and collected until diagnosis of an IFI, loss to follow-up, death, or completion of 120 days post-RIC, whichever came first.
Information regarding antifungal use, including the type and duration of antifungal drugs used for prophylaxis, from the institutional pharmacy database was confirmed and matched with the electronic patient medical record. Candidate predictive variables were screened for their association with documented IFI and their frequency among patients receiving echinocandin versus voriconazole or posaconazole prophylaxis. These variables included the following: baseline disease characteristics, admission to the high-efficiency particulate air (HEPA) filter room, the type of immunosuppressive chemotherapy regimen received during first remission-induction chemotherapy, episodes and duration of hospitalization and neutropenia, time to overall remission (9), and the use of primary antifungal prophylaxis during the study period.
Statistical analysis.
Categorical variables were compared using the chi-square test or Fisher's exact test, and continuous variables were compared using Wilcoxon rank sum tests. Cox proportional hazard models were used to identify predictive factors for documented IFI and mortality. First, univariate analyses were performed to evaluate the predictive effect of each factor alone. Then, any factor with a P value < 0.20 from its univariate test was selected to construct a full multivariate Cox regression model. Finally, the full model was reduced to a final model using the stepwise selection method so that all the factors remaining in the model were statistically significant. The proportional hazard assumptions were tested for the final Cox models by including the interactions of all the predictors with log of survival time. Hospitalization, neutropenia, overall remission, and anti-Aspergillus triazole, echinocandin, and fluconazole use were treated as time-dependent variables in the analysis. In addition, Kaplan-Meier curves were constructed to estimate the probability of being IFI free stratified by antifungal prophylaxis strategy. All tests were two-sided with a significance level of 0.05. The analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
Study cohort.
Demographic and clinical characteristic comparisons between 21 subjects with documented IFI and 104 patients who were IFI free 120 days after beginning RIC are shown in Table 1. A majority (82%) of the AML study population remained in the hospital for the first 42 days after initiating RIC. After the inclusion criteria described above were applied, data from 21 patients with episodes of IFI and 104 controls were available for analysis.
TABLE 1.
Candidate risk factors for documented IFI in patients with AML during first 120 days after first remission-induction chemotherapy
| Demographicp | Documented IFI (n = 21) | No IFI (n = 104) | P valuea |
|---|---|---|---|
| Male, n (%) | 7 (33) | 62 (60) | 0.05 |
| Median age (IQR), yrs | 63 (57–70) | 65 (51–73) | 0.7 |
| Hospitalizationb | 0.11 | ||
| Median no. of hospitalizations (IQR) | 1 (1–1) | 2 (1–3) | |
| Median duration (IQR), days | 21 (14–29) | 31 (22–39) | |
| Admission to the HEPA filter room, n (%) | 8 (38) | 35 (34) | 0.7 |
| Underlying conditions,c n (%) | |||
| Lung disease or infectiond | 5 (24) | 26 (25) | 0.95 |
| Concomitant bacterial infectione | 5 (24) | 15 (14) | 0.3 |
| Cardiovascular disease or condition | 8 (38) | 32 (31) | 0.46 |
| Diabetes mellitus or hyperglycemiaf | 5 (24) | 18 (17) | 0.57 |
| History of renal failure or renal dysfunctiong | 1 (5) | 15 (14) | 0.23 |
| Abnormal liver testsh | 2 (10) | 13 (13) | 0.76 |
| No. (%) with other malignancyi | 7 (33) | 19 (18) | 0.13 |
| No. (%) chemotherapy naive | 16/21 (80) | 94/103 (91) | 0.04 |
| WHO AML classification,j n (%) | |||
| Therapy-related AML | 4/21 (19) | 4/102 (4) | 0.03 |
| MDS-related changes | 8/21 (38) | 29/102 (28) | 0.46 |
| Recurrent genetic abnormalities | 5/21 (24) | 20/102 (20) | 0.71 |
| Myeloid sarcoma | 0/21 (0) | 3/102 (3) | 0.31 |
| Acute leukemia of ambiguous lineage | 0/21 (0) | 2/102 (2) | 0.37 |
| Not specified | 4/21 (19) | 44/102 (43) | 0.07 |
| Cytogenetic risk group,k n (%) | |||
| Favorable | 5 (24) | 19 (18) | 0.58 |
| Intermediate I | 1 (5) | 9 (9) | 0.65 |
| Intermediate II | 7 (33) | 30 (29) | 0.32 |
| Adverse | 8 (38) | 46 (44) | 0.41 |
| Remission-induction chemotherapy, n (%) | |||
| Cytarabine-based regimen | 16 (76) | 77 (74) | 0.82 |
| Other regimen | 5 (24) | 27 (26) | 0.99 |
| Investigational chemotherapyl | 14 (67) | 37 (36) | 0.10 |
| Clofarabine-based regimenm | 10 (48) | 19 (18) | 0.006 |
| Overall remission | 0.3 | ||
| Overall remission, n (%)n | 4 (19) | 71 (68) | |
| Neutropenia | 0.12 | ||
| Neutropenia at start of prophylaxis, n (%) | 12 (57) | 54 (52) | |
| Median no. of episodes of neutropenia (IQR) | 1 (1–2) | 3 (1–4) | |
| Median duration of neutropenia (IQR), dayso | 23 (16–31) | 47 (28–70) | |
| Primary antifungal prophylaxis | |||
| Anti-Aspergillus azole (voriconazole or posaconazole) | 0.009 | ||
| Anti-Aspergillus azole use, n (%) | 10 (48) | 77 (74) | |
| Median duration of anti-Aspergillus azoles (days), IQR | 19 (13–25) | 75 (29–101) | |
| Fluconazole | 0.4 | ||
| Fluconazole use, n (%) | 7 (33) | 40 (38) | |
| Median duration of fluconazole (days), IQR | 5 (2–35) | 31 (7–80) | |
| Echinocandin | 0.002 | ||
| Echinocandin use, n (%) | 17 (81) | 66 (63) | |
| Median duration of echinocandins (days), IQR | 11 (7–21) | 17 (9–28) |
Univariate Cox regression analysis.
Time-dependent variable.
At-hospital admission or history.
Lung infection at hospital admission or concomitant to AML history.
At-hospital admission or concomitant to AML history according to the patient's treating physician based on clinical, microbiology, and antibiotic prescription data.
Diagnosis of diabetes mellitus or induced hyperglycemia (glucose ≥ 200 mg/dl).
Diagnosis of renal failure or a 50% increase in serum creatinine level.
Diagnosis of liver disease or abnormal liver blood tests (serum alanine aminotransferase and/or aspartate aminotransferase levels > 3.0 × upper limit of normality [ULN] and/or total bilirubin > 1.5 × ULN).
Solid cancers in breast (9 patients), skin (7), prostate (4), parotid (2), thyroid (1), vocal cord (1), and cervix uteri (1); chronic myelomonocytic leukemia (2); acute lymphoblastic leukemia (1); Hodgkin's lymphoma (1); not specified (3).
Data are from Vardiman et al. (20).
Data are from Estey (21).
Eleven investigational chemotherapy protocols.
Three investigational clofarabine-containing protocols in FRIC: (i) clofarabine plus low-dose cytarabine followed by consolidation of clofarabine plus low-dose cytarabine alternating with decitabine in frontline AML and high-risk MDS (n = 20 patients); (ii) clofarabine, idarubicin, and cytarabine combination as induction therapy for younger patients with AML (n = 7 patients); (iii) phase I/II study of plerixafor and clofarabine in previously untreated older (≥60 years of age) adult patients with AML with two or more unfavorable prognostic factors for whom standard induction chemotherapy is unlikely to be of benefit (n = 2 patients).
Overall remission as described by Faderl et al. (9).
Considering all episodes of neutropenia.
HEPA, high-efficiency particulate air; MDS, myelodysplastic syndrome.
Antifungal prophylaxis in documented IFI cases.
Table S1 in the supplemental material describes the epidemiology, clinical features, and outcome determined for 21 AML patients with documented IFIs during the 120-day study period. Documented IFIs developed a median of 20 days (interquartile range [IQR], 15 to 32 days) after RIC (see Table S1). During periods of echinocandin prophylaxis, breakthrough infections included culture- or histology-proven Paecilomyces pulmonary and rib osteomyelitis infections (n = 1), fusariosis (n = 1), and sinopulmonary mold infection (n = 1); probable aspergillosis (n = 6); coccidiomycosis (n = 1); candidemia (n = 3); and Saprochaete capitata (Blastoschizomyces capitatus) bloodstream infection (n = 1). Breakthrough infections during posaconazole/voriconazole prophylaxis included proven mold infection (sterile hyphae) (n = 1); probable aspergillosis (n = 4); and probable fusariosis (n = 1).
Predictive factors for IFI and mortality.
Univariate analysis revealed that patients with documented IFIs were more likely to be female (P = 0.05), have had prior chemotherapy-related AML (P = 0.03), have a history of prior chemotherapy (P = 0.04), and have received clofarabine-based RIC (P = 0.006) or echinocandin prophylaxis (P = 0.002). Patients who died during the first 120 days after beginning RIC were more likely to have had lung disease or infection (P = 0.04) or cardiovascular disease (P = 0.05) as an underlying condition and less likely to have achieved remission during chemotherapy (P = 0.02) and to have received posaconazole/voriconazole primary antifungal prophylaxis (P = 0.026).
In the final multivariate Cox regression model for IFI, risk-only echinocandin prophylaxis (P = 0.002) and receipt of clofarabine-based chemotherapy (P = 0.004) were retained as independent factors associated with breakthrough IFI. Independent predictors for increased mortality were hospitalization (P = 0.017) and having lung disease or infection as an underlying condition (P = 0.031). In our study cohort, receipt of echinocandin (P = 0.47) or posaconazole/voriconazole prophylaxis (P = 0.09) did not independently influence the patient mortality rate.
Comparison of anti-Aspergillus prophylaxis data.
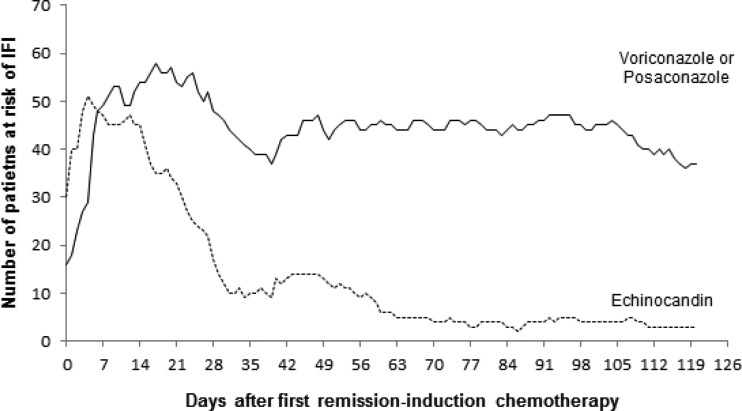
In univariate analysis, patients who initially received primary antifungal prophylaxis with an echinocandin versus a mold-active triazole were older (median age of 69 versus 66, P = 0.027) and less likely to be treated with standard cytarabine-based RIC protocols (61% versus 86%, P = 0.01) and achieved lower overall remission rates during RIC (42% versus 69%, P = 0.015) (Table 2). Patients who received only echinocandin prophylaxis generally experienced a shorter duration of neutropenia (median of 28 versus 46 days, P = 0.04) and received prophylaxis for a shorter period (19 versus 86 days, P < 0.001) (Fig. 1) before switching to another agent or drug discontinuation. The total number of prophylaxis days (with or without receiving fluconazole during any prophylaxis period) was 1,650 days in the echinocandin group (ratio of 43 days per patient) versus 3,164 days in the anti-Aspergillus azole group (ratio of 75 days per patient). The majority (84/152, 55%) of patients who received voriconazole prophylaxis in our study received the oral formulation, representing 98% of voriconazole prophylaxis days (4,193/4,266 days). The frequencies of overlapping periods of fluconazole were comparable in patients receiving echinocandin versus voriconazole/posaconazole prophylaxis (50% versus 31%, respectively, P = 0.11), and the durations of fluconazole prophylaxis for the two groups were similar. The median time to initiate anti-Aspergillus drug class after first remission-induction chemotherapy was 2 days less in the echinocandin group than in the voriconazole/posaconazole group (medians of 1 and 3 days; P = 0.04).
TABLE 2.
Clinical and treatment-associated risk factors for IFI and mortality among AML patients who received voriconazole/posaconazole versus echinocandin primary antifungal prophylaxis
| Demographic or clinical characteristicp | Voriconazole/posaconazole (n = 42) | Echinocandin (n = 38) | P |
|---|---|---|---|
| Male, n (%) | 26 (62) | 23 (61) | 0.9 |
| Median age (IQR), yrs | 66 (38–71) | 69 (61–77) | 0.03 |
| Race, white, n (%) | 33 (79) | 30 (79) | 0.97 |
| Admission to the HEPA filter room during FRIC, n (%) | 10 (24) | 16 (42) | 0.10 |
| Underlying conditions,a n (%) | |||
| Lung disease or infectionb | 11 (26) | 7 (18) | 0.41 |
| Bacterial infectionc | 9 (21) | 3 (8) | 0.12 |
| Cardiovascular disease or condition | 15 (36) | 11 (29) | 0.52 |
| Diabetes mellitus or induced hyperglycemiad | 6 (14) | 7 (18) | 0.62 |
| Renal failuree | 7 (17) | 7 (18) | 0.84 |
| Abnormal liver testf | 5 (12) | 4 (11) | >0.99 |
| Other malignancyg | 6 (14) | 8 (21) | 0.43 |
| Chemotherapy naïve | 38 (90) | 35 (92) | >0.99 |
| WHO AML classifications,h n (%) | |||
| Therapy-related AML | 1/41 (2) | 3/38 (5) | 0.61 |
| MDS-related changes | 15/41 (37) | 13/38 (34) | 0.83 |
| Recurrent genetic abnormalities | 12/41 (29) | 8/38 (21) | 0.4 |
| Myeloid sarcoma | 1/41 (2) | 1/38 (3) | >0.99 |
| Acute leukemia of ambiguous lineage | 0/41 (0) | 1/38 (3) | 0.48 |
| Not otherwise specified | 13/41 (32) | 14/38 (37) | 0.63 |
| Cytogenetic risk group,i n (%) | |||
| Favorable | 12 (29) | 6 (16) | 0.17 |
| Intermediate I | 4 (10) | 2 (5) | 0.68 |
| Intermediate II | 16 (38) | 16 (42) | 0.71 |
| Adverse | 10 (24) | 14 (37) | 0.20 |
| FRIC protocol, n (%) | |||
| Cytarabine-containing regimen | 36 (86) | 23 (61) | 0.01 |
| Other regimen | 6 (14) | 15 (39) | |
| Investigational chemotherapyj | 14 (33) | 21 (55) | 0.07 |
| Clofarabine-containing protocolk | 10 (24) | 10 (26) | 0.80 |
| Overall remission,l n (%) | 29 (69) | 16 (42) | 0.02 |
| Neutropenia (ANC ≤ 500 cells/mm3) | |||
| At start of PAP drug, n (%) | 21 (50) | 16 (42) | 0.48 |
| Median no. of episodes (IQR) | 3 (1–4) | 2 (1–3) | 0.33 |
| Median duration (IQR),m days | 46 (26–61) | 28 (16–45) | 0.04 |
| Primary antifungal prophylaxis | |||
| Median no. of days to start PAP after FRIC, (IQR) | 3 (0–5) | 1 (0–4) | 0.04 |
| Median duration of prophylaxis (IQR),n days | 86 (45–106) | 19 (10–88) | <0.001 |
| Prophylaxis periods ≥ 5 days,n n (%) | 42 (100) | 35 (92) | 0.10 |
| Concomitant fluconazole use, n (%) | 13 (31) | 19 (50) | 0.11 |
| Median duration of fluconazole use (days),o IQR | 11 (5–31) | 21 (3–89) | 0.59 |
At-hospital admission or history.
Lung infection at hospital admission or concomitant to AML history.
At-hospital admission or concomitant to AML history according to patient's treating physician based on clinical, microbiology, and antibiotic prescription data.
Diagnosis of diabetes mellitus or induced hyperglycemia (glucose ≥ 200 mg/dl).
Diagnosis of renal failure or a 50% increase in serum creatinine level.
Diagnosis of liver disease or abnormal liver blood tests (serum alanine aminotransferase and/or aspartate aminotransferase levels > 3.0 × upper limit of normality [ULN] and/or total bilirubin > 1.5 × ULN).
Solid cancers in breast (9 patients), skin (7), prostate (4), parotid (2), thyroid (1), vocal cord (1) and cervix uteri (1); chronic myelomonocytic leukemia (2); acute lymphoblastic leukemia (1); Hodgkin's lymphoma (1); not specified (3 patients).
Data are from Vardiman et al. (20).
Data are from Estey (21).
Eleven investigational chemotherapy protocols.
Three investigational clofarabine-containing protocols in FRIC (see footnote to Table 1).
Overall remission as described by Faderl et al. (9).
Considering all episodes of neutropenia.
Prophylaxis period, prophylaxis with same drug and formulation without discontinuation.
Duration per prophylaxis period.
AML, acute myeloid leukemia; ANC, absolute neutrophil count; FRIC, first remission-induction chemotherapy; HEPA, high-efficiency particulate air; MDS, myelodysplastic syndrome; PAP, primary antifungal prophylaxis; WHO, World Health Organization.
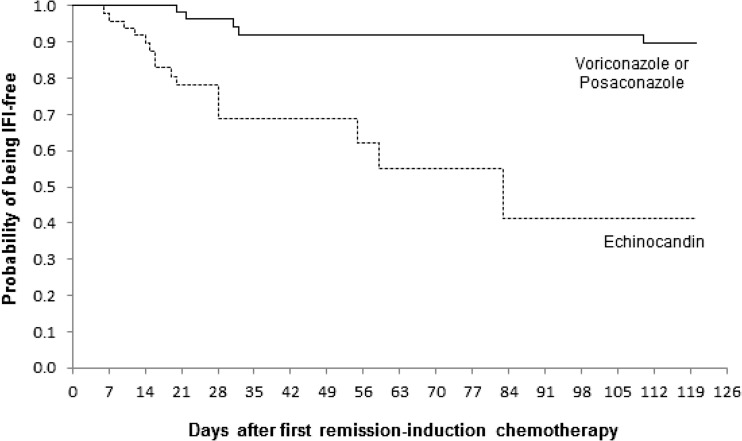
FIG 1.
Kaplan-Meier estimates of being documented IFI-free during the 120 days after first remission-induction chemotherapy. Patients were stratified on the basis of the current prophylaxis agent, which was analyzed as a time-dependent covariate. No P value was calculated because 45 patients had changes in their antifungal prophylaxis during the analysis period.
The frequency of documented IFI, in particular, invasive candidiasis, was higher among patients who received only echinocandin versus anti-Aspergillus azole-based prophylaxis (8% versus 0%, P = 0.09). To compare rates of IFI among patients, including those who switched antifungal prophylaxis during the study period (n = 45 patients), we constructed Kaplan-Meier curves for the probability of being free of IFI stratified by antifungal prophylaxis as a time-dependent covariate (Fig. 2). Marked differences in the probability of being IFI free were evident between patients who received primary antifungal prophylaxis with voriconazole or posaconazole and patients who received an echinocandin, even though the rates of empirical antifungal therapy use by the two prophylaxis groups were similar (32% versus 40%, P = 0.41). All-cause mortality rates did not differ between the echinocandin and anti-Aspergillus triazole prophylaxis patients (13% and 10% P = 0.73).
FIG 2.
Numbers of patients at risk of IFI during the 120 days after first remission-induction chemotherapy. Patients were stratified on the basis of the current prophylaxis agent, which was treated as a time-dependent covariate.
DISCUSSION
In a previous epidemiological analysis of IFIs in the AML population, we found significantly higher IFI rates during remission-induction chemotherapy (RIC) among patients who received prophylaxis with an echinocandin than among those who received mold-active triazoles (voriconazole or posaconazole) (7.1 versus 1.1 per 1,000 prophylaxis days, P < 0.0001) (3). Given the relatively limited evidence supporting front-line use of echinocandins for primary prophylaxis in AML, we suspected that echinocandin prophylaxis might have been used predominantly in older or higher-risk AML patients (i.e., those with chemotherapy-associated AML) who had multiple comorbidities that prevented use of a triazole. Alternatively, echinocandin prophylaxis may have been used more frequently for patients whose drug interactions or risk for increased hepatic toxicity with investigational chemotherapy was a concern (3), which precluded the use of voriconazole or posaconazole. Because many of these variables could be associated with increased IFI risk, it is important to ascertain whether echinocandin prophylaxis is an independent risk factor, per se, for breakthrough IFI in AML patients undergoing RIC.
Our analysis revealed clofarabine-containing chemotherapy regimen and echinocandin prophylaxis to be two independent risk factors for developing documented IFI during the first 120 days of RIC. Clofarabine is a broad-spectrum purine nucleoside analog considered to be an effective agent for older patients with AML who are unsuitable for anthracycline-based regimens or who have unfavorable risk factors/cytogenetics, which are common in therapy-associated AML (9–11). Clofarabine is associated with significant myelosuppression and gastrointestinal toxicity compared to lower-dose cytarabine regimens used in older AML patients, which may account for the higher rate of breakthrough IFI (9, 11–14). Therefore, it is not surprising that clofarabine RIC was retained as an independent risk factor for breakthrough IFI. Nevertheless, clofarabine-based RIC was used in similar proportions of AML patients who received echinocandin versus voriconazole or posaconazole prophylaxis (26% versus 24%, P = 0.80). Similarly, other IFI risk factors identified in univariate analysis associated with IFI (AML classification, cytogenetics, prior chemotherapy exposure, failed response to RIC) and neutropenia frequency, depth, and duration did not favor patients who received voriconazole or posaconazole prophylaxis (Table 2). Hence, we believe that our analysis points to the hypothesis that echinocandin antifungals are less effective prophylactic agents than triazole antifungals for preventing IFI in AML patients receiving RIC.
Although the number of infections available for analysis was limited, differences in the pattern of breakthrough IFIs also suggest that the echinocandins may be less effective as PAP, in agreement with our previous findings where the incidence density rates of both mold and yeast IFIs per prophylaxis day were significantly in favor of azoles (3). Compared to patients receiving posaconazole/voriconazole prophylaxis, patients receiving echinocandins had slightly higher numbers of proven (culture-based) cases of mold infections. Yet the largest difference appeared to be in the rates of breakthrough yeast infections, specifically, yeasts that have intrinsic resistance or a propensity for breakthrough infections during echinocandin therapy (i.e., Candida glabrata, C. parapsilosis, Saprochaete capitata [Blastoschizomyces capitatus]), which may have been prevented with triazole prophylaxis. Besides the differences in spectra of activity, pharmacokinetic limitations of echinocandins versus broad-spectrum triazoles may also play a role in the higher IFI rate (15–18).
Our data set has several limitations, including its retrospective nature and relatively small sample size that was composed of primarily higher-risk, older AML patients from a single large cancer treatment center. Moreover, we were not able to capture data concerning why particular primary antifungal prophylaxis regimens were selected, discontinued, or changed by the treating hematologists. As such, we had to retrospectively designate a duration of therapy that could be considered prophylaxis (at least 3 days before switching) in our analysis. To overcome problems with switching therapies, we also analyzed rates of breakthrough IFI modeling prophylaxis as a time-dependent variable (Fig. 2). As highlighted in our previous study (3), IFI rates are probably underestimated because diagnosis relies heavily on positive results in galactomannan tests, which have reduced sensitivity in patients receiving antifungal prophylaxis (19). Finally, we analyzed all breakthrough IFIs as a single outcome, even though the pathogenesis and risk factors for invasive molds versus yeast bloodstream infections differ.
In conclusion, we found that antifungal prophylaxis is not uniformly effective in preventing IFI during RIC of AML, especially among members of a cohort of older, higher-risk patients. We also found that the class of prophylactic agent received significantly influences the patient's risk and the type of breakthrough IFI. Overall, use of echinocandin prophylaxis during RIC was associated with a significantly higher risk of breakthrough IFI compared to use of mold-active triazoles, especially with yeast. This excess risk could not be easily explained by underlying hematological disease status, severity of immunosuppression, or chemotherapy-associated risk factors. Nevertheless, larger multicentric prospective studies or well-designed AML patient registry databases of antifungal prophylaxis would be required to confirm our findings of reduced efficacy of echinocandins as primary antifungal prophylaxis during RIC for AML.
Supplementary Material
ACKNOWLEDGMENTS
We thank Paula Molinari Farias for participating in the pilot study and Cai Wu for providing pharmacy data. D.P.K. acknowledges the Frances King Black Endowment for Cancer Center.
The study was supported in part by an educational grant of Pfizer Inc. to D.P.K. D.P.K. has received research support and honoraria from Pfizer, Astellas Pharma US, and Merck and Co., Inc., and serves on the advisory board for Merck & Co., Inc.; R.E.L. has received research support from Merck & Co., Inc., and serves on the advisory boards for Merck & Co., Inc., and Gilead Inc. The other authors declare that we have no conflicts of interest.
Footnotes
Published ahead of print 3 March 2014
Supplemental material for this article may be found at http://dx.doi.org/10.1128/AAC.01527-13.
REFERENCES
- 1.Ananda-Rajah MR, Grigg A, Downey MT, Bajel A, Spelman T, Cheng A, Thursky KT, Vincent J, Slavin MA. 2012. Comparative clinical effectiveness of prophylactic voriconazole/posaconazole to fluconazole/itraconazole in patients with acute myeloid leukemia/myelodysplastic syndrome undergoing cytotoxic chemotherapy over a 12-year period. Haematologica 97:459–463. 10.3324/haematol.2011.051995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Auberger J, Lass-Florl C, Aigner M, Clausen J, Gastl G, Nachbaur D. 2012. Invasive fungal breakthrough infections, fungal colonization and emergence of resistant strains in high-risk patients receiving antifungal prophylaxis with posaconazole: real-life data from a single-centre institutional retrospective observational study. J. Antimicrob. Chemother. 67:2268–2273. 10.1093/jac/dks189 [DOI] [PubMed] [Google Scholar]
- 3.Gomes MZ, Mulanovich VE, Jiang Y, Lewis RE, Kontoyiannis DP. 25 November 2013. Incidence density of invasive fungal infections during primary antifungal prophylaxis in newly diagnosed acute myeloid leukemia patients in a tertiary cancer center, 2009 to 2011. Antimicrob. Agents Chemother. 10.1128/AAC.01525-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rogers TR, Slavin MA, Donnelly JP. 2011. Antifungal prophylaxis during treatment for haematological malignancies: are we there yet? Br. J. Haematol. 153:681–697. 10.1111/j.1365-2141.2011.08650.x [DOI] [PubMed] [Google Scholar]
- 5.Kontoyiannis DP. 2012. Invasive mycoses: strategies for effective management. Am. J. Med. 125:S25–S38. 10.1016/j.amjmed.2011.10.009 [DOI] [PubMed] [Google Scholar]
- 6.Cornely OA, Bohme A, Buchheidt D, Einsele H, Heinz WJ, Karthaus M, Krause SW, Kruger W, Maschmeyer G, Penack O, Ritter J, Ruhnke M, Sandherr M, Sieniawski M, Vehreschild JJ, Wolf HH, Ullmann AJ. 2009. Primary prophylaxis of invasive fungal infections in patients with hematologic malignancies. Recommendations of the Infectious Diseases Working Party of the German Society for Haematology and Oncology. Haematologica 94:113–122. 10.3324/haematol.11665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mattiuzzi GN, Cortes J, Alvarado G, Verstovsek S, Koller C, Pierce S, Blamble D, Faderl S, Xiao L, Hernandez M, Kantarjian H. 2011. Efficacy and safety of intravenous voriconazole and intravenous itraconazole for antifungal prophylaxis in patients with acute myelogenous leukemia or high-risk myelodysplastic syndrome. Support. Care Cancer 19:19–26. 10.1007/s00520-009-0783-3 [DOI] [PubMed] [Google Scholar]
- 8.De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA, Denning DW, Patterson TF, Maschmeyer G, Bille J, Dismukes WE, Herbrecht R, Hope WW, Kibbler CC, Kullberg BJ, Marr KA, Munoz P, Odds FC, Perfect JR, Restrepo A, Ruhnke M, Segal BH, Sobel JD, Sorrell TC, Viscoli C, Wingard JR, Zaoutis T, Bennett JE, European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group ; National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. 2008. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin. Infect. Dis. 46:1813–1821. 10.1086/588660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faderl S, Wetzler M, Rizzieri D, Schiller G, Jagasia M, Stuart R, Ganguly S, Avigan D, Craig M, Collins R, Maris M, Kovacsovics T, Goldberg S, Seiter K, Hari P, Greiner J, Vey N, Recher C, Ravandi F, Wang ES, Vasconcelles M, Huebner D, Kantarjian HM. 2012. Clofarabine plus cytarabine compared with cytarabine alone in older patients with relapsed or refractory acute myelogenous leukemia: results from the CLASSIC I trial. J. Clin. Oncol. 30:2492–2499. 10.1200/JCO.2011.37.9743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Faderl S, Verstovsek S, Cortes J, Ravandi F, Beran M, Garcia-Manero G, Ferrajoli A, Estrov Z, O'Brien S, Koller C, Giles FJ, Wierda W, Kwari M, Kantarjian HM. 2006. Clofarabine and cytarabine combination as induction therapy for acute myeloid leukemia (AML) in patients 50 years of age or older. Blood 108:45–51. 10.1182/blood-2005-08-3294 [DOI] [PubMed] [Google Scholar]
- 11.Faderl S, Ravandi F, Huang X, Wang X, Jabbour E, Garcia-Manero G, Kadia T, Ferrajoli A, Konopleva M, Borthakur G, Burger J, Feliu J, Kantarjian HM. 2012. Clofarabine plus low-dose cytarabine followed by clofarabine plus low-dose cytarabine alternating with decitabine in acute myeloid leukemia frontline therapy for older patients. Cancer 118:4471–4477. 10.1002/cncr.27429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tran H, Yang D. 2012. Clofarabine in the treatment of newly diagnosed acute myeloid leukemia in older adults. Ann. Pharmacother. 46:89–96. 10.1345/aph.1Q295 [DOI] [PubMed] [Google Scholar]
- 13.Tiley S, Claxton D. 2013. Clofarabine in the treatment of acute myeloid leukemia in older adults. Ther. Adv. Hematol. 4:5–13. 10.1177/2040620712461666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.UK Medicines and Healthcare Products Regulatory Agency (MHRA). 2011. (updated 12 March 2013) Summary of product characteristics (Evoltra 1mg/ml concentrate for solution for infusion). http://www.medicines.org.uk/EMC/medicine/18023/SPC/Evoltra+1mg+ml+concentrate+for+solution+for+infusion/ Accessed 17 November 2013
- 15.Lewis RE. 2012. Importance of pharmacokinetic considerations for selecting therapy in the treatment of invasive fungal infections. Am. J. Ther. 19:51–63. 10.1097/MJT.0b013e3181ff7e10 [DOI] [PubMed] [Google Scholar]
- 16.Lewis RE. 2011. Current concepts in antifungal pharmacology. Mayo Clin. Proc. 86:805–817. 10.4065/mcp.2011.0247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Denning DW. 2003. Echinocandin antifungal drugs. Lancet 362:1142–1151. 10.1016/S0140-6736(03)14472-8 [DOI] [PubMed] [Google Scholar]
- 18.Stone JA, Holland SD, Wickersham PJ, Sterrett A, Schwartz M, Bonfiglio C, Hesney M, Winchell GA, Deutsch PJ, Greenberg H, Hunt TL, Waldman SA. 2002. Single- and multiple-dose pharmacokinetics of caspofungin in healthy men. Antimicrob. Agents Chemother. 46:739–745. 10.1128/AAC.46.3.739-745.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marr KA, Laverdiere M, Gugel A, Leisenring W. 2005. Antifungal therapy decreases sensitivity of the Aspergillus galactomannan enzyme immunoassay. Clin. Infect. Dis. 40:1762–1769. 10.1086/429921 [DOI] [PubMed] [Google Scholar]
- 20.Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, Harris NL, Le Beau MM, Hellstrom-Lindberg E, Tefferi A, Bloomfield CD. 2009. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 114:937–951. 10.1182/blood-2009-03-209262 [DOI] [PubMed] [Google Scholar]
- 21.Estey EH. 2012. Acute myeloid leukemia: 2012 update on diagnosis, risk stratification, and management. Am. J. Hematol. 87:89–99. 10.1002/ajh.22246 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.