Abstract
We characterized an anti-cancer fusion protein consisting of anthrax lethal factor (LF) and the catalytic domain of Pseudomonas exotoxin A by (i) mutating the N-terminal amino acids and by (ii) reductive methylation to dimethylate all lysines. Dimethylation of lysines was achieved quantitatively and specifically without affecting binding of the fusion protein to PA or decreasing the enzymatic activity of the catalytic moiety. Ubiquitination in vitro was drastically decreased for both the N-terminally mutated and dimethylated variants, and both appeared to be slightly more stable in the cytosol of treated cells. The dimethylated variant showed greatly reduced neutralization by antibodies to LF. The two described modifications offer unique advantages such as increased cytotoxic activity and diminished antibody recognition, and thus may be applicable to other therapeutic proteins that act in the cytosol of cells.
Recent years have seen increased effort directed toward development of protein-based anti-tumor drugs. Thus, several antibodies have been approved by the FDA in the last decade for the treatment of various cancers. A related and potentially more powerful approach making use of the high specificity binding of antibodies to tumor markers is the development of “immunotoxins”, fusions of tumor-specific antibodies (or fragments thereof) to bacterial or plant toxins1.
In this laboratory, efforts have emphasized an alternative approach to achieving tumor cell specificity by using modified anthrax toxin. Anthrax toxin depends on proteolytic activation of the receptor-bound protective antigen protein (PA) by cell surface proteases2. Replacing the furin-cleaved sequence with sequences recognized by matrix metalloproteases or urokinase plasminogen activator has yielded tumor-specific anti-cancer fusion proteins that are efficacious in mouse tumor models3. Both the wildtype and the modified PA assemble into an oligomeric protein-conducting channel that delivers the anthrax toxin catalytic effector proteins lethal factor (LF) and edema factor to endosomes and then translocates them to the cytosol. For targeting of tumors, the native anthrax effector protein LF was replaced with a fusion containing the N-terminal PA-binding 254 amino acid-containing domain of anthrax toxin lethal factor (LFn) and the Pseudomonas aeruginosa exotoxin A (PE) catalytic domain (PEIII) to obtain the fusion protein FP594. The LFn domain delivers PEIII to the cytosol and PEIII transfers ADP-ribose to eukaryotic elongation factor 2 (eEF2), resulting in protein synthesis inhibition and cell death. This system is highly effective in achieving tumor-specific cell-surface PA activation and cytosolic delivery of PEIII. It has been successfully tested for a number of tumor types5, and is expected to be active on nearly all types of solid tumors.
The cytosolic activity of these effector molecules greatly depends on their efficacy in avoiding cytosolic degradation, e.g. by the proteasome. Proteins targeted for degradation are labeled by ubiquitin and directed to the 26S proteasome6. Certain factors influence the half-life of proteins in the cytosol and Alexander Varshavsky identified the N-terminal amino acid of certain proteins to be highly relevant for their cytosolic stability7. This N-end rule identified certain amino acids at the N-terminus to be stabilizing residues (e.g. Met, Gly, or Ala) while other residues clearly result in faster degradation of proteins (e.g. Arg, Lys, or Asp)8. We were able to identify certain stabilizing N-terminal amino acids for LF that result in increased stability of the protein in the cytosol and in increased cytotoxicity both in cells and in an animal model9. Thus the N-end rule should impact the efficacy of anthrax toxin-based anti-tumor agents.
Reductive methylation is an efficient chemical reaction which converts a primary amine into a tertiary dimethyl amine. Reductive methylation is a two-step process. First, reaction of protein amino groups with formaldehyde results in reversible formation of Schiff base (imine) adducts between the aldehyde and the protein amino groups. Second, the modification is made stable by a reducing agent (usually a borane compound such as a borane dimethyl amine complex), which converts the imine to a carbon-nitrogen single bond. The resulting mono-methylated protein amino group undergoes a second round of the same reaction to give the dimethylated form10. The dimethylated amine is protonated at neutral pH, like the original lysine side chain primary amine, but it cannot act as a nucleophile to form covalent bonds. Thus, reductively methylated proteins are not subject to ubiquitination pathways.
In this study, we examined modifications of the therapeutic fusion protein FP59 that were predicted to improve its potency on target cells. We mutated the N-terminus of LFn according to results obtained in earlier studies and reductively methylated all lysines. The results obtained indicate that both modifications improve the stability by preventing ubiquitination and subsequent proteasomal degradation.
Results
Construction of FP59-AGG and reductive methylation
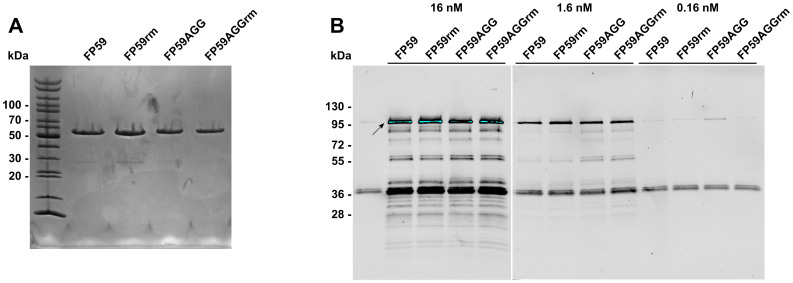
In our recent studies, LF and EF were found to have higher cytotoxic activity on cultured cells and in animals when the N-terminal amino acid was alanine as opposed to certain other amino acids9,11, consistent with the view that these proteins are subject to the N-end rule pathway of protein degradation. FP59 has two additional amino acids (His and Met) at the N-terminus of the LFn domain that resulted from cloning manipulations. In the present study, we constructed the FP59 variant FP59AGG lacking the His and Met residues of FP59 and thereby having the original N-terminal sequence of native LF. Both proteins were successfully expressed and purified. In order to further improve cytosolic stability, both proteins were reductively methylated. This post-translational chemical modification results in dimethylation of all accessible lysine residues of a protein and prevents the ubiquitination of the proteins. The purified proteins FP59 and FP59AGG, as well as the reductively modified variants FP59rm and FP59AGGrm, were available at high purity for further studies (Figure 1A).
Figure 1. Analysis of FP59 fusion protein variants.
(A) Purified fusion proteins FP59 and FP59AGG were reductively methylated and analyzed by SDS-PAGE and Coomassie staining. This experiment was performed once to confirm the determined concentration of the proteins and to demonstrate purity of the samples. (B) All four FP59 variants were analyzed for the enzymatic activity of the PEIII domain by analysis of the ADP-ribosylation in vitro. Fusion proteins were incubated with partly purified eukaryotic elongation factor 2 from yeast in the presence of biotinylated NAD+ for 1 h at 37°C. Samples were analyzed by Western blotting and ADP-ribosylated eEF2 detected by streptavidin. This experiment was performed twice and one exemplary result is shown here.
Of the 35 lysine present in FP59, only 3 are located in the PEIII domain, suggesting that reductive methylation was unlikely to modify its catalytic activity. We examined this question by measuring ADP-ribosylation activity using partly purified eEF2 and biotinylated NAD+ (Figure 1B). Enzymatically active PEIII modifies eEF2 by covalent attachment of biotinylated ADP-ribose, which can be detected by dye-labeled streptavidin. Full length biotinylated eEF2 (100 kDa, arrow) was detected in reactions catalyzed by all four FP59 variants, and all variants had very similar enzymatic activity. The gel also showed a prominent band at around 35 kDa, which is a known cleavage product of eEF2 that is also a substrate for ADP-ribosylation. These results show that neither the removal of the His-Met N-terminus nor the reductive methylation reduced PEIII enzymatic activity.
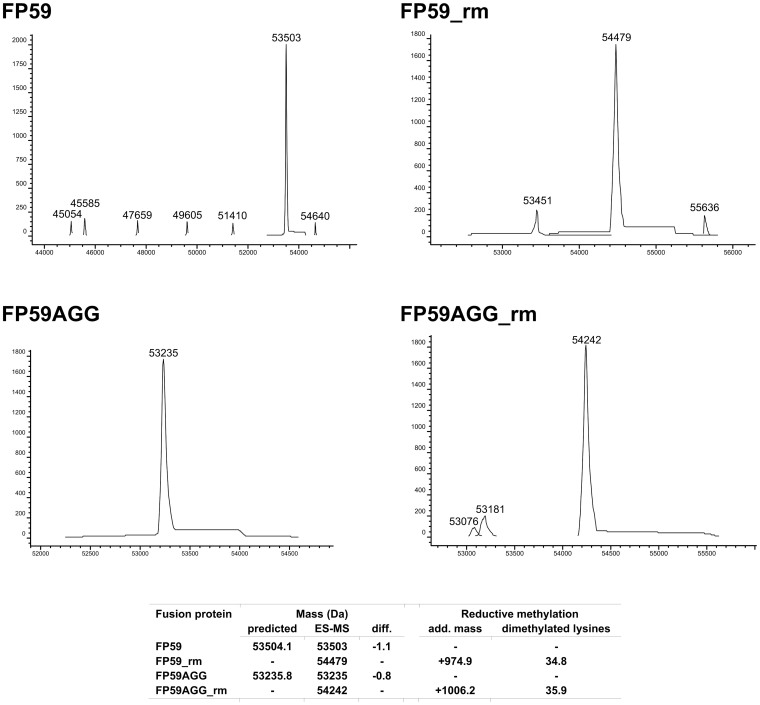
Confirmation of reductive methylation of FP59 proteins
The reductively methylated proteins were analyzed by electrospray ionization mass spectrometry to confirm the correct molecular masses for FP59 and FP59AGG as well as to determine the exact masses of the methylated variants and the corresponding number of dimethylated lysines. The results indicated that essentially all 35 lysine residues in both FP59 and FP59AGG were fully dimethylated (Figure 2). The primary alpha-amine at the N-terminus of proteins is also subject to reductive methylation, so there are predicted to be 36 added dimethyl amine groups, which would add 1008 Da, very close to what was observed. The prominent peak in each analysis demonstrated the high degree of homogeneity of the modified proteins and the purity of the samples. Thus, the reductive methylation reaction successfully modifies all lysine residues without side reactions at other amino acids.
Figure 2. Mass spectrometry analyses of FP59 variants.
Electron spray ionization mass spectrometry analysis of FP59, FP59rm, FP59AGG, and FP59AGGrm. The graphs show the results of the deconvolution of the data obtained for each fusion proteins with the respective masses. The table summarizes the results and shows the predicted masses, differences to the observed results, additional masses for the dimethylated fusion proteins and the resulting number of dimethylated lysines.
Binding kinetics for FP59 variants
All FP59 variants were analyzed by SPR for binding to proteolytically activated PA, which is an essential step in their internalization to the cytosol. Purified PA63 was immobilized on the SPR chip surface and the binding of the FP59 variants was measured. The analysis revealed similar binding kinetics for both FP59 and FP59AGG as well as the dimethylated variants (Table 1). The KD for FP59rm is approximately 2-fold lower than of the three other FP59 variants. However, this variation is within the expected range of results and therefore not considered significant.
Table 1. Binding kinetics of the FP59 variants. Results were obtained from surface plasmon resonance analyses (n = 8 trials). Errors are the S.E.M.
| Protein | ka (×106 M−1s−1) | kd (×10−3 s−1) | KD (pM) |
|---|---|---|---|
| FP59 | 5.9 ± 0.9 | 1.0 ± 0.2 | 170 ± 50 |
| FP59rm | 10 ± 10 | 0.63 ± 0.07 | 62 ± 4 |
| FP59AGG | 8 ± 1 | 1.2 ± 0.2 | 150 ± 20 |
| FP59AGGrm | 9 ± 1 | 1.1 ± 0.2 | 120 ± 10 |
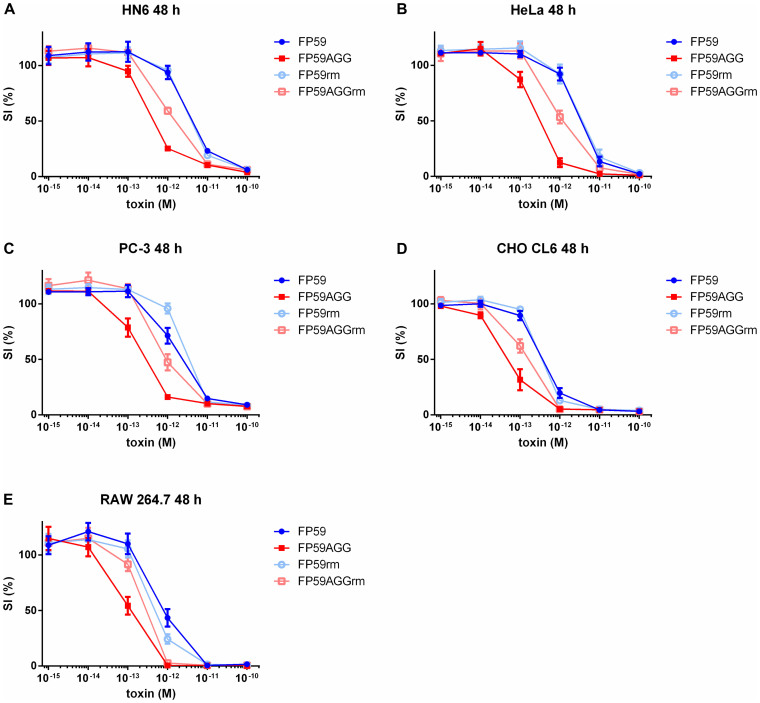
Cytotoxic activity of FP59 variants
Cytotoxicity assays were performed on human cancer cell lines (HN6, HeLa, and PC-3 cells) and murine RAW264.7 macrophages, as well as Chinese hamster CHO CL6 cells (Figure 3). All variants were highly cytotoxic in combination with PA, with SI50 values in the low pM range, with FP59AGG being the most cytotoxic variant on all tested cell lines (Table 2). The SI50 values for FP59 and FP59rm were not significantly different except on PC-3 cells. FP59AGGrm was slightly less cytotoxic than FP59AGG (between 2.3- and 4.2-fold). FP59AGG was much more cytotoxic than FP59 on every cell line (6.7–10.6-fold decreased SI50 values).
Figure 3. Cytotoxicity of FP59 variants on several cell lines.
(A) Human head and neck squamous cell carcinoma cell line HN6, (B) human cervical carcinoma cell line HeLa, (C) human prostate adenocarcinoma cell line PC-3, (D) Chinese hamster ovary cell line CHO CL6 and (E) murine leukemic monocyte/macrophage RAW 264.7 cells were exposed to a fixed concentration of PA (250 ng/mL) and different concentrations of the FP59 fusion proteins for 48 h and viable cells were quantitated in an MTT assay. Relative survival (SI) was calculated as the percentage of living cells after treatment in relation to untreated cells. Error bars indicate S.E.M. of three independent experiments performed in triplicate.
Table 2. SI50 values of the FP59 variants. Results were obtained from cytotoxicity assays (n = three independent experiments in triplicates). Errors are the S.E.M.
| SI50 (10−13 M) | |||||
|---|---|---|---|---|---|
| Protein | CHO CL6 | HN6 | RAW | PC-3 | HeLa |
| FP59 | 4.0 ± 0.6 | 47.5 ± 5.5 | 10.0 ± 2.9 | 25.4 ± 5.5 | 36.1 ± 5.9 |
| FP59rm | 3.8 ± 0.2 | 44.5 ± 3.3 | 5.6 ± 1.3 | 38.9 ± 3.6 | 43.6 ± 13.9 |
| FP59AGG | 0.6 ± 0.2* | 5.2 ± 0.5* | 1.3 ± 0.4* | 3.2 ± 0.7* | 3.4 ± 0.7 |
| FP59AGGrm | 1.5 ± 0.2 | 16.7 ± 1.3 | 3.0 ± 0.4 | 12.2 ± 2.7 | 14.4 ± 3.3 |
*p values < 0.05 in comparison to FP59 (for FP59rm and for FP59AGG) or FP59AGG (for FP59AGGrm) calculated by one-way ANOVA and Tukey's multiple comparison test.
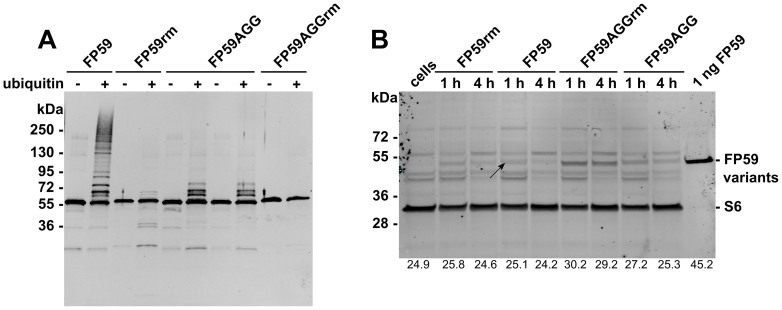
Ubiquitination of various FP59 proteins
We studied in vitro ubiquitination of the four FP59 variants in order to predict their susceptibility to ubiquitination and degradation after delivery to the cytosol. The FP59 variants were incubated in vitro with ubiquitination reagents and the extent of ubiquitination detected by immunodetection (Fig. 4A). FP59 showed many bands of high molecular mass of more than 90 kDa after ubiquitination, indicating extensive ubiquitination. Reductive methylation of FP59 nearly completely prevented ubiquitination of FP59. The N-terminal mutation of FP59AGG greatly inhibited ubiquitination of the fusion protein, with only three bands of increased molecular mass being detected after treatment. Reductive methylation of FP59AGG completely prevented any ubiquitination. The increases in molecular mass of approximately 1 kDa (35 lysines × 28 Da = 980 Da, Fig. 2) as determined by mass spectrometry for both FP59rm and FP59AGGrm upon dimethylation of all lysine residues was consistent with the slight decrease in electrophoretic mobility in comparison to the non-modified variants FP59 and FP59AGG (Fig. 4A).
Figure 4. Ubiquitination and cytosolic detection of fusion proteins in CHO CL6 cells.
(A) Ubiquitination of FP59 variants was performed in vitro for all FP59 variants. The reaction mixtures (labeled “+” if containing ubiquitin and labeled “−” if lacking ubiquitin) were preincubated with deubiquitinating enzyme inhibitor ubiquitin aldehyde and for an additional 1 h after addition of fusion proteins. Ubiquitination was analyzed after SDS-PAGE, Western blotting and immunodetection by anti-LF. This experiment was performed twice and one exemplary result is shown here. (B) The fusion proteins FP59rm, FP59, FP59AGGrm, and FP59AGG (2 μg/mL) were incubated in the presence of 1 μg/mL PA on CHO CL6 cells for 1 h and 4 h. Cytosolic fractions were isolated and analyzed by anti-LF and anti-S6 immunodetection following Western blotting. Purified FP59 was loaded as a control (1 ng). This experiment was performed six times and one exemplary result is shown here. Signal intensities were quantified and are shown at the bottom of panel (B).
Stability of fusion proteins in the cytosol
Intracellular detection of the fusion proteins was done using CHO CL6 cells, which express the capillary morphogenesis gene 2 anthrax toxin receptor and internalize the fusion proteins efficiently, thereby facilitating their detection in the cytosolic fractions. FP59 was detected in the cytosolic fraction in very low amounts after 1 and 4 h toxin exposure (arrow, Figure 4B). FP59rm and FP59AGG were detected in slightly higher amounts. The reductively methylated variant of FP59, FP59AGGrm, was detected in the highest quantities in the cytosol. All signals were slightly lower after 4 h, suggesting some degradation of the proteins in the cell. The signal intensity of each band was quantified and is shown at the bottom of Figure 4B.
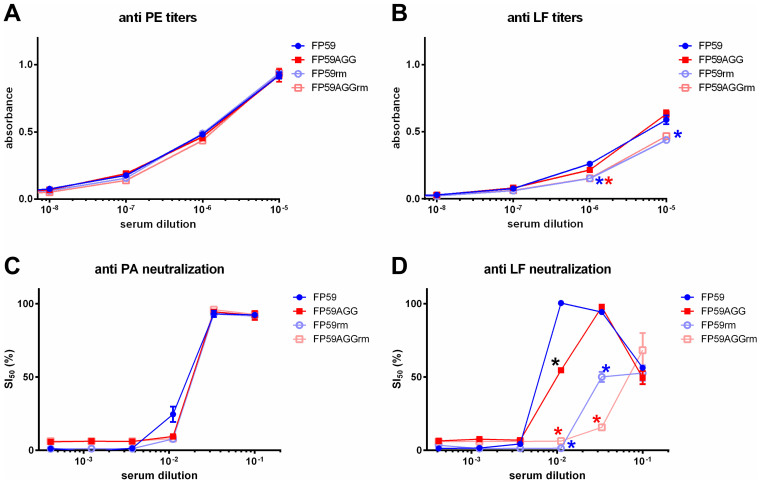
Enzyme-linked immunosorbent and neutralization assays
The dimethylation of lysine residues of FP59 and FP59AGG would be expected to alter any surface epitopes that contained lysine residues. This would be detectable by ELISA and in toxin neutralization assays. The analysis of FP59 variants by ELISA showed no differences in reactivity with polyclonal anti-Pseudomonas exotoxin antibody (Figure 5A). In the case of the detection by the polyclonal anti-LF antibody, lower antibody signals were obtained for FP59rm and FP59AGGrm (Figure 5B). No differences were observed between FP59 and FP59AGG and between FP59rm and FP59AGGrm. Toxin neutralization was determined in a cytotoxicity assay with pre-incubation of the FP59 variants with either a polyclonal anti-PA antiserum or a polyclonal anti-LF antiserum (Figures 5C and 5D). The concentration of the FP59 variants was sufficiently high to guarantee complete killing of the cells (10 ng/mL (190 nM) with very little variation due to the slightly different molecular masses of the proteins). Pre-incubation with anti-PA protected the cells from all FP59 variants similarly at a 30-fold dilution of the antiserum by neutralizing PA present in each sample. Pre-incubation with anti-LF antiserum resulted in drastically reduced neutralization of the two dimethylated variants FP59rm and FP59AGGrm in comparison to the non-modified fusion proteins. Thus, while a 90-fold dilution of the anti-LF antibody protected the cells completely from FP59 and partially from FP59AGG, this concentration of anti-LF had no effect on the dimethylated variants. Higher antibody concentrations (i.e., a 10-fold dilution) reduced cell viability, possibly due to azide added to the anti-LF antiserum as a preservative.
Figure 5. Epitope modification by reductive methylation.
(A and B) The four FP59 variants were analyzed for their susceptibility to antibodies against Pseudomonas exotoxin A (anti-PE, A) and anthrax toxin lethal factor (anti-LF, B) by ELISA. The FP59 variants were coated in 96-well plates (200 ng/well) and detected by various dilutions of anti-PE and anti-LF. (C and D) The four FP59 variants were analyzed for their susceptibility to antibodies against LF and PA. The fusion proteins (10 ng/mL) were incubated with PA (250 ng/mL) in the presence of anti-PA (C) or anti-LF (D) antisera prior to adding to RAW 264.7 macrophages for 24 h at 37°C. Viable cells were quantitated in an MTT assay. Relative survival (SI) was calculated as the percentage of living cells after treatment in relation to untreated cells. Error bars (A–D) indicate S.E.M. of two independent experiments performed in triplicate. Significant differences (p values < 0.05) between FP59 and FP59rm (indicated by a blue asterisk), between FP59AGG and FP59AGGrm (indicated by a red asterisk), and between FP59 and FP59AGG were calculated by one-way ANOVA and Tukey's multiple comparison test (GraphPad Prism 6.01) both for the ELISA results (A and B) and the neutralization assay (C and D).
Discussion
A variety of factors have been considered in efforts to improve the efficacies of therapeutic fusion proteins (reviewed in12). One approach has been to seek to increase the delivery of fusion proteins into the cytosol of target (e.g., tumor) cells13. This is obviously of importance for many anti-cancer fusion proteins that act catalytically to damage cytosolic targets as a way to elicit cell killing. The majority of fusion proteins of this type are derived from bacterial and plant toxins that target protein synthesis14,15. It was noted many years ago that some bacterial proteins that are taken up into host cells to manipulate cellular processes have a very low lysine content, balanced by an increased arginine content, compared to other proteins16. We now recognize that this property probably evolved as a way to evade host-mediated ubiquitination and subsequent degradation. The stability of many proteins in the cytosol follows the N-end rule described by Alexander Varshavsky8, which ascribes the differing susceptibility of proteins to ubiquitination to the identity of the N-terminal residue. Falnes et al. demonstrated in their work that the catalytic domain of diphtheria toxin is less cytotoxic when the N-terminal amino acid is one which, according to the N-end rule, destabilizes the toxin17. A number of other toxins and therapeutic proteins have been shown to be subject to the N-end rule.
The N-end rule applies as well for the anthrax toxin lethal factor9. Since the anti-tumor fusion protein FP59 contains the LFn domain it was anticipated that modifications on its N-terminus would influence the cytosolic stability and subsequently the cytotoxicity. By restoring the wildtype N-terminus of LFn in the variant FP59AGG the cytotoxicity of the fusion protein was significantly increased compared to FP59, which had the additional His-Met sequence at the N-terminus of LFn (Figure 3). Since PA receptors are present on most of the cell types, the combination of PA and FP59 is highly toxic to nearly all cells. Several PA variants have been developed to specifically target tumor cells, which allows the potent toxic activity of FP59 to be highly restricted to tumor cells18,19. Our data regarding the properties of the FP59 variant having the wildtype AGG N-terminus (FP59AGG) will be of value for future application of this therapeutic fusion protein.
Reductive methylation has been used in recent years for several purposes, e.g. enhancing protein crystallization20, radioactive labeling of proteins for improving nuclear magnetic resonance spectroscopy21, and for studies on protein-DNA interactions22. Weng et al. demonstrated reductive alkylation of the protein toxin saporin while preserving the activity of the enzyme23. However, to our knowledge this is the first report on using reductive methylation on therapeutic fusion proteins in order to improve their cytosolic stability and modify their surface epitopes. Our results demonstrate that dimethylation of lysine residues successfully prevented ubiquitination of FP59 and greatly increased its stability and therefore concentration in the cytosol of cells 4 h after toxin internalization. This effect was also seen with FP59AGG, but to a lesser extent. This is apparently because FP59AGG is already substantially protected from ubiquitination due to its native N-terminal amino acid being one known from the N-end rule to be a stabilizing residue. Thus, FP59AGG profits less from reductive methylation in comparison to FP59. Despite the decreased ubiquitination and increased cytosolic stability, no increase in cytotoxicity was observed for FP59rm or FP59AGGrm. While the reductively methylated fusion proteins had no detectable loss in binding to PA or reduced ADP-ribosylation activity, it is possible that the modification causes some decreases in the rate or extent of internalization, and this was balanced by increased cytosolic stability.
The relevance of the N-end rule for the efficacy of anthrax toxin edema factor was recently demonstrated, with differences of up to 100-fold in potency on cells and in animals being attributed to the identity of the N-terminal residue11. FP59 is based on LF and the differences between optimal and destabilizing N-terminal amino acids found in the original study of LF showed only modest differences, up to 5-fold9,. Clearly, the degree to which the N-end rule will affect the potency of other toxins and therapeutic proteins will depend on many factors, such as the presence of lysine residues in surface locations favorable for ubiquitination, the particular E3 ligase involved, etc.
In recent years a number of anti-tumor fusion proteins has been developed that have shown good potential in therapy. However, a major limitation has been the host immune response to these proteins. Several studies have been directed to deletion of predicted or experimentally identified epitopes so as to decrease immunogenicity while retaining anti-tumor activity24,25. Reductive methylation of lysines had no apparent adverse effect on the activity of FP59 and FP59AGG, and thus offers a potential method for modifying cell surface epitopes of therapeutic proteins. The decreased reactivity of the reductively methylated FP59 variants with anti-LF polyclonal antibodies resulted in drastically reduced antibody neutralization by anti-LF antibodies (Figure 5). This result suggests a strategy for modifying the cell surface of fusion proteins to change potential epitopes of the protein. Ideally, sequential useof FP59AGG and FP59AGGrm would allow multiple administrations without neutralization of the second fusion protein by antibodies raised against the first fusion protein. This approach may not be suitable for enzymes that require lysines for their activity or to maintain specific structural features. This is evident from preliminary studies of other enzymes, such as anthrax toxin edema factor, cytolethal distending toxin, saporin, and β-lactamase; these lost most of their activity following reductive methylation (Table S1, Figures S1 and S2).
The fusion proteins studied here are delivered into the cytosol of targeted cells via the highly efficient delivery system of anthrax toxin. The extensively studied protein-conducting channel of PA26,27 efficiently delivers proteins into the cytosol via the PA/LFn system, examples being fusions of LFn to diphtheria toxin catalytic domain28 and to shiga toxin29. Polypeptides must completely unfold to pass through the narrow lumen of the oligomeric PA channel26,30. The fact that both FP59rm and FP59AGGrm were successfully detected in the cytosol demonstrates that the dimethylation of lysines does not interfere with protein translocation by increasing the amino acid side chain size or by changing protein folding properties.
We show here that a cytosolic-acting protein drug, FP59, can be improved by altering its N-terminal amino acid and by reductive methylation of lysines. This method may be applicable to other protein drugs acting in the cytosol of targeted cells, improving their stability and cytotoxicity as well as decreasing their immunogenicity.
Methods
Cloning, protein expression and purification
Plasmid pYS5-FP59, a Bacillus expression vector containing fusion gene FP59 was used to express wildtype and mutated FP59 proteins2. FP59 consists of LFn (N-terminal 254 residues of anthrax toxin lethal factor with the sequence HMAGGHGD…QEINL) and PEIII (C-terminal 216-residue catalytic domain of Pseudomonas exotoxin A with the sequence AEFL…REDLK). The Quick Change-II site directed mutagenesis kit (Stratagene, La Jolla, CA) was used according to the manufacturer's instructions to delete the His-Met codons in the coding sequence of FP59. The obtained sequence of FP59-AGG (N-terminal amino acid sequence of LFn AGGHGD…) was confirmed by sequencing. Proteins PA, a translocation deficient PA variant PAΔFF (PA deleted of Phe314–Phe315) and the FP59 variants were purified from virulence plasmid-cured, non-infectious B. anthracis strain BH450 as described earlier31,32. The 63-kDa fragment of PA (PA63) was purified from furin-treated PA as previously described for other PA variants32. All proteins were analyzed by electrospray ionization mass spectrometry to confirm that the masses matched those calculated from their sequences.
Reductive methylation of proteins
Reductive methylation was performed as described by Rayment et al.10. Borane dimethyl amine complex (DMAB, Sigma, St. Louis, MO) was used as reducing agent in the reductive methylation reaction. The substrate protein, 200 μL of either FP59 or FP59AGG, at 3 mg/mL in 50 mM HEPES, pH 7.5, was supplemented by a final concentration of 20 mM DMAB, mixed thoroughly and immediately a final concentration of 40 mM formaldehyde solution (16%) was added. The mixture was incubated on ice for 2 h. The reductive methylation procedure was repeated a second time (yielding final concentrations of 40 mM DMAB and 80 mM formaldehyde) before addition of a final concentration of 50 mM DMAB and overnight incubation on ice. The reaction was quenched by addition of a final concentration of 160 mM glycine, pH 8.6, and incubated on ice for 1 h. Samples were dialyzed twice (50 mM HEPES, pH 7.2, and then 50 mM HEPES, pH 7.2, 2 mM dithiothreitol). Samples were analyzed by electrospray ionization mass spectrometry to confirm and quantitate the extent of reductive methylation.
Enzyme-linked immunosorbent assay
The FP59 variants were coated (75 μL, 2.67 ng/μL in phosphate-buffered saline (PBS) in 96-well EIA/RIA plates (Corning Incorporated, Corning, NY)) for 2 h, blocked with 5% dry milk powder solution in PBS for 30 min and incubated with 60 μL of various dilutions of either anti-Pseudomonas exotoxin A polyclonal rabbit antibody (Sigma, St. Louis, MO) or anti-LF polyclonal rabbit antibody (raised in this laboratory against full length LF) for 1 h. Secondary horse-radish peroxidase-conjugated anti-rabbit antibody (final concentration 0.2 μg/mL 1:2000, 60 μL in PBS, 1 h, Santa Cruz Biotechnology, Dallas, TX) was added and quantified by a colorimetric reaction using 100 μL of substrate solution (40 mM citric acid, pH 3.95, 0.2 g/L 3,3′5,5′ tetramethylbenzidine, 0.1 g/L H2O2). The reaction was stopped with 50 μL of 2 M H2SO4 after 5 min and the absorbance read at 450 nm and 492 nm as reference.
Enzymatic activity of FP59 variants
The ADP-ribosylation assay to determine enzymatic activity of PEIII was performed with purified yeast eukaryotic elongation factor 2 (eEF2) as described before33. Active PEIII transfers biotinylated ADP-ribose from biotinylated nicotinamide adenine dinucleotide (NAD+) to eEF2. The samples were separated by electrophoresis and biotinylated eEF2 detected by Western blotting with infrared dye 800 nm-coupled streptavidin (final concentration 0.1 μg/mL; LI-COR Biosciences, Lincoln, NE).
Ubiquitination and intracellular detection of fusion proteins
In vitro ubiquitination was performed using the Ubiquitin Protein Conjugation Kit (Calbiochem/Merck, Darmstadt, Germany). Reaction mixtures (3 μL) containing the deubiquitinating enzyme inhibitor ubiquitin aldehyde (Calbiochem/Merck, Darmstadt, Germany) were incubated for 5 min at 37°C before addition of 0.5 μL 100 ng/μL of the FP59 variants. The samples were incubated for 1 h at 37°C in the presence or absence of ubiquitin and submitted to SDS-PAGE, Western blotting and immunodetection (by polyclonal rabbit anti-LF serum and anti-S6 rabbit monoclonal antibody (Cell Signaling, Danvers, MA)) and infrared dye-conjugated secondary antibody (Rockland Immunochemicals, Gilbertsville, PA) on the Odyssey Imager infrared detection system (LI-COR Biosciences, Lincoln, NE). Detection of FP59 variants in cytosolic fractions was performed using CHO CL6 cells (1 × 106 cells overnight in 12-well plates). Cells were incubated with 1 μg/mL PA or PAΔFF (PA deleted of Phe314 and Phe315, a mutant that fails to deliver LF from endosomes to the cytosol31) and 1 μg/mL of the FP59 variants in 0.5 mL medium for 1 or 4 h. Following the incubation, all cells were washed twice with PBS, incubated with trypsin/EDTA at 37°C until all cells could be transferred into new tubes for collection by centrifugation (5 min, 4°C, 1000 × g). For cytosol isolation, cells were resuspended in 125 μg/mL saponin (Sigma, St. Louis, MO) in PBS, supplemented with protease inhibitor cocktail (Roche, Mannheim, Germany) and incubated 10 min on ice34. The supernatants after centrifugation (30 min, 4°C, 16,000 × g) were separated by SDS-PAGE and Western blotted using the iBlot system and the Western Blot Signal Enhancer kit (Thermo, Waltham, MA) for signal enhancement. FP59 variants were detected by polyclonal rabbit anti-LF serum and infrared dye-conjugated secondary antibodies (Rockland Immunochemicals, Gilbertsville, PA) in parallel on the Odyssey Imager infrared detection system (LI-COR Biosciences, Lincoln, NE). Band intensities were achieved by determining the signal intensity of elliptic areas on the membranes by the Odyssey Application Software 2.0.
Binding kinetics for FP59 variants
Studies to assess the binding of the FP59 variants to PA were performed by surface plasmon resonance (SPR) using a ProteOn XPR36 Protein Interaction Array System (Bio-Rad Laboratories, Hercules, CA) after immobilization of PA63 by amine coupling chemistry using the manufacturer's recommended protocol. Briefly, after activation of a high protein immobilization capacity GLH chip surface with a mixture of 0.4 M 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide and 0.1 M N-hydroxysulfosuccinimide injected for 300 s at 30 μL/min, PA63 was immobilized by passing a 50 μg/mL solution of the protein at pH 5 (to achieve positively charged PA) over the surface for 150 s at 25 μL/min. The surface was deactivated with a 30 μL/min injection of 1 M ethanolamine for 200 s. A concentration series for each FP59 variant (between 1.56 and 400 nM) was passed over the surface at 100 μL/min for 60 s, then dissociation was recorded for 600 s. The surface was then regenerated with a 30-s injection of 50 mM HCl at 50 μL/min. Running buffer for these studies was 10 mM HEPES, pH 7.4, 150 mM NaCl, 0.005% Tween-20. Data were evaluated with ProteOn Manager software (version 3.1.0.6) using the Langmuir interaction model. Reported values are the mean of at least six measurements.
Statistics
The statistical significance of different 50% survival index (SI50, 50% cell survival in comparison to untreated controls) values for cytotoxicity assays was determined by using GraphPad Prism 6.01 and data obtained from a nonlinear regression curve fit. The method used for the nonlinear regression curve fit was “log(inhibitor) versus normalized response” (by using a least square fit). Differences were determined by a one-way ANOVA and Tukey's multiple comparison test using alpha values of 0.05. The same method for determining statistical differences has been used for the results obtained by ELISA and in the neutralization assay.
Author Contributions
Experimental design by C.B., P.K.G., S.H.L., performance of experiments by C.B., P.K.G., S.B., C.E.L., B.H., R.J.F., writing of the manuscript by C.B., P.K.G., S.H.L., preparation of figures by C.B. All authors reviewed the manuscript.
Supplementary Material
Supplemental Information
Acknowledgments
This research was supported by the Intramural Research Program of the NIH, National Institute of Allergy and Infectious Diseases (NIAID), Bethesda, MD, USA. The authors thank J. Eric Anderson for mass spectrometric analysis of the proteins described here.
References
- Fuchs H. & Bachran C. Targeted tumor therapies at a glance. Curr Drug Targets 10, 89–93 (2009). [DOI] [PubMed] [Google Scholar]
- Liu S., Netzel-Arnett S., Birkedal-Hansen H. & Leppla S. H. Tumor cell-selective cytotoxicity of matrix metalloproteinase-activated anthrax toxin. Cancer Res 60, 6061–6067 (2000). [PubMed] [Google Scholar]
- Liu S. et al. Matrix metalloproteinase-activated anthrax lethal toxin demonstrates high potency in targeting tumor vasculature. J Biol Chem 283, 529–540, 10.1074/jbc.M707419200 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S. & Leppla S. H. Optimized production and purification of Bacillus anthracis lethal factor. Protein Expr Purif 18, 293–302, 10.1006/prep.2000.1208 (2000). [DOI] [PubMed] [Google Scholar]
- Abi-Habib R. J., Liu S., Bugge T. H., Leppla S. H. & Frankel A. E. A urokinase-activated recombinant diphtheria toxin targeting the granulocyte-macrophage colony-stimulating factor receptor is selectively cytotoxic to human acute myeloid leukemia blasts. Blood 104, 2143–2148, 10.1182/blood-2004-01-0339 (2004). [DOI] [PubMed] [Google Scholar]
- Thrower J. S., Hoffman L., Rechsteiner M. & Pickart C. M. Recognition of the polyubiquitin proteolytic signal. EMBO J 19, 94–102, 10.1093/emboj/19.1.94 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachmair A., Finley D. & Varshavsky A. In vivo half-life of a protein is a function of its amino-terminal residue. Science 234, 179–186 (1986). [DOI] [PubMed] [Google Scholar]
- Varshavsky A. The N-end rule pathway and regulation by proteolysis. Protein Sci 10.1002/pro.666 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta P. K., Moayeri M., Crown D., Fattah R. J. & Leppla S. H. Role of N-terminal amino acids in the potency of anthrax lethal factor. PLoS One 3, e3130, 10.1371/journal.pone.0003130 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayment I. Reductive alkylation of lysine residues to alter crystallization properties of proteins. Methods Enzymol 276, 171–179 (1997). [PubMed] [Google Scholar]
- Leysath C. E. et al. Anthrax edema factor toxicity is strongly mediated by the N-end rule. PLoS One 8, e74474, 10.1371/journal.pone.0074474 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetzel C., Bachran C., Tur M. K., Fuchs H. & Stocker M. Improved immunotoxins with novel functional elements. Curr Pharm Des 15, 2700–2711 (2009). [DOI] [PubMed] [Google Scholar]
- Bachran C. et al. The saponin-mediated enhanced uptake of targeted saporin-based drugs is strongly dependent on the saponin structure. Exp Biol Med (Maywood) 231, 412–420 (2006). [DOI] [PubMed] [Google Scholar]
- Bachran C., Heisler I., Fuchs H. & Sutherland M. Influence of protein transduction domains on target-specific chimeric proteins. Biochem Biophys Res Commun 337, 602–609, 10.1016/j.bbrc.2005.09.095 (2005). [DOI] [PubMed] [Google Scholar]
- Weldon J. E. et al. A protease-resistant immunotoxin against CD22 with greatly increased activity against CLL and diminished animal toxicity. Blood 113, 3792–3800, 10.1182/blood-2008-08-173195 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- London E. & Luongo C. L. Domain-specific bias in arginine/lysine usage by protein toxins. Biochem Biophys Res Commun 160, 333–339 (1989). [DOI] [PubMed] [Google Scholar]
- Falnes P. O., Ariansen S., Sandvig K. & Olsnes S. Requirement for prolonged action in the cytosol for optimal protein synthesis inhibition by diphtheria toxin. J Biol Chem 275, 4363–4368 (2000). [DOI] [PubMed] [Google Scholar]
- Su Y. et al. Systematic urokinase-activated anthrax toxin therapy produces regressions of subcutaneous human non-small cell lung tumor in athymic nude mice. Cancer Res 67, 3329–3336, 10.1158/0008-5472.CAN-06-4642 (2007). [DOI] [PubMed] [Google Scholar]
- Abi-Habib R. J. et al. A urokinase-activated recombinant anthrax toxin is selectively cytotoxic to many human tumor cell types. Mol Cancer Ther 5, 2556–2562, 10.1158/1535-7163.MCT-06-0315 (2006). [DOI] [PubMed] [Google Scholar]
- Fan Y. & Joachimiak A. Enhanced crystal packing due to solvent reorganization through reductive methylation of lysine residues in oxidoreductase from Streptococcus pneumoniae. J Struct Funct Genomics 11, 101–111, 10.1007/s10969-010-9079-6 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham S. J., Kobayashi T., Solaro R. J. & Gaponenko V. Differences in lysine pKa values may be used to improve NMR signal dispersion in reductively methylated proteins. J Biomol NMR 43, 239–246, 10.1007/s10858-009-9306-2 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor I. A., Webb M. & Kneale G. G. Surface labelling of the type I methyltransferase M.EcoR124I reveals lysine residues critical for DNA binding. J Mol Biol 258, 62–73, 10.1006/jmbi.1996.0234 (1996). [DOI] [PubMed] [Google Scholar]
- Weng A. et al. Enhancement of saporin cytotoxicity by Gypsophila saponins--more than stimulation of endocytosis. Chem Biol Interact 181, 424–429, 10.1016/j.cbi.2009.07.007 (2009). [DOI] [PubMed] [Google Scholar]
- Liu W. et al. Recombinant immunotoxin engineered for low immunogenicity and antigenicity by identifying and silencing human B-cell epitopes. Proc Natl Acad Sci U S A 109, 11782–11787, 10.1073/pnas.1209292109 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smallshaw J. E. et al. Genetic engineering of an immunotoxin to eliminate pulmonary vascular leak in mice. Nat Biotechnol 21, 387–391, 10.1038/nbt800 (2003). [DOI] [PubMed] [Google Scholar]
- Thoren K. L. & Krantz B. A. The unfolding story of anthrax toxin translocation. Mol Microbiol 80, 588–595, 10.1111/j.1365-2958.2011.07614.x (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pentelute B. L., Sharma O. & Collier R. J. Chemical dissection of protein translocation through the anthrax toxin pore. Angew Chem Int Ed Engl 50, 2294–2296, 10.1002/anie.201006460 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne J. C., Blanke S. R., Hanna P. C. & Collier R. J. Protective antigen-binding domain of anthrax lethal factor mediates translocation of a heterologous protein fused to its amino- or carboxy-terminus. Mol Microbiol 15, 661–666 (1995). [DOI] [PubMed] [Google Scholar]
- Arora N. & Leppla S. H. Fusions of anthrax toxin lethal factor with shiga toxin and diphtheria toxin enzymatic domains are toxic to mammalian cells. Infect Immun 62, 4955–4961 (1994). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesche J., Elliott J. L., Falnes P. O., Olsnes S. & Collier R. J. Characterization of membrane translocation by anthrax protective antigen. Biochemistry 37, 15737–15746, 10.1021/bi981436i (1998). [DOI] [PubMed] [Google Scholar]
- Singh Y., Klimpel K. R., Arora N., Sharma M. & Leppla S. H. The chymotrypsin-sensitive site, FFD315, in anthrax toxin protective antigen is required for translocation of lethal factor. J Biol Chem 269, 29039–29046 (1994). [PubMed] [Google Scholar]
- Liu S., Leung H. J. & Leppla S. H. Characterization of the interaction between anthrax toxin and its cellular receptors. Cell Microbiol 9, 977–987, 10.1111/j.1462-5822.2006.00845.x (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachran C., Sutherland M., Bachran D. & Fuchs H. Quantification of diphtheria toxin mediated ADP-ribosylation in a solid-phase assay. Clin Chem 53, 1676–1683, 10.1373/clinchem.2007.085365 (2007). [DOI] [PubMed] [Google Scholar]
- Newman Z. L., Leppla S. H. & Moayeri M. CA-074Me protection against anthrax lethal toxin. Infect Immun 77, 4327–4336, 10.1128/IAI.00730-09 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Information