Abstract
Tuberculosis (TB) has aptly been called the great mimicker. A 14-year-old boy, who had been treated for Hodgkin's Lymphoma 2 years back and had been in remission, underwent a whole body 18F-fludeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) scan, owing to a recent onset of backache and difficulty in walking. The study showed an FDG avid destructive lesion of the posterior elements of the sixth, seventh and eighth dorsal vertebrae along with a hypermetabolic collection in the adjacent paraspinal muscles with extension into the spinal canal, causing encasement of the thecal sac as well. Based on this constellation of findings, a diagnosis of atypical spinal TB was made, which was subsequently proven on histopathology. The present case illustrates that spinal TB, including the atypical form can be diagnosed on PET/CT even in clinically unsuspected cases.
Keywords: Atypical spinal tuberculosis, positron emission tomography/computed tomography, mimicker
INTRODUCTION
Tuberculosis (TB) is a pandemic and is among the top 10 killer infectious diseases, second only to the human immunodeficiency virus.[1] It has a worthy reputation as one of the great mimickers in medicine with a multitude of clinical pictures and variations.[2] Skeletal involvement is not common and is observed in 1-3% of affected individuals and of these, half have spinal involvement.[3] The present case depicts an unusual presentation in a clinically unsuspected case, wherein the diagnosis was made on positron emission tomography/computed tomography (PET/CT) examination. Knowledge of atypical variants of spinal TB is imperative for an accurate diagnosis and appropriate management.
CASE REPORT
This was a case report of a 14-year-old boy who presented with backache and difficulty in walking. Past history revealed that he had been treated for Hodgkin's Lymphoma 2 years ago and was presently in remission. Examination revealed localized tenderness in the mid-back, with decreased power in bilateral lower limbs. The patient underwent a whole-body PET/contrast-enhanced CT (CECT) scan on the suspicion of tumor recurrence. The study showed a destructive lesion of posterior elements of the sixth, seventh and eighth dorsal vertebrae which was fluorodeoxyglucose (FDG) avid [Figure 1]. In addition, an FDG avid peripherally enhancing collection was noted in the adjacent paraspinal muscles with extension into the spinal canal, causing encasement of the thecal sac as well. Additional sites of increased FDG avidity were noted in the mediastinal and hilar lymphnodes. A metabolically active focus was also noted in the spleen, which was seen as a subtle hypodense lesion on CECT [Figure 2]. Based on these findings, a diagnosis of extrapulmonary TB with Pott's spine and paraspinal abscess was made. The patient was started on antitubercular therapy and underwent posterior decompression and stabilization. Pus drained from the paraspinal abscess was positive for acid fast bacilli. Tissue biopsy revealed a histiocytic granuloma consistent with TB.
Figure 1.
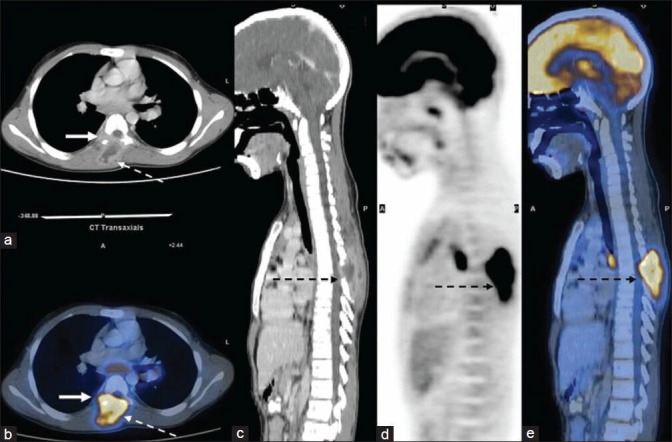
Transaxial and sagittal contrast-enhanced computed tomography (a and c) fused positron emission tomography/computed tomography (PET/CT) (b and e) and sagittal PET (d) image showing fludeoxyglucose (FDG) avid destructive lesion of posterior elements of dorsal vertebra (arrows) with an FDG avid peripherally enhancing collection in the adjacent paraspinal muscles extending into the spinal canal, causing encasement of the thecal sac as well (dotted arrows)
Figure 2.
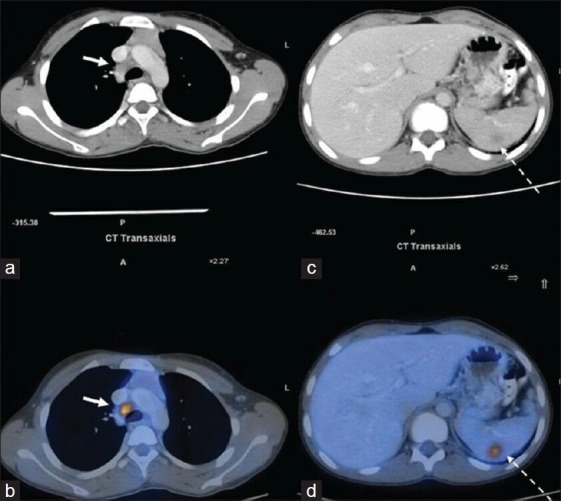
Transaxial contrast-enhanced computed tomography (a and c) and fused positron emission tomography/computed tomography (b and d) image shows fludeoxyglucose mediastinal lymphnodes (arrows). Additionally, a metabolically active focus was also noted in the spleen (dotted arrows)
DISCUSSION
Skeletal TB is not common, but of the affected patients, approximately half have spinal involvement.[4] There are three major patterns of vertebral involvement: Paradiscal, anterior and central.[5] Spinal TB characteristically involves the paradiscal area of the vertebral bodies with narrowing of the disc space.[6] In the paradiscal form, which accounts for more than half of all cases, infection usually begins at the anteroinferior part of the vertebral body and destroys the cartilaginous endplates.[7] Anterior lesions are subperisosteal, located under the anterior longitudinal ligament with extension of pus over multiple vertebral segments producing anterior scalloping.[8] Central lesions are centered on the vertebral body with disc sparing.[9] Posterior elements of vertebrae are rarely involved in isolation. An atypical presentation of spinal TB presents a challenge for an appropriate diagnosis and early treatment, due to the atypical clinical and radiologic features. Its incidence has been reported to be 2.1% in a recent study.[6] Atypical tuberculous spondylitis can be divided into three categories: Type 1 is the invasion only to neural arch; Type 2 is the invasion and destruction of a single vertebral body; and Type 3 is mass in the spinal canal, not invading the bones.[10] The rarity of the location may lead to delayed diagnosis, with subsequent neurological deficits. The main differential diagnoses of spinal TB include pyogenic and fungal osteomyelitis, trauma, multiple myeloma, lymphoma, eosinophilic granuloma and metastatic deposits.[11] Magnetic resonance imaging has been described as the most useful diagnostic tool for typical and atypical spinal TB as it provides greater detail of soft-tissue and disc and allows better visualization of posterior vertebral elements.[12] Recently, a few studies have been undertaken to delineate the role of PET/CT in the management of extrapulmonaty TB. Owing to the whole-body imaging provided by PET/CT, all metabolically active sites can be picked up in one single study, as seen in our case. It has been suggested that FDG PET as a non-invasive diagnostic tool, could give additional information about the disease status, enabling improved therapeutic management of mycobacterial infection.[13] It could be used as an important objective parameter in the management of TB and could reliably differentiate responders from non-responders at 2 months, a time point at which physicians choose a battery of tests to detect treatment response or failure.[14] A study undertaken to evaluate the diagnostic value of dual time point imaging (DTPI) of 18F-FDG PET/CT for detecting the infective lesions in patients with extrapulmonary TB revealed that early whole body PET/CT imaging may be sufficient for the detection of the EPTB lesions and DTPI of PET/CT may also not be a useful technique in differentiating between EPTB and non-EPTB lesions.[15]
There have been reports in the past wherein tubercular lesions have been mistaken for malignancy, including lymphoma.[16] In the present case too, the occurrence of mediastinal and hilar lymphadenopathy, splenic lesion and vertebral involvement [Figure 3] could well have been mistaken for lymphoma recurrence. However, the pattern of FDG uptake in the spine, with isolated involvement of lower dorsal vertebrae and associated paraspinal abscess with epidural extension, with sparing of other common sites of bone marrow involvement, made the possibility of atypical TB more likely. As TB commonly causes increased 18F-FDG uptake; therefore, positive 18F-FDG-PET results should be interpreted with caution in differentiating benign from malignant abnormalities.[17] A detailed and meticulous technique should be adopted in interpretation of PET/CT images, taking into account the PET findings in conjunction with the CT findings. The present case illustrates that spinal TB, including the atypical form can be diagnosed on PET/CT even in clinically unsuspected cases.
Figure 3.
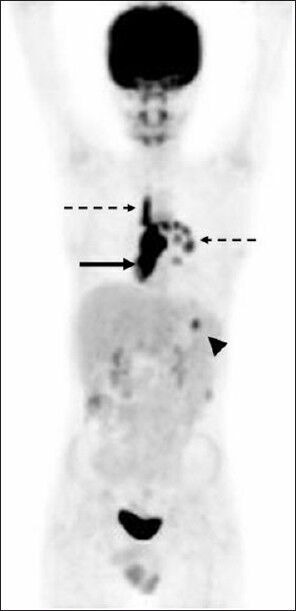
Maximum intensity projection image showing the presence of mediastinal and hilar lymphadenopathy (dotted arrows); splenic lesion (arrow head) and vertebral involvement (arrow) which could well have been mistaken for lymphoma recurrence
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Jain AK, Dhammi IK, Modi P, Kumar J, Sreenivasan R, Saini NS. Tuberculosis spine: Therapeutically refractory disease. Indian J Orthop. 2012;46:171–8. doi: 10.4103/0019-5413.93685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Polley P, Dunn R. Noncontiguous spinal tuberculosis: Incidence and management. Eur Spine J. 2009;18:1096–101. doi: 10.1007/s00586-009-0966-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kourbeti IS, Tsiodras S, Boumpas DT. Spinal infections: Evolving concepts. Curr Opin Rheumatol. 2008;20:471–9. doi: 10.1097/BOR.0b013e3282ff5e66. [DOI] [PubMed] [Google Scholar]
- 4.Tuli SM, Srivastava TP, Varma BP, Sinha GP. Tuberculosis of spine. Acta Orthop Scand. 1967;38:445–58. doi: 10.3109/17453676708989653. [DOI] [PubMed] [Google Scholar]
- 5.Doub HP, Badgley CE. The roentgen signs of tuberculosisof the vertebral body. AJR Am J Roentgenol. 1932;27:827–37. [Google Scholar]
- 6.Yalniz E, Pekindil G, Aktas S. Atypical tuberculosis of the spine. Yonsei Med J. 2000;41:657–61. doi: 10.3349/ymj.2000.41.5.657. [DOI] [PubMed] [Google Scholar]
- 7.Boachie-Adjei O, Squillante RG. Tuberculosis of the spine. Orthop Clin North Am. 1996;27:95–103. [PubMed] [Google Scholar]
- 8.Smith AS, Weinstein MA, Mizushima A, Coughlin B, Hayden SP, Lakin MM, et al. MR imaging characteristics of tuberculous spondylitis vs vertebral osteomyelitis. AJR Am J Roentgenol. 1989;153:399–405. doi: 10.2214/ajr.153.2.399. [DOI] [PubMed] [Google Scholar]
- 9.Ekw HO, Leong JC. The pediatric spine: Principles and practice. In: Weinstein SL, editor. Tuberculosis of the Spine. 3rd ed. New York: Raven; 1994. pp. 837–49. [Google Scholar]
- 10.Naim-Ur-Rahman, Al-Arabi KM, Khan FA. Atypical forms of spinal tuberculosis. Acta Neurochir (Wien) 1987;88:26–33. doi: 10.1007/BF01400511. [DOI] [PubMed] [Google Scholar]
- 11.Kirkman MA, Sridhar K. Posterior listhesis of a lumbar vertebra in spinal tuberculosis. Eur Spine J. 2011;20:1–5. doi: 10.1007/s00586-010-1524-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tuli SM. Tuberculosis of the spine: A historical review. Clin Orthop Relat Res. 2007;460:29–38. doi: 10.1097/BLO.0b013e318065b75e. [DOI] [PubMed] [Google Scholar]
- 13.Kosterink JG. Positron emission tomography in the diagnosis and treatment management of tuberculosis. Curr Pharm Des. 2011;17:2875–80. doi: 10.2174/138161211797470183. [DOI] [PubMed] [Google Scholar]
- 14.Basu S. 18F-FDG PET/CT as a sensitive and early treatment monitoring tool: Will this become the major thrust for its clinical application in infectious and inflammatory disorders? J Nucl Med. 2012;53:165. doi: 10.2967/jnumed.111.095026. [DOI] [PubMed] [Google Scholar]
- 15.Razak HR, Geso M, Abdul Rahim N, Nordin AJ. Imaging characteristics of extrapulmonary tuberculosis lesions on dual time point imaging (DTPI) of FDG PET/CT. J Med Imaging Radiat Oncol. 2011;55:556–62. doi: 10.1111/j.1754-9485.2011.02309.x. [DOI] [PubMed] [Google Scholar]
- 16.D'Souza MM, Tripathi M, Shrivastav M, Sharma R, Mondal A. Tuberculosis mimicking malignancy. Hell J Nucl Med. 2009;12:69–70. [PubMed] [Google Scholar]
- 17.Treglia G, Taralli S, Calcagni ML, Maggi F, Giordano A, Bonomo L. Is there a role for fluorine 18 fluorodeoxyglucose-positron emission tomography and positron emission tomography/computed tomography in evaluating patients with mycobacteriosis. A systematic review? J Comput Assist Tomogr. 2011;35:387–93. doi: 10.1097/RCT.0b013e318219f810. [DOI] [PubMed] [Google Scholar]


