Abstract
Background
Several epidemiologic studies showed the significant association of insulin resistance with asthma.
Objective
The aim of this study was to evaluate the association of insulin resistance with airway hyperresponsiveness (AHR) in adult population.
Methods
1,058 subjects who visited to the Seoul National University Hospital Gangnam Center from October 2007 to January 2009 for a routine health check-up were enrolled. All subjects completed a questionnaire, anthropometric measurements such as body mass index (BMI) and waist circumference, blood tests, pulmonary function test, and methacholine bronchial provocation test (MBPT). Insulin resistance was estimated from the homeostasis model of assessment of insulin resistance (HOMA-IR).
Results
Thirty-three subjects (3.1%) had AHR based on MBPT. The subjects with AHR had higher BMI, waist circumference, and HOMA-IR than those without AHR (p < 0.001, p = 0.003, and p = 0.002, respectively). In case of men, fasting insulin level and HOMA-IR had significant correlation with forced expiratory volume in 1 second (%) (r = -0.1440, p = 0.011, and r = -0.1156, p = 0.042, respectively). Fasting insulin level and HOMA-IR were higher in men with AHR than in those without (p = 0.046 and p = 0.040, respectively). In binary logistic regression analysis after adjustment for age, HOMA-IR was the significant risk factor for AHR in men (HOMA-IR: odds ratio [OR], 3.21; 95% confidence interval [CI], 1.00-10.30). In case of women, fasting insulin, glucose level, or insulin resistance had no significant correlation with lung function. BMI, waist circumference, and HOMA-IR were significantly higher in women with AHR than in those without (p = 0.001, p = 0.011, and p = 0.010, respectively). In binary logistic regression analysis after adjustment for age, BMI and HOMA-IR were the significant risk factors for AHR in women (BMI: OR, 2.20; 95% CI, 1.23-3.82; insulin resistance: OR, 1.05; 95% CI, 1.00-1.09).
Conclusion
Insulin resistance was significantly associated with bronchial hyperreactivity, which is the most characteristic feature of asthma.
Keywords: Asthma, Obesity, Bronchial hyperreactivity, Insulin resistance
INTRODUCTION
Both obesity and asthma are common chronic diseases in many westernized countries. The prevalence of both obesity and asthma has been increasing dramatically in times [1]. Many clinical studies showed the consistent association of obesity with asthma in terms of causal relationship, dose-dependency, and reversal of asthma by intervention, although the precise mechanism between obesity and asthma remains unclear [2, 3, 4, 5, 6]. Several mechanisms have been suggested as possible explanations about the relationship between obesity and asthma, including mechanical effects of obesity on the lung, chronic inflammation, common genetic factors, and comorbid conditions related to obesity such as gastroesophageal ref lux disease and sleep apnea [7]. Obesity is a state of chronic systemic inflammation, and may cause the metabolic complications such as insulin resistance, diabetes mellitus, and cardiovascular disease [8]. In particular, insulin resistance, a hallmark of obesity, plays a central role in the pathogenesis of these metabolic complications related to obesity. Several clinical studies have shown that elevated plasma glucose level and a diagnosis of diabetes mellitus were associated with impaired lung function [9, 10, 11, 12]. In addition, several epidemiological studies have shown that elevated insulin level and insulin resistance were associated with decreased lung function [13, 14, 15]. However, recent cross-sectional and longitudinal studies showed conflicting results about the association of insulin resistance with asthma [16, 17, 18, 19]. These studies suggest that obesity and asthma may be related through common inflammatory pathways associated with insulin resistance. However, the relationship between insulin resistance and airway hyperresponsiveness (AHR) has not been evaluated until now although AHR is a hallmark of asthma. The aim of this study was to evaluate the relationship between insulin resistance and AHR in adult population.
MATERIALS AND METHODS
Study population
This study protocol was approved by the Institutional Review Board at Seoul National University Hospital. This study was conducted for subjects who visited to the Seoul National University Hospital Gangnam Center for a routine health check-up from October 2007 to January 2009. Medical records were retrospectively reviewed. All subjects completed a questionnaire about previous and current medical history, current medications, respiratory symptoms, and smoking status. Subjects who had current respiratory symptoms, past or current history of asthma, diagnosis of diabetes mellitus, current medications for diabetes, plasma glucose level of more than 126 mg/dL, or significant comorbid conditions such as malignancy, heart disease, or autoimmune disease were excluded. Current smoker and ex-smoker were excluded because of the possibility of misclassification of chronic obstructive pulmonary disease (COPD) as asthma. Anthropometric measurements such as weight, height, and waist circumference were measured by trained personnel in our center.
Anthropometric measurements
Weight and height were measured in light clothes without shoes. Body mass index (BMI) was calculated as weight per the square of height (kg/m2). BMI was categorized according to the modified World Health Organization (WHO) criteria from the Asia-Pacific guideline: normal (<23 kg/m2), overweight (≥23, <25 kg/m2), and obese (≤25 kg/m2) [20]. The waist circumference was measured at midpoint between the lower rib cage and iliac crest according to the WHO recommendation.
Methacholine bronchial provocation test
Methacholine bronchial provocation test (MBPT) was carried out using modified Chai's method as previously described [21]. Briefly, forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1) were measured using a spirometer (Sensor medics 2,130, Sensor Medics, Yorba Linda, CA, USA), taking the largest values of triplicate FVC and FEV1 measurements. Subjects with respiratory tract infections during six previous weeks were excluded to avoid false positive result. A Rosenthal-French dosimeter (Laboratory for Applied Immunology, Baltimore, MD, USA) was used to deliver aerosols generated by a nebulizer (DeVilbiss, Carlsbad, CA, USA). Subjects inhaled five breaths of increasing methacholine concentrations either until the FEV1 fell to less than 80% of its baseline value or until the highest concentration was reached. The triplicate FEV1 measurements made at 90 s after each inhalation and the largest value was used for analysis. If the concentration of methacholine which caused a 20% fall in FEV1 (PC20) was less than 25 mg/mL, the subject was considered to have AHR to methacholine.
Assessment of insulin resistance
Insulin resistance was estimated from the homeostasis model of assessment of insulin resistance (HOMA-IR) [22]. The HOMA-IR was calculated from fasting plasma glucose and fasting serum insulin concentrations using the following formula (fasting plasma glucose [mmol/L] × fasting serum insulin [mU/L]/22.5) Insulin resistance was defined as HOMA-IR index in the upper 25% quartile of the population as baseline [23].
Statistical analysis
Statistical analysis was performed using the statistical program SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA). Independent t-test was used to compare continuous variables such as age, FEV1 (%), FVC (%), FEV1/FVC (%), waist circumference, glycated hemoglobin, fasting insulin level, and fasting glucose level between the study groups. Chi-square test was used to compare categorical variables such as sex, BMI, and HOMR-IR. Partial correlation after adjustment for age was used to evaluate the relationship between lung function and metabolic parameters such as fasting insulin or glucose level, and HOMA-IR. The risk factors for bronchial hyperreactivity in the study population were estimated using binary logistic regression analysis according to sex after adjustment for age. Statistical significance was defined as p value <0.05.
RESULTS
The baseline characteristics in our study population were summarized in Table 1. Three hundred and ten men (29.3%) and 748 women (70.7%) were enrolled in the study. All subjects were never-smokers and had no respiratory symptoms at the time of enrollment in the study.
Table 1.
Participant characteristics
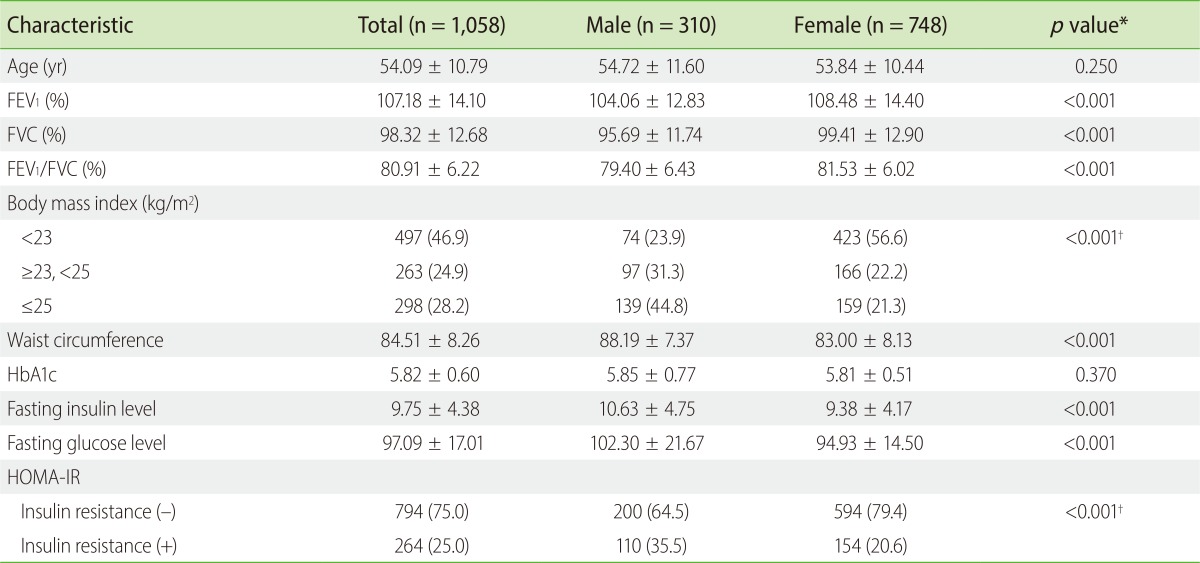
Values are presented as mean ± standard deviation or number (%).
FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; HbA1c, glycated hemoglobin; HOMA-IR, homeostasis model of assessment of insulin resistance.
*Independent t-test. †Chi-square test.
FEV1 (%), FVC (%), and FEV1/FVC (%) were significantly lower in men than in women (p < 0.001). BMI and waist circumference were significantly higher in men than in women (p < 0.001). Fasting insulin level, fasting glucose level and HOMA-IR was also higher in men than in women (p < 0.001).
Of 1,058 subjects, 33 subjects (3.1%) including 12 men and 21 women, showed AHR based on MBPT. The subjects with AHR had lower FEV1 (%) and FEV1/FVC (%) compared with the subjects without AHR (p < 0.001). BMI, waist circumference, and HOMA-IR was higher in subjects with AHR than those without (p < 0.001, p = 0.003, and p = 0.002, respectively) (Table 2). In case of men, fasting insulin level and HOMA-IR had significant correlation with FEV1 (%) (r = -0.1440, p =0.011, and r = -0.1156, p = 0.042, respectively). Men with AHR had lower FEV1 (%) and FEV1/FVC (%) compared with those without AHR (p = 0.001 and p < 0.001, respectively) (Table 3). Fasting insulin level and HOMA-IR were significantly higher in men with AHR than in those without (p = 0.046 and p = 0.040, respectively) although BMI, waist circumference, and fasting glucose level did not differ between the two groups (Table 3). In binary logistic regression analysis after adjustment for age, HOMA-IR were the significant risk factor for AHR in men (HOMA-IR: odds ratio [OR], 3.21; 95% confidence interval [CI], 1.00-10.30) (Table 4). However, the effects of insulin resistance on AHR became insignificant after adjusting for age and BMI (Table 4). In case of women, fasting insulin, glucose level, or insulin resistance had no significant correlation with lung function. Women with AHR had lower FEV1 (%) and FEV1/FVC (%) compared with those without AHR (p = 0.006 and p = 0.005, respectively) (Table 3). BMI, waist circumference, and HOMA-IR were significantly higher in women with AHR than in those without (p = 0.001, p = 0.011, and p = 0.043 respectively) although fasting insulin and glucose level did not differ between the groups (Table 3). In binary logistic regression analysis in women after adjustment for age, BMI and insulin resistance were the significant risk factors for AHR (BMI: OR, 2.20; 95% CI, 1.23-3.82; insulin resistance: OR, 1.05; 95% CI, 1.00-1.09) (Table 4). However, the effects of insulin resistance on AHR became insignificant after adjusting for age and BMI although BMI was consistently the significant risk factor for AHR after adjusting for age and insulin resistance (Table 4).
Table 2.
Comparison of lung function, obesity measures, and blood tests between the subjects with AHR and without AHR
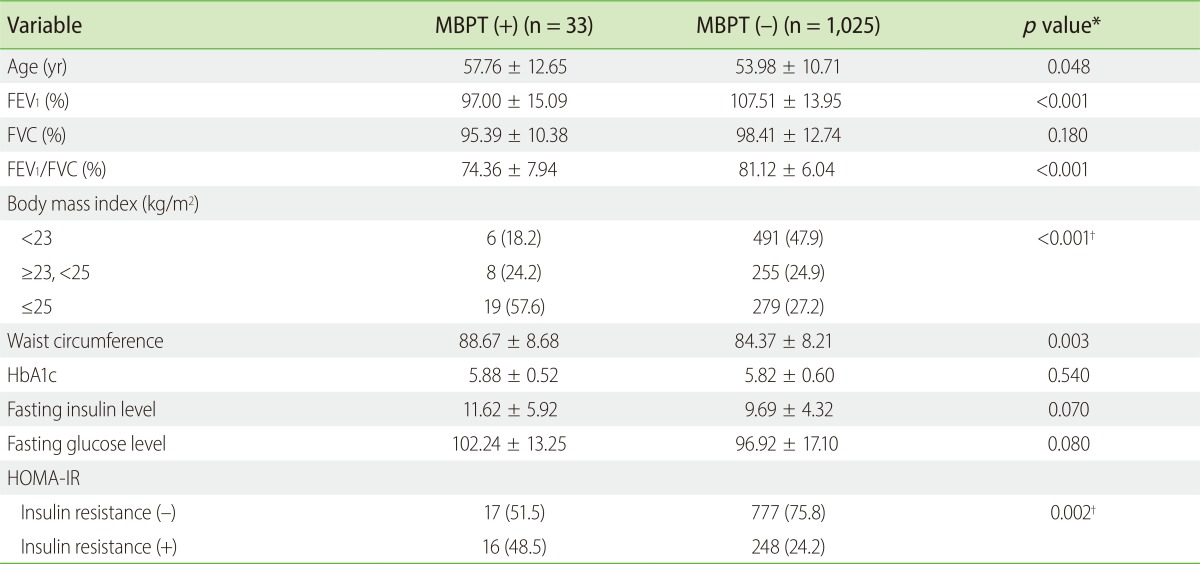
Values are presented as mean ± standard deviation or number (%).
AHR, airway hyperresponsiveness; MBPT, methacholine bronchoprovocation test; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; HbA1c, glycated hemoglobin; HOMA-IR, homeostasis model of assessment of insulin resistance.
*Independent t-test. †Chi-square test.
Table 3.
Comparison of lung function, obesity measures, and blood tests according to sex between the subjects with AHR and without AHR
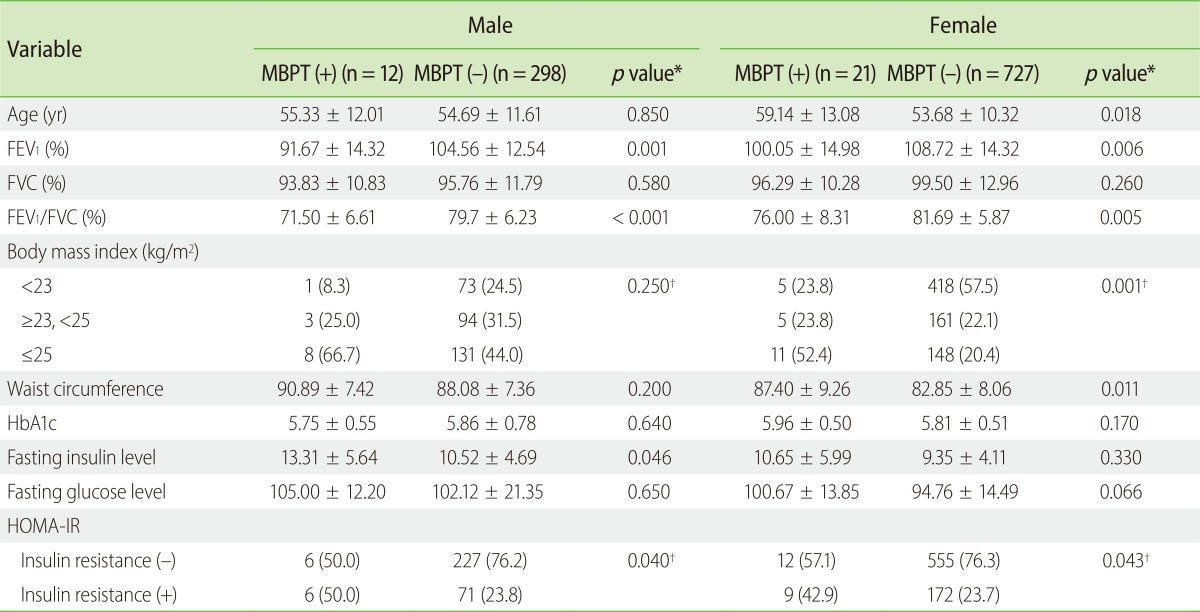
Values are presented as mean ± standard deviation or number (%).
AHR, airway hyperresponsiveness; MBPT, methacholine bronchoprovocation test; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; HbA1c, glycated hemoglobin; HOMA-IR, homeostasis model of assessment of insulin resistance.
*Independent t-test. †Chi-square test.
Table 4.
The risk factors for airway hyperresponsiveness according to sex
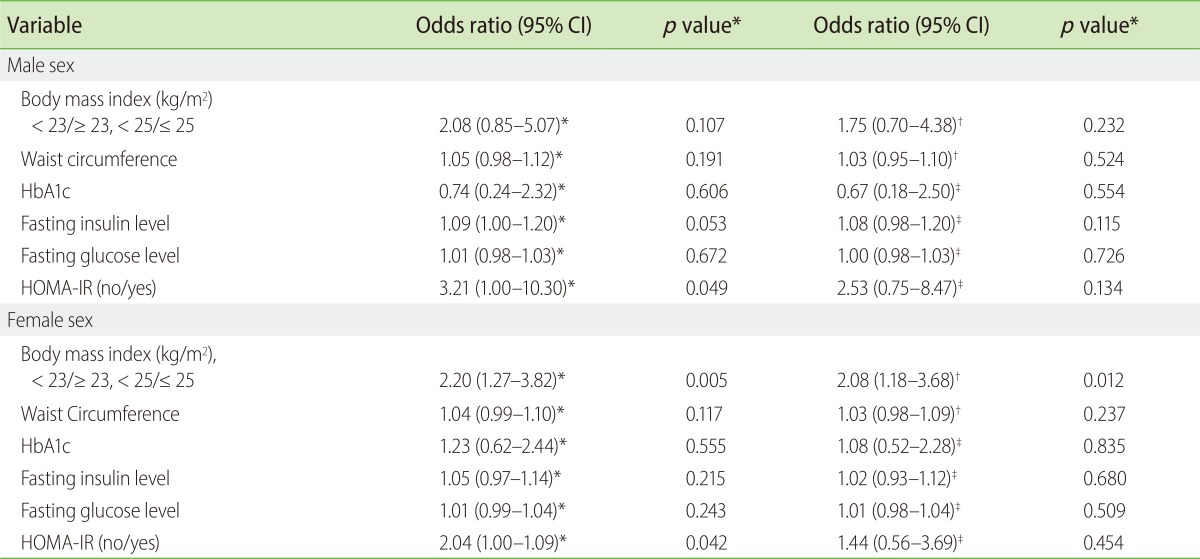
CI, confidence interval; HbA1c, glycated hemoglobin; HOMA-IR, homeostasis model of assessment of insulin resistance.
*Adjusted for age. †Adjusted for HOMA-IR. ‡Adjusted for body mass index.
DISCUSSION
To our knowledge, this is the first study that showed the significant association of insulin resistance with AHR. Insulin resistance was the significant risk factor for AHR in both men and women. BMI was the significant risk factor for AHR, especially in women. Fasting insulin level and insulin resistance had significant correlation with lung function in men.
A few cross-sectional and longitudinal studies have shown that glycemic state was significantly associated with impaired lung function. These studies showed that elevated fasting glucose level, the diagnosis of diabetes, or poor glycemic control in diabetes was significantly associated with impaired lung function [9, 10, 11, 12]. Elevated plasma glucose level was significantly associated with impaired lung function even in nondiabetics [9]. In our study, fasting insulin level and insulin resistance were significantly associated with lung function in men although fasting glucose level was not. This result is consistent with previous studies that have shown the association of elevated insulin level and insulin resistance with lung function [13, 14, 15]. The association of insulin resistance with impaired lung function was consistent even in nondiabetic males [13]. In contrast, the relationship between insulin resistance and asthma has been conflicting [16, 17, 18, 19]. A retrospective study of 146 asthmatics first reported that insulin resistance was significantly more common in morbidly obese asthma patients than in morbidly obese non-asthma patients [16]. In a cross-sectional study of 3,609 Danish adults, obesity was associated with increased risk of allergic sensitization, allergic and nonallergic asthma, whereas insulin resistance was associated with allergic sensitization and allergic asthma [17]. In this study, the relationship between obesity, allergic sensitization, and allergic asthma became insignificant after adjustment for insulin resistance. However, the relationship between insulin resistance, allergic sensitization, and allergic asthma was consistent after adjustment for obesity, suggesting that the effect of insulin resistance was stronger than that of obesity on allergic sensitization, and allergic asthma. A recent prospective study of 4,516 Danish adults demonstrated that obesity measures including BMI, waist circumference, waist-to-hip ratio, and insulin resistance were significantly associated with wheezing and asthma-like symptoms [18]. The association of obesity measures with wheezing and asthma-like symptoms decreased after adjustment for insulin resistance, suggesting that the effect of insulin resistance was stronger than that of obesity in wheezing and asthma-like symptoms. These studies suggest that obesity and asthma may be related through common inflammatory pathways associated with insulin resistance. However, in the National Health and Nutrition Examination Survey of 10,348 individuals in the United States, obesity was independently associated with asthma after controlling after insulin resistance and socio-demographic factors, but insulin resistance was not associated with atopy or asthma.
Despite the conflicting results between insulin resistance and asthma, there have been no studies about the association of insulin resistance with AHR, which is the most characteristic feature of asthma. As far as we know, this is the first study that showed the significant association of insulin resistance with AHR. In our study, insulin resistance was the significant risk factor for AHR in both men and women. However, the association of insulin resistance and AHR became insignificant in both men and women after adjusting for age and BMI, suggesting that insulin resistance is associated with AHR through mechanisms also involved in the development of obesity.
Only never-smokers were enrolled in the study, and excluded the possibility that COPD patients were enrolled in our study. Furthermore, AHR was defined on the result of MBPT. Previous studies about the relationship between insulin resistance and asthma has a limitation because the definition of asthma was based on self-reported questionnaire.
Obesity is a state of chronic low grade systemic inflammation, and inflammatory markers such as tumor necrosis factor-α (TNF-α), interleukin-6, and vascular endothelial growth factor increased in obese subjects [7, 11]. This proinflammatory state of obesity is associated with insulin resistance and increased risk of type II diabetes. In particular, TNF-α may play an important role on obesity-related insulin resistance [24, 25]. TNF-α level increased in the blood and airways of asthma patients [26, 27]. Furthermore, the administration of inhaled recombinant TNF-α to normal subjects or mild asthmatics led to increased AHR and airway inflammation [28, 29]. Considering these previous study results, TNF-α inflammatory pathway may be the possible mechanism explaining the association of insulin resistance with AHR although those cytokines involved in the pathogenesis of insulin resistance were not measured in our study.
There were several limitations in our study. First, it remains unclear whether increased AHR in our study subjects is primarily associated with metabolic abnormalities related to insulin resistance both because the cytokines related to insulin resistance were not measured. Second, the study population was not representative of general population, and the sample size with AHR was small, especially in men, because the subjects without respiratory symptoms who visited for a routine health check-up were enrolled in our study. The failure to find a relationship between BMI and AHR in men may be attributable to the small sample size. Third, the relationship between insulin resistance and asthma was unknown in our study because only healthy subjects without respiratory symptoms were enrolled.
Future study including measurement of inflammatory mediators related to insulin resistance is needed to reveal the mechanism about the relationship between insulin resistance and AHR.
References
- 1.Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma--United States, 1980-1999. MMWR Surveill Summ. 2002;51:1–13. [PubMed] [Google Scholar]
- 2.Ford ES, Mannino DM, Redd SC, Mokdad AH, Mott JA. Body mass index and asthma incidence among USA adults. Eur Respir J. 2004;24:740–744. doi: 10.1183/09031936.04.00088003. [DOI] [PubMed] [Google Scholar]
- 3.Chen Y, Dales R, Jiang Y. The association between obesity and asthma is stronger in nonallergic than allergic adults. Chest. 2006;130:890–895. doi: 10.1378/chest.130.3.890. [DOI] [PubMed] [Google Scholar]
- 4.Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175:661–666. doi: 10.1164/rccm.200611-1717OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aaron SD, Fergusson D, Dent R, Chen Y, Vandemheen KL, Dales RE. Effect of weight reduction on respiratory function and airway reactivity in obese women. Chest. 2004;125:2046–2052. doi: 10.1378/chest.125.6.2046. [DOI] [PubMed] [Google Scholar]
- 6.Maniscalco M, Zedda A, Faraone S, Cerbone MR, Cristiano S, Giardiello C, Sofia M. Weight loss and asthma control in severely obese asthmatic females. Respir Med. 2008;102:102–108. doi: 10.1016/j.rmed.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 7.Shore SA. Obesity and asthma: possible mechanisms. J Allergy Clin Immunol. 2008;121:1087–1093. doi: 10.1016/j.jaci.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Hajer GR, van Haeften TW, Visseren FL. Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur Heart J. 2008;29:2959–2971. doi: 10.1093/eurheartj/ehn387. [DOI] [PubMed] [Google Scholar]
- 9.Lange P, Groth S, Kastrup J, Mortensen J, Appleyard M, Nyboe J, Jensen G, Schnohr P. Diabetes mellitus, plasma glucose and lung function in a cross-sectional population study. Eur Respir J. 1989;2:14–19. [PubMed] [Google Scholar]
- 10.Lange P, Groth S, Mortensen J, Appleyard M, Nyboe J, Schnohr P, Jensen G. Diabetes mellitus and ventilatory capacity: a five year follow-up study. Eur Respir J. 1990;3:288–292. [PubMed] [Google Scholar]
- 11.Walter RE, Beiser A, Givelber RJ, O'Connor GT, Gottlieb DJ. Association between glycemic state and lung function: the Framingham Heart Study. Am J Respir Crit Care Med. 2003;167:911–916. doi: 10.1164/rccm.2203022. [DOI] [PubMed] [Google Scholar]
- 12.Davis WA, Knuiman M, Kendall P, Grange V, Davis TM Fremantle Diabetes Study. Glycemic exposure is associated with reduced pulmonary function in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care. 2004;27:752–757. doi: 10.2337/diacare.27.3.752. [DOI] [PubMed] [Google Scholar]
- 13.Lazarus R, Sparrow D, Weiss ST. Impaired ventilatory function and elevated insulin levels in nondiabetic males: the Normative Aging Study. Eur Respir J. 1998;12:635–640. doi: 10.1183/09031936.98.12030635. [DOI] [PubMed] [Google Scholar]
- 14.Lawlor DA, Ebrahim S, Smith GD. Associations of measures of lung function with insulin resistance and Type 2 diabetes: findings from the British Women's Heart and Health Study. Diabetologia. 2004;47:195–203. doi: 10.1007/s00125-003-1310-6. [DOI] [PubMed] [Google Scholar]
- 15.Engström G, Hedblad B, Nilsson P, Wollmer P, Berglund G, Janzon L. Lung function, insulin resistance and incidence of cardiovascular disease: a longitudinal cohort study. J Intern Med. 2003;253:574–581. doi: 10.1046/j.1365-2796.2003.01138.x. [DOI] [PubMed] [Google Scholar]
- 16.Al-Shawwa BA, Al-Huniti NH, DeMattia L, Gershan W. Asthma and insulin resistance in morbidly obese children and adolescents. J Asthma. 2007;44:469–473. doi: 10.1080/02770900701423597. [DOI] [PubMed] [Google Scholar]
- 17.Husemoen LL, Glumer C, Lau C, Pisinger C, Mørch LS, Linneberg A. Association of obesity and insulin resistance with asthma and aeroallergen sensitization. Allergy. 2008;63:575–582. doi: 10.1111/j.1398-9995.2007.01613.x. [DOI] [PubMed] [Google Scholar]
- 18.Thuesen BH, Husemoen LL, Hersoug LG, Pisinger C, Linneberg A. Insulin resistance as a predictor of incident asthma-like symptoms in adults. Clin Exp Allergy. 2009;39:700–707. doi: 10.1111/j.1365-2222.2008.03197.x. [DOI] [PubMed] [Google Scholar]
- 19.Ma J, Xiao L, Knowles SB. Obesity, insulin resistance and the prevalence of atopy and asthma in US adults. Allergy. 2010;65:1455–1463. doi: 10.1111/j.1398-9995.2010.02402.x. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Geneva: World Health Organization; 1999. pp. 20–21. [Google Scholar]
- 21.Kim YK, Kim SH, Tak YJ, Jee YK, Lee BJ, Kim SH, Park HW, Jung JW, Bahn JW, Chang YS, Choi DC, Chang SI, Min KU, Kim YY, Cho SH. High prevalence of current asthma and active smoking effect among the elderly. Clin Exp Allergy. 2002;32:1706–1712. doi: 10.1046/j.1365-2222.2002.01524.x. [DOI] [PubMed] [Google Scholar]
- 22.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- 23.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 24.Cottam DR, Mattar SG, Barinas-Mitchell E, Eid G, Kuller L, Kelley DE, Schauer PR. The chronic inflammatory hypothesis for the morbidity associated with morbid obesity: implications and effects of weight loss. Obes Surg. 2004;14:589–600. doi: 10.1381/096089204323093345. [DOI] [PubMed] [Google Scholar]
- 25.Hotamisligil GS, Murray DL, Choy LN, Spiegelman BM. Tumor necrosis factor alpha inhibits signaling from the insulin receptor. Proc Natl Acad Sci U S A. 1994;91:4854–4858. doi: 10.1073/pnas.91.11.4854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berry MA, Hargadon B, Shelley M, Parker D, Shaw DE, Green RH, Bradding P, Brightling CE, Wardlaw AJ, Pavord ID. Evidence of a role of tumor necrosis factor alpha in refractory asthma. N Engl J Med. 2006;354:697–708. doi: 10.1056/NEJMoa050580. [DOI] [PubMed] [Google Scholar]
- 27.Howarth PH, Babu KS, Arshad HS, Lau L, Buckley M, McConnell W, Beckett P, Al Ali M, Chauhan A, Wilson SJ, Reynolds A, Davies DE, Holgate ST. Tumour necrosis factor (TNFalpha) as a novel therapeutic target in symptomatic corticosteroid dependent asthma. Thorax. 2005;60:1012–1018. doi: 10.1136/thx.2005.045260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thomas PS, Heywood G. Effects of inhaled tumour necrosis factor alpha in subjects with mild asthma. Thorax. 2002;57:774–778. doi: 10.1136/thorax.57.9.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thomas PS, Yates DH, Barnes PJ. Tumor necrosis factor-alpha increases airway responsiveness and sputum neutrophilia in normal human subjects. Am J Respir Crit Care Med. 1995;152:76–80. doi: 10.1164/ajrccm.152.1.7599866. [DOI] [PubMed] [Google Scholar]


