Abstract
Background:
The recently identified circulating sCD36 has been proposed to reflect tissue CD36 expression, and is upregulated in case of obesity, insulin resistance and hepatic steatosis. The aim of this study was to explore the effect of weight loss secondary to bariatric surgery in relation to sCD36 among morbidly obese individuals. Furthermore, we investigated the levels of sCD36 in relation to obesity-related metabolic complications, low-grade inflammation and fat distribution.
Methods:
Twenty morbidly obese individuals (body mass index (BMI) 43.0±5.4 kg m−2) with a referral to Roux-en-Y gastric bypass were included. Anthropometric measurements and fasting blood samples were collected at a preoperative baseline visit and 3 months after surgery. sCD36 was measured by an in-house assay, whereas insulin sensitivity and the hepatic fat accumulation were estimated by the homeostasis model assessment (HOMA-%S) and liver fat percentage (LF%), respectively.
Results:
Postoperatively, BMI was reduced by 20% to 34.3±5.2 kg m−2 (P<0.001). sCD36 was reduced by 31% (P=0.001) and improvements were observed in the amount of fat mass (P<0.001), truncal fat mass (P<0.001), circulating triglycerides (P=0.001), HOMA-%S (P=0.007), LF% (P=0.001) and the inflammatory marker high-sensitive C-reactive protein (P=0.005). sCD36 correlated with triglycerides (ρ=0.523, P=0.001) and truncal fat mass (ρ=0.357, P=0.026), and triglycerides were found to be an independent predictor of sCD36. At baseline, participants with the metabolic syndrome had a higher LF% and higher levels of the inflammatory biomarker YKL-40 (P=0.003 and P=0.014) as well as a tendency towards higher levels of sCD36.
Conclusion:
sCD36 was reduced by weight loss and associated with an unhealthy fat accumulation and circulating triglycerides, which support the proposed role of sCD36 as a biochemical marker of obesity-related metabolic complications and risks.
Introduction
Obesity is a major, increasing problem worldwide, and a great threat to the general health, leading to increased morbidity and mortality.1, 2 Metabolic complications and comorbidities, such as cardiovascular disease, type 2 diabetes mellitus (T2DM), insulin resistance and hepatic steatosis are commonly seen in relation to obesity.3 Abdominal obesity is generally considered as an unhealthy fat accumulation and seems to be important in insulin resistance as well as a contributing factor to the metabolic syndrome; a condition, which describes the presence of a cluster of risk factors associated with diabetes and cardiovascular disease.3, 4 In a 16 year follow-up study among healthy women, it was reported that 61% of new T2DM-cases could be attributed to obesity, and the risk of T2DM was found increased with an increasing body mass index (BMI).5 Likewise, the prevalence of non-alcohol related hepatic steatosis (non-alcoholic fatty liver disease) is high among obese individuals as well as patients with T2DM.6, 7, 8
Activation of the innate immune system and the establishment of a low-grade inflammatory state are considered to have a role in the common pathogenesis of obesity and insulin resistance and the subsequent development of T2DM.9, 10, 11 It has been hypothesized that adipocyte hypertrophy, as a result of adipose tissue expansion, leads to a local hypoxic condition, which may have a crucial role in the initiation of the inflammatory processes, and in which macrophage infiltration and proinflamatory cytokines seem to contribute to the impairment of the normal adipocyte function.8, 12 The relations between circulating lipids and obesity are not completely understood, but particularly the levels of free fatty acids (FFA) and triglycerides are considered to be elevated in case of obesity, especially due to the increased volume of adipose tissue, a reduced FFA clearance13, 14 as well as the obesity-induced insulin resistance and thus increased lipolysis.
CD36 is a multifunctional membrane protein expressed by many cell types.15 The receptor has an important function in the facilitation of fatty acid uptake, which precedes the secretion and storage as triglycerides, and thus contribute to insulin resistance in muscle-, fat- and liver cells, respectively.16, 17, 18, 19, 20 Beside the function as a fatty acid translocase, CD36 is proposed to be involved in the inflammatory responses in both adipocytes and macrophages during complications of diet-induced obesity.21 Recently, a non-cell bound circulating form of CD36 (sCD36) has been identified and proposed to reflect tissue CD36 expression.22, 23 Measures of liver fat content and the severity of steatosis were recently reported to be associated with circulating levels of sCD36,24, 25 and further connections between sCD36 and insulin resistance, BMI as well as obesity-driven low-grade inflammation have been proposed.22, 24, 26, 27
High-sensitive C-reactive protein (hsCRP), an unspecific marker of systemic and subclinical inflammation, is found to be related to obesity.28 YKL-40 is a locally produced glycoprotein involved in inflammation and endothelial dysfunction, and it seems to be of pathogenic importance in the low-grade inflammation that precedes the development of cardiovascular disease.29 Several clinical studies have described elevated YKL-40 levels in subjects with diabetes or cardiovascular conditions, including an association between YKL-40 and both all-cause and cardiovascular mortality.29
Bariatric surgery is currently the only treatment of morbidly obese subjects resulting in a long term, sustained weight loss and thus a decreased volume of visceral adipose tissue and metabolic improvements, especially in relation to the glucose metabolism and insulin sensitivity.30, 31, 32 In order to study the relationship between CD36 and fat accumulation and distribution, and to substantiate previous findings of sCD36 as a risk marker of components in the metabolic syndrome, we investigated the relations between sCD36 and insulin sensitivity, fat distribution, plasma lipids, ectopic hepatic fat accumulation and obesity-driven low-grade inflammation among morbidly obese individuals before and after gastric bypass. Our hypotheses were that sCD36 would decrease along with surgically induced weight loss and would be associated with central obesity as well as obesity-related metabolic complications, such as insulin sensitivity, ectopic hepatic fat accumulation, and levels of circulating triglycerides.
Materials and methods
Study population and clinical examinations
Twenty morbidly obese subjects referred to bariatric surgery were included in the study. Of surgery-related reasons, the participants had lost approximately 8% of their body weight before inclusion in this study. They all met the Danish criteria for bariatric surgery:⩾20 years of age and BMI⩾40 kg m−2 or BMI⩾35 kg m−2 and comorbidities (two participants had T2DM, one hypertension and three arthrosis). All patients were dismissed within 24 h after surgery and no patients suffered from postoperative complications.
The participants were examined twice; at baseline before the operation and 3 months postoperatively. At both visits, following an overnight fast, venous blood samples were collected, measures of weight and height were retrieved, and the body content of fat mass was measured using a full body dual-energy X-ray absorptiometry scanner. Weight and dual-energy X-ray absorptiometry-scan are missing from one participant at the 3 months follow-up visit.
The study was approved by the Danish Data Protection Agency (id. 00908 HEH.750.86-4) and the ethics committee in the Capital Region of Denmark (H-3-2009-100), and informed written consent was obtained from all participants prior to inclusion.
Surgical procedure
Surgery was performed at the Hamlet Hospital, Copenhagen, Denmark by either of two surgeons with expertise in Roux-en-Y gastric bypass, using a standard laparoscopic Roux-en-Y gastric bypass technique. The main characteristics of the Roux-en-Y gastric bypass were construction of a gastric pouch of approximately 25 ml, a biliopancreatic limb of 60 cm and a Roux-limb of 120 cm.
Biochemical analysis
Circulating plasma sCD36 was measured in duplicates using an in-house enzyme-linked immunosorbent assay as previously described.22 sCD36 concentrations are expressed relative to a plasma pool in arbitrary units. Internal controls were run in quadruplicate on each plate. Intra- and combined intra- and interassay coefficients of variation for this assay were around 6 and 16.4%. Serum YKL-40 was measured by an enzyme-linked immunosorbent assay method (Quidel, San Diego, CA, USA), with intra- and interassay coefficients of variation of 5.8% and 6.0%, respectively. hsCRP was measured with a highly sensitive, latex-particle-enhanced immunoturbidimetric assay (DAKO, Glostrup, Denmark). Remaining biochemical parameters (hemoglobin, leukocytes, alanine aminotransferase, aspartate aminotransferase, glycosylated hemoglobin, plasma glucose, connecting peptide, serum insulin, total cholesterol, high-density lipoprotein, low-density lipoprotein and triglycerides) were analyzed using routine standardized methods in our biochemical laboratory.
Insulin sensitivity
Insulin sensitivity was estimated using the homeostasis model assessment (HOMA-%S) (http://www.dtu.ox.ac.uk/homacalculator/index.php).
Liver fat percentage
Liver fat percentage (LF%) is based on an algorithm used to predict the degree of fat accumulation in hepatocytes based on the presence of the metabolic syndrome and T2DM as well as fasting insulin and the liver enzymes aspartate aminotransferase and alanine aminotransferase.33
Statistics
Continuous variables are presented as mean±s.d. Paired and unpaired nonparametric statistical analyses were used for differences between the pre- and postoperative states and the presence or absence of the metabolic syndrome at baseline, respectively. Correlations were analyzed by a nonparametric correlation test on pooled data (Spearman's rho correlation's test). Multiple regression analyses were performed to identify independent variables predicting sCD36 as the continuous dependent variable. Statistical analyses were two-sided, and P-values⩽0.05 were considered statistically significant. All analyses were made with the statistical software package SPSS (version 11.5 SPSS; Chicago, IL, USA).
Results
Weight loss and improvements in body fat distribution and circulating plasma lipids 3 months after bariatric surgery
Selected clinical and biochemical data from the pre- and 3 months postoperative visits are presented in Table 1. At the baseline visit, the mean age was 41.2±11 years, the average BMI was 43.0±5.4 kg m−2 and 13 of the participants were defined as having the metabolic syndrome.4 Following surgery, an average weight loss of 23.9 kg was observed after 3 months, and thus a significant decrease in BMI of 20%. Furthermore, the amount of body fat and the fat distribution were improved by highly significant decreases in fat mass (30%), in particular the truncal fat mass (33%). Along with the surgically induced weight loss, the circulating lipids, total cholesterol and triglycerides decreased significantly by 8% and 24%, respectively. At baseline, 45% had elevated levels of triglycerides (triglycerides⩾1.7 mmol l−1 or 150 mg dl−1 34). Positive correlations were found between levels of circulating triglycerides and fat mass (ρ=0.376, P=0.018), including truncal fat (ρ=0.366, P=0.022) as well as between triglycerides and BMI (ρ=0.363, P=0.023).
Table 1. Clinical and biochemical characteristics of the study population pre- and 3 months postoperatively.
| Preoperatively | Postoperatively | P-value | |
|---|---|---|---|
| Weight | 120.0±18.1 | 96.1±17.4† | <0.001* |
| BMI (kg m−2) | 43.0±5.4 | 34.3±5.2† | <0.001* |
| Hemoglobin (mmol l−1) | 8.5±0.5 | 8.4±0.6 | 0.14 |
| Leukocytes (mia l−1) | 8.4±2.2 | 7.0±1.6 | <0.001* |
| ALT (U l−1) | 31±14 | 29 ±16 | 0.754 |
| AST (U l−1) | 30±8 | 31±12 | 0.812 |
| HbA1c (%) | 5.9±0.4 | 5.8±0.6 | 0.131 |
| Plasma glucose (mmol l−1) | 5.7±0.9 | 5.3±1.2 | 0.161 |
| C-peptide (pmol l−1) | 1196±560 | 894±554 | 0.120 |
| Serum insulin (pmol l−1) | 172±149 | 82±66 | 0.023* |
| Total cholesterol (mmol l−1) | 4.9±1.0 | 4.5±0.9 | 0.027* |
| HDL (mmol l−1) | 1.1±0.3 | 1.1±0.3 | 0.659 |
| LDL (mmol l−1) | 3.0±0.9 | 2.8±0.7 | 0.299 |
| Triglycerides (mmol l−1) | 1.7±0.6 | 1.3±0.4 | 0.001* |
| Fat mass (kg) | 54.8±11.0 | 38.5±11.4† | <0.001* |
| Truncal fat (g) | 26.6±4.0 | 17.9±4.9† | <0.001* |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; C-peptide, connecting peptide; HbA1c, glycosylated hemoglobin; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Values are mean±s.d. *Significant P-values.
n=20, except † (n=19).
sCD36 decreased markedly following bariatric surgery and associations with anthropometric characteristics and circulating triglycerides were observed
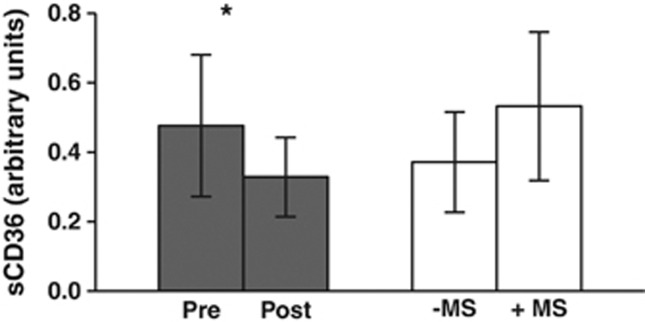
After bariatric surgery, a 31% reduction in circulating sCD36 was found (P=0.001, Figure 1). At the baseline visit, the participants defined as having the metabolic syndrome had a non-significant, but 30% higher plasma concentration of sCD36 (P=0.097). Significant positive correlations were found between sCD36 and the anthropometric measurements: weight (ρ=0.322, P=0.045), fat mass (ρ=0.358, P=0.025) and truncal fat mass (ρ=0.357, P=0.026), respectively, whereas sCD36 tended to associate with BMI (ρ=0.281, P=0.083). Among the circulating lipids, a significant correlation was found between circulating sCD36 and triglycerides (ρ=0.523, P=0.001).
Figure 1.
Circulating plasma levels of sCD36. Levels of sCD36 are expressed as means and error bars represent±s.d. Gray bars  show the concentrations of sCD36 at the preoperative baseline visit (Pre, n=20) and 3 months postoperatively (Post, n=20), *P=0.001. White bars □ show baseline levels of sCD36 in relation to the presence (+MS, n=13) or absence (− MS, n=7) of the metabolic syndrome. +MS, presence of the metabolic syndrome; −MS, absence of the metabolic syndrome.
show the concentrations of sCD36 at the preoperative baseline visit (Pre, n=20) and 3 months postoperatively (Post, n=20), *P=0.001. White bars □ show baseline levels of sCD36 in relation to the presence (+MS, n=13) or absence (− MS, n=7) of the metabolic syndrome. +MS, presence of the metabolic syndrome; −MS, absence of the metabolic syndrome.
Increased insulin sensitivity and associations between sCD36 and plasma glucose were observed after bariatric surgery
Following bariatric surgery, improvements in insulin sensitivity, estimated by a markedly 41% increase in HOMA-%S (42.7% vs 60.4%, P=0.007) were observed. HOMA-%S correlated negatively with the anthropometric measurements fat mass (ρ=−0.362, P=0.024), truncal fat (ρ=−0.366, P=0.022), and BMI (ρ=−0.390, P=0.014). Furthermore, negative correlations between HOMA-%S and the circulating lipids triglycerides (ρ=−0.433, P=0.005) and total cholesterol (ρ=−0.313, P=0.049) were observed. No significant association was found between sCD36 and insulin sensitivity, whereas sCD36 and fasting plasma glucose were significantly correlated (ρ=0.382, P=0.015).
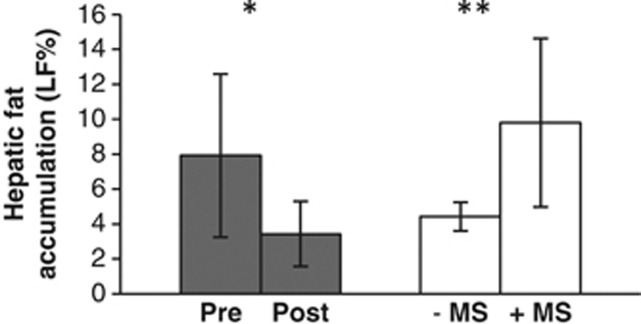
Decreased LF% along with weight loss and improved insulin sensitivity after bariatric surgery
At the baseline visit, the average LF% was 7.9% and 3 months after the surgery, it was significantly decreased by 57% (P=0.001, Figure 2). Participants with the metabolic syndrome had at baseline a higher LF% of 55%, compared with participants without the metabolic syndrome (P=0.003, Figure 2). Correlations were observed between LF% and truncal fat mass (ρ=0.383, P=0.016), BMI (ρ=0.388, P=0.015), weight (ρ=0.359, P=0.015), triglycerides (ρ=0.313, P=0.049), hsCRP (ρ=0.315, 0.048) and fasting plasma glucose (ρ=0.569, P<0.001), respectively; whereas LF% tended to be associated with fat mass (ρ=0.290, P=0.074) and sCD36 (ρ=0.284, P=0.075).
Figure 2.
Hepatic fat accumulation estimated by LF%. LF% are expressed as means and error bars represent±s.d. Gray bars  show LF% at the preoperative baseline visit (Pre, n=20) and 3 months postoperatively (Post, n=20), *P=0.001. White bars □ show baseline LF% in relation to the presence (+MS, n=13) or absence (−MS, n=7) of the metabolic syndrome, **P=0.003. +MS, presence of the metabolic syndrome; −MS, absence of the metabolic syndrome.
show LF% at the preoperative baseline visit (Pre, n=20) and 3 months postoperatively (Post, n=20), *P=0.001. White bars □ show baseline LF% in relation to the presence (+MS, n=13) or absence (−MS, n=7) of the metabolic syndrome, **P=0.003. +MS, presence of the metabolic syndrome; −MS, absence of the metabolic syndrome.
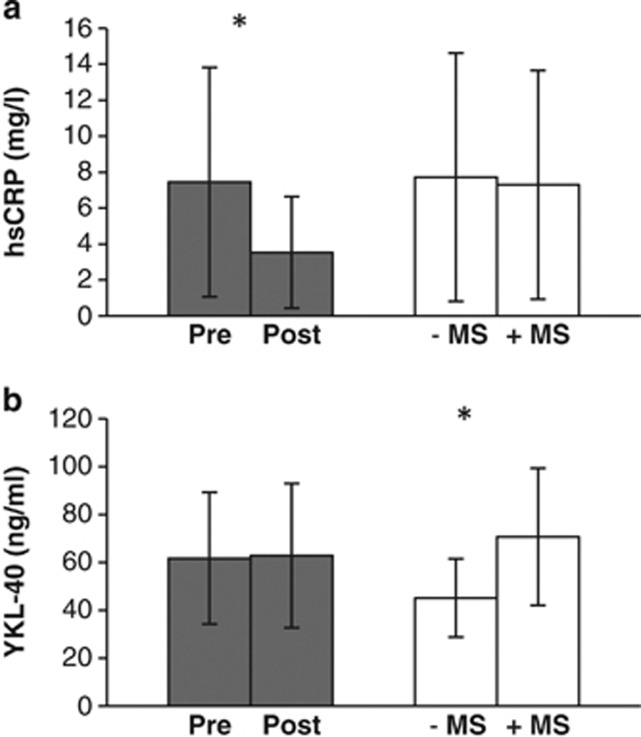
Inflammatory markers and bariatric surgery
A 53% reduction in hsCRP was observed postoperatively (P=0.005), whereas no significant changes were found among the levels of YKL-40 (Figure 3). Significant positive correlations were observed between hsCRP and weight (ρ=0.489, P=0.002), BMI (ρ=0.463, P=0.003), fat mass (ρ=0.462, P=0.003), truncal fat mass (ρ=0.490, P=0.002) and leukocytes (ρ=0.520, P=0.001), as well as the circulating lipids total cholesterol (ρ=0.350, P=0.027) and triglycerides (ρ=0.447, P=0.004). hsCRP and HOMA-%S were inversely correlated (ρ=−0.452, P=0.003). Associations between plasma YKL-40 and anthropometric data, insulin sensitivity and biochemical parameters were not found. Participants with the metabolic syndrome at baseline had significantly higher levels of YKL-40 (P=0.014), wheras no differences were observed in hsCRP levels (Figure 3). No significant correlations were demonstrated between sCD36 and the inflammatory markers hsCRP and YKL-40.
Figure 3.
The inflammatory biomarkers hsCRP and YKL-40. Levels of hsCRP and YKL-40 are expressed as means and error bars represent±s.d. Gray bars  show levels of hsCRP and YKL-40 at the preoperative baseline visit (Pre, n=20) and 3 months postoperatively (Post, n=20). White bars □ show baseline levels of hsCRP and YKL-40 in relation to the presence (+MS, n=13) or absence (−MS, n=7) of the metabolic syndrome. (a) *P=0.005. (b) *P=0.014. +MS, presence of the metabolic syndrome; −MS, absence of the metabolic syndrome.
show levels of hsCRP and YKL-40 at the preoperative baseline visit (Pre, n=20) and 3 months postoperatively (Post, n=20). White bars □ show baseline levels of hsCRP and YKL-40 in relation to the presence (+MS, n=13) or absence (−MS, n=7) of the metabolic syndrome. (a) *P=0.005. (b) *P=0.014. +MS, presence of the metabolic syndrome; −MS, absence of the metabolic syndrome.
Multiple regression analyses
The dependency of sCD36 as a function of truncal fat mass, triglycerides, leukocyte count and LF% was tested by multiple regression analysis, and the only independent predictor of sCD36 was triglycerides (β=0.500, P=0.001).
Discussion
In this study, we aimed to investigate the role of sCD36 in relation to obesity and its metabolic complications. To our knowledge, no previous studies have examined the effect of weight loss on the circulating levels of sCD36 in adults. Previous studies have documented that sCD36 was significantly elevated among obese and diabetic subjects, and that BMI has been shown to increase across sCD36 quartiles in a large healthy population.22, 24 The present study population consisted of morbidly obese adults undergoing bariatric surgery. Along with significant weight loss and improvements in metabolic disturbances, fat distribution, and hepatic fat accumulation, we observed a marked reduction in circulating sCD36. The levels of sCD36 were found to be associated with an unhealthy fat distribution as well as circulating levels of triglycerides. The findings are in line with the proposed important role of CD36 in the development of metabolic complications to obesity15, 23 and further support circulating sCD36 as a potential indicator of these complications.23, 24, 35
The pathogenesis underlying the adverse metabolic impacts of obesity is not fully understood. Low-grade inflammation and accumulation of ectopic fat in the arterial wall, as well as in the liver and muscles, which may lead to insulin resistance, seem to have an important role.8 Both an oversupply of FFA in the circulation and obesity-related low-grade inflammation are identified as important factors in the development of insulin resistance.13, 14, 36, 37 CD36 is important for increased fat uptake in the gut and accumulation in the liver.20, 38 The FFA in the circulation are derived from either lipoprotein particles containing large amounts of triglycerides (chylomicrons from the gut and very-low density lipoprotein particles from the liver) or from local lipolysis in adipose tissues.13 Compared with subcutaneous fat, visceral adipose tissue is highly metabolically active as well as more insulin resistant and thus less sensitive to the insulin mediated inhibition of lipolysis, resulting in high portal fatty acid fluxes to the liver.3, 37 The amount of truncal fat, measured by dual-energy X-ray absorptiometry-scan can, to some extent, be assumed to reflect the presence of the primary intraabdominally localized visceral adipose tissue, knowing that obese subjects present substantial amounts of subcutaneous fat in the region as well. The associations between triglycerides and fat mass, truncal fat mass as well as hepatic fat accumulation in this extremely obese study population, support the notion that overload of visceral fat cells is associated with increased levels of circulating triglycerides and ectopic fat accumulation,34 and this adverse effect of obesity could be affected in a positive direction by surgically induced weight loss. CD36 may be involved in this ectopic fat accumulation, as we, along with decreased sCD36 after weight loss and improvements in fat distribution, found correlations between sCD36 and circulating triglycerides, like previously shown.22, 24, 26 Furthermore, correlations between sCD36 and body fat, and notably sCD36 and the amount of truncal fat supported results from a study on patients with polycystic ovary syndrome,27 as well as the proposed role of sCD36 as a biomarker of the metabolic syndrome and its associated risks. Overall, high levels of sCD36 can be considered as reflecting a protective role of CD36 against elevated levels of circulating triglycerides, especially seen in relation to extensive amounts of lipolytic and metabolically active visceral adipose tissue, or considered as a result of a secondary and obesity-related metabolic process.
Another pivotal point is the low-grade inflammation related to the metabolic complications of obesity, and the pathogenesis of insulin resistance. The transcription of CD36 is linked to impaired insulin signaling in macrophages.39 In contrast to previous results,22, 24, 26, 27 this study demonstrated no associations between circulating sCD36 and insulin sensitivity, even though a 41% improvement in HOMA-%S was observed and that gastric bypass is known to improve insulin sensitivity within a few days after surgery.30, 31, 32 This lack of consistency may be due to the methods used to predict the sensitivity for insulin on the cellular level. Previous correlations between sCD36 and insulin sensitivity were based on the dynamic hyperinsulinemic euglycemic clamp technique, which is regarded as the golden standard of measuring insulin sensitivity, opposite the HOMA in the present study, an algorithm based on basal steady-state glucose and insulin or connecting peptide concentrations. Due to the method differences, measurements from two methods may not be directly comparable.40
The estimated hepatic fat accumulation decreased markedly after gastric bypass surgery and the subsequent weight loss. This is in line with,41 another study concerning bariatric surgery reporting a reduction in hepatic steatosis of around 50% measured by magnetic resonance imaging. In addition to correlations with anthropometric measurements, especially the amount of truncal fat, we found that LF% correlated to fasting plasma glucose, indicating that the ectopic hepatic fat accumulation is related to the presence of an unbalanced glucose homeostasis. The obesity-related overload of FFA in the circulation, particularly the increased portal flow, may exceed the metabolic capacity of the cells, resulting in accumulation of FFA and intermediates of the FFA-metabolism and in a negative impact on the insulin-signaling-pathway.37 Especially in the hepatocytes, the elevated FFA causes an increased synthesis of triglycerides, accumulation of toxic lipid products, a development of inflammatory conditions and hepatic insulin resistance, respectively. Therefore, this may result in an impaired insulin mediated inhibition of hepatic gluconeogenesis, lipogenesis and triglyceride secretion through very-low density lipoprotein production.42, 43 Diet-induced obesity and fatty acids exposure in rodents have been attributed to an increased cellular CD36 expression, and found to be associated with an increased secretion and storage of triglycerides.18, 19 In humans, the expression of CD36 is found to be significantly associated with both insulin resistance and the degree of steatosis.44 A direct association between sCD36 and LF% has previously been demonstrated in a large study of healthy individuals,24 and, additionally, sCD36 has been shown to be the most important predictor of liver steatosis determined by microscopy, in a study of patients with hepatitis C.25 The present findings of elevated sCD36 along with LF% in individuals with the metabolic syndrome support the importance of CD36 in the accumulation of hepatic fat, and the supposed potential of circulating sCD36 as a surrogate marker of complications to the metabolic syndrome, such as steatosis, diabetes35 and the risk of atherosclerosis.24, 45
In addition to the function as a fatty acid translocase, the expression of CD36 has previously been associated with adipose tissue inflammation, through the promotion of a proinflammatory cytokine expression, in a study regarding diet-induced obesity.21 Furthermore, an association between sCD36 and the inflammatory cytokine interleukin-6 has previously been reported.26 We measured the inflammatory markers hsCRP and YKL-40. hsCRP has previously been shown to be related to abdominal obesity and hsCRP as well as YKL-40 have been related to T2DM and insulin resistance.28, 46 No associations were found between sCD36 and hsCRP or YKL-40 in the present study. However, hsCRP levels decreased significantly following gastric bypass and weight loss, and in consistence with a previous study,46 strong correlations between hsCRP and anthropometric measurements, circulating lipids and insulin sensitivity were found. Conversely, the inflammatory biomarker YKL-40 was unaffected by weight loss, a finding which is in conflict with a previous, and almost similar study,47 where a 31% decrease in YKL-40 was observed after bariatric surgery and a mean follow-up of 17.4 months. However, only few details about the apparently in-house method used for YKL-40 measurement are given in this study, and thus lack of consistency among YKL-40 assays may partly account for the discrepant results. In addition, the follow-up period of 17.4 months may impact YKL-40 different from 3 months follow-up as in the present set-up. In addition, another study found that only diet-induced, but not surgically induced weight loss, resulted in a decrease of circulating YKL-40 levels,48 which supports our results in the present study. YKL-40 in relation to obesity has not previously been investigated in any great detail, and further studies are required to explain the role of this inflammatory biomarker in relation to obesity and weight loss. If the inflammatory markers as well as sCD36 were evaluated in participants with or without the metabolic syndrome, levels of YKL-40 were found to be significantly higher in the presence of the metabolic syndrome. Furthermore, the levels of sCD36 tended to be higher in participants with the metabolic syndrome, whereas no differences of hsCRP levels were found. This might indicate that hsCRP levels reflect a state of systemic subclinical inflammation, which is not necessarily linked to the metabolic syndrome, as opposed to the levels of sCD36 and YKL-40, which, to a larger extent, reflect the metabolic disturbances at different levels and the resulting metabolic morbidity.
A weakness of this study is the small sample size, which increases the risk of type 2 error and may explain the borderline significant results and the lack of consistency to previous studies. Due to the weight loss before surgery, the participants were already in a catabolic state at the time of inclusion, which may lead to an underestimation of the metabolic effects related to weight loss. LF% is based on an algorithm predicting liver fat content as measured by magnetic resonance imaging. However, this algorithm only predicts half of the variability in magnetic resonance imaging measured liver fat,33 and more reliable results would have been achieved by magnetic resonance imaging or by direct histological measurement of liver cell fat content in liver biopsies.
For the first time, we reported decreasing levels of sCD36 following bariatric surgery, along with weight-loss-related metabolic improvements, including improvements in fat distribution and ectopic hepatic fat accumulation. Despite associations between sCD36 and an unhealthy fat distribution, triglycerides were the only independent predictor of sCD36, indicating a relation to the obesity-related dyslipidemia. The results of our study support the proposed role of the membrane receptor CD36 in the development of some of the complications to diet-induced obesity, and with circulating sCD36 as a measurable biochemical marker of these complications. Our results must be verified in larger study populations, and experimental studies are needed to further determine the mechanisms and roles of sCD36 in the development of obesity-related complications.
Acknowledgments
We wish to thank the skillful laboratory assistance of Ulla Kjærulff-Hansen and Hanne Dorthe Mogensen, Endocrine Research Lab, Copenhagen University Hospital Herlev, Denmark as well as Lone Larsen, Clinical Institute, Aarhus University Hospital. Furthermore, we want to thank Morten H Nielsen, Department of Clinical Biochemistry, Aalborg University Hospital, for assistance in preparation of figures. The study was supported by grants from The Research Foundation of Herlev Hospital, The Danish Council for Independent Research, Medical Sciences (FSS), the Novo Nordisk Insulin Foundation and the Obel Family Foundation.
A Handberg is the inventor of two patent applications on sCD36 as a biomarker of the metabolic syndrome. The patent IP rights are owned by the Idea's Clinic of Aalborg University Hospital. The remaining authors declare no conflict of interest.
References
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, et al. Body weight and mortality among women. N Engl J Med. 1995;333:677–685. doi: 10.1056/NEJM199509143331101. [DOI] [PubMed] [Google Scholar]
- Obesity: preventing and managing the global epidemic. Report of a WHO consultation World Health Organ Tech Rep Ser 2000894i–xii., 1-253. [PubMed] [Google Scholar]
- Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345:790–797. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–1609. doi: 10.1053/j.gastro.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients. 2013;5:1544–1560. doi: 10.3390/nu5051544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snel M, Jonker JT, Schoones J, Lamb H, de Roos A, Pijl H, et al. Ectopic fat and insulin resistance: pathophysiology and effect of diet and lifestyle interventions. Int J Endocrinol. 2012;2012:983814. doi: 10.1155/2012/983814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259:87–91. doi: 10.1126/science.7678183. [DOI] [PubMed] [Google Scholar]
- Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest. 2006;116:1793–1801. doi: 10.1172/JCI29069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickup JC. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care. 2004;27:813–823. doi: 10.2337/diacare.27.3.813. [DOI] [PubMed] [Google Scholar]
- Ye J. Emerging role of adipose tissue hypoxia in obesity and insulin resistance. Int J Obes (Lond) 2009;33:54–66. doi: 10.1038/ijo.2008.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klop B, Elte JW, Cabezas MC. Dyslipidemia in obesity: mechanisms and potential targets. Nutrients. 2013;5:1218–1240. doi: 10.3390/nu5041218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden G. Obesity, insulin resistance and free fatty acids. Curr Opin Endocrinol Diabetes Obes. 2011;18:139–143. doi: 10.1097/MED.0b013e3283444b09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Love-Gregory L, Abumrad NA. CD36 genetics and the metabolic complications of obesity. Curr Opin Clin Nutr Metab Care. 2011;14:527–534. doi: 10.1097/MCO.0b013e32834bbac9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou D, Samovski D, Okunade AL, Stahl PD, Abumrad NA, Su X. CD36 level and trafficking are determinants of lipolysis in adipocytes. FASEB J. 2012;26:4733–4742. doi: 10.1096/fj.12-206862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastie CC, Hajri T, Drover VA, Grimaldi PA, Abumrad NA. CD36 in myocytes channels fatty acids to a lipase-accessible triglyceride pool that is related to cell lipid and insulin responsiveness. Diabetes. 2004;53:2209–2216. doi: 10.2337/diabetes.53.9.2209. [DOI] [PubMed] [Google Scholar]
- Koonen DP, Jacobs RL, Febbraio M, Young ME, Soltys CL, Ong H, et al. Increased hepatic CD36 expression contributes to dyslipidemia associated with diet-induced obesity. Diabetes. 2007;56:2863–2871. doi: 10.2337/db07-0907. [DOI] [PubMed] [Google Scholar]
- Chabowski A, Zendzian-Piotrowska M, Konstantynowicz K, Pankiewicz W, Miklosz A, Lukaszuk B, et al. Fatty acid transporters involved in the palmitate and oleate induced insulin resistance in primary rat hepatocytes. Acta Physiol (Oxf) 2013;207:346–357. doi: 10.1111/apha.12022. [DOI] [PubMed] [Google Scholar]
- Abumrad NA, Davidson NO. Role of the gut in lipid homeostasis. Physiol Rev. 2012;92:1061–1085. doi: 10.1152/physrev.00019.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai L, Wang Z, Ji A, Meyer JM, van der Westhuyzen DR. Scavenger receptor CD36 expression contributes to adipose tissue inflammation and cell death in diet-induced obesity. PLoS One. 2012;7:e36785. doi: 10.1371/journal.pone.0036785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handberg A, Levin K, Hojlund K, Beck-Nielsen H. Identification of the oxidized low-density lipoprotein scavenger receptor CD36 in plasma: a novel marker of insulin resistance. Circulation. 2006;114:1169–1176. doi: 10.1161/CIRCULATIONAHA.106.626135. [DOI] [PubMed] [Google Scholar]
- Koonen DP, Jensen MK, Handberg A. Soluble CD36- a marker of the (pathophysiological) role of CD36 in the metabolic syndrome. Arch Physiol Biochem. 2011;117:57–63. doi: 10.3109/13813455.2010.543136. [DOI] [PubMed] [Google Scholar]
- Handberg A, Hojlund K, Gastaldelli A, Flyvbjerg A, Dekker JM, Petrie J, et al. Plasma sCD36 is associated with markers of atherosclerosis, insulin resistance and fatty liver in a nondiabetic healthy population. J Intern Med. 2012;271:294–304. doi: 10.1111/j.1365-2796.2011.02442.x. [DOI] [PubMed] [Google Scholar]
- Petta S, Handberg A, Marchesini G, Camma C, Di Marco V, Cabibi D, et al. High sCD36 plasma level is associated with steatosis and its severity in patients with genotype 1 chronic hepatitis C. J Viral Hepat. 2013;20:174–182. doi: 10.1111/j.1365-2893.2012.01641.x. [DOI] [PubMed] [Google Scholar]
- Handberg A, Lopez-Bermejo A, Bassols J, Vendrell J, Ricart W, Fernandez-Real JM. Circulating soluble CD36 is associated with glucose metabolism and interleukin-6 in glucose-intolerant men. Diab Vasc Dis Res. 2009;6:15–20. doi: 10.3132/dvdr.2009.003. [DOI] [PubMed] [Google Scholar]
- Glintborg D, Hojlund K, Andersen M, Henriksen JE, Beck-Nielsen H, Handberg A. Soluble CD36 and risk markers of insulin resistance and atherosclerosis are elevated in polycystic ovary syndrome and significantly reduced during pioglitazone treatment. Diabetes Care. 2008;31:328–334. doi: 10.2337/dc07-1424. [DOI] [PubMed] [Google Scholar]
- Brooks GC, Blaha MJ, Blumenthal RS. Relation of C-reactive protein to abdominal adiposity. Am J Cardiol. 2010;106:56–61. doi: 10.1016/j.amjcard.2010.02.017. [DOI] [PubMed] [Google Scholar]
- Rathcke CN, Vestergaard H. YKL-40—an emerging biomarker in cardiovascular disease and diabetes. Cardiovasc Diabetol. 2009;8:61. doi: 10.1186/1475-2840-8-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirksen C, Jorgensen NB, Bojsen-Moller KN, Jacobsen SH, Hansen DL, Worm D, et al. Mechanisms of improved glycaemic control after Roux-en-Y gastric bypass. Diabetologia. 2012;55:1890–1901. doi: 10.1007/s00125-012-2556-7. [DOI] [PubMed] [Google Scholar]
- Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis Am J Med 2009122248–256.e5. [DOI] [PubMed] [Google Scholar]
- Falken Y, Hellstrom PM, Holst JJ, Naslund E. Changes in glucose homeostasis after Roux-en-Y gastric bypass surgery for obesity at day three, two months, and one year after surgery: role of gut peptides. J Clin Endocrinol Metab. 2011;96:2227–2235. doi: 10.1210/jc.2010-2876. [DOI] [PubMed] [Google Scholar]
- Kotronen A, Peltonen M, Hakkarainen A, Sevastianova K, Bergholm R, Johansson LM, et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology. 2009;137:865–872. doi: 10.1053/j.gastro.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Miller M, Stone NJ, Ballantyne C, Bittner V, Criqui MH, Ginsberg HN, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–2333. doi: 10.1161/CIR.0b013e3182160726. [DOI] [PubMed] [Google Scholar]
- Handberg A, Norberg M, Stenlund H, Hallmans G, Attermann J, Eriksson JW. Soluble CD36 (sCD36) clusters with markers of insulin resistance, and high sCD36 is associated with increased type 2 diabetes risk. J Clin Endocrinol Metab. 2010;95:1939–1946. doi: 10.1210/jc.2009-2002. [DOI] [PubMed] [Google Scholar]
- Berzigotti A, Abraldes JG. Impact of obesity and insulin-resistance on cirrhosis and portal hypertension. Gastroenterol Hepatol. 2013;36:527–533. doi: 10.1016/j.gastrohep.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Capurso C, Capurso A. From excess adiposity to insulin resistance: the role of free fatty acids. Vascul Pharmacol. 2012;57:91–97. doi: 10.1016/j.vph.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Nauli AM, Nassir F, Zheng S, Yang Q, Lo CM, Vonlehmden SB, et al. CD36 is important for chylomicron formation and secretion and may mediate cholesterol uptake in the proximal intestine. Gastroenterology. 2006;131:1197–1207. doi: 10.1053/j.gastro.2006.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang CP, Han S, Okamoto H, Carnemolla R, Tabas I, Accili D, et al. Increased CD36 protein as a response to defective insulin signaling in macrophages. J Clin Invest. 2004;113:764–773. doi: 10.1172/JCI19528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- van Werven JR, Schreuder TC, Aarts EO, Nederveen AJ, Meijer JW, Berends FJ, et al. Hepatic steatosis in morbidly obese patients undergoing gastric bypass surgery: assessment with open-system 1 H-MR spectroscopy. AJR American journal of roentgenology. 2011;196:W736–W742. doi: 10.2214/AJR.10.5215. [DOI] [PubMed] [Google Scholar]
- Lomonaco R, Ortiz-Lopez C, Orsak B, Webb A, Hardies J, Darland C, et al. Effect of adipose tissue insulin resistance on metabolic parameters and liver histology in obese patients with nonalcoholic fatty liver disease. Hepatology. 2012;55:1389–1397. doi: 10.1002/hep.25539. [DOI] [PubMed] [Google Scholar]
- Yki-Jarvinen H. Liver fat in the pathogenesis of insulin resistance and type 2 diabetes. Dig Dis. 2010;28:203–209. doi: 10.1159/000282087. [DOI] [PubMed] [Google Scholar]
- Miquilena-Colina ME, Lima-Cabello E, Sanchez-Campos S, Garcia-Mediavilla MV, Fernandez-Bermejo M, Lozano-Rodriguez T, et al. Hepatic fatty acid translocase CD36 upregulation is associated with insulin resistance, hyperinsulinaemia and increased steatosis in non-alcoholic steatohepatitis and chronic hepatitis C. Gut. 2011;60:1394–1402. doi: 10.1136/gut.2010.222844. [DOI] [PubMed] [Google Scholar]
- Handberg A, Skjelland M, Michelsen AE, Sagen EL, Krohg-Sorensen K, Russell D, et al. Soluble CD36 in plasma is increased in patients with symptomatic atherosclerotic carotid plaques and is related to plaque instability. Stroke. 2008;39:3092–3095. doi: 10.1161/STROKEAHA.108.517128. [DOI] [PubMed] [Google Scholar]
- Rathcke CN, Johansen JS, Vestergaard H. YKL-40 a biomarker of inflammation, is elevated in patients with type 2 diabetes and is related to insulin resistance. Inflamm Res. 2006;55:53–59. doi: 10.1007/s00011-005-0010-8. [DOI] [PubMed] [Google Scholar]
- Hempen M, Kopp HP, Elhenicky M, Hobaus C, Brix JM, Koppensteiner R, et al. YKL-40 is elevated in morbidly obese patients and declines after weight loss. Obes Surg. 2009;19:1557–1563. doi: 10.1007/s11695-009-9917-4. [DOI] [PubMed] [Google Scholar]
- Catalan V, Gomez-Ambrosi J, Rodriguez A, Ramirez B, Rotellar F, Valenti V, et al. Increased circulating and visceral adipose tissue expression levels of YKL-40 in obesity-associated type 2 diabetes are related to inflammation: impact of conventional weight loss and gastric bypass. J Clin Endocrinol Metab. 2011;96:200–209. doi: 10.1210/jc.2010-0994. [DOI] [PubMed] [Google Scholar]