Abstract
The depletion of tumor stromal cells that are marked by their expression of the membrane protein fibroblast activation protein-α (FAP) overcomes immune suppression and allows an anti-cancer cell immune response to control tumor growth. In subcutaneous tumors established with immunogenic Lewis lung carcinoma cells expressing ovalbumin (LL2/OVA), the FAP+ population comprises CD45+ and CD45− cells. In the present study, we further characterize the tumoral FAP+/CD45+ population as a minor sub-population of F4/80hi/CCR2+/CD206+ M2 macrophages. Using bone marrow chimeric mice in which the primate diphtheria toxin receptor (DTR) is restricted either to the FAP+/CD45+ or to the FAP+/CD45− subset, we demonstrate by conditionally depleting each subset that both independently contribute to the immune suppressive tumor microenvironment. A basis for the function of the FAP+/CD45+ subset is shown to be the immune inhibitory enzyme, heme oxygenase-1 (HO-1). The FAP+/CD45+ cells are the major tumoral source of HO-1, and an inhibitor of HO-1, Sn mesoporphyrin, causes the same extent of immune-dependent arrest of LL2/OVA tumor growth as does the depletion of these cells. Since this observation of immune suppression by HO-1 expressed by the FAP+/CD45+ stromal cell is replicated in a transplanted model of pancreatic ductal adenocarcinoma, we conclude that pharmacologically targeting this enzyme may improve cancer immunotherapy.
Keywords: FAP, macrophage, tumor, immunity, heme oxygenase-1
Introduction
The failure of the immune system to control the growth of immunogenic cancers has been ascribed to two general processes: cancer immunoediting and immune suppression. Immunoediting has been demonstrated in models of autochthonous soft tissue sarcomas induced either by a mutagenic agent, methylcholanthrene (1), or by tissue-specific, Cre/LoxP-regulated expression of oncogenic K-rasG12D and deletion of p53 (2). Tumoral immune suppression has been shown in models of transplanted, ectopic tumors (3), and recently in an autochthonous model of lung adenocarcinoma (4). In relation to immune suppression, progress has been made in the clinic with the introduction of therapeutic antibodies to CTLA-4, PD-1, and PD-L1 that antagonize immune checkpoints (5-7). However as a high frequency of patients do not respond to these therapeutic antibodies, it is appropriate to continue studies of the tumoral stromal cells that have immune suppressive function, including the cell that is identified by its expression of the membrane dipeptidyl dipeptidase, fibroblast activation protein-α (FAP) (8).
FAP+ stromal cells were first demonstrated in human adenocarcinomas, and subsequently were found in various non-neoplastic, chronic inflammatory lesions (9, 10). Recently, in a genetically modified mouse model in which FAP+ cells express the primate diphtheria toxin receptor (DTR), the conditional depletion of these cells from an established, immunogenic, transplanted tumor caused its growth arrest. The control of tumor growth induced by depleting FAP+ cells depended on adaptive immunity, but did not involve enhanced priming of the CD8+ T cells, leading to the conclusion that FAP+ stromal cells suppressed the function of effector T cells in the tumor microenvironment (8).
Understanding the means of immune suppression by tumoral FAP+ stromal cells is especially challenging because two subtypes occur, a CD45− mesenchymal population and a hematopoietic subset that is CD45+/CD11b+/Gr-1− (8). The present study focuses on the FAP+/CD45+ tumoral cells, demonstrating that they are a subset of inflammatory macrophages with an M2 phenotype that mediate immune suppression by their expression of HO-1.
Material and Methods
Mice
FAP/enhanced green fluorescent protein (EGFP) bacterial artificial chromosome (BAC) transgenic (Tg) and FAP/DTR BAC Tg mice have previously been described (8). C57BL/6-Ly5.1 (CD45.1) mice, C57BL/6 Rag2−/−, and C57BL/6 (CD45.2) (The Jackson Laboratory) were used as indicated. The use of animals was approved by the Ethical Review Committee at the University of Cambridge and the Home Office, UK.
Subcutaneous tumor studies and HO inhibition
Lewis lung carcinoma (LL2)/Thy1.1, LL2/Thy1.1-ovalbumin (OVA) (original line purchased from ATCC), and PDA (11381, D. Tuveson, CRUK Cambridge Institute) were injected into mice, and the subsequent tumors measured as previously described (8). Sn (IV) mesoporphyrin IX dichloride (SnMP) (Frontier Scientific) was dissolved in 0.1M NaOH, and diluted using 0.1M NaHCO3, pH7. For blocking interferon-gamma (IFN-γ) and tumor necrosis factor-alpha (TNF-α), mice were injected intraperitoneally (I.P.) at day -1 and 0, relative to SnMP administration, with 12.5 μg/g anti-IFN-γ (XMG1.2) and 10 μg/g anti-TNF-α (MP6-XT3) or 22.5 μg/g non-immune IgG (eBRG1) (eBioscience). Tumor tissue was enzyme-digested to release single cells as previously described (8).
Flow cytometry
Antibodies were purchased from eBioscience unless otherwise stated, the following antibodies were used: CCR2 (R&D Systems), CD3 (145-2C11), CD4 (RM4-5), CD8β (eBioH35-17.2), CD11b (M1/70), CD11c (N418), CD14 (Sa2-8), CD16/32 (93), CD31 (390), CD45 (30-F11), CD45.1 (Biolegend, A20), CD45.2 (Biolegend, 104), CD69 (H1.2F3), F4/80 (BM8), Gr-1 (RB6-8C5), LAMP-1 (eBio1D4B), MHCII (M5/114.15), Thy1.2 (53-2.1). Anti-mannose receptor (CD206) (R&D Systems) was fluorescently conjugated using the Alexa Fluor® 488 antibody labeling kit (Invitrogen) prior to use. Fc receptors were blocked using anti-CD16/32 (BD Bioscience, 2.4G2). Foxp3+ CD4 T cells were stained using the Mouse Regulatory T cell staining kit (eBioscience) according to the manufacturer’s protocol. FAP+ cells were stained as previously described (8). Tissue factor-expressing cells were stained with goat anti-tissue factor (R&D Systems) and detected as described for FAP staining (8). Dead cells were excluded using 7-amino actinomycin D (7-AAD) (Calbiochem). Data were collected using a BD LSR II cytometer and analyzed using FlowJo software (Treestar Inc.).
Bone marrow chimeras
Bone marrow cells were flushed from the femurs and tibias of male FAP/DTR BAC Tg (CD45.2) or C57BL/6-Ly5.1 (CD45.1) mice and stained for FAP as previously described in PBS, 1% FCS (8). The streptavidin was Phycoerythrin (PE)-conjugated (eBioscience). Bone marrow cells were depleted of FAP-expressing cells using anti-PE Microbeads (Miltenyi Biotech) on LD columns according to manufacturer’s protocol to prevent transfer of any donor CD45− FAP+ cells present in the bone marrow. FAP-depleted bone marrow cells (10×106) were transferred via tail vein injection into recipient female mice, which had been lethally irradiated using a Cesium-137 source irradiator with 2 doses of 6 Gy, 3 hr apart. After 16 weeks, when the bone marrow had reconstituted, LL2/OVA cells were injected. FAP+ cells expressing the FAP/DTR BAC transgene were ablated through the administration of DTX (List Biologicals) at 25ng/g/24 hr via I.P. injection.
Immunofluorescence
Frozen OCT-embedded tumor tissue, which were grown in FAP/EGFP BAC Tg mice, were sectioned and stained as previously described for the preservation of native GFP fluorescence (8). The following antibodies were used; rat anti-F4/80 (AbD Serotec, CI:A3-1), rabbit anti-HO-1 (Insight Biotechnology, EP1391Y) and these were detected using NL637 goat anti-rat IgG (R&D Systems) and Alexa Fluor-546 donkey anti-rabbit IgG (Invitrogen). Nuclei were stained using 4′,6-diamidino-2-phenylindole dihydrochloride (DAPI) (Invitrogen). Images were acquired using a Leica SP2 confocal microscope and associated LCS analysis software.
qRT PCR analysis
mRNA from tumor tissue and sorted cells was extracted using the Absolutely RNA® Miniprep Kit (Agilent Technologies). mRNA from sorted populations was amplified using the Transplex® Complete whole transcriptome amplification kit (Sigma-Aldrich), and subsequent cDNA purified using a PCR Purification Kit (Qiagen) according to the manufacturer’s protocols. qRT PCR was performed as previously described using the SuperScript® III Platinum® One-step qRT-PCR system (Invitrogen) (8). The following primer/probes (Applied Biosystems) were used; HO-1 mm00516006_m1, HO-2 mm00468922_m1, IFN-γ mm99999071_m1, Tbp mm01277045_m1, TNF-α mm99999068_m1.
Statistical analyzes
Statistical analysis of tumor growth rates was performed using the ‘CompareGrowthCurves’ function of the statmod software package (11). For comparing treatment groups, a Mann Whitney U test was used when n was <6 and a two-tailed Student’s T test when n was ≥ 6 and greater using GraphPad Prism 6 software.
Results and Discussion
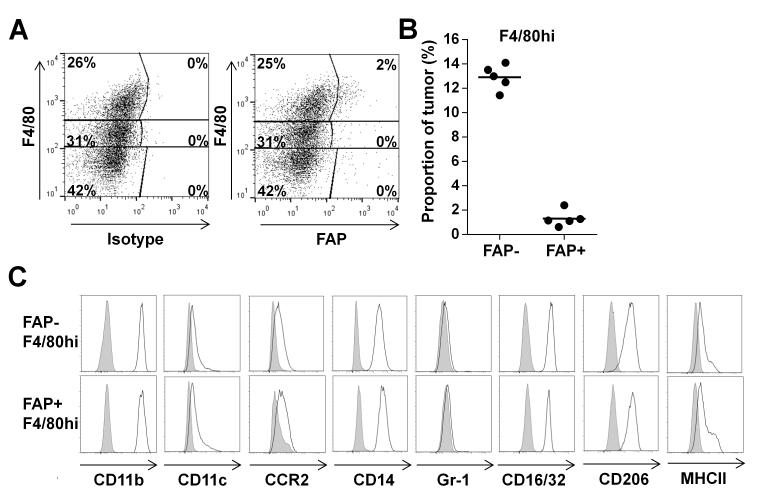
The present study was prompted by the recent finding that stromal cells expressing the membrane protein, FAP, mediate immune suppression in immunogenic transplanted tumors established with the LL2/OVA cancer cell line (8). Since this report showed that the population of tumoral FAP+ cells comprised CD45+ and CD45− subsets, this first follow-up study addresses the important aim of defining their respective immune suppressive functions. To characterize the hematopoietic FAP+ stromal cell, which was equally prevalent in LL2 and LL2/OVA tumors (Supplementary Fig. S1), single cell suspensions derived from subcutaneous LL2/OVA tumors were subjected to flow cytometry analysis after staining with antibodies specific for CD45, F4/80 and FAP. All FAP+/CD45+ cells were present in the F4/80hi population (Fig. 1A), and comprised a mean of 1.3 ± 0.7% of all tumoral cells and approximately 10% of all F4/80hi cells (Fig. 1B). The cell surface phenotype of the FAP+/F4/80hi subset did not differ from that of FAP−/F4/80hi cells, in that all were CCR2+, CD11b+, CD11clo, CD14+, CD16/32+, Gr-1−, MHCIIlo and CD206+ (mannose receptor) (Fig. 1C). The absence of Gr-1 excluded their identity as MDSCs (12), and the expression of CD14 indicated that they were not fibrocytes (13) (Fig. 1 C). Thus, FAP is expressed by a minor proportion of tumoral macrophages that has an inflammatory M2 phenotype, being CCR2+, MHCIIlo, CD11clo, and CD206+ (Fig. 1C).
Figure 1.
FAP expression by tumoral CD45+ cells marks a subpopulation of F4/80hi macrophages. A, A representative FACS dot plot of gated CD45+ cells from a single cell suspension of an LL2/OVA tumor stained with the additional antibodies shown. B, The proportion of cells in five LL2/OVA tumors that were F4/80hi and either FAP+ or FAP−. C, FACS histograms of gated tumoral FAP+ and FAP− F4/80hi cells stained with the specific antibodies shown (open) and isotype controls (Shaded).
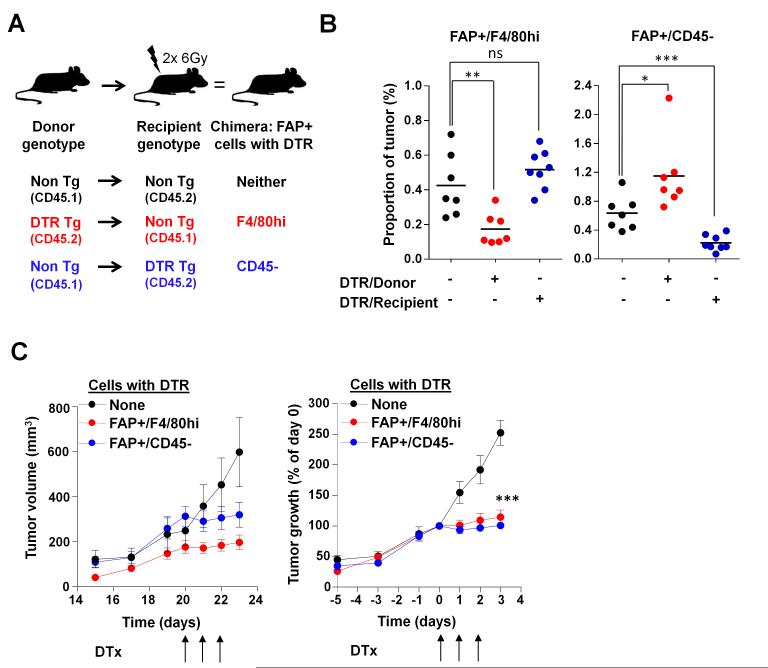
To determine whether this FAP+ subset of tumoral F4/80hi macrophages had immune suppressive function, we generated bone marrow chimeric mice by adoptively transferring male bone marrow from C57BL/6-Ly5.1 or FAP/DTR BAC Tg mice that had been depleted of FAP+ cells into lethally-irradiated female recipients that were either C57BL/6-Ly5.1, C57BL/6 (CD45.2) or FAP/DTR BAC Tg (Fig 2A). In the resulting chimeric mice, peripheral blood leukocytes were always of at least 95% donor origin (Supplementary Fig. S2). The recipient origin of FAP+/CD45− cells in tumors was verified by a lack of the Y chromosome (data not shown). The bone marrow chimeric mice were challenged by subcutaneous injection of LL2/OVA cells. When tumors were established, mice were given DTX for three consecutive days, which led to the depletion of only the DTR-expressing subset of tumoral FAP+ cells (Fig. 2B). At the initiation of DTX there was no statistically significant difference in the tumor sizes between the non-Tg control and either DTR chimeric group (p>0.05) (Supplementary Fig. S3). However, thereafter there was slowing of tumor growth in both types of chimeric mice, but not in mice lacking the expression of DTR in either FAP+ subset (Fig. 2C). Therefore, FAP+ cells of both hematopoietic and mesenchymal origin have immune suppressive function, and, in this tumor model, both are required for tumor immune protection.
Figure 2.
The selective depletion of DTR-expressing FAP+/CD45+ and FAP+/CD45− tumoral cells from bone marrow chimeric mice by the administration of DTX. A, Sketch depicting the donor-recipient combinations for generating the chimeric mice. B, The proportions of each of the two subsets of FAP+ cells in LL2/OVA tumors in individual bone marrow chimeric mice that had received DTX for three consecutive days. C, The tumor volumes (left) and the calculated percent change in growth (right) of LL2/OVA tumors in the groups of bone marrow chimeric mice that were given DTX for three consecutive days. ns- not significant, * p<0.05, ** p<0.01, *** p<0.001.
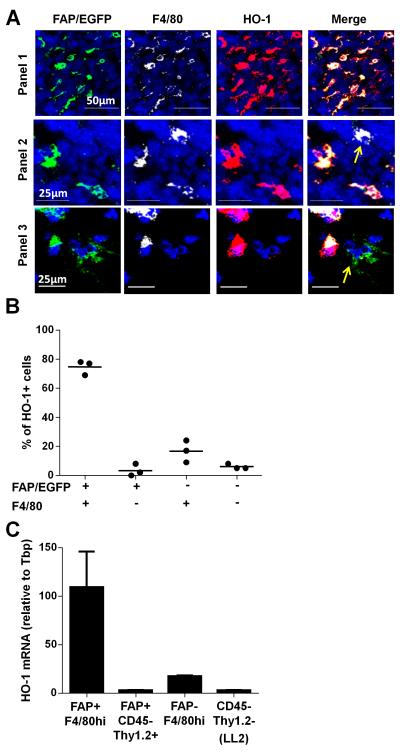
Having determined that the FAP+/F4/80hi stromal cells were capable of immune suppression in the LL2/OVA tumor, we sought a mechanism for this function. The findings of an association of the immunomodulatory enzyme, HO-1, with M2 macrophages (14), and of the M2 phenotype of the FAP+/F4/80hi tumoral cells (Fig. 1C) suggested the possibility that HO-1 may be involved in this process. Indeed FAP+/F4/80+ cells could be found expressing HO-1 in frozen sections from the tumors grown in the bone marrow chimeric mice lacking the expression of DTR in either FAP+ subset (Supplementary Fig. S4). The FAP+/F4/80+ cells, although distributed throughout the tumor, tended to be localized towards the tumor periphery. To evaluate the relative contribution of FAP+ F4/80+ cells to total tumoral HO-1, LL2 cells were implanted in FAP/EGFP BAC Tg mice in which FAP+ cells expressed EGFP, and frozen sections of the subsequent tumors were assessed by confocal microscopy for EGFP fluorescence, and expression of F4/80 and HO-1 (Fig. 3A). Across three tumors, 75 ± 4.9% of the HO-1-expressing tumoral cells were double positive for EGFP and F4/80 (Fig. 3B). Moreover, HO-1 mRNA was chiefly detected in FACS sort-purified FAP+/F4/80hi cells (Fig. 3C). Therefore, the FAP+/F4/80+ stromal cell comprised the majority of HO-1-expressing cells in the LL2 tumor. It should be noted that there was comparatively little expression of the closely-related enzyme HO-2 in LL2/OVA tumors compared to HO-1 (Supplementary Fig.S5).
Figure 3.
Expression of HO-1 by the FAP+/F4/80+ tumoral macrophages. A, Frozen sections of LL2 tumors from FAP/EGFP BAC Tg mice in which FAP+ cells are identified by native EGFP fluorescence (green) were also stained with DAPI (blue) and antibodies specific for F4/80 (white) and HO-1 (red). B, Randomly selected HO-1+ cells across multiple sections and fields were evaluated in three separate LL2 tumors for co-expression of FAP/EGFP and F4/80 (>300 total HO-1+ events were characterized). C, Relative HO-1 mRNA expression in sub-populations of FACS-sorted tumoral populations from an LL2/OVA tumor.
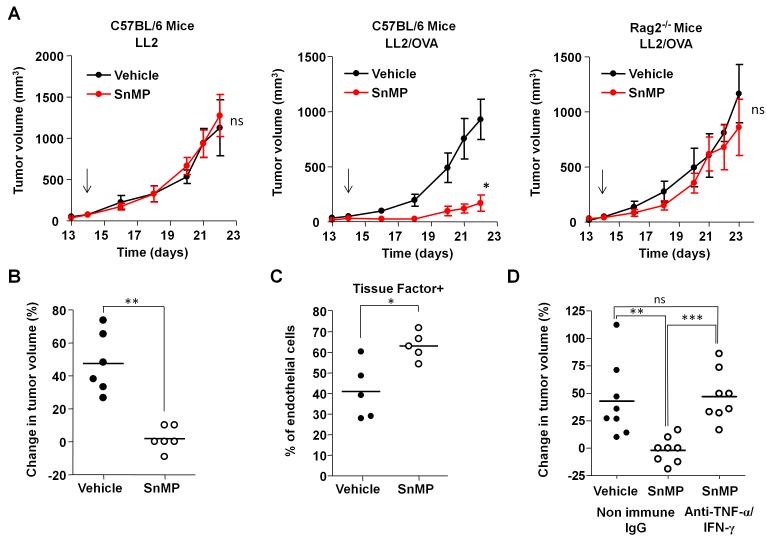
To determine whether the expression of HO-1 by the tumoral FAP+/F4/80hi macrophages contributed to their immune suppressive function, C57BL/6 mice bearing established non-immunogenic LL2 or immunogenic LL2/OVA tumors were treated with SnMP, a specific inhibitor of HO that has no identified off-target effects or toxicities. A response to a porphyrin-related inhibitor of HO-1, the most selective of which is SnMP, has been considered to be indicative of the role of this enzyme in a biological process (15-20). Whilst inhibition of HO using SnMP did not affect the growth rate of the LL2 tumors (Fig. 4A), it significantly slowed the growth of immunogenic LL2/OVA tumors, with this response occurring as early as 24 hr after the initiation of the treatment (Fig. 4A). The effect of SnMP on the growth of the LL2/OVA tumor was confirmed to be immune-mediated, since the inhibitor had no effect on the growth of LL2/OVA tumors in Rag2−/− mice (Fig. 4A).
Figure 4.
Effect of inhibiting HO-1 on adaptive immune- and cytokine-dependent regulation of tumor growth. A, C57BL/6 mice bearing established, non-immunogenic LL2 or immunogenic LL2/OVA tumors, and Rag2−/− mice with LL2/OVA tumors were treated with daily administration of SnMP (25μMol/Kg) or vehicle control, with the arrow denoting the initiation of treatment. B and C, Mice bearing established LL2/OVA tumors were treated with SnMP (25μMol/Kg) or vehicle for 24 hr after which the change in tumor volumes (B) and the expression of TF by CD31+ endothelial cells were measured (C). D, Mice bearing LL2/OVA tumors that had been pre-treated with neutralizing anti-TNF-α and anti-IFN-γ antibodies or with isotype control antibody were given SnMP (25μMol/Kg) or vehicle, and tumor volumes were measured 24 hr later. The curves describing tumor growth in (A) were compared for differences using the “CompareGrowthCurves” permutation test. ns- not significant, * p<0.05, ** p<0.01, *** p<0.001.
A subcutaneous tumor established with a cell line derived from an autochthonous pancreatic ductal adenocarcinoma (PDA) also demonstrated the occurrence of FAP+/F4/80+/HO-1+ stromal cells (Supplementary Fig. S6A). Inhibition of HO-1 by the administration of SnMP to C57BL/6 mice bearing established PDA tumors, which induce an immune response to an unknown antigen(s), slowed tumor growth by a mechanism that was immune-mediated, as demonstrated by the absence of tumor control in SnMP-treated Rag2−/− mice bearing subcutaneous PDA tumors (Supplementary Fig. S6B and C).
The acute cessation of LL2/OVA growth induced by SnMP (Fig.4B) was not associated with a change in the immune cell composition of the tumors (Supplementary Fig. S7A) or with an increase in the activation state of the tumoral CD8 T cells, as assessed by CD69 and Lamp-1 expression (Supplementary Fig. S7B). Immune control induced by SnMP did correlate with an increase in activated tumoral CD31+ tissue factor+ (TF, coagulation factor III, CD142) endothelial cells (Fig. 4B). The T cell cytokines, TNF-α and IFN-γ, act synergistically to activate endothelial cells (21). Since SnMP did not alter the mRNA levels of IFN-γ and TNF-α in the LL2/OVA tumors (Supplementary Fig. S8), inhibition of HO-1 may have sensitized endothelial cells to these cytokines. For example, one of the products of HO-1, carbon monoxide, suppresses the pro-apoptotic effects of TNF-α on endothelial cells (22). To address this possibility, mice bearing LL2/OVA tumors were treated with neutralizing antibodies to IFN-γ and TNF-α and then treated with SnMP. In the presence of these anti-cytokine antibodies, SnMP did not arrest the growth of LL2/OVA tumors (Fig. 4D), consistent with the activity of HO-1 in the tumor microenvironment being related to suppressing the response of endothelial cells to these cytokines.
Of the many studies of HO-1 and inflammation, perhaps the most relevant to the current findings are those demonstrating the ability of this enzyme and its product, carbon monoxide, to suppress rejection of allografts in rodent transplantation models (23). Although this earlier study did not determine which cells expressed HO-1, the present finding that HO-1 is predominantly expressed by tumoral FAP+/F4/80hi cells, when coupled with the demonstration of their immune suppressive function, is consistent with the theme that the host response to cancers involves tissue-protective processes that occur in other biological settings. Whilst the molecular basis for the immune suppression that is mediated by the mesenchymal FAP+/CD45− stromal cell remains to be determined, the present findings suggest that SnMP, which has been given to humans to inhibit heme oxygenases (19), may have clinical efficacy in overcoming tumoral immune suppression when HO-1-expressing stromal cells are found to be present.
Supplementary Material
Acknowledgements
The authors would like to acknowledge Dr Alice Denton for tail vein injections of mice, Dr Brian Huntly for supplying the C57BL/6-Ly5.1 mice (University of Cambridge), Mr Loic Tauzin for cell sorting, Dr Stefanie Reichelt and Dr Alexander Schreiner for advice on confocal microscopy analyses (CRUK Cambridge Institute), and Mr John Cruise for the preparation of tumor tissue mRNA.
Grant Support This research was supported by the Wellcome Trust, the Ludwig Institute for Cancer Research, and the Anthony Cerami and Anne Dunne Foundation for World Health. JNA was supported by the Irvington Institute Fellowship Program of the Cancer Research Institute, USA.
Financial Support: DTF: Wellcome Trust (1), the Anthony Cerami and Anne Dunne Foundation for World Health (1), and the Ludwig Institute for Cancer Research (1). JNA: Cancer Research Institute, USA (1).
Footnotes
Conflicts of Interest: No potential conflicts of interest were disclosed.
References
- 1.Matsushita H, Vesely MD, Koboldt DC, Rickert CG, Uppaluri R, Magrini VJ, et al. Cancer exome analysis reveals a T-cell-dependent mechanism of cancer immunoediting. Nature. 2012;482:400–4. doi: 10.1038/nature10755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DuPage M, Mazumdar C, Schmidt LM, Cheung AF, Jacks T. Expression of tumour-specific antigens underlies cancer immunoediting. Nature. 2012;482:405–9. doi: 10.1038/nature10803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yu P, Rowley DA, Fu YX, Schreiber H. The role of stroma in immune recognition and destruction of well-established solid tumors. Current Opinion in Immunology. 2006;18:226–31. doi: 10.1016/j.coi.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 4.DuPage M, Cheung AF, Mazumdar C, Winslow MM, Bronson R, Schmidt LM, et al. Endogenous T cell responses to antigens expressed in lung adenocarcinomas delay malignant tumor progression. Cancer Cell. 2011;19:72–85. doi: 10.1016/j.ccr.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–54. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. The N Engl J Med. 2012;366:2455–65. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraman M, Bambrough PJ, Arnold JN, Roberts EW, Magiera L, Jones JO, et al. Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-alpha. Science. 2010;330:827–30. doi: 10.1126/science.1195300. [DOI] [PubMed] [Google Scholar]
- 9.Garin-Chesa P, Old LJ, Rettig WJ. Cell surface glycoprotein of reactive stromal fibroblasts as a potential antibody target in human epithelial cancers. Proc Natl Acad Sci U S A. 1990;87:7235–9. doi: 10.1073/pnas.87.18.7235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bauer S, Jendro MC, Wadle A, Kleber S, Stenner F, Dinser R, et al. Fibroblast activation protein is expressed by rheumatoid myofibroblast-like synoviocytes. Arthritis Res Ther. 2006;8:R171. doi: 10.1186/ar2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elso C, Kumar B, Smyth G, Foote S, Handman E. Dissociation of disease susceptibility, inflammation and cytokine profile in lmr1/2 congenic mice infected with Leishmania major. Genes Immun. 2004;5:188–96. doi: 10.1038/sj.gene.6364056. [DOI] [PubMed] [Google Scholar]
- 12.Marigo I, Dolcetti L, Serafini P, Zanovello P, Bronte V. Tumor-induced tolerance and immune suppression by myeloid derived suppressor cells. Immunol Rev. 2008;222:162–79. doi: 10.1111/j.1600-065X.2008.00602.x. [DOI] [PubMed] [Google Scholar]
- 13.Abe R, Donnelly SC, Peng T, Bucala R, Metz CN. Peripheral blood fibrocytes: differentiation pathway and migration to wound sites. J Immunol. 2001;166:7556–62. doi: 10.4049/jimmunol.166.12.7556. [DOI] [PubMed] [Google Scholar]
- 14.Weis N, Weigert A, von Knethen A, Brune B. Heme oxygenase-1 contributes to an alternative macrophage activation profile induced by apoptotic cell supernatants. Mol Biol Cell. 2009;20:1280–8. doi: 10.1091/mbc.E08-10-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meffert MK, Haley JE, Schuman EM, Schulman H, Madison DV. Inhibition of hippocampal heme oxygenase, nitric oxide synthase, and long-term potentiation by metalloporphyrins. Neuron. 1994;13:1225–33. doi: 10.1016/0896-6273(94)90060-4. [DOI] [PubMed] [Google Scholar]
- 16.Lutton JD, Abraham NG, Drummond GS, Levere RD, Kappas A. Zinc porphyrins: Potent inhibitors of hematopoieses in animal and human bone marrow. Proc Natl Acad Sci. USA. 1997;94:1432–6. doi: 10.1073/pnas.94.4.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Di Noia MA, Van Driesche S, Palmieri F, Yang LM, Quan S, Goodman AI, Abraham NG. Heme oxygenase-1 enhances renal mitochondrial transport carriers and cytochrome C oxidase activity in experimental diabetes. J Biol Chem. 2006;281:15687–93. doi: 10.1074/jbc.M510595200. [DOI] [PubMed] [Google Scholar]
- 18.Burt TD, Seu L, Mold JE, Kappas A, McCune JM. Naive human T cells are activated and proliferate in response to the heme oxygenase-1 inhibitor tin mesoporphyrin. J Immunol. 2010;185:5279–88. doi: 10.4049/jimmunol.0903127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Valaes T, Petmezaki S, Henschke C, Drummond GS, Kappas A. Control of jaundice in preterm newborns by an inhibitor of bilirubin production: studies with tin-mesoporphyrin. Pediatrics. 1994;93:1–11. [PubMed] [Google Scholar]
- 20.Cunnington AJ, de Souza JB, Walther M, Riley EM. Malaria impairs resistance to Salmonella through heme- and heme oxygenase-dependent dysfunctional granulocyte mobilization. Nat Med. 2011;18:120–7. doi: 10.1038/nm.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Doukas J, Pober JS. IFN-gamma enhances endothelial activation induced by tumor necrosis factor but not IL-1. J Immunol. 1990;145:1727–33. [PubMed] [Google Scholar]
- 22.Brouard S, Otterbein LE, Anrather J, Tobiasch E, Bach FH, Choi AMK, Soares MP. Carbon monoxide generated by heme oxygenase-1 suppresses endothelial apoptosis. J Exp Med. 2000;192:1015–25. doi: 10.1084/jem.192.7.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Minamoto K, Harada H, Lama VN, Fedarau MA, Pinsky DJ. Reciprocal regulation of airway rejection by the inducible gas-forming enzymes heme oxygenase and nitric oxide synthase. J Exp Med. 2005;202:283–94. doi: 10.1084/jem.20050377. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.