Abstract
Aim:
To compare the effects of two stereoisomeric forms of glycyrrhetinic acid on different components of Na+ current, HERG and Kv1.5 channel currents.
Methods:
Wild-type (WT) and long QT syndrome type 3 (LQT-3) mutant ΔKPQ Nav1.5 channels, as well as HERG and Kv1.5 channels were expressed in Xenopus oocytes. In addition, isolated human atrial myocytes were used. Two-microelectrode voltage-clamp technique was used to record the voltage-activated currents.
Results:
Superfusion of 18β-glycyrrhetinic acid (18β-GA, 1–100 μmol/L) blocked both the peak current (INa,P) and late current (INa,L) generated by WT and ΔKPQ Nav1.5 channels in a concentration-dependent manner, while 18α-glycyrrhetinic acid (18α-GA) at the same concentrations had no effects. 18β-GA preferentially blocked INa,L (IC50=37.2±14.4 μmol/L) to INa,P (IC50=100.4±11.2 μmol/L) generated by ΔKPQ Nav1.5 channels. In human atrial myocytes, 18β-GA (30 μmol/L) inhibited 47% of INa,P and 87% of INa,L induced by Anemonia sulcata toxin (ATX-II, 30 nmol/L). Superfusion of 18β-GA (100 μmol/L) had no effects on HERG and Kv1.5 channel currents.
Conclusion:
18β-GA preferentially blocked the late Na current without affecting HERG and Kv1.5 channels.
Keywords: anti-arrhythmia agent, 18β-glycyrrhetinic acid, Nav1.5 channel, HERG channel, Kv1.5 channel, human atrial myocyte, Anemonia sulcata toxin, long QT syndrome
Introduction
Activation of the cardiac voltage-gated sodium channel (Nav1.5) generates two types of inward currents, a large peak transient current (<3 ms) (INa,P) and another current of weak intensity that spans the action potential (>300 ms). The transient current initiates the rapid upstroke of the action potential, whereas the late persistent sodium current (INa,L) does not have a well-defined function, although it has been shown to affect the duration of the action potential. Recently, the role of INa,L in controlling cardiac action potential repolarization and its importance in arrhythmogenesis has received increased attention1.
An abnormal increase in INa,L current, produced by the delayed opening of Na+ channels, prolongs action potential repolarization and can lead to failed repolarization (early after-depolarizations) and Na+-induced Ca2+ overloading that triggers delayed after-depolarizations, calcium oscillations, and rapid tachyarrhythmia such as ventricular tachycardia (VT) or fibrillation1. The reduction of INa,L would therefore be expected to have therapeutic potential2, 3, 4. For example, ranolazine, a relatively selective inhibitor of INa,L, has been shown to be effective in reducing angina and the incidence of non-sustained VT in patients with ischemic heart disease5, 6, 7.
Pronounced INa,L was also observed in the congenital long QT syndrome (LQTS) caused by the mutation of Nav1.5. The most severe defect observed to date has been associated with the ΔKPQ mutation. The loss of three amino acids in the intercellular linker between domains 3 and 4 has been associated with LQTS. In the clinic, LQTS can most commonly be produced as an adverse effect to the drug due to blockade of the rapid component of the delayed rectifier potassium current, IKr8. HERG expresses a rapid delayed rectifier current (IKr), and the testing of potential drugs for their ability to block HERG is required for drug approval8. Kv1.5 conducts ultrarapid delayed rectifier current (IKur) in the human atria9, 10, and the loss-of-function mutation might also result in LQTS and cardiac arrest11.
Recently, we reported that glycyrrhetinic acid (GA), an active ingredient of licorice12, blocks both INaP and INa,L13. However, GA exists in two different stereoisomeric forms, the trans form and the cis form. The two forms have different physical and chemical properties and pharmacological effects14. Therefore, the purpose of the present study was to determine the action of 18β-GA and 18α-GA on INa,P and INa,L using wild-type (WT) and mutant ΔKPQ Nav1.5 channels expressed in Xenopus oocytes. Our results indicate that 18β-GA blocked WT and ΔKPQ Nav1.5 channels; however, 18α-GA had no significant effect on either channel. We further characterized the inhibition of WT and ΔKPQ Nav1.5 channels by 18β-GA and have demonstrated that 18β-GA preferentially blocks the INa,L produced by ΔKPQ Nav1.5 channels in a concentration-dependent tonic manner. Moreover, we investigated the effects of 18β-GA on HERG and Kv1.5 channels and found that 18β-GA had no obvious effects on either channel. Finally, we evaluated the blockage effects of 18β-GA on INa,P and INa,L induced by ATX-II in human atrial myocytes, to further determine the prospects of this drug for treatment in human cardiovascular disease.
Materials and methods
Drugs
18α-GA and 18β-GA were purchased from Sigma (USA) and prepared initially as a 100 mmol/L stock solution by dissolving in 100% DMSO. Before use in an experiment, the stock solution was diluted with ND96 solution to reach the desired final concentration. The percentage of DMSO in the final solution was ≤0.1%, which alone showed no detectable effect on the sodium current. ATX-II was purchased from Sigma (USA) and dissolved in distilled water.
In vitro transcription of cRNA and functional expression in Xenopus oocytes
In vitro transcription of cRNAs and the isolation of oocytes were performed as previously described13, 15, 16. The plasmid pTracer-SV40 containing WT or ΔKPQ human Nav1.5 genes was a kind gift from Dr Thomas ZIMMER of Friedrich Schiller University Jena. HERG was subcloned into the pSP64 plasmid, which was a kind gift from Prof Michael C SANGUINETTI (University of Utah, USA). The human Kv1.5 gene (a gift from Dr Maria L GARCIA, Merck & Co, Inc, USA) was subcloned into a pCI-neo vector. Stage IV and V oocytes were injected with cRNA and then incubated in ND96 solution supplemented with 100 U/mL penicillin, 100 U/mL streptomycin and 2.5 mmol/L sodium pyruvate at 18 °C for 3 to 7 d before use in voltage-clamp experiments. ND96 solution contains (in mmol/L) 96 NaCl, 2 KCl, 1.8 CaCl2, 2 MgCl2, and 5 HEPES; the pH was adjusted to 7.5 with NaOH. The amount of cRNA injected was varied according to the purpose of the experiment. For INa,P, the amount of cRNA was adjusted to yield peak currents in the range of 4–8 μA to minimize space clamp heterogeneities and series resistance errors; INa,L measurements required peak current amplitudes of greater than 10 μA to maximize the signal.
Two-microelectrode voltage clamp
Standard two-microelectrode voltage clamp techniques and a TEV-200A amplifier (Dagan Corporation) were used to record currents at room temperature (22–24 °C). Glass microelectrodes were filled with 3 mol/L KCl, and their tips were broken to obtain resistances of 0.5 to 1.5 MΩ. pCLAMP software (version 9.0; Molecular Devices, Union City, CA, USA) and a 1322A analog/digital interface (Molecular Devices) were used to generate voltage commands.
The voltage protocols used to obtain currents are described in the results. The data for activation and steady-state inactivation were fitted with a simple Boltzmann function: I/Imax={1+exp[Vm–V1/2)/k]}, where I/Imax is the relative current, V1/2 is the half-maximum voltage of activation or inactivation, and k is the slope factor. The recovery time course was fitted with the biexponential function: I/Imax=Ao+Af(1–exp[-t/τf])+As(1–exp[-t/τs]), where τ and A are the time constants and the corresponding relative amplitude, respectively.
The amplitudes of INa,P were measured as maximal amplitudes during the first 5 ms of the depolarizing pulse and the INa,L as the mean current amplitude of the last 10 ms of the pulse. The concentration required for a 50% block of current (IC50) was determined by fitting the data to a Hill equation using five concentrations of drug (6–27 oocytes/point).
Human atrial myocyte isolation and whole-cell patch clamp
Human atrial myocytes were enzymatically dissociated as described previously17. Right atrial appendage tissues were obtained during atriotomy in patients undergoing coronary artery bypass grafting. All patients were free of supraventricular tachyarrhythmia and symptomatic congestive heart failure, and all atrial tissues were grossly normal at the time of cardiac surgery. Using a patch-clamp amplifier (Axon-200 B, Molecular Devices), the whole-cell patch clamp technique was used to record the INa. The series resistance averaged 1.6±0.4 MΩ after compensating for approximately 80% of the initial value. The pipette solution contained (in mmol/L) 120 CsCl, 1 CaCl2, 5 MgCl2, 5 Na2ATP, 10 TEACl, 11 EGTA and 10 HEPES (pH 7.3 with CsOH). The bath solution for INa,P recording contained (in mmol/L) 25 NaCl, 105 CsCl, 1.8 CaCl2, 1 MgCl2, 0.05 CdCl2, 10 HEPES and 10 glucose (pH 7.4 with CsOH). The bath solution used to measure the INa,L induced by ATX-II recording contained (in mmol/L) 135 NaCl, 1.8 CaCl2, 1 MgCl2, 0.05 CdCl2, 10 HEPES and 10 glucose (pH 7.4 with NaOH).
Data analysis
pCLAMP 9.0 and Origin 7.5 (Microcal Software, Northampton, MA, USA) software were used for data acquisition and analysis. Values are expressed as the mean±SD. Analyses of variance (ANOVA) for repeated measures and the Holm-Sidak multiple comparison post-test or Student's t-test (InStat 2.04; GraphPad Software) were employed to determine statistical significance (P<0.05).
Results
Effects of 18α-GA and 18β-GA on WT and ΔKPQ Nav1.5 channels
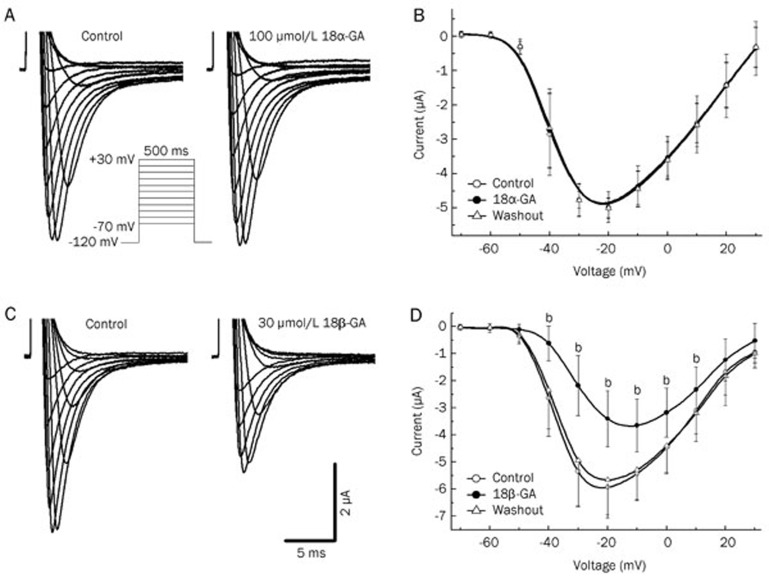
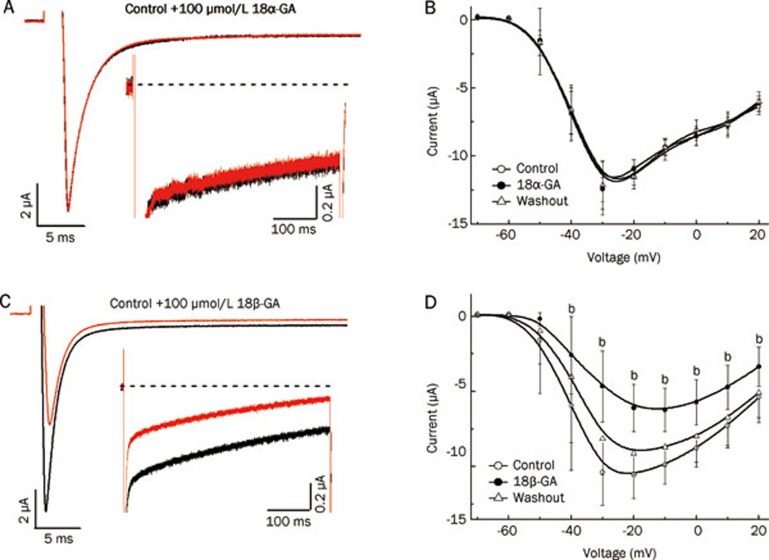
We first compared the effects of 18α-GA and 18β-GA on INa produced by WT (Figure 1) and ΔKPQ (Figure 2) Nav1.5 channels expressed in Xenopus oocytes. Currents were elicited by a series of 500-ms depolarizing steps from a hold potential of -120 mV with an interpulse interval of 10 s. Original INa,P traces of WT Nav1.5 channel-mediated current before and after superfusion with 100 μmol/L 18α-GA or 30 μmol/L 18β-GA are shown in Figures 1A and 1C, respectively. Figures 2A and 2C show one typical current trace of ΔKPQ Nav1.5 channel current elicited by a depolarizing pulse to -20 mV, which demonstrates the incomplete inactivation of INa,L and the effects of 100 μmol/L 18α-GA and 100 μmol/L 18β-GA, respectively. Application of 18β-GA significantly inhibited the INa produced by both WT and ΔKPQ Nav1.5 channels (Figures 1D and 2D), while 18α-GA had no obvious effects on WT and ΔKPQ Nav1.5 channels (Figures 1B and 2B).
Figure 1.
Effects of 18α-GA and 18β-GA on INa,P mediated by the WT Nav1.5 channel. (A) and (C) Representative current traces elicited by 500-ms test pulses from -70 mV to 30 mV with 10 mV increments at 0.1 Hz in typical oocytes perfused before and after in 100 μmol/L 18α-GA (A) or 30 μmol/L 18β-GA (C). The membrane potential was held at -120 mV. (B) and (D) Averaged current-voltage relationships of INa,P before and after perfusion with 100 μmol/L 18α-GA (B) or 30 μmol/L 18β-GA (D); n=6 per group; bP<0.05.
Figure 2.
Effects of 18α-GA and 18β-GA on ΔKPQ Nav1.5 channels. (A) and (C) Original current recordings in the absence and presence of 100 μmol/L 18α-GA (A) or 18β-GA (C). Current was elicited by a depolarizing pulse from a holding potential of -120 mV to -30 mV for 500 ms. Insets show magnified current traces for comparison of the late component. (B) and (D) Averaged current-voltage relationships of INa,P before and after perfusion with 100 μmol/L 18α-GA (B) or 18β-GA (D); n=6 per group; bP<0.05.
Concentration-dependent tonic block of WT and ΔKPQ Nav1.5 channels by 18β-GA
We then examined the dose-dependent and tonic blockage effects of 18β-GA on WT and ΔKPQ Nav1.5 channels. Oocytes were held at -120 mV, and currents were evoked by depolarization to -20 mV every 10 s. This infrequent pulsing protocol should minimize the effects of a frequency-dependent block, therefore providing a reasonable estimate of the extent to which 18β-GA induces a tonic block of INa. The upper panel of Figure 3A shows the experimental recordings of INa,P from WT Nav1.5 channels before and after the successive application of 1, 30, and 100 μmol/L 18β-GA. The upper panels of Figures 3B and 3C show the superimposed INa,P and INa,L traces of ΔKPQ Nav1.5 channels and the blocking effects of 18β-GA at 1, 30 and 100 μmol/L, respectively.
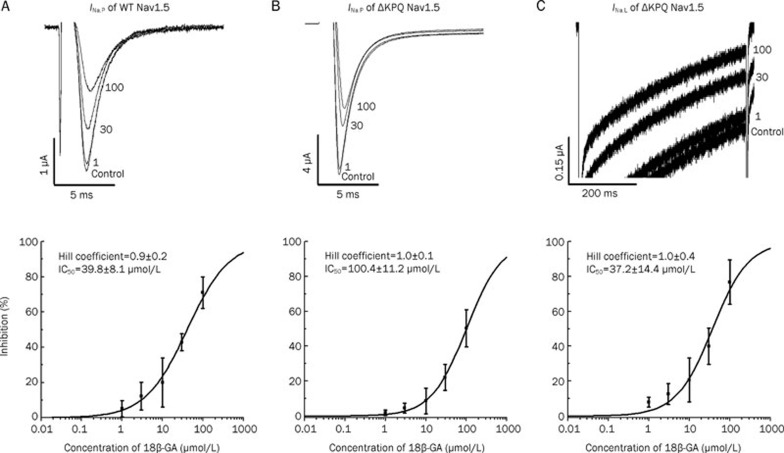
Figure 3.
Concentration-dependent block by 18β-GA of WT INa,P (A), ΔKPQ INa,P (B), and INa,L (C). INa was elicited by a depolarizing pulse from a holding potential of -120 mV to -30 mV for 500 ms at 0.1 Hz. Representative traces (upper panels) were superimposed before (control) and during perfusion of 18β-GA (1–100 μmol/L). (B, C) are traces from the same oocyte on an expanded scale. Summarized dose-response data (lower panels) fitted with the Hill equation. IC50 values and the Hill coefficient are provided in the figure. n=6–27 oocytes/point.
Because there was no detectable INa,L in WT Nav1.5 channels, only the suppression of INa,P was analyzed. The lower panels of Figure 3 show the concentration-response curves for 18β-GA after application to the WT and ΔKPQ Nav1.5 channels. The smooth lines represent the best fits of the data using the Hill equation, with the parameters of the fits shown in Figure 3. The Hill coefficients of 18β-GA binding to WT and ΔKPQ Nav1.5 channels were not significantly different from 1, suggesting that only one drug molecule is necessary to block the channel. The 18β-GA block of INa,P and INa,L in ΔKPQ Nav1.5 channels exhibited IC50 values of 100.4±11.2 μmol/L and 37.2±14.4 μmol/L, respectively. These results demonstrated that 18β-GA exhibited greater degrees of tonic inhibition of INa,L compared with INa,P when applied to ΔKPQ Nav1.5 channels.
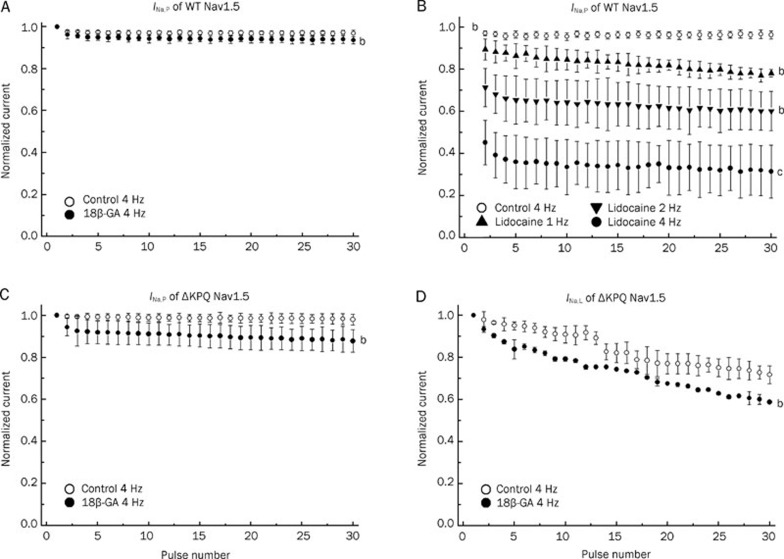
Rate-dependent block of WT andΔKPQ Nav1.5 channels by 18β-GA
To study the rate-dependent block (phasic block), a series of 30 repetitive impulses to -20 mV from a holding potential of -120 mV were applied at 1, 2, and 4 Hz, according to the method proposed by Rajamani et al18. The amplitude of currents was normalized to the current during the first impulse and plotted as a function of the pulse number. Lidocaine is a clinically used class I anti-arrhythmic agent, and its action on Nav1.5 channels has been studied extensively (reviewed by Sheets et al19). In the presence of 18β-GA (30 μmol/L), INa,P of WT Nav1.5 channels did not change after 30 repetitive depolarizing events at 4 Hz (approximately 0.93 at the 30th pulse, n=6 in each group, Figure 4A). On the contrary, lidocaine (100 μmol/L) caused a significant rate-dependent reduction in the current conducted by the WT Nav1.5 channel (P<0.05 at 1 Hz and 2 Hz, P<0.01 at 4 Hz, n=5, Figure 4B), which is similar to other reports20, 21. The INa,P mediated by the WT Nav1.5 channel (Figure 4A) shows that the administration of 18β-GA at 100 μmol/L caused an additional phasic block of INa,P and INa,L at ΔKPQ Nav1.5 channels (P<0.05, n=6, Figures 4C and 4D).
Figure 4.
Rate-dependent blockade of WT and ΔKPQ Nav1.5 channels. INa was elicited by a series of 30 depolarizing pulses of -120 mV to -20 mV at different stimulation frequencies. The relative current amplitude elicited by each pulse was normalized to the respective amplitudes the currents elicited by the first pulse and plotted against each pulse number: for WT INa,P, 30 μmol/L 18β-GA at 4 Hz (A) (n=6) and 100 μmol/L lidocaine at 1, 2, and 4 Hz (B) (n=5); for ΔKPQ, 100 μmol/L 18β-GA of INa,P (C) and INa,L (D) at 4 Hz (n=6). bP<0.05, cP<0.01.
Voltage dependence of the activation and inactivation of WT and ΔKPQ Nav1.5 channels in the absence and presence of 18β-GA
Voltage-dependent activation and steady-state inactivation of WT and ΔKPQ Nav1.5 channels were measured and fitted with Boltzmann equations. The former was evaluated as normalized conductance-voltage relationships, and the latter was determined using a double-pulse as indicated in the protocol diagram in Figure 1S. The parameters are summarized in Table 1. Treatment with 18β-GA significantly shifted the V1/2 of activation curves in the positive direction and V1/2 of the steady-state inactivation curves in the negative direction; these shifts were completely recovered after washout. These results confirmed and extended our previous study on GA13 and suggested that 18β-GA alters the gating function of both WT and ΔKPQ Nav1.5 channels.
Table 1. Comparative activation and inactivation parameters of WT (at 30 μmol/L) and ΔKPQ (at 100 μmol/L) INa,P in the absence (control) and presence of 18β-GA. Mean±SD. n=6 per group. bP<0.05 vs control.
| WT |
ΔKPQ |
|||||||
|---|---|---|---|---|---|---|---|---|
| Activation | Inactivation | Activation | Inactivation | |||||
| V1/2 | K | V1/2 | K | V1/2 | K | V1/2 | K | |
| Control | −33.8±1.8 | 6.7±1.6 | −81.8±0.4 | 7.2±0.3 | −36.2±1.8 | 7.0±1.5 | −75.1±0.4 | 4.8±0.4 |
| 18β-GA | −25.1±1.9b | 7.7±1.7 | −88.1±0.3b | 6.9±0.2b | −28.6±1.6b | 7.8±1.3b | −80.5±0.5b | 5.1±0.4 |
| Washout | −31.6±1.7 | 7.6±1.5 | −83.0±0.4 | 7.2±0.4 | −33.2±1.8 | 7.0±1.5 | −75.4±0.4 | 4.7±0.4 |
The recovery time course of WT and ΔKPQ Nav1.5 channels from inactivation had fast (τf) and slow components (τs) (Figure 1S and Table 2). The application of 18β-GA significantly slowed the recovery of WT (30 μmol/L) and ΔKPQ (100 μmol/L) Nav1.5 channels. Table 2 summarizes the above parameters of WT and ΔKPQ Nav1.5 channels. These results suggest that 18β-GA could act on both fast and slow inactivation components of WT and ΔKPQ Nav1.5 channels.
Table 2. Recovery inactivation parameters of WT (at 30 μmol/L) and ΔKPQ (at 100 μmol/L) INa,P in the absence (control) and presence of 18β-GA. Mean±SD. n=6 per group. bP<0.05 vs control.
| Control |
18β-GA |
|||
|---|---|---|---|---|
| τf | τs | τf | τs | |
| WT | 11.8±2.4 | 261.7±26.0 | 22.1±7.4b | 342.7±36.1b |
| ΔKPQ | 5.8±1.1 | 201.2±40.5 | 7.3±2.0b | 272.0±34.0b |
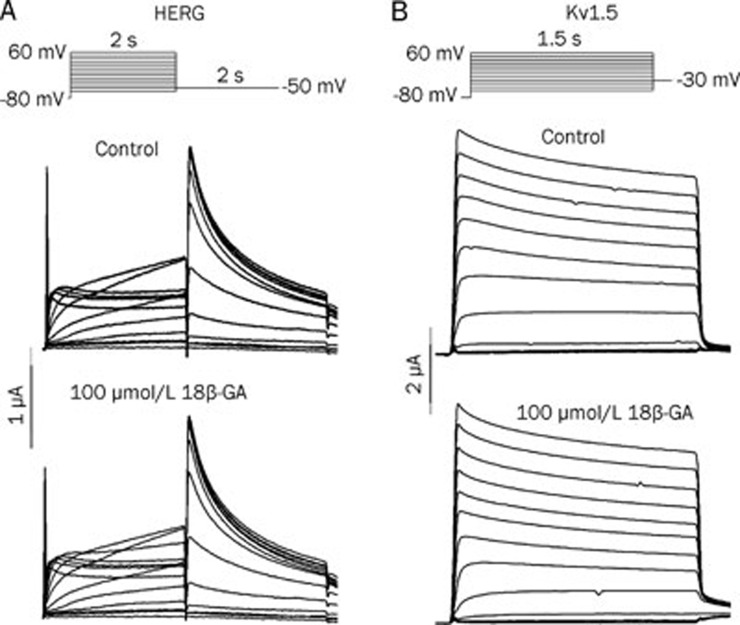
Effects of 18β-GA on HERG and Kv1.5 channels
Our previous study demonstrated that GA had no significant effect on L-type calcium current (ICa,L) or hyperpolarization-activated inward current (If) in rabbit sinoatrial node pacemaker cells13. In this study, we extended our previous study to investigate the effects of 18β-GA on HERG and Kv1.5 channels. Figures 5A and 5B show the experimental current recordings obtained from HERG and Kv1.5 channels before and after the application of 100 μmol/L 18β-GA. The voltage protocols are presented in the inset of Figure 5. 18β-GA at 100 μmol/L had no inhibitory effects on either HERG (n=6) or Kv1.5 channels (n=7). No significant effect of 18α-GA (100 μmol/L) on HERG was observed (data not shown).
Figure 5.
Effects of 18β-GA on HERG (A) and Kv1.5 potassium channels expressed in Xenopus oocytes. The voltage protocols are shown in the upper panels. 18β-GA at 100 μmol/L had no significant effects on HERG (n=6) or Kv1.5 channels (n=7).
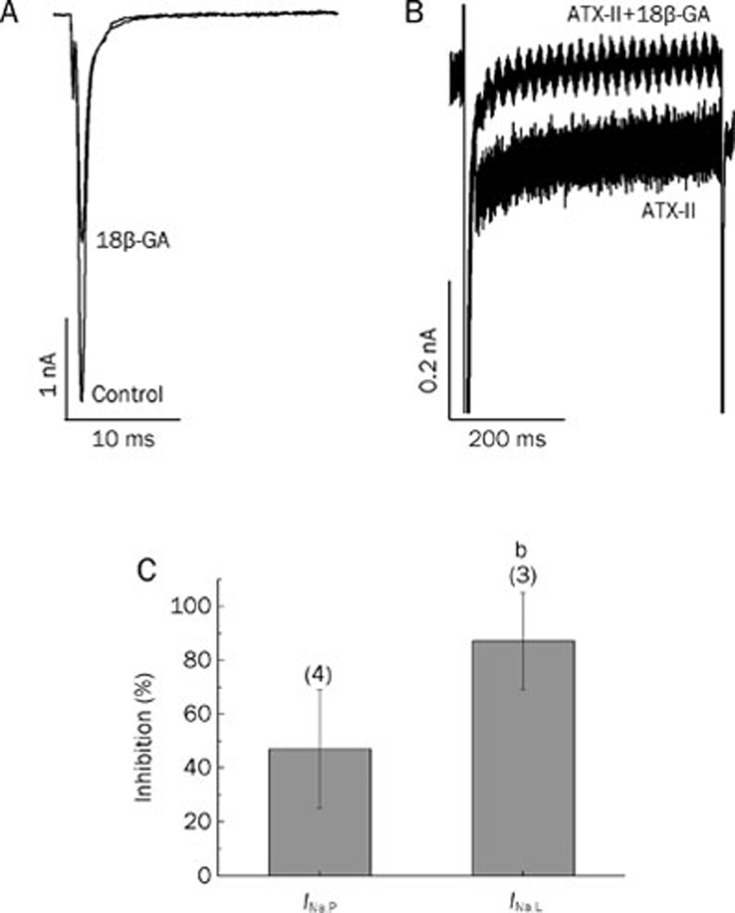
Inhibition of INa,P and INa,L induced by ATX-II in human atrial myocytes after exposure to 18β-GA
Figure 6A shows superimposed typical recordings of INa,P in the absence and presence of 30 μmol/L 18β-GA in freshly isolated human atrial myocytes. Figure 6B shows typical traces of INa,L induced by ATX-II (30 nmol/L) and the effect of 18β-GA at 30 μmol/L. Currents were obtained with a depolarizing step to -20 mV from a holding potential of -80 mV. 18β-GA at 30 μmol/L blocked the INa,P and INa,L induced by ATX-II by approximately 47% and 87%, respectively (P<0.05, Figure 6C). These results confirmed the preferential blockage effects of 18β-GA on INa,L produced by ΔKPQ Nav1.5 channels expressed in Xenopus oocytes.
Figure 6.
Effects of 18β-GA on INa,P and INa,L induced by ATX-II in isolated human atrial myocytes. (A) Original INa,P recoding in control oocytes and in the presence of 30 μmol/L 18β-GA. Current was elicited by a depolarizing pulse from a holding potential of -80 mV to -30 mV for 100 ms. (B) Representative INa,L induced by ATX-II (30 nmol/L) in the absence and in the presence of 30 μmol/L 18β-GA. Current was elicited by a depolarizing pulse from a holding potential of -80 mV to -30 mV for 500 ms. (C) The bar graph shows the percentage of inhibition of INa,P and INa,L induced by ATX-II mediated by 30 μmol/L 18β-GA. The numbers of cells are indicated in parentheses. bP<0.05.
Discussion
In the present study, we compared the electrophysiological effects of two stereoisomeric forms of glycyrretinic acid, 18α- and 18β-GA, on WT and ΔKPQ Nav1.5 channels expressed in Xenopus oocytes. The key findings were that 18β-GA inhibited both channels, while 18α-GA had no significant effects on either WT or ΔKPQ channels. This is the first study to examine the effects of 18β-GA on WT and ΔKPQ Nav1.5 channels as well as HERG and Kv1.5 potassium channels. Our results suggest that 18β-GA preferentially blocks the INa,L generated by ΔKPQ Nav1.5 channels in a concentration-dependent tonic manner without significant effects on either HERG or Kv1.5 potassium channels. The greater inhibition of 18β-GA on INa,L induced by ATX-II was also observed in human atrial myocytes.
In this study, we compared the pharmacological effects of two stereoisomeric forms of GA (18α- and 18β-) on WT and ΔKPQ Nav1.5 channels. We observed that 18α-GA had no significant effects on either WT or ΔKPQ Nav1.5 channels, even at a very high concentration (100 μmol/L). 18β-GA, however, significantly inhibited both WT and ΔKPQ Nav1.5 channels. Our results demonstrated that 18β-GA but not 18α-GA blocked WT and ΔKPQ Nav1.5 channels. One possible explanation regarding the difference in blocking effects between the two stereoisomers is the stereochemical structure. Conformational analysis showed that in 18α-GA, the hydrogen atom of C18 is not in the same plane with the carboxyl chain of C30. In contrast, in 18β-GA, the hydrogen atom and the carboxyl chain are in the same plane. Consistent with our results, different potencies of 18α-GA and 18β-GA have been observed in other pharmacological contexts22, 23. For example, 18α-GA blocks voltage-gated potassium channels in vascular smooth muscle cells, while 18β-GA does not24.
Our previous study showed that GA blocked the INa,P mediated by the WT Nav1.5 channel (approximately 33% at 90 μmol/L) and the INa,L mediated by the ΔKPQ Nav1.5 channel (IC50=67±7.08 μmol/L)13. In this study, 18β-GA inhibited the INa,P mediated by the WT Nav1.5 channel with an IC50 of 40 μmol/L and blocked INa,P and INa,L currents mediated by the ΔKPQ Nav1.5 channel at IC50 values of 100 μmol/L and 37 μmol/L, respectively. Therefore, 18β-GA was a more potent INa,P and INa,L blocker than GA; its potency to block INa,L was approximately three-fold greater than its potency in blocking the INa,P mediated by the ΔKPQ Nav1.5 channel.
Following tonic block, 30 depolarizing pulses were delivered to determine the extent of phasic block, the rate-dependent block, at different frequencies (1, 2, and 4 Hz). For the WT Nav1.5 channel, at 4 Hz, the INa,P remaining at the 30th pulse was 94% of the 1st pulse in the presence of 30 μmol/L 18β-GA. In contrast to 18β-GA, lidocaine caused a much greater reduction at the 30th pulse vs the 1st pulse (∼21%). This result implies that 18β-GA caused much less phasic block than lidocaine. Similar results were also found for the INa,P and INa,L currents of the ΔKPQ Nav1.5 channel. Our results suggest that 18β-GA caused a potent tonic block with little additional phasic block at WT and ΔKPQ Nav1.5 channels, which was different from the effect of lidocaine as well as the reported effects of mexiletine25 and ranolazine18.
Phasic block is a characteristic of most class I anti-arrythmic drugs19, but it also accounts for the unfavorable lethal pro-arrythymias induced by these drugs26. 18β-GA, which exhibits less potent phasic block, may prevent excessive blockage of INa in the treatment of tachyarrhythmia and may reduce the frequency of bradycardia. We found that INa,L exhibited a significant rate-dependent reduction similar to the observation reported by Guo et al27, who suggested that the INa,L mediated by the ΔKPQ Nav1.5 channel was more pronounced at low heart rates. This may explain the clinical findings that ventricular tachyarrythmias and sudden cardiac death in patients with LQT3 tend to occur during sleep or at rest, when the heart rate is slow28. Ranolazine has recently been used to treat LQT-3 patents expressing the ΔKPQ channel29. Ranolazine exhibits strong rate-dependent inhibition, as ranolazine produced less inhibition when INa,L was more pronounced at a slower heart rate18. Unlike ranolazine18, 18β-GA produced a potent tonic block of INa,L, which resulted in stronger anti-arrythmic effects. Recently, a more selective potent INa,L blocker, F15845, also characterized by tonic blockade, has been demonstrated to be effective in preventing ischemia-induced arrhythmia30.
HERG expresses IKr, and blockage of HERG is believed to cause LQT, which can induce EAD and a Torsades de-Pointes-type of ventricular arrhythmia, as observed after treatment with class I or class III anti-arrhythmic drugs including ranolazine9, 31, 32. Kv1.5 conducts IKur in the human atria9, 10. This channel is also found in the ventricle, but its role remains unknown. 18β-GA at 100 μmol/L demonstrated no inhibition of HERG or Kv1.5 channels, which suggested that 18β-GA might not increase QT. However, further study is required to investigate the effects of 18β-GA on QT because other potassium currents, such as transient outward current (Ito), slow delayed rectifier current (IKs) and inward rectifier current (IK1), also determine QT duration.
Up-regulated INa,L has been demonstrated to be a major contributor to intracellular Na+ accumulation during many pathological conditions, such as ischemia or hypoxia, leading to elevated levels of intracellular Ca2+ that have entered the cell through the reverse-mode Na+–Ca2+ exchanger, which is followed by arrhythmogenesis and ultimately cell death. The inhibition of INa,L and prevention of Na+overload may therefore be cardioprotective3, 33, 34, 35, 36. 18β-GA preferentially blocks the INa,L induced by ATX-II (mimicking INa,L activation evoked by ischemia36) in isolated human atrial myocytes. Experiments on isolated human atrial myocytes confirmed the potency of 18β-GA to reduce INa,L in a more physiological environment. Through blockade of INa,L, 18β-GA can alleviate INa,L-associated arrhythmias37 and cardiac injury after myocardial ischemia38.
In conclusion, our results show that 18β-GA but not 18α-GA preferentially blocks INa,L.. 18β-GA had no significant effects on HERG or Kv1.5 channels. Our results suggest that 18β-GA has significant potential for development as a novel anti-arrhythmic agent, particularly in INa,L-associated arrhythmias and myocardial ischemia. Care should be taken in applying the results from heterologous expression studies to the clinical management of patients. Temperature, lipid environment, subunit composition and additional post-translational modifications of Na+ channels in cardiomyocytes may also affect the degree of blockade by 18β-GA. Nonetheless, further evaluation of the therapeutic potential of 18β-GA is warranted.
Author contribution
Jia-hong XIA, Ming LEI, and Yi-mei DU designed the research program; Yi-mei DU, Cheng-kun XIA, Ning ZHAO, and Qian DONG performed the research; Yi-mei DU, Cheng-kun XIA, Ming LEI, and Jia-hong XIA analyzed the data and drafted the article.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No 30971243, 81170164 to Dr Yi-mei DU, No 30872542 to Dr Jia-hong XIA) and the Open Foundation of Hubei Key Laboratory of Biological Targeted Therapy No 2010-79 to Dr Cheng-kun XIA.
We thank Drs Thomas ZIMMER (Friedrich Schiller University, Germany), Michael C SANGUINETTI (University of Utah, USA) and Maria L GARCIA (Merck & Co, Inc, USA) for generously providing the cDNA plasmid vector.
Footnotes
Supplementary figure is available at the Acta Pharmacologica Sinica website.
Supplementary Information
Effects of 18β-GA on the kinetics of INa,P of WT and ΔKPQ Nav1.5 channels.
References
- Noble D, Noble PJ. Late sodium current in the pathophysiology of cardiovascular disease: consequences of sodium-calcium overload. Heart. 2006;92:v1–v5. doi: 10.1136/hrt.2005.078782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale SL, Shryock JC, Belardinelli L, Sweeney M, Kloner RA. Late sodium current inhibition as a new cardioprotective approach. J Mol Cell Cardiol. 2008;44:954–67. doi: 10.1016/j.yjmcc.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Morita N, Lee JH, Xie Y, Sovari A, Qu Z, Weiss J N, et al. Suppression of re-entrant and multifocal ventricular fibrillation by the late sodium current blocker ranolazine. J Am Coll Cardiol. 2011;57:366–75. doi: 10.1016/j.jacc.2010.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shryock JC, Belardinelli L. Inhibition of late sodium current to reduce electrical and mechanical dysfunction of ischaemic myocardium. Br J Pharmacol. 2008;153:1128–32. doi: 10.1038/sj.bjp.0707522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antzelevitch C, Burashnikov A, Sicouri S, Belardinelli L. Electrophysiologic basis for the antiarrhythmic actions of ranolazine. Heart Rhythm. 2011;8:1281–90. doi: 10.1016/j.hrthm.2011.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobshagen C, Belardinelli L, Hasenfuss G, Maier LS. Ranolazine for the treatment of heart failure with preserved ejection fraction: background, aims, and design of the RALI-DHF study. Clin Cardiol. 2011;34:426–32. doi: 10.1002/clc.20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti CR. Ion channel therapy of ischemic heart disease: from calcium channel blockers to late sodium current inhibition. Clin Cardiol. 2011;34:66–7. doi: 10.1002/clc.20882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witchel HJ. Drug-induced hERG block and long QT syndrome. Cardiovasc Ther. 2011;29:251–9. doi: 10.1111/j.1755-5922.2010.00154.x. [DOI] [PubMed] [Google Scholar]
- Nerbonne JM. Molecular basis of functional voltage-gated K+ channel diversity in the mammalian myocardium. J Physiol. 2000;525:285–98. doi: 10.1111/j.1469-7793.2000.t01-1-00285.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedida D, Wible B, Wang Z, Fermini B, Faust F, Nattel S, et al. Identity of a novel delayed rectifier current from human heart with a cloned K+ channel current. Circ Res. 1993;73:210–6. doi: 10.1161/01.res.73.1.210. [DOI] [PubMed] [Google Scholar]
- Nielsen NH, Winkel BG, Kanters JK, Schmitt N, Hofman-Bang J, Jensen HS, et al. Mutations in the Kv1.5 channel gene KCNA5 in cardiac arrest patients. Biochem Biophys Res Commun. 2007;354:776–82. doi: 10.1016/j.bbrc.2007.01.048. [DOI] [PubMed] [Google Scholar]
- Fiore C, Eisenhut M, Ragazzi E, Zanchin G, Armanini D. A history of the therapeutic use of liquorice in Europe. J Ethnopharmacol. 2005;99:317–24. doi: 10.1016/j.jep.2005.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y, Zhang S, Wu H, Zou A, Lei M, Cheng L, et al. Glycyrretinic acid blocks cardiac sodium channels expressed in Xenopus oocytes. J Ethnopharmacol. 2009;125:318–23. doi: 10.1016/j.jep.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Wang ZY, Agarwal R, Zhou ZC, Bickers DR, Mukhtar H. Inhibition of mutagenicity in Salmonella typhimurium and skin tumor initiating and tumor promoting activities in SENCAR mice by glycyrrhetinic acid: comparison of 18 alpha- and 18 beta-stereoisomers. Carcinogenesis. 1991;12:187–92. doi: 10.1093/carcin/12.2.187. [DOI] [PubMed] [Google Scholar]
- Du YM, Zhang XX, Tu DN, Zhao N, Liu YJ, Xiao H, et al. Molecular determinants of Kv1.5 channel block by diphenyl phosphine oxide-1. J Mol Cell Cardiol. 2010;48:1111–20. doi: 10.1016/j.yjmcc.2010.02.010. [DOI] [PubMed] [Google Scholar]
- Tu DN, Liao YH, Zou AR, Du YM, Run Q, Wang XP, et al. Electropharmacological properties of telmisartan in blocking hKv1.5 and HERG potassium channels expressed on Xenopus laevis oocytes. Acta Pharmacol Sin. 2008;29:913–22. doi: 10.1111/j.1745-7254.2008.00839.x. [DOI] [PubMed] [Google Scholar]
- Xiao H, Wang M, Du Y, Yuan J, Zhao G, Tu D, et al. Agonist-like autoantibodies against calcium channel in patients with dilated cardiomyopathy Heart Vessels 2011. doi: 10.1007/s00380-011-0176-7 [DOI] [PubMed]
- Rajamani S, El-Bizri N, Shryock JC, Makielski JC, Belardinelli L. Use-dependent block of cardiac late Na+ current by ranolazine. Heart Rhythm. 2009;6:1625–31. doi: 10.1016/j.hrthm.2009.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheets MF, Fozzard HA, Lipkind GM, Hanck DA. Sodium channel molecular conformations and antiarrhythmic drug affinity. Trends Cardiovasc Med. 2010;20:16–21. doi: 10.1016/j.tcm.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gintant GA, Hoffman BF. Use-dependent block of cardiac sodium channels by quaternary derivatives of lidocaine. Pflugers Arch. 1984;400:121–9. doi: 10.1007/BF00585029. [DOI] [PubMed] [Google Scholar]
- Fan XR, Ma JH, Zhang PH, Xing JL. Blocking effect of methylflavonolamine on human NaV1.5 channels expressed in Xenopus laevis oocytes and on sodium currents in rabbit ventricular myocytes. Acta Pharmacol Sin. 2010;31:297–306. doi: 10.1038/aps.2010.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chintharlapalli S, Papineni S, Jutooru I, Mcalees A, Safe S. Structure-dependent activity of glycyrrhetinic acid derivatives as peroxisome proliferator-activated receptor {gamma} agonists in colon cancer cells. Mol Cancer Ther. 2007;6:1588–98. doi: 10.1158/1535-7163.MCT-07-0022. [DOI] [PubMed] [Google Scholar]
- Zani F, Cuzzoni MT, Daglia M, Benvenuti S, Vampa G, Mazza P. Inhibition of mutagenicity in Salmonella typhimurium by Glycyrrhiza glabra extract, glycyrrhizinic acid, 18 alpha- and 18 beta-glycyrrhetinic acids. Planta Med. 1993;59:502–7. doi: 10.1055/s-2006-959748. [DOI] [PubMed] [Google Scholar]
- Guan BC, Si JQ, Jiang ZG. Blockade of gap junction coupling by glycyrrhetinic acids in guinea pig cochlear artery: a whole-cell voltage- and current-clamp study. Br J Pharmacol. 2007;151:1049–60. doi: 10.1038/sj.bjp.0707244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang DW, Yazawa K, Makita N Jr, George AL, Bennett PB. Pharmacological targeting of long QT mutant sodium channels. J Clin Invest. 1997;99:1714–20. doi: 10.1172/JCI119335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mestre M, Djellas Y, Carriot T, Cavero I. Frequency-independent blockade of cardiac Na+ channels by riluzole: comparison with established anticonvulsants and class I anti-arrhythmics. Fundam Clin Pharmacol. 2000;14:107–17. doi: 10.1111/j.1472-8206.2000.tb00398.x. [DOI] [PubMed] [Google Scholar]
- Guo D, Lian J, Liu T, Cox R, Margulies KB, Kowey PR, et al. Contribution of late sodium current (INa–L) to rate adaptation of ventricular repolarization and reverse use-dependence of QT-prolonging agents. Heart Rhythm. 2011;8:762–9. doi: 10.1016/j.hrthm.2010.12.026. [DOI] [PubMed] [Google Scholar]
- Schwartz PJ, Priori SG, Spazzolini C, Moss AJ, Vincent GM, Napolitano C, et al. Genotype-phenotype correlation in the long-QT syndrome: gene-specific triggers for life-threatening arrhythmias. Circulation. 2001;103:89–95. doi: 10.1161/01.cir.103.1.89. [DOI] [PubMed] [Google Scholar]
- Moss AJ, Zareba W, Schwarz KQ, Rosero S, Mcnitt S, Robinson JL. Ranolazine shortens repolarization in patients with sustained inward sodium current due to type-3 long-QT syndrome. J Cardiovasc Electrophysiol. 2008;19:1289–93. doi: 10.1111/j.1540-8167.2008.01246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignier C, Rougier JS, Vie B, Culie C, Verscheure Y, Vacher B, et al. Selective inhibition of persistent sodium current by F 15845 prevents ischaemia-induced arrhythmias. Br J Pharmacol. 2010;161:79–91. doi: 10.1111/j.1476-5381.2010.00884.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanguinetti MC, Jiang C, Curran ME, Keating MT. A mechanistic link between an inherited and an acquired cardiac arrhythmia: HERG encodes the IKr potassium channel. Cell. 1995;81:299–307. doi: 10.1016/0092-8674(95)90340-2. [DOI] [PubMed] [Google Scholar]
- Rajamani S, Shryock JC, Belardinelli L. Rapid kinetic interactions of ranolazine with HERG K+ current. J Cardiovasc Pharmacol. 2008;51:581–9. doi: 10.1097/FJC.0b013e3181799690. [DOI] [PubMed] [Google Scholar]
- Lindegger N, Hagen BM, Marks AR, Lederer WJ, Kass RS. Diastolic transient inward current in long QT syndrome type 3 is caused by Ca2+ overload and inhibited by ranolazine. J Mol Cell Cardiol. 2009;47:326–34. doi: 10.1016/j.yjmcc.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vacher B, Pignier C, Letienne R, Verscheure Y, Le Grand B. F 15845 inhibits persistent sodium current in the heart and prevents angina in animal models. Br J Pharmacol. 2009;156:214–25. doi: 10.1111/j.1476-5381.2008.00062.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L, Ma J, Li H, Wang C, Grandi E, Zhang P, et al. Late sodium current contributes to the reverse rate-dependent effect of IKr inhibition on ventricular repolarization. Circulation. 2011;123:1713–20. doi: 10.1161/CIRCULATIONAHA.110.000661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belardinelli L, Shryock J C, Fraser H. Inhibition of the late sodium current as a potential cardioprotective principle: effects of the late sodium current inhibitor ranolazine. Heart. 2006;92:v6–v14. doi: 10.1136/hrt.2005.078790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R, Yuan C.Experimental anti-arrhythmic effects of zhigancao (prepared licorice) injection Zhongguo Zhong Yao Za Zhi 199116617–9.Chinese. [PubMed] [Google Scholar]
- Miura T, Ohnuma Y, Kuno A, Tanno M, Ichikawa Y, Nakamura Y, et al. Protective role of gap junctions in preconditioning against myocardial infarction. Am J Physiol Heart Circ Physiol. 2004;286:H214–21. doi: 10.1152/ajpheart.00441.2003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Effects of 18β-GA on the kinetics of INa,P of WT and ΔKPQ Nav1.5 channels.