Abstract
Objective
Women with inflammatory bowel diseases (IBD) utilize contraception at a lower rate than the general population. We sought to identify factors associated with contraceptive use and selection of more effective methods in IBD patients at risk for unintended pregnancy.
Study Design
An online survey was distributed to women with IBD in January 2013. Contraceptive methods were categorized by effectiveness and associations with use explored by demographics, disease characteristics, and reproductive goals.
Results
162 respondents were analyzed: 62% had Crohn’s disease and 38% ulcerative colitis. Mean age was 31 (range 20–45), 97% identified as White, and 53% were nulliparas. 74% were currently using IBD medications. A quarter of participants (23%) used no contraception, 17% used highly effective methods, 41% used short-term hormonal methods, and 19% chose barrier/behavioral methods. Prior IBD-related surgery, biologic therapy use, and low education attainment were associated with no contraception use. Of contraceptive users, age, parity, insurance status, IBD surgery and prior immunomodulator use were associated with highly effective method selection.
Conclusions
A quarter of women with IBD at-risk for pregnancy in this study population reported no contraceptive method use. Higher levels of IBD activity influence contraceptive use and method selection, which could guide future patient and provider educational interventions.
Implications
Pregnancy planning is important for women with inflammatory bowel diseases to avoid adverse outcomes in a disease-poor state. Use of contraception assists in avoidance of unintended pregnancy. IBD characteristics are targets for educational interventions to improve uptake of highly effective contraceptive methods.
Keywords: Contraceptive efficacy, chronic disease, reproductive health
Introduction
Inflammatory Bowel Diseases (IBD) are comprised of two chronic, relapsing disorders: Crohn’s disease and ulcerative colitis. Greater than 90% of patients with IBD carry one of these diagnoses, while the remaining are categorized as indeterminate colitis due to overlapping features of both diagnoses [1]. The disease onset is bimodal with a peak incidence in the 2nd–4th decades and most frequently in 20–29 year olds [2]. As IBD is commonly diagnosed during reproductive years, a quarter of women with IBD conceive for the 1st time after disease diagnosis and the disease does not affect female fertility rates [3, 4].
Family planning is important for women with IBD to optimize disease control and avoid potentially harmful treatments or medication exposure in an unplanned pregnancy [5]. Adverse pregnancy outcomes, including an increase in spontaneous abortion, preterm delivery and low-birth weight have all been associated with disease activity at the time of conception [6–9]. The majority of medications used for IBD are safe in pregnancy, although many of the new biologic therapies have minimal pregnancy data [5]. In addition, anti-inflammatory medications used for IBD management are associated with increased risk of congenital anomalies and adverse pregnancy outcomes in some studies, although the data may be confounded by disease activity at time of use [10]. Pregnancy planning and preconception counseling with both gastroenterology and obstetrics allows time for therapy modifications, such as discontinuation of methotrexate, an immunomodulator used for IBD that is a known teratogen.
Despite the need for pregnancy planning to decrease the risk of disease-related adverse outcomes, women with IBD utilize contraception at a lower rate than the general population [11, 12]. Contraceptive method choice by women with IBD is similar to the general population in the United States, with few women using highly effective methods (intrauterine device, implant, or sterilization) [11]. In addition, literature is sparse on both the effect of contraceptive methods on IBD symptoms and the effect of IBD on contraceptive tolerance or efficacy, resulting in lack of evidence for patient counseling on these issues.
The 2010 Centers for Disease Control United States Medical Eligibility Criteria for Contraceptive Use based recommendations for contraceptive use by IBD patients on a systematic review by Zapata, et al [13, 14]. Implants and IUDs are the most effective reversible methods and are recommended with “no restrictions” for women with IBD (category 1). The advantages of Depo-Provera and progestin-only pills outweigh theoretical health risks and the risk of unintended pregnancy (category 2). Combination estrogen-progesterone methods also have benefits outweighing any risk (category 2), except in women with IBD with an increased risk of venous thrombo-embolism (category 3) [13].
Despite the safety and efficacy of hormonal contraception in women with IBD, there remains a paucity of data on factors associated with contraceptive use in this population, specifically for highly effective methods. Our primary objective was to identify factors associated with contraceptive use by women with IBD at risk for pregnancy. Secondary objectives included (1) identification of factors associated with highly effective contraceptive method selection in women with IBD and (2) description of contraceptive practices of women with IBD at risk for pregnancy who are current methotrexate users.
Materials and Methods
The Institutional Review Board of Northwestern University approved this study. English-speaking women, age (18–45), with IBD (Crohn’s disease, ulcerative colitis, or indeterminate colitis) and at-risk for pregnancy were eligible. We developed a survey using SurveyMonkey® online software and the first page detailed that survey continuation implied study consent. Questions included demographic and disease characteristics, current and past medication use, menstrual and pregnancy history, infertility, sexual frequency, desire for future childbearing and timeline, reasons for pregnancy timeline (i.e. disease control, partner pressure, age, etc.), and current contraceptive method choice. Several questions screened for diagnoses other than IBD (e.g. irritable bowel syndrome, microscopic colitis, celiac sprue, etc.) and excluded those individuals from further participation. The survey was piloted and modified via cognitive phone interviews with six women with IBD recruited through the Center for Psychosocial Research in Gastroenterology (CPRGI) at Northwestern University.
Primary survey distribution occurred via email to the reproductive age women with IBD registered on the CPRGI listserv with a reminder email at one week in January 2013. This listserv includes patients of the faculty gastroenterology clinics at Northwestern University interested in research opportunities and participants of previous research studies through CPRGI. Secondary recruitment was conducted through Twitter® accounts and Facebook® group pages for online IBD support groups, such as “Girls with Guts®” and “The Great Bowel Movement®.” We placed a reminder post at three days and the survey closed at seven days. Participants from the CPRGI listserv received a $10 gift card for compensation and there was no link between survey data and the gift card email address for anonymity. The participants from social media sites were anonymous and not eligible for compensation.
We identified participants “at risk” for unintended pregnancy by excluding those with a hysterectomy, lesbian sexual orientation, no reported sexual activity or menstruation for greater than six months, those with diagnosed infertility, and women who were currently pregnant or actively trying for pregnancy. All descriptive data are represented as means/medians or proportions, as appropriate. For analysis, we grouped contraceptive methods utilizing the World Health Organization (WHO) efficacy tiers [15]: (1) tier 1 methods of long-active contraceptives (implant, intrauterine device, or male/female sterilization), (2) tiers 2, 3, and 4 (short acting hormonal methods, barrier, or behavioral contraceptive methods), and (3) no contraceptive method. We explored associations with demographics, disease characteristics, and reproductive goals by t test or global chi square test. The first comparison was between the non-users and all other contraceptive method users and the second between highly effective (tier 1) users and all other contraceptive methods (tiers 2,3, and 4 users). We performed univariate logistic regression to determine factors associated with any method use in the first model and factors associated with highly effective method choice over other contraceptive methods in the second model. Analysis was completed with Stata/SE 12.0 (StataCorp, College Station, TX).
Results
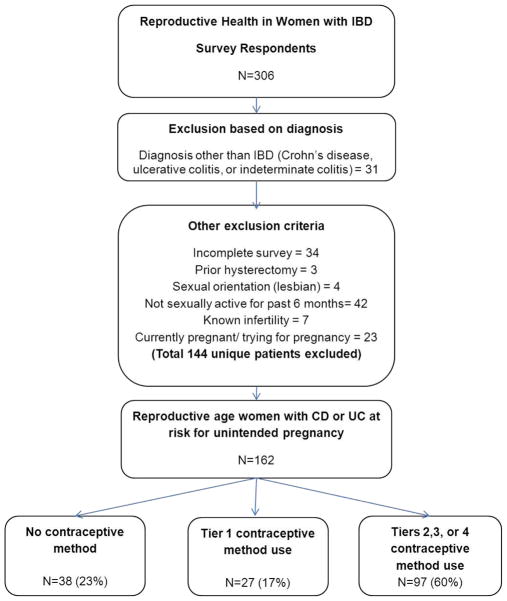
Of 306 respondents, 52.9% (n=162) met inclusion criteria as reproductive age women with IBD who were at-risk for pregnancy. CPRGI listserv respondents accounted for 31% of the study participants with a survey response rate of 61% (n=51/83). As respondents from the CPRGI listserv were anonymous, we could not assess differences from non-respondents. The remaining 111 study participants responded to social media postings, therefore a response rate or characteristics of non-respondents cannot be calculated for this group. Exclusion criteria for analysis and the number of respondents excluded for each indication are listed in Figure 1. We compared available data for excluded respondents to those included in the study population. Excluded respondents were more likely to be younger than those included (28 vs. 31 years, P=0.006). No significant differences were found in diagnosis type or duration of diagnosis and further variables could not be compared due to survey disqualification and incomplete data.
Figure 1. Flow diagram of analyzed participants and contraceptive method use.
IBD = Inflammatory bowel diseases; CD = Crohn’s disease; UC = ulcerative colitis; Tier 1 contraceptive = sterilization, implant, intrauterine devices; Tier 2 = hormonal contraceptive methods; Tier 3 = barrier methods ; Tier 4 = behavioral contraceptive methods
Crohn’s disease accounted for 62% (n=101) of diagnoses and 38% (n=61) of participants had ulcerative colitis. No eligible participants had indeterminate colitis. Mean participant age was 31 years (range 20–45), 97% identified as White, and 77% (n=125) were married or cohabiting. The median parity was 0 (range 0–6) with 53% nulliparas. Previous IBD-related surgery was documented by 56% (n = 90) of the women and 74% (n = 120) currently used IBD medications. (Table 1)
Table 1.
Participant characteristics
| n (%) N= 162 | |
|---|---|
| Demographics | |
| Mean Age (range) | 31 (20–45) |
| Race: White | 158 (97) |
| Ethnicity: Hispanic | 10 (6) |
| Education: College and above | 4.7 (10) |
| Relationship status: Married or cohabiting | 149 (92) |
| Religious affiliation: Any | 107 (66) |
| Employment status | |
| Working | 94 (58) |
| Disability | 28 (17) |
| Student | 21 (13) |
| Non-working | 19 (12) |
| Insurance type | |
| Private | 130 (80) |
| Public (Medicare or Medicaid) | 18 (11) |
| Uninsured | 14 (9) |
| IBD History | |
| Diagnosis | |
| Ulcerative colitis | 61 (38) |
| Crohn's disease | 101 (62) |
| Previous IBD-related surgery | 90 (56) |
| Current IBD medication use | 120 (74) |
| Aminosalicylates | 50 (31) |
| Immunomodulators | 37 (23) |
| Topical steroids | 5 (3) |
| Systemic steroids | 27 (17) |
| Biologic therapies | 60 (37) |
| Past IBD medication use | |
| Aminosalicylates | 132 (82) |
| Immunomodulators | 100 (62) |
| Topical steroids | 42 (26) |
| Systemic steroids | 135 (83) |
| Biologic therapies | 80 (49) |
| Reproductive characteristics | |
| Median parity (range) | 0 (0–6) |
| Contraceptive method by World Health Organization Efficacy Tier | |
| No Method | 38 (23) |
| Tier 1 (sterilization, IUD, or implant) | 27 (17) |
| Tier 2 (short-term hormonal methods) | 66 (41) |
| Tier 3 (barrier methods) | 27 (17) |
| Tier 4 (behavioral methods) | 4 (2) |
IBD = Inflammatory Bowel Disease; IUD = Intrauterine Device;
- Aminosalicylates include balsalazide (B), sulfasalazine (A), mesalamine (C), and olsalazine (C)
- Immunomodulators include azathioprine (D), 6-mercaptopurine (D), and methotrexate (X)
- Topical steroids include hydrocortisone (C) enemas, suppositories, and other formulations
- Systemic steroids include budesonide (B), prednisone (C), methylprednisolone (C), and prednisolone (C)
- Biologic therapies include infliximab (B), adalimumab (B), certolizumab (B), and natalizumab (C)
We categorized contraceptive methods by the WHO tiers for efficacy. [15] A quarter of participants (23%, n=38) used no method of contraception. 17% (n=27) of respondents used highly effective, long-acting contraceptive methods including implants, intrauterine devices, and sterilization (tier 1). The majority of participants (41%, n=66) chose moderately effective short-term hormonal contraceptives (tier 2). The least effective contraceptive methods of barriers (tier 3) and behavioral methods (tier 4) were selected by 19% of women (n=31). (Table 1)
Participants with a history of IBD-related surgery (P=0.03) or past biologic therapy use (P=0.05) were less likely to use any contraceptive method compared to those without prior surgery or biologic use. Education attainment of high school or less was also associated with no contraceptive use (P=0.03), although the numbers were small in this group. Use of a WHO tier 1 contraceptive method was associated with older age (P=0.0008), private health insurance (P=0.04), and increasing parity (P=0.001). Those with prior immunomodulator use (P=0.05) and participants with prior IBD-related surgery who used a contraceptive method (P=0.02) were more likely to use a tier 1 method over other methods. (Table 2)
Table 2.
Summary Associations for (1) users of no contraceptive method versus any contraceptive method and (2) users of a highly effective method (tier 1) versus any other contraceptive method (tiers 2, 3, or 4) by demographic, disease, and reproductive characteristics
| Summary table (n=162) | No contraceptive method n (%) N=38 | Any contraceptive method (WHO Tier 1–4) n (%) N=124 | P value | Tier 1 contraceptive method n (%) N=27 | Tier 2,3, or 4 contraceptive method n (%) N=97 | P value |
|---|---|---|---|---|---|---|
| Demographic Characteristics | ||||||
| Age in years: Mean (±SD) | 31.8 (6.6) | 31.0 (6.5) | 0.49 | 34.6 (6.0) | 30.0 (6.0) | 0.0008 |
| Race | 0.23 | 0.39 | ||||
| Non-White | 2 (5.3) | 2 (1.6) | 1 (3.7) | 1 (1.0) | ||
| White | 36 (94.7) | 122 (98.4) | 26 (96.3) | 96 (99.0) | ||
| Education | 0.04 | 1 | ||||
| High school or less | 6 (15.8) | 7 (5.6) | 1 (3.7) | 6 (6.2) | ||
| College or greater | 32 (84.2) | 117 (94.4) | 26 (96.3) | 91 (93.8) | ||
| Relationship status | 0.46 | 0.31 | ||||
| Married/cohabitating | 31 (81.6) | 94 (75.8) | 23 (85.2) | 71 (73.2) | ||
| Dating/single | 7 (18.4) | 30 (24.2) | 4 (14.8) | 26 (26.8) | ||
| Religion | 0.41 | 0.74 | ||||
| No affiliation | 15 (39.5) | 40 (32.3) | 8 (29.6) | 32 (33.0) | ||
| Any affiliation | 23 (60.5) | 84 (67.7) | 19 (70.4) | 65 (67.0) | ||
| Employment | 0.46 | 0.1 | ||||
| Currently working | 24 (63.2) | 70 (56.5) | 19 (70.4) | 51 (52.6) | ||
| Not working/student | 14 (36.8) | 54 (43.5) | 8 (29.6) | 46 (47.4) | ||
| Insurance Type | 0.57 | 0.04 | ||||
| Private plan | 32 (91.4) | 98 (86.7) | 24 (100) | 74 (83.2) | ||
| Medicaid/Medicare | 3 (8.6) | 15 (13.3) | 0 | 15 (16.8) | ||
| Disease Characteristics | ||||||
| Diagnosis | 0.85 | 0.32 | ||||
| Ulcerative colitis | 33.6 (36) | 32.4 (34) | 8 (29.6) | 39 (40.2) | ||
| Crohn's disease | 66.4 (71) | 67.6 (71) | 19 (70.4) | 58 (59.8) | ||
| No. months since diagnosis: Mean (±SD) | 104.7 (61.2) | 115.4 (81.1 | 0.45 | 132.0 (83.5) | 110.8 (80.2) | 0.23 |
| History IBD-related surgery | 27 (71.1) | 63 (50.8) | 0.03 | 19 (70.4) | 44 (45.4) | 0.02 |
| Current IBD Medications | 24 (63.2) | 96 (77.4) | 0.08 | 21 (77.3) | 75 (77.8) | 0.96 |
| Current Aminosalicylate Use | 7 (18.4) | 43 (34.7) | 0.06 | 10 (37.0) | 33 (34.0) | 0.77 |
| Current immunomodulator Use | 9 (23.7) | 28 (22.6) | 0.89 | 5 (18.5) | 23 (23.7) | 0.57 |
| Current topical steroid use | 1 (2.6) | 4 (3.2) | 1 | 0 | 4 (4.1) | 0.58 |
| Current systemic steroid use | 7 (18.4) | 20 (16.1) | 0.74 | 5 (18.5) | 15 (15.5) | 0.7 |
| Current biologic use | 14 (36.4) | 46 (37.1) | 0.98 | 14 (51.9) | 32 (33.0) | 0.07 |
| Past Aminosalicylate Use | 34 (89.5) | 98 (79.0) | 0.15 | 23 (85.2) | 75 (77.3) | 0.44 |
| Past immunomodulator Use | 24 (63.2) | 76 (61.3) | 0.84 | 21 (77.8) | 55 (56.7) | 0.05 |
| Past topical steroid use | 10 (26.3) | 32 (25.8) | 0.95 | 9 (33.3) | 23 (23.7) | 0.31 |
| Past systemic steroid use | 33 (86.8) | 102 (82.3) | 0.51 | 21 (77.8) | 81 (83.5) | 0.49 |
| Past biologic use | 24 (63.2) | 56 (45.2) | 0.05 | 14 (51.9) | 42 (43.3) | 0.43 |
| Reproductive History/Goals | 0.001 | |||||
| Number prior livebirths | 0.36 | |||||
| 0 | 16 (42.1) | 70 (56.5) | 9 (33.3) | 61 (62.9) | ||
| 1 | 3 (7.9) | 9 (7.3) | 1 (3.7) | 8 (8.2) | ||
| 2 | 10 (26.3) | 20 (16.1) | 4 (14.8) | 16 (16.5) | ||
| ≥3 | 9 (23.7) | 25 (20.1) | 13 (48.2) | 12 (12.4) | ||
| Feeling of urgency to become pregnant | 12 (52.2) | 35 (41.7) | 0.37 | 2 (25) | 33 (43.4) | 0.46 |
SD = Standard Deviation; IBD = Inflammatory Bowel Disease
- Aminosalicylates include balsalazide (B), sulfasalazine (A), mesalamine (C), and olsalazine (C)
- Immunomodulators include azathioprine (D), 6-mercaptopurine (D), and methotrexate (X)
- Topical steroids include hydrocortisone (C) enemas, suppositories, and other formulations
- Systemic steroids include budesonide (B), prednisone (C), methylprednisolone (C), and prednisolone (C)
- Biologic therapies include infliximab (B), adalimumab (B), certolizumab (B), and natalizumab (C)
Six survey participants at-risk for unintended pregnancy currently used methotrexate. Despite sexual activity and use of a known teratogen, contraceptive utilization varied. Two women (33%) denied use of any contraceptive method, two used a combined hormonal method (vaginal ring), one woman had a levonorgestrol intrauterine device, and one relied on male sterilization. All six were nulliparas; one felt a sense of urgency to become pregnant due to her age, but wanted her IBD under control prior to pregnancy. Five women did not desire a pregnancy in the near future due to IBD activity, personal timing reasons, or plans for adoption rather than pregnancy.
Discussion
We sought to explore factors associated with contraceptive use and method selection in women with IBD who are at-risk for pregnancy. Lack of contraceptive utilization in this population was associated with disease-related characteristics, such as previous IBD surgery or biologic therapy use, which imply a more severe disease course. Uptake of a highly effective contraceptive method was more common in older, parous women and disease activity leading to surgery or immunosuppressive therapy was also associated with use. Comparisons to the general population are limited due to the sample size and selection bias, although it remains important to note that 62% of all women and 89% of those at risk for unintended pregnancy use contraception in the general population [12]. In this study population of women with IBD at risk for unintended pregnancy, 23% were not using any form of a contraceptive method; a frequency considerably higher than that for at-risk women in the general population, in spite of the women’s chronic disease status.
As highly effective contraceptive methods are without restriction [13], intrauterine devices and implants should be a first line recommendation for women with IBD, specifically those remote from pregnancy planning, or with a high level of disease activity requiring surgery or intensive medical management. The associations with highly effective method selection in this study population are primarily related to age, parity, and insurance status; all findings consistent with data in the general population [12]. The disease characteristics of previous IBD surgery or past immunomodulator use that were associated with highly effective method selection may imply that patients with increased disease activity are altering reproductive planning.
The association with a history of IBD-related surgery and lack of any contraceptive use is concerning. The IBD literature contains research identifying pelvic surgery as a cause of decreased fertility in women with the disease [16, 17]. Although a more current study countered these findings and identified increasing age and voluntary childlessness as causes of decreased fertility after surgery [18], patients are still counseled pre-operatively on this potential effect [19]. If women assume that they cannot get pregnant, use of contraception may be affected, placing women with higher levels of disease activity at risk of unintended pregnancy. In addition, women with extensive small bowel resections and high output ostomies are at risk for short-gut syndrome, or malabsorption and malnutrition due to higher transit times. Malabsorption of oral contraceptive pills limits this method choice for such women and additional counseling should occur to improve alternate method uptake [20].
Similar to other chronic disease populations, this study highlights a need to identify barriers to contraceptive method use and selection of highly effective methods by women with IBD [21, 22]. Women with IBD are cared for by gastroenterologists who prescribe medications for IBD management, but may not have the knowledge or comfort level to discuss contraceptive options [23]. In addition, communication between gastroenterologists and reproductive health providers may be patient-driven only, minimizing the ability to gain timely access to contraceptive counseling when a medication change occurs [24]. The sample of women in this study on methotrexate, a known teratogen, is small, but one-third was not utilizing any contraceptive method. The development of new biologic therapies for IBD has allowed women to improve disease control, but data supporting safety in pregnancy or lactation remains sparse [5]. The overall lack of evidence, research, and targeted educational initiatives for both patients and providers surrounding reproductive care of women with IBD is in conflict with the patient interest on these topics noted on online social media sites, such as those utilized for this study’s recruitment.
The generalizability of our study is limited by the small sample size and the study design. Highly-educated and privately-insured patients were oversampled in this study, as educational attainment and employment status in IBD patients are similar to the general population [25]. Most participants identified as white, which may be only a slight over-representation, as IBD is greater than three-fold more prevalent in non-Hispanic whites [26]. The online recruitment strategy limited the study population to English-speaking women with Internet access, and may not represent contraceptive method choice from low-literacy or non-English speaking groups. Survey anonymity did not allow for confirmation of the participants’ diagnoses through medical records; thus some analyzed data may not represent true IBD diagnoses. A comparison of respondents to non-respondents was limited in this study design. We excluded a large number of respondents to assess a sample of women at-risk for unintended pregnancy and, disqualified respondents were significantly younger than those included. The small number of participants in some groups limited the ability to control for confounders in the analysis, as multivariable models were not robust. Finally, the closed ended survey questions did not allow for a full range of responses regarding method choice.
Despite limitations, this is one of the only studies to evaluate contraceptive use in the IBD population and we found a quarter of the study sample was not utilizing any form of contraception. Both gastroenterologists and reproductive health providers are charged with prioritizing family planning needs during encounters with reproductive age women affected by this chronic disease. A further exploration of the effect of disease characteristics and treatment modalities on contraceptive method choice is necessary to assist providers in individualized counseling for women with IBD and avoidance of adverse outcomes due to an unintended pregnancy.
Acknowledgments
Dana R. Gossett, MD, MSCI for assistance in survey development. The Women’s Reproductive Health Research Career Development Grant (NIH/NICHD Grant K12 HD050121) funded this study.
Footnotes
Source: Northwestern University Feinberg School of Medicine
Conflicts: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lin J, Cao Q, Zhang J, Li Y, Shen B, Zhao Z, et al. Micro RNA expression patterns in indeterminate colitis. Mod Pathol. 2013;26(1):148–54. doi: 10.1038/modpathol.2012.131. [DOI] [PubMed] [Google Scholar]
- 2.Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterol. 2012;142:46–54. doi: 10.1053/j.gastro.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Baiocco PJ, Korelitz BI. The influence of inflammatory bowel disease and its treatment on pregnancy and fetal outcome. J Clin Gastroenterol. 1984;6:211–6. [PubMed] [Google Scholar]
- 4.Tavernier N, Fumery M, Peyrin-Biroulet L, Colombel JF, Gower-Rousseau C. Systematic review: fertility in non-surgically treated inflammatory bowel disease. Aliment Pharmacol Ther. 2013 Oct;38(8):847–53. doi: 10.1111/apt.12478. [DOI] [PubMed] [Google Scholar]
- 5.Yarur A, Kane SV. Update on pregnancy and breastfeeding in the era of biologics. Dig Liver Dis. 2013 Oct;45(10):787–94. doi: 10.1016/j.dld.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Riis L, Vind I, Politi P, Wolters F, Vermeire S, Tsianos E, et al. Does pregnancy change the disease course? A study in a European cohort of patients with inflammatory bowel disease. Am J Gastroenterol. 2006;101:1539–45. doi: 10.1111/j.1572-0241.2006.00602.x. [DOI] [PubMed] [Google Scholar]
- 7.Fonager K, Sorenson HT, Olsen J, Dahlerup JF, Rasmussen SN. Pregnancy outcome for women with Crohn's disease: a follow-up study based on linkage between national registries. Am J Gastroenterol. 1998;93:2426–30. doi: 10.1111/j.1572-0241.1998.00698.x. [DOI] [PubMed] [Google Scholar]
- 8.Norgard B, Fonager K, Sorenson HT, Olsen J. Birth outcomes of women with ulcerative colitis: a nationwide Danish cohort study. Am J Gastroenterol. 2000;95:3165–70. doi: 10.1111/j.1572-0241.2000.03290.x. [DOI] [PubMed] [Google Scholar]
- 9.Stephansson O, Larsson H, Pedersen L, Kieler H, Granath F, Ludvigsson JF, et al. Crohn's disease is a risk factor for preterm birth. Clin Gastroenterol Hepatol. 2010;8:509–15. doi: 10.1016/j.cgh.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 10.Norgard BM. Birth outcome in women with ulcerative colitis and Crohn's disease, and pharmacoepidemiological aspects of anti-inflammatory drug therapy. Dan Med Bull. 2011;58(12):B4360. [PubMed] [Google Scholar]
- 11.Marri SR, Ahn C, Buchman AL. Voluntary childlessness is increased in women with inflammatory bowel disease. Inflamm Bowel Dis. 2007;13:591–9. doi: 10.1002/ibd.20082. [DOI] [PubMed] [Google Scholar]
- 12.Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. Vital Health Stat 23. 2010;29:1–44. [PubMed] [Google Scholar]
- 13.Centers for Disease Control. [Accessed Dec 29, 2011];US Medically Eligibility Criteria for Contraceptive Use. 2010 http://www.cdc.gov/mmwr/pdf/rr/rr5904.pdf.
- 14.Zapata LB, Paulen ME, Cansino C, Marchbanks PA, Curtis KM. Contraceptive use among women with inflammatory bowel disease: A systematic review. Contraception. 2010;82:72–85. doi: 10.1016/j.contraception.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 15.Steiner MJ, Trussell J, Mehta N, Condon S, Subramanian S, Bourne D. Communicating contraceptive effectiveness: A randomized controlled trial to inform a World Health Organization family planning handbook. Am J Obstet Gynecol. 2006;195(1):85–91. doi: 10.1016/j.ajog.2005.12.053. [DOI] [PubMed] [Google Scholar]
- 16.Olsen KO, Joelsson M, Laurberg S, Oresland T. Fertility after ileal pouch-anal anastomosis in women with ulcerative colitis. Br J Surg. 1999;86(4):493–5. doi: 10.1046/j.1365-2168.1999.01076.x. [DOI] [PubMed] [Google Scholar]
- 17.Ording Olsen K, Juul S, Berndtsson I, Oresland T, Laurberg S. Ulcerative colitis: female fecundity before diagnosis, during disease, and after surgery compared with a population sample. Gastroenterology. 2002;122(1):15–9. doi: 10.1053/gast.2002.30345. [DOI] [PubMed] [Google Scholar]
- 18.Johnson P, Richard C, Ravid A, Spencer L, Pinto E, Hanna M, Cohen Z, McLeod R. Female infertility after ileal pouch-anal anastomosis for ulcerative colitis. Dis Colon Rectum. 2004;47(7):1119–26. doi: 10.1007/s10350-004-0570-7. [DOI] [PubMed] [Google Scholar]
- 19.Doherty GA, Cheifetz AS. Management of acute severe ulcerative colitis. Expert Rev Gastroenterol Hepatol. 2009;3(4):395–405. doi: 10.1586/egh.09.24. [DOI] [PubMed] [Google Scholar]
- 20.Severijnen R, Bayat N, Tolboom J, Bongaerts G. Enteral drug absorption in patients with short small bowel : a review. Clin Pharmacokinet. 2004;43(14):951–62. doi: 10.2165/00003088-200443140-00001. [DOI] [PubMed] [Google Scholar]
- 21.Manaf RA, Ismail IZ, Latiff LA. Contraceptive use among women with chronic medical conditions and factors associated with its non-use in Malaysia. Glob J Health Sci. 2012;4:91–9. doi: 10.5539/gjhs.v4n5p91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yazdany J, Trupin L, Kaiser R, Schmajuk G, Gillis JZ, Chakravarty E, et al. Contraceptive counseling and use among women with systemic lupus erythematosus: a gap in health care quality? Arthritis Care Res. 2011;63:358–65. doi: 10.1002/acr.20402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moleski SM, Choudhary C. Special considerations for women with IBD. Gastroenterol Clin North Am. 2011;40:387–98. doi: 10.1016/j.gtc.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 24.Gawron LM, Hammond C, Keefer L. Documentation of Reproductive Health Counseling and Contraception in Women with Inflammatory Bowel Diseases. Patient Educ Couns. 2013;94(1):134–7. doi: 10.1016/j.pec.2013.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nguyen GC, Chong CA, Chong RY. National estimates of the burden of inflammatory bowel disease among racial and ethnic groups in the United States. J Crohns Colitis. 2013 Sep 29; doi: 10.1016/j.crohns.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 26.Marri SR, Buchman AL. The education and employment status of patients with inflammatory bowel diseases. Inflamm Bowel Dis. 2005;11(2):171–7. doi: 10.1097/00054725-200502000-00011. [DOI] [PubMed] [Google Scholar]