Abstract
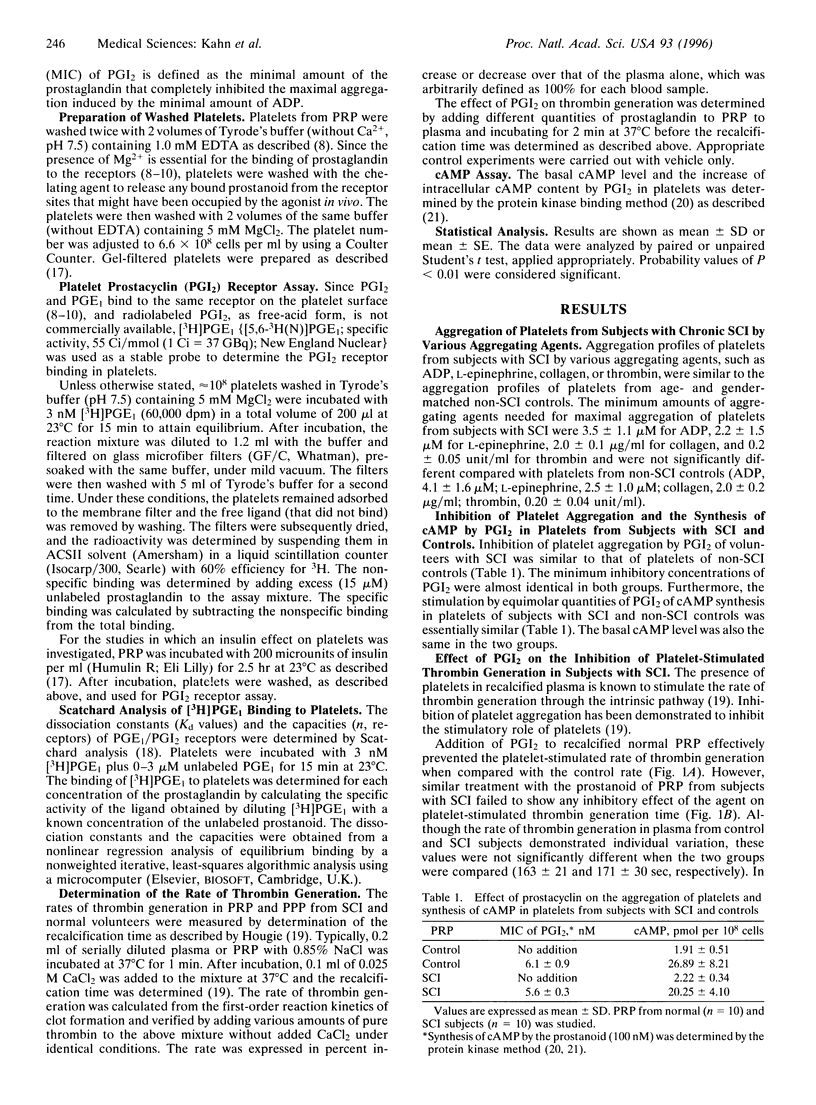
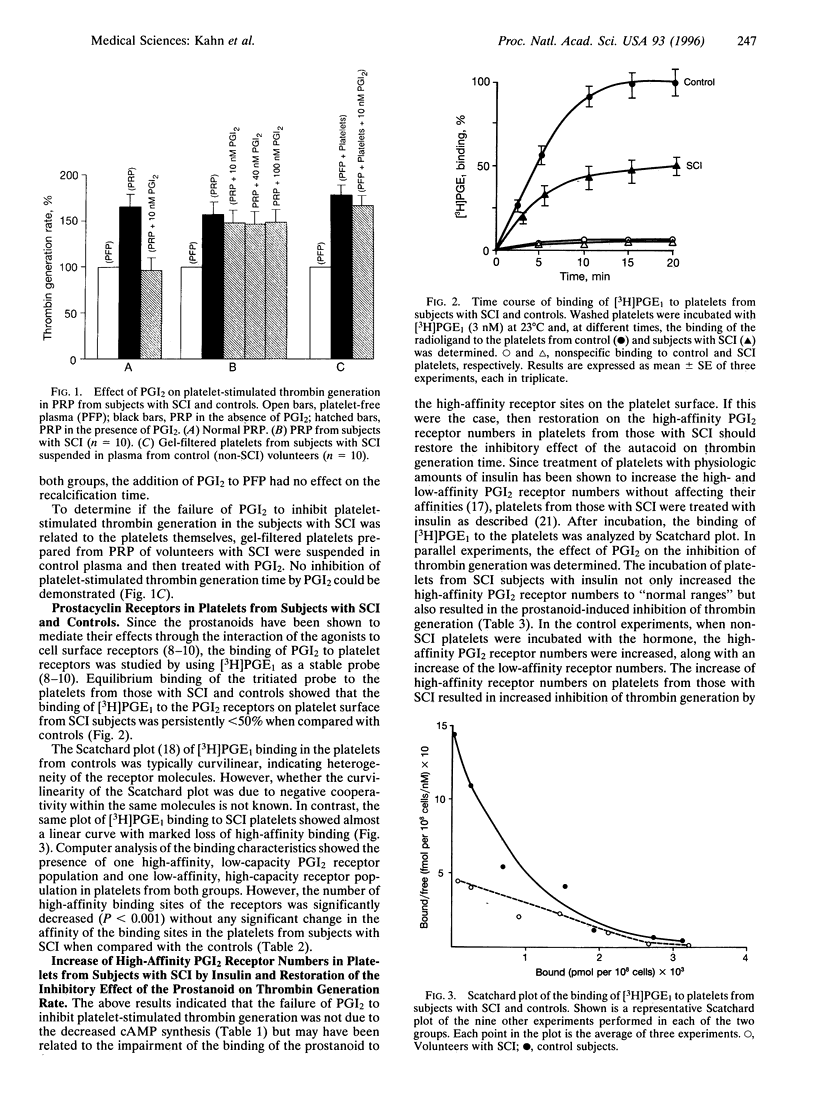
Coronary artery disease is a leading cause of death in individuals with chronic spinal cord injury (SCI). However, platelets of those with SCI (n = 30) showed neither increased aggregation nor resistance to the antiaggregatory effects of prostacyclin when compared with normal controls (n = 30). Prostanoid-induced cAMP synthesis was similar in both groups. In contrast, prostacyclin, which completely inhibited the platelet-stimulated thrombin generation in normal controls, failed to do so in those with SCI. Scatchard analysis of the binding of [3H]prostaglandin E1, used as a prostacyclin receptor probe, showed the presence of one high-affinity (Kd1 = 8.11 +/- 2.80 nM; n1 = 172 +/- 32 sites per cell) and one low-affinity (Kd2 = 1.01 +/- 0.3 microM; n2 = 1772 +/- 226 sites per cell) prostacyclin receptor in normal platelets. In contrast, the same analysis in subjects with SCI showed significant loss (P < 0.001) of high-affinity receptor sites (Kd1 = 6.34 +/- 1.91 nM; n1 = 43 +/- 10 sites per cell) with no significant change in the low affinity-receptors (Kd2 = 1.22 +/- 0.23; n2 = 1820 +/- 421). Treatment of these platelets with insulin, which has been demonstrated to restore both of the high- and low-affinity prostaglandin receptor numbers to within normal ranges in coronary artery disease, increased high-affinity receptor numbers and restored the prostacyclin effect on thrombin generation. These results demonstrate that the loss of the inhibitory effect of prostacyclin on the stimulation of thrombin generation was due to the loss of platelet high-affinity prostanoid receptors, which may contribute to atherogenesis in individuals with chronic SCI.
Full text
PDF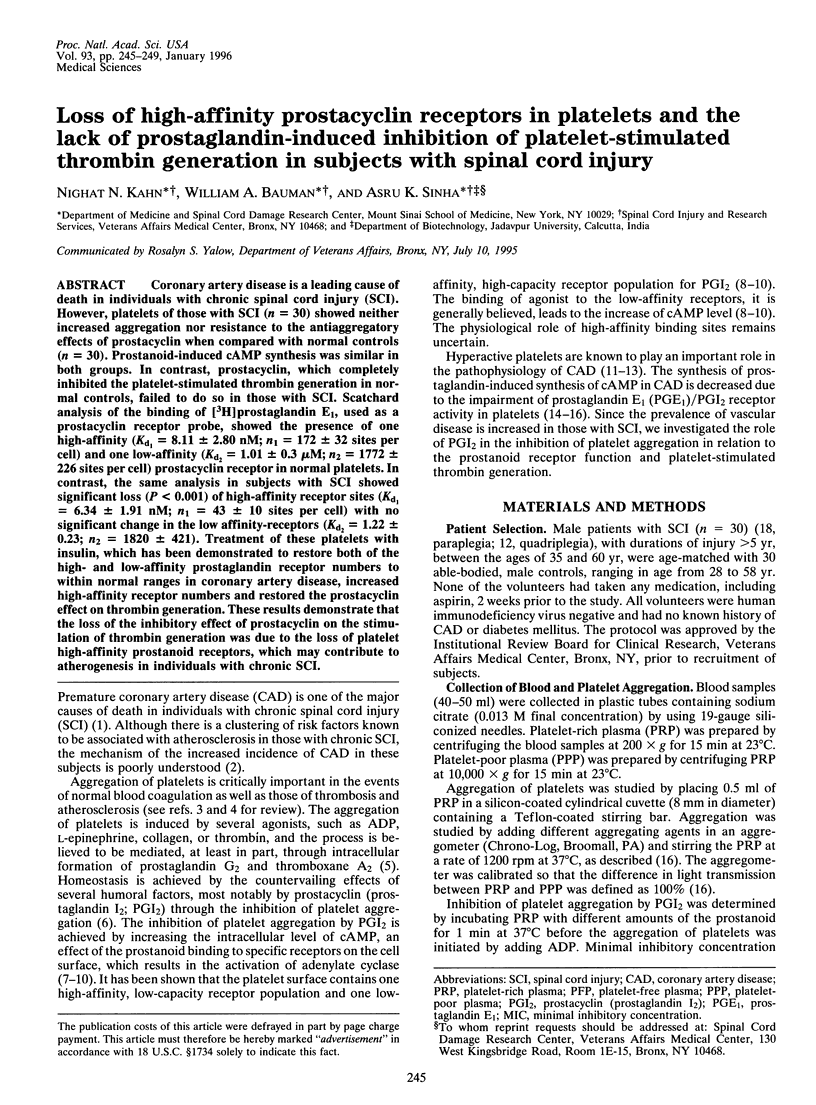


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Borges P. M., Hackler R. H. The urologic status of the Vietnam war paraplegic: a 15-year prospective followup. J Urol. 1982 Apr;127(4):710–711. doi: 10.1016/s0022-5347(17)54009-4. [DOI] [PubMed] [Google Scholar]
- DeWood M. A., Spores J., Notske R., Mouser L. T., Burroughs R., Golden M. S., Lang H. T. Prevalence of total coronary occlusion during the early hours of transmural myocardial infarction. N Engl J Med. 1980 Oct 16;303(16):897–902. doi: 10.1056/NEJM198010163031601. [DOI] [PubMed] [Google Scholar]
- DiCorleto P. E. Cellular mechanisms of atherogenesis. Am J Hypertens. 1993 Nov;6(11 Pt 2):314S–318S. [PubMed] [Google Scholar]
- Dutta-Roy A. K., Sinha A. K. Purification and properties of prostaglandin E1/prostacyclin receptor of human blood platelets. J Biol Chem. 1987 Sep 15;262(26):12685–12691. [PubMed] [Google Scholar]
- Fuster V., Steele P. M., Chesebro J. H. Role of platelets and thrombosis in coronary atherosclerotic disease and sudden death. J Am Coll Cardiol. 1985 Jun;5(6 Suppl):175B–184B. doi: 10.1016/s0735-1097(85)80552-0. [DOI] [PubMed] [Google Scholar]
- Gilman A. G. A protein binding assay for adenosine 3':5'-cyclic monophosphate. Proc Natl Acad Sci U S A. 1970 Sep;67(1):305–312. doi: 10.1073/pnas.67.1.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamberg M., Svensson J., Samuelsson B. Thromboxanes: a new group of biologically active compounds derived from prostaglandin endoperoxides. Proc Natl Acad Sci U S A. 1975 Aug;72(8):2994–2998. doi: 10.1073/pnas.72.8.2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam R. J. Roles of cyclic nucleotides in platelet function. Ciba Found Symp. 1975;35:121–151. doi: 10.1002/9780470720172.ch7. [DOI] [PubMed] [Google Scholar]
- Hedin U., Frebelius S., Sanchez J., Dryjski M., Swedenborg J. Antithrombin III inhibits thrombin-induced proliferation in human arterial smooth muscle cells. Arterioscler Thromb. 1994 Feb;14(2):254–260. doi: 10.1161/01.atv.14.2.254. [DOI] [PubMed] [Google Scholar]
- Jaschonek K., Karsch K. R., Weisenberger H., Tidow S., Faul C., Renn W. Platelet prostacyclin binding in coronary artery disease. J Am Coll Cardiol. 1986 Aug;8(2):259–266. doi: 10.1016/s0735-1097(86)80037-7. [DOI] [PubMed] [Google Scholar]
- Johansson J. S., Nied L. E., Haynes D. H. Cyclic AMP stimulates Ca(2+)-ATPase-mediated Ca2+ extrusion from human platelets. Biochim Biophys Acta. 1992 Mar 23;1105(1):19–28. doi: 10.1016/0005-2736(92)90158-i. [DOI] [PubMed] [Google Scholar]
- Kahn N. N., Mueller H. S., Sinha A. K. Impaired prostaglandin E1/I2 receptor activity of human blood platelets in acute ischemic heart disease. Circ Res. 1990 Apr;66(4):932–940. doi: 10.1161/01.res.66.4.932. [DOI] [PubMed] [Google Scholar]
- Kahn N. N., Mueller H. S., Sinha A. K. Restoration by insulin of impaired prostaglandin E1/I2 receptor activity of platelets in acute ischemic heart disease. Circ Res. 1991 Jan;68(1):245–254. doi: 10.1161/01.res.68.1.245. [DOI] [PubMed] [Google Scholar]
- Kahn N. N., Sinha A. K. Inhibition of prostaglandin E1-induced activation of adenylate cyclase in human blood platelet membrane. Biochim Biophys Acta. 1988 Oct 28;972(1):45–53. doi: 10.1016/0167-4889(88)90101-2. [DOI] [PubMed] [Google Scholar]
- Kahn N. N., Sinha A. K. Stimulation of prostaglandin E1 binding to human blood platelet membrane by insulin and the activation of adenylate cyclase. J Biol Chem. 1990 Mar 25;265(9):4976–4981. [PubMed] [Google Scholar]
- Moncada S., Gryglewski R., Bunting S., Vane J. R. An enzyme isolated from arteries transforms prostaglandin endoperoxides to an unstable substance that inhibits platelet aggregation. Nature. 1976 Oct 21;263(5579):663–665. doi: 10.1038/263663a0. [DOI] [PubMed] [Google Scholar]
- Neri Serneri G. G., Modesti P. A., Fortini A., Abbate R., Lombardi A., Gensini G. F. Reduction in prostacyclin platelet receptors in active spontaneous angina. Lancet. 1984 Oct 13;2(8407):838–841. doi: 10.1016/s0140-6736(84)90874-2. [DOI] [PubMed] [Google Scholar]
- Ross R. The pathogenesis of atherosclerosis--an update. N Engl J Med. 1986 Feb 20;314(8):488–500. doi: 10.1056/NEJM198602203140806. [DOI] [PubMed] [Google Scholar]
- Samsa G. P., Patrick C. H., Feussner J. R. Long-term survival of veterans with traumatic spinal cord injury. Arch Neurol. 1993 Sep;50(9):909–914. doi: 10.1001/archneur.1993.00540090018005. [DOI] [PubMed] [Google Scholar]
- Schafer A. I., Cooper B., O'Hara D., Handin R. I. Identification of platelet receptors for prostaglandin I2 and D2. J Biol Chem. 1979 Apr 25;254(8):2914–2917. [PubMed] [Google Scholar]
- Shultz P. J., Knauss T. C., Mené P., Abboud H. E. Mitogenic signals for thrombin in mesangial cells: regulation of phospholipase C and PDGF genes. Am J Physiol. 1989 Sep;257(3 Pt 2):F366–F374. doi: 10.1152/ajprenal.1989.257.3.F366. [DOI] [PubMed] [Google Scholar]
- Siegl A. M., Smith J. B., Silver M. J., Nicolaou K. C., Ahern D. Selective binding site for [3H]prostacyclin on platelets. J Clin Invest. 1979 Feb;63(2):215–220. doi: 10.1172/JCI109292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smitherman T. C., Milam M., Woo J., Willerson J. T., Frenkel E. P. Elevated beta thromboglobulin in peripheral venous blood of patients with acute myocardial ischemia: direct evidence for enhanced platelet reactivity in vivo. Am J Cardiol. 1981 Sep;48(3):395–402. doi: 10.1016/0002-9149(81)90065-5. [DOI] [PubMed] [Google Scholar]
- Thompson W. D., Smith E. B., Stirk C. M., Kochhar A. Atherosclerotic plaque growth: presence of stimulatory fibrin degradation products. Blood Coagul Fibrinolysis. 1990 Oct;1(4-5):489–493. [PubMed] [Google Scholar]
- de Boer A. C., Turpie A. G., Butt R. W., Johnston R. V., Genton E. Platelet release and thromboxane synthesis in symptomatic coronary artery disease. Circulation. 1982 Aug;66(2):327–333. doi: 10.1161/01.cir.66.2.327. [DOI] [PubMed] [Google Scholar]


