Abstract
Background
The strategy of evaluating every donation opportunity warrants an investigation into the financial feasibility of this practice. The purpose of this investigation is to measure resource utilization required for procurement of transplantable organs in an organ procurement organization (OPO).
Methods
Donors were stratified into those that met OPTN-defined eligible death criteria (ED Donors, n=589) and those that did not (NED Donors, n=703). Variable direct costs and time utilization by OPO staff for organ procurement were measured and amortized per organ transplanted using permutation methods and statistical bootstrapping/resampling approaches.
Results
More organs per donor were procured (3.66 ± 1.2 vs. 2.34 ± 0.8, p<0.0001) and transplanted (3.51 ± 1.2 vs. 2.08 ± 0.8, p<0.0001) in ED donors compared to NED donors. The variable direct costs were significantly lower in NED donors ($29,879.4 ± 11590.1 vs. $19,019.6 ± 7599.60, p<0.0001). In contrast, the amortized variable direct costs per organ transplanted were significantly higher in the NED donors ($8,414.5 ± 138.29 vs. $9,272.04 ± 344.56, p<0.0001). ED donors where thoracic organ procurement occurred were 67% more expensive than in abdominal-only organ procurement. The total time allocated per donor was significantly shorter in NED donors (91.2 ± 44.9 hours vs. 86.8 ± 78.6, p=0.01). In contrast, the amortized time per organ transplanted was significantly longer in the NED donors (23.1 ± 0.8 hours vs. 36.9 ± 3.2, p<0.001).
Discussion
The variable direct costs and time allocated per organ transplanted is significantly higher in donors that do not meet the eligible death criteria.
Keywords: Eligible Death Donor, Non-Eligible Death Donor, Organ Procurement, Deceased Donor Organs, Variable Direct Cost, Resource Allocation
INTRODUCTION
One of the four Organ Donor Breakthrough Collaborative overarching strategies for success is “aggressive pursuit of every donation opportunity”.(1, 2) Conceptually, this approach makes sense and this strategy has resonated with the transplant community. Aggressive donor evaluation approaches coupled with an increased willingness of transplant programs to use organs from borderline donors has increased the overall supply of transplantable organs.(3, 4) The strategy of evaluating every donation opportunity warrants an investigation into the financial feasibility of this practice: Who pays for the additional resources to workup borderline donors where the OPO may experience a “dry run”? Who pays for procuring (non-renal) organs that are discarded? For the most part, OPOs generate their revenue through reimbursement for transplantable organs. A donor where several transplantable organs are procured is ideal; donors that yield a low number of transplantable organs hurt the OPO business model and the reportable performance metrics used to evaluate OPOs. Third party payers do not pay more for an organ that comes from a borderline donor requiring more resources to procure (and conceptually they may want to do exactly the opposite).
The purpose of this investigation is to measure resource utilization required for procurement of transplantable organs in an organ procurement organization (OPO). Donors were stratified into those that met OPTN-defined eligible death criteria and those that did not. The eligible death criteria was used because OPOs accurately capture this data that, in turn, is used for performance measures.(5) Donors that meet eligible death criteria represent the most ideal donors where the most organs are procured and transplanted. The hypothesis is that increased resources are required for the procurement of transplantable organs from donors that do not meet eligible death criteria.
RESULTS
a) Family authorization in eligible death vs. non-eligible death donors
Of the decedents whose families were approached for authorization, 46% were eligible death donors (589/1292). Authorization was obtained more often from the families of eligible death donors than from non-eligible death donors. Authorization was obtained from 63% (371/589) of eligible death donors compared to 38% (266/703) in non-eligible death donors (OR 2.80, 95% CI 2.23 – 3.51).
b) Organs Procured and Transplanted or Discarded in Eligible death vs. Non-eligible death Donors Where Familial Authorization was Obtained
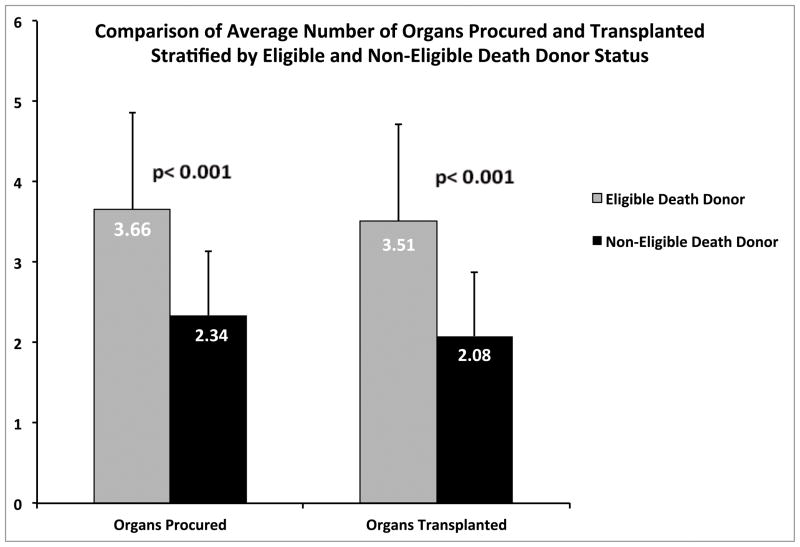
Organ procurement was performed in 99% (367/371) of the eligible death donors compared to 60% (160/266) of the non-eligible death donors (OR 60.78, 95% CI 22.02 – 167.80). More organs per donor were procured from eligible death donors compared to non-eligible death donors (3.66 ± 1.2 vs. 2.34 ± 0.8, p<0.0001) and more organs were transplanted per donor in eligible death donors compared to non-eligible death donors (3.51 ± 1.2 vs. 2.08 ± 0.8, p<0.0001). (Figure 1) Correspondingly, 4% (54/1343) of organs were discarded in the eligible death donors compared to 10% (43/375) in the non-eligible death donors (p<0.0001).
Figure 1.
Number of organs procured and transplanted per donor as a function of Eligible death vs. Non-eligible death donor status. Data represented as mean ± standard deviation.
Of the 160 non-eligible death donors in which organ procurement was performed, 375 organs were procured and 332 organs were transplanted. The number of transplanted organs in the 160 non-eligible death donors was 0 organs in 8 (5%) donors, 1 organ in 24 (15%) donors, 2 organs in 77 (49%) donors, 3 organs in 50 (31%) donors and 4 organs in 1 (1%) donor. Close examination of the 23 “single organ transplanted” non-eligible death donors revealed that 88% (21/24) were liver-only donors of which all 21 were planned liver-only organ procurement in decedents with poor renal function or renal failure patients and/or over 70 years of age with non-transplantable thoracic organs. Similarly, close examination of the 77 “dual organ transplanted” non-eligible death donors revealed that 83% (64/77) were kidney-only donors of which 66% (42/64) were planned kidney-only organ procurement in decedents with established liver disease and non-transplantable thoracic organs. A single pancreas was procured and discarded from a non-eligible death donor. A dual lung procurement was performed and both organs subsequently discarded from a non-eligible death donor. Finally, 7 hearts were procured and 5 transplanted from non-eligible death donors.
c) Variable Direct Cost for Donor Evaluation and Management, Organ Procurement, and Organ Allocation
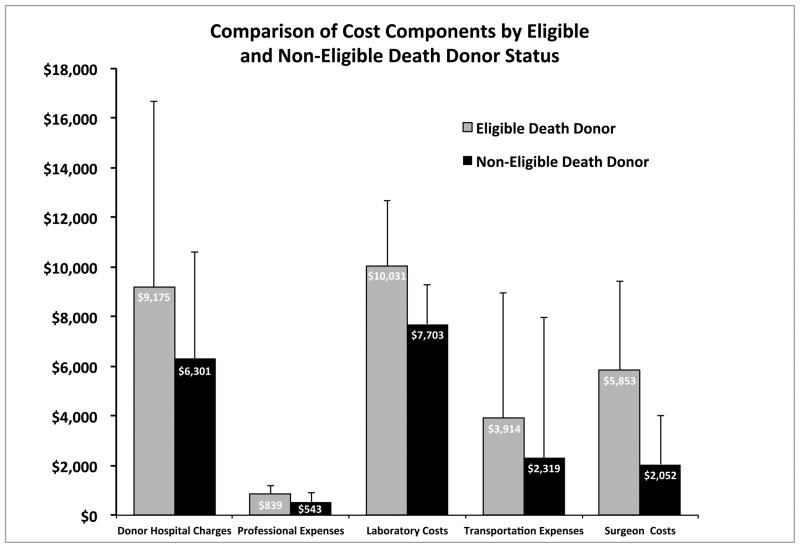
The variable direct costs for organ procurement in an eligible death donor were significantly higher than in a non-eligible death donor (For each donor: $29,879.41 ± 11,590.10 vs. $19,018.60 ± 7,599.60, p<0.0001). (Table 1) The individual expenses were significantly higher in the eligible death donors compared to the non-eligible death donors including the donor hospital fees, professional expenses, laboratory expenses, transportation expenses and surgeon procurement costs. (Figure 2) Much of this incremental cost in the eligible death donors was related to the thoracic organ evaluation, management and procurement. For example, the variable direct cost for abdominal organ only donors compared to abdominal plus thoracic organ donors was $22,573.10 ± 8,964.00 vs. $37,675.20 ± 10,918.10 (p<0.0001).
Table 1.
Total and amortized variable direct organ procurement costs, and total and amortized organ procurement time utilization stratified by eligible death and non-eligible death donor status. Statistical comparisons were performed via a two-sample t-test assuming unequal variances, employing permutation methods and bootstrapping techniques.
| Eligible death Donor | Non-eligible death Donor | Significance | |
|---|---|---|---|
| Total Cost/Donor | $29,879.4 ± 11,590.10 | $19,019.6± 7,599.6 | <0.0001 |
| Cost/Organ Procured | $8,076.13 ± 131.76 | $8,208.85 ± 282.02 | 0.58 |
| Cost/Organ Transplanted | $8,414.46 ± 138.29 | $9,272.04 ± 344.56 | <0.0001 |
| Total Time/Donor | 91.2 ± 44.9 | 86.8± 78.6 | 0.01 |
| Time/Organ Procured | 22.3 ± 0.7 | 32.3± 2.8 | <0.01 |
| Time/Organ Transplanted | 23.1 ± 0.8 | 36.9± 3.2 | <0.001 |
Figure 2.
Bar graph depicting the component variable direct costs associated of organ procurement as a function of Eligible death vs. Non-eligible death donor status. Data represented as mean ± standard deviation.
There was no significant difference in the variable direct cost per organ procured between eligible death and non-eligible death donors (For each organ procured: $8,076.13 ± 131.76 vs. $8,208.85 ± 282.02, p=0.58). However, due to the higher discard rate in the non-eligible death donors, the amortized variable direct cost per organ transplanted was less in the eligible death compared to the non-eligible death donors (For each organ transplanted: $8,414.46 ± 138.29 vs. $9,272.04 ± 344.56, p< 0.0001). (Table 1) The increased variable direct costs were only significant when comparing all organs from eligible death and non--eligible death donors. There were no significant differences when comparing the variable direct “costs per same organ” for heart, liver or kidney organs procured from eligible death compared with non-eligible death donors. (Table 2)
Table 2.
Adjudicated variable direct organ procurement costs for heart, liver and kidney procurement stratified by eligible death and non-eligible death donor status. Statistical comparisons were performed via a two-sample t-test assuming unequal variances.
| Organ | n | Eligible death Donor | n | Non-eligible death Donor | Significance |
|---|---|---|---|---|---|
| Kidney | 346 | $12,229.10 ± 4228.20 | 128 | $12,096.20 ± 4,259.80 | 0.76 |
| Liver | 321 | $8,833.40 ± 3125.80 | 71 | $9,847.60 ± 6,831.30 | 0.23 |
| Heart | 109 | $9,981.90 ± 3305.60 | 5 | $12,541.00 ± 5,874.20 | 0.32 |
d) Alabama Organ Center Time Utilization
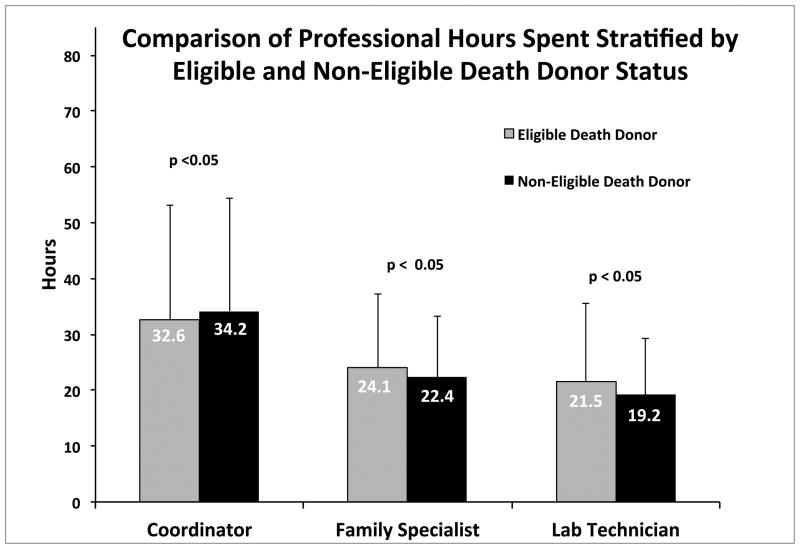
Significantly more overall time was spent working up eligible death donors compared to non-eligible death donors (91.2 ± 44.9 hours vs. 86.8 ± 78.6 hours, p<0.01). (Table 1) The individual time intervals demonstrated an equivalent referral to evaluation time (11.1 ± 19.1 hours vs. 12.2 ± 23.2 hours, p=0.84). The donor management time (on site evaluation to cross clamp time) was significantly increased in the eligible death donors compared to the non-eligible death donors (24.9 ± 14.3 hours vs. 22.9 ± 25.4 hours, p<0.05). There was a trend towards a shorter cross-clamp to case completion time in the eligible death donors compared to the non-eligible death donors (2.9 ± 6.0 hours vs. 3.6 ± 4.9 hours, p=0.11), although the difference did not achieve significance. Times spent on donor evaluation and management by the family support specialist, organ procurement specialist and laboratory technician all were significantly increased in the eligible death donors compared to the non-eligible death donors. (Figure 3)
Figure 3.
Bar graph depicting the component resource utilization associated of organ procurement as a function of Eligible death vs. Non-eligible death donor status. Data represented as median ± interquartile range.
The amortized time per organ procured was significantly shorter in the eligible death donors compared to the non-eligible death donors (22.3 ± 0.7 hours vs. 32.3 ± 2.8 hours, p<0.01). Similarly, the amortized time per organ transplanted was significantly shorter in the eligible death donors compared to the non-eligible death donors (23.1 ± 0.8 hours vs. 36.9 ± 3.2 hours, p<0.001). (Table 1)
e) Liver Only and Kidney Only non-Eligible Death Donors
A separate set of analyses were performed evaluating the “liver-only” donors (n=35, liver single organ procured and transplanted) versus all others (n=492) donors. The aggregate variable direct costs were significantly lower in the liver-only donors compared to the all others donors ($16,015.90 ± 8,953.20 vs. $27,225.50 ± 11,560.90, p<0.0001). In contrast, the amortized variable direct cost per organ transplanted was significantly higher in the liver-only compared to the all others donors ($16,015.90 ± 8,953.20 vs. $7,947.50 ± 115.82, p<0.0001).
A similar set of analyses were performed evaluating the “kidney-only” donors (n=77, kidneys-only procured and transplanted) versus the all others (n=450) donors. The aggregate variable direct costs were significantly lower in the kidney-only donors compared to the all others donors ($17,566.80 ± 5,477.10 vs. $27,712 .00± 11,738.60, p<0.0001). The amortized variable direct cost per organ transplanted was not significantly different in the kidney-only compared to the all others donors ($8,783.41 ± 363.63 vs. $7,999.28. ± 124.43, p=0.07).
DISCUSSION
Increased resources are required for procurement of transplantable organs from donors that do not meet the eligible death criteria. Compared to eligible death donors, non-eligible death donor authorization is much lower (63% vs. 38%), organ procurement is performed in fewer of the donors where familial authorization was obtained (99% vs. 60%), the number of organs procured per donor is less (3.66 vs. 2.34) and the number of organs discarded is substantial (4% vs. 10%). Although the aggregate variable direct costs were lower in non-eligible death donors, the amortized variable direct cost per organ transplanted was significantly higher compared to eligible death donors. A similar paradigm was observed in time spent per donor where less time was spent working up non-eligible death donors, but the amortized time spent per organ transplanted was significantly higher compared to eligible death donors. The paradox is that more time and money are spent on procuring transplantable organs that, in general, are of inferior quality compared to organs from donors that meet the OPTN eligible death criteria.
The eligible death donors incurred more overall expenses, much of which was associated with thoracic organ evaluation and management. The increase in breakdown expenses observed in the eligible death donors seem to make sense with what is observed clinically with potential thoracic organ donors: adding thyroid hormone to aid in weaning off vasopressors to then repeat the echo, ventilator recruitment maneuvers and then repeat chest x-ray and blood gas, waiting till morning for a cardiac catherization, delays in coordinating cardiac and thoracic procurement teams, etc. One can readily see how these frequent thoracic organ evaluation and management steps would add to the total donor evaluation time, increased hospital charges and increased professional expenses. Add to this the increased likelihood of flying vs. driving (to decrease thoracic organ cold ischemia time) thus increasing the transportation costs and a second surgeon procurement fee, the increased aggregate variable direct cost of an eligible death donor is realized.
To tease out the added cost of thoracic organ evaluation and management, we performed a subgroup analysis of just eligible death donors and compared liver/kidney-only donors vs. any donor where thoracic organs were transplanted and found that, on average, a donor in which thoracic organs were procured and transplanted was 67% more expensive than an abdominal organ-only donor. Thoracic organ evaluation and management is expensive and cost accounting schemes need to be able to capture thoracic organ evaluation expenses, especially in donors for which no thoracic organs are procured or transplanted, and prevent the adjudication of thoracic organ expenses to abdominal organs. One example of this is where an echocardiogram and cardiac catheterization are performed but the heart is not deemed usable and only abdominal organs are procured. The development of an a priori algorithm to determine likelihood of transplantable thoracic organs prior to incurring the costs of invasive and time-consuming work-up represents an opportunity to contain costs.
Subgroup analysis was performed evaluating the “cost per same organ” -- eligible death vs. non-eligible death donors. Individual organ procurement expenses are adjudicated to the specific organ generating the expense where possible by the Alabama Organ Center. For example, an echocardiogram expense would be allocated to the heart whereas general infectious serologies and NAT testing expenses would be equally distributed to each organ procured. There were only heart, liver and kidneys procured from non-eligible death donors for comparison. Despite significant cost differences observed in the aggregate comparison, there were no significant differences between eligible death and non-eligible death donor for individual cost comparisons of heart, liver and kidney organ procurement (Table 2). The lack of significant differences observed on the individual organ comparisons is likely due to decreased statistical power comparing two groups with a large variance.
A second subgroup analysis was performed looking specifically at liver-only and kidney-only donors. This, arguably, is a more clinically important analysis than the artificial division of OPTN eligible and non-eligible death donors. Here, we found that the aggregate variable direct cost of a liver-only donor was only 59% of the variable direct cost of a liver-plus donor (liver plus at least one other organ procured and transplanted). When the cost was amortized per organ procured and transplanted, however, the variable direct cost of a liver procured from a liver-only donor was 179% compared to an organ procured and transplanted from a “liver-plus” donor, higher than the 135% reported by the Michigan Donation Service Area.(6) Conversely, the amortized organ variable direct costs in kidney-only donors were not significantly different from a kidney-plus donor (kidneys plus at least one other organ procured and transplanted).
The real issue at hand is does the increased resource utilization associated transplanted organs from non-eligible death donor really matter? The answer to that question is a function of perspective: aggressively pursue every transplantable organ vs. a business model of running an OPO. A simplified way to understand how a non-profit OPO functions is that essentially all the OPO operating expenses are tallied up and adjudicated to the organs that were transplanted. From a purely business standpoint, the multiple organs procured from eligible death donors cover the expenses incurred during the workup of non-eligible death donors.
As with all retrospective database studies, this investigation has limitations. First, determining variable direct costs vs. indirect costs for a medium-sized non-profit organization is an inexact science. Second, the kidney organ acquisition fee charged by the Alabama Organ Center, but set by CMS is one of the lowest in the nation, which may limit the generalizability of the findings for more resource-intensive organ procurement organizations. Third, this study does not consider the increased expenses incurred in recipients of marginal donors because the analyses are conducted from an OPO cost perspective. Studies clearly demonstrate increased hospital and professional expenses in kidney recipients of extended criteria donors(7), in liver recipients of high donor-risk index livers(8) and in liver recipients of donation after cardiac death donors(9).
In conclusion, this study demonstrates that the variable direct costs and time allocated per organ transplanted is significantly higher in donors that do not meet the eligible death criteria. Subgroup analyses also demonstrated significant increase in resource utilization in liver-only donors compared to multi-organ donors. Although increased, the disparity for organ procurement from donors that do not meet eligible death criteria is small in overall magnitude thus affirming the recommended practice of “aggressive pursuit of every donation opportunity”.
METHODS
Ethics approval for this study was obtained from the University of Alabama Institutional Review Board Protocol #N100301001.
a) Data Collected
Data from decedent referrals from 2006 – 2011 were obtained from the AOC internal donor referral database. Decedent eligible death status is determined per published criteria.(5) The following date and time points are recorded for all decedent referrals: referral, (on site) evaluation, cross-clamp and case completion. The AOC employs family support specialists that provide bereavement counseling and solicit donor authorization. On site evaluation begins when the AOC family support specialists arrive at the donor hospital. An AOC clinical coordinator manages the case from referral to completion. They arrive at the donor hospital to manage the donor only when authorization is obtained. An AOC laboratory technician begins working when donor blood arrives to the lab for analysis, manages the organs ex vivo (including renal perfusion) and delivers the organs to the operating room for implantation or to the airport for shipping to alternative transplant centers.
The AOC accounting department provided the following data: donor hospital charges billed, donor hospital charges paid, professional fees paid to the donor hospital staff (e.g. anesthesia, cardiology for catheterization), professional fees paid to abdominal and thoracic procurement surgeons as well as laboratory and tissue typing expenses.
b) Resource Allocation
Resource allocation was determined only for decedents in which organ procurement occurred. Data for donors in which no procurement took place were incomplete and thus not included in the analysis.
Variable Direct Cost for Donor Evaluation and Management, Organ Procurement, and Organ Allocation
These costs were calculated as the sum of variable direct costs divided by the number of organs transplanted.
Donor hospital reimbursements for decedent management from the time of authorization through organ procurement.
Professional expenses including intensive care unit management, imaging interpretation, cardiac echo and catheterization, bronchoscopies, anesthesia, pathology and others.
Transportation costs both for the currying of blood to the reference laboratory for testing as well as transportation of the surgical teams to and from the donor hospital (cab fare, airfare, ambulance, etc.).
Donor “evaluation” laboratory costs run at the Alabama Organ Center reference laboratory on all prospective donors (basic labs including hematology, serum chemistries, liver function testing, coagulation profile and infectious screening including, blood cultures, urine cultures, viral serology and viral nucleic acid NAT-testing).
Tissue Typing (ABO and human leukocyte antigen) costs for all donors in which non-liver organs were being considered for procurement (flat fee, one per donor).
Cross match costs for all renal and pancreas transplants, and some heart and lung transplants (flat fee per cross match performed).
Abdominal organ procurement costs (flat fee paid to surgeon for one or more abdominal organs procured).
Thoracic organ procurement costs (flat fee paid for heart procurement and a flat fee for lung(s) procurement).
Alabama Organ Center Time Utilization
Sum of the time spent by the AOC personnel divided by the number of organs transplanted measured in hours.
Time spent by the AOC donor family support specialist for decedent family counseling and authorization solicitation. This timeframe was determined by subtracting the cross-clamp time from the on-site donor evaluation time.
Time spent by the AOC coordinators for donor evaluation and management, organ procurement and organ allocation. This timeframe was determined by subtracting the case complete time from the donor referral time.
Time spent by the AOC laboratory technician. This timeframe was determined by subtracting the case complete time from the evaluation time.
c) Statistical Analysis
Examination of the data began by examining measures of central tendency (sample mean and median) as well as measures of dispersion (variance, standard deviations). Comparison of average total costs, average cost per organ procured, average cost per organ transplanted, and average time per donor were compared between OPTN eligible and not OPTN eligible using a two-sample t-test assuming unequal variances as well as the non-parametric method Wilcoxon Rank Sum. Due to the method’s robustness to extreme values and outliers, results from the Wilcoxon Rank Sum analyses are reported. Amortized costs were calculated by summing over all costs associated with organ procurement and transplantation and dividing by the total number of organs procured. Because the variable direct cost data are not normally distributed and thus violate one of the key assumptions of the t-test, permutation methods and bootstrapping techniques were employed to calculate p-values comparing amortized costs between OPTN eligible and not OPTN eligible. For each permutation test and bootstrap estimation, 1000 simulations were conducted. All analyses were conducted using the SAS 9.3 (Cary, NC).
Acknowledgments
Research was supported by a grant from the University of Alabama at Birmingham Health Services Foundation (D DuBay), a Charles Barkley Research Award (D DuBay) and NIH NIDDK 1 K23 DK091514 (D DuBay)
Special thanks to Walt Montgomery and Melissa Wallace from the Alabama Organ Center for donor data retrieval.
Abbreviations
- OPTN
Organ Procurement and Transplantation Network
- OPO
Organ Procurement Organization
- AOC
Alabama Organ Center
- OR
Odds Ratio
- 95% CI
95% Confidence Interval
Footnotes
| Author Contributions | |
|---|---|
| Division of Abdominal Transplant Department of Surgery University of Alabama at Birmingham |
DuBay-design, research, writing Gray-design, writing White-design, writing Locke-analysis, writing Eckhoff-design, writing |
| Biostatistics Division School of Public Health University of Alabama at Birmingham |
Redden-analysis |
| Preventive Medicine Department of Medicine University of Alabama at Birmingham |
Fouad-analysis, writing |
| Alabama Organ Center Health Services Foundation Birmingham, AL |
Meeks-analysis, writing Taylor-analysis, writing |
| Dept of Health Care Organization and Policy School of Public Health University of Alabama at Birmingham |
Kilgore-design, analysis, writing |
None of the Authors have any conflicts of interest to report as defined by the journal Transplantation
References
- 1.Anonymous. US Department of Health and Human Services: Donate the gift of life. [cited 2011 March 30]. Available from: http://www.organdonor.gov/research/breakthroughcollaborative.html.
- 2.Anonymous. Organ Procurement and Transplantation Network and Scientific Registry of Transplant Recipients (SRTR) OPTN/SRTR 2010 Annual Data Report. [cited 2011 March 30]. Available from: http://optn.transplant.hrsa.gov/news/newsDetail.asp?id=307.
- 3.Marks WH, Wagner D, Pearson TC, Orlowski JP, Nelson PW, McGowan JJ, et al. Organ donation and utilization, 1995–2004: entering the collaborative era. Am J Transplant. 2006;6(5 Pt 2):1101–10. doi: 10.1111/j.1600-6143.2006.01269.x. Epub 2006/04/15.eng. [DOI] [PubMed] [Google Scholar]
- 4.DuBay DA, Lynch R, Cohn J, Ads Y, Punch JD, Pelletier SJ, et al. Is routine ureteral stenting cost-effective in renal transplantation? J Urol. 2007 Dec;178(6):2509–13. doi: 10.1016/j.juro.2007.08.037. discussion 13. Epub 2007/10/17.eng. [DOI] [PubMed] [Google Scholar]
- 5.Anonymous. Organ Procurement and Transplant Network. 2013 Sep 30; Available from: http://optn.transplant.hrsa.gov/PublicComment/pubcommentPropSub_298.pdf.
- 6.Punch JD, AK, Pietroski RE. Liver Alone donors, a useful, but expensive, source of liver grafts Abstract #33. Vol. 84. International Society of Organ Donation and Procurement; 2009. [cited 2013 February 15]. Available from: http://www.scribd.com/doc/23519561/Design-Fleck-%C2%B7-Zimmermann-Berlin-Fotos-%C2%A9-Bcc-1. [Google Scholar]
- 7.Englesbe MJ, Ads Y, Cohn JA, Sonnenday CJ, Lynch R, Sung RS, et al. The effects of donor and recipient practices on transplant center finances. Am J Transplant. 2008 Mar;8(3):586–92. doi: 10.1111/j.1600-6143.2007.02098.x. Epub 2008/02/26.eng. [DOI] [PubMed] [Google Scholar]
- 8.Axelrod DA, Schnitzler M, Salvalaggio PR, Swindle J, Abecassis MM. The economic impact of the utilization of liver allografts with high donor risk index. Am J Transplant. 2007 Apr;7(4):990–7. doi: 10.1111/j.1600-6143.2006.01724.x. Epub 2007/03/30.eng. [DOI] [PubMed] [Google Scholar]
- 9.Jay CL, Lyuksemburg V, Kang R, Preczewski L, Stroupe K, Holl JL, et al. The increased costs of donation after cardiac death liver transplantation: caveat emptor. Ann Surg. 2010 Apr;251(4):743–8. doi: 10.1097/SLA.0b013e3181d3d3da. Epub 2010/03/13.eng. [DOI] [PubMed] [Google Scholar]