Abstract
Background:
Temper outbursts in youth with obsessive-compulsive disorder (OCD) are a common source of concern, but remain poorly understood. This study examined a set of hypotheses related to: (a) the prevalence of temper outbursts in paediatric OCD, (b) the associations of temper outbursts with OCD severity and depressive symptoms; and (c) the influence of temper outbursts on treatment response.
Methods:
The prevalence of temper outbursts was estimated in a specialist OCD clinical sample (n = 387) using parent- and child-report. This was replicated in a community sample (n = 18,415). Associations of temper outbursts with obsessive-compulsive symptoms and with depressed mood were examined using logistic regression models. The influence of temper outbursts on treatment response was examined in a subsample of 109 patients treated with cognitive behaviour therapy (CBT) with or without medication.
Results:
Over a third of young people with OCD displayed temper outbursts, and rates were similar across the clinical and community samples. Temper outbursts were two to three times more common in youth with OCD than in healthy controls. However, OCD symptom severity was not a strong predictor of child- or parent-reported temper outbursts. Instead, both child- and parent- reported temper outbursts were significantly associated to depressive symptoms. CBT strongly reduced OCD and depressive symptoms, as well as the severity of temper outbursts. There was no significant difference in post-treatment OCD or depression scores between those with temper outbursts compared to those without.
Conclusions:
Temper outbursts are common in youth with OCD and are particularly related to depressed mood. They improve with CBT for OCD and do not seem to impede OCD treatment response.
Keywords: Obsessive-compulsive disorder, paediatric, depression, disruptive behaviour, cognitive behaviour therapy
Introduction
Temper outbursts are a common source of concern in young people with obsessive-compulsive disorder (OCD). Parents of youth with OCD frequently describe their children as having ‘screaming outbursts’ and ‘tantrums lasting several hours every day’.1 This study used a clinical and a community sample to examine: (a) the prevalence of temper outbursts in youth with OCD, (b) the associations of temper outbursts with obsessive-compulsive and depressive symptoms and (c) the influence of temper outbursts on treatment response.
OCD affects 1–4% of young people (Flament et al., 1988; Heyman et al., 2001) and is associated with high comorbidity rates. The reported rates of disruptive behaviour disorders in youth with OCD varies greatly between studies, from 9% (Ivarsson, Melin, & Wallin, 2008) to 57% (Geller, Biederman, Griffin, Jones, & Lefkowitz, 1996). Clinical experience suggests that temper outbursts, which are typically described as a disruptive behaviour, are commonly observed in young people with OCD, and often occur in the context of interruption of rituals and refusal of OCD-related demands. Indirect evidence supporting this anecdotal clinical observation comes from a recent worldwide survey, where a majority of OCD experts reported disruptive behaviours as characterising at least a quarter of their paediatric OCD cases (Lebowitz, Vitulano, Mataix-Cols, & Leckman, 2011). Disruptive behaviours, however, cover a broad range of symptoms, from feelings of anger to premeditated aggressive acts. There are several reasons to view temper outbursts, or irritability more generally, separately from other disruptive behaviours in terms of aetiology (Stringaris, Zavos, Leibenluft, Maughan, & Eley, 2012), longitudinal course (Rowe, Costello, Angold, Copeland, & Maughan, 2010) and potentially treatment responsiveness (Kolko & Pardini, 2010). Although temper outbursts can lead to aggressive behaviours they often simply culminate in verbal outbursts or nonaggressive ‘huffing and puffing’ (Stringaris & Goodman, 2009b).
This study had three aims regarding temper outbursts in childhood OCD. The first aim was to examine the prevalence of temper outbursts in paediatric OCD and compare it to that of other disruptive behaviours, such as fighting or stealing. Consistent with clinical observation, we hypothesised that temper outbursts would be more common than behaviours involving aggression. This was tested in a large clinical sample of children with OCD and replicated in a community sample. Within the community sample, rates of temper outbursts were compared between those with OCD and non-OCD anxiety disorders to test whether temper outbursts were related to anxiety in general or specific to OCD (Stringaris & Goodman, 2009a). Parent- and self-reported measures were used to avoid reporter-specific bias.
The second aim was to study the associations of temper outbursts with obsessive-compulsive and depressive symptoms. First, we tested the clinical notion that temper outbursts are associated with more severe OCD. Previous studies suggest that disruptive behaviours are related to greater OCD severity (Lebowitz, Omer, & Leckman, 2011; Storch, Lewin, Geffken, Morgan, & Murphy, 2010) or to particular OCD symptom dimensions, such as checking (Radomsky, Ashbaugh, & Gelfand, 2007) or hoarding (Storch et al., 2007). However, most previous studies have not distinguished between temper outbursts and aggression or premeditated acts. In a recent study, Storch and colleagues investigated rage attacks specifically, and found a positive association between clinician-rated rage and OCD severity in youth (Storch et al., 2012). Although more narrowly defined than ‘disruptive behaviours’, the construct of rage encompassed verbal attacks, physical aggression and destructive behaviour. Furthermore, rage was associated with disruptive behaviour disorders and the authors noted possible measurement overlap between rage and more general disruptive behaviour.
Second, it was of interest to test whether temper outbursts in youth with OCD are related to depressive symptoms. Previous studies show that the likelihood of manifesting temper outbursts varies according to the likelihood of experiencing negative emotions, such as depression and generalised anxiety (Stringaris, Maughan, & Goodman, 2010). A previous study also shows that temper outbursts, as part of irritability, share common genetic risk factors with depression (Stringaris et al., 2012). Thus, we hypothesised that temper outbursts in childhood OCD would be strongly linked to depressive symptoms. This could have potential therapeutic implications in light of the frequent comorbidity between paediatric OCD and depression (Geller et al., 1996; Heyman, Mataix-Cols, & Fineberg, 2006).
The third aim was to investigate the clinical significance of temper outbursts in children with OCD. First, we tested whether temper outbursts were associated with greater impairment and family accommodation (Langley, Lewin, Bergman, Lee, & Piacentini, 2010; Storch et al., 2010). Furthermore, previous research has shown that disruptive behaviours negatively affect OCD treatment outcome (Garcia et al., 2010; Storch et al., 2008). Therefore, we tested treatment responsiveness of temper outbursts and their effect on treatment outcome.
Methods
Participants
Young people consecutively referred to the national specialist paediatric OCD Clinic at the Maudsley Hospital, London between 2005 and 2011 were included in the current study (n = 387). All data were collected as previously described (Nakatani et al., 2011). Approval for the study was received from the South London and Maudsley Clinical Audit and Effectiveness Committee. All patients met ICD-10 criteria for OCD.
For comparison with the clinic sample, we used published epidemiological data from the British Child and Adolescent Mental Health Surveys of 1999 and 2004 (Ford, Goodman, & Meltzer, 2003; Green, Mcginnity, Meltzer, Ford, & Goodman, 2005) of 18,415 children aged 5–16 years. Diagnoses were assigned using the Development and Well-Being Assessment (Goodman, Ford, Richards, Gatward, & Meltzer, 2000), which was completed by all parents and young people aged 11–16. In addition, parents and young people aged 11–16 completed the Strengths and Difficulties Questionnaire (Goodman, 2001).
Measures
The Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) is a standard clinician-administered measure for OCD symptom severity (Scahill et al., 1997). The symptom checklist was used to calculate scores on the four OCD symptom dimensions (Bloch, Landeros-Weisenberger, Rosario, Pittenger, & Leckman, 2008).
The Children’s Obsessive-Compulsive Inventory (ChOCI) is a questionnaire assessing obsessive-compulsive symptoms in young people and has a parent- and child-version (Uher, Heyman, Turner, & Shafran, 2008).
The Strengths and Difficulties Questionnaire (SDQ) (Goodman, 2001) is a 25-item questionnaire capturing emotional, conduct and hyperactivity/inattention symptoms, peer problems and pro-social behaviour and assesses impact. The conduct subscale comprises five items, which probe for presence of fighting, lying, stealing, disobedience and temper outbursts. This last item was used to measure temper outbursts in this study. Items are rated as ‘not true’, ‘somewhat true’ or ‘certainly true’; the two lowest categories were combined for use in graphs.
The Beck Depression Inventory for Youth (BDI-Y) is a self-report measure for depressive symptoms. Unlike the adult version, the BDI-Y does not include an irritability item. The generally accepted T-score cut-off of ≥55 was used as an indicator of clinical depression in the clinical OCD sample (Beck, Beck, & Jolly, 2001).
The Family Accommodation Scale (FAS) is a parent-report measure of parental involvement in their offspring’s OCD symptoms. It consists of four subscales (Participation, Modification, Distress and Consequences) (Peris et al., 2008). In this study, we used maternal-reported FAS scores.
The parent-report of the Development and Well-Being Assessment (Goodman et al., 2000), was available in a subset of the clinical sample (n = 263, 68%). It includes three items on irritability (Stringaris & Goodman, 2009b), which were endorsed by n = 83 (21%) of parents. The sum of these items was significantly correlated with parent-, but not child-reported temper outbursts as measured using the SDQ: r = 0.49, p < 0.001 and r = 0.19, p = 0.11, respectively.
Treatment
Cognitive behaviour therapy (CBT) was protocol-driven and focused on exposure with response prevention. Parents were involved in CBT sessions to varying degrees depending on the developmental level of the young person and the extent to which parents were involved in their child’s rituals (Nakatani et al., 2011). Patients who received CBT and had post-treatment data available (n = 109) were generally geographically nearer to the clinic compared with those who were treated elsewhere. There were no differences in clinical/demographic variables between those with and without post-treatment data. A proportion (40%) received medication. In most cases, medication had reached a stable dose before CBT commenced. Those receiving medication had a higher CY-BOCS total score than those not on medication (29.6 vs. 25.4, SD = 6.5, p < 0.001), but did not differ in terms of age, gender, or prevalence of temper outbursts.
Statistical analysis
We estimated the prevalence of temper outbursts by using proportions and confidence intervals. In the epidemiological sample, we tested the difference between youth with OCD, non-OCD anxiety disorders and healthy controls using Chi-squared tests. To address the second aim, logistic regression models tested whether temper outbursts were predicted by OCD severity or symptom dimension scores, or depressive symptoms. Sobel–Goodman mediation tests were used to test for the mediating effect of depressed mood in the relationship between temper outbursts and OCD. To address the third aim, linear regression was used with temper outbursts as the predictor of the impact scores of the SDQ and the FAS. To test the effect of temper outbursts on treatment, linear regression models were used with post-treatment OCD and depressive scores as the outcome and temper outbursts as the predictor. Effect sizes (calculated by dividing the mean of the differences by the standard deviation) were used to assess the impact of temper outbursts on symptom change. Subsequently, baseline levels of OCD and depressive symptoms were used as covariates in the regression models to test for interaction effects. Significance was set at the p-value of 0.05. The Bonferroni method was used to correct for multiple testing.
Results
Attrition analysis
There were no differences in demographic/clinical characteristics between individuals with and without complete data on any of the measures used in this study (see online appendix, Table S1).
Characteristics of the two samples
Within the clinic sample, the mean age was 14.4 years (SD = 2.24, range 7–18) and mean age at onset of OCD was 10.7 years (SD = 3.15, range 3–18). The mean CY-BOCS total score was 26.31 (SD = 5.63), indicating moderate severity. As an approximation of comorbidity rates, SDQ subscale scores were dichotomised as being above or below the clinical cut-off (see online appendix, Table S2).In addition, the sum of four emotional items of the SDQ (somatic complaints, worries, nervousness and fears) was used as a measure for anxiety symptom severity. The mean anxiety scores were 5.07 (95% CI = 4.85–5.30) and 5.34 (95% CI = 5.11–5.57) for child- and parent-report respectively.
Table 1 shows the comorbidity rates of the OCD group in the community sample as measured using the DAWBA. Youth with OCD in the community sample scored significantly higher than healthy controls on both the child- [4.18 (SD = 1.91) vs. 2.35 (SD = 1.71), p < 0.001] and parent-reported anxiety scale [4.13 (SD = 2.50) vs. 1.49 (SD = 1.58), p < 0.001].
Table 1.
Comorbidity rates in youth with OCD in the community sample (n = 40)
| Comorbid diagnosis | Numbers (%) of cases |
|---|---|
| Non-OCD anxiety disorder | 14 (35.0) |
| Oppositional defiant disorder | 9 (22.5) |
| Depressive disorder | 7 (17.5) |
| ADHD | 3 (7.5) |
| Conduct disorder | 2 (5.0) |
| Pervasive developmental disorder | 1 (2.5) |
| Eating disorder | 1 (2.5) |
OCD, obsessive-compulsive disorder; ADHD, attention deficit hyperactivity disorder.
Aim 1: Prevalence of temper outbursts in childhood OCD
Clinic sample
Temper outbursts were endorsed as ‘certainly true’ on the SDQ by 38.5% (95% CI = 32.9–44.0%) of young people with OCD in the clinical sample, and 43.5% (95% CI = 38.0–49.0%) of their parents (Figure 1). The intraclass correlation coefficient between parent- and self-report of temper outbursts was 0.32 (p < 0.001).
Figure 1.
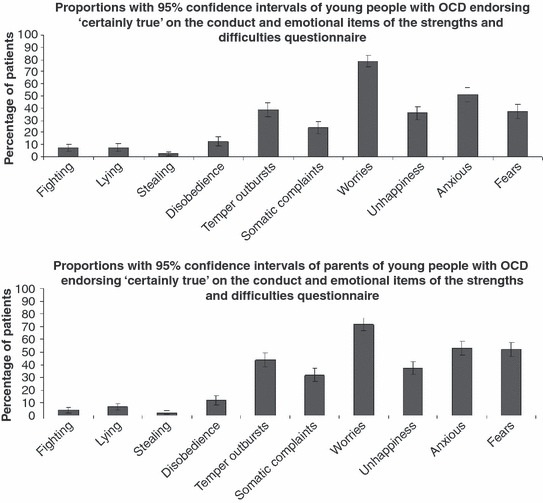
Prevalence rates of the conduct and emotional SDQ items in youth with OCD in the clinical sample
Temper outbursts were significantly more common (all p < 0.001) than other SDQ conduct items, e.g. 11 times more common than fighting on the parent-report, and occurred with similar frequency to emotional items on the SDQ (Figure 1).
There were no gender differences in the prevalence of temper outbursts by either child- (42.9% in female subjects vs. 34.9% in male subjects, χ2 = 3.73, df = 2, p = 0.155) or parent-report (43.1% in female subjects vs. 43.8% in male subjects, χ2 = 0.33, df = 2, p = 0.848). Both parent- (15.2 years vs. 14.0 years, p = 0.002) and child-reported temper outbursts were commoner in younger children (14.9 years vs. 13.9 years, p = 0.002).
Community sample
In the community sample n = 40 (0.2%) received a diagnosis of OCD. Temper outbursts were endorsed as ‘certainly true’ on the SDQ by 28.6% (95% CI = 10.7–46.4%) of young people with OCD and 38.5% (95% CI = 22.5–54.4%) of parents. As with the clinic sample, temper outbursts were endorsed more frequently than other SDQ conduct items, but occurred with similar frequency to SDQ emotional items (see online appendix, Figure S1).
As in the clinical sample, there were no gender differences in the prevalence of temper outbursts by either child- (41.7% in female subjects vs. 18.8% in male subjects, Fisher’s exact p = 0.277) or parent-report (38.9% in female subjects vs. 38.1% in male subjects, χ2 = 0.004, df = 2, p = 0.998). Both parent- (13.7 years vs. 10.5 years, p = 0.006) and child-reported temper outbursts were commoner in younger children (14.5 years vs. 13.4 years, p = 0.065).
Temper outbursts were significantly more prevalent in OCD than in healthy controls on both child- (28.6% vs. 11.7%, Fisher’s exact p = 0.027) and parent-report (38.5% vs. 11.3%, p < 0.001). They were equally common in OCD and non-OCD anxiety disorders [n = 614 (3.3%)], by both child- (28.6% vs. 31.9%, χ2 = 5.94, df = 2, p = 0.051) and parent-report (38.5% vs. 40.0%, χ2 = 0.14, df = 2, p = 0.933). Further information about the group with non-OCD anxiety disorders is presented in text-box A of the online appendix.
Aim 2: The association of temper outbursts with obsessive-compulsive and depressive symptoms
Temper outbursts and OCD symptoms
Figure 2 (top panel) demonstrates that CY-BOCS total scores did not vary by the level of temper outbursts. In logistic regression models, CY-BOCS total score was not a significant predictor of child- [OR = 1.02 (95% CI = 0.98–1.06), p = 0.416] or parent-reported temper outbursts [OR = 1.02 (95% CI = 0.98–1.06), p = 0.369].
Figure 2.
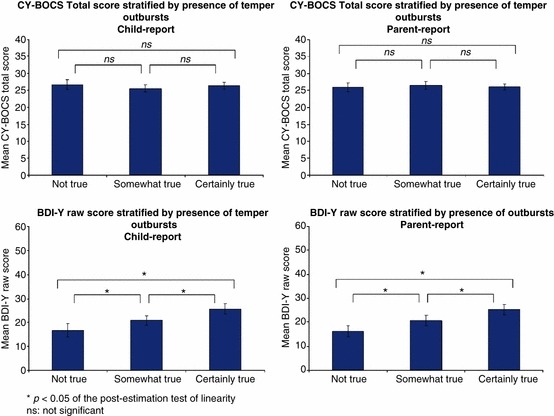
Variation in OCD (top) and depressive symptoms (bottom) by presence of temper outbursts
It is unlikely that these negative findings can be accounted for by a lack of variance in CY-BOCS total scores, because the CY-BOCS total score was normally distributed in our sample (Shapiro–Wilks test p = 0.327); and the CY-BOCS total score significantly predicted child- and parent-reported SDQ emotional items (Table S2 and Figure S2 in the online appendix) and BDI-Y raw score [β = 0.74 (95% CI = 0.54–0.95), p < 0.001]. Moreover, lack of power is unlikely to explain these negative findings. Our sample size afforded us a power of 1.00 for finding a difference of five points in CY-BOCS total score between the lower and the upper category of the temper outbursts item on both parent- and child-report.
None of the OCD symptom dimensions were significant predictors of child- or parent-reported temper outburst after corrected for multiple testing. (online appendix, Table S2).
These negative findings were explored in a further set of analyses. In particular, we wanted to exclude the possibility that lack of association between temper outbursts and OCD severity was due to reporting-source effects. This could have happened because the CY-BOCS is clinician-rated, whereas the BDI-Y is rated by the child (as is the child temper outbursts item). We therefore repeated the analyses using the child- and parent-reported ChOCI as predictors. On the basis of our previous findings, child-reported temper outbursts were not significantly predicted by the parent-reported ChOCI total score [OR = 1.02 (95% CI = 0.99–1.04), p = 0.228]. However, parent-reported temper outbursts were significantly predicted by the child ChOCI total [OR = 1.04 (95% CI = 1.01–1.06), p = 0.012]. Also, parent ChOCI total score was a significant predictor of parent-reported temper outbursts [OR = 1.04 (95% CI = 1.02–1.07), p = 0.001].
Temper outbursts and depressed mood
Figure 2 (bottom panel) shows that BDI-Y scores varied significantly by level of temper outbursts for both child- and parent-report. Indeed, even after controlling for age and gender, child-reported temper outbursts were significantly predicted by BDI-Y raw score [OR = 1.06 (95% CI = 1.03–1.08), p < 0.001]. Even across informants, BDI-Y raw score significantly predicted parent-reported temper outbursts [OR = 1.06 (95% CI = 1.04–1.08), p < 0.001].
Temper outbursts were significantly more prevalent in the depressed group (BDI-Y T-score ≥55) compared with the nondepressed group (Figure 3), with respect to both child- (47.1% vs. 29.1%, χ2 = 9.17, df = 2, p = 0.010) and parent-reported temper outbursts (42.9% vs. 28.1%, χ2 = 6.98, df = 2, p = 0.031).
Figure 3.
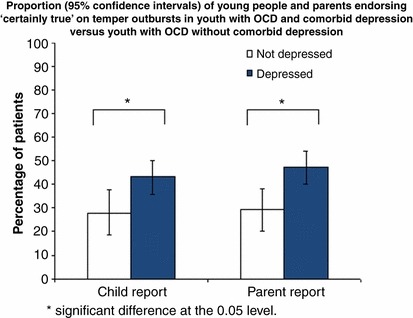
Proportion of depressed versus nondepressed youth with OCD endorsing the temper outburst item
In the community sample, we explored whether the presence of comorbid depression would be associated with higher rates of temper outbursts in the non-OCD anxiety group. We found that both child-reported (45.45% vs. 28.86%, χ2 = 5.70, df = 1, p = 0.02) and parent-reported temper outbursts (51.43% vs. 38.53%, χ2 = 4.30, df = 1, p = 0.04) were more common in those with comorbid depression than in those without.
Post hoc analyses
We studied the role of depressive symptoms in the relationship between ChOCI scores and temper outbursts. Indeed, the association between parent-reported temper outbursts and child ChOCI total score became nonsignificant after mediation analysis with BDI-Y raw score as the mediator (Sobel’s test for mediation; p < 0.001). A association remained between parent ChOCI total score and parent-reported temper outbursts (p = 0.001).
Aim 3: The relationship between temper outbursts, impairment and treatment outcome
Association with impairment and family accommodation
Youth with temper outbursts scored significantly higher on the impact score of the SDQ over and above OCD severity [β = 0.91 (95% CI = 0.40–1.42), p < 0.001], as did their parents [β = 1.04 (95% CI = 0.51–1.57), p < 0.001]. Table 2 shows that both parent- and child-reported temper outbursts significantly predicted maternal FAS scores, particularly the Consequences subscale. BDI-Y raw score only played a significant mediating role in the relationship between child-reported temper outbursts and the Consequences subscale.
Table 2.
Regression coefficients for the relationship between maternal FAS (outcome) and temper outbursts (predictor), including the proportion of this association mediated by depressive symptoms
| Child report | Proportion mediated by BDI-Y raw score (%) | Parent report | Proportion mediated by BDI-Y raw score (%) | |
|---|---|---|---|---|
| Total score | 1.64c | – | 4.81a | 15c |
| Participation score | 0.60c | – | 1.67a | 17c |
| Modification score | 0.09c | – | 1.08a | 28c |
| Distress score | 0.54c | – | 0.33a | 13c |
| Consequences score | 1.23a | 27b | 2.09a | 8c |
BDI-Y, Beck Depression Inventory for Youth; FAS, Family Accommodation Scale.
Significant at the 0.01 level.
Significant at the 0.05 level in the Sobel mediation test.
Not significant at the 0.05 level.
Treatment response
Effect of temper outbursts on change in CY-BOCS scores: The top panels of Figure 4 show that youth with and without temper outbursts had similar post-treatment CY-BOCS scores, indicating that temper outbursts were not significant predictors [child-report: β = 0.25 (95% CI = −2.08 to 2.57), p = 0.834; parent-report: β = 1.15 (95% CI = −1.18 to 3.47), p = 0.329]. Also, CY-BOCS scores changed at a similar rate [child-report: β = −0.12 (95% CI = −0.45 to 0.22), p = 0.486; parent-report: β = −0.022 (95% CI = −0.33 to 0.29), p = 0.887].
Figure 4.
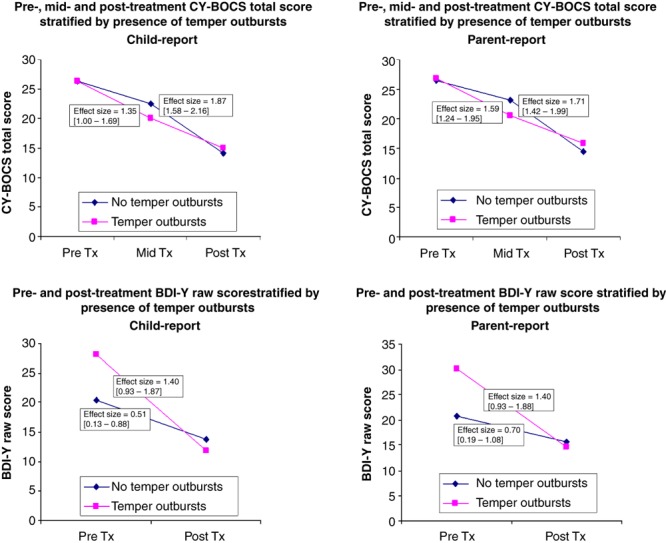
Effects of the presence of temper outbursts on treatment response in relation to obsessive-compulsive (top) and depressive symptoms (bottom)
Effect of temper outburst on change in BDI-Y scores: The bottom panels of Figure 4 show that patients with and without temper outbursts had similar post-treatment BDI-Y raw scores, indicating that temper outbursts were not significant predictors [child-report: β = 0.88 (95% CI = −4.76 to 3.01), p = 0.653; parent-report: β = −0.28 (95% CI = −5.21 to 4.64) p = 0.908]. In contrast, BDI-Y scores changed more rapidly for those with temper outbursts than those without, also illustrated by the difference in treatment effect size between those with and without temper outbursts [child-report: 1.40 (95% CI = 0.93–1.87) vs. 0.51 (95% CI = 0.13–0.88), p = 0.001; and parent-report: 1.40 (95% CI = 0.92–1.88) vs. 0.70 (95% CI = 0.19–1.08), p = 0.003]. However, this became non significant once baseline BDI-Y score was taken into account in the parent-[β = −0.18 (95% CI = −0.50 to 0.15), p = 0.274], but not child-report [β = −0.30 (95% CI = −0.56 to −0.05), p = 0.021].
Changes in temper outbursts with treatment: Child-reported temper outbursts decreased by 61% (χ2 = 17.89, df = 4, p = 0.001) and parent-reported temper outbursts decreased by 35% (χ2 = 19.56, df = 4, p = 0.001).
Post hoc analyses: Medication status did not influence the above results (online appendix Table S5).
Discussion
This study showed that temper outbursts are common in young people with OCD and best predicted by depressive symptoms, rather than by OCD symptoms. As expected, CBT strongly reduced OCD symptoms as well as temper outbursts and depressive symptoms. Also, depressive symptoms decreased more rapidly in those with temper outbursts compared to those without.
The first aim was to establish the prevalence of temper outbursts in young people with OCD. We found that temper outbursts were common and affected over a third of young people with OCD attending a specialist clinic, consistent with impressions of expert clinicians (Lebowitz, Vitulano, et al., 2011). These rates are unlikely to reflect referral or Berkson biases, as rates of temper outbursts were similar in the community sample. In addition, temper outbursts were similar between OCD and non-OCD anxiety disorders, suggesting a nonspecific relationship between temper outbursts and anxiety disorders, perhaps indicating that temper outbursts reflect negative affectivity in young people. Temper outbursts were more common than other disruptive behaviours (e.g. 11 times more common than parent-reported fighting), but occurred with similar frequency to emotional symptoms.
Our second aim was to examine the associations of temper outbursts with obsessive-compulsive and depressive symptoms. We found that temper outbursts were more common in OCD compared to healthy controls. However, temper outbursts did not vary by OCD severity: there was no association with CY-BOCS or child-reported ChOCI, and only parent-reported ChOCI was weakly associated with parent-reported temper outbursts. This apparent lack of association is unlikely to be due to lack of statistical power or variance in this sample. There was also no association between temper outbursts and any of the OCD symptom dimensions. This contrasts with previous findings that disruptive behaviours and rage are associated with greater OCD severity (Lebowitz, Omer, et al., 2011; Storch et al., 2012) and symptoms of checking and hoarding (Radomsky et al., 2007; Storch et al., 2007). This again highlights the importance of distinguishing temper outbursts from other disruptive behaviours. Our results appear consistent with a threshold effect of OCD on temper outbursts: after passing a certain severity level, further increases in OCD symptoms have little bearing on temper outbursts.
This study found that temper outbursts in youth with OCD are strongly related to depressive symptoms. And this positive relationship was also found among young people with non-OCD anxiety disorders in the community sample. This is consistent with previous research showing that irritability in childhood (of which temper outbursts are a part) predicts depression in later life (Stringaris & Goodman, 2009a), and that this may be due to shared genetic risk factors (Stringaris et al., 2012). This raises the possibility of a temperamental vulnerability that is associated with affective symptoms and irritability (Stringaris et al., 2010).
The final aim of the present study was to investigate the clinical significance of temper outbursts in youth with OCD. This study shows that both parent- and child-reported temper outbursts were associated with greater impairment, highlighting the clinical importance of these behaviours. Furthermore, temper outbursts also predicted maternal accommodation of OCD symptoms, possibly reflecting mothers’ attempts to reduce temper outbursts. Encouragingly, we found that temper outbursts significantly diminished after manualised CBT for OCD that incorporated conventional psychoeducation, exposure with response prevention and relapse prevention. Given the design, we were not able to test possible mediators of change in the current study, and this should be examined in future studies including multiple time points. However, the decrease in temper outbursts may reflect a reduction in depressive symptoms over the course of CBT as the young person’s OCD symptoms improve, which is similar to previous studies demonstrating that depression tends to be secondary to OCD and disappears following remission of OCD symptoms [e.g.(Zitterl et al., 2000)].
Importantly, we found that temper outbursts did not predict or moderate post-treatment obsessive-compulsive symptoms. This is in contrast with previous studies showing that disruptive behaviours in general predict poorer CBT outcome (Garcia et al., 2010; Storch et al., 2008). This discrepancy may reflect differences in the behavioural symptoms being studied; our study focused on temper outbursts specifically, as opposed to the broader range of disruptive behaviours that have been examined previously. Interestingly, whereas temper outburst were common in our sample, other disruptive behaviours were not.
Alternatively, the discrepancy may be accounted for by varying characteristics of CBT between studies. In this study, it was clinical practice routinely to involve parents in CBT sessions. They were taught how to assist their child in exposure with response prevention using contingency management strategies to reinforce their child’s attempts to overcome symptoms. In a recent worldwide survey, 86% of OCD experts report that parent training is the intervention of choice for coercive behaviours in paediatric OCD (Lebowitz, Vitulano, et al., 2011), and a number of single case reports have highlighted successful use of parent training in conjunction with CBT for individuals with comorbid OCD and ODD [e.g. (Ale & Krackow, 2011)]. Our findings suggest that for children with temper outbursts as opposed to disruptive behaviour disorders, CBT with parental involvement may be an effective treatment, suggesting that additional parenting interventions may not be necessary in these cases. It should be noted that in the current study the extent of parental involvement was flexible, and it is possible that it varied depending on the presence of temper outbursts.
Our findings also show that temper outbursts were not a predictor of post-treatment depressive symptoms. However, the effect sizes for those with temper outbursts were at least two times higher than for those without. For child-, but not parent-report, treatment moderation remained significant, even after adjusting for the higher BDI-Y scores at baseline among those young people with temper outbursts. There was no a priori hypothesis with regard to these findings and replication is needed before drawing further inferences.
This study has a number of methodological strengths, such as the combined use of a large clinical sample with treatment follow-up and a large epidemiological sample, and the use of multiple informants. There are also several limitations. First, the measure of temper outbursts used in this study did not capture the functionality of this behaviour and furthermore, the measure was a single item. However, our findings held across parent- and child-report, showing that chance is an unlikely explanation for our findings. Moreover, temper outbursts as measured in this study correlated strongly with a previously used irritability measure (Stringaris & Goodman, 2009a) within a subsample that had these data available. Second, our findings might be limited by the naturalistic design of this study. However, we demonstrated no differences between those with complete and missing data, and hence this was unlikely to have influenced our results. Third, it is of note that the prevalence of OCD in the community sample was relatively low. However, as discussed by Heyman et al. ()2001, this is probably due to the younger age of this sample compared with most other epidemiological studies. Fourth, we were limited by the differences in treatment packages between young people, i.e. although treatment was protocol-driven, it was not consistently the same for every patient as in treatment trials. However, we showed that this is unlikely to have influenced our findings. Finally, within the clinical sample, depression was not assessed using a structured diagnostic instrument; instead BDI-Y scores were used to classify patients as depressed.
In summary, this study offers empirical evidence that temper outbursts are common in youth with OCD and non-OCD anxiety disorders and that they are particularly associated with depressed mood. Importantly, they improve with treatment and do not seem to influence the outcome of CBT for OCD. Future studies should examine the mechanisms underlying the association between temper outbursts and depressed mood in young people with OCD.
Key points
Temper outbursts are common in young people with OCD and other anxiety disorders, relative to healthy controls. They are more common than other disruptive behaviours, but occur with similar frequency to symptoms of emotional distress.
Temper outburst are not associated with severity or type of OCD symptoms. However, they are strongly related to depressive symptoms.
Importantly, temper outbursts decrease following CBT for OCD and the presence of temper outbursts at baseline does not predict CBT outcome.
Temper outbursts may be a marker of emotional distress in young people with OCD, and CBT for OCD is equally effective for those with and without temper outbursts.
Acknowledgments
The authors are grateful to Professor Goodman, Institute of Psychiatry, London, for providing the B-CAMHS sample and for critical discussions on earlier drafts. This study was partly funded by a grant from the South London and Maudsley NHS Foundation Trust. A.S. gratefully acknowledges the support of the Wellcome Trust. G.K. and K.B. should be regarded as joint first authors for this publication
Footnotes
Quotes from parents systematically collected prior to their child’s assessment at the OCD Clinic.
Correspondence
Georgina Krebs, OCD Clinic for Young People, South London and Maudsley Hospital, De Crespigny Park, London SE5 8AZ, UK; Email: georgina.krebs@slam.nhs.uk
Supporting information
Additional supporting information may be found in the online version of this article:
Table S1 Comparison of demographic characteristics in young people with complete and missing data
Table S2 Percentage of young people with OCD in the clinical (middle column) and epidemiological sample (right column) falling into the abnormal range of the SDQ subscales (parent report)
Table S3 Percentage of young people with OCD in the clinical (middle column) and epidemiological sample (right column) falling into the abnormal range of the SDQ subscales (child report)
Table S4 Logistic regression coefficients of the emotional items of the SDQ and the CY-BOCS
Table S5 Treatment analyses by medication status at baseline. *Significant at 0.05 level. **Significant at 0.05 level
Figure S1 Percentages of young people andparents endorsing ‘certainly true’ on the conduct and emotional SDQ items (community sample)
Figure S2 Bar graphs of mean CY-BOCS total scores for the categories of SDQ items
Supporting info item
References
- Ale CM. Krackow E. Concurrent treatment of early childhood OCD and ODD: A case illustration. Clinical Case Studies. 2011;10:312–323. [Google Scholar]
- Beck JS, Beck AT. Jolly JB. Beck youth inventories for children and adolescents. San Antonio, TX: The Psychological Corporation; 2001. [Google Scholar]
- Bloch MH, Landeros-Weisenberger A, Rosario MC, Pittenger C. Leckman JF. Meta-analysis of the symptom structure of obsessive-compulsive disorder. American Journal of Psychiatry. 2008;165:1532–1542. doi: 10.1176/appi.ajp.2008.08020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flament MF, Whitaker A, Rapoport JL, Davies M, Berg CZ, Kalikow K. Shaffer D. Obsessive compulsive disorder in adolescence: An epidemiological study. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:764–771. doi: 10.1097/00004583-198811000-00018. [DOI] [PubMed] [Google Scholar]
- Ford T, Goodman R. Meltzer H. The British Child and Adolescent Mental Health Survey 1999: The prevalence of DSM-IV disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- Garcia AM, Sapyta JJ, Moore PS, Freeman JB, Franklin ME, March JS. Foa EB. Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1024–1033. doi: 10.1016/j.jaac.2010.06.013. quiz 1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller DA, Biederman J, Griffin S, Jones J. Lefkowitz TR. Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1637–1646. doi: 10.1097/00004583-199612000-00016. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Goodman R, Ford T, Richards H, Gatward R. Meltzer H. The Development and Well-Being Assessment: Description and initial validation of an integrated assessment of child and adolescent psychopathology. Journal of Child Psychology and Psychiatry. 2000;41:645–655. [PubMed] [Google Scholar]
- Green H, Mcginnity A, Meltzer H, Ford T. Goodman R. Mental health of children and young people in Great Britain, 2004. Basingstoke: Palgrave MacMillan; 2005. [Google Scholar]
- Heyman I, Fombonne E, Simmons H, Ford T, Meltzer H. Goodman R. Prevalence of obsessive-compulsive disorder in the British nationwide survey of child mental health. British Journal of Psychiatry. 2001;179:324–329. doi: 10.1192/bjp.179.4.324. [DOI] [PubMed] [Google Scholar]
- Heyman I, Mataix-Cols D. Fineberg NA. Obsessive-compulsive disorder. British Medical Journal. 2006;333:424–429. doi: 10.1136/bmj.333.7565.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivarsson T, Melin K. Wallin L. Categorical and dimensional aspects of co-morbidity in obsessive-compulsive disorder (OCD) European Child & Adolescent Psychiatry. 2008;17:20–31. doi: 10.1007/s00787-007-0626-z. [DOI] [PubMed] [Google Scholar]
- Kolko DJ. Pardini DA. ODD dimensions, ADHD, and callous-unemotional traits as predictors of treatment response in children with disruptive behavior disorders. Journal of Abnormal Psychology. 2010;119:713–725. doi: 10.1037/a0020910. [DOI] [PubMed] [Google Scholar]
- Langley AK, Lewin AB, Bergman RL, Lee JC. Piacentini J. Correlates of comorbid anxiety and externalizing disorders in childhood obsessive compulsive disorder. European Child & Adolescent Psychiatry. 2010;19:637–645. doi: 10.1007/s00787-010-0101-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz ER, Omer H. Leckman JF. Coercive and disruptive behaviors in pediatric obsessive-compulsive disorder. Depression and Anxiety. 2011;28:899–905. doi: 10.1002/da.20858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz ER, Vitulano LA, Mataix-Cols D. Leckman JF. Editorial perspective: when OCD takes over … the family! Coercive and disruptive behaviours in paediatric obsessive compulsive disorder. Journal of Child Psychology and Psychiatry. 2011;52:1249–1250. doi: 10.1111/j.1469-7610.2011.02480.x. [DOI] [PubMed] [Google Scholar]
- Nakatani E, Krebs G, Micali N, Turner C, Heyman I. Mataix-Cols D. Children with very early onset obsessive-compulsive disorder: Clinical features and treatment outcome. Journal of Child Psychology and Psychiatry. 2011;52:1261–1268. doi: 10.1111/j.1469-7610.2011.02434.x. [DOI] [PubMed] [Google Scholar]
- Peris TS, Bergman RL, Langley A, Chang S, Mccracken JT. Piacentini J. Correlates of accommodation of pediatric obsessive-compulsive disorder: Parent, child, and family characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:1173–1181. doi: 10.1097/CHI.0b013e3181825a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radomsky AS, Ashbaugh AR. Gelfand LA. Relationships between anger, symptoms, and cognitive factors in OCD checkers. Behaviour Research and Therapy. 2007;45:2712–2725. doi: 10.1016/j.brat.2007.07.009. [DOI] [PubMed] [Google Scholar]
- Rowe R, Costello EJ, Angold A, Copeland WE. Maughan B. Developmental pathways in oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology. 2010;119:726–738. doi: 10.1037/a0020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scahill L, Riddle MA, Mcswiggin-Hardin M, Ort SI, King RA, Goodman WK. Leckman JF. Children’s Yale-Brown Obsessive Compulsive Scale: Reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB. Murphy TK. Rage attacks in pediatric obsessive-compulsive disorder: Phenomenology and clinical correlates. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:582–592. doi: 10.1016/j.jaac.2012.02.016. [DOI] [PubMed] [Google Scholar]
- Storch EA, Lack CW, Merlo LJ, Geffken GR, Jacob ML, Murphy TK. Goodman WK. Clinical features of children and adolescents with obsessive-compulsive disorder and hoarding symptoms. Comprehensive Psychiatry. 2007;48:313–318. doi: 10.1016/j.comppsych.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Storch EA, Lewin AB, Geffken GR, Morgan JR. Murphy TK. The role of comorbid disruptive behavior in the clinical expression of pediatric obsessive-compulsive disorder. Behaviour Research and Therapy. 2010;48:1204–1210. doi: 10.1016/j.brat.2010.09.004. [DOI] [PubMed] [Google Scholar]
- Storch EA, Merlo LJ, Larson MJ, Geffken GR, Lehmkuhl HD, Jacob ML. Goodman WK. Impact of comorbidity on cognitive-behavioral therapy response in pediatric obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:583–592. doi: 10.1097/CHI.0b013e31816774b1. [DOI] [PubMed] [Google Scholar]
- Stringaris A. Goodman R. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the American Academy of Child and Adolescent Psychiatry. 2009a;48:404–412. doi: 10.1097/CHI.0b013e3181984f30. [DOI] [PubMed] [Google Scholar]
- Stringaris A. Goodman R. Three dimensions of oppositionality in youth. Journal of Child Psychology and Psychiatry. 2009b;50:216–223. doi: 10.1111/j.1469-7610.2008.01989.x. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Maughan B. Goodman R. What’s in a disruptive disorder? Temperamental antecedents of oppositional defiant disorder: Findings from the Avon longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:474–483. doi: 10.1097/00004583-201005000-00008. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Zavos H, Leibenluft E, Maughan B. Eley TC. Adolescent irritability: Phenotypic associations and genetic links with depressed mood. American Journal of Psychiatry. 2012;169:47–54. doi: 10.1176/appi.ajp.2011.10101549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uher R, Heyman I, Turner CM. Shafran R. Self-, parent-report and interview measures of obsessive-compulsive disorder in children and adolescents. Journal of Anxiety Disorders. 2008;22:979–990. doi: 10.1016/j.janxdis.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Zitterl W, Demal U, Aigner M, Lenz G, Urban C, Zapotoczky HG. Zitterl-Eglseer K. Naturalistic course of obsessive compulsive disorder and comorbid depression. Longitudinal results of a prospective follow-up study of 74 actively treated patients. Psychopathology. 2000;33:75–80. doi: 10.1159/000029124. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


