Abstract
Data suggest anxious drivers may engage in problematic behaviors that place themselves and others at increased risk of negative traffic events. Three domains of problematic behavior – exaggerated safety/caution, performance deficits, and hostile/aggressive behaviors – previously were identified during development of the Driving Behavior Survey (DBS), a novel measure of anxiety-related behavior. Extending this research, the current study examined the psychometric properties of DBS scores among individuals with posttraumatic stress disorder (PTSD) subsequent to motor vehicle trauma (N = 40). Internal consistencies and 12-week test-retest reliabilities for DBS scales ranged from good to excellent. Comparison of scores to normative student data indicated dose-response relationships for safety/caution and performance deficit subscales, with increased frequency of anxious behavior occurring within the PTSD sample. Associations with standard clinical measures provide additional evidence for anxiety-related driving behavior as a unique marker of functional impairment, distinct from both avoidance and disorder-specific symptoms.
Keywords: driving anxiety, driving behavior, motor vehicle accident, posttraumatic stress disorder, assessment
Evidence from the clinical and traffic safety literatures indicate associations between elevated anxiety and problematic driving behaviors including performance errors, attentional lapses, aggressive violations, and at-fault collisions (e.g., Dula, Adams, Miesner, & Leonard, 2010; Matthews et al., 1998; Shahar, 2009; Taylor & Koch, 1995). Further research suggests these effects may be particularly robust among individuals with driving-specific fear (e.g., Taylor, Deane, & Podd, 2007a). The implications of this research for behavioral intervention have motivated recent efforts to isolate and assess specific domains of anxiety-related driving behavior (Clapp, Olsen, Beck, et al., 2011). The aim of the present study was to evaluate the measurement properties of a novel measure of anxious driving behavior within a help-seeking sample of motor vehicle accident (MVA) survivors.
The influence of trait-level anxiety on driving performance is a common subject of investigation within the transportation and traffic safety literatures. While the relationship between these constructs is complex (see Taylor, Deane, & Podd, 2008 for a comprehensive review), several studies provide evidence for a detrimental effect of generalized trait-anxiety on driving performance. Early research by Shoham, Geva, Markovski, and Kaplinsky (1976) proposed that “anxious” drivers may be at similar risk of dangerous behavior as “reckless” drivers based on archival data of Israeli motorists. Follow-up analysis supported this hypothesis, noting significant associations between anxiety and the occurrence of traffic offenses (Shoham, Rahav, Markovski, Chard, & Baruch, 1984). Contemporary research also indicates associations between characterological anxiety and problematic traffic outcomes including risky driving behavior, performance deficits, aggressive violations, and at-fault accidents (Dula et al., 2010; Fairclough, Tattersall, & Houston, 2006; Lucidi et al., 2010; Shahar, 2009).
Further evidence of problematic behavior is noted in research detailing the impact of driving-specific fear. Treatment manuals and clinical reviews indicate a range of maladaptive behavior (e.g., skill deficits, excessive caution, erratic driving) as a consequence of driving anxiety related to phobia, panic, and posttraumatic stress (Antony, Craske, & Barlow, 2006; Koch & Taylor, 1995; Taylor, Deane, & Podd, 2002; Taylor & Koch, 1995). Problematic behavior detailed in this literature is supported through both self-report and observational studies involving fearful drivers. In an analysis of Greek motorists, Kontogiannis (2006) observed that driving-specific anxiety was associated with greater occurrence of driving errors controlling for age, gender, driving experience, and annual mileage. Similarly, Matthews et al. (1998) found driving anxiety to be associated with performance errors and poor vehicle control within the context of a driving simulation task. Most recently, Taylor et al. (2007a) evaluated driving proficiency on a standardized road test among motorists selected for high- and low-levels of driving fear. Anxious drivers in this study committed a greater number of traffic errors and rated themselves as having poorer driving skill relative to non-anxious controls. Observations provided by road test administrators further corroborated lower levels of skill within the subset of anxious motorists. In sum, convergent evidence from these literatures suggests a range of maladaptive behaviors characteristic of individuals who continue to drive despite feeling anxious. Assessment of these behaviors is important for both (a) understanding risk factors and processes contributing to driving-related impairment, and (b) expanding systematic evaluation of interventions targeting travel-related anxiety.
The Driving Behavior Survey (DBS; Clapp, Olsen, Beck, et al., 2011) is a self-report instrument developed to assess the frequency of anxiety-related driving behavior. For this measure, anxious driving behavior was operationalized as an increase, decrease, or general disorganization of behavior occurring as a consequence of anxiety during operation of a motor vehicle. Scale construction followed an internal consistency approach (Clark & Watson, 1995) with the final measure developed iteratively across multiple samples of student motorists. Three unique domains of problematic behavior were identified based on factor analytic procedures. The first contained a collection of exaggerated safety and/or excessively cautious behaviors similar to those noted in the clinical literature (e.g., Mayou, Simken, & Threlfall, 1991; Taylor & Koch, 1995). Behaviors in this domain (e.g., maintaining excessive distances from other motorists, driving far below the posted speed limit, reducing speed before progressing through intersections) are conceptualized as efforts to enhance perceptions of safety and control. Unfortunately, efforts to reduce acute traffic distress are believed to facilitate the long-term maintenance of anxiety (Clark, 1999; Salkovskis, 1991) and may inadvertently increase accident risk to the extent that excessively cautious behaviors violate accepted traffic norms.
The second domain involves a series of anxiety-based performance deficits similar to those noted in the traffic and transportation safety literatures (e.g., Dula et al., 2010; Kontogiannis, 2006; Matthews et al., 1998). Behaviors in this domain (e.g., difficulty staying in the correct lane, sudden or inappropriate adjustments in speed, inability to perform basic traffic operations) are thought to occur primarily as a function of anxiety-based cognitive interference. Whereas low to moderate levels of anxiety often serve to facilitate performance, excessive anxiety is believed to compete with working memory resources necessary for processing task-relevant information (e.g., monitoring speed, direction, and vehicle position; Taylor et al., 2008).
The final domain of problematic behavior involves anxiety-based hostility and driving aggression. Although hostile/aggressive driving behavior (e.g., shouting, honking, aggressive gesturing) is less commonly examined as a consequence of driving-specific fear, trait-level anxiety consistently demonstrates associations with both driving anger and aggressive violations (Deffenbacher, Huff, Lynch, Oetting, & Salvatore, 2000; Lucidi et al., 2010; Shahar, 2009; Ulleberg, 2002). In this research, trait anxiety is believed to decrease the threshold for aggressive response to traffic-related stress, increasing risk for collisions, violations, and dangerous driving behavior (Deffenbacher et al., 2000; Deffenbacher, Lynch, Filetti, Dahlen, & Oetting, 2003). Research specifically targeting behavioral response to driving anxiety suggests that state-level fear may confer similar risk for driving-related hostility and aggression (Clapp, Olsen, Beck, et al., 2011; Clapp, Olsen, Danoff-Burg, et al., 2011).
Scale development efforts using general samples of student drivers (i.e., not selected for any specific characteristics) provide initial evidence of the factorial validity, internal consistency, temporal stability, and convergent associations of DBS scores (Clapp, Olsen, Beck, et al., 2011). Follow-up research with student drivers endorsing traffic collision involvement offers additional support for the internal consistency and construct validity of responses (Clapp, Olsen, Danoff-Burg, et al., 2011). Although the DBS exhibits potential as an intervention tool, no study to date has examined the measurement properties of the scale within a clinical sample. This is notable given that best-practice standards for psychological testing require formal evaluation of a measure prior to use in populations for which validation data are unavailable (APA, 1999; Standard 1.4).
The aim of the current study was to evaluate the reliability and performance of DBS scores in a help-seeking sample of community drivers with MVA-related posttraumatic stress disorder (PTSD). PTSD historically has been defined as an anxiety disorder developing in response to a traumatic event involving actual or threatened death, serious injury, and/or threat to the physical integrity of oneself or others (APA, 1980; 2000). Characteristic symptoms include reexperiencing the event (e.g., intrusive thoughts, distressing dreams), avoidance of thoughts and/or situations associated with the trauma, numbing of emotional response (e.g., detachment, flattened affect), and heightened arousal (e.g., irritability, hypervigilance). Although driving anxiety is diagnostically complex and pervasive in both clinical and non-clinical populations (Ehlers, Hofmann, Herda, & Roth, 1994; Taylor & Deane, 2000; Taylor, Deane, & Podd, 2007b; Taylor et al., 2002), individuals who develop PTSD following serious motor vehicle trauma have been shown to be at increased risk of elevated driving fear. Research indicates the overwhelming majority of individuals presenting for treatment acknowledge enduring driving-related tasks with elevated or extreme distress, with some estimates exceeding 90% of cases (e.g. Blanchard & Hickling, 2004; Kuch, Swinson, Kirby, 1985). Functional impairment as a consequence of driving-related anxiety is severe and has been identified as one of the most frequent motivations for help-seeking in this population (e.g., Blanchard & Hickling, 2004; Kuch, Cox, & Direnfeld, 1995). The extant data also provide evidence for observable changes in driving behavior following significant motor vehicle trauma (e.g., Interministerial Task Force, 1981; Mayou et al., 1991). Whereas increased caution and defensiveness are expected, dangerous or otherwise problematic behaviors as a result of driving-related anxiety have been identified as characteristic of individuals seeking treatment for MVA-related PTSD (Beck & Coffey, 2005; Koch & Taylor, 1995; Taylor & Koch, 1995).
A series of analyses were used to evaluate the psychometric properties of DBS scores in the current treatment-seeking sample. The stability of DBS scales was determined through estimates of internal consistency and 12-week test-retest reliability. Construct validity was evaluated through mean-comparisons with normative data obtained from unselected student (Clapp, Olsen, Beck, et al., 2011) and student collision (Clapp, Olsen, Danoff-Burg, et al., 2011) samples. Dose-response relations between severity of driving-related anxiety and domains of anxious driving behavior were expected, with DBS scores among treatment-seeking individuals hypothesized to exceed those observed in non-clinical samples. Finally, a series of exploratory analyses examined associations with a set of standard clinical measures. Of specific interest were relations with indices of PTSD severity, depressive symptomatology, and overt travel avoidance.
1. Method
1.1. Participants
1.1.1. Treatment-Seeking Sample
Clinical data were collected as part of a larger study examining the efficacy of a brief written exposure intervention for individuals with MVA-related PTSD (see Sloan, Marx, Bovin, Feinstein, & Gallagher, 2012 for details). All participants were recruited from the greater Boston, MA area through public service announcements and community postings (e.g., flyers placed near public transportation stops, public libraries, grocery stores). Inclusion criteria required participants to be at least 18 years of age and present with a primary diagnosis of MVA-related PTSD. The criterion MVA was required to have occurred at least 3-months prior to enrollment in the study. Exclusion criteria included evidence of psychosis, organic mental disorder, active substance dependence, unstable bipolar disorder, English illiteracy, and/or high risk for suicidal behavior (e.g., suicide attempt in past two months).
Researchers were contacted by a total of 145 individuals. Of these, 68 did not qualify based on responses to an initial phone screen. Ten of the 77 individuals qualifying for inclusion based on the initial screen did not present for the initial assessment. Of the 67 individuals who were formally evaluated, 18 did not meet inclusion criteria and 3 declined to continue with the study. Forty-six participants were randomized either to the written exposure intervention or a wait-list control condition. Of these individuals, six were unable to complete the DBS as they did not identify as current drivers. As such, the final sample for this research included 40 individuals with a primary diagnosis of MVA-related PTSD.
The majority of study participants were female (62.5%). Age ranged from 22 to 65 (M = 40.8). Participants were ethnically diverse with similar proportions of the sample identifying as Caucasian (35.0%) and African-American (37.5%). Education level also was diverse, ranging from professional degrees to secondary school or less. Sixty percent of participants reported some level of employment (full or part-time). Average duration from the criterion MVA was 35.5 months. Demographic characteristics of the treatment-seeking sample are presented in Table 1.
Table 1.
Sample characteristics (N = 40)
| Age (M, SD) | M = 40.8 | SD = 13.3 |
| Sex (female) | 25 | 62.5% |
| Race/ethnicity | ||
| Caucasian | 14 | 35.0% |
| African American | 15 | 37.5% |
| Hispanic | 4 | 10% |
| Asian | 1 | 2.5% |
| Other | 6 | 15.0% |
| Education | ||
| ≤ High School | 8 | 20% |
| Some college | 15 | 37.5% |
| B.A. | 8 | 20% |
| Graduate coursework | 9 | 22.5% |
| Employment | ||
| Full-time | 14 | 35.0% |
| Part-time | 10 | 25.0% |
| Unemployed | 7 | 17.5% |
| Retired/Disability | 5 | 12.5% |
| Student | 3 | 7.5% |
| Service | 1 | 2.5% |
| Months since accident (M, SD) | M = 35.5 | SD = 48.3 |
| Total psychiatric diagnoses (M, SD) a | M = 2.0 | SD = 1.4 |
Total psychiatric diagnoses includes primary diagnosis of MVA-related PTSD
1.1.2. Normative Student Samples
The unselected student sample (N = 515) was composed of college-aged motorists participating in the initial development research for the DBS (see Clapp, Olsen, Beck, et al., 2011; Samples 2 & 3). Nearly half of participants were female (45.6%) with a mean age of 19.1 (SD = 1.7). Students were predominantly Caucasian (79.2%) with 7.0% identifying as African American, 8.0% as Asian, and 1.9% as Hispanic. Less than half of the sample (42.7%) reported prior accident involvement. The student collision sample (N = 317) was composed of college-aged motorists reporting involvement in at least one traffic collision (see Clapp, Olsen, Danoff-Burg, et al., 2011). Inclusion criteria did not require the respondent to be the driver in the reported collision, and no a-priori assumptions were made regarding actual accident severity. Again, nearly half of participants were female (47.6%) with a mean age of 19.5 (SD = 1.8). Students were predominantly Caucasian (70.3%) with 12.9% identifying as African American, 7.3% as Asian, and 6.3% as Hispanic. Mean duration since the most severe collision in this sample was 22.7 (SD = 19.6) months.
1.2. Procedure
Informed consent was obtained from community members in the larger treatment outcome study upon their arrival for initial assessment. Participants then completed a series of self-report measures and semi-structured clinical interviews. Interviews were conducted by doctoral-level psychologists. All assessments were recorded with 15% selected at random for independent review. Of the 40 individuals in the present sample, 19 were randomized to receive a five-week written exposure therapy (WET; see Sloan et al., 2012 for full details). The remaining 21 individuals were randomized to a minimal contact, wait-list control condition. Participants were re-assessed six weeks following the initial interview (post-treatment for WET participants) and again at 18-weeks (3 month follow-up for WET participants). Wait-list participants were offered treatment following completion of the 18-week assessment. All procedures were approved by local Institutional Review Boards.
1.3. Measures
Assessment instruments relevant to the present study are detailed below. All measures were administered at each assessment point.
1.3.1. Driving Behavior Survey (DBS)
Anxious driving behavior was evaluated using the DBS (Clapp, Olsen, Beck, et al., 2011). As described, the DBS is a 21-item scale indexing the frequency of anxious driving behavior across three domains: exaggerated safety/caution behavior, anxiety-based performance deficits, and hostile/aggressive behavior. Items are rated on a 1 (never) to 7 (always) Likert-type scale with scores calculated as the mean of endorsed scale items. Higher scores indicate greater frequency of anxious behavior. Evidence of factorial validity and convergent associations are provided by Clapp, Olsen, Beck, et al. (2011). Estimates of internal consistency among college-aged motorists range from good to excellent for safety/caution (α = .78 to .90), performance deficit (α = .75 to .85), and hostile/aggressive scales (α = .86 to .91; Clapp, Olsen, Beck, et al., 2011; Clapp, Olsen, Danoff-Burg, et al., 2011). Four-week test-retest reliabilities in the development sample were .68, .61, and .89 for safety/caution, performance deficit, and hostile/aggressive scales, respectively.
1.3.2. Clinician-Administered PTSD Scale (CAPS)
The CAPS (Weathers, Keane, & Davidson, 2001) was used to establish PSTD diagnosis in the larger treatment study and to provide a continuous index of PTSD symptom severity. Individual CAPS items correspond to the 17 cardinal symptoms of PTSD as specified in DSM-IV (APA, 2000). Frequency and intensity ratings for each symptom are scored on a 0–4 Likert-type scale with CAPS total scores computed as the sum of all ratings (range: 0 to 136). Continuous scores for symptoms of reexperiencing (B1–B5), avoidance (C1–C2), numbing (C3–C7), and hyperarousal (D1–D5) are given as the sum of frequency and intensity ratings within each cluster. For the current study, symptoms with frequency ≥ 1 and intensity ≥ 2 were counted towards diagnosis (Blanchard et al., 1996). Individuals meeting all DSM-IV (APA, 2000) symptom criteria and having a CAPS total score ≥ 40 received a formal diagnosis of PTSD (Weathers et al., 2001). Previous psychometric research estimates mean CAPS scores for help-seeking MVA survivors with (n = 99) and without (n = 130) PTSD at 70.1 (SD = 17.6) and 24.7 (SD = 18.7) points, respectively (Coffey, Gudmundsdottir, Beck, Palyo, & Miller, 2006). CAPS scores demonstrate strong psychometric properties with one-week test-retest reliability ranging between .90 and .96 (Weathers et al., 2001). Inter-rater reliabilities for PTSD diagnosis in this sample was excellent (κ = .94).
1.3.3. Beck Depression Inventory-II (BDI-II)
Associations between domains of anxious driving behavior and the BDI-II (Beck, Steer, & Brown, 1996) were examined given the widespread use of the measure in both clinical research and applied settings. BDI-II items are summed to form a continuous index of depressive severity with total scores ranging from 0 to 63. Scores ranging from 0–13, 14–19, 20–28, and 29–63 are indicative of minimal, mild, moderate, and severe depressive symptoms, respectively (Beck, Steer, & Brown, 1996). Extensive research with the BDI-II provides strong evidence for the reliability and construct validity of scores (Beck et al., 1996; Quilty, Zhang, & Bagby, 2010). Internal consistency of baseline BDI-II scores in the current sample was high (α = .90).
1.3.4. Driving and Riding Avoidance Scale (DRAS)
The DRAS (Stewart & St. Peter, 2004) was administered as an index of overt travel avoidance. For this measure, avoidance of 20 driving scenarios are rated on a 0 (rarely) to 3 (most of the time) Likert-type scale. Items are summed to provide a total score (range 0–60), with higher scores indicating greater travel avoidance. The mean DRAS score in a development sample of university students reporting traffic collision involvement (N = 386) was 7.64 (SD = 8.88; Stewart & St. Peter, 2004). Scores from this measure evidence high test-retest reliability and internal consistency (Steward & St. Peter, 2004). Internal consistency of baseline scores in the current sample was excellent (α = .96).
1.4. Analytic Plan
The stability of DBS scores was evaluated through estimates of internal consistency and test-retest reliability. Internal consistency estimates were calculated from baseline scores collected during the initial assessment. Test-retest reliabilities were based on comparison of scores collected at the 6- and 18-week assessments. Scores from the post-treatment assessment periods were evaluated to distinguish stability estimates from the primary effects of intervention (see Sloan et al., 2012).
Dose-response relations as a function of MVA-related anxiety were examined through comparison with published student norms (Clapp, Olsen, Beck, et al., 2011; Clapp, Olsen, Danoff-Burg, et al., 2011). Effect sizes and corresponding 95% confidence intervals are reported as Cohen’s d (i.e., small = .20, medium = .50, large = .80; Cohen, 1988).
Pearson correlations were used to examine associations with PTSD severity, depressive symptoms, and travel avoidance. Effect sizes and corresponding 95% confidence intervals for these analyses are reported as r coefficients (i.e., small = .10, medium = .30, large = .50; Cohen, 1988).
2. Results
2.1. Reliability
Internal consistency in this sample was excellent. Cronbach's alpha for exaggerated safety/caution, anxiety-based performance deficits, and aggressive/hostile scales at baseline were 0.93, 0.93, and 0.85, respectively. Twelve-week test-retest reliabilities (6-week to 18-week post-randomization) were examined for the period during which participants did not receive psychosocial intervention. Twelve-week estimates for safety/caution, anxiety-based performance deficits, and aggressive/hostile behavior scales were 0.80, 0.85, and 0.80, respectively.
2.2. Dose-Response Relations
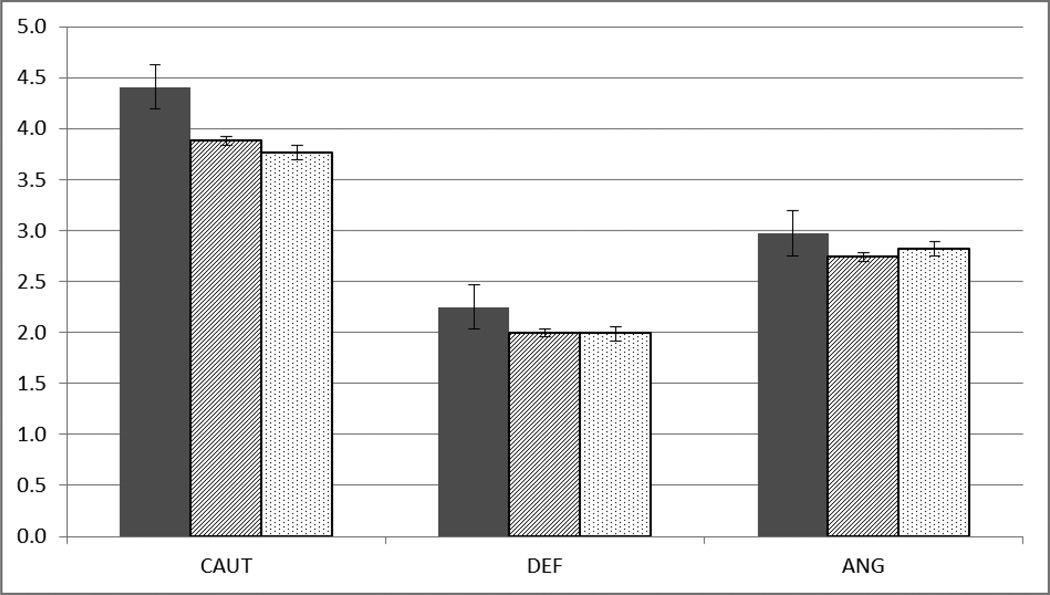
Comparisons with normative data for unselected student and student collision samples are illustrated in Figure 1. Relative to unselected student drivers, individuals with MVA-related PTSD evidenced greater levels of exaggerated safety/caution behavior (p < .001; d = .44, CI95 [.23, .88]) and anxiety-based performance deficits (p = .047; d = .24, CI95 [.01, .65]). No significant differences were noted with regard to the frequency of hostile/aggressive driving behavior (p = .223; d = .19, CI95 [−1.22, .52]). Relative to student drivers reporting involvement in unspecified traffic collisions, individuals with MVA-related PTSD evidenced greater levels of exaggerated safety/caution (p = .004; d = .46, CI95 [.02, .81]). Differences in anxiety-based performance deficits (p = .102; d = .19, CI95 [−.05, .61]) and hostile/aggressive behavior (p = .510; d = .11, CI95 [−.22, .44]) did not reach threshold for statistical significance.
Figure 1.
Driving Behavior Survey scores for clinical and non-clinical samples a
 Treatment-seeking PTSD (N = 40): CAUT (M = 4.41, SD = 1.54); DEF (M = 2.25, SD = 1.35); ANG (M = 2.97, SD = 1.31).
Treatment-seeking PTSD (N = 40): CAUT (M = 4.41, SD = 1.54); DEF (M = 2.25, SD = 1.35); ANG (M = 2.97, SD = 1.31).
 Unselected student sample from Clapp, Olsen, Beck, et al. (2011; N = 518): CAUT (M = 3.88, SD = 0.89); DEF (M = 2.00, SD = 0.70); ANG (M = 2.74, SD = 1.14).
Unselected student sample from Clapp, Olsen, Beck, et al. (2011; N = 518): CAUT (M = 3.88, SD = 0.89); DEF (M = 2.00, SD = 0.70); ANG (M = 2.74, SD = 1.14).
 Student collision sample from Clapp, Olsen, Danoff-Burg, et al. (2011; N = 317): CAUT (M = 3.76, SD = 1.32); DEF (M = 1.99, SD = 0.88); ANG (M = 2.82, SD = 1.36).
Student collision sample from Clapp, Olsen, Danoff-Burg, et al. (2011; N = 317): CAUT (M = 3.76, SD = 1.32); DEF (M = 1.99, SD = 0.88); ANG (M = 2.82, SD = 1.36).
a CAUT = excessive safety/caution behaviors; DEF = anxiety-based performance deficits; ANG = hostile/aggressive driving behavior; Error bars indicate standard errors for each sample.
2.3. Exploratory Associations
Associations with PTSD severity, depressive symptoms, and overt travel avoidance are provided in Table 2. CAPS total scores evidenced a medium relation with hostile/aggressive driving behavior (r = .30, CI95 [−.01, .56]; p = .057) and minimal associations with other DBS scales. Analysis of individual symptom clusters indicated a medium effect for the relation between hyperarousal and hostile/aggressive behavior (r = .36, CI95 [.05, .60]; p = .024) with other associations failing to reach criteria for statistical significance. Hostile/aggressive driving behavior also evidenced a marginal association with overt travel avoidance (r = .30, CI95 [−.01, .56]; p = .062) while the severity of depressive symptoms was related only to the frequency of anxiety-based performance deficits (r = .37, CI95 [.06, .61]; p = .020).
Table 2.
Correlations and descriptive statistics for clinical measures
| CAUT | DEF | ANG | M | SD | |
|---|---|---|---|---|---|
| CAPS | −.109 | .073 | .304† | 65.15 | 17.49 |
| - Reexperiencing | −.149 | −.230 | .228 | 16.43 | 5.30 |
| - Avoidance | .127 | .133 | .163 | 9.58 | 2.54 |
| - Numbing | −.162 | .137 | .154 | 17.28 | 8.33 |
| - Hyperarousal | −.013 | .151 | .357* | 21.88 | 6.76 |
| BDI-II | .184 | .366* | .283 | 16.23 | 9.13 |
| DRAS | .220 | .206 | .298† | 30.58 | 16.82 |
Note: CAUT=Driving Behavior Survey (DBS) exaggerated safety/caution; DEF=DBS performance deficits; ANG=DBS hostile/aggressive behavior; CAPS=Clinician-Administered PTSD Scale total scores; Reexperiencing=CAPS B1–B5; Avoidance=CAPS C1–C2; Numbing=CAPS C3–C7; Hyperarousal=CAPS D1–D5; DRAS=Driving and Riding Avoidance Scale; BDI-II = Beck Depression Inventory-II;
p ≤ .06
p ≤ .05
3. Discussion
The aim of the present study was to evaluate the measurement properties of DBS scales among individuals with MVA-related PTSD. Results offer preliminary evidence for the reliability and validity of scores within this population. Internal consistency of DBS performance deficit, safety/caution, and hostile/aggressive scales ranged from good to excellent, as did estimates of 12-week test-retest reliability. Performance deficit and safety caution scales demonstrated greater internal consistency and test-retest reliability relative to previous estimates obtained from student motorists (Clapp, Olsen, Beck, et al., 2011; Clapp, Olsen, Danoff-Burg, et al., 2011). Interestingly, reliability estimates for hostile/aggressive driving behavior were at or below those observed in student samples. It should be noted, however, that existing research indicates a robust negative relationship between age and anger (Garrity & Demick, 2001). Given the proposed relation of trait-level anger to anxiety-based hostility and aggression (Clapp, Olsen, Beck, et al., 2011; Clapp, Olsen, Danoff-Burg, et al., 2011), it is possible that greater levels of baseline anger among student motorists could account for the comparatively lower – but acceptable – estimates of stability in this older community sample. Continued research is needed to more fully determine the influence of age on anxiety-based driving aggression.
These data also indicate plausible dose-response relations between pathological travel anxiety and domains of problematic driving behavior. The frequency of exaggerated safety behavior in this clinical sample was significantly greater than that observed in unselected students drivers and student drivers reporting involvement in unspecified traffic collisions. Population estimates for comparisons with non-clinical samples approached conventional standards for large effects. Evidence for increased frequency of safety/caution behavior is particularly relevant given the prominence of these behaviors in the clinical and treatment literature (Antony et al., 2006; Koch & Taylor, 1995; Taylor & Koch, 1995; Taylor et al., 2002). Hypotheses regarding dose-response relationships for anxiety-based performance deficits were partially supported. Elevated frequency of performance deficits was noted relative to unselected student motorists, but increased occurrence in the clinical sample failed to reach significance relative to students reporting involvement in traffic collisions
Increased frequency of hostile/aggressive driving behavior relative to student samples was modest and failed to reach criteria for significance. The absence of effects for this scale is surprising, particularly given that anger and irritability are included as formal symptoms of PTSD (APA, 2000). However, considering evidence for the prevalence of reckless and aggressive behavior among youthful drivers (Arnett, Offer, & Fine, 1997; Machin & Sankey, 2008; Ulleberg, 2002), it is interesting to note the occurrence of aggressive behavior in this older PTSD sample appears commensurate with that characteristic of emerging adulthood.
It also is possible that modest differences in hostile/aggressive behaviors is attributable, in part, to the nature of index trauma.1 Interpersonal trauma is associated with increased prevalence of PTSD and poorer affect regulation relative to non-interpersonal events such as MVA (e.g., Ehring & Quack, 2010; Kessler, Sonnega, Bromet, Hughes, & Nelson 1995). PTSD as a consequence of combat-related trauma demonstrates particularly robust associations with anger difficulties and overt aggression (Beckham, Moore, & Reynolds, 2000; Orth & Wieland, 2006). Although anger symptoms continue to be influential in the maintenance of PTSD subsequent to MVA (e.g., Mayou, Ehlers, & Bryant, 2002), examination of anxiety-based driving aggression within veterans samples may be warranted, particularly given known difficulties with traffic-related cues in this population (e.g., Kuhn, Drescher, Ruzek, & Rosen, 2010; Sayer et al., 2010; Strom et al., 2012).
Exploratory associations with clinical scales further support the validity of DBS scores in this help-seeking population. Results indicated a moderate correlation between severity of PTSD and anxiety-based hostile/aggressive behavior. Follow-up analysis with individual symptom clusters suggests this relation may reflect the common role of anger in both driving aggression and PTSD. These effects also are consistent with prior research indicating a relation between hostile/aggressive driving behavior and life stress exposure (Clapp, Olsen, Danoff-Burg, et al., 2011). Depressive symptoms, by contrast, evidenced a moderate association with anxiety-based performance deficits. Rumination and/or attentional biases may account for shared variance in these measures; additional research is needed to determine the specific influence of cognitive processes in the relation between depression and anxiety-related deficits in performance. Finally, severity of overt travel avoidance evidenced small to medium correlations across all DBS scales. These effects are consistent with those observed among unselected student motorists and support the relative independence of anxious driving behavior as a construct distinct from explicit travel avoidance (Clapp, Olsen, Beck, et al., 2011).
Together, these data provide evidence for the reliability and validity of DBS scores in a clinically relevant, but unexamined, population. However, a number of methodological and conceptual issues should be considered in the interpretation of these data. First, the sample available for these analyses was small, contributing to a number of effects that failed to reach formal criteria for statistical significance. Indices of effect size indicate a number of moderately sized relations, but further research is needed to strengthen conclusions regarding the stability of these associations. Second, effects observed within this diagnostically homogenous sample may not generalize to other relevant populations (e.g., driving phobia, panic disorder, social phobia). Although the presence of differential effects across disorders is plausible, the available research indicates notable similarities in the presentation of driving-related fear across specific disorders (e.g., Ehlers et al., 1994; Taylor et al., 2002, 2007b). Modest correlations with indices of PTSD further support the relative independence of DBS scales from formal symptoms of psychopathology. Continued investigation within increasingly diverse samples will be helpful in isolating the common and unique characteristics of anxious driving behaviors across individual disorders. Finally, it is unclear whether results were influenced by the experimental setting under which these data were collected. Future assessment independent of randomized controlled trials may strengthen conclusions regarding the measurement properties of this instrument.
4. Conclusion
Convergent evidence from multiple literatures indicates a number of problematic behaviors among individuals who continue to drive despite significant traffic-related anxiety. Maladaptive driving behaviors may inadvertently serve to maintain anxious responding as well as place the individual at increased risk for negative traffic events. Results of the current study suggest that anxious driving behaviors among individuals with MVA-related PTSD may be assessed reliably and efficiently via DBS scores. Continued investigation is needed, but these data offer preliminary evidence for the utility of anxious driving behavior as an alternative marker of functional impairment among individuals with clinical levels of driving-related anxiety.
Highlights.
Anxiety during operation of a motor vehicle may impact driving performance
Excessive safety, performance deficits, and aggressive driving domains were assessed
Persons with posttraumatic stress disorder evidence reliable scores in each domain
Anxious travel behavior seems more severe in clinical relative to normative samples
Anxious driving behavior shows promise as an index of functional impairment
Acknowledgments
This study was supported in part by National Institute of Mental Health grants (T32MH019836 awarded to Terence M. Keane for which Aaron Baker was supported; R34MH077658-02 awarded to Denise M. Sloan) and by the Lillian and Morrie Moss Chair of Excellence, University of Memphis (J. Gayle Beck).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
We would like to thank an anonymous reviewer for this observation.
Contributor Information
Joshua D. Clapp, Email: jclapp@uwyo.edu.
Aaron S. Baker, Email: Aaron.Baker2@va.gov.
Scott D. Litwack, Email: Scott.Litwack@va.gov.
Denise M. Sloan, Email: Denise.Sloan@va.gov.
J. Gayle Beck, Email: jgbeck@memphis.edu.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed. Washington, DC: Author; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 2000. text revision. [Google Scholar]
- American Psychiatric Association. Standards for educational and psychological testing. Washington DC: American Educational Research Association; 1999. [Google Scholar]
- Antony MM, Craske MG, Barlow DH. Mastery of your specific phobia: Client workbook. 2nd ed. New York: Oxford University Press; 2006. [Google Scholar]
- Arnett JJ, Offer D, Fine MA. Reckless driving in adolescence: “State” and “Trait” factors. Accident Analysis & Prevention. 1997;29:57–63. doi: 10.1016/s0001-4575(97)87007-8. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown G. Manual for the Beck Depression Inventory II. (BDI-II) San Antonio, TX: Psychological Cooperation; 1996. [Google Scholar]
- Beck J, Coffey SF. Group cognitive behavioral treatment for PTSD: Treatment of motor vehicle accident survivors. Cognitive and Behavioral Practice. 2005;12:267–277. doi: 10.1016/s1077-7229(05)80049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckham JC, Moore SD, Reynolds V. Interpersonal hostility and violence in Vietnam combat veterans with chronic posttraumatic stress disorder: A review of theoretical models and empirical evidence. Aggression and Violent Behavior. 2000;5:451–466. [Google Scholar]
- Blanchard EB, Hickling EJ. After the crash: Psychological assessment and treatment of survivors of motor vehicle accidents. 2nd ed. Washington, DC US: American Psychological Association; 2004. What are the psychosocial effects of MVAs on survivors? pp. 57–97. [Google Scholar]
- Blanchard EB, Hickling EJ, Barton KA, Taylor AE, Loos WR, Jones-Alexander J. One-year prospective follow-up of motor vehicle accident victims. Behaviour Research and Therapy. 1996;34:775–786. doi: 10.1016/0005-7967(96)00038-1. [DOI] [PubMed] [Google Scholar]
- Clapp JD, Olsen SA, Beck JG, Palyo SA, Grant DM, Gudmundsdottir B, Marques L. The Driving Behavior Survey: Scale construction and validation. Journal of Anxiety Disorders. 2011;25:96–105. doi: 10.1016/j.janxdis.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clapp JD, Olsen SA, Danoff-Burg S, Hagewood JH, Hickling EJ, Hwang VS, Beck JG. Factors contributing to anxious driving behavior: The role of stress history and accident severity. Anxiety Disorders. 2011;25:592–598. doi: 10.1016/j.janxdis.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DM. Anxiety disorders: Why they persist and how to treat them. Behaviour Research and Therapy. 1999;37:S5–S27. doi: 10.1016/s0005-7967(99)00048-0. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Constructing validity: Basic issues in objective scale development. Psychological Assessment. 1995;7:309–319. doi: 10.1037/pas0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SR, Gudmundsdottir B, Beck J, Palyo SA, Miller L. Screening for PTSD in Motor Vehicle Accident Survivors Using the PSS-SR and IES. Journal of Traumatic Stress. 2006;19:119–128. doi: 10.1002/jts.20106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- Deffenbacher JL, Huff ME, Lynch RS, Oetting ER, Salvatore NF. Characteristics and treatment of high-anger drivers. Journal of Counseling Psychology. 2000;47:5–17. [Google Scholar]
- Deffenbacher JL, Lynch RS, Filetti LB, Dahlen ER, Oetting ER. Anger, aggression, risky behavior, and crash-related outcomes in three groups of drivers. Behaviour Research and Therapy. 2003;41:333–349. doi: 10.1016/s0005-7967(02)00014-1. [DOI] [PubMed] [Google Scholar]
- Dula CS, Adams CL, Miesner MT, Leonard RL. Examining relationships between anxiety and dangerous driving. Accident Analysis and Prevention. 2010;42:2050–2056. doi: 10.1016/j.aap.2010.06.016. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Hofmann SG, Herda CA, Roth WT. Clinical characteristics of driving phobia. Journal of Anxiety Disorders. 1994;8:323–339. [Google Scholar]
- Ehring T, Quack D. Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy. 2010;41:587–598. doi: 10.1016/j.beth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Fairclough SH, Tattersall AJ, Houston K. Anxiety and performance in the British driving test. Transportation Research Part F. 2006;9:53–52. [Google Scholar]
- Garnefski N, Kraaij V. Cognitive emotion regulation questionnaire – development of a short 18-item version (CERQ-short) Personality and Individual Differences. 2006;41:1045–1053. [Google Scholar]
- Garnefski N, Kraaij V, Spinhoven P. Negative life events, cognitive emotion regulation, and emotional problems. Personality and Individual Differences. 2001;30:1311–1327. [Google Scholar]
- Garrity RD, Demick J. Relations among personality traits, mood states, and driving behaviors. Journal of Adult Development. 2001;8:109–118. [Google Scholar]
- Interministerial Task Force on Motor Vehicle Injuries. Injury: An Ontario survey of the societal and personal costs of hospitalized motor vehicle accident victims (Technical Report) Ontario: Ontario Ministry of Transport and Communications; 1981. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Koch WJ, Taylor S. Assessment and treatment of motor vehicle accident victims. Cognitive and Behavioral Practice. 1995;2:327–342. [Google Scholar]
- Kontogiannis T. Patterns of driver stress and coping strategies in a Greek sample and their relationship to aberrant behaviors and traffic accidents. Accident Analysis and Prevention. 2006;38:913–924. doi: 10.1016/j.aap.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Kuch K, Cox BJ, Direnfeld DM. A brief self-rating scale for PTSD after road vehicle accident. Journal of Anxiety Disorders. 1995;9:503–514. [Google Scholar]
- Kuch K, Swinson RP, Kirby M. Post-traumatic stress disorder after car accidents. The Canadian Journal of Psychiatry. 1985;30:426–427. doi: 10.1177/070674378503000610. [DOI] [PubMed] [Google Scholar]
- Kuhn E, Drescher K, Ruzek J, Rosen C. Aggressive and unsafe driving in male veterans receiving residential treatment for PTSD. Journal of Traumatic Stress. 2010;23:399–402. doi: 10.1002/jts.20536. [DOI] [PubMed] [Google Scholar]
- Lucidi F, Giannini AM, Sgalla R, Mallia L, Devoto A, Reichmann S. Young novice driver subtypes: Relationship to driving violations, errors, and lapses. Accident Analysis and Prevention. 2010;42:1689–1696. doi: 10.1016/j.aap.2010.04.008. [DOI] [PubMed] [Google Scholar]
- Machin MA, Sankey KS. Relationships between young drivers’ personality characteristics, risk perceptions, and driving behavior. Accident Analysis and Prevention. 2008;40:541–547. doi: 10.1016/j.aap.2007.08.010. [DOI] [PubMed] [Google Scholar]
- Matthews G, Dorn L, Hoyes TW, Davies DR, Glendon AI, Taylor RG. Driver stress and performance on a driving simulator. Human Factors. 1998;40:136–149. doi: 10.1518/001872098779480569. [DOI] [PubMed] [Google Scholar]
- Mayou RA, Ehlers AA, Bryant BB. Posttraumatic stress disorder after motor vehicle accidents: 3-year follow-up of a prospective longitudinal study. Behaviour Research and Therapy. 2002;40:665–675. doi: 10.1016/s0005-7967(01)00069-9. [DOI] [PubMed] [Google Scholar]
- Mayou R, Simken S, Threlfall J. The effects of road traffic accidents on driving behaviour. Injury. 1991;22:365–368. doi: 10.1016/0020-1383(91)90095-v. [DOI] [PubMed] [Google Scholar]
- Orth U, Wieland E. Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: A meta-analysis. Journal of Consulting and Clinical Psychology. 2006;74:698–706. doi: 10.1037/0022-006X.74.4.698. [DOI] [PubMed] [Google Scholar]
- Quilty LC, Zhang KA, Bagby RM. The latent structure of the Beck Depression Inventory-II in outpatients with major depression. Psychological Assessment. 2010;22:603–608. doi: 10.1037/a0019698. [DOI] [PubMed] [Google Scholar]
- Salkovskis PM. The importance of behaviour in the maintenance of anxiety and panic: A cognitive account. Behavioural Psychotherapy. 1991;19:6–19. [Google Scholar]
- Sayer NA, Noorbaloochi S, Frazier P, Carlson K, Gravely A, Murdoch M. Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatric Services. 2010;61:589–597. doi: 10.1176/ps.2010.61.6.589. [DOI] [PubMed] [Google Scholar]
- Shahar A. Self-reported driving behaviors as a function of trait anxiety. Accident Analysis and Prevention. 2009;41:241–245. doi: 10.1016/j.aap.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Shoham SG, Geva N, Markovski R, Kaplinsky N. Internalization of norms, risk-perception, and anxiety as related to driving offences. British Journal of Criminology. 1976;16:142–155. [Google Scholar]
- Shoham SG, Rahav G, Markovski R, Chard F, Baruch I. “Anxious” and “Reckless” drivers. Deviant Behavior. 1984;5:181–191. [Google Scholar]
- Sloan DM, Marx BP, Bovin MJ, Feinstein BA, Gallagher MW. Written exposure as an intervention for PTSD: A randomized clinical trial with motor vehicle accident survivors. Behaviour Research and Therapy. 2012;50:627–635. doi: 10.1016/j.brat.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart AE, St. Peter CC. Driving and riding avoidance following motor vehicle crashes in a non-clinical sample: Psychometric properties of a new measure. Behaviour Research and Therapy. 2004;42:859–879. doi: 10.1016/S0005-7967(03)00203-1. [DOI] [PubMed] [Google Scholar]
- Strom TQ, Leskela J, James LM, Thuras PD, Voller E, Weigel R, Holz K. An exploratory examination of risk-taking behavior and PTSD symptom severity in a veteran sample. Military Medicine. 2012;177:390–396. doi: 10.7205/milmed-d-11-00133. [DOI] [PubMed] [Google Scholar]
- Taylor J, Deane FP. Comparison and characteristics of motor vehicle accident (MVA) and non-MVA driving fears. Journal of Anxiety Disorders. 2000;14:453–470. doi: 10.1016/s0887-6185(99)00040-7. [DOI] [PubMed] [Google Scholar]
- Taylor J, Deane FP, Podd J. Driving-related fear: A review. Clinical Psychology Review. 2002;22:631–645. doi: 10.1016/s0272-7358(01)00114-3. [DOI] [PubMed] [Google Scholar]
- Taylor J, Deane FP, Podd J. Driving fear and driving skills: Comparison between fearful and control samples using standardised on-road assessment. Behaviour Research and Therapy. 2007a;45:805–818. doi: 10.1016/j.brat.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Taylor J, Deane FP, Podd J. Diagnostic features, symptom severity, and help-seeking in a media-recruited sample of women with driving fear. Journal of Psychopathology and Behavioral Assessment. 2007b;29:81–91. [Google Scholar]
- Taylor J, Deane FP, Podd J. The relationship between driving anxiety and driving skill: A review of human factors and anxiety-performance theories to clarify future research needs. New Zealand Journal of Psychology. 2008;37:28–37. [Google Scholar]
- Taylor S, Koch WJ. Anxiety disorders due to motor vehicle accidents: Nature and treatment. Clinical Psychology Review. 1995;15:721–738. [Google Scholar]
- Ulleberg P. Personality subtypes of young drivers: Relationship to risk taking preferences, accident involvement, and response to a traffic safety campaign. Transportation Research Part F: Traffic Psychology and Behavior. 2002;4:279–297. [Google Scholar]
- Weathers FW, Keane TR, Davidson JRT. Clinician Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]