Abstract
Clinical reports have highlighted a role for retinoids in the etiology of mood disorders. Although we had shown that recruitment of the nuclear receptor retinoic acid receptor-α (RAR-α) to corticotropin-releasing hormone (CRH) promoter is implicated in activation of the hypothalamus–pituitary–adrenal (HPA) axis, further insight into how retinoids modulate HPA axis activity is lacking. Here we show that all-trans retinoic acid (RA)-induced HPA activation involves impairments in glucocorticoid receptor (GR) negative feedback. RA was applied to rats chronically through intracerebroventricular injection. A 19-day RA exposure induced potent HPA axis activation and typical depression-like behavior. Dexamethasone failed to suppress basal corticosterone (CORT) secretion, which is indicative of a disturbed GR negative feedback. In the hypothalamic paraventricular nucleus, increased CRH+ and c-fos+ cells were found while a negative R−2+/ER+ correlation was present between the number of RAR-α+ and GR+ cells. This was paralleled by increased RAR-α and decreased GR protein expression in the hypothalamus. Additional in vitro studies confirmed that RA abolished GR-mediated glucocorticoid-induced suppression of CRH expression, indicating a negative cross-talk between RAR-α and GR signaling pathways. Finally, the above changes could be rapidly normalized by treatment with GR antagonist mifepristone. We conclude that in addition to the ‘classic' RAR-α-mediated transcriptional control of CRH expression, disturbances in GR negative feedback constitute a novel pathway that underlies RA-induced HPA axis hyperactivity. The rapid normalization by mifepristone may be of potential clinical interest in this respect.
Keywords: all-trans retinoic acid, corticotropin-releasing hormone, depression, glucocorticoid receptor, hypothalamus–pituitary–adrenal axis, mifepristone (RU38486)
Introduction
The retinoid family comprises vitamin A, its metabolite 13-cis-retinoic acid (13-cis-RA) and all-trans retinoic acid (RA). 13-cis-RA reaches bioactivity mostly via isomerization to RA, which has a high affinity for the nuclear receptor retinoic acid receptor (RAR).1 Emerging evidence demonstrate that retinoids are essential for the developing2, 3, 4 as well as adult brain.5, 6, 7 Through dietary vitamin A consumption or treatment of severe acne with 13-cis-RA, excessive retinoid intake in humans has been implicated in mood disorders like depression. Evidence are from abundant clinical case reports uncovering the association between retinoid treatment and depressive symptoms.8, 9, 10, 11 Recently, abnormal endogenous retinoid signaling has also been found in the brain of depressed patients.12,13 In the paraventricular nucleus (PVN) of patients with affective disorders, both the density of RAR-α-immunoreactive (IR) neurons and the numbers of corticotropin-releasing hormone (CRH)–RAR-α double-stained neurons were found to be significantly increased.12 Moreover, compromised RA and BDNF-TrkB signaling was found in the prefrontal cortex of mood disorder patients, which was supported by a reduced expression of the key elements of RA synthesis and metabolism in the dorsolateral prefrontal cortex/anterior cingulate cortex of elderly depressed patients.13
Hypothalamus–pituitary–adrenal (HPA) axis hyperactivity is often seen in depressive patients.14 CRH plays a central role in controlling stress response and regulating HPA axis activity.15 Previously, we had shown that RAR-α upregulates CRH gene expression by its recruitment to the CRH promoter.12 Chronic RA treatment further induces HPA axis hyperactivity and anxiety-related behavior.16 These findings provided an essential underlying mechanism for the involvement of RA in the pathophysiology of depression. Fine-tuning the regulation of HPA axis activity through glucocorticoid receptor (GR)-mediated negative feedback is essential for adaptation to stress.17,18 The peripheral impairments in GR negative feedback and elevations in basal cortisol levels that are paralleled by a central overproduction of CRH and vasopressin are prominent features in neuropsychiatric disorders.19, 20, 21 Stressful life events also increase the risk of developing depression, while depressed patients with an incompletely attenuated HPA axis after antidepressant therapy have a higher risk for a relapse.22, 23, 24, 25, 26 Furthermore, direct intracerebroventricular (i.c.v.) injection of CRH induces several behavioral symptoms of depression in rodents.27 On the other hand, successful antidepressant or anti-glucocorticoid treatment may facilitate feedback inhibition by targeting GR.28, 29, 30, 31 However, whether alterations in GR-mediated negative feedback are involved in the RA-induced HPA changes remains elusive.
In the present study, we investigated: (i) whether acute RA infusion alters plasma CORT levels through RAR-α (ii) whether chronic RA administration modulates HPA axis activity and induces any depression-like behavior via alterations in GR negative feedback; (iii) possible effects of RA on GR-mediated glucocorticoid suppression of CRH expression in vitro; and finally, (iv) whether these parameters can be normalized by treatment with the GR antagonist mifepristone (RU38486).
Materials and methods
Animals
All animal experiments and procedures were approved by the animal ethical committee of University of Science and Technology of China and in accordance with the guide for care and use of laboratory animals of the National Institutes of Health. A total of 66 male adult Sprague–Dawley rats (8–10 weeks of age, 300–350 g) were housed under controlled conditions of a 12/12-h light/dark cycle with a standard diet and water ad libitum and were handled daily for one week before experiments started. Twelve-hour light cycle in the animal room was from 0700 to 1900. Temperature and humidity were kept constant (20–22 °C and 50–55%, respectively).
Details for the acute experiment study are provided in Supplementary Methods.
For the chronic experiment, 36 rats were assigned either to a vehicle (VEH; n=12), RA (n=12), vehicle plus mifepristone (VEH+MIF; n=6) or a RA plus mifepristone group (RA+MIF; n=6). Among the 36 rats, 24 rats (n=6 for each treatment group) were used for plasma corticosterone (CORT) evaluation, behavioral tests and subsequent immunohistochemical study. The other 12 rats (n=6 for each VEH and RA group) were used for western blot analysis of brain hypothalamic samples.
I.c.v. surgery
I.c.v. surgery was performed 7 days before drug administration. With standard Kopf stereotaxic apparatus, a guide cannula was placed into the lateral cerebral ventricle (anterior posterior, 1.0 mm; lateral, 1.5 mm; 3.5 mm ventral from dura). Intravenous cannulation of the right jugular vein was performed according to previously described methods.32 All probe locations were verified in thionin-stained 40-μm cryostat sections. Only animals with a correct probe placement were used for data analysis.
Drug administration and blood sampling
Drug administration was performed manually by inserting an infusion probe cannula connected to either a Hamilton syringe (chronic model) or a syringe pump (acute model). Blood was sampled from an intravenous cannula in a sound-isolated room with minimal disturbance. Blood samples of 0.2 ml were replaced with equivalent volumes of heparinized saline.
For the chronic treatment, drugs were given daily between 0900 and 0930. The RA group received 20 μg RA (Sigma-Aldrich, St Louis, MO, USA) dissolved in 2 μl 1:1 v/v dimethyl sulfoxide (DMSO):saline avoiding light exposure16,33 once daily for 19 consecutive days. The VEH group received 2 μl 1:1 v/v DMSO:saline each day. Mifepristone treatment groups received 100 ng mifepristone (Sigma-Aldrich),34 without (VEH+MIF group) or with 20 μg RA together (RA+MIF group), which was dissolved in 2 μl 1:1 v/v DMSO:saline and injected daily during the last 5 days. At 45 min before the last day drug injection, blood samples were collected.
Stress effects on HPA activity
Animals were subjected to a 10-min forced swimming stress at 1530, that is, 6 h after the last chronic drug injection.35 Blood samples were collected immediately after stress. After sampling, rats were dried and warmed for 15 min.
Dexamethasone (DEX) suppression test (DST)
The next day after chronic drug treatment, DEX (Sigma-Aldrich; 100 μg in 0.1 ml saline)36 was injected through an intravenous cannula at 0900 hours. Blood samples were collected before DEX injection for a basal value (t=0 min) and then sequentially at t=45 min and t=90 min. At t=90 min, animals were subjected to acute stress (10-min forced swimming). CORT levels were examined directly after stress termination (t=100 min), and subsequently at t=110 min and 130 min.
Depression/anxiety-related behavioral tests
All behavioral tests were performed between 0800 and 0000 hours after 20 min adaptation. Twenty-four chronically treated rats (n=6 for each of the four groups) were tested. Detailed procedures for open-field test are shown in the Supplementary Methods.
Sucrose preference test
The sucrose preference test was performed at 1130 on the same day after the DST and before the other behavioral tests. Animals were trained to drink 1% (w/v) sucrose solution for 24 h. The next day, they were given free access to two bottles containing normal water and sucrose solution. To avoid left/right preference, bottle order (left–right placement of water vs sucrose) was alternated for each rat during the middle of both the adaptation and testing period. Bottles were weighed at the beginning and end of the testing period of 24 h. The percentage of sucrose solution from total liquid consumed during 24 h was measured for anhedonia, a core symptom of ‘depression-like behavior'.37
Elevated plus maze
The elevated plus maze test evaluates anxiety-related behavior.16,38,39 Rats were placed in the central arena of a black plus-shaped maze, facing an open arm and were left to explore for 5 min. The duration and frequency at which open arms were explored was analyzed by video camera and processed by EthoVision (Noldus, Wageningen, The Netherlands).
Open-field test
Details for the open-field tests are provided in the Supplementary Methods.
Plasma CORT
Blood samples were collected in heparin-coated tubes, immediately chilled on ice and centrifuged at 4000 r.p.m. for 15 min at 4 °C. Plasma was stored at −80 °C for measuring plasma CORT using an enzyme-linked immunosorbent assay kit (RapidBio Lab, Calabasas, CA, USA).
Brain tissue, immunohistochemistry and image acquisition
For killing, all animals were anesthetized in the morning (0900–1100) with sodium pentobarbital (1 mg/kg) in individual cages. After behavioral tests, the 24 chronically treated rats (n=6 for each group) were perfused transcardially with saline followed by 4% paraformaldehyde. Brains were cryoprotected in 30% sucrose before sections (40 μm thick) were cut. Another 12 chronically treated rats (n=6 for each VEH and RA group) were quickly decapitated the next day after the last day chronic drug injection. Hypothalami were dissected according to literature40 before being quickly frozen in liquid nitrogen and stored at −80 °C.
Immunohistochemical staining of each marker was performed in every eighth section taken along the rostrocaudal axis throughout PVN according to standard procedures,41 with primary antibodies of anti-CRH (rabbit, 1:2000; Bachem, Torrance, CA, USA), anti-c-fos (rabbit, 1:800; Santa Cruz, Santa Cruz, CA, USA), anti-RAR-α (rabbit, 1:100; Abcam, Cambridge, UK) and anti-GR (rabbit, 1:200; Santa Cruz). Information on antibody specificity has been provided in the Supplementary File. Amplification was performed with biotinylated goat-anti-rabbit secondary antibodies (1:200; Vector Laboratories, Burlingame, CA, USA) and avidin-biotin complex (1:800; Vector Laboratories). Chromogen development was performed with diaminobenzidine. Photographs were collected using a Nikon E800u microscope (Nikon, Tokyo, Japan) and a Canon Digital camera (PowerShot S40, Canon, Tokyo, Japan). Immunopositive cells were counted manually at a × 100 magnification, which was followed by confirmation at × 400 magnification (for details see Supplementary Methods) by an investigator blind to the experimental conditions.16,42
Western blot
Hypothalamic samples were used to quantify RAR-α and GR protein as described.12 Protein samples were detected with anti-RAR-α (rabbit, 1:500; Santa Cruz) and GR primary antibody (rabbit, 1:50 000; Abcam) and then horseradish peroxidase-conjugated goat-anti-rabbit IgG (1:2000; Promega, Madison, WI, USA), using horseradish peroxidase-conjugated β-actin (KC-5A08, 1:2000; Kangchen, Shanghai, China) as internal control. Signals were detected with an ECL chemiluminescence system (SuperSignal West Pico chemiluminescent Substrate, Pierce, IL, USA). Immunoblots were quantified using a high-resolution scanner. Background subtraction was performed and density was calculated using ImageJ software (Wayne Rasband, National Institute of Mental Health, Bethesda, MD, USA). Results were expressed as percentage of β-actin.
In vitro studies
The human neuroblastoma BE(2)C cell line expressing CRH, both intrinsically and upon RA treatment,43,44 was cultured with Dulbecco's modified Eagle's medium/F12 (DF; Sigma, St Louis, MO, USA) supplied with 10% fetal bovine serum (FBS; Gibco, Grand Island, NY, USA). Cultures were maintained at 37 °C in 5% CO2 and a humidified atmosphere.
GR-mediated glucocorticoid repression of CRH gene expression
As GR is not endogenously expressed in BE(2)C cells,45 a transient transfection was performed with previously tested 6RGR-based rat GR-α plasmid.46,47 Twenty-four hours after plating, cells were transfected with 0.3 μg GR-α or an empty plasmid (NE) using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA). Four hours after transfection, culture media were changed to phenol red-free DF containing 10% FBS and 1 μM RA or VEH (0.1% DMSO in final volume) with or without 100 nM DEX or/and 100 nM mifepristone. 1 μM RA,12 100 nM DEX45 and 100 nM mifepristone48 were dissolved in 0.1% DMSO and diluted in DF with 10% FBS before application. Cells were harvested 24 h later.
Real-time quantitative RT-PCR analysis
CRH mRNA expression was analyzed with β-actin as internal control. Total RNA was extracted using Trizol extraction (Invitrogen). cDNA was synthesized using reverse transcriptase (Promega). Real-time quantitative RT-PCR was performed using SYBR Green Mix (Takara, Dalian, China) and amplified with an ABI Prism 7000 system (Applied Biosystems, Foster City, CA, USA). The following upper and lower primers were used: human CRH (NM_000756) forward: 5′-CATCTCCCTGGATCTCACCTTC-3′ reverse: 5′-AATAATCTCCATGAGTTTCCTGTTG-3′ human β-actin (NM_001101 65) forward: 5′-CCCAGCCATGTACGTTGCTA-3′ reverse: 5′-TCACCGGAGTCCATCACGAT-3′. The relative amount of target gene was calculated using the 2−ΔΔCt method.49
Statistics
Data are expressed as mean±s.e.m. All statistics were performed using SPSS 17.0. (IBM SPSS Statistics, Armonk, NY, USA). For evaluation of basal CORT values, behavioral and immunohistochemistry results, data were subjected to a one-way analysis of variance (ANOVA) followed by post-hoc Tukey's test. For stress-induced CORT changes, repeated measure ANOVA was followed by post-hoc Tukey's test. In DST, CORT data were subjected to repeated measure ANOVA separately under basal and stress condition. One-way ANOVA was used to compare time effects within each group, followed by a post-hoc Tukey's test. Spearman's correlation test was used to analyze correlations between: (i) the number of RAR-α- and GR-immunopositive cells in the PVN; and (ii) sucrose preference and corresponding plasma CORT. For results of western blot and real-time quantitative RT-PCR study, Student's t-tests were used to compare between the groups. A P-value of 0.05 was considered significant.
Results
Acute treatment study
Plasma CORT concentration changes in response to time during a 2-h acute infusion of each drug are shown in Supplementary Figure S1.
Chronic treatment study
Basal and stress-induced CORT changes and depression/anxiety-related behavior
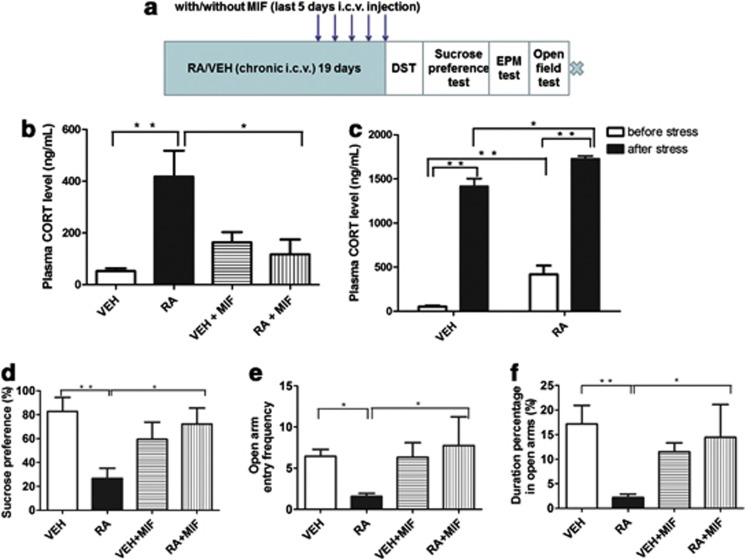
The experimental schedule of chronic treatment study is described in Figure 1a. Body weight changes after chronic drug treatment were compared among the four groups (Supplementary Figure S2). Effects of chronic RA-induced alterations in the stress response were evaluated. Under basal conditions, significantly different CORT levels were found among the VEH, RA, VEH+MIF and RA+MIF groups (F(3,16)=6.916, P=0.003) (Figure 1b). Post-hoc analysis revealed the basal CORT concentration in the RA group to be higher than that in the VEH group (P=0.003); mifepristone treatment significantly normalized basal CORT values in the RA group (P=0.014 RA+MIF vs RA) but mifepristone alone had no effect (P=0.586 VEH+MIF vs VEH). As shown in Figure 1c, under acute stress, CORT concentration is significantly higher in the RA compared with VEH group (F(1,8)=24.557, P=0.001).
Figure 1.
Plasma corticosterone (CORT) concentration and depression/anxiety-related behavioral changes in the chronic all-trans retinoic acid (RA) treatment experiment. (a) Experimental design of chronic drug treatment experiment. Animals were chronically exposed to RA or vehicle (VEH) via intracerebroventricular (i.c.v.) injection for 19 days, in combination with or without mifepristone (MIF) injection during the last 5 days. This resulted in four chronic treatment groups: VEH group, RA group, VEH plus MIF (VEH+MIF) group and an RA plus MIF (RA+MIF) group (n=6 animals per group). After chronic treatment, animals were subject to four sequential sets of behavioral tests and evaluated for depression/anxiety-related behavior: dexamethasone suppression test (DST; at day 20), sucrose preference test (starting adaptation at day 20 after DST, and tested at day 21), elevated plus maze (EPM) test (at day 22) and open-field test (at day 23). At day of 24, animals were killed. (b) Basal plasma CORT concentrations compared among the four chronic treatment groups. (c) Acute stress-induced CORT concentration changes compared between the chronic RA group and the VEH group. Animals were subject to a 10-min acute forced swimming stress. Note that the plasma CORT values before stress in these two groups are the same as the basal CORT concentration as shown in panel b. (d) Sucrose preference percentage compared among the four chronic treatment groups. (e) The frequencies of open arm entry and (f) the percentage of duration in the open arms measured in the EPM experiment compared among the four chronic treatment groups. All data are presented as mean±s.e.m. (n=6 animals per group). *P<0.05; **P<0.01.
A difference in sucrose uptake was found among the four groups (F(3,19)=5.318, P=0.008; Figure 1d). Sucrose preference in RA group was significantly decreased compared with VEH group (P=0.01). Remarkably, the RA-induced decrease in sucrose uptake was normalized by mifepristone (P=0.03 RA+MIF vs RA). Mifepristone alone was ineffective (P=0.594 VEH+MIF vs VEH).
In the elevated plus maze experiment, a significant difference in both entry frequency (F(3,19)=3.890, P=0.025) and duration percentage in open arms (F(3,19)=6.567, P=0.003) was found among the four groups (Figures 1e and f). Both parameters were significantly decreased in the RA compared with VEH group (P=0.048 and P=0.004, respectively), which were again normalized by mifepristone (P=0.043 and P=0.034 RA+MIF vs RA). Mifepristone itself had no effect on both parameters (P=1.000 and P=0.623 VEH+MIF vs VEH). Results of the open-field experiment are shown in Supplementary Figure S3.
DST
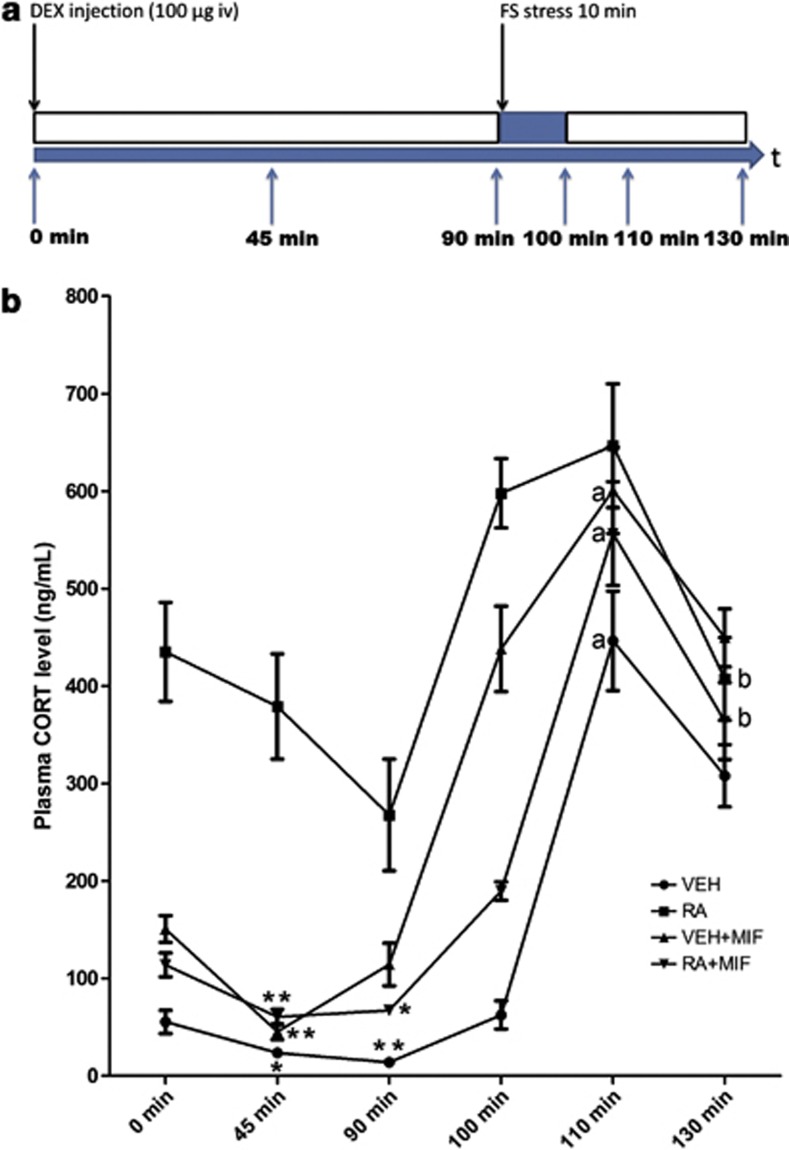
To examine the GR-mediated glucocorticoid-negative feedback, we analyzed HPA changes by chronic RA exposure before and after stress under conditions of a DEX challenge. The design of the DST is shown in Figure 2a.
Figure 2.
Dexamethasone (DEX) suppression test (DST). (a) Protocol of the DST. Blood sample was first collected immediately before a DEX injection (t=0 min, intravenous injection of 100 μg DEX in 0.1 ml saline) and then sequentially at 45 min (t=45 min) and 90 min (t=90 min) after DEX injection. At 90 min after DEX injection (t=90 min), an acute stress challenge (10 min forced swimming) was given. Blood was collected immediately after stress termination (t=100 min) and then sequentially at 10 min and 30 min after stress termination (t=110 and 130 min, respectively). (b) Plasma corticosterone (CORT) concentration changes in response to time after DEX injection and 10 min acute stress were compared among the four chronic treatment groups: vehicle (VEH) group, all-trans retinoic acid (RA) group, VEH plus mifepristone (VEH+MIF) group and RA plus mifepristone (RA+MIF) group. Data are presented as mean±s.e.m. (n=6 animals per group). *P<0.05; **P<0.01 (significantly different within group compared at t=45 min vs t=0 min and at t=90 min vs t=0 min); a: P<0.05 (significantly different within group compared at t=110 min vs t=100 min); b: P<0.05 (significantly different within group compared at t=130 min vs t=110 min).
Under basal conditions, DEX treatment significantly suppressed plasma CORT concentration (time effect, F(2,9)=6.723, P=0.016); this effect was significantly different among groups (group effect, F(3,27)=82.023, P<0.001; Figure 2b). In the VEH group, basal CORT secretion significantly differed by time (F(2,9)=8.266, P=0.009); CORT was suppressed significantly at both t=45 min (P=0.037) and t=90 min (P=0.009) compared with t=0 min. However, this was not observed in the RA group (F(2,9)=2.478, P=0.139). Basal CORT secretion differed over time also in the VEH+MIF group (F(2,9)=11.728, P=0.003), where CORT was suppressed at t=45 min (P=0.003 vs t=0 min) but not at t=90 min (P=0.278 vs t=0 min). In the RA+MIF group, also a significantly different time effect was found (F(2,9)=10.843, P=0.004): CORT was suppressed at both t=45 min (P=0.005) and t=90 min (P=0.012) compared with t=0 min. The above results indicate an impaired GR negative feedback in RA-treated rats, which could be normalized by mifepristone.
Acute stress altered plasma CORT concentration significantly (time effect, F(2,9)=48.03, P<0.001). Again, a significant treatment effect was found (group effect, F(3,27)=26.13, P<0.001); time × group effect (F(6, 27)=6.099, P<0.001). In detail, after acute stress, both VEH and RA groups showed significant time effects (F(2,9)=29.676, P<0.001 and F(2,9)=6.746, P=0.016, respectively). However, increased CORT was found in the VEH (P<0.001) but not in the RA group (P=0.765) at t=110 min compared with t=100 min. A decrease in CORT was found in the RA (P=0.017) but not in the VEH group (P=0.054) at t=130 min compared with t=110 min. Both VEH+MIF and RA+MIF groups showed significant time effects (F(2,9)=5.206, P=0.031 and F(2,9)=22.553, P<0.001, respectively). Both groups showed increased CORT concentrations at t=110 min (P=0.043 and P<0.001 vs t=100 min), but only RA+MIF group showed decreases in CORT at t=130 min compared with t=110 min (P=0.016). The rapid rise in CORT after stress, even after a DEX challenge in RA-treated rats, is thus indicative of a hyperactive HPA axis.
Changes of CRH, c-fos, RAR-α and GR immunoreactivity in the PVN and changes of hypothalamic RAR-α and GR protein expression
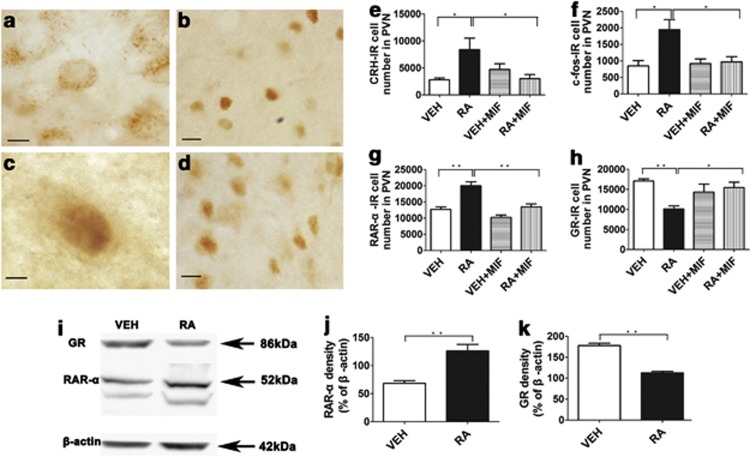
Representative examples of individual immunopositive cells for CRH, c-fos, RAR-α and GR in the hypothalamic PVN are shown in Figures 3a, b, c and d, respectively. Immunostaining patterns of each marker in the PVN were compared among different groups as shown in Supplementary Figure S4.
Figure 3.
Changes of corticotropin-releasing hormone (CRH), c-fos, nuclear receptor retinoic acid receptor-α (RAR-α) and glucocorticoid receptor (GR)-immunoreactive (IR) cell numbers in the hypothalamic paraventricular nucleus (PVN) and changes of RAR-α and GR protein expression in the hypothalamus. Examples of individual immunopositive cells for: (a) CRH (scale bar: 20 μm); (b) c-fos (scale bar: 20 μm); (c) RAR-α (scale bar: 10 μm); and (d) GR (scale bar: 20 μm) in the hypothalamic PVN. × 1000 magnification. Comparison of the numbers of (e) CRH-IR; (f) c-fos-IR; (g) RAR-α-IR; and (h) GR-IR cells in the hypothalamic PVN among the four chronic treatment groups: vehicle (VEH) group, all-trans retinoic acid (RA) group, VEH plus mifepristone (VEH+MIF) group and RA plus mifepristone (RA+MIF) group. (i) Western blot example of RAR-α and GR protein expression in the hypothalamus of chronic VEH- vs RA-treated rats. Arrows point to the molecular weight bands of GR (86 kDa), RAR-α (52 kDa) and internal control β-actin (42 kDa). Average protein density of RAR-α (j) and GR (k) expression in the hypothalamus was compared between chronic VEH and RA groups. All data are presented as mean±s.e.m. (n=6 animals per group). *P<0.05; **P<0.01.
The immunoreactive cells for CRH, c-fos, RAR-α and GR in the PVN were quantified to compare differences among the groups. As shown in Figure 3e, a significantly different CRH-IR cell number was found among groups (F(3,20)=3.944, P=0.023). CRH-IR cell number was higher in the RA than in the VEH group (P=0.047), which was normalized by mifepristone treatment (P=0.025 RA-MIF vs RA). Similar results were found for the c-fos-IR cells (F(3,20)=5.547, P=0.006) that were significantly increased in the RA vs VEH group (P=0.018), and also normalized by mifepristone (P=0.028 RA+MIF vs RA) (Figure 3f).
Figure 3g shows differences in RAR-α-IR cell numbers between groups (F(3,20)=20.056, P<0.001). RAR-α-IR cells were significantly increased in the RA group (P<0.001 vs VEH), which was normalized by mifepristone (P<0.001 RA+MIF vs RA). The number of GR-IR cells was also significantly different among groups (F(3,20)=5.544, P=0.006). GR-IR cells were significantly decreased in the RA compared with the VEH group (P=0.006); this was again normalized by mifepristone (P=0.03 RA+MIF vs RA; Figure 3h). For all the four markers examined, mifepristone treatment alone was ineffective (all P>0.05, VEH+MIF vs VEH).
Figure 3i shows western examples of RAR-α and GR protein expression in the hypothalamus of chronic VEH vs RA group. Consistent with the immunohistochemistry, RAR-α density based on isolations from the hypothalamus of RA group (n=6, 126.27±11.53% of β-actin) was significantly increased compared with the VEH group (n=6, 68.36±4.65%, P<0.01; Figure 3j). In contrast, GR density in the hypothalamus of the RA group (n=6, 112.45±3.76% of β-actin) was significantly decreased compared with the VEH group (n=6, 177.64±5.85%, P<0.01; Figure 3k).
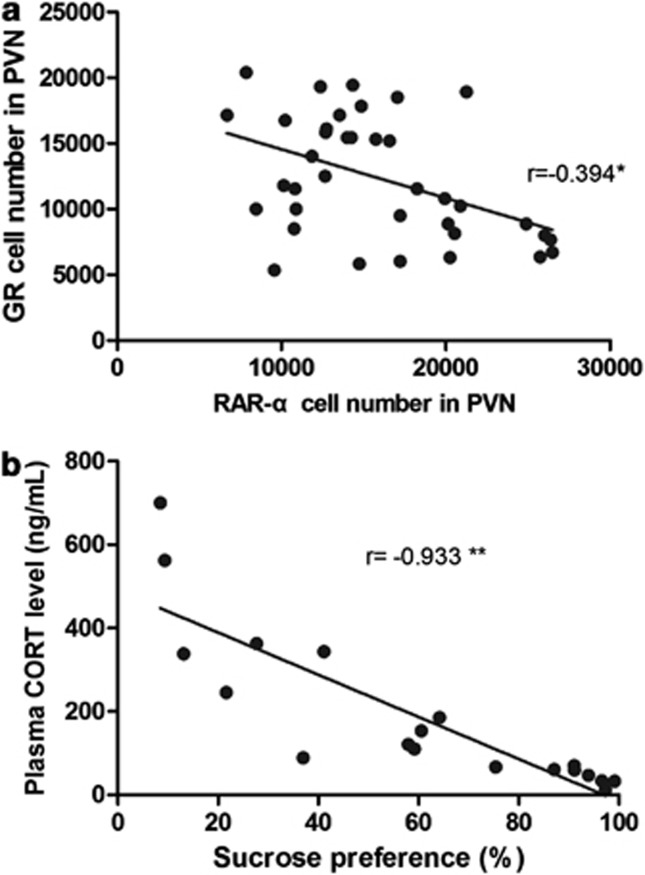
Correlations between RAR-α- and GR-immunopositive cell numbers and between sucrose preference and plasma CORT
We next examined the relationship between the number of RAR-α-IR and GR-IR cells in the PVN. Figure 4a shows a significant negative correlation between the RAR-α-IR and GR-IR cell numbers in the hypothalamic PVN (correlation coefficient R=−0.394, P=0.016). To investigate potential effects of plasma CORT on depressive behavior, we examined the correlation between sucrose preference (a measure for anhedonia, core symptom of depression) and corresponding plasma CORT levels, that was also found significantly negative (correlation coefficient R=−0.933, P<0.001; Figure 4b).
Figure 4.
(a) Correlations between nuclear receptor retinoic acid receptor-α (RAR-α)- and glucocorticoid receptor (GR)-immunoreactive (IR) cell number in the hypothalamic paraventricular nucleus (PVN); and (b) correlations between sucrose preference percentage and the corresponding plasma corticosterone (CORT) concentration. Note that the number of RAR-α-IR and GR-IR cells is based on pooled data from the four chronic treatment groups analyzed throughout the entire PVN as shown in Figures 3g and h; the value of sucrose preference percentage and corresponding plasma CORT is also based on pooled data from the four chronic treatment groups as shown in Figures 1b and d. *P<0.05; **P<0.01
In vitro studies
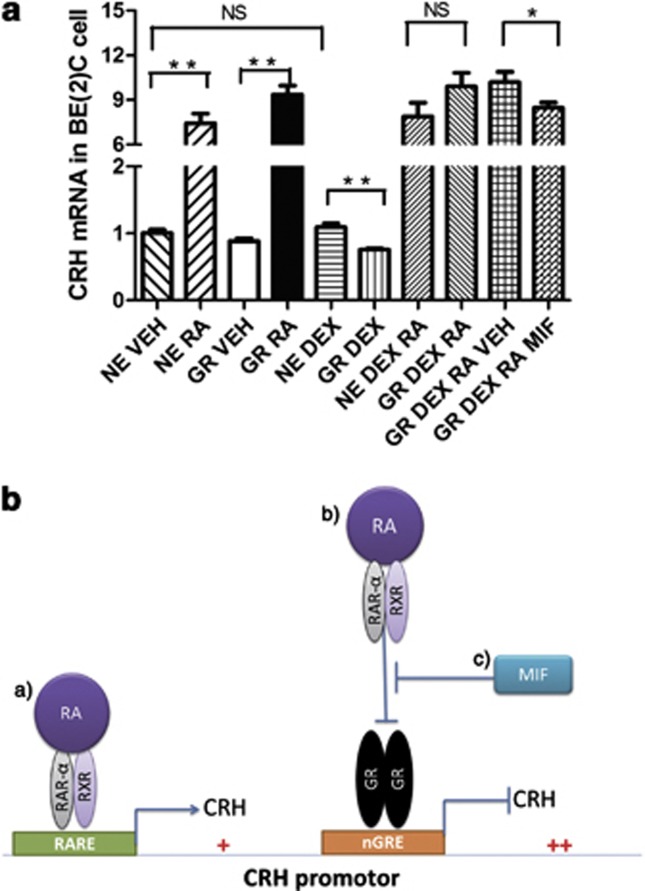
GR-mediated glucocorticoid repression of CRH mRNA in BE(2)C cells
In vitro studies were performed to address how RA modulates GR-mediated suppression of CRH expression. Figure 5a shows that RA treatment significantly increased CRH mRNA expression in BE(2)C cells (both NE RA vs NE VEH and GR RA vs GR VEH, P<0.001); DEX treatment alone had no effect (NE DEX vs NE VEH, P=0.273). Under conditions of GR overexpression, DEX significantly decreased CRH expression (GR DEX vs NE DEX, P<0.001); whereas in the presence of RA, such inhibition was abolished (GR DEX RA vs NE DEX RA, P=0.153). Mifepristone significantly normalized the attenuated DEX repression of CRH expression by RA (GR DEX RA MIF vs GR DEX RA VEH, P<0.05). VEH of mifepristone alone had no effect (GR DEX RA VEH vs GR DEX RA, P=0.805).
Figure 5.
All-trans retinoic acid (RA) interfered with glucocorticoid receptor (GR)-mediated glucocorticoid suppression of corticotropin-releasing hormone (CRH) mRNA in BE(2)C cells. (a) Effects of different treatment conditions on CRH mRNA expression in the BE(2)C cell line in the presence or absence of transient transfection of GR-α plasmid. NE: empty plasmid control; GR: rat GR-α plasmid; DEX: 100 nM dexamethasone; VEH: 0.1% DMSO in final volume; RA: 1 μM RA; MIF: 100 nM mifepristone. Data are presented as mean±s.e.m. (n=6 per group). NS: not significant; *P<0.05; **P<0.01. (b) A model shows two pathways in RA-induced CRH overexpression: (A) mediated by RAR-α transcriptional activation via RA response element (RARE) at the CRH promoter and (B) mediated by RAR-α de-repression of GR transcriptional repression via negative glucocorticoid response element (nGRE) at the CRH promoter, which could be restored by mifepristone (MIF) co-treatment (C).
Together, RA abolished the GR-mediated repression of CRH expression by glucocorticoids, an effect that can be restored by co-treatment with the GR antagonist mifepristone (illustrated by the model shown in Figure 5b).
Discussion
Following our earlier demonstration that RAR-α upregulates CRH expression,12 we now show that disturbed GR negative feedback is involved in RA-induced HPA hyperactivity. We demonstrate that (i) acute RA infusion elevates CORT secretion through RAR-α (ii) chronic RA treatment increased CRH and decreased GR expression in the hypothalamic PVN, indicative of impaired HPA feedback inhibition; (iii) RA abolished GR-mediated repression of CRH expression by glucocorticoids in vitro, indicating a negative cross-talk between RAR-α and GR signaling; (iv) the RA-induced HPA hyperactivity, CRH overexpression and disturbances in GR negative feedback could all be quickly normalized by treatment with the GR antagonist mifepristone.
Clinical basis of the current study
In humans, accutane (13-cis-RA or isotretinoin) is usually used orally at 0.5–2.0 mg kg−1 per day over a 4-month treatment period. Clinical evidence shows that treatment with 13-cis-RA in a restricted dose range as low as 0.5–1 mg kg−1 per day can cause depression in susceptible individuals.8,11,50 In adult mice, when given at a clinical dose of 1 mg kg−1 by daily intraperitoneal (i.p.) injection for 3–6 weeks, 13-cis-RA produces depression-related behavior9 and suppresses hippocampal-dependent learning.51 Our previous work had revealed that hyperactivation of HPA axis occurs after applying RA at a dose at the upper limit of what is used for clinical treatment of acne (2 mg kg−1 per day), which translated into daily i.p. injection of young rats for 6 weeks.16 In the current study, to ensure an efficient and direct incorporation into the brain, we performed an i.c.v. injection of 20 μg RA into adult rats daily for 19 days at a dose 30–40 times lower than by systemic i.p. injection. This dose is also based on a reported neuroprotective i.c.v. dosage of 9-cis-RA.33 Our results with this dose show comparable effects on the activation of HPA axis.
Decreased expression of GR in hypothalamus contributes to RA-induced deficient HPA negative feedback
Activation of the HPA axis is driven by CRH neurons in the hypothalamic PVN.52 The increased c-fos expression that occurred particularly in the parvocellular portion of the PVN after chronic RA exposure indicates CRH neurons are activated, as confirmed by CRH immunostaining. In addition, the DEX non-suppression profile is consistent with an impaired GR negative feedback. Our hypothesis that the GR links RA signaling and HPA hyperactivity is further supported by the negative correlation between the RAR-α-IR and GR-IR cell numbers in the PVN, and by the increased RAR-α and decreased GR protein expression in the hypothalamus. Moreover, co-localization of RAR-α and GR in the PVN (our unpublished data), a primary target region for glucocorticoid-mediated negative feedback and HPA suppression,53, 54, 55 may further suggest the existence of a complex local RA-glucocorticoid signaling cross-talk. As the GR is pivotal for both DEX suppression of CRH transcription44,56 and stress reactivity control,57, 58, 59 decreased expression of hypothalamic GR is indicative of a disinhibition of the HPA axis. In turn, this may result in hypothalamic CRH overexpression,60,61 enhanced excitation of CRH neurons and stress hyper-sensitivity.
Negative cross-talk between RAR-α and GR signaling
Our in vitro experiment suggests that RA abolished the GR-mediated suppression of CRH expression by glucocorticoid, compatible with a negative cross-talk between RAR-α and GR signaling transduction systems. In a situation of GR overexpression, activated RAR-α might interfere with formation of the GR repressing complex on the nGRE of the CRH promoter, presumably by either preventing the recruitment of co-repressors62 or destabilizing the repressing complex. In support of this view, ligated RAR-α was recently found to co-immunoprecipitate with ligated GR and to physically interact directly in thymocytes.63 A similar mechanism of direct protein-protein interaction and tethering of GR and AP-1 (c-Jun/c-Fos) has been suggested to contribute to their mutual transcriptional repression.64 Thus, we propose that RA may act as a de-repressor of GR transcriptional repression at CRH promoter, and hence lead to CRH overexpression. However, the precise molecular mechanism by which such regulation occurs at the transcriptional level awaits future study.
Mifepristone restored the impaired GR negative feedback
The negative correlation we found between the sucrose preference percentage and the plasma CORT levels suggests excess cortisol could mediate depressive symptoms like anhedonia. Blocking this response might be beneficial; and indeed mifepristone has been shown to be beneficial in patients with Cushing's disease or psychotic depression65, 66, 67, 68, 69, 70 and in stress-related readouts in rodent models,41,71,72 notably already following a brief treatment. We here administered mifepristone for 5 days to be consistent with previous basic and clinical studies. The present normalized c-fos activation in the PVN by mifepristone suggests a restoration of intrinsic central cellular components of the HPA axis. Mifepristone may reinstate the sensitivity of GR negative feedback through a rapid normalization of GR expression within the PVN, as shown in Figure 3h. Such a facilitation in HPA feedback inhibition has been documented before.73 Additionally, in vitro studies confirmed that mifepristone can restore GR function in repressing CRH transcription, suggesting its partial agonist properties.74,75 Mifepristone was reported to actively recruit specific co-repressors to the GR,74 which would lead to a more tight conformation of GR bound to specific GREs.76 Furthermore, as a GR antagonist with strong affinity to GR, it could effectively block the depressive behavioral consequences of excessive CORT by preventing transactivation of GR-responsive genes.77 GR blockade may further stimulate the function of mineralocorticoid receptor (MR), which contributes to tonic inhibitory control of the HPA axis.17 However, while traditionally known for its GR antagonistic activity, mifepristone also exerts effects on the progesterone receptor at lower concentrations and can influence the CRH system.78 Thus, some observed results could result from its mixed pharmacological profile. Nevertheless, our current study showed that RA-induced HPA hyperactivity, disturbed GR negative feedback and CRH overexpression could all be rapidly normalized by treatment with mifepristone.
There are also several limitations in the present study. First, with regard to the in vitro effect, we only predicted potential modulation of mifepristone based on reported structural and conformational changes by interactions between GR and mifepristone. To test our hypothesis in detail, it would require extra work at molecular level, such as identification of critical amino-acid residues involved. Second, we performed i.c.v. injection of RA at a single dose (20 μg RA) daily for 19 days. Further comparison of varying doses to understand its efficacy range awaits future study.
Taken together, we propose that RA activates the HPA axis through (i) an increased hypothalamic CRH production, mediated via RAR-α transcriptional activation; (ii) a deficient negative feedback at the level of hypothalamic GR expression, which implicates changes in GR sensitivity to underlie RA-induced hyperactivity of the HPA axis. In humans, such maladaptive changes in the HPA axis after excessive RA treatment or vitamin A consumption may set the stage for stress-related neuropsychiatric disorders. The rapid reversal by mifepristone may hence be of interest for the development of therapeutic options for HPA-related aspects of depression.
Acknowledgments
This work was supported by the Natural Science Foundation of China (81100811 and 91132304), Strategic Priority Research Program of the Chinese Academy of Science (XDB02030001) and China Postdoctoral Science Foundation (2011M501053). PJL is supported by the HersenStichting Nederland and the ISAO. We thank Dr A Korosi (SILS-CNS, University of Amsterdam) for assistance and Dr OC Meijer (Leiden University) for kind provision of the rat GR-α plasmid and for his constructive comments to our manuscript. We also thank Professor Ronald M Evans (The Salk Institute for Biological Studies) for the hGR-α plasmid.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Translational Psychiatry website (http://www.nature.com/tp)
Supplementary Material
References
- Tsukada M, Schroder M, Roos TC, Chandraratna RA, Reichert U, Merk HF, et al. 13-cis retinoic acid exerts its specific activity on human sebocytes through selective intracellular isomerization to all-trans retinoic acid and binding to retinoid acid receptors. J Invest Dermatol. 2000;115:321–327. doi: 10.1046/j.1523-1747.2000.00066.x. [DOI] [PubMed] [Google Scholar]
- Durston AJ, Timmermans JP, Hage WJ, Hendriks HF, de Vries NJ, Heideveld M, et al. Retinoic acid causes an anteroposterior transformation in the developing central nervous system. Nature. 1989;340:140–144. doi: 10.1038/340140a0. [DOI] [PubMed] [Google Scholar]
- Maden M, Holder N. The involvement of retinoic acid in the development of the vertebrate central nervous system. Development. 1991;Suppl 2:87–94. [PubMed] [Google Scholar]
- Maden M. Retinoic acid in the development, regeneration and maintenance of the nervous system. Nat Rev Neurosci. 2007;8:755–765. doi: 10.1038/nrn2212. [DOI] [PubMed] [Google Scholar]
- Jacobs S, Lie DC, DeCicco KL, Shi Y, DeLuca LM, Gage FH, et al. Retinoic acid is required early during adult neurogenesis in the dentate gyrus. Proc Natl Acad Sci USA. 2006;103:3902–3907. doi: 10.1073/pnas.0511294103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aoto J, Nam CI, Poon MM, Ting P, Chen L. Synaptic signaling by all-trans retinoic acid in homeostatic synaptic plasticity. Neuron. 2008;60:308–320. doi: 10.1016/j.neuron.2008.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang HL, Zhang Z, Hintze M, Chen L. Decrease in calcium concentration triggers neuronal retinoic acid synthesis during homeostatic synaptic plasticity. J Neurosci. 2011;31:17764–17771. doi: 10.1523/JNEUROSCI.3964-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner JD, Shearer KD, McCaffery PJ. Retinoic acid and affective disorders: the evidence for an association. J Clin Psychiatry. 2012;73:37–50. doi: 10.4088/JCP.10r05993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Reilly KC, Shumake J, Gonzalez-Lima F, Lane MA, Bailey SJ. Chronic administration of 13-cis-retinoic acid increases depression-related behavior in mice. Neuropsychopharmacology. 2006;31:1919–1927. doi: 10.1038/sj.npp.1300998. [DOI] [PubMed] [Google Scholar]
- McCance-Katz EF, Price LH. Depression associated with vitamin A intoxication. Psychosomatics. 1992;33:117–118. doi: 10.1016/S0033-3182(92)72033-7. [DOI] [PubMed] [Google Scholar]
- Wysowski DK, Pitts M, Beitz J. Depression and suicide in patients treated with isotretinoin. N Engl J Med. 2001;344:460. doi: 10.1056/NEJM200102083440616. [DOI] [PubMed] [Google Scholar]
- Chen XN, Meng QY, Bao AM, Swaab DF, Wang GH, Zhou JN. The involvement of retinoic acid receptor-alpha in corticotropin-releasing hormone gene expression and affective disorders. Biol Psychiatry. 2009;66:832–839. doi: 10.1016/j.biopsych.2009.05.031. [DOI] [PubMed] [Google Scholar]
- Qi XR, Zhao J, Liu J, Fang H, Swaab DF, Zhou JN.Abnormal retinoid and TrkB signaling in the prefrontal cortex in mood disorders Cerebral Cortex 2013. doi: 10.1093/cercor/bht203 [DOI] [PubMed]
- de Kloet ER, Joels M, Holsboer F. Stress and the brain: from adaptation to disease. Nat Rev Neurosci. 2005;6:463–475. doi: 10.1038/nrn1683. [DOI] [PubMed] [Google Scholar]
- Kageyama K, Suda T. Regulatory mechanisms underlying corticotropin-releasing factor gene expression in the hypothalamus. Endocr J. 2009;56:335–344. doi: 10.1507/endocrj.k09e-075. [DOI] [PubMed] [Google Scholar]
- Cai L, Yan XB, Chen XN, Meng QY, Zhou JN. Chronic all-trans retinoic acid administration induced hyperactivity of HPA axis and behavioral changes in young rats. Eur Neuropsychopharmacol. 2010;20:839–847. doi: 10.1016/j.euroneuro.2010.06.019. [DOI] [PubMed] [Google Scholar]
- De Kloet ER, Vreugdenhil E, Oitzl MS, Joels M. Glucocorticoid feedback resistance. Trends Endocrinol Metab. 1997;8:26–33. doi: 10.1016/s1043-2760(96)00205-6. [DOI] [PubMed] [Google Scholar]
- Myers B, McKlveen JM, Herman JP. Neural regulation of the stress response: the many faces of feedback. Cell Mol Neurobiol. 2012;45:292–298. doi: 10.1007/s10571-012-9801-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swaab DF, Bao AM, Lucassen PJ. The stress system in the human brain in depression and neurodegeneration. Ageing Res Rev. 2005;4:141–194. doi: 10.1016/j.arr.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Schmidt MV, Sterlemann V, Wagner K, Niederleitner B, Ganea K, Liebl C, et al. Postnatal glucocorticoid excess due to pituitary glucocorticoid receptor deficiency: differential short- and long-term consequences. Endocrinology. 2009;150:2709–2716. doi: 10.1210/en.2008-1211. [DOI] [PubMed] [Google Scholar]
- Czeh B, Welt T, Fischer AK, Erhardt A, Schmitt W, Muller MB, et al. Chronic psychosocial stress and concomitant repetitive transcranial magnetic stimulation: effects on stress hormone levels and adult hippocampal neurogenesis. Biol Psychiatry. 2002;52:1057–1065. doi: 10.1016/s0006-3223(02)01457-9. [DOI] [PubMed] [Google Scholar]
- Zobel AW, Yassouridis A, Frieboes RM, Holsboer F. Prediction of medium-term outcome by cortisol response to the combined dexamethasone-CRH test in patients with remitted depression. Am J Psychiatry. 1999;156:949–951. doi: 10.1176/ajp.156.6.949. [DOI] [PubMed] [Google Scholar]
- Raadsheer FC, Hoogendijk WJ, Stam FC, Tilders FJ, Swaab DF. Increased numbers of corticotropin-releasing hormone expressing neurons in the hypothalamic paraventricular nucleus of depressed patients. Neuroendocrinology. 1994;60:436–444. doi: 10.1159/000126778. [DOI] [PubMed] [Google Scholar]
- Raadsheer FC, van Heerikhuize JJ, Lucassen PJ, Hoogendijk WJ, Tilders FJ, Swaab DF. Corticotropin-releasing hormone mRNA levels in the paraventricular nucleus of patients with Alzheimer's disease and depression. Am J Psychiatry. 1995;152:1372–1376. doi: 10.1176/ajp.152.9.1372. [DOI] [PubMed] [Google Scholar]
- Stenzel-Poore MP, Heinrichs SC, Rivest S, Koob GF, Vale WW. Overproduction of corticotropin-releasing factor in transgenic mice: a genetic model of anxiogenic behavior. J Neurosci. 1994;14:2579–2584. doi: 10.1523/JNEUROSCI.14-05-02579.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang SS, Kamphuis W, Huitinga I, Zhou JN, Swaab DF.Gene expression analysis in the human hypothalamus in depression by laser microdissection and real-time PCR: the presence of multiple receptor imbalances Mol Psychiatry 200813786–799., 741. [DOI] [PubMed] [Google Scholar]
- Holsboer F. Stress, hypercortisolism and corticosteroid receptors in depression: implications for therapy. J Affect Disord. 2001;62:77–91. doi: 10.1016/s0165-0327(00)00352-9. [DOI] [PubMed] [Google Scholar]
- Anacker C, Zunszain PA, Carvalho LA, Pariante CM. The glucocorticoid receptor: pivot of depression and of antidepressant treatment. Psychoneuroendocrinology. 2011;36:415–425. doi: 10.1016/j.psyneuen.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barden N. Modulation of glucocorticoid receptor gene expression by antidepressant drugs. Pharmacopsychiatry. 1996;29:12–22. doi: 10.1055/s-2007-979536. [DOI] [PubMed] [Google Scholar]
- Pariante CM. Risk factors for development of depression and psychosis. Glucocorticoid receptors and pituitary implications for treatment with antidepressant and glucocorticoids. Ann NY Acad Sci. 2009;1179:144–152. doi: 10.1111/j.1749-6632.2009.04978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EB. Psychotic depression—beyond the antidepressant/antipsychotic combination. Curr Psychiatry Rep. 2012;14:619–623. doi: 10.1007/s11920-012-0315-6. [DOI] [PubMed] [Google Scholar]
- Liu J, Bisschop PH, Eggels L, Foppen E, Fliers E, Zhou JN, et al. Intrahypothalamic estradiol modulates hypothalamus-pituitary-adrenal-axis activity in female rats. Endocrinology. 2012;153:3337–3344. doi: 10.1210/en.2011-2176. [DOI] [PubMed] [Google Scholar]
- Shen H, Luo Y, Kuo CC, Deng X, Chang CF, Harvey BK, et al. 9-Cis-retinoic acid reduces ischemic brain injury in rodents via bone morphogenetic protein. J Neurosci Res. 2009;87:545–555. doi: 10.1002/jnr.21865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Acker SA, Fluttert MF, Sibug RM, De Kloet ER. Intracerebroventricular administration of a glucocorticoid receptor antagonist enhances the cardiovascular responses to brief restraint stress. Eur J Pharmacol. 2001;430:87–91. doi: 10.1016/s0014-2999(01)01341-3. [DOI] [PubMed] [Google Scholar]
- Zhu H, Huang Q, Xu H, Niu L, Zhou JN. Antidepressant-like effects of sodium butyrate in combination with estrogen in rat forced swimming test: involvement of 5-HT(1A) receptors. Behav Brain Res. 2009;196:200–206. doi: 10.1016/j.bbr.2008.08.039. [DOI] [PubMed] [Google Scholar]
- Andrews MH, Wood SA, Windle RJ, Lightman SL, Ingram CD. Acute glucocorticoid administration rapidly suppresses basal and stress-induced hypothalamo-pituitary-adrenal axis activity. Endocrinology. 2012;153:200–211. doi: 10.1210/en.2011-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loas G. Vulnerability to depression: a model centered on anhedonia. J Affect Disord. 1996;41:39–53. doi: 10.1016/0165-0327(96)00065-1. [DOI] [PubMed] [Google Scholar]
- Pellow S, Chopin P, File SE, Briley M. Validation of open:closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J Neurosci Methods. 1985;14:149–167. doi: 10.1016/0165-0270(85)90031-7. [DOI] [PubMed] [Google Scholar]
- Walf AA, Frye CA. The use of the elevated plus maze as an assay of anxiety-related behavior in rodents. Nat Protoc. 2007;2:322–328. doi: 10.1038/nprot.2007.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Hu P, Qi XR, Meng FT, Kalsbeek A, Zhou JN. Acute restraint stress increases intrahypothalamic oestradiol concentrations in conjunction with increased hypothalamic oestrogen receptor beta and aromatase mRNA expression in female rats. J Neuroendocrinol. 2011;23:435–443. doi: 10.1111/j.1365-2826.2011.02123.x. [DOI] [PubMed] [Google Scholar]
- Hu P, Oomen C, van Dam AM, Wester J, Zhou JN, Joels M, et al. A single-day treatment with mifepristone is sufficient to normalize chronic glucocorticoid induced suppression of hippocampal cell proliferation. PLoS One. 2012;7:e46224. doi: 10.1371/journal.pone.0046224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao AM, Hestiantoro A, Van Someren EJ, Swaab DF, Zhou JN. Colocalization of corticotropin-releasing hormone and oestrogen receptor-alpha in the paraventricular nucleus of the hypothalamus in mood disorders. Brain. 2005;128:1301–1313. doi: 10.1093/brain/awh448. [DOI] [PubMed] [Google Scholar]
- Stephanou A, Melino G, Knight RA, Annicchiarico-Petruzzelli M, Sarlis NJ, Finazzi-Agro A, et al. Interleukin-6 and corticotrophin-releasing hormone mRNA are modulated during differentiation of human neuroblastoma cells. Neuropeptides. 1992;23:45–49. doi: 10.1016/0143-4179(92)90009-l. [DOI] [PubMed] [Google Scholar]
- Yamamori E, Iwasaki Y, Taguchi T, Nishiyama M, Yoshida M, Asai M, et al. Molecular mechanisms for corticotropin-releasing hormone gene repression by glucocorticoid in BE(2)C neuronal cell line. Mol Cell Endocrinol. 2007;264:142–148. doi: 10.1016/j.mce.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Taniguchi Y, Iwasaki Y, Tsugita M, Nishiyama M, Taguchi T, Okazaki M, et al. Glucocorticoid receptor-beta and receptor-gamma exert dominant negative effect on gene repression but not on gene induction. Endocrinology. 2010;151:3204–3213. doi: 10.1210/en.2009-1254. [DOI] [PubMed] [Google Scholar]
- Meijer OC, Kalkhoven E, van der Laan S, Steenbergen PJ, Houtman SH, Dijkmans TF, et al. Steroid receptor coactivator-1 splice variants differentially affect corticosteroid receptor signaling. Endocrinology. 2005;146:1438–1448. doi: 10.1210/en.2004-0411. [DOI] [PubMed] [Google Scholar]
- van der Laan S, Lachize SB, Vreugdenhil E, de Kloet ER, Meijer OC. Nuclear receptor coregulators differentially modulate induction and glucocorticoid receptor-mediated repression of the corticotropin-releasing hormone gene. Endocrinology. 2008;149:725–732. doi: 10.1210/en.2007-1234. [DOI] [PubMed] [Google Scholar]
- Przybycien-Szymanska MM, Mott NN, Pak TR. Alcohol dysregulates corticotropin-releasing-hormone (CRH) promoter activity by interfering with the negative glucocorticoid response element (nGRE) PLoS One. 2011;6:e26647. doi: 10.1371/journal.pone.0026647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- Hazen PG, Carney JF, Walker AE, Stewart JJ. Depression--a side effect of 13-cis-retinoic acid therapy. J Am Acad Dermatol. 1983;9:278–279. doi: 10.1016/s0190-9622(83)80154-6. [DOI] [PubMed] [Google Scholar]
- Crandall J, Sakai Y, Zhang J, Koul O, Mineur Y, Crusio WE, et al. 13-cis-retinoic acid suppresses hippocampal cell division and hippocampal-dependent learning in mice. Proc Natl Acad Sci USA. 2004;101:5111–5116. doi: 10.1073/pnas.0306336101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman JP, Ostrander MM, Mueller NK, Figueiredo H. Limbic system mechanisms of stress regulation: hypothalamo-pituitary-adrenocortical axis. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:1201–1213. doi: 10.1016/j.pnpbp.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Kovacs KJ, Mezey E. Dexamethasone inhibits corticotropin-releasing factor gene expression in the rat paraventricular nucleus. Neuroendocrinology. 1987;46:365–368. doi: 10.1159/000124846. [DOI] [PubMed] [Google Scholar]
- Sawchenko PE. Evidence for a local site of action for glucocorticoids in inhibiting CRF and vasopressin expression in the paraventricular nucleus. Brain Res. 1987;403:213–223. doi: 10.1016/0006-8993(87)90058-8. [DOI] [PubMed] [Google Scholar]
- Di S, Malcher-Lopes R, Halmos KC, Tasker JG. Nongenomic glucocorticoid inhibition via endocannabinoid release in the hypothalamus: a fast feedback mechanism. J Neurosci. 2003;23:4850–4857. doi: 10.1523/JNEUROSCI.23-12-04850.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malkoski SP, Dorin RI. Composite glucocorticoid regulation at a functionally defined negative glucocorticoid response element of the human corticotropin-releasing hormone gene. Mol Endocrinol. 1999;13:1629–1644. doi: 10.1210/mend.13.10.0351. [DOI] [PubMed] [Google Scholar]
- Gutierrez-Mecinas M, Trollope AF, Collins A, Morfett H, Hesketh SA, Kersante F, et al. Long-lasting behavioral responses to stress involve a direct interaction of glucocorticoid receptors with ERK1/2-MSK1-Elk-1 signaling. Proc Natl Acad Sci USA. 2011;108:13806–13811. doi: 10.1073/pnas.1104383108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L, Holscher C, Anwyl R, Rowan MJ. Glucocorticoid receptor and protein/RNA synthesis-dependent mechanisms underlie the control of synaptic plasticity by stress. Proc Natl Acad Sci USA. 1998;95:3204–3208. doi: 10.1073/pnas.95.6.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi XR, Kamphuis W, Wang S, Wang Q, Lucassen PJ, Zhou JN, et al. Aberrant stress hormone receptor balance in the human prefrontal cortex and hypothalamic paraventricular nucleus of depressed patients. Psychoneuroendocrinology. 2013;38:863–870. doi: 10.1016/j.psyneuen.2012.09.014. [DOI] [PubMed] [Google Scholar]
- Pariante CM, Miller AH. Glucocorticoid receptors in major depression: relevance to pathophysiology and treatment. Biol Psychiatry. 2001;49:391–404. doi: 10.1016/s0006-3223(00)01088-x. [DOI] [PubMed] [Google Scholar]
- Jeanneteau FD, Lambert WM, Ismaili N, Bath KG, Lee FS, Garabedian MJ, et al. BDNF and glucocorticoids regulate corticotrophin-releasing hormone (CRH) homeostasis in the hypothalamus. Proc Natl Acad Sci USA. 2012;109:1305–1310. doi: 10.1073/pnas.1114122109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surjit M, Ganti KP, Mukherji A, Ye T, Hua G, Metzger D, et al. Widespread negative response elements mediate direct repression by agonist-liganded glucocorticoid receptor. Cell. 2011;145:224–241. doi: 10.1016/j.cell.2011.03.027. [DOI] [PubMed] [Google Scholar]
- Toth K, Sarang Z, Scholtz B, Brazda P, Ghyselinck N, Chambon P, et al. Retinoids enhance glucocorticoid-induced apoptosis of T cells by facilitating glucocorticoid receptor-mediated transcription. Cell Death Differ. 2011;18:783–792. doi: 10.1038/cdd.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang-Yen HF, Chambard JC, Sun YL, Smeal T, Schmidt TJ, Drouin J, et al. Transcriptional interference between c-Jun and the glucocorticoid receptor: mutual inhibition of DNA binding due to direct protein-protein interaction. Cell. 1990;62:1205–1215. doi: 10.1016/0092-8674(90)90396-v. [DOI] [PubMed] [Google Scholar]
- Belanoff JK, Flores BH, Kalezhan M, Sund B, Schatzberg AF. Rapid reversal of psychotic depression using mifepristone. J Clin Psychopharmacol. 2001;21:516–521. doi: 10.1097/00004714-200110000-00009. [DOI] [PubMed] [Google Scholar]
- Fleseriu M, Biller BM, Findling JW, Molitch ME, Schteingart DE, Gross C. Mifepristone, a glucocorticoid receptor antagonist, produces clinical and metabolic benefits in patients with Cushing's syndrome. J Clin Endocrinol Metab. 2012;97:2039–2049. doi: 10.1210/jc.2011-3350. [DOI] [PubMed] [Google Scholar]
- Blasey CM, Block TS, Belanoff JK, Roe RL. Efficacy and safety of mifepristone for the treatment of psychotic depression. J Clin Psychopharmacol. 2011;31:436–440. doi: 10.1097/JCP.0b013e3182239191. [DOI] [PubMed] [Google Scholar]
- Flores BH, Kenna H, Keller J, Solvason HB, Schatzberg AF. Clinical and biological effects of mifepristone treatment for psychotic depression. Neuropsychopharmacology. 2006;31:628–636. doi: 10.1038/sj.npp.1300884. [DOI] [PubMed] [Google Scholar]
- van der Lely AJ, Foeken K, van der Mast RC, Lamberts SW. Rapid reversal of acute psychosis in the Cushing syndrome with the cortisol-receptor antagonist mifepristone (RU 486) Ann Intern Med. 1991;114:143–144. doi: 10.7326/0003-4819-114-2-143. [DOI] [PubMed] [Google Scholar]
- Watson S, Gallagher P, Porter RJ, Smith MS, Herron LJ, Bulmer S, et al. A randomized trial to examine the effect of mifepristone on neuropsychological performance and mood in patients with bipolar depression. Biol Psychiatry. 2012;72:943–949. doi: 10.1016/j.biopsych.2012.05.029. [DOI] [PubMed] [Google Scholar]
- Oomen CA, Mayer JL, de Kloet ER, Joels M, Lucassen PJ. Brief treatment with the glucocorticoid receptor antagonist mifepristone normalizes the reduction in neurogenesis after chronic stress. Eur J Neurosci. 2007;26:3395–3401. doi: 10.1111/j.1460-9568.2007.05972.x. [DOI] [PubMed] [Google Scholar]
- Wulsin AC, Herman JP, Solomon MB. Mifepristone decreases depression-like behavior and modulates neuroendocrine and central hypothalamic-pituitary-adrenocortical axis responsiveness to stress. Psychoneuroendocrinology. 2010;35:1100–1112. doi: 10.1016/j.psyneuen.2010.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Haarst AD, Oitzl MS, de Kloet ER. Facilitation of feedback inhibition through blockade of glucocorticoid receptors in the hippocampus. Neurochem Res. 1997;22:1323–1328. doi: 10.1023/a:1022010904600. [DOI] [PubMed] [Google Scholar]
- Schulz M, Eggert M, Baniahmad A, Dostert A, Heinzel T, Renkawitz R. RU486-induced glucocorticoid receptor agonism is controlled by the receptor N terminus and by corepressor binding. J Biol Chem. 2002;277:26238–26243. doi: 10.1074/jbc.M203268200. [DOI] [PubMed] [Google Scholar]
- Rogatsky I, Hittelman AB, Pearce D, Garabedian MJ. Distinct glucocorticoid receptor transcriptional regulatory surfaces mediate the cytotoxic and cytostatic effects of glucocorticoids. Mol Cell Biol. 1999;19:5036–5049. doi: 10.1128/mcb.19.7.5036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandit S, Geissler W, Harris G, Sitlani A. Allosteric effects of dexamethasone and RU486 on glucocorticoid receptor-DNA interactions. J Biol Chem. 2002;277:1538–1543. doi: 10.1074/jbc.M105438200. [DOI] [PubMed] [Google Scholar]
- Nieman LK, Chrousos GP, Kellner C, Spitz IM, Nisula BC, Cutler GB, et al. Successful treatment of Cushing's syndrome with the glucocorticoid antagonist RU 486. J Clin Endocrinol Metab. 1985;61:536–540. doi: 10.1210/jcem-61-3-536. [DOI] [PubMed] [Google Scholar]
- Cadepond F, Ulmann A, Baulieu EE. RU486 (mifepristone): mechanisms of action and clinical uses. Annu Rev Med. 1997;48:129–156. doi: 10.1146/annurev.med.48.1.129. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.