Abstract
BACKGROUND
Perineal trauma after vaginal delivery can have significant long-term consequences. It is unknown if a larger infant head circumference (HC) or smaller maternal perineal anatomy are risk factors for perineal trauma after vaginal delivery.
METHODS
We conducted a prospective cohort study of low-risk nulliparous women. Data collected included maternal characteristics, antepartum POP-Q measurements of the perineal body and genital hiatus, labor characteristics, perineal trauma, and infant head circumference. Perineal trauma was defined as trauma that extended into the muscles of the perineum (second degree or deeper). Univariate and multivariate logistic models were created to calculate odd ratios (OR) and 95% confidence intervals (CI).
RESULTS
We observed 448 vaginal births. Multivariate analysis demonstrated a significant association between infant head circumference at birth and perineal trauma, OR 1.22 for each increase of 1cm in HC (95% CI 1.05-1.43). There was no association between perineal body or genital hiatus length and perineal trauma.
CONCLUSIONS
In nulliparous low-risk women a larger infant head circumference at birth increases the likelihood of perineal trauma, although the effect is modest. Antenatal perineal body and genital hiatus measurements do not predict perineal trauma. These results do not support alteration in mode of delivery or other obstetric practices.
Keywords: Perineal trauma, childbirth outcomes, perineal body, genital hiatus
Introduction
Perineal trauma following vaginal birth affects up to 85% (1) of women and is associated with increased postpartum pain (2), anal incontinence (3) and sexual dysfunction (4, 5). Previously identified risk factors for perineal trauma include race (6), parity, operative vaginal delivery (forceps greater than vacuum), episiotomy, and infant weight (7, 8). Occiput posterior position of the infant head at birth has also been identified as a risk factor for third and fourth-degree perineal trauma in nulliparous women and in women undergoing operative delivery (8, 9), findings that may be influenced by the larger presenting diameter of the fetal skull. Infant head circumference is often assumed by providers and patients to be a causal factor in perineal trauma, however, supportive data are limited, and the dynamics of the birth process, including infant head molding and intrinsic tissue properties, are complex (10,11). The Childbirth and Pelvic Symptoms Study (CAPS) found that larger infant head circumference was associated with severe perineal trauma, although this was not a primary outcome of interest in the study and was not further investigated in the final multivariate analysis (12). A large infant HC was associated with increased risk of levator muscle injury among women who underwent postpartum ultrasound (US) and this risk was increased further when combined with a prolonged second stage (13). However this finding was not reproduced in a second prospective study of endoanal US performed on postpartum day one, which had a high episiotomy rate (14). Additional research has linked a large infant HC to a longer second stage (15, 16).
While the association between fetal head circumference and perineal trauma has been explored, little is known about the association between maternal perineal anatomy measurements and lacerations following vaginal birth. A short perineal body (PB) has been suggested to lead to a greater risk of severe third and fourth-degree perineal trauma, but past studies were confounded by high episiotomy rates (17, 18).
The primary aim of our study was to determine if a larger infant head circumference as measured shortly after birth increased the degree of perineal trauma in low-risk nulliparous women. The secondary aim was to determine if a shorter pre-partum maternal perineal body or genital hiatus increased the risk of perineal trauma.
Methods
We conducted a secondary analysis of a prospective cohort of nulliparous women recruited in pregnancy and followed through the second postpartum year designed to describe postpartum pelvic floor changes among primiparous women. The recruitment period was from 2006-2011 with a set target recruitment number of 630 women. The sample size was established based on power calculations for the primary analysis, focusing on longer-term postpartum pelvic floor changes. The University Research Review Committee approved the study, and all women gave written informed consent. Participating women had prenatal care provided by the nurse midwifery service, were low-risk, and recruited antenatal. Eligibility criteria were age ≥ 18 years of age, ability to read either English or Spanish, singleton gestation, absence of serious medical problems, gestational age of >/= 36 weeks at delivery, and no late second trimester pregnancy losses. Midwifery patients who transferred to the Obstetrics and Gynecology service intrapartum were included in this analysis, as the OBGYN service performed all operative vaginal and cesarean deliveries. Women who delivered prior to 35 weeks estimated gestational age or who were no longer eligible for nurse midwifery care prior to admission to labor and delivery were excluded from these analyses.
On enrollment midwives collected antepartum, demographic data (age, education, body mass index, and race), and completed the validated Pelvic Organ Prolapse Quantification (POPQ) exam (19), which includes perineal body (PB) and genital hiatus (GH) measurements. Midwives were formally trained in the performance of POPQ examinations on live models at the start of the study; a subset of women underwent POPQ exam with a second observer to evaluate inter rater reliability between midwives. Intrapartum labor and delivery characteristics were recorded, as well as the maternal weight gain and tobacco use during pregnancy. Oxytocin administration included women undergoing labor augmentation and labor induction. The active portion of the second stage of labor was defined as the actual time spent pushing after reaching complete cervical dilation. The customary method of delivery in this population is hands on for perineal protection, but this was not standardized or recorded as a variable in this study. Infant head circumference at birth was recorded by measurement to the nearest 0.5cm in the newborn nursery shortly after birth by nursery personnel (registered nurses or health technicians) who were not aware of the type or degree of maternal trauma.
The attendant midwife recorded all genital tract trauma immediately following the birth on standardized forms. Genital tract trauma was described according to location of lacerations and tissue layers involved. Severity of trauma was categorized for perineal lacerations into first, second, third and fourth-degree lacerations, depending on tissue layers involved. First-degree lacerations involved only the vaginal mucosa or perineal skin. Second-degree lacerations involved the muscles of the perineal body without involvement of the anal sphincter complex. Third-degree lacerations included any laceration of the external anal sphincter, and fourth-degree lacerations included laceration of the rectal mucosa. Women without any trauma were described as intact. Trauma was dichotomized into perineal trauma: the presence of perineal trauma disrupting the muscles of the perineum (second, third or fourth-degree lacerations) compared to intact/minor trauma: women who were intact or had only first-degree perineal or non-perineal trauma. For most lacerations greater than or equal to second-degree laceration, a second observer assessed the perineum to assess inter rater reliability of trauma. Our midwifery group has previously reported a high inter-rater reliability in the determination of the degree of trauma (20).
Statistical analysis was carried out with SAS. Univariate associations with perineal trauma were assessed using Fisher’s exact test for categorical variables and the non-parametric Wilcoxon test for continuous variables. Multivariate logistic regression analysis was used to estimate adjusted odds ratios (OR) with perineal trauma and 95% confidence intervals (CI). Spearman correlation analysis was used to aid in determining collinearity between potential effects in the logistic models. Backward elimination was used to build a multivariate model to evaluate associations with perineal trauma, including variables that were individually associated with perineal trauma. A 5% threshold for statistical significance was used. The same model was obtained using stepwise selection with the same threshold. The c-statistic for assessing prediction adequacy of the logistic regression was c=0.71(21).
Results
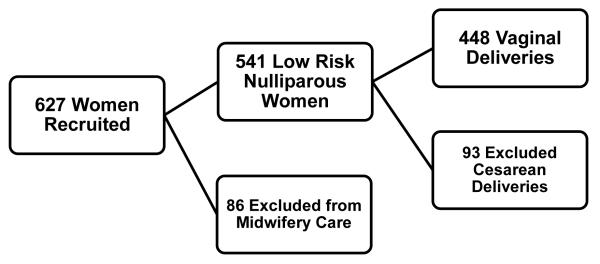
Of 627 women recruited, 541 were eligible for inclusion as the remaining women left midwifery care secondary to early pregnancy loss, relocation, insurance changes or medical complications of pregnancy. Ninety-three women delivered by cesarean section, and the remaining 448 women who delivered vaginally were analyzed in this study (See Figure 1). Few women underwent operative vaginal delivery (25 vacuum deliveries and 1 forceps delivery) representing a combined 5.8% of deliveries. Only 8 (2%) women received episiotomies. One episiotomy was with an operative delivery, and the remaining seven were with spontaneous vaginal deliveries. There were 429 deliveries with the fetus in occiput anterior position and 19 deliveries with non- occiput anterior position (either occiput posterior or occiput transverse). There were 151 women with perineal trauma (129 second-degree perineal lacerations, 19 third-degree lacerations, and 3 fourth-degree lacerations) and 297 women who were intact or with minor trauma (210 and 87 women respectively, see Table 1). Of the women who sustained second- degree lacerations or greater (77/129), 60% had a second observer, all but one of whom agreed with the second-degree diagnosis. During the antepartum measurement of the perineal body and genital hiatus, 17 women underwent repeat exams for inter-rater reliability testing of the POPQ exam; agreement between examiners was high (82% complete agreement) for prolapse stage, and all POPQ points were within 1 cm of agreement for 82% of measures and perineal body measurements were within 0.5 cm for 82% of measures.
Figure 1.
Study Participants
This figure depicts a flow diagram of the number of study participants over the course of the study.
Table 1.
Perineal Trauma
| Total N=448 | n (%) |
|---|---|
| Intact or other trauma | 297 (66.3) |
| Intact | 210 (46.88) |
| First-degree laceration or Non-perineal laceration |
87 (19.42) |
| Perineal trauma | 151 (33.7) |
| Second-degree laceration | 129 (28.79) |
| Third-degree laceration | 19 (4.24) |
| Fourth-degree laceration | 3 (0.67) |
Women who sustained perineal trauma were slightly older, more educated and more likely to be non-Hispanic white (see Table 2). In univariate analyses (see Table 3) perineal trauma was associated with a larger infant HC, infant length, and infant weight (all p<0.05). Perineal trauma was also associated in univariate analyses with total length of the second stage of labor, time of active second stage of labor, delivery of the head with contraction, compound presentation, occiput posterior or occiput transverse position, and operative vaginal delivery (all p< 0.05; see Table 3). The maternal characteristics of PB length and GH length were not significantly associated with perineal trauma (see Table 2). Additional grouping compared women within the lower quartile of PB length and the upper quartile of infant HC to women within the upper quartile of PB length and the lower quartile of infant HC; again no association was identified with perineal trauma (p=0.48). As this was a secondary analysis a power calculation was not done for the perineal measurements, however a future study with the same sample size and a probability of perineal trauma as estimated in this study would have 80% power to detect an odds ratio between perineal trauma and PB length of 1.55 for each increase of 1cm in PB length, using a two-sided test in a logistic regression model.
Table 2.
Comparison of Maternal Demographic Information Based on Degree of Trauma
| Total N=448 | Intact/Minor Trauma, n= 297 |
Perineal Trauma, n=151 |
p-value |
|---|---|---|---|
| Age (years), n=448 | 23.0 (±4.4)* | 25.7 (±5.3) | <0.001 |
| Years of education, n=436 | 13.3 (±2.4) | 14.9 (±2.7) | <0.001 |
| BMI, n=445 | 24.6 (±5.6) | 24.8 (±4.8) | 0.35 |
| Weight gain (lbs.), n=447 | 35.5 (±13.1) | 35.5 (±14.8) | 0.84 |
| Race, n=448 | 0.001 | ||
| Non-Hispanic White | 112 (37.71) | 81 (53.64) | |
| Hispanic | 150 (50.51) | 51 (33.77) | |
| Asian | 4 (1.35) | 6 (3.97) | |
| Black | 15 (5.05) | 3 (1.99) | |
| Native American | 16 (5.39) | 10 (6.62) | |
| Tobacco use (%), n=448 | 19 (6.4) | 11 (7.3) | 0.74 |
BMI: body mass index.
Data are mean (± standard deviation) or n (%)
Table 3.
Univariate Analysis for Risk of Perineal Trauma
| Total N=448 | Intact/Minor Trauma, n= 297 |
Perineal Trauma, n=151 |
p-value |
|---|---|---|---|
|
Maternal/Infant Measurements
|
|||
| Infant HC (cm), n=429 | 33.8 (±1.5) * | 34.3 (±1.4) | <0.001 |
| Infant length (cm), n=428 | 50.0 (±3.13) | 50.8 (±3.3) | <0.001 |
| Infant weight (gm), n=448 | 3171.1 (±437.7) | 3304.1 (±384.6) | <0.01 |
| PB length (cm), n=445 | 3.6 (±0.8) | 3.7 (±0.8) | 0.35 |
| GH length (cm), n=445 | 2.7 (±0.8) | 2.6 (±0.8) | 0.31 |
|
Labor and Delivery Variables
|
|||
| Oxytocin augmentation, n=443 | 133 (45.2) | 79 (53.0) | 0.12 |
| Epidural use, n=447 | 181 (60.9) | 88 (58.7) | 0.64 |
| Total time 2 nd stage (mins), n= 429 | 82.2 (±79.9) | 115.5 (±101.9) | <0.001 |
| Time active 2 nd stage (mins), n=433 | 60.6 (±48.8) | 94.8 (±81.4) | <0.001 |
| Delivery with push, n= 389 | 104 (40.3) | 66 (49.6) | 0.08 |
| Delivery with contraction, n=403 | 168 (63.2) | 102 (74.5) | 0.02 |
| Fetal bradycardia at delivery, n=442 | 34 (11.6) | 14 (9.4) | 0.6 |
| Compound presentation, n=439 | 23 (7.9) | 24 (16.2) | 0.01 |
| OP or OT position, n=448 | 5 (1.7) | 14 (9.3) | 0.02 |
| Operative vaginal delivery, n=447 | 12 (4) | 14 (9.3) | 0.03 |
n: number with data present for that particular variable; HC: head circumference; AC: abdominal circumference; PB: perineal body; GH: genital hiatus; OP: occiput posterior; OT: occiput transverse
Data are mean (± standard deviation) or n (%)
Spearman correlation analysis showed that total second stage length and length of active second stage were strongly positively correlated (0.87, p <0.001), as was maternal age and education level (0.74, p <0.001). Education and total second stage length were not considered in multivariate risk models given their strong correlations with age and length of active second stage, respectively. Statistically significant positive correlation was also found between infant HC and newborn weight (0.57, p < 0.001).
Backward elimination was used to build a multivariate model to predict perineal trauma. The initial model included the variables measured at time of delivery or at baseline that were individually associated with perineal trauma, excluding the total time of the second stage of labor and education (see Tables 2 and 3). The final model included age, HC, compound presentation and time in active second stage as risk factors (see Table 4). Based on the selected model, the odds of perineal trauma increases by 1.22 (95% CI 1.05-1.43) for each increase of 1cm in HC and by 1.38 (95% CI 1.08-1.72) for each 1 hour increase in time of active second stage. Similarly, having a compound presentation increases the odds of perineal trauma by 2.40 (95% CI 1.14-4.66) whereas the odds increases by 1.10 (95% CI 1.05-1.16) for each 1 year increase in mother’s age.
Table 4.
Multivariate Analysis with Perineal Trauma versus Intact/other Trauma as the Outcome*
| Exposure | Adjusted OR | 95% CI | p-value |
|---|---|---|---|
| Age (years) | 1.10 | 1.05-1.16 | <0.001 |
| Infant HC (cm) | 1.22 | 1.05-1.43 | 0.01 |
| Compound Presentation | 2.40 | 1.14-4.66 | 0.02 |
| Time of Active Second Stage (Hours) | 1.38 | 1.08-1.72 | 0.01 |
OR: odds ratio; CI: confidence interval; HC: head circumference
Factors entered into the regression model: age, race, infant HC, infant length, infant weight, compound presentation, total length of the second stage of labor, delivery of the head with contraction, occiput posterior or occiput transverse position, and operative vaginal delivery.
A final univariate analysis was performed with trauma dichotomized into third or fourth-degree lacerations compared to intact or first/second degree trauma. Neither infant HC nor maternal perineal measurements were significantly associated (p-value >0.05) with third or fourth degree lacerations, but the study did not have adequate power to address this question given the low number of third and fourth-degree lacerations.
Discussion
Affirming the belief of many women, physicians and midwives, our study demonstrated that the larger an infant’s head circumference at birth, the greater the likelihood of perineal trauma at vaginal delivery in nulliparous women, although the effect is modest. In contradiction to other studies, we found that antenatal perineal measurements did not predict presence of trauma. Our data do not support an association between small maternal perineal body nor small genital hiatus length and increased rates of perineal trauma. Even when comparing dyad subsets with large infant head circumference and short perineal body to those with a small infant head circumference and large perineal body, we could not demonstrate an ability to predict perineal trauma. Others have suggested that a short perineal body length and small genital hiatus were associated with increased rates of perineal trauma; however, in these prior studies, 65-76% of women underwent episiotomy (17, 18).
In this study, age and race remain significant predictors of major perineal trauma suggesting that intrinsic tissue properties or intrapartum variables rather than maternal size may explain the occurrence of perineal trauma. Our study population represents a diverse low risk group of women with a low episiotomy rate, but it does not address what the ideal episiotomy rate would be. Although both non-occiput anterior position and operative delivery were significant in the univariate analysis, neither met the threshold for significance in the multivariate model. This may be in part to the low numbers in both of these categories and to the fact that the operative deliveries were mostly vacuum deliveries (with the exception of a single forceps delivery).
Strengths of our study include prospective data collection, a large sample size, and low episiotomy and operative delivery rates. In addition, we included only low risk healthy women, who are representative of the majority of women who give birth in the US. One limitation is that postpartum infant head size is influenced in part by the bony maternal pelvis and clinical or radiologic maternal pelvimetry was not performed. As these maternal measures are unlikely to be widely adopted, we feel that clinical measurements are more representative of what clinicians can do in practice. Induction of labor has been identified both as a risk factor and a protective factor for perineal trauma (22, 23), and although we do not distinguish between labor augmentation and labor induction, we do include oxytocin administration in our analysis. While representative of low risk obstetric practice, the low numbers of third and fourth degree lacerations limit the power to detect whether a significant association exists between third and fourth degree lacerations and infant HC or maternal perineal measurements.
Although we have demonstrated a significant association between infant head circumference and perineal trauma, the effect is modest. Our study does not support increased concern for perineal trauma or alteration in mode of delivery or other obstetric practices due to a short perineal body, genital hiatus length or increased infant head circumference.
Acknowledgments
The author Rogers R.G. reports being a member of the American Urogynecologic Society executive committee and receiving not-for-profit grant support from Pfizer, whose medications are not the subject of this analysis.
Supported by the NICHD 1R01HD049819-01A2, the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health through Grant Number 8UL1TR000041.
Footnotes
DISCLOSURE: The authors Komorowski L., LeemanL., Fullilove A.,BedrickE., and Migliaccio L. report no conflict of interest.
References
- 1).McCandlish R, Bowler U, Van Asten H, Berridge G, Winter C, Sames L. A randomized controlled trial of care of the perineum during second stage of normal labor. British Journal of Obstetrics & Gynaecology. 1998;105:1262–1272. doi: 10.1111/j.1471-0528.1998.tb10004.x. [DOI] [PubMed] [Google Scholar]
- 2).Leeman L, Fullilove A, Borders N, et al. Postpartum perineal pain in a low episiotomy setting: association with severity of genital trauma, labor care, and birth variables. Birth. 2009 Dec;36.4:283–8. doi: 10.1111/j.1523-536X.2009.00355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Borello-France D, Burgio KL, Richter HE, et al. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006 Oct;108(4):863–72. doi: 10.1097/01.AOG.0000232504.32589.3b. [DOI] [PubMed] [Google Scholar]
- 4).Rathfisch G, Dikencik BK, Kizilkaya Beji N, et al. Effects of perineal trauma on postpartum sexual function. J Adv Nurs. 2010 Dec;66(12):2640–9. doi: 10.1111/j.1365-2648.2010.05428.x. [DOI] [PubMed] [Google Scholar]
- 5).Rogers RG, Borders N, Leeman LM, et al. Does spontaneous genital tract trauma impact postpartum sexual function? J Midwifery Womens Health. 2009 Mar-Apr;54(2):98–103. doi: 10.1016/j.jmwh.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Goldberg J, Hyslop T, Tolosa JE, et al. Racial differences in severe perineal lacerations after vaginal delivery. Am J Obstet Gynecol. 2003 Apr;188(4):1063–7. doi: 10.1067/mob.2003.251. [DOI] [PubMed] [Google Scholar]
- 7).Landy H, Laughon S, Bailit J, et al. Characteristics associated with severe perineal and cervical lacerations during vaginal delivery. Obstet Gynecol. 2011 Mar;117(3):627–35. doi: 10.1097/AOG.0b013e31820afaf2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Groutz A, Hasson J, Wengier A, et al. Third-and fourth- degree perineal tears: prevalence and risk factors in the third millennium. Am J Obstet Gynecol. 2011 Apr;204(4):47.e1–4. doi: 10.1016/j.ajog.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 9).Bradley M, Kaminski R, Streitman D, Dunn S, Krans E. Effect of rotation on perineal lacerations in forceps-assisted vaginal deliveries. Obstet Gynecol. 2013 Jul;122(1):132–7. doi: 10.1097/AOG.0b013e31829752fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Sorbe B, Dahlgren S. Some important factors in the molding of the fetal head during vaginal delivery- a photographic study. Int J Gynaecol Obstet. 1983 Jun;21(3):205–12. doi: 10.1016/0020-7292(83)90081-4. [DOI] [PubMed] [Google Scholar]
- 11).Souza S, Ross J, Milner R. Alterations in head shape of newborn infants after caesarean section or vaginal delivery. Arch Dis Child. 1976 Aug;51(8):624–7. doi: 10.1136/adc.51.8.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).FitzGerald M, Weber A, Howden N, Cundiff G, Brown M. Risk factor for anal sphincter tear during vaginal delivery. Obstet Gynecol. 2007 Jan;109(1):29–34. doi: 10.1097/01.AOG.0000242616.56617.ff. [DOI] [PubMed] [Google Scholar]
- 13).Valsky D, Lipschuetz M, Bord A, et al. Fetal head circumference and length of second stage of labor are risk factors for levator ani muscle injury, diagnosed by 3-dimensional transperineal ultrasound in primiparous women. Am J Obstet Gynecol. 2009 Jul;201(1):91.e1–7. doi: 10.1016/j.ajog.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 14).Sudol-Szopinnska I, Radkiewicz J, Szopinski T, et al. Postpartum endoanal ultrasound finding in primiparous women after vaginal delivery. Acta Radiol. 2010 Sep;51(7):819–24. doi: 10.3109/02841851.2010.491090. [DOI] [PubMed] [Google Scholar]
- 15).Evander C, Högber U, Ekéus The influence of fetal head circumference on labor outcome: a population-based register study. Acta Obstet Gynecol Scand. 2012;91:470–475. doi: 10.1111/j.1600-0412.2012.01358.x. [DOI] [PubMed] [Google Scholar]
- 16).Kennelly M, Anjum R, Lyons S, Burke G. Postpartum fetal head circumference and its influence on labor duration in nullipara. J Obstet Gynaecol. 2003 Sep;23(5):469–9. doi: 10.1080/0144361031000153701. [DOI] [PubMed] [Google Scholar]
- 17).Deering SH, Carlson N, Stitely M, et al. Perineal body length and lacerations at delivery. J Reprod Med. 2004 Apr;49(4):306–10. [PubMed] [Google Scholar]
- 18).Rizk DE, Thomas L. Relationship between the length of the perineum and position of the anus and vaginal delivery in primigravidae. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11(2):79–83. doi: 10.1007/s001920050074. [DOI] [PubMed] [Google Scholar]
- 19).Hall A, Theofrastous J, Cundiff G, Harris R, et al. Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol. 1996;175:1467–71. doi: 10.1016/s0002-9378(96)70091-1. [DOI] [PubMed] [Google Scholar]
- 20).Albers L, Sedler K, Bedrick E, Teaf D, Peralta P. Midwifery care measures in the second stage of labor and reduction of genital tract trauma at birth: a randomized trial. J Midwifery Womens Health. 2005 Sep-Oct;50(5):365–72. doi: 10.1016/j.jmwh.2005.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21).Austin P, Steverber E. Interpreting the concordance statistic of a logistic regression model: relation to the variance and odds ratio of a continuous explanatory variable. BCM Med Res Methodol. 2012 Jun 20;12:82. doi: 10.1186/1471-2288-12-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Sheiner E, Levy A, Walfilsch A, Hallak M, Mazor M. Third degree perineal tears in a university medical center where midline episiotomties are not performed. Arch Gynecol Obstet. 2005 Apr;271(4):307–10. doi: 10.1007/s00404-004-0610-5. [DOI] [PubMed] [Google Scholar]
- 23).Eskandar O, Shet O. Risk factors for 3rd and 4th degree perineal tears. J Obstet Gynaecol. 2009 Feb;29(2):119–22. doi: 10.1080/01443610802665090. [DOI] [PubMed] [Google Scholar]