Abstract
Abnormal T cell activation and cell death underlie the pathology of systemic lupus erythematosus. Although mitochondrial hyperpolarization (MHP) represents an early and reversible checkpoint of T cell activation and apoptosis, lupus T cells exhibit persistent MHP. NO has recently been recognized as a key signal of mitochondrial biogenesis and mediator of MHP in human T lymphocytes. In this study, we show that persistent MHP was associated with increased mitochondrial mass (+47.7 ± 2.8%; p = 0.00017) and increased mitochondrial (+21.8 ± 4.1%; p = 0.016) and cytoplasmic Ca2+ content in T cells from 19 systemic lupus erythematosus patients with respect to 11 control donors (+38.0 ± 6.4%; p = 0.0023). Electron microscopy revealed that lupus lymphocytes contained 8.76 ± 1.0 mitochondria, while control donors contained 3.18 ± 0.28 mitochondria per cell (p = 0.0009). Increased mitochondrial mass in T cells was associated with 2.08 ± 0.09-fold enhanced NO production by lupus monocytes (p = 0.0023). Activation of T cells through the TCR initiates a biphasic elevation in cytosolic free Ca2+ concentration, a rapid initial peak observed within minutes, and a plateau phase lasting up to 48 h. In response to CD3/CD28 costimulation, rapid Ca2+ fluxing was enhanced while the plateau phase was diminished in lupus T cells. NO-induced mitochondrial biogenesis in normal T cells enhanced the rapid phase and reduced the plateau of Ca2+ influx upon CD3/CD28 costimulation, thus mimicking the Ca2+ signaling profile of lupus T cells. Mitochondria constitute major Ca2+ stores and NO-dependent mitochondrial biogenesis may account for altered Ca2+ handling by lupus T cells. The Journal of Immunology, 2004, 173: 3676–3683.
Systemic lupus erythematosus (SLE)3 is a chronic inflammatory disease characterized by T and B cell dysfunction and production of antinuclear Abs (1). Abnormal T cell activation and cell death underlie the pathology of SLE (2, 3). Potentially autoreactive T and B lymphocytes during development (4) and after completion of an immune response are removed by apoptosis (5). Paradoxically, lupus T cells exhibit both enhanced spontaneous apoptosis and defective activation-induced cell death. Increased spontaneous apoptosis of PBL has been linked to chronic lymphopenia (6) and compartmentalized release of nuclear autoantigens in patients with SLE (7). By contrast, defective CD3-mediated cell death may be responsible for persistence of autore-active cells (8). Unlike normal T cells, T lymphocytes of SLE patients exhibit persistent mitochondrial hyperpolarization (MHP), cytoplasmic alkalinization, increased reactive oxygen intermediate (ROI) production, and ATP depletion that mediate enhanced spontaneous and diminished activation-induced apoptosis and sensitize lupus T cells to necrosis (9). Apoptosis is a physiological process that results in nuclear condensation and breakup of the cell into membrane-enclosed apoptotic bodies suitable for phagocytosis by macrophages, thus preventing inflammation. By contrast, necrosis is a pathological process that results in cellular swelling, followed by lysis and release of proteases, oxidizing molecules, and other proinflammatory and chemotactic factors resulting in inflammation and tissue damage (10). Indeed, lymphocyte necrosis occurs in the bone marrow (11) and lymph nodes of lupus patients (12) and may significantly contribute to the inflammatory process (13).
Innate and adaptive immune responses resulting in activation, proliferation, or programmed cell death are dependent on controlled ROI production and ATP synthesis in mitochondria. In turn, synthesis of ATP during oxidative phosphorylation is driven by the mitochondrial transmembrane potential (Δψm, negative inside and positive outside) (14). Δψm is dependent upon the electron transport chain transferring electrons from NADH to molecular oxygen and proton transport mediated by the F0F1-ATPase complex. Disruption of Δψm has been proposed as the point of no return in apoptotic signaling that leads to caspase activation and disassembly of the cell (15). Interestingly, elevation of Δψm, or MHP and ROI production precede disruption of Δψm, activation of caspases, and phosphatidylserine (PS) externalization in Fas (16)-, TNF-α (17)-, and H2O2-induced apoptosis of Jurkat human leukemia T cells and normal human PBL (18). These observations were confirmed and extended to p53 (19), TNF-α (17), staurosporin (20), camptothecin (21), and NO-induced apoptosis (22). Elevation of Δψm or MHP is independent from activation of caspases and represents an early event in apoptosis (16, 19). MHP is also triggered by activation of the CD3-CD28 complex (9) or stimulation with Con A (16), IL-10, IL-3, IFN-γ, or TGF-β (23). Therefore, elevation of Δψm or MHP represents an early but reversible switch not exclusively associated with apoptosis. With Δψm hyperpolarization and extrusion of H+ ions from the mitochondrial matrix, the cytochromes within the electron transport chain become more reduced, which favors generation of ROI (24). Δψm and ROI levels as well as cytoplasmic pH are elevated in patients with SLE in comparison to healthy or rheumatoid arthritis controls (9, 23). Intracellular ATP concentration is a key switch in the cell’s decision to die via apoptosis or necrosis (25). T cell activation-induced MHP is associated with transient inhibition of F0F1-ATPase, ATP depletion, and sensitization to necrosis (9), suggesting that Δψm elevation is a critical checkpoint of T cell fate decisions. Persistent MHP and ATP depletion play key roles in abnormal T cell death, enhanced spontaneous and diminished activation- induced cell death, and predisposition for necrosis in patients with SLE (9).
NO is an intercellular and intracellular messenger (26) that has recently been recognized as a key signal of mitochondrial respiration (27) and biogenesis (28). NO, acting as a competitive antagonist, can cause a reversible inhibition of cytochrome c oxidase complex IV which may result in MHP (22) and ATP depletion (27). Recently, NO production was found to mediate CD3/CD28 costimulation-induced MHP and ROI production and sustained Ca2+ fluxing in human T lymphocytes (29). NO is highly diffusible and not restricted to its site of production (30). In the present study, we show that persistent MHP is associated with increased mitochondrial mass and Ca2+ content in T cells of patients with SLE. Activation of T cells through CD3/CD28 costimulation initiates a biphasic elevation in cytosolic free Ca2+ concentration: while rapid fluxing is enhanced, the plateau phase is diminished in lupus T cells. Monocytes of patients with SLE exhibit increased NO production. Pretreatment of normal human PBL with exogenous NO augmented Δψm, increased mitochondrial mass, and enhanced rapid Ca2+ fluxing while reducing sustained elevation of intracellular Ca2+ in response to CD3/CD28 costimulation, thus mimicking the Ca2+ profile of lupus T cells. The results suggest that increased NO production by monocytes may be responsible for MHP and altered Ca2+ signaling in T cells of patients with SLE.
Materials and Methods
Human subjects
Nineteen patients with SLE were investigated. All patients satisfied the criteria for a definitive diagnosis (31). Seventeen females (age, 41.3 ± 5.3 years; range, 19–65 years) and two males (age, 46.0 ± 10.2 years; range, 25–55 years) were studied. As controls, 11 age- and sex-matched healthy subjects were examined. Disease activity was assessed by the SLE Disease Activity Index (SLEDAI) score (32). Fourteen patients had a SLEDAI ≤ 5 and were considered relatively inactive. The remaining five patients with SLEDAI > 5 were considered active.
Cell culture and T cell activation
PBMC were isolated from heparinized venous blood on Ficoll-Hypaque gradient. PBL were separated from monocytes by adherence to autologous serum-coated petri dishes (33). PBL were resuspended at 106 cells/ml in RPMI 1640 medium supplemented with 10% FCS, 2 mM L-glutamine, 100 IU/ml penicillin, and 100 µg/ml gentamicin in 12-well plates at 37°C in a humidified atmosphere with 5% CO2. Cross-linking of the CD3 Ag was performed by addition of PBL to plates precoated with 1 µg/ml/well OKT3 mAb (CRL 8001 from American Type Culture Collection, Manassas, VA) for 1 h at 37°C. CD28 costimulation was performed by addition of 500 ng/ml mAb CD28.2 (BD Pharmingen, San Diego, CA). Rapid Ca2+ signaling was investigated after direct addition of OKT3 and CD28.2 Abs to PBL preloaded with Fluo-3 (see below).
Cell viability assays
Apoptosis was monitored by observing cell shrinkage, nuclear fragmentation, and quantified by flow cytometry after concurrent staining with fluorescein-conjugated annexin V (Annexin VFITC; R&D Systems, Minneapolis, MN; fluorescence channel 1 (FL-1)) and propidium iodide (FL-2) as earlier described (9). Staining with Cy5-conjugated annexin V (annexin V-Cy5; Biovision, Mountain View, CA) was used to monitor PS externalization (FL-3) in parallel with monitoring Δψm, ROI, NO, and Ca2+ levels as well as expression of surface Ags (see below). Specific combinations are described in each figure legend. Staining with annexin V alone or in combination with mitochondrial probes was conducted in 10mMHEPES (pH 7.4), 140mMNaCl, and 2.5mM CaCl2.
Flow cytometric analysis of Δψm and mitochondrial mass
Δψm was estimated by staining with 1 µM tetramethylrhodamine methyl ester (TMRM; excitation, 543 nm; emission, 567 nm recorded in FL-2) for 15 min at 37°C in the dark before flow cytometry (29). Δψm was also assessed by staining with 20 nm 3,3′-dihexyloxacarbocyanine iodide (DiOC6), a cationic lipophilic dye (16), for 15 min at 37°C in the dark before flow cytometry (excitation, 488 nm; emission, 525 nm recorded in FL-1). Fluorescence of DiOC6 is oxidation independent and correlates with Δψm (34). Δψm was also quantitated using a potential-dependent J-aggregate- forming lipophilic cation, 5,5′,6,6′-tetrachloro-1,1′,3,3′-tetraethylbenzimidazolocarbocyanine iodide (JC-1) (35). JC-1 selectively incorporates into mitochondria, where it forms monomers (fluorescence in green, 527 nm) or aggregates, at high transmembrane potentials (fluorescence in red, 590 nm) (35, 36). Cells were incubated with 0.5 µM JC-1 for 15 min at 37°C before flow cytometry. Δψm changes were also confirmed by staining with 1 µM CMXRos (excitation, 579 nm; emission, 599 nm recorded in FL-2). Cotreatment with a protonophore, 5 µM carbonyl cyanide m-chlorophenylhydrazone (Sigma-Aldrich, St. Louis, MO) for 15 min at 37°C resulted in decreased TMRM, DiOC6, JC-1, and CMXRos fluorescence and served as a positive control for disruption of Δψm (16). Since altered incorporation of potentiometric dyes may represent a change in mitochondrial mass, the latter was monitored by staining with potential insensitive mitochondrial dyes: 100 nM Mito Tracker Green-FM (excitation, 490 nm; emission, 516 nm recorded in FL-1) or 50 nM nonyl acridine orange (NAO, excitation, 490 nm; emission, 540 nm recorded in FL-1). All fluorescent probes were obtained from Molecular Probes (Eugene, OR).
Measurement of intracellular NO levels
Production of NO was assessed by using 4-amino-5-methylamino-2′,7′- difluorofluorescein diacetate (DAF-FM; Molecular Probes) or a NO sensor kit (BD Clontech, Palo Alto, CA). DAF-FM passively diffuses across cellular membranes, once inside cells it is deacetylated by intracellular esterases and caged in the cell. DAF-FM is essentially nonfluorescent until it reacts with NO to form a fluorescent benzotriazole. Measurement of NO was calibrated by incubating PBL with NO donors (Z)-1-[2-(2-aminoethyl)- N-(2-ammonioethyl)amino]diazen-1-ium-1,2-diolate diethylenetriamine (NOC-18; 200 µM to 1.8 mM) or sodium nitroprusside (400 µM to 10 mM). Following testing, 1–10 µM dye concentration during incubation times ranging from 10 min to 3 h, maximum NO sensitivity was achieved by loading cells with 1 µM DAF-FM for 2 h in 37°C. Excitation and emission maximum of DAF-FM are 495 and 515 nm, respectively.
Measurement of cytoplasmic and mitochondrial calcium level
Cytoplasmic calcium levels ([Ca2+]c) were assessed by loading the cells with 1 µM Fluo-3-acetoxymethyl ester (excitation, 506 nm; emission, 526 nm recorded in FL-1; Molecular Probes). After entering the cell, acetoxymethyl ester hydrolysis occurs and, thereafter, the dye is trapped in the cytosol. Fluo-3 elicits a large fluorescence intensity increase on binding calcium. To investigate early Ca2+ fluxing, cells were prelabeled by Fluo-3 and stimulated with OKT3 and anti-CD28 mAbs while Fluo-3 fluorescence of CD3+/annexinV− T cells was continuously recorded by flow cytometry. Ca2+ levels 4 and 24 h subsequent to CD3/CD28 costimulation were obtained by staining with Fluo-3 at termination of incubation, in parallel with staining with dyes monitoring Δψm, mitochondrial mass, NO production, PS externalization, and T cell Ag expression. Mitochondrial calcium levels ([Ca2+]m) were estimated by loading the cells with 4 µM Rhod2/acetoxymethyl ester which is compartmentalized into the mitochondria (37). Samples were analyzed using a BD Biosciences LSRII flow cytometer equipped with 20-mW argon (emission at 488 nm) and 16-mW heliumneon lasers (emission at 634 nm). Using four-color immunofluorescence, cytosolic and mitochondrial Ca2+ levels, Δψm, mitochondrial mass, NO production, and PS externalization within T cell subsets were concurrently analyzed by parallel staining with 1) Fluo-3, mitotracker green (MTG), NAO, DAF-FM, or DiOC6 (all FL-1); 2) Rhod-2 or TMRM (FL-2); 3) annexin V-Cy5 (FL-3); and 4) allophycocyanin-Cy7-conjugated mAb UCHT1 recognizing the CD3∈ chain or allophycocyanin-Cy7-conjugated anti-CD14 recognizing monocytes (FL-4; BD Pharmingen). Dead cells and debris were excluded from the analysis by electronic gating of forward and side scatter measurements. Each measurement was conducted on 10,000 cells. In each experiment, control and lupus cells were analyzed in parallel.
Electron microscopy
PBL (106) were pelleted at 1000 × g, fixed overnight with 2.5% glutaraldehyde in PBS, postfixed in 1% OsO4, dehydrated in a graded ethanol series, infiltrated with propylene oxide, and embedded in Araldite 502 epoxy resin. Ultrathin sections were stained with uranyl acetate and Reynold’s lead citrate before examination using a Tecnai BioTWIN 12 transmission electron microscope (FEI, Hillsboro, OR).
Statistics
Results were analyzed by Student’s t test or Mann-Whitney U rank sum test for nonparametric data. Correlation was measured using Pearson’s correlation coefficient. Changes were considered significant at p < 0.05.
Results
Coordinate changes in CD3/CD28 costimulation-induced MHP, NO production, and Ca2+ levels in lupus T cells
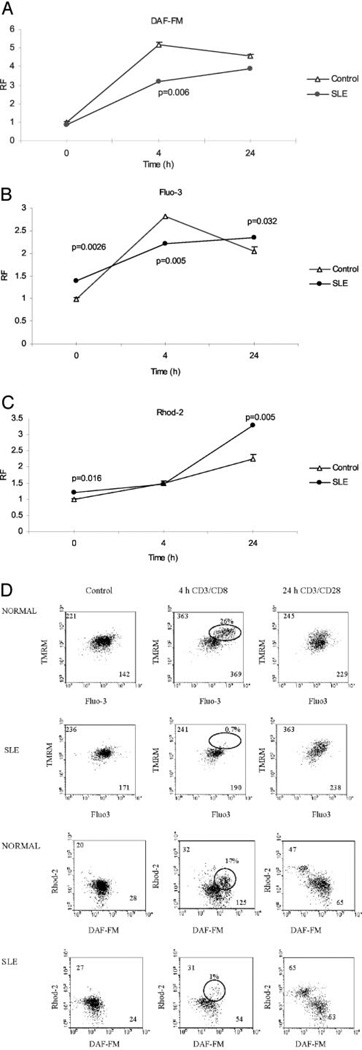
Activation of T cells through the TCR initiates a biphasic elevation in the cytosolic free Ca2+ concentration, a rapid initial peak observed within 5–10 min, and a plateau phase lasting 4 to 48 h (38). Mitochondria can take up, store, and release Ca2+, and the Δψm in combination with NO production plays a substantial role in shaping Ca2+ signals in many cell types (37, 39), including human T lymphocytes (29). CD3/CD28 costimulation-induced MHP of normal T cells depends on NO production (29). Therefore, we investigated the contribution of this signaling cascade to mitochondrial dysfunction in SLE. Results are expressed as relative fluorescence (RF) values with respect to those of unstimulated cells normalized at 1.0 (100%). Baseline NO levels, assessed by DAF-FM fluorescence, were similar in CD3+/annexinV− T cells of 19 lupus patients, as compared with T cells from 11 control donors (Fig. 1A). Unlike baseline NO production, [Ca2+]c were elevated by 38.0 ± 6.4% in lupus T cells (p = 0.0026; Fig. 1B). Baseline [Ca2+]m were also higher in lupus T cells by 21.8 ± 4.1% (p = 0.016; Fig. 1C). In response to CD3/CD28 costimulation for 4 h, NO production was enhanced 5.19 ± 1.15-fold in control T cells and 3.21 ± 0.08-fold, a significantly lesser extent (p < 0.0062), in lupus T cells. Although NO production declined in control cells, it continued to rise in lupus T cells by 24 h (Fig. 1A). Likewise, CD3/CD28 costimulation-induced elevations of sustained cytosolic (Fig. 1B) and [Ca2+]m were delayed in lupus T cells (Fig. 1C). Maximal [Ca2+]c elevation in control T cells, 2.81 ± 0.09-fold, occurred 4 h after CD3/CD28 stimulation, while T cell activation induced a more moderate rise, 1.59 ± 0.03-fold, in [Ca2+]c of lupus T cells (p < 0.0001; Fig. 1B). [Ca2+]m were markedly, 2.73 ± 0.09-fold (p = 0.005), enhanced in lupus T cells 24 h after CD3/CD28 costimulation (Fig. 1C). T cell activation resulted in the appearance of a CD3+/annexin V− cell population with MHP, elevated [Ca2+]c and [Ca2+]m, as well as detectable NO production 4 h after CD3/CD28 costimulation (Fig. 1D). Formation of such cell populations was abrogated in lupus T cells (Fig. 1D).
Figure 1.
Effect of CD3/CD28 costimulation on NO production and Ca2+ signaling in T cells from 11 control and 19 lupus donors. NO production was monitored by DAF-FM fluorescence (A) while [Ca2+]c and [Ca2+]m levels were assessed by Fluo-3 (B) and Rhod-2 fluorescence (C), respectively, in CD3+/annexin V− cells. D, Detection of CD3+/annexin V− cell population with elevated Δψm, [Ca2+]c, and [Ca2+]m as well as and NO production. Following CD3/CD28 costimulation, Δψm was measured by TMRM fluorescence (FL-2); [Ca2+]c and [Ca2+]m levels were assessed by Fluo-3 (FL-1) and Rhod-2 fluorescence (FL-2), while NO production was monitored by DAF-FM fluorescence (FL-1) gated on CD3+/annexin V− cells. Values in dot plots indicate mean channel FL-1 and FL-2 fluorescence, respectively. Results are expressed as RF values with respect to those of unstimulated cells normalized at 1.0 (100%). Data present mean ± SE. Error bars are occasionally covered by data symbols. Values of p reflect differences between 19 lupus and 11 control donors.
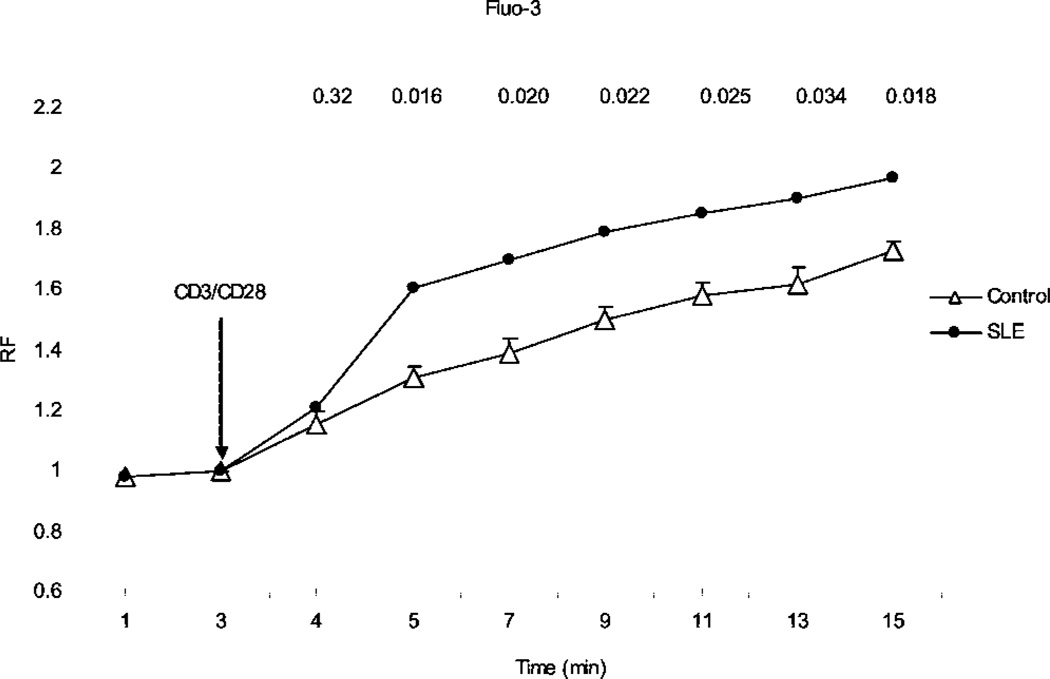
To investigate early Ca2+ fluxing, cells were prelabeled by Fluo-3 and stimulated with OKT3 and anti-CD28 mAbs while Fluo-3 fluorescence of CD3+/annexinV− T cells was continuously recorded by flow cytometry (Fig. 2). As early as 2 min after T cell activation, with respect to control T cells, a markedly enhanced Ca2+ signal was detected in lupus patients (p = 0.016). Increased [Ca2+]c in lupus T cells lasted up to 15 min following CD3/CD28 costimulation (p = 0.018). This initial surge in [Ca2+]c is due to the release of Ca2+ from intracellular stores, such as mitochondria (38, 39). Thus, increased baseline [Ca2+]m may be responsible for enhanced early Ca2+ fluxing in lupus T cells.
Figure 2.
Rapid Ca2+ fluxing in CD3/CD28 costimulated PBL from 19 lupus and 11 control donors. PBL were preloaded with Fluo-3 and stimulated with OKT3 and anti-CD28 mAbs while Fluo-3 fluorescence of CD3+/annexinV− T cells was continuously recorded by flow cytometry. Results are expressed as RF values with respect to those of unstimulated cells normalized at 1.0. Data present mean ± SE. Numbers over each time point indicate p values reflecting differences between lupus and control donors.
Persistent MHP is associated with increased mitochondrial mass in lupus T cells
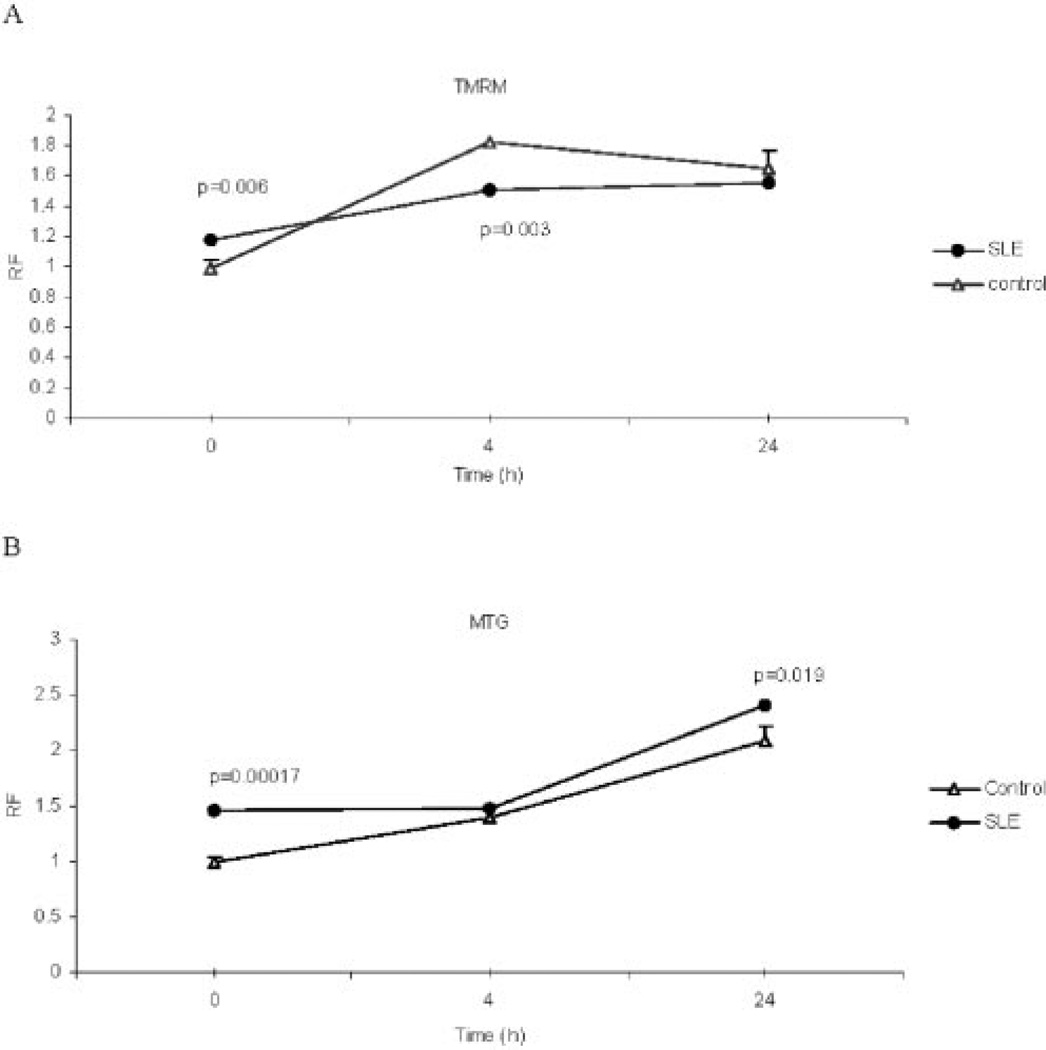
Mitochondria constitute major Ca2+ stores (40), thus increased mitochondrial mass may account for altered Ca2+ handling in lupus T cells. In addition to inducing MHP (22), NO was found to be a key signal of mitochondrial biogenesis (28). Therefore, persistent MHP may be related to increased mitochondrial mass in lupus T cells. In accordance with previous findings, baseline Δψm, as assessed by fluorescence of potentiometric dyes TMRM (Fig. 3A), DiOC6, or JC-1 (9, 23), was elevated in CD3+/annexinV− T cells from 19 patients with SLE, as compared to T cells from 11 control donors (+17.7 ± 6.7%; p = 0.006). To determine whether enhanced incorporation of potentiometric dyes may represent a change in mitochondrial mass, the latter was estimated by staining with potential insensitive mitochondrial dyes, MTG and NAO. In comparison to 11 healthy controls, MTG fluorescence was increased in CD3+/annexinV− T cells from 19 lupus patients by 47.7 ± 2.8% (p = 0.00017; Fig. 3B). NAO staining gave similar results (data not shown). The increase of mitochondrial mass exceeded the extent of Δψm elevation (p < 0.0001), suggesting that persistent MHP may represent enhanced mitochondrial biogenesis in lupus T cells.
Figure 3.
Assessment of Δψm (A) and mitochondrial mass (B) in lupus and control T cells. PBL from 11 healthy controls and 19 patients with SLE were stimulated with CD3/CD28 Abs for 4 and 24 h. Δψm was monitored by TMRM and mitochondrial mass was assessed by MTG fluorescence in CD3+/annexin V− cells. Results are expressed as RF values with respect to those of unstimulated cells normalized at 1.0. Data present mean ± SE. Values of p reflect differences between lupus and control donors.
In response to CD3/CD28 costimulation, Δψm was increased by 81.9 ± 4.2% at 4 h and 66.5 ± 1.8% at 24 h in control T cells (Fig. 3A). Mitochondrial mass was increased by 40.3 ± 3.5% at 4 h and by 109.0 ± 4.5% at 24 h, respectively, in control T cells (Fig. 3B). Thus, CD3/CD28 costimulation predominantly induced MHP at 4 h and increased mitochondrial mass at 24 h in normal T cells. In accordance with earlier findings (9, 23), Δψm was increased in lupus patients by a lesser extent, 50.0 ± 6.1% (p = 0.015) at 4 h and 55.2 ± 2.5% at 24 h (p < 0.0001). In lupus T cells, CD3/ CD28 costimulation-induced enlargement of mitochondrial mass was delayed and detected only at 24 h (Fig. 3B).
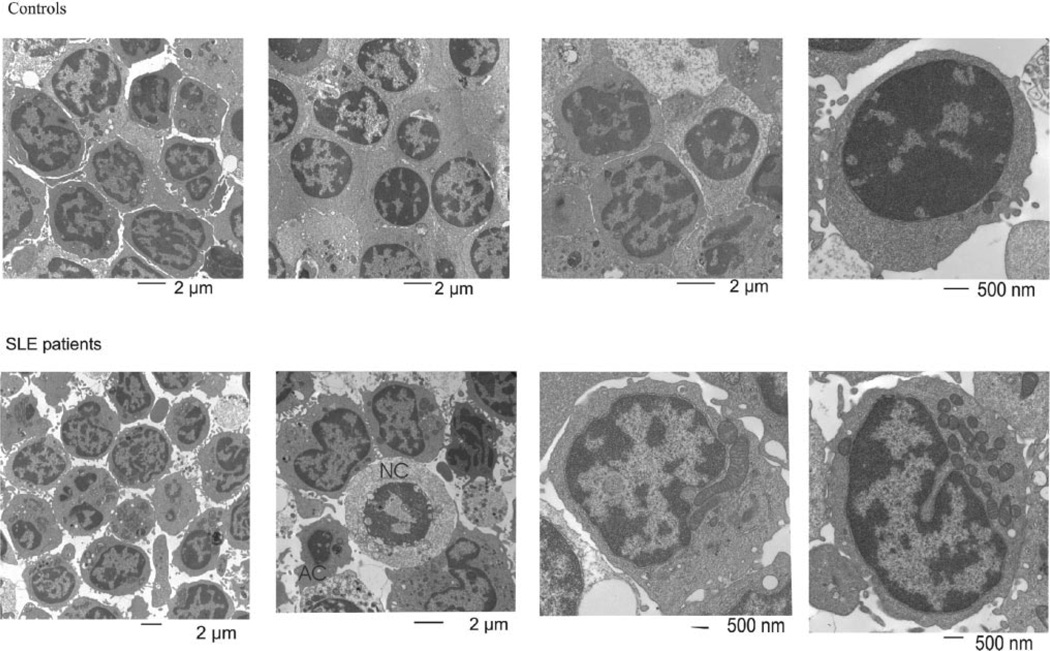
To investigate whether increased mitochondrial mass was associated with proliferation or larger size of mitochondria, PBL from five lupus and five healthy blood donors were examined by electron microscopy (Fig. 4). Monocyte-depleted PBL of control (91.8 ± 1.16%) and lupus donors had similar CD3+ T cell content (91.5 ± 1.03%). Based on analysis of 100 cells per donor, lupus patients contained 8.76 ± 1.0 mitochondria per cell, while healthy subjects contained 3.18 ± 0.28 mitochondria per cell (p = 0.0009). Additionally, lupus PBL harbored mitochondria that were severalfold enlarged, thus corresponding to stabilized megamitochondria (41) capable of storing increased amounts of Ca2+. Persistence of MHP ex vivo in tissue culture medium over 1 wk was consistent with structural changes, such as increased numbers and size of mitochondria in lupus PBL.
Figure 4.
Transmission electron microscopy of control and lupus PBL. Images represent analysis of 100 cells per donor from five healthy and five lupus subjects. Size scale is shown for each image. Green arrows show mitochondria of normal size, while red arrows indicate megamitochondria. Apoptotic cells (AC) with shrunken size and fragmented nuclei and necrotic cells (NC) with round-shaped swollen nuclei and cytoplasm lacking mitochondria are marked.
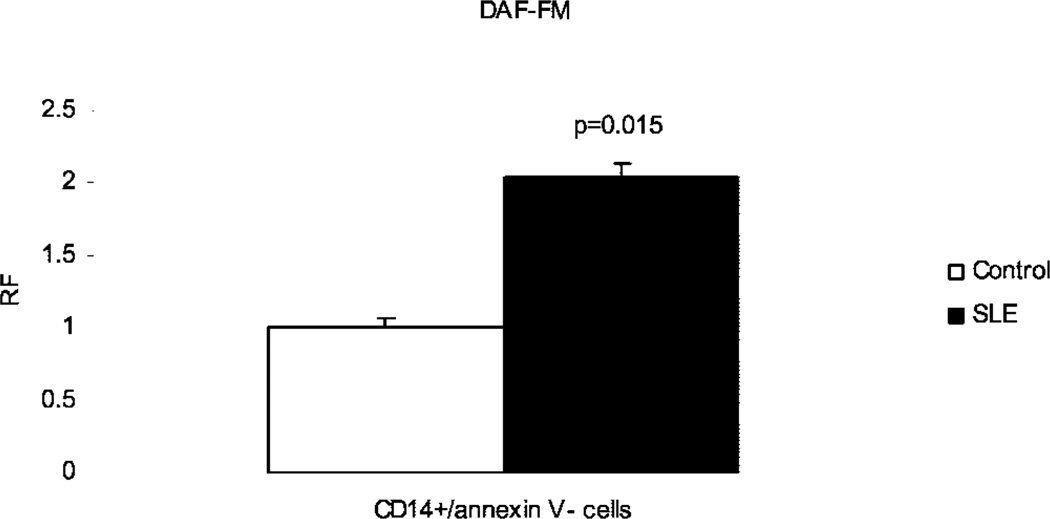
Increased NO production by monocytes from patients with SLE
NO has recently been recognized as a key signal triggering MHP (22) that can, in turn, lead to biogenesis and proliferation of mitochondria (28). Therefore, increased NO production may account for mitochondrial dysfunction in lupus T cells. However, baseline NO production was similar in annexin V−/CD3+ T cells from lupus and control donors (Fig. 1A). Since NO generated by one cell can regulate the respiration of adjacent cells, production of NO by mononuclear cell subsets was further investigated. Monocytes were enriched by adherence to plastic and identified by gating on CD14+ cells. In comparison to healthy controls, NO production by annexin V−/CD14+ monocytes was increased by 2.08 ± 0.09-fold (p = 0.015) in lupus patients (Fig. 5). No differences were seen in NO production between lupus and control donors in B cells and other CD14+ and CD3+ cells (data not shown).
Figure 5.
Assessment of NO production in control and lupus monocytes. NO production was monitored by DAF-FM fluorescence in CD14+/annexin V− cells. Data reflect mean ± SE of measurements in 10 healthy and 11 lupus donors.
To assess the influence of lupus monocytes on normal T cells, 106 monocyte-depleted PBL from four normal donors were incubated with 2 × 105 monocytes from four lupus or four control donors for 24 h at 37°C. Δψm was assessed by TMRM fluorescence, while [Ca2+]c was measured by Fluo-3 fluorescence gating on CD3-allophycocyanin-Cy7-positive/annexin V-Cy5-negative T cells in 16 cocultures, 8 with lupus and 8 with healthy monocytes. In comparison to control monocytes, lupus monocytes increased Δψm and [Ca2+]c in control T cells by 25.2% (p = 0.0012) and 37.4% (p = 0.0037), respectively. These results suggested that monocyte-derived factors, possibly NO, may contribute to mitochondrial dysfunction in lupus T cells.
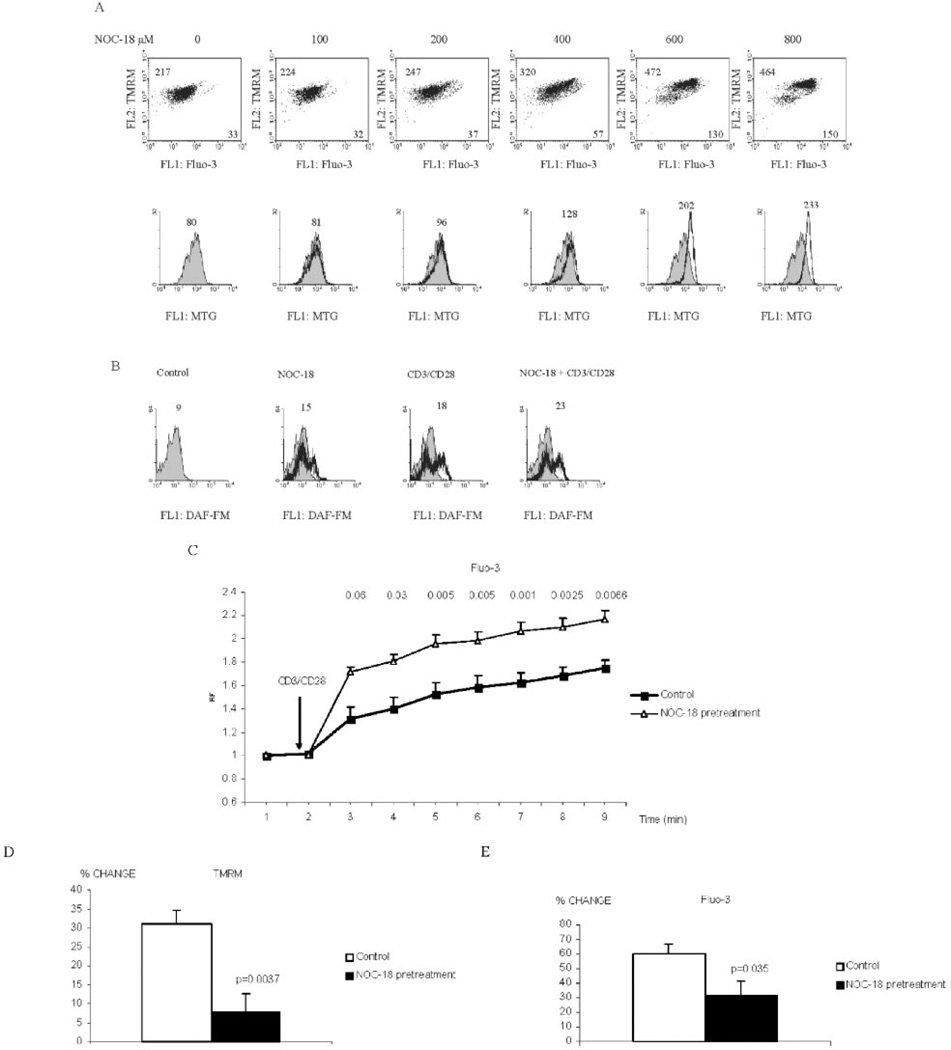
NO-induced mitochondrial biogenesis enhances the rapid phase and reduces the plateau of T cell activation-induced Ca2+ fluxing
NO was found to induce MHP and increase [Ca2+]c and [Ca2+]m levels in normal human T lymphocytes (29). Incubation of PBL with NOC-18, capable of slowly releasing NO, dose-dependently increased Δψm and Ca2+ levels as well as mitochondrial mass, as monitored by TMRM, Fluo-3, and MTG fluorescence, respectively (Fig. 6A). Pretreatment of PBL for 24 h with 600 µM NOC-18 increased MTG fluorescence by 2.24 ± 0.17-fold (p = 0.0009). To investigate whether NO-induced mitochondrial biogenesis may account for altered Ca2+ signaling in lupus T cells, monocytedepleted PBL from healthy donors were pretreated with NOC-18 for 24 h. After removal of NOC-18 by washing with medium three times, T cells were activated by CD3/CD28 costimulation and Δψm as well as intracellular Ca2+ levels were assessed by concurrent staining with TMRM and Fluo-3. Intracellular NO levels were monitored by DAF-FM staining (Fig. 6B). As shown in Fig. 6C, T cell activation-induced rapid Ca2+ fluxing was markedly enhanced by pretreatment with 200 µM NOC-18. As quickly as 2 min and lasting up to 9 min after T cell activation, a more robust rise of intracellular Ca2+ levels was noted in NOC-18-pretreated cells (p = 0.03–0.001). Such differences were observed up to 15 min following CD3/CD28 costimulation (data not shown). Alternatively, T cell activation-induced sustained elevations of Δψm (Fig. 6D) and Ca2+ levels were diminished in NOC-18-pretreated cells (Fig. 6E). NO pretreatment altered CD3/CD28 costimulation-induced Ca2+ signaling, thus mimicking the pattern observed in lupus T cells.
Figure 6.
Effect of NO pretreatment on CD3/CD28-induced Ca2+ fluxing. A, Dose-dependent induction by NO donor NOC-18 of MHP monitored by TMRM, elevation of [Ca2+]c monitored by Fluo-3, and mitochondrial mass assessed by MTG fluorescence. Values in dot plots (row 1) indicate mean channel FL-1 (Fluo-3) and FL-2 fluorescence (TMRM), respectively. Values over histograms (row 2) indicate mean channel of MTG fluorescence (FL-1). Histograms of NOC-18-treated cells (open curves) are overlayed on control cells (shaded curves). B, Monitoring of NO levels by DAF-FM fluorescence in cells exposed to 200 µM NOC-18 for 24 h and subsequent CD3/CD28 stimulation for 4 h. C, Effect of NO on rapid Ca2+ fluxing induced by CD3/CD28 costimulation. PBL were pretreated with 200 µM NOC-18 for 24 h, washed, preloaded with Fluo-3, exposed to CD3/CD28, and analyzed by flow cytometry. D, Effect of NO on CD3/CD28-induced MHP. After pretreatment with 200 µM NOC-18 for 24 h, PBL were stimulated with CD3/CD28 for 24 h and Δψm was assessed by TMRM fluorescence in CD3+/annexin V− cells. E, Effect of NO on sustained elevation of [Ca2+]c. After pretreatment with 200 µM NOC-18 for 24 h, PBL were stimulated with CD3/CD28 for 24 h and [Ca2+]c levels were assessed by Fluo-3 fluorescence in CD3+/annexin V− cells. Data in C–E represent mean ± SE of independent experiments using four healthy donors. Values of p reflect the effect of NOC-18 pretreatment.
Discussion
Adaptive immune responses by T lymphocytes are mediated by interaction of the TCR with a specific peptide-MHC Ag complex on the APC. The outcome of TCR engagement depends on concomitant signaling through costimulatory molecules (CD28, CD40L, LFA-1, CD2) and cytokines (42). Intracellular signal transduction is mediated via protein tyrosine kinases (LYN, SYK), phosphatases (CD45, SHP-1), and phospholipase Cγ1 (43), leading to cleavage of phosphatidylinositol diphosphate and biphasic calcium mobilization (28, 38). As early as 2 min after T cell activation, with respect to control T cells, a markedly enhanced Ca2+ signal was detected in lupus patients. This initial surge in intracellular Ca2+ concentration is due to the release of Ca2+ from intracellular stores, such as mitochondria (38, 39). [Ca2+]m was markedly enhanced in lupus T cells 24 h after CD3/CD28 costimulation (2.73 ± 0.09-fold, p = 0.005; Fig. 1C). Thus, increased mitochondrial mass and formation of megamitochondria may be responsible for increased sequestration and storage of Ca2+ in mitochondria which, in turn, may lead to enhanced early Ca2+ fluxing in lupus T cells (44). By contrast, sustained elevations of cytosolic Ca2+ levels were reduced and delayed in lupus T cells. Maximal elevation of cytosolic Ca2+ levels in control T cells, 2.81 ± 0.09-fold, occurred 4 h after CD3/CD28 stimulation, while T cell activation induced a more moderate rise, 1.59 ± 0.03-fold, in cytosolic Ca2+ of lupus T cells (p < 0.0001). Capacitative entry through the plasma membrane is thought to account for the plateau phase of Ca2+ signaling (39). Hyporesponsiveness in the late phase of Ca2+ signaling has been attributed to oxidative stress in human T lymphocytes (45). Lower sustained Ca2+ levels may play a role in reduced IL-2 production in patients with SLE (1). Thus, persistent MHP and oxidative stress (9, 23) may account for the altered pattern of Ca2+ handling in lupus T cells. As previously documented, MHP was observed in patients with SLE but not in healthy donors or patients with rheumatoid arthritis (9, 23). MHP (9) or Ca2+ levels in lupus T cells were unrelated to SLEDAI, similar to earlier findings (44).
Ca2+ fluxing is regulated by NO via modulation of Δψm (27, 39). NO has recently been recognized as a key signal for MHP (22) that initiates mitochondrial biogenesis (28) through enlargement and proliferation of mitochondria (46). Although NO-induced transient MHP is mediated via reversible inhibition of cytochrome c oxidase (27), downstream events leading to mitochondrial biogenesis have not been clearly defined (46). Monocytes of patients with SLE exhibit increased NO production. These observations are consistent with previous findings on elevated serum 3-nitrotyrosine levels, suggestive of increased NO production in patients with SLE (47). Since NO generated by one cell can regulate the respiration of adjacent cells (30), increased NO production by monocytes may lead to mitochondrial hypertrophy and proliferation in lupus T cells. Mitochondria constitute major Ca2+ stores (40), thus increased mitochondrial mass may account for altered Ca2+ handling upon activation of T cells in patients with SLE.
Persistent MHP and ATP depletion play key roles in abnormal T cell death, enhanced spontaneous and diminished activation-induced cell death, and predisposition for necrosis in patients with SLE (9). Apoptosis is a physiological process that results in nuclear condensation and breakup of the cell into membrane-enclosed apoptotic bodies suitable for phagocytosis by macrophages, thus preventing inflammation. By contrast, necrosis is a pathological process that results in cellular swelling, followed by lysis and release of proteases, oxidizing molecules, and other proinflammatory and chemotactic factors resulting in inflammation and tissue damage (10). Indeed, lymphocyte necrosis occurs in the bone marrow (11) and lymph nodes of lupus patients (12) and may significantly contribute to the inflammatory process (13). Swollen lymph nodes of patients with SLE harbor increased numbers of necrotic T lymphocytes and dendritic cells (DC) (12, 48). Tissue lesions (49, 50) and blood of patients with SLE harbor activated plasmacytoid DC (51, 52). Necrotic, but not apoptotic, cell death generates inflammatory signals necessary for the activation and maturation of DC, the most potent APCs (53–55). CD14+ monocytes isolated from the blood of lupus patients, but not those from healthy individuals, act as DC (56). Necrotic but not apoptotic cells also release heat shock proteins gp96, heat shock protein 90. heat shock protein 70, and calreticulin (54), which enhance NO production (57, 58) and expression of costimulatory molecules CD40 and CD86 by monocytes and DC (55). Thus, a positive feedback loop between T cells as well as monocytes and DC may play a major role in relentless proinflammatory signaling in SLE. The present data are consistent with a key role for intercellular NO signaling in persistent MHP in altered Ca2+ fluxing and cell death pathway selection in lupus T cells.
Acknowledgments
This work was supported in part by Grants DK 49221 and AI 48079 from the National Institutes of Health and the Central New York Community Foundation.
3
Abbreviations used in this paper: SLE, systemic lupus erythematosus; Δψm, mitochondrial transmembrane potential; MHP, mitochondrial hyperpolarization; ROI, reactive oxygen intermediates; TMRM, tetramethylrhodamine methyl ester; DiOC6, 3,3′-dihexyloxacarbocyanine iodide; JC-1, 5,5′,6,6′-tetrachloro-1,1′,3,3′-tetraethylbenzimidazolocarbocyanine iodide; DAF-FM, 4-amino-5-methylamino-2′,7′-difluorofluorescein diacetate; NOC-18, (Z)-1-[2-(2-aminoethyl)-N-(2-ammonioethyl)amino] diazen-1-ium-1,2-diolate diethylenetriamine; MTG, mitotracker green; NAO, nonyl acridine orange; [Ca2+]c, cytoplasmic calcium level; [Ca2+]m, mitochondrial calcium level; PS, phosphatidylserine; SLEDAI, SLE Disease Activity Index; RF, relative fluorescence; DC, dendritic cell; FL, fluorescence channel.
References
- 1.Kammer GM, Perl A, Richardson BC, Tsokos GC. Abnormal T cell Signal transduction in systemic lupus erythematosus. Arthritis Rheum. 2002;46:1139. doi: 10.1002/art.10192. [DOI] [PubMed] [Google Scholar]
- 2.Elkon KB. Apoptosis in SLE—too little or too much? Clin. Exp. Rheumatol. 1994;12:553. [PubMed] [Google Scholar]
- 3.Perl A, Banki K. Molecular mimicry, altered apoptosis, and immunomodulation as mechanisms of viral pathogenesis in systemic lupus erythematosus. In: Kammer GM, Tsokos GC, editors. Lupus: Molecular and Cellular Pathogenesis. Totowa, NJ: Humana Press; 1999. pp. 43–64. [Google Scholar]
- 4.Cohen JJ, Duke RC, Fadok VA, Sellins KS. Apoptosis and programmed cell death in immunity. Annu. Rev. Immunol. 1992;10:267. doi: 10.1146/annurev.iy.10.040192.001411. [DOI] [PubMed] [Google Scholar]
- 5.Thompson CB. Apoptosis in the pathogenesis and treatment of disease. Science. 1995;267:1456. doi: 10.1126/science.7878464. [DOI] [PubMed] [Google Scholar]
- 6.Emlen W, Niebur JA, Kadera R. Accelerated in vitro apoptosis of lymphocytes from patients with systemic lupus erythematosus. J. Immunol. 1994;152:3685. [PubMed] [Google Scholar]
- 7.Casciola-Rosen LA, Anhalt G, Rosen A. Autoantigens targeted in systemic lupus erythematosus are clustered in two populations of surface structures on apoptotic keratinocytes. J. Exp. Med. 1994;179:1317. doi: 10.1084/jem.179.4.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kovacs B, Vassilopoulos D, Vogelgesang SA, Tsokos GC. Defective CD3-mediated cell death in activated T cells from patients with systemic lupus erythematosus: role of decreased intracellular TNF-α. Clin. Immunol. Immunopathol. 1996;81:293. doi: 10.1006/clin.1996.0192. [DOI] [PubMed] [Google Scholar]
- 9.Gergely PJ, Grossman C, Niland B, Puskas F, Neupane H, Allam F, Banki K, Phillips PE, Perl A. Mitochondrial hyperpolarization and ATP depletion in patients with systemic lupus erythematosus. Arthritis Rheum. 2002;46:175. doi: 10.1002/1529-0131(200201)46:1<175::AID-ART10015>3.0.CO;2-H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fiers W, Beyaert R, Declercq W, Vandenabeele P. More than one way to die: apoptosis, necrosis and reactive oxygen damage. Oncogene. 1999;18:7719. doi: 10.1038/sj.onc.1203249. [DOI] [PubMed] [Google Scholar]
- 11.Lorand-Metze I, Carvalho MA, Costallat LT. Morphology of bone marrow in systemic lupus erythematosus (German) Pathologe. 1994;15:292. doi: 10.1007/s002920050057. [DOI] [PubMed] [Google Scholar]
- 12.Ko YH, Dal Lee J. Fine needle aspiration cytology in lupus lymphadenopathy: a case report. Acta Cytol. 1992;36:748. [PubMed] [Google Scholar]
- 13.Eisner MD, Amory J, Mullaney B, Tierney L, Jr, Browner WS. Necrotizing lymphadenitis associated with systemic lupus erythematosus. Semin. Arthritis Rheum. 1996;26:477. doi: 10.1016/s0049-0172(96)80028-x. [DOI] [PubMed] [Google Scholar]
- 14.Skulachev VP. Mitochondrial physiology and pathology; concepts of programmed death of organelles, cells and organisms. Mol. Aspects Med. 1999;20:139. doi: 10.1016/s0098-2997(99)00008-4. [DOI] [PubMed] [Google Scholar]
- 15.Susin SA, Zamzami N, Castedo M, Daugas H-G, Wang E, Geley S, Fassy F, Reed RC, Kroemer G. The central executioner of apoptosis: multiple connections between protease activation and mitochondria in Fas/Apo-1/CD95- and ceramide-induced apoptosis. J. Exp. Med. 1997;186:25. doi: 10.1084/jem.186.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Banki K, Hutter E, Gonchoroff N, Perl A. Elevation of mitochondrial transmembrane potential and reactive oxygen intermediate levels are early events and occur independently from activation of caspases in Fas signaling. J. Immunol. 1999;162:1466. [PMC free article] [PubMed] [Google Scholar]
- 17.Gottlieb E, Vander Heiden MG, Thompson CB. Bcl-xL prevents the initial decrease in mitochondrial membrane potential and subsequent reactive oxygen species production during tumor necrosis factor α-induced apoptosis. Mol. Cell Biol. 2000;20:5680. doi: 10.1128/mcb.20.15.5680-5689.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Puskas F, Gergely P, Banki K, Perl A. Stimulation of the pentose phosphate pathway and glutathione levels by dehydroascorbate, the oxidized form of vitamin C. FASEB J. 2000;14:1352. doi: 10.1096/fj.14.10.1352. [DOI] [PubMed] [Google Scholar]
- 19.Li P-F, Dietz R, von Harsdorf R. p53 regulates mitochondrial membrane potential through reactive oxygen species and induces cytochrome c-independent apoptosis blocked by bcl-2. EMBO J. 1999;18:6027. doi: 10.1093/emboj/18.21.6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scarlett JL, Sheard PW, Hughes G, Ledgerwood EC, Ku H-H, Murphy MP. Changes in mitochondrial membrane potential during staurosporin-induced apoptosis in Jurkat cells. FEBS Lett. 2000;475:267. doi: 10.1016/s0014-5793(00)01681-1. [DOI] [PubMed] [Google Scholar]
- 21.Sanchez-Alcazar JA, Ault JG, Khodjakov A, Schneider E. Increased mitochondrial cytochrome c levels and mitochondrial hyperpolarization precede camptothecin-induced apoptosis in Jurkat cells. Cell Death Differ. 2000;7:1090. doi: 10.1038/sj.cdd.4400740. [DOI] [PubMed] [Google Scholar]
- 22.Almeida A, Almeida J, Bolanos JP, Moncada S. Different responses of astrocytes and neurons to nitric oxide: the role of glycolytically generated ATP in astrocyte protection. Proc. Natl. Acad. Sci. USA. 2001;98:15294. doi: 10.1073/pnas.261560998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gergely PJ, Niland B, Gonchoroff N, Pullmann R, Jr, Phillips PE, Perl A. Persistent mitochondrial hyperpolarization, increased reactive oxygen intermediate production, and cytoplasmic alkalinization characterize altered IL-10 signaling in patients with systemic lupus erythematosus. J. Immunol. 2002;169:1092. doi: 10.4049/jimmunol.169.2.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stryer L. Biochemistry. New York: Freeman; 1988. Oxidative phosphorylation; p. 397. [Google Scholar]
- 25.Leist M, Single B, Castoldi AF, Kuhnle S, Nicotera P. Intracellular adenosine triphosphate (ATP) concentration: a switch in the decision between apoptosis and necrosis. J. Exp. Med. 1997;185:1481. doi: 10.1084/jem.185.8.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacMicking J, Xie QW, Nathan C. Nitric oxide and macrophage function. Annu. Rev. Immunol. 1997;15:323. doi: 10.1146/annurev.immunol.15.1.323. [DOI] [PubMed] [Google Scholar]
- 27.Brown GC. Nitric oxide and mitochondrial respiration. Biochim. Biophys. Acta. 1999;1411:351. doi: 10.1016/s0005-2728(99)00025-0. [DOI] [PubMed] [Google Scholar]
- 28.Nisoli E, Clementi E, Paolucci C, Cozzi V, Tonello C, Sciorati C, Bracale R, Valerio A, Francolini M, Moncada S, Carruba MO. Mitochondrial biogenesis in mammals: the role of endogenous nitric oxide. Science. 2003;299:896. doi: 10.1126/science.1079368. [DOI] [PubMed] [Google Scholar]
- 29.Nagy G, Koncz A, Perl A. T cell activation-induced mitochondrial hyperpolarization is mediated by Ca2+- and redox-dependent production of nitric oxide. J. Immunol. 2003;171:5188. doi: 10.4049/jimmunol.171.10.5188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown GC, Foxwell N, Moncada S. Transcellular regulation of cell respiration by nitric oxide generated by activated macrophages. FEBS Lett. 1998;439:321. doi: 10.1016/s0014-5793(98)01404-5. [DOI] [PubMed] [Google Scholar]
- 31.Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 32.Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH. and the Committee on Prognosis Studies in SLE. 1992 Derivation of the SLEDAI: a disease activity index for lupus patients. Arthritis Rheum. 35:630. doi: 10.1002/art.1780350606. [DOI] [PubMed] [Google Scholar]
- 33.Perl A, Gonzalez-Cabello R, Lang I, Gergely P. Effector activity of OKT4+ and OKT8+ T-cell subsets in lectin-dependent cell-mediated cytotoxicity against adherent HEp-2 cells. Cell. Immunol. 1984;84:185. doi: 10.1016/0008-8749(84)90089-3. [DOI] [PubMed] [Google Scholar]
- 34.Tanner MK, Wellhausen SR, Klein JB. Flow cytometric analysis of altered mononuclear cell transmembrane potential induced by cyclosporin. Cytometry. 1993;14:59. doi: 10.1002/cyto.990140111. [DOI] [PubMed] [Google Scholar]
- 35.Smiley ST, Reers M, Mottola-Hartshorn C, Lin M, Chen A, Smith TW, Jr, Steele GD, Bo Chen L. Intracellular heterogeneity in mitochondrial membrane potentials revealed by a J-aggregate-forming cation JC-1. Proc. Natl. Acad. Sci. USA. 1991;88:3671. doi: 10.1073/pnas.88.9.3671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cossarizza A, Franceschi C, Monti D, Salvioli S, Bellesia E, Rivabene R, Biondo L, Rainaldi G, Tinari A, Malorni W. Protective effect of N-acetylcysteine in tumor necrosis factor-α-induced apoptosis in U937 cells: the role of mitochondria. Exp. Eye Res. 1995;220:232. doi: 10.1006/excr.1995.1311. [DOI] [PubMed] [Google Scholar]
- 37.Hajnoczky G, Robb-Gaspers LD, Seitz MB, Thomas AP. Decoding of cytosolic calcium oscillations in the mitochondria. Cell. 1995;82:415. doi: 10.1016/0092-8674(95)90430-1. [DOI] [PubMed] [Google Scholar]
- 38.Imboden JB, Weiss A. The T-cell antigen receptor regulates sustained increases in cytoplasmic free Ca2+ through extracellular Ca2+ influx and ongoing intracellular Ca2+ mobilization. Biochem. J. 1987;247:695. doi: 10.1042/bj2470695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duchen MR. Mitochondria and calcium: from cell signalling to cell death. J. Physiol. 2000;529:T68. doi: 10.1111/j.1469-7793.2000.00057.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pariente JA, Camello C, Camello PJ, Salido GM. Release of calcium from mitochondrial and nonmitochondrial intracellular stores in mouse pancreatic acinar cells by hydrogen peroxide. J. Membr. Biol. 2001;179:27. doi: 10.1007/s002320010034. [DOI] [PubMed] [Google Scholar]
- 41.Wakabayashi T. Megamitochondria formation: physiology and pathology. J. Cell. Mol. Med. 2002;6:497. doi: 10.1111/j.1582-4934.2002.tb00452.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lenardo M, Chan KM, Hornung F, McFarland H, Siegel R, Wang J, Zheng L. Mature T lymphocyte apoptosis–immune regulation in a dynamic and unpredictable antigenic environment. Annu. Rev. Immunol. 1999;17:221. doi: 10.1146/annurev.immunol.17.1.221. [DOI] [PubMed] [Google Scholar]
- 43.Koretzky GA, Boerth NJ. The role of adapter proteins in T cell activation. Cell. Mol. Life Sci. 1999;56:1048. doi: 10.1007/s000180050492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vassilopoulos D, Kovacs B, Tsokos GC. TCR/CD3 complexmediated signal transduction pathway in T cells and T cell lines from patients with systemic lupus erythematosus. J. Immunol. 1995;155:2269. [PubMed] [Google Scholar]
- 45.Cemerski S, Cantagrel A, Van Meerwijk JP, Romagnoli P. Reactive oxygen species differentially affect T cell receptor-signaling pathways. J. Biol. Chem. 2002;277:19585. doi: 10.1074/jbc.M111451200. [DOI] [PubMed] [Google Scholar]
- 46.Nisoli E, Clementi E, Moncada S, Carruba MO. Mitochondrial biogenesis as a cellular signaling framework. Biochem. Pharmacol. 2004;67:1. doi: 10.1016/j.bcp.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 47.Oates JC, Christensen EF, Reilly CM, Self SE, Gilkeson GS. Prospective measure of serum 3-nitrotyrosine levels in systemic lupus erythematosus: correlation with disease activity. Proc. Assoc. Am. Phys. 1999;111:611. doi: 10.1046/j.1525-1381.1999.99110.x. [DOI] [PubMed] [Google Scholar]
- 48.Kojima M, Nakamura S, Morishita Y, Itoh H, Yoshida K, Ohno Y, Oyama T, Asano S, Joshita T, Mori S, et al. Reactive follicular hyperplasia in the lymph node lesions from systemic lupus erythematosus patients: a clinicopathological and immunohistological study of 21 cases. Pathol. Int. 2000;50:304. doi: 10.1046/j.1440-1827.2000.01052.x. [DOI] [PubMed] [Google Scholar]
- 49.Mori M, Pimpinelli N, Romagnoli P, Bernacchi E, Fabbri P, Giannotti B. Dendritic cells in cutaneous lupus erythematosus: a clue to the pathogenesis of lesions. Histopathology. 1994;24:311. doi: 10.1111/j.1365-2559.1994.tb00531.x. [DOI] [PubMed] [Google Scholar]
- 50.Farkas L, Beiske K, Lund-Johansen F, Brandtzaeg P, Jahnsen FL. Plasmacytoid dendritic cells (natural interferon- α/β-producing cells) accumulate in cutaneous lupus erythematosus lesions. Am. J. Pathol. 2001;159:237. doi: 10.1016/s0002-9440(10)61689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ronnblom L, Alm GV. The natural interferon-α producing cells in systemic lupus erythematosus. Hum. Immunol. 2002;63:1181. doi: 10.1016/s0198-8859(02)00757-7. [DOI] [PubMed] [Google Scholar]
- 52.Pascual V, Banchereau J, Palucka AK. The central role of dendritic cells and interferon-α in SLE. Curr. Opin. Rheumatol. 2003;15:548. doi: 10.1097/00002281-200309000-00005. [DOI] [PubMed] [Google Scholar]
- 53.Gallucci S, Lolkema M, Matzinger P. Natural adjuvants: endogenous activators of dendritic cells. Nat. Med. 1999;5:1249. doi: 10.1038/15200. [DOI] [PubMed] [Google Scholar]
- 54.Basu S, Binder RJ, Suto R, Anderson KM, Srivastava PK. Necrotic but not apoptotic cell death releases heat shock proteins, which deliver a partial maturation signal to dendritic cells and activate the NF-κB pathway. Int. Immunol. 2000;12:1539. doi: 10.1093/intimm/12.11.1539. [DOI] [PubMed] [Google Scholar]
- 55.Sauter B, Albert ML, Francisco L, Larsson M, Somersan S, Bhardwaj N. Consequences of cell death: exposure to necrotic tumor cells, but not primary tissue cells or apoptotic cells, induces the maturation of immunostimulatory dendritic cells. J. Exp. Med. 2000;191:423. doi: 10.1084/jem.191.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Blanco P, Palucka AK, Gill M, Pascual V, Banchereau J. Induction of dendritic cell differentiation by IFN-α in systemic lupus erythematosus. Science. 2001;294:1540. doi: 10.1126/science.1064890. [DOI] [PubMed] [Google Scholar]
- 57.Panjwani NN, Popova L, Srivastava PK. Heat shock proteins gp96 and hsp70 activate the release of nitric oxide by APCs. J. Immunol. 2002;168:2997. doi: 10.4049/jimmunol.168.6.2997. [DOI] [PubMed] [Google Scholar]
- 58.Huang YM, Xiao BG, Westerlund I, Link H. Phenotypic and functional properties of dendritic cells isolated from human peripheral blood in comparison with mononuclear cells and T cells. Scand. J. Immunol. 1999;49:177. doi: 10.1046/j.1365-3083.1999.00491.x. [DOI] [PubMed] [Google Scholar]