Abstract
Objective
Studies have implicated foot posture and foot function as risk factors for lower extremity pain. Empirical population-based evidence for this assertion is lacking; therefore, the purpose of this study was to evaluate cross-sectional associations of foot posture and foot function to lower extremity joint pain in a population-based study of adults.
Methods
Participants were members of the Framingham Foot Study. lower extremity joint pain was determined by the response to the NHANES-type question, “On most days do you have pain, aching or stiffness in your [hips, knees, ankles, or feet]?” Modified Arch Index (MAI) classified participants as having planus, rectus (referent) or cavus foot posture. Center of Pressure Excursion Index (CPEI) classified participants as having over-pronated, normal (referent) or over-supinated foot function. Crude and adjusted (age, gender, BMI) logistic regression determined associations of foot posture and function to lower extremity pain.
Results
Participants with planus structure had higher odds of knee (1.57, 95% CI: 1.24– 1.99) or ankle (1.47, 95% CI: 1.05–2.06) pain, whereas those with a cavus foot structure had increased odds of ankle pain only (7.56, 95% CI: 1.99–28.8) and pain at one lower extremity site (1.37, 95% CI: 1.04–1.80). Associations between foot function and lower extremity joint pain were not statistically significant, except for a reduced risk of hip pain in those with an over-supinated foot function (0.69, 95% CI: 0.51–0.93).
Conclusions
These findings offer a link between foot posture and lower extremity pain, highlighting the need for longitudinal or intervention studies.
Keywords: high-arched feet, flat feet, low-arched feet, lower extremity pain
1. Introduction
Lower extremity joint pain is highly prevalent. Estimates suggest that up to 40% of women and 30% of men have experienced non-minor musculoskeletal pain in the past month (1, 2), with older adults, women, and obese individuals at greater risk of lower extremity joint pain (3-6). A suspected, but lesser known, risk factors for lower extremity joint pain may include foot posture (i.e., planus, cavus, and rectus) and foot function (i.e., over-pronated, over-supinated, and normal), as individuals with lower extremity joint pain are more likely to have planus (low-arched) (7-13) cavus (high-arched) (8-11, 14-17), over-pronated (7, 8, 18-23), or over-supinated (8, 20, 24, 25) feet. However, associations with foot posture or foot function to risk of lower extremity joint pain are not universal (10, 26, 27).
Evidence regarding foot posture or foot function as a lower extremity joint pain risk factor is sparse, conflicting, and typically evaluates specialized populations (e.g., athletes (10, 11, 18, 20, 21, 24-27), military trainees (8, 10, 22), patients (12, 14-16)). A retrospective study of triathletes reported that risk of an overuse injury was increased four-fold in those with an over-supinated foot function (24), while a similar study of professional baseball players showed no association between lower extremity joint pain to foot posture or foot function (26). A prospective study of US Naval Special Warfare trainees noted that planus, cavus, and abnormal foot and ankle function was associated with lower extremity injuries (8), while a similar study of Australian Defense Force Academy military trainees showed no association with foot posture and lower extremity pain (10). Part of the discrepancy in results may reside in the specific populations evaluated in these studies, as studies of foot posture and foot pain present conflicting results depending on the level of physical activity of the study participants (14, 15).
Biomechanical evidence also supports the notion that feet with extremes of foot posture (i.e., planus or cavus) or foot function (i.e., over-pronated or over-supinated) are associated with altered lower extremity functional alignment (11, 21, 28) and muscle activation patterns (29, 30). These studies suggest over-pronated foot function yields excessive internal rotation of the shank with excessive anterior pelvic tilt (23, 31) as well as altered knee movements and excessive joint stress (21), whereas a cavus foot may add excessive stress at the ankle due to limited ankle eversion range of motion (11).
While studies have reported associations of foot posture and foot function to lower extremity joint pain, these studies have restrictive participant inclusion criteria (8, 10-12, 14-16, 18, 20-22, 25, 28), failed to adjust for common intrinsic factors of lower extremity pain (11, 18, 19) (e.g., gender, body mass index (BMI), age (3-6)), or utilized a convenience sample of healthy participants to test external devices, such as orthotics, to experimentally manipulate foot posture or function (28, 29). As a result, the generalizability of these results to the adult population may be compromised. Therefore, the purpose of this study was to evaluate the cross-sectional associations of foot posture and foot function to lower extremity joint pain in a population-based study of adult men and women.
2. Methods
2.1 Participants
Study participants are members of the population-based Framingham Foot Study (32), which for this analysis included the Framingham Heart Study and Offspring (33) and community cohorts. The community cohort consists of Framingham residents, recruited between 2002-2005 through random digit dialling from town lists, who were who over 50 years of age and not members of the Framingham Heart Study.
Hebrew SeniorLife and Boston University Institutional Review Boards approved the Framingham Foot Study, and all participants signed an informed consent prior to enrolment. Between 2002 and 2008, participants in the Framingham Foot Study received a plantar pressure and loading assessment during standing and walking, and they were queried regarding musculoskeletal pain.
Inclusion criteria in this analysis included those with complete data on lower extremity joint pain, bilateral measures of foot posture and function, and covariate data. Participants with amputations were excluded.
2.2 Lower Extremity Joint Pain
Lower extremity joint pain was determined by the response to the NHANES-type (US-based National Health and Nutrition Examination Survey) question, “On most days do you have pain, aching or stiffness in your [LE joints]?” Lower extremity joints queried included the hips, knees, ankles and feet. Participants response options were: (i) yes, right side only, (ii) yes, left side only, (iii) yes, both sides, and (iv), no pain on either side. Unilateral and bilateral pain at each site were weighted the same, with responses dichotomized to yes or no.
To evaluate widespread lower extremity joint pain, we created variables of: (i) pain in one lower extremity site, (ii) pain in two lower extremity sites, (iii) pain in three or more lower extremity sites, and (iv) no lower extremity pain (referent).
2.3 Foot Posture and Foot Function
A pressure mat (Matscan, Tekscan Inc., Boston MA) was used to collect data regarding foot posture and function during quiet bipedal standing and during gait, respectively. The Matscan system is a 43.6 × 36.9 cm system with 2288 sensels for a resolution of 1.4 sensels/ cm2, which is placed on the floor and has a height of 0.2cm. Matscan data were recorded at 40 frames per second. With each participant, the Matscan was calibrated by having the individual stand on the mat to set it to the individual's bodyweight.
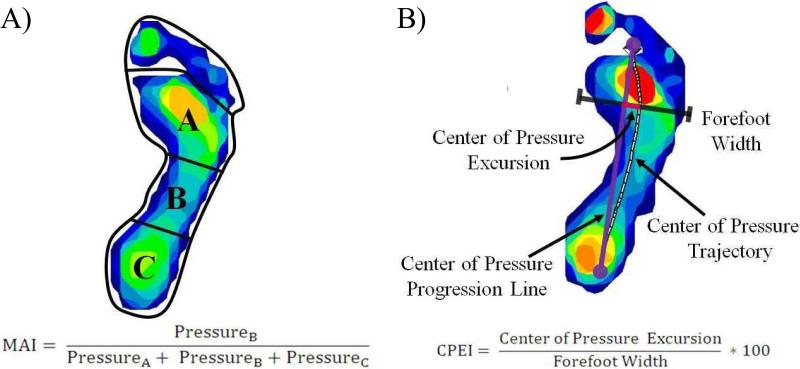
To determine foot posture, participants were asked to stand in their usual bipedal stance, and the pressure under the foot was recorded on the Matscan system. From the quiet bipedal pressure data, each foot was individually analyzed to calculate its Modified Arch Index (MAI) value (Figure 1A). To determine the MAI value, the foot, not including the toes, is divided into three equal parts, and the pressure in the middle third is divided by the total pressure in all three foot regions (34). MAI is correlated with other measures of foot posture, notably navicular height (35).
Figure 1.
Example foot scan and calculation to determine (A) Modified Arch Index (MAI) and (B) Center of Pressure Excursion Index (CPEI) values. To calculate MAI, the foot, not including the toes, is divided into three equal parts, and the pressure in the middle third is divided by the total pressure in all three foot regions. To calculate CPEI, a center of pressure progression line is drawn from the first and last points of each foot's center of pressure trajectory. The distance of the center of pressure trajectory curve at the distal third of the foot from the constructed center of pressure progression line is recorded as the center of pressure excursion. The center of pressure excursion value is normalized by foot width and multiplied by 100 to obtain a percentage excursion of the center of pressure.
To determine foot function, participants were asked to walk barefoot at their usual pace over the Matscan using the two-step method (36). The two-step method involves participants stepping on the pressure mat on the second step and has a similar reliability and reduces the participant burden as they only have to take a minimum of four steps for the assessment, when compared to the mid-gait approach (36). Prior to the gait data collection, participants practiced walking using this protocol to become familiar with the requirements of the assessment in order to ensure that the collected data were representative of the participant's normal gait. Each trial was visually inspected by the examiner, and if the participant seemed to deviate his or her gait (e.g., overreaching) to target the pressure mat, the participant had another trial collected. There were two trials collected, one for each foot. From the walking data, each foot was analyzed to calculate its center of pressure excursion index (CPEI) value (Figure 1B). To determine the CPEI value, a line is drawn from the first and last points of each foot's center of pressure trajectory, and the distance of the center of pressure curve at the distal third of the foot from the constructed line is recorded. This value is normalized by foot width and multiplied by 100 to obtain a percentage excursion of the center of pressure (37). CPEI has been shown to be sensitive to changes in clinical measures of static foot alignment (37).
As each participant had two values of CPEI and MAI, the more extreme MAI and CPEI value, relative to median, were used in the analysis, similar to prior studies of bilateral conditions (38, 39). To classify foot posture and function, the distributions of MAI and CPEI values used were divided into quintiles. Feet in the top and bottom 20% of the MAI values were defined as planus and cavus, respectively, with the middle 60% the rectus feet. Feet in the top and bottom 20% of CPEI values were defined as over-supinated and over-pronated, respectively, with the middle 60% classified as having normal foot function.
2.4 Other Covariates
In this analysis, covariates included gender, age, and body mass index (BMI). Weight was measured with the participant barefoot using a standardized balance beam scale and recorded to the nearest 0.5 pound (0.23 kg). Participant height, without shoes, was measured in inches to the nearest 0.25 inch (6.35mm) using a calibrated stadiometer. Weight and height were used to determine BMI.
Although smoking and alcohol use are available data with the Framingham Foot Study, a similarly-aged population-based study of joint pain showed that these covariates were not significant risk factors of lower extremity pain (40); therefore, we did not adjust for these in our analysis.
2.6 Data Analysis
Means and standard deviations or frequencies of participants’ characteristics variables were calculated for included participants. To assess odds of lower extremity pain at the individual joints (e.g., hip pain, knee pain) by foot structure and foot function, logistic regression analyses were used for each joint. To assess odds of lower extremity pain at the specific individual joints (e.g., hip pain only, knee pain only) by foot structure and foot function, a multinomial logistic regression analysis was used. To evaluate if widespread lower extremity pain was associated with foot posture or foot function, multinomial logistic regression using number of sites of lower extremity pain was used, with the referent being individuals with no lower extremity pain. Because lower extremity pain is thought to have common patterns (e.g., knee and foot pain) (41), a multinomial logistic regression evaluated the patterns of pain in individuals with two site of lower extremity pain.
In addition to these crude models, adjusted models were evaluated for all the regressions analyses. Adjusted models included covariates of age, BMI, and gender (3-6). Further, as prior studies have used either a normal or cavus (12) foot posture as the referent population, associations between the extremes of foot posture were evaluated as well as between extremes of foot function.
All statistical analyses were conducted using the SAS statistical analysis package, version 9.3 (SAS Institute, Cary, NC), with alpha set to p≤0.05.
3. Results
Of the eligible 2188 participants in the Framingham Offspring and community cohorts, there were 1856 participants included in this study, with 944 (50.9%) experiencing lower extremity pain (Table 1). There were 332 participants excluded for missing data (327 were missing center of pressure excursion [CPEI] data and five were missing covariate data). Of the lower extremity sites assessed, knee pain was the most common at 29.4% (N=546), foot pain at 26.2% (N=487), hip pain at 17.5% (N=325), and ankle pain 11.2% (N=207). There were 525 (28.3%), 256 (13.8%), and 163 (8.8%) participants who had pain in one, two, or three or more lower extremity sites, respectively.
Table 1.
Participant characteristics. Data presented as mean ± standard deviation or number of participants (% of participants). LE = lower extremity; BMI = body mass index; MAI = modified arch index; CPEI = center of pressure excursion index.
| All Study Participants (N=1856) | |
|---|---|
| Age, years | 63.8 ± 8.9 |
| Women (%) | 1034 (56) |
| BMI, kg/m2 | 28.6 ± 5.6 |
| MAI value | 0.115 ± 0.101 |
| CPEI value | 13.9 ± 9.95 |
| Hip Pain (%) | 325 (17.5) |
| Hip Pain Only (%) | 102 (5.5) |
| Knee Pain (%) | 546 (29.4) |
| Knee Pain Only (%) | 230 (12.4) |
| Ankle Pain (%) | 207 (11.2) |
| Ankle Pain Only (%) | 19 (1.0) |
| Foot Pain (%) | 487 (26.2) |
| Foot Pain Only (%) | 174 (9.4) |
| Single LE Pain Site (%) | 525 (28.3) |
| Two LE Pain Sites (%) | 256 (13.8) |
| Three or more LE Pain Site (%) | 163 (8.8) |
| No LE Pain (%) | 912 (49.1) |
Individuals who had a foot with a Modified Arch Index (MAI) value greater than 0.164 were considered to have planus feet, whereas less than 0.030 were considered to be cavus, with rectus feet being in between these cut-points (Table 2). Individuals who had a CPEI less than 7.30 were considered to have over-pronated feet, whereas greater than 21.00 were considered to be over-supinated feet, with normal foot function being in between these cut-points.
Table 2.
Modified Arch Index (MAI) values to define pes planus, cavus, and rectus foot posture, and Center of Pressure Excursion Index (CPEI) values to define over-pronated, over-supinated, and normal foot function.
| Foot Posture | MAI Range | Foot Function | CPEI Range |
|---|---|---|---|
| Planus | 0.164 – 0.713 | Over-Pronated | −25.30 – 7.30 |
| Rectus | 0.031 – 0.163 | Normal | 7.40 – 20.90 |
| Cavus | 0 – 0.030 | Over-Supinated | 21.00 – 43.70 |
3.1 Foot Posture
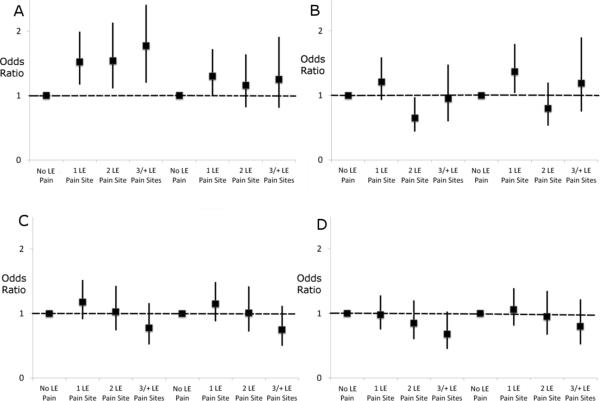
Individuals with a planus foot posture were more likely to have knee (1.57, 95% confidence interval [CI]: 1.24 – 1.99) and ankle pain (1.47, 95% CI: 1.05 – 2.06) compared to individuals with a rectus foot posture (Table 3), with confidence intervals widening after adjusting for age, gender and body mass index (BMI). In the multivariate analysis to evaluate the effects of foot posture on a single-site of pain (Table 4), results were similar, with individuals with planus foot posture having higher odds of knee pain only (1.94, 95% CI: 1.38 – 2.74) and ankle pain only (5.04, 95% CI: 1.29 – 19.7). After adjusting for age, gender and BMI, the odds of knee pain only remained significant (1.52, 95% CI: 1.05 – 2.19), while the odds of ankle pain only were reduced (3.58, 95% CI: 0.88 – 14.6) with wider confidence intervals. Individuals with planus feet showed increased odds of a single lower extremity site, two lower extremity sites, and three or more lower extremity sites of pain, relative to a rectus foot; after adjustment, odds ratios were attenuated (Figure 2). When pain patterns were evaluated in individuals with two lower extremity sites of pain, there were no significant differences in odds of lower extremity pain by foot posture; however, there was an overall tendency of higher odds of pain for individuals with planus feet and lower odds of pain with cavus feet (supplemental data).
Table 3.
Crude and adjusted odds ratios (OR) with 95% confidence intervals (95% CI) of associations of foot posture and foot function to lower extremity pain at any joint.
| Unadjusted OR | Adjusted OR† | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||
| Foot Posture | |||||||
| Hip Pain | Planus v. Rectus | 1.25 | 0.94, 1.66 | 0.130 | 1.12 | 0.83, 1.53 | 0.457 |
| Cavus v. Rectus | 0.98 | 0.71, 1.34 | 0.881 | 1.04 | 0.75, 1.44 | 0.804 | |
| Planus v. Cavus | 1.28 | 0.91, 1.79 | 0.157 | 1.08 | 0.74,1.57 | 0.697 | |
| Knee Pain | Planus v. Rectus | 1.57 | 1.24, 1.99 | <0.001 | 1.17 | 0.91, 1.52 | 0.222 |
| Cavus v. Rectus | 0.86 | 0.66, 1.13 | 0.283 | 1.05 | 0.80, 1.39 | 0.719 | |
| Planus v. Cavus | 1.82 | 1.36, 2.42 | <.001 | 1.12 | 0.81, 1.53 | 0.504 | |
| Ankle Pain | Planus v. Rectus | 1.47 | 1.05, 2.06 | 0.026 | 1.14 | 0.79, 1.64 | 0.488 |
| Cavus v. Rectus | 1.00 | 0.68, 1.47 | 0.994 | 1.16 | 0.78, 1.71 | 0.475 | |
| Planus v. Cavus | 1.47 | 0.98, 2.20 | 0.062 | 0.99 | 0.63, 1.54 | 0.946 | |
| Foot Pain | Planus v. Rectus | 1.22 | 0.95, 1.56 | 0.114 | 1.04 | 0.80, 1.35 | 0.784 |
| Cavus v. Rectus | 0.84 | 0.64, 1.11 | 0.221 | 0.92 | 0.70, 1.22 | 0.569 | |
| Planus v. Cavus | 1.45 | 1.08, 1.95 | 0.015 | 1.13 | 0.81, 1.56 | 0.480 | |
| Foot Function | |||||||
| Hip Pain | Over-pronated v. Normal | 0.82 | 0.62, 1.08 | 0.154 | 0.76 | 0.57,1.02 | 0.065 |
| Over-supinated v. Normal | 0.69 | 0.51, 0.93 | 0.016 | 0.78 | 0.57, 1.05 | 0.103 | |
| Over-pronated v. Over-supinated | 1.18 | 0.86, 1.61 | 0.315 | 0.98 | 0.71, 1.36 | 0.919 | |
| Knee Pain | Over-pronated v. Normal | 0.92 | 0.72, 1.16 | 0.473 | 0.94 | 0.73, 1.20 | 0.599 |
| Over-supinated v. Normal | 0.90 | 0.70, 1.14 | 0.374 | 0.97 | 0.75, 1.26 | 0.826 | |
| Over-pronated v. Over-supinated | 1.02 | 0.79, 1.32 | 0.855 | 0.96 | 0.74, 1.26 | 0.784 | |
| Ankle Pain | Over-pronated v. Normal | 0.86 | 0.61, 1.22 | 0.388 | 0.86 | 0.61, 1.23 | 0.408 |
| Over-supinated v. Normal | 0.92 | 0.65, 1.30 | 0.629 | 0.99 | 0.69, 1.42 | 0.969 | |
| Over-pronated v. Over-supinated | 0.94 | 0.65, 1.36 | 0.727 | 0.87 | 0.59, 1.28 | 0.470 | |
| Foot Pain | Over-pronated v. Normal | 1.10 | 0.87, 1.41 | 0.427 | 1.08 | 0.84, 1.39 | 0.557 |
| Over-supinated v. Normal | 0.89 | 0.69, 1.15 | 0.373 | 0.97 | 0.74, 1.26 | 0.811 | |
| Over-pronated v. Over-supinated | 1.24 | 0.95, 1.62 | 0.108 | 1.11 | 0.85, 1.47 | 0.443 | |
Adjusted by gender, age, and body mass index
Table4.
Crude and adjusted odds ratios (OR) with 95% confidence intervals (95% CI) of associations of foot posture and foot function to lower extremity pain at only one joint.
| Unadjusted OR | Adjusted OR† | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||
| Foot Posture | |||||||
| Hip Pain Only | Planus v. Rectus | 1.24 | 0.73 - 2.09 | 0.434 | 1.22 | 0.70 - 2.10 | 0.484 |
| Cavus v. Rectus | 1.46 | 0.89 - 2.39 | 0.131 | 1.50 | 0.91 - 2.49 | 0.114 | |
| Planus v. Cavus | 0.85 | 0.48 - 1.49 | 0.562 | 0.81 | 0.44 - 1.50 | 0.50 | |
| Knee Pain Only | Planus v. Rectus | 1.94 | 1.38 - 2.74 | <0.001 | 1.52 | 1.05 - 2.19 | 0.026 |
| Cavus v. Rectus | 1.11 | 0.76 - 1.63 | 0.589 | 1.36 | 0.92 - 2.02 | 0.127 | |
| Planus v. Cavus | 1.75 | 1.17 - 2.61 | 0.006 | 1.12 | 0.72 - 1.74 | 0.631 | |
| Ankle Pain Only | Planus v. Rectus | 5.04 | 1.29 - 19.7 | 0.020 | 3.58 | 0.88 - 14.6 | 0.076 |
| Cavus v. Rectus | 5.93 | 1.59 - 22.1 | 0.008 | 7.56 | 1.99 - 28.8 | 0.003 | |
| Planus v. Cavus | 0.85 | 0.31 - 2.32 | 0.751 | 0.47 | 0.15 - 1.51 | 0.206 | |
| Foot Pain Only | Planus v. Rectus | 1.09 | 0.73 - 1.64 | 0.666 | 1.03 | 0.67 - 1.57 | 0.897 |
| Cavus v. Rectus | 1.03 | 0.69 - 1.53 | 0.906 | 1.09 | 0.72 - 1.64 | 0.687 | |
| Planus v. Cavus | 1.07 | 0.67 - 1.70 | 0.784 | 0.95 | 0.57 - 1.57 | 0.827 | |
| Foot Function | |||||||
| Hip Pain Only | Over-pronated v. Normal | 0.91 | 0.57 - 1.44 | 0.706 | 0.85 | 0.53 - 1.37 | 0.504 |
| Over-supinated v. Normal | 0.65 | 0.38 - 1.09 | 0.101 | 0.70 | 0.41 - 1.19 | 0.185 | |
| Over-pronated v. Over-supinated | 1.41 | 0.82 - 2.44 | 0.217 | 1.21 | 0.69 - 2.13 | 0.502 | |
| Knee Pain Only | Over-pronated v. Normal | 1.17 | 0.82 - 1.66 | 0.395 | 1.20 | 0.53 - 1.73 | 0.325 |
| Over-supinated v. Normal | 1.19 | 0.83 - 1.69 | 0.345 | 1.27 | 0.88 - 1.83 | 0.196 | |
| Over-pronated v. Over-supinated | 0.98 | 0.69 - 1.41 | 0.928 | 0.94 | 0.65 - 1.37 | 0.764 | |
| Ankle Pain Only | Over-pronated v. Normal | 0.98 | 0.30 - 3.26 | 0.979 | 1.04 | 0.31 - 3.49 | 0.948 |
| Over-supinated v. Normal | 1.58 | 0.54 - 4.61 | 0.402 | 1.60 | 0.54 - 4.71 | 0.399 | |
| Over-pronated v. Over-supinated | 0.62 | 0.20 - 1.93 | 0.411 | 0.65 | 0.20 - 2.09 | 0.474 | |
| Foot Pain Only | Over-pronated v. Normal | 1.40 | 0.95 - 2.05 | 0.082 | 1.32 | 0.89 - 1.93 | 0.164 |
| Over-supinated v. Normal | 0.90 | 0.60 - 1.37 | 0.637 | 0.99 | 0.65 - 1.51 | 0.949 | |
| Over-pronated v. Over-supinated | 1.55 | 1.03 - 2.33 | 0.036 | 1.33 | 0.87 - 2.04 | 0.182 | |
Adjusted by gender, age, and body mass index
Figure 2.
Crude and adjusted (gender, age, body mass index) odds ratios (OR) with 95% confidence intervals (95% CI) of associations of foot posture and foot structure to number of site of lower extremity (LE) pain. Foot posture associations are A) planus and B) cavus feet relative to rectus feet. Foot function associations are C) over-pronated and D) over-supinated feet relative to normal feet. and foot function to LE pain. OR and adjusted OR values of number of LE pain sites are provided in supplement A, with the OR and adjusted OR values for the patterns of pain for two LE pain sites provided in supplement B.
Individuals with cavus foot posture had 5.93 (95% CI: 1.59 – 22.1) increased odds of ankle pain, and after adjustment the increased odds were maintained (7.56, 95% CI: 1.99 – 28.8). Relative to rectus feet and after adjusting for age, BMI and gender, cavus feet had higher odds of lower extremity pain at one site (1.37, 95% CI: 1.04 – 1.80).
3.2 Foot Function
Individuals with an over-pronated foot function had lower odds of hip pain (0.69, 95% CI: 0.51 – 0.93) relative to those with a normal foot function, but after adjustment the association was reduced. In general, compared to individuals with normal foot function, individuals with over-pronated or with over-supinated foot function had similar odds of pain at the lower extremity sites assessed. Further, odds of a single lower extremity site, two lower extremity sites, and three or more lower extremity sites of pain showed no significant associations in the crude or adjusted models, regardless of referent population. When pain patterns were evaluated in individuals with two sites of lower extremity pain, odds of both hip and knee pain were decreased with an over-supinated foot function (0.49, 95% CI: 0.25 – 0.98); after adjustment these associations were attenuated (0.56, 95% CI: 0.28 – 1.13).
4. Discussion
The purpose of this cross-sectional study was to evaluate the associations of foot posture and foot function to lower extremity joint pain in a population-based study of adult men and women. Relative to rectus foot posture, those with a planus foot had greater odds of knee and ankle pain, whereas those with a cavus foot posture had increased odds of ankle pain. Further, individuals with a cavus foot type had greater odds overall of having one site of lower extremity joint (i.e., hips, knees, ankle, foot) pain. Foot function during gait, as measured by CPEI showed no associations to lower extremity joint pain; however those with an over-supinated foot were at reduced odds of having hip pain as well as concurrent hip and knee pain. The results suggest that having extremes of foot posture (cavus or planus) predisposes individuals to a greater risk of lower extremity joint pain, whereas extremes of foot function (over-pronated or over-supinated) show little effect on odds of lower extremity joint pain. As foot posture is modifiable using foot orthoses (42), whereas other common risk factors (e.g., increasing age, gender, obesity (3-6)) are less modifiable, these findings may have implications for the prevention and/or treatment of knee and ankle pain in adults.
Our results suggest that foot posture (planus and cavus feet), rather than foot function (over-pronated and over-supinated feet) may be an independent risk factor for lower extremity joint pain. Similar to our work, prior research suggests that knee pain is associated with a planus foot (8, 10-12), while both cavus (17) and planus (13) foot type are associated with ankle injuries and pain. While some studies report similar findings (8, 10-12), our work is counter to others (18-22, 24, 25). Our results may differ from these prior findings; however, many of the differences are mitigated through study design characteristics (18, 20-22, 24, 25), such as using restrictive inclusion/exclusion criteria, and referent populations (18, 19).
The novelty in understanding our results in relation to prior work does not lay in comparisons with prior cross-sectional, retrospective, or even prospective studies, but in footwear and orthotic intervention studies, especially with regard to knee pain, which is a major contributor to disabilities in adults (43).
A common aspect of non-pharmacological intervention studies of lower extremity pain is the use of orthotic devices and shoewear modifications for these patients (44). Lateral wedge orthotics for patients with medial compartment knee OA is a common, conservative treatment strategy. Lateral wedge orthotics shift the center of pressure laterally to reduce knee adductor moments (45), which has been linked to medial knee OA progression and knee joint pain (47, 48). Correspondingly, individuals with a planus foot posture display a more medial center of pressure when standing, relative to cavus or rectus foot postures (49), which may explain the increased risk of knee pain within the planus foot posture noted within our study. These lateral wedge orthotics that shift the center of pressure laterally decreases use of NSAIDs (nonsteroidal anti-inflammatory drugs) and yield better orthotic compliance compared to those with the neutral-wedged insole for the populations with symptomatic knee OA (47).
Lateral wedge orthotics can also increase gluteus medius muscle activity (50), which is altered in those with knee (51) or hip pain (52). Increases in gluteus medius muscle activity stabilize the hip and control lumbopelvic motion (53). Causes of the muscle activation changes with orthotics are unknown; however, orthotic use may influence plantar tactile sense (54) and foot alignment or posture (55) to enhance muscle activation and gait (56). In light of our current findings, these studies highlight the need to evaluate the mechanism by which orthotics and shoewear interventions affect the kinetic chain, starting with how foot posture and function influence alignment, function and pain in the hips, knees, ankles, and feet.
4.2 Strengths & Limitations
Although we found associations of foot posture and function to lower extremity joint pain, these results should be evaluated with consideration to the study's strength and limitations. First, our analysis was a cross-sectional evaluation of foot biomechanics and regional foot pain, meaning that causal relations cannot be inferred. While lower extremity pain, particularly knee pain with joint space narrowing (57), may cause planus feet through a change in knee alignment as compensation for the pain, results of other studies suggest foot posture is a predictor of knee pain (12). Further, given that MAI is noted as the pedobarographic measure to use as a surrogate for foot structure (35), it is not a direct measure of arch structure or forefoot-rearfoot alignment, which may also be an important component of foot posture (58). Further, neither MAI nor CPEI have clinically-defined cut-points to determine foot posture or foot function. However, our 20% cut-points are similar or more restrictive than the proposed cut-points of cavus and planus feet using MAI, which are noted as lower than 0.047 (59) or lower than 0.0926 (34) for cavus feet, and greater than 0.158 (59) or greater than 0.1778 for planus feet (34). Given the lack of clinically-derived cut-points, using locomotor extremes, such as the top and bottom 20% of MAI and CPEI values, may provide evidence of structure-function relationships (60). Further, although other studies have suggested multiple trials may be required for a reliable measure using the Tekscan Matscan (61), given the large participant numbers only one scan per foot was collected. However, in prior work on the Framingham Foot Study, it was noted that with a reliability of 0.50 (Metscan reliability measures noted as greater than 0.70) (61), a sample size of less than 300 participants was needed to appropriately power the study (62). Therefore, due to the higher sample size of our study, we are confident that the findings noted are not an artifact of the single scan of each foot and that the study was adequately powered given the single assessment of foot posture and foot function. These results suggest that foot posture is associated with lower extremity pain, and further work using radiographic and/or kinematic measures to assess foot posture and its relation to lower extremity pain is warranted.
The strengths of this study include its participants, data collection, and analysis. The Framingham Foot Study is a well-described, population-based cohort of adults evaluating foot posture, foot function, and lower extremity joint pain. The range of participant demographics (e.g., men and women, aged 36 to 100 years, BMI range of 15.3 to 58.5 kg/m2) provides greater generalizability of the study results. Moreover, the MAI is a simple, clinically-relevant measure of foot posture that can identify whether individuals have planus feet (35) and are at an increased risk of knee, ankle or widespread lower extremity pain. Although confirmatory studies, including longitudinal studies, of foot posture and lower extremity joint pain are needed to substantiate our cross-sectional results, this work suggests that foot posture should be an important consideration in evaluating lower extremity joint pain risk.
5. Conclusion
Planus foot posture, as measured by the modified arch index (MAI), is associated with greater risk of knee and widespread lower extremity pain, while cavus foot posture is associated with ankle joint pain; foot function, as measured by center of pressure excursion index (CPEI) shows no association with lower extremity joint pain. These findings offer preliminary support of a mechanistic link between foot posture and lower extremity pain. This study also points to a need for longitudinal studies to evaluate the role of foot posture in lower extremity pain and intervention studies to evaluate if corrective orthotics or shoewear can be used to prevent or treat lower extremity pain.
Supplementary Material
Significance and Innovations.
Planus foot structure associated with increased odds of knee and ankle pain
Cavus foot structure associated with increased odds of ankle pain or pain at one lower extremity site
Extremes of foot function not associated with increased odds of lower extremity pain
Acknowledgements
Funding for this project was provided by the NIH's National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01-AR047853).
Grant Support: National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01-AR047853).
Footnotes
Conflict of Interest: None
References
- 1.Gureje O, Simon GE, Von Korff M. A cross-national study of the course of persistent pain in primary care. Pain. 2001;92(1-2):195–200. doi: 10.1016/s0304-3959(00)00483-8. [DOI] [PubMed] [Google Scholar]
- 2.Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: a World Health Organization Study in Primary Care. JAMA. 1998;280(2):147–51. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 3.Miranda H, Viikari-Juntura E, Martikainen R, Riihimäki H. A prospective study on knee pain and its risk factors. Osteoarthritis and Cartilage. 2002;10(8):623–30. doi: 10.1053/joca.2002.0796. [DOI] [PubMed] [Google Scholar]
- 4.Picavet HSJ, Schouten JSAG. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC3-study. Pain. 2003;102(1–2):167–78. doi: 10.1016/s0304-3959(02)00372-x. [DOI] [PubMed] [Google Scholar]
- 5.van der Waal JM, Bot SD, Terwee CB, van der Windt DA, Schellevis FG, Bouter LM, et al. The incidences of and consultation rate for lower extremity complaints in general practice. Ann Rheum Dis. 2006;65(6):809–15. doi: 10.1136/ard.2005.036988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bingefors K, Isacson D. Epidemiology, co-morbidity, and impact on health-related quality of life of self-reported headache and musculoskeletal pain—a gender perspective. European Journal of Pain. 2004;8(5):435–50. doi: 10.1016/j.ejpain.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Menz HB, Tiedemann A, Kwan MM, Plumb K, Lord SR. Foot pain in community-dwelling older people: an evaluation of the Manchester Foot Pain and Disability Index. Rheumatology (Oxford) 2006;45(7):863–7. doi: 10.1093/rheumatology/kel002. [DOI] [PubMed] [Google Scholar]
- 8.Kaufman KR, Brodine SK, Shaffer RA, Johnson CW, Cullison TR. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999;27(5):585–93. doi: 10.1177/03635465990270050701. [DOI] [PubMed] [Google Scholar]
- 9.Molgaard C, Lundbye-Christensen S, Simonsen O. High prevalence of foot problems in the Danish population: a survey of causes and associations. Foot (Edinb) 2010;20(1):7–11. doi: 10.1016/j.foot.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Burne SG, Khan KM, Boudville PB, Mallet RJ, Newman PM, Steinman LJ, et al. Risk factors associated with exertional medial tibial pain: a 12 month prospective clinical study. Br J Sports Med. 2004;38(4):441–5. doi: 10.1136/bjsm.2002.004499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams DS, 3rd, McClay IS, Hamill J. Arch structure and injury patterns in runners. Clin Biomech (Bristol, Avon) 2001;16(4):341–7. doi: 10.1016/s0268-0033(01)00005-5. [DOI] [PubMed] [Google Scholar]
- 12.Gross KD, Felson DT, Niu J, Hunter DJ, Guermazi A, Roemer FW, et al. Association of flat feet with knee pain and cartilage damage in older adults. Arthritis Care & Research. 2011;63(7):937–44. doi: 10.1002/acr.20431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mei-Dan O, Kahn G, Zeev A, Rubin A, Constantini N, Even A, et al. The medial longitudinal arch as a possible risk factor for ankle sprains: a prospective study in 83 female infantry recruits. Foot Ankle Int. 2005;26(2):180–3. doi: 10.1177/107110070502600211. [DOI] [PubMed] [Google Scholar]
- 14.Ribeiro AP, Trombini-Souza F, Tessutti V, Rodrigues Lima F, Sacco ICN, João SMA. Rearfoot alignment and medial longitudinal arch configurations of runners with symptoms and histories of plantar fasciitis. Clinics. 2011;66(6):1027–33. doi: 10.1590/S1807-59322011000600018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buchbinder R. Plantar fasciitis. New England Journal of Medicine. 2004;350(21):2159–66. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 16.Burns J, Crosbie J, Hunt A, Ouvrier R. The effect of pes cavus on foot pain and plantar pressure. Clin Biomech (Bristol, Avon) 2005;20(9):877–82. doi: 10.1016/j.clinbiomech.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Morrison KE, Kaminski TW. Foot characteristics in association with inversion ankle injury. J Athl Train. 2007;42(1):135–42. [PMC free article] [PubMed] [Google Scholar]
- 18.Reinking MF. Exercise-related leg pain in female collegiate athletes: the influence of intrinsic and extrinsic factors. Am J Sports Med. 2006;34(9):1500–7. doi: 10.1177/0363546506287298. [DOI] [PubMed] [Google Scholar]
- 19.Irving DB, Cook JL, Young MA, Menz HB. Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. BMC Musculoskelet Disord. 2007;8:41. doi: 10.1186/1471-2474-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dahle LK, Mueller MJ, Delitto A, Diamond JE. Visual assessment of foot type and relationship of foot type to lower extremity injury. J Orthop Sports Phys Ther. 1991;14(2):70–4. doi: 10.2519/jospt.1991.14.2.70. [DOI] [PubMed] [Google Scholar]
- 21.McClay IS, Manal KT. Coupling parameters in runners with normal and excessive pronation. J Appl Biomech. 1997;13:107–24. [Google Scholar]
- 22.Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med. 2004;32(3):772–80. doi: 10.1177/0095399703258776. [DOI] [PubMed] [Google Scholar]
- 23.Rothbart BA, Estabrook L. Excessive pronation: a major biomechanical determinant in the development of chondromalacia and pelvic lists. J Manipulative Physiol Ther. 1988;11(5):373–9. [PubMed] [Google Scholar]
- 24.Burns J, Keenan AM, Redmond A. Foot type and overuse injury in triathletes. J Am Podiatr Med Assoc. 2005;95(3):235–41. doi: 10.7547/0950235. [DOI] [PubMed] [Google Scholar]
- 25.Cain LE, Nicholson LL, Adams RD, Burns J. Foot morphology and foot/ankle injury in indoor football. Journal of Science and Medicine in Sport. 2007;10(5):311–9. doi: 10.1016/j.jsams.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 26.Donatelli R, Wooden M, Ekedahl SR, Wilkes JS, Cooper J, Bush AJ. Relationship between static and dynamic foot postures in professional baseball players. J Orthop Sports Phys Ther. 1999;29(6):316–25. doi: 10.2519/jospt.1999.29.6.316. discussion 26-30. [DOI] [PubMed] [Google Scholar]
- 27.Reinking MF, Austin TM, Hayes AM. Risk factors for self-reported exercise-related leg pain in high school cross-country athletes. J Athl Train. 2010;45(1):51–7. doi: 10.4085/1062-6050-45.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nawoczenski DA, Saltzman CL, Cook TM. The effect of foot structure on the three-dimensional kinematic coupling behavior of the leg and rear foot. Phys Ther. 1998;78(4):404–16. doi: 10.1093/ptj/78.4.404. [DOI] [PubMed] [Google Scholar]
- 29.Bird AR, Bendrups AP, Payne CB. The effect of foot wedging on electromyographic activity in the erector spinae and gluteus medius muscles during walking. Gait Posture. 2003;18:81–91. doi: 10.1016/s0966-6362(02)00199-6. [DOI] [PubMed] [Google Scholar]
- 30.Williams DS, 3rd, Davis IM, Scholz JP, Hamill J, Buchanan TS. High-arched runners exhibit increased leg stiffness compared to low-arched runners. Gait Posture. 2004;19(3):263–9. doi: 10.1016/S0966-6362(03)00087-0. [DOI] [PubMed] [Google Scholar]
- 31.Duval K, Lam T, Sanderson D. The mechanical relationship between the rearfoot, pelvis and low-back. Gait Posture. 2010;32(4):637–40. doi: 10.1016/j.gaitpost.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 32.Dufour AB, Broe KE, Nguyen US, Gagnon DR, Hillstrom HJ, Walker AH, et al. Foot pain: is current or past shoewear a factor? Arthritis Rheum. 2009;61(10):1352–8. doi: 10.1002/art.24733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP. The Framingham Offspring Study. Design and preliminary data. Prev Med. 1975;4(4):518–25. doi: 10.1016/0091-7435(75)90037-7. [DOI] [PubMed] [Google Scholar]
- 34.Chu WC, Lee SH, Chu W, Wang TJ, Lee MC. The use of arch index to characterize arch height: a digital image processing approach. IEEE Trans Biomed Eng. 1995;42(11):1088–93. doi: 10.1109/10.469375. [DOI] [PubMed] [Google Scholar]
- 35.Shiang TY, Lee SH, Lee SJ, Chu WC. Evaluating different footprints parameters as a predictor of arch height. Engineering in Medicine and Biology Magazine, IEEE. 1998;17(6):62–6. doi: 10.1109/51.731323. [DOI] [PubMed] [Google Scholar]
- 36.McPoil TG, Cornwall MW, Dupuis L, Cornwell M. Variability of plantar pressure data. A comparison of the two-step and midgait methods. J Am Podiatr Med Assoc. 1999;89(10):495–501. doi: 10.7547/87507315-89-10-495. [DOI] [PubMed] [Google Scholar]
- 37.Song J, Hillstrom HJ, Secord D, Levitt J. Foot type biomechanics. comparison of planus and rectus foot types. J Am Podiatr Med Assoc. 1996;86(1):16–23. doi: 10.7547/87507315-86-1-16. [DOI] [PubMed] [Google Scholar]
- 38.Crosbie J, Burns J. Are in-shoe pressure characteristics in symptomatic idiopathic pes cavus related to the location of foot pain? Gait Posture. 2008;27(1):16–22. doi: 10.1016/j.gaitpost.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 39.Robbins SM, Birmingham TB, Callaghan JP, Jones GR, Chesworth BM, Maly MR. Association of pain with frequency and magnitude of knee loading in knee osteoarthritis. Arthritis Care & Research. 2011;63(7):991–7. doi: 10.1002/acr.20476. [DOI] [PubMed] [Google Scholar]
- 40.Adamson J, Ebrahim S, Dieppe P, Hunt K. Prevalence and risk factors for joint pain among men and women in the West of Scotland Twenty-07 study. Ann Rheum Dis. 2006;65(4):520–4. doi: 10.1136/ard.2005.037317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Garrow AP, Silman AJ, Macfarlane GJ. The Cheshire Foot Pain and Disability Survey: a population survey assessing prevalence and associations. Pain. 2004;110(1-2):378–84. doi: 10.1016/j.pain.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 42.Razeghi M, Batt ME. Biomechanical analysis of the effect of orthotic shoe inserts: a review of the literature. Sports Med. 2000;29(6):425–38. doi: 10.2165/00007256-200029060-00005. [DOI] [PubMed] [Google Scholar]
- 43.Miller ME, Rejeski WJ, Messier SP, Loeser RF. Modifiers of change in physical functioning in older adults with knee pain: the Observational Arthritis Study in Seniors (OASIS). Arthritis Care & Research. 2001;45(4):331–9. doi: 10.1002/1529-0131(200108)45:4<331::AID-ART345>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 44.Rao S, Riskowski JL, Hannan MT. Musculoskeletal conditions of the foot and ankle: assessments and treatment options. Best Pract Res Clin Rheumatol. 2012;26(3):345–68. doi: 10.1016/j.berh.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Butler RJ, Marchesi S, Royer T, Davis IS. The effect of a subject-specific amount of lateral wedge on knee mechanics in patients with medial knee osteoarthritis. J Orthop Res. 2007;25(9):1121–7. doi: 10.1002/jor.20423. [DOI] [PubMed] [Google Scholar]
- 46.Thorp LE, Wimmer MA, Sumner DR, Lidtke R, Block JA. Custom shoe inserts induce beneficial long-term gait adaptations in medial knee osteoarthritis. Arthritis Rheum. 2007;56:S120. [Google Scholar]
- 47.Pham T, Maillefert JF, Hudry C, Kieffert P, Bourgeois P, Lechevalier D, et al. Laterally elevated wedged insoles in the treatment of medial knee osteoarthritis. A two-year prospective randomized controlled study. Osteoarthritis Cartilage. 2004;12(1):46–55. doi: 10.1016/j.joca.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 48.Barrios JA, Crenshaw JR, Royer TD, Davis IS. Walking shoes and laterally wedged orthoses in the clinical management of medial tibiofemoral osteoarthritis: a one-year prospective controlled trial. Knee. 2009;16(2):136–42. doi: 10.1016/j.knee.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 49.Williams DS, McClay IS. Measurements used to characterize the foot and the medial longitudinal arch: reliability and validity. Phys Ther. 2000;80(9):864–71. [PubMed] [Google Scholar]
- 50.Hertel J, Sloss BR, Earl JE. Effect of foot orthotics on quadriceps and gluteus medius electromyographic activity during selected exercises. Arch Phys Med Rehabil. 2005;86(1):26–30. doi: 10.1016/j.apmr.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 51.Brindle TJ, Mattacola C, McCrory J. Electromyographic changes in the gluteus medius during stair ascent and descent in subjects with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2003;11(4):244–51. doi: 10.1007/s00167-003-0353-z. [DOI] [PubMed] [Google Scholar]
- 52.Geraci MC, Jr., Brown W. Evidence-based treatment of hip and pelvic injuries in runners. Phys Med Rehabil Clin N Am. 2005;16(3):711–47. doi: 10.1016/j.pmr.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 53.Gottschalk F, Kourosh S, Leveau B. The functional anatomy of tensor fasciae latae and gluteus medius and minimus. J Anat. 1989;166:179–89. [PMC free article] [PubMed] [Google Scholar]
- 54.Ochsendorf DT, Mattacola CG, Arnold BL. Effect of orthotics on postural sway after fatigue of the plantar flexors and dorsiflexors. J Athl Train. 2000;35(1):26–30. [PMC free article] [PubMed] [Google Scholar]
- 55.Novick A, Kelley DL. Position and Movement Changes of the Foot with Orthotic Intervention during the Loading Response of Gait. J Orthop Sports Phys Ther. 1990;11(7):301–12. doi: 10.2519/jospt.1990.11.7.301. [DOI] [PubMed] [Google Scholar]
- 56.Eils E, Behrens S, Mers O, Thorwesten L, Volker K, Rosenbaum D. Reduced plantar sensation causes a cautious walking pattern. Gait Posture. 2004;20(1):54–60. doi: 10.1016/S0966-6362(03)00095-X. [DOI] [PubMed] [Google Scholar]
- 57.Riegger-Krugh C, Keysor JJ. Skeletal malalignments of the lower quarter: correlated and compensatory motions and postures. J Orthop Sports Phys Ther. 1996;23(2):164–70. doi: 10.2519/jospt.1996.23.2.164. [DOI] [PubMed] [Google Scholar]
- 58.Trimble MH, Bishop MD, Buckley BD, Fields LC, Rozea GD. The relationship between clinical measurements of lower extremity posture and tibial translation. Clin Biomech (Bristol, Avon) 2002;17(4):286–90. doi: 10.1016/s0268-0033(02)00010-4. [DOI] [PubMed] [Google Scholar]
- 59.Xiong S, Goonetilleke RS, Witana CP, Weerasinghe TW, Au EY. Foot arch characterization: a review, a new metric, and a comparison. J Am Podiatr Med Assoc. 2010;100(1):14–24. doi: 10.7547/1000014. [DOI] [PubMed] [Google Scholar]
- 60.Dickinson MH, Farley CT, Full RJ, Koehl MAR, Kram R, S L. How animals move: an integrative view. Science. 2000;288:100–6. doi: 10.1126/science.288.5463.100. [DOI] [PubMed] [Google Scholar]
- 61.Hafer JF, Lenhoff MW, Song J, Jordan JM, Hannan MT, Hillstrom HJ. Reliability of plantar pressure platforms. Gait Posture. 2013 doi: 10.1016/j.gaitpost.2013.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Riskowski JL, Hagedorn TJ, Dufour AB, Hannan MT. Functional foot symmetry and its relation to lower extremity physical performance in older adults: the Framingham Foot Study. J Biomech. 2012;45(10):1796–802. doi: 10.1016/j.jbiomech.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.