Abstract
Background
Several reports have suggested low bone mineral density (BMD) in patients with adolescent idiopathic scoliosis (AIS). We determined bone mineral status in patients with AIS to evaluate the effect of brace treatment on BMD.
Methods
BMD was measured in 46 patients (mean age, 17.8 ± 4.9 years) with AIS (17 with brace and 29 without brace) by dual-energy X-ray absorptiometry scan and compared the results to an age-matched (mean age, 16.6 ± 3.9 years) control group (n = 54).
Results
The AIS group had significantly lower bone mass at the lumbar spine (Z-score, -1.500 vs. -0.832) and hip (Z-score, -1.221 vs. -0.754) except at the femoral neck. No difference in BMD was found between patients with AIS who used a brace and those who did not.
Conclusions
The results confirmed that BMD was low in AIS patients and it was not affected by brace treatment.
Keywords: Adolescent idiopathic scoliosis, Braces, Osteopenia, Osteoporosis, Anthropometry, Bone mineral density
Idiopathic scoliosis is a three dimensional curvature of the spine with no clear underlying etiology. Adolescent idiopathic scoliosis (AIS) is the single most common form of spinal deformity seen in orthopedic practice affecting children aged 10 years to maturity.
Since Burner et al.1) first reported low bone mineral density (BMD) in patients with AIS in 1982, several studies have evaluated the relationship between osteoporosis and scoliosis in pediatric and adult patients. Most investigators have found that the prevalence of osteoporosis in patients with AIS is much higher than that in the general pediatric and adolescent populations.2,3)
Bone mass increases progressively during childhood, but mainly during adolescence. Approximately 90% of adult bone mass is gained during the first two decades of life.4) The causes of osteoporosis or osteopenia in patients with AIS are unknown and whether poor bone quality is an etiological factor remains controversial.5) We compared bone mineral status in patients with AIS and a control group and evaluated the effect of brace treatment on BMD in these patients.
METHODS
The subjects were patients with AIS (age, 10-30 years, before the estimated age of peak bone mass). The diagnosis of idiopathic scoliosis was confirmed after history taking, a physical examination, and a radiographic evaluation by two senior consulting spine surgeons. Forty-six patients referred to the Chamran University Hospital Clinic for a routine follow-up were included. Patients with congenital, neuromuscular, or metabolic etiologies and those with skeletal dysplasia or endocrine and connective tissue disorders were excluded from the study.
Healthy boys and girls of similar age were recruited from outpatients who were referred to Chamran Clinic with minor trauma of the extremities. All normal controls were physically examined to exclude any hidden scoliosis before enrolling them in the study. Exclusion criteria for the control group were the same as those for the AIS group.
Assessment of Anthropometry
Anthropometric measurements included body height and weight. Body mass index (BMI) was derived from the body weight (kg) divided by the height squared (kg/m2).
Evaluation of Bone Mineral Status
BMD of the lumbar spine (L1-L4) and unilateral proximal femur (neck, Ward's triangle, and greater trochanter) were measured by dual-energy X-ray absorptiometry (DEXA; Hologic, Discovery, QDR series, GE Medical, Milwaukee, WI, USA) in both the patient and control groups.
Statistics
The statistical analysis consisted of two parts: (1) a multivariate analysis of variance was used to compare the BMDs and anthropometric data between patients with AIS and age-matched normal controls; and (2) Pearson correlation analysis was used to evaluate the association between BMD and the anthropometric parameters. A p < 0.05 was considered significant.
RESULTS
Subject Characteristics
Among the 100 subjects included, 46 were in the AIS group and 54 healthy people were in the control group. The AIS group was subdivided into two subgroups: 29 patients were in group 1 (without brace treatment and waiting for operation) and 17 patients were in group 2 (with brace treatment). Patients in group 2 used a brace for at least 6 months prior to the study. A Milwaukee brace was used in 11 patients and the Thoraco-Lumbo-Sacral Orthosis (TLSO; Boston brace) was used in six patients.
Tables 1 and 2 show the distribution of subjects in the AIS and control groups according to chronological age and sex. Mean age was not different between the two groups (17.8 ± 4.9 years vs. 16.6 ± 3.9 years; p > 0.05).
Table 1.
Sex Distribution among the AIS and Control Groups
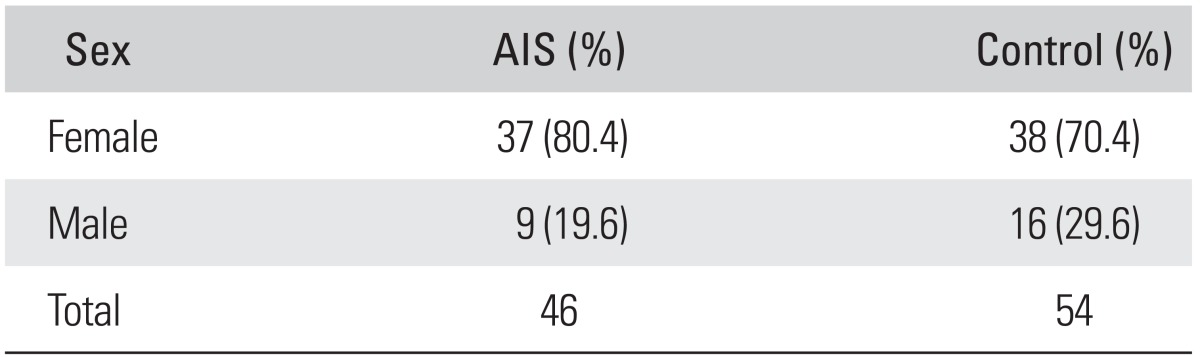
AIS: adolescent Idiopathic scoliosis.
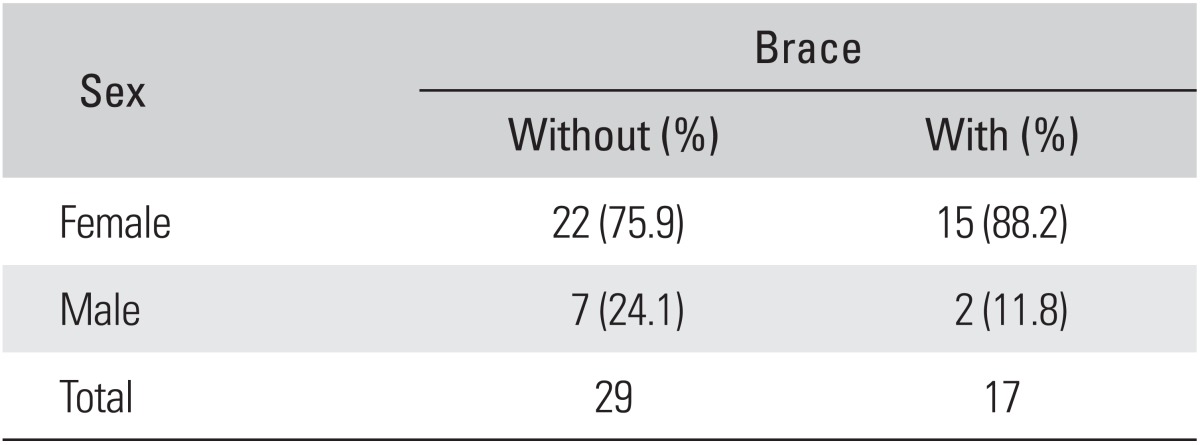
Table 2.
Subject Distribution according to Sex and Use of Brace in the Adolescent Idiopathic Scoliosis Group
Anthropometric Measurements
Mean body weight in the AIS group was 47.07 ± 9.22 kg and that in the control group was 54.22 ± 11.8 kg. Mean height in the AIS group was 158 ± 9.1 cm and that in the control group was 159 ± 7.2 cm. The difference in body weight was significant, but no difference was found in height between the two groups (p < 0.05), explaining why the difference in BMI was significant (Table 3).
Table 3.
Anthropometric Measurements between the AIS and Control Groups
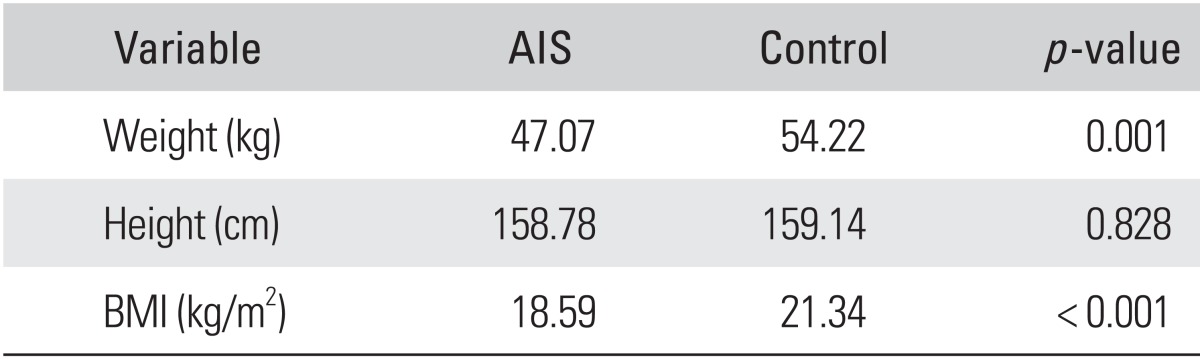
AIS: adolescent Idiopathic scoliosis, BMI: body mass index.
Analysis of the anthropometric data in the AIS group (Table 4) revealed no differences between body weight, height, or BMI in patients with and without brace treatment (p > 0.05).
Table 4.
Anthropometric Data in the AIS Group
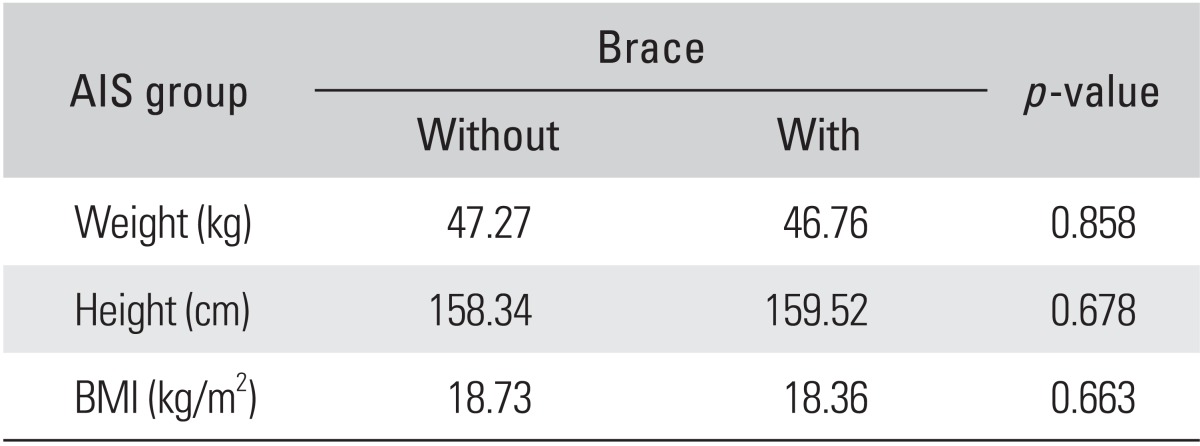
AIS: adolescent idiopathic scoliosis, BMI: body mass index.
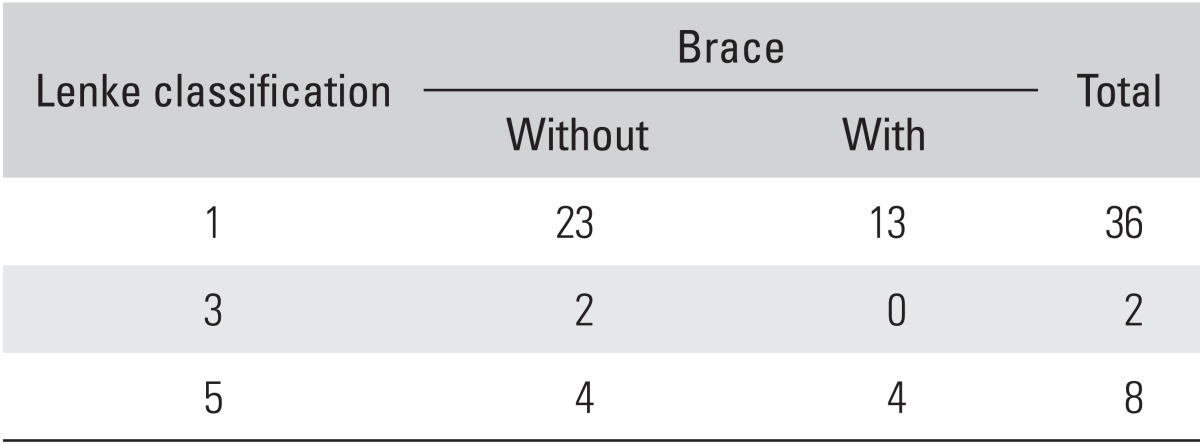
We used the Lenke classification for AIS curves in our patients. Among the 46 patients in the AIS group, 73.9% had right-sided scoliosis (Table 5), and the most common curve type (78.3%) was Lenke type I (Table 6).
Table 5.
Curve Side of Scoliosis
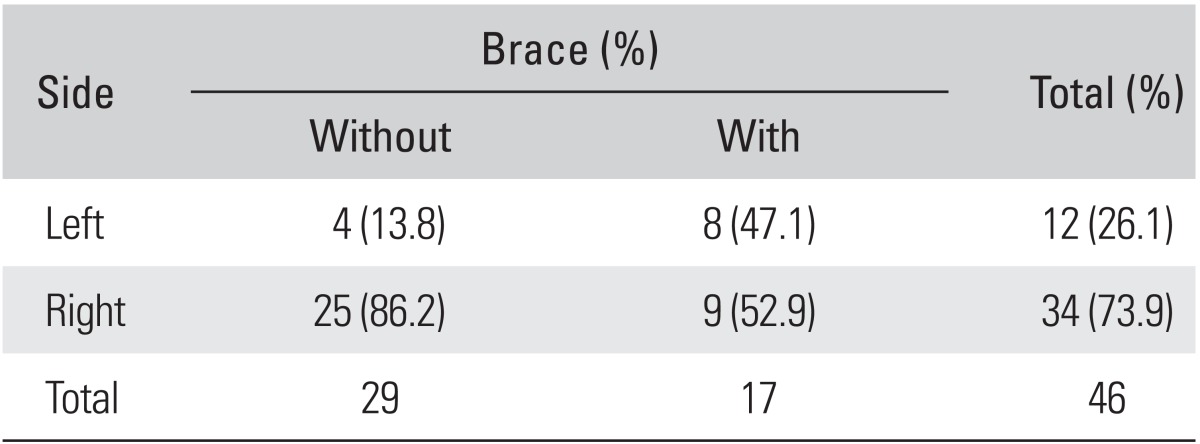
Table 6.
Lenke Classification of the Curve
Low BMD in AIS
All BMD values at the lumbar spine and hip were significantly lower in patients with AIS than those in the control group except at the femoral neck area (Table 7). In addition, a significant difference was found between lumbar spine and hip measurements in the groups. The difference in hip and lumbar spine Z-score values was also significant between the two groups (Table 8).
Table 7.
Comparison of BMD between the AIS and Control Groups
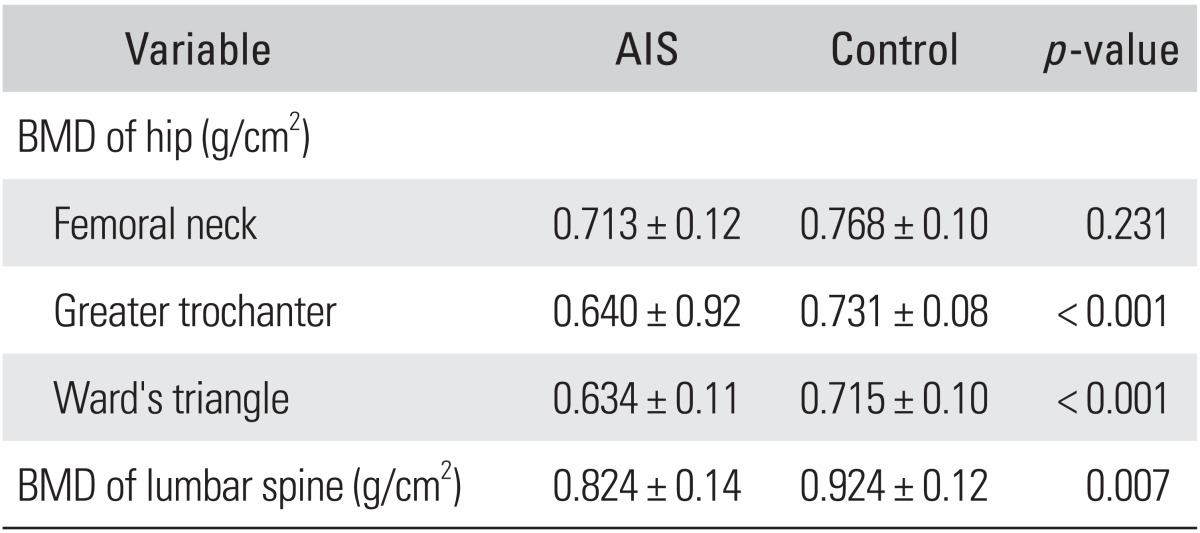
Values are presented as mean ± SD.
BMD: bone mineral density, AIS: adolescent idiopathic scoliosis.
Table 8.
Z-score in the AIS and Control Groups
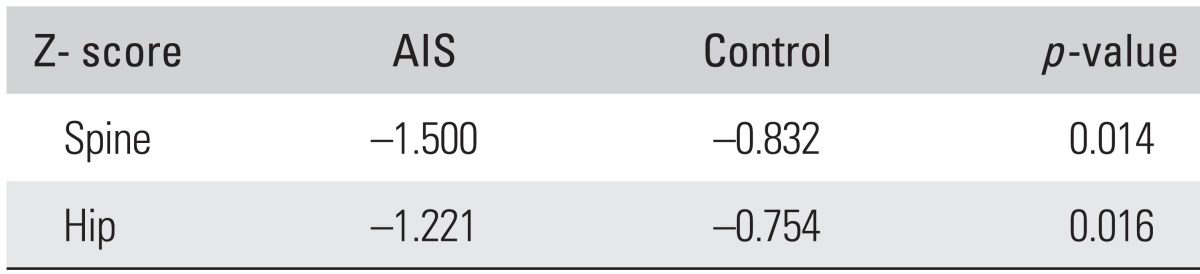
AIS: adolescent idiopathic scoliosis.
Based on lumbar spine Z-score values, osteopenia was found in 37% and osteoporosis in 28.4% of the patients with AIS, which was significantly higher than those in the control group (p < 0.05). The results in the control group were 29.6% and 7.4% respectively (Fig. 1). Osteopenia and osteoporosis in the hip region were also significantly more common in the AIS group than those in the control group (Fig. 2). No difference in BMD was found between patients with AIS who used a brace and those who did not (Table 9).
Fig. 1.
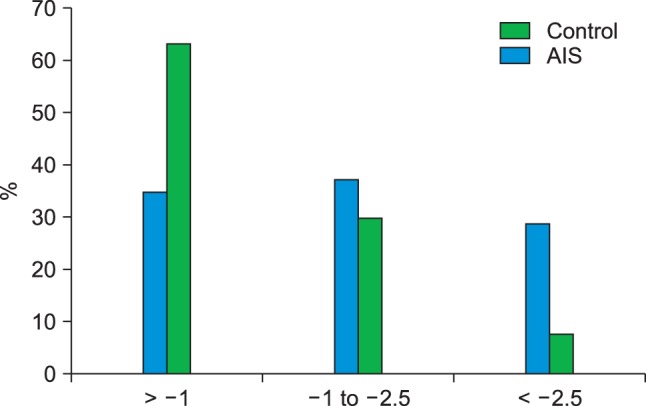
Comparison of Z-score of the lumbar spine between the adolescent idiopathic scoliosis (AIS) and control groups.
Fig. 2.
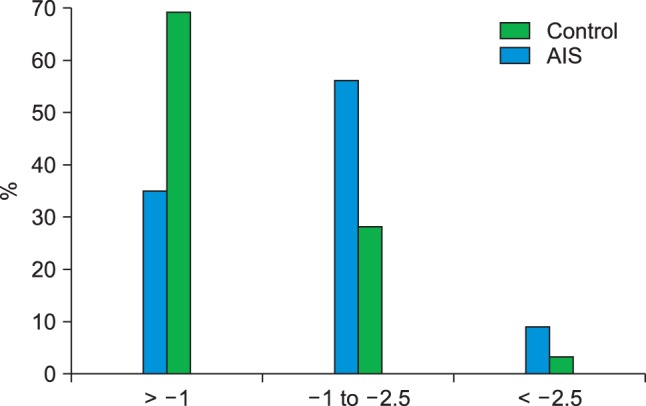
Comparison of the hip Z-score between the adolescent idiopathic scoliosis (AIS) and control groups.
Table 9.
Comparison of BMD between the "Brace" and "No Brace" Groups of Patients with AIS
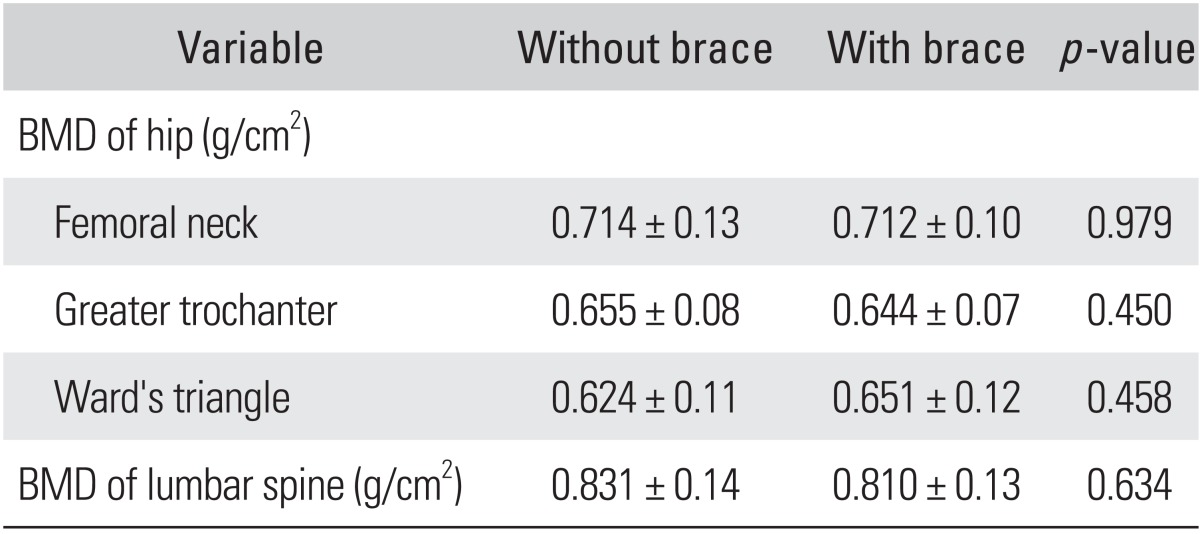
Values are presented as mean ± SD.
BMD: bone mineral density, AIS: adolescent idiopathic scoliosis.
DISCUSSION
Osteoporosis is the most common metabolic bone disorder of adults but is very rare in the young. BMD in children can be affected by body weight, body height, physical activity, or nutritional status.6) Regular exercise significantly increases peak bone mass.7)
Several studies have described the association between osteopenia and spinal deformities in patients with idiopathic scoliosis;8,9,10,11) however, most series consisted of a small number of subjects with poorly documented demographic data, age, and anthropometric parameters.
The causes of osteoporosis or osteopenia in patients with AIS remain unknown and whether poor bone quality in these patients is a primary or secondary cause remains undetermined. Lee et al.12) reported that low calcium intake in patients with AIS may be a contributing factor, whereas Cheung et al.13) suggested that the low bone mass in patients with AIS may result from abnormal bone mineralization and, thus, they fail to catch up with increased bone growth during the peripubertal period.
Several techniques are available to assess bone mineral status such as single-photon absorptiometry, dual photon absorptiometry, DEXA, quantitative computed tomography, and qualitative ultrasound. DEXA is the gold standard because of the low radiation dose (2-5 mrem), wide availability, ease of use, short scan time, high resolution images, good precision (1%-2%), and stable calibration.
The T-score is the number of standard deviations below the average for a young adult at peak bone density, whereas the Z-score is the number of standard deviations below an average person of the same age. According to WHO criteria, osteoporosis is defined as T-score < -2.5 and osteopenia as a T-score from -1 to -2.5. As the study and control group had not reached peak bone mass (30 years), the Z-score was taken for analysis of osteoporosis and osteopenia.
In the present study, BMD of the lumbar spine in 65.4% of the patients with AIS was < -1 standard deviation of the age-matched normal population, while the result in the control group was 37%. We confirmed the correlation between AIS and low bone mineral status in this group of patients. Although patients with AIS had a generally low BMD at different sites, it was interesting to find that BMD of the lumbar spine was less affected than that of the hip in these patients. However, this may, in part, be related to error in the BMD measurement by the DEXA scan, caused by the deformity and axial rotation of the vertebrae, which always occurs in AIS.
Bracing is the most common form of non-invasive treatment for patients with scoliosis at risk for progression. Several investigations have been conducted concerning this issue and formed some conflicting conclusions.14,15,16,17) We found no significant difference in BMD values of the lumbar spine and hip between patients with AIS with brace treatment and those waiting for surgery without a brace.
Do we need to treat osteopenia and osteoporosis in these patients? Would that affect the progress of scoliosis and, from a long-term perspective, the anticipated adult osteoporosis problem? These implications merit more longitudinal controlled research. A follow-up longitudinal study of the nutritional status and physical activity in patients with AIS compared with those in normal controls will be necessary for a better understanding of this phenomenon.
ACKNOWLEDGEMENTS
This study was carried out in Research Center for Bone & Joint Diseases, Department of Orthopedic Surgery, Chamran Hospital, Shiraz University of Medical Sciences, Shiraz, Iran.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Burner WL, 3rd, Badger VM, Sherman FC. Osteoporosis and acquired back deformities. J Pediatr Orthop. 1982;2(4):383–385. doi: 10.1097/01241398-198210000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Li XF, Li H, Liu ZD, Dai LY. Low bone mineral status in adolescent idiopathic scoliosis. Eur Spine J. 2008;17(11):1431–1440. doi: 10.1007/s00586-008-0757-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sadat-Ali M, Al-Othman A, Bubshait D, Al-Dakheel D. Does scoliosis causes low bone mass? A comparative study between siblings. Eur Spine J. 2008;17(7):944–947. doi: 10.1007/s00586-008-0671-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leonard MB, Zemel BS. Current concepts in pediatric bone disease. Pediatr Clin North Am. 2002;49(1):143–173. doi: 10.1016/s0031-3955(03)00113-5. [DOI] [PubMed] [Google Scholar]
- 5.Cheng JC, Leung SS, Lee WT, et al. Determinants of axial and peripheral bone mass in Chinese adolescents. Arch Dis Child. 1998;78(6):524–530. doi: 10.1136/adc.78.6.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng JC, Maffulli N, Leung SS, Lee WT, Lau JT, Chan KM. Axial and peripheral bone mineral acquisition: a 3-year longitudinal study in Chinese adolescents. Eur J Pediatr. 1999;158(6):506–512. doi: 10.1007/s004310051131. [DOI] [PubMed] [Google Scholar]
- 7.Cheng JC, Hung VW, Lee WT, et al. Persistent osteopenia in adolescent idiopathic scoliosis: longitudinal monitoring of bone mineral density until skeletal maturity. Stud Health Technol Inform. 2006;123:47–51. [PubMed] [Google Scholar]
- 8.Cheng JC, Qin L, Cheung CS, et al. Generalized low areal and volumetric bone mineral density in adolescent idiopathic scoliosis. J Bone Miner Res. 2000;15(8):1587–1595. doi: 10.1359/jbmr.2000.15.8.1587. [DOI] [PubMed] [Google Scholar]
- 9.Li XF, Li H, Liu ZD, Dai LY. Low bone mineral status in adolescent idiopathic scoliosis. Eur Spine J. 2008;17(11):1431–1440. doi: 10.1007/s00586-008-0757-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng JC, Guo X, Sher AH. Persistent osteopenia in adolescent idiopathic scoliosis: a longitudinal follow up study. Spine (Phila Pa 1976) 1999;24(12):1218–1222. doi: 10.1097/00007632-199906150-00008. [DOI] [PubMed] [Google Scholar]
- 11.Courtois I, Collet P, Mouilleseaux B, Alexandre C. Bone mineral density at the femur and lumbar spine in a population of young women treated for scoliosis in adolescence. Rev Rhum Engl Ed. 1999;66(12):705–710. [PubMed] [Google Scholar]
- 12.Lee WT, Cheung CS, Tse YK, et al. Generalized low bone mass of girls with adolescent idiopathic scoliosis is related to inadequate calcium intake and weight bearing physical activity in peripubertal period. Osteoporos Int. 2005;16(9):1024–1035. doi: 10.1007/s00198-004-1792-1. [DOI] [PubMed] [Google Scholar]
- 13.Cheung CS, Lee WT, Tse YK, et al. Generalized osteopenia in adolescent idiopathic scoliosis: association with abnormal pubertal growth, bone turnover, and calcium intake? Spine (Phila Pa 1976) 2006;31(3):330–338. doi: 10.1097/01.brs.0000197410.92525.10. [DOI] [PubMed] [Google Scholar]
- 14.Cook SD, Harding AF, Morgan EL, et al. Trabecular bone mineral density in idiopathic scoliosis. J Pediatr Orthop. 1987;7(2):168–174. doi: 10.1097/01241398-198703000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Thomas KA, Cook SD, Skalley TC, et al. Lumbar spine and femoral neck bone mineral density in idiopathic scoliosis: a follow-up study. J Pediatr Orthop. 1992;12(2):235–240. doi: 10.1097/01241398-199203000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Snyder BD, Katz DA, Myers ER, Breitenbach MA, Emans JB. Bone density accumulation is not affected by brace treatment of idiopathic scoliosis in adolescent girls. J Pediatr Orthop. 2005;25(4):423–428. doi: 10.1097/01.bpo.0000158001.23177.8d. [DOI] [PubMed] [Google Scholar]
- 17.Sun X, Qiu Y, Zhu Z. The accumulation of bone mineral content and density in idiopathic scoliotic adolescents treated with bracing. Stud Health Technol Inform. 2006;123:233–238. [PubMed] [Google Scholar]


