Abstract
Purpose
We developed and tested a multi-modal intervention, delivered in the home health care setting, aimed at increasing osteoporosis treatment rates to prevent fractures.
Material and Methods
The intervention focused on home health nurses. Key components included: nursing education; development of a nursing care plan; patient teaching materials and creation of physician materials. Nursing education consisted of a lecture covering osteoporosis, fracture risks and prevention, and the effectiveness of anti-osteoporosis treatment options. Patients received education materials concerning osteoporosis and anti-osteoporosis medications. A pocket-sized treatment algorithm card and standardized order sets were prepared for physicians. Focus groups of physicians and nurses were conducted to obtain feedback on the materials and methods to facilitate effective nurse-physician communication. Successful application required nurses to identify patients with a fracture history, initiate the care plan, prompt physicians on risk status, and provide patient education. The intervention was piloted in one field office.
Results
In the year prior to the intervention, home health patients (n=92) with a fracture history were identified in the pilot field office and only 20 (22%) received osteoporosis prescription therapy. In the three months following the intervention, 21 newly enrolled patients were identified and 9 (43%) had received osteoporosis prescription medications.
Conclusions
Home health care provides a venue where patients and physicians can be informed by nurses about osteoporosis and fracture risks and, consequently, initiate appropriate therapy. This multi-modal intervention is easily transportable to other home health agencies and adaptable to other medical conditions and settings.
Keywords: osteoporosis, home health, fracture, dissemination, cluster randomized trial, patient education
1. Introduction
Osteoporosis is a major public health problem worldwide that contributes to more than 2 million fractures each year in the United States alone [1]. Not only are fractures associated with a loss of mobility, but up to 22% of women and 33% of men with a hip fracture will not live a full year [2] and approximately 44% of survivors will suffer a second fracture within five years [3]. Despite guidelines from the National Osteoporosis Foundation (NOF)a to consider United States Food and Drug Administration approved medical therapies in postmenopausal women and men aged 50 years and older following a hip or vertebral fracture [4] and evidence that these therapies have been shown to decrease fracture risk in patients who have had fragility fractures [5-16], studies have shown that only 3-32% of patients receive any osteoporosis care after sustaining a hip fracture [17-21].
Half of the Medicare patients discharged from the hospital after a hip fracture receive home health care services [22], and this may provide an excellent setting for secondary fracture prevention through the receipt of anti-osteoporosis medications known to reduce recurrent fractures [5-16, 23]. Although the opportunity to intervene through home health programs appears great, few studies have focused on this setting. Through our ongoing partnership with a state-wide home health care agency admitting over 8,000 home health patients per year, we found that only 17% of persons newly enrolled in home health after discharge from a hip fracture received secondary prevention measures for osteoporosis in the form of anti-osteoporosis medications [17]. Further, other studies have documented the difficulty of increasing appropriate physician prescribing of osteoporosis medications. Studies of physician-based interventions to improve osteoporosis care conducted in different settings revealed only small effects, at best [24-26]. Thus, we need new health system approaches to improve quality of care in this challenging clinical area, where even approaches as widely accepted as case management have not yet been proven [27]. This paper reports on the development of an intervention designed to improve osteoporosis care in a home health setting and the findings from the pilot testing of the intervention. We also describe our plans for a future large scale evaluation of the intervention to be implemented in multiple home health agencies.
This project employed a multi-modal approach to improve osteoporosis care for home care patients at high risk for fractures. Specifically, we developed a high-intensity intervention aimed at increasing receipt of anti-osteoporosis medications in the home health care setting and pilot tested the intervention in one home health office. The intervention includes: (1) training and development of materials to enhance nurse-patient and nurse-physician risk communication; (2) development of standard care pathways incorporated into the home health agency’s electronic medical record (EMR) system (Homecare Homebase, LP, Dallas, TX); (3) and creation of standardized physician order sets (i.e. dietary supplements and prescription anti-osteoporosis medications) accompanied by a pocket-sized treatment algorithm card. In developing our intervention, we were mindful that home health nurses were the key to success.
2. Material and methods
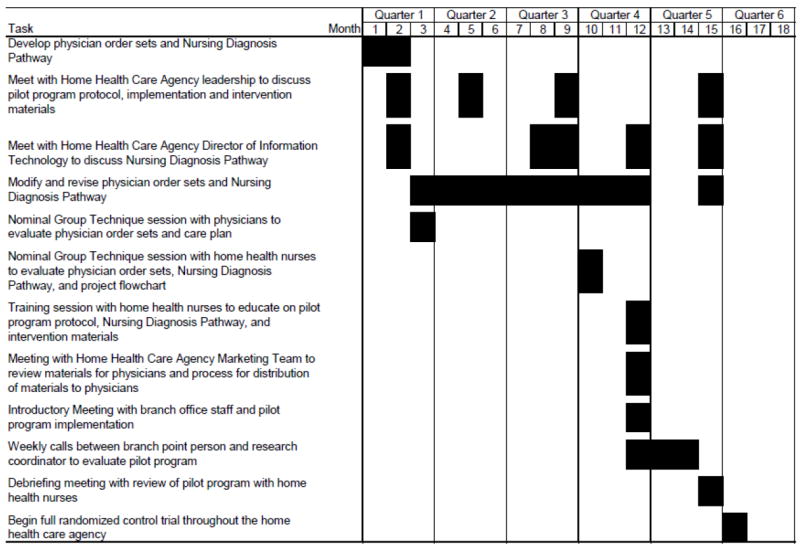
The following sections and Figure 2 provide information on the timing and steps of the development and implementation of the pilot program and the intervention components used. To minimize cost and start up time, we used existing materials (i.e. treatment algorithm card) or modified materials already used by the home health care agency or practicing physicians (i.e. standardized order sets) for each intervention component. This had the added benefit of increasing efficiency of implementation as the home health care agency staff had some familiarity with the intervention components prior to implementation. Over the pilot project period of 15 months, the commitment from the research coordinator was approximately 20% full time equivalent; four project investigators contributed an additional 5-10% full time equivalent for this same period of time.
Fig. 2.
2.1. Intervention development
The intervention was developed in partnership between university researchers and Alacare Home Health and Hospice, Inc. (Birmingham, AL), a private, not-for-profit, Medicare-certified home health agency with offices throughout Alabama admitting over 8,000 patients referred annually by over 3,500 rural and urban physicians. Of particular note, the agency utilizes an EMR that captures detailed information on diagnoses, over-the counter and prescription medications, and nurses’ clinical assessments and progress notes. The EMR is used by 150 home health providers in 17 states (Homecare Homebase, LP, Dallas, TX).
A key component of the intervention was to educate home health nurses about osteoporosis and fragility fractures and also about the availability and effectiveness of preventive therapies. The intervention prepared nurses to interact with patients as health educators and with physicians as patient advocates. In the former role, the nurse used the standardized care pathways to educate and inform their patients. In the latter role, the nurse used a pocket-sized treatment algorithm card (Appendix 1) and standardized order sets (Appendix 2) as tools to promote appropriate physician prescribing consistent with national osteoporosis guidelines [28-29]. The overarching goal was to bring nurses and physicians to the understanding that the presence of a fragility fracture (in the absence of cancer or other conditions that would not require traditional osteoporosis treatments) was diagnostic for osteoporosis, and treatment should be considered without the need to conduct further testing, which may be inconvenient for home care patients.
2.2. Integration of the intervention into standard care
The typical patient sequence of care is outlined in Figure 1. Once a patient was referred to the home health agency, the home health nurse completed a comprehensive intake assessment and created a care plan. After the intake assessment, patient care plans are uploaded to the EMR and must be approved by a quality assurance (QA) nurse assigned to each branch office. To ensure that appropriate care plans are activated for each patient, the QA nurse either approved or rejected each aspect of the care plan based on its appropriateness for the patient. Once approved, the home health nurse then carried out the care plan over the subsequent in-home care visits. At the same time, the treating physician was sent the care plan and standardized order sets, as indicated.
Fig. 1.
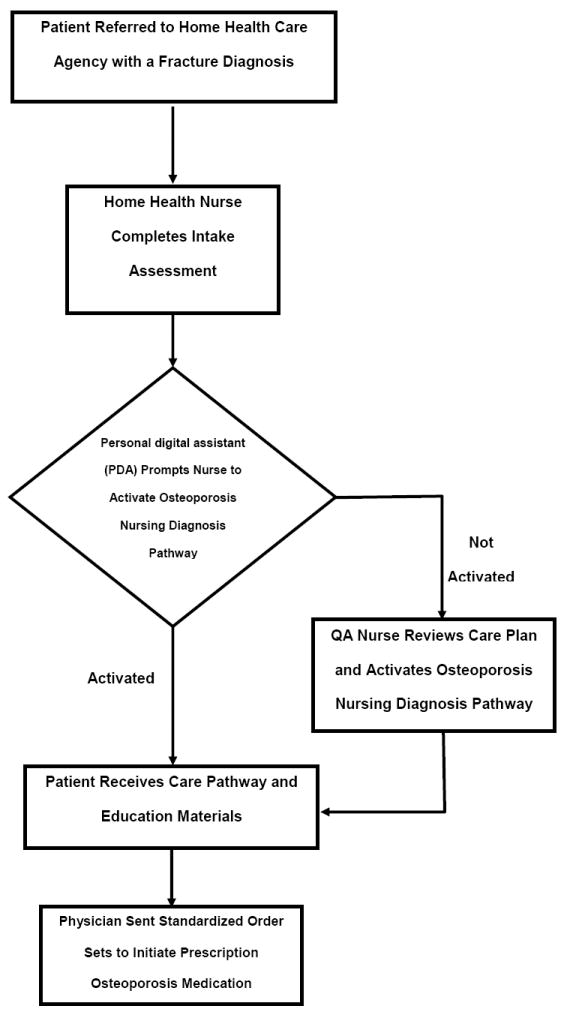
For our program, home health nurses first identified patients at high risk for fracture and activated a Nursing Diagnosis Pathway (NDP) focused on osteoporosis care that included patient education information such as risk factors for osteoporosis (Appendix 3). The QA nurse would confirm that the patient had a fracture ICD-9 diagnosis code (733.1x, 800 – 829) and ensure that the osteoporosis NDP was activated as part of the care plan.
2.3. Preliminary steps
2.3.1 Home health nurse and physician Input
Nominal Group Technique (NGT) sessions were used to develop the process and materials for improving nurse-patient and nurse-physician communication. NGT fosters creativity by helping group members articulate meaningful responses to targeted questions, avoiding the ambiguity common in unstructured discussions [30-31]. After developing draft intervention components, project investigators (MLK, JRC) and the research coordinator (RO) conducted separate one hour NGT sessions with a group of 15 home health nurses and with a group of 10 physicians who refer patients for home health care. Prior to their NGT session, home health nurses received continuing education credits for attending a thirty minute educational talk on osteoporosis. Physicians were compensated with a $250 honorarium for their participation. During each NGT session, all intervention components—NDP, nurse-patient communication, nurse-physician communication, standardized order sets—were reviewed and refined following the principles of usability testing” [32].
2.3.2. Nurse Education and Training
Prior to implementing the pilot program, we conducted a training session with the home health nurses. The training session lasted approximately one hour and occurred at the branch office during the weekly team meeting. The training session included detailed information on the evidence regarding the prevalence of osteoporosis, fracture risks and sequelae, and fracture prevention measures, including use of prescription drugs. Training also addressed how to convey the patients’ risk for future fracture and need for fracture prevention to both patients and physicians. Nurses were trained and provided with supporting evidence from the medical literature to answer physician questions regarding fracture risks, treatment thresholds, national osteoporosis management guidelines, and medication orders. This aspect of the intervention prepared the nurse to better communicate the risks and benefits of osteoporosis treatment to patients, thus promoting initial acceptance and sustained adherence to treatment, improving patient (or caregiver) understanding, and increasing the ability of patients to communicate with their physicians about osteoporosis.
2.3.3. Development of a Nursing Diagnosis Pathway (NDP)
We worked closely with the home health care agency’s Director of Information Technology to build our NDP on the existing template used by the agency for all of their NDPs. This allowed us to implement our NDP immediately at no cost and required no additional training of nurses to familiarize them with the general layout of our NDP. Implementation only required for the home health nurse to reboot her hand held device used to access all NDPs. The NDP was a plan of care contained within the EMR and activated for patients identified as being at high risk because of a prior fracture. The NDP outlined steps to be taken by nurses to reduce fracture risks (Appendix 3). First, the nurse determined whether the patient was currently taking medications for osteoporosis. If so, the NDP provided information concerning the medication and how it is taken that is to be communicated to patients with learning objectives specified. For example, a patient prescribed an oral bisphosphonate medication was taught to take the medicine first thing in the morning with a full glass of water, 30 minutes prior to eating or drinking anything. They were also instructed to not lie down for a minimum of 30 minutes after taking the pill. The learning objective was for the patient to provide verbal understanding (i.e. correctly repeat back the instructions to the nurse). If the patient was not on medication, then the NDP called for notification of the physician and provision of standardized order sets to facilitate the physician’s choice of treatment. In either case, the NDP detailed a set of learning objects related to osteoporosis including verbal understanding of (1) what osteoporosis is, (2) what causes weak bones, (3) predictors of osteoporosis, (4) ways to prevent bone loss and fractures, (5) sources of calcium and vitamin D, and (6) how and what to discuss with their physician.
2.3.4. Development of Patient Education Materials
The primary material for patient teaching was the free pamphlet, prepared by the US Department of Health and Human Services, The Surgeon General’s Report on Bone Health and Osteoporosis: What It Means To You [33]. The learning objectives in the NDP were tailored to reflect information in the report. Secondly, nurses discussed strategies for patients to use in discussing bone health and prevention with their physicians. The basis of this patient education was the techniques described in —How to Talk to Your Doctor” [34-37]. An initial supply was provided to the branch office by the research coordinator. Pamphlets were re-ordered as needed by the research coordinator.
2.3.5. Development of Physician Materials
Using feedback received from the NGT sessions with both home health nurses and physicians, we developed standardized order sets for both prescription anti-osteoporosis medications and calcium and vitamin D supplements (Appendix 2). To increase familiarity for the prescribing physician and home health nurse, the layout of each order sheet was based on a standard prescription pad. Furthermore, the order sets were designed to minimize the time obligation for physicians while providing all available options for osteoporosis medication. Medications were grouped by route of administrations and presented in alphabetical order. A check box was located next to each medication allowing physicians to simply check which medication they would like to prescribe. The sets also included instructions on faxing the orders to either the patient’s pharmacy or the home health care branch where the patient was receiving care.
The order sets were developed to assist physicians to tailor a customized, specific osteoporosis management plan without preference to any particular prescription medication. Recommended options include prescription medications approved to treat osteoporosis, vitamin D and calcium supplements, and other measures aimed at fracture prevention (e.g., hip protectors, fall risk assessment and mitigation). Although a variety of osteoporosis care options are presented and could be customized for each patient, the default pathway, based on national osteoporosis performance measures included receipt of an anti-osteoporosis prescription medication, calcium, and vitamin D [28, 38-39]. Order sets were printed at the branch office as needed.
Physicians also received a previously developed pocket treatment card (Appendix 1) that included a treatment algorithm and frequently asked questions related to treating patients with a history of a fracture in the home health care setting [40]. This pocket card along with an article that explained the rationale behind the treatment algorithm was distributed to physicians in the community who referred patients to home health care. These cards were supplied to the home health care agency by the research coordinator. The distribution to physicians occurred at the time of intervention implementation, and was carried out by the home health care agency marketing team members that routinely met with the physicians treating the home health patients.
2.4. Pilot program implementation
One branch office was designated as the pilot location. A one hour introductory meeting was held with all of the branch personnel that would be involved with the project (home health nurses, marketing team, branch manager, quality assurance nurse). The first thirty minutes of the meeting included information on preventing recurrent fractures in home health care patients and was presented by project investigators (JC, JLL, and MLK). The second half of the meeting consisted of an overview of the research process, the intervention program, a review of the intervention components including the nursing diagnosis pathway, and time for questions and answers. Initial feedback from home health care agency personnel led to slight modifications to the physician order sets. With the assistance of the branch manager, we developed plans for contacting physicians and tracking patients from the branch. The branch manager also assigned a mid-level nurse manager as point person to oversee the implementation and maintenance of the pilot program. This point person spent 2-2 ½ hours each week tracking patients, ensuring that the NDP was activated, and following up with the physician office if order sets were not returned.
Following the introductory meeting, the research coordinator (RO) contacted the branch point person every two weeks for a fifteen minute telephone meeting to obtain a status update and discuss any problems with the program. When problems occurred, the project investigators were informed and decided on a resolution. These discussions also led to additional modifications to the standardized order sets.
Three months after the introductory meeting, project investigators held a second one hour meeting with the pilot branch personnel to discuss what aspects of the program were working and what areas needed improvement. Home health nurses had successfully implemented the care pathway for all patients with a history of fractures and the point person had faxed the order sets to the referring physicians. At the completion of the three month pilot period, branch personnel had no additional recommendations for modifications of the process or the materials.
3. Pilot Study Findings
To evaluate the efficacy of the pilot intervention, we first identified all patients with a fracture diagnosis (i.e. 733.1x, 800.x-829.x) from the EMR in the home health care agency’s data warehouse. We then examined de-identified data including the past use, initiation, and (if relevant), discontinuation of bisphosphonates identified using National Drug Codes and drug name, vitamin D, and calcium supplements for the period(s) patients were in home care. The main outcome of interest was receipt of anti-osteoporosis medication while enrolled in home health care. We conducted a simple comparison of medication prescription rates the three months before and the three months after the intervention was implemented, using Fishers exact tests to assess statistical significance and t-Tests for difference in proportions to determine confidence intervals. Results from our pilot test can be seen in Table 1. The differences between before and after pilot period proportions for use of anti-osteoporosis medications and for calcium and vitamin D supplements (Table 1) were 22% (95% CI 0%-44%, p < 0.05) and 31% (95% CI 9%-51%, p < 0.001) respectively.
Table 1.
Results from pilot study.
| Time Period | Fracture Diagnoses N | Prescribed OP Drug N (%) | Calcium and/or Vitamin D N (%) |
|---|---|---|---|
| 2007a (pre-intervention) | 92 | 20 (21) | 11 (12) |
| 12/2008 – 2/2009a (post-intervention) | 21 | 9 (43) | 9 (43) |
At single branch office where intervention was piloted
4. Discussion and conclusion
4.1. Discussion
This project addresses the very significant public health problem of osteoporosis related fractures faced by vulnerable older adults in an understudied health care setting. While a reduction in fractures is the ultimate goal of all osteoporosis interventions, increasing the rates of guideline-recommended process of care measures, specifically the receipt of prescription anti-osteoporosis therapies, serves as the endpoint in this pilot study. Due to the limited sample size and follow up time it was beyond the scope of this pilot program to study fracture outcomes. However, results from clinical trials [5-16] indicate that changes in the osteoporosis care process (i.e., treatment with osteoporosis agents) result in a significant reduction in fracture outcomes. Our work builds on the federal mandate prompted by the Institute of Medicine to improve continuity of care and improve communications among providers [41], as is now promulgated as an osteoporosis performance indicators that was developed by the American Medical Associations Physician Consortium [28], approved by Ambulatory Quality Alliance [38], and now part of the Centers for Medicare & Medicaid Services Physician Voluntary Reporting Program [39]. Given previous work demonstrating the difficulty in improving physician-directed osteoporosis practice patterns [24-26] and the absence of studies testing practice improvement interventions in the home health setting, we chose to test a high-intensity intervention versus usual care. Our project is unique in that the focus of our intervention was the home health nurse. We engaged a team of experienced, multidisciplinary researchers. Our first priority was to design a comprehensive integrated intervention with the greatest likelihood of producing meaningful public health improvement in a novel setting, for osteoporosis where there are proven treatments that are currently very poorly utilized [28]. Simplification of participation on the part of all providers, but especially physicians, may be a key factor in increased implementation of evidence based practices.
While we successfully increased receipt of anti-osteoporosis medications, there were a few challenges that occurred during the piloting of the program. One ongoing challenge was staff turnover. New nurses had to be informed of the program and instructed on what their role was. This “training” fell to the branch point person and nurse managers adding to their existing workload. An alternative approach for future incarnations would be a training tool kit with a DVD and manual that would be provided to each new staff member.
A second challenge was assuring the receipt of materials and order sets by the prescribing physician. Based on feedback from the nurses and the branch point person, we quickly realized that one universal approach would not suffice for the various physicians. For example, some physicians requested the materials by fax while other requested them be delivered in person by the marketing team or field nurse. Consequently, the branch point person had to maintain each physician’s preference has part of her tracking of each patient.
4.2. Conclusion
Since the intervention materials are not agency or health system specific, this multi-modal intervention should be easily transportable to other home health agencies. Furthermore, we developed the materials so that they can be quickly modified thereby making them adaptable to other medical conditions and settings. We experienced this first hand as order sets were modified in the field based on physician preference. To help with implementing in other health care settings, we will develop a training manual and tool kit that will be made freely available through the national Center for Education and Research on Therapeutics (CERTs) network and part of the Nursing Communication Seminar. This will also help address the challenge of staff turnover described earlier.
In addition to the training manual and tool kit, the automated reminders and standardized order sets will be built upon the Homecare Homebase Electronic Health Record, which is used by over 150 home health care agencies throughout the nation. If proven effective, the Homecare Homebase leadership is enthusiastic about promoting wide-spread dissemination of the intervention. Finally, we will prepare executive summaries suitable for distribution through the National CERTs websites, the Education and Dissemination Core, the American Society of Health-System Pharmacists, the National Association for Home Health and Hospice, and the Deep South Musculoskeletal CERTs partners.
We are currently conducting a group-randomized trial to evaluate our intervention on a larger scale. The unit of intervention and the unit of randomization is the regional home health office and the unit of observation is the patient. Home health offices have been randomly assigned to receive either the intervention, or to continue current standard operations. Randomization was stratified by baseline treatment rates and the number of eligible patients. The study is ongoing.
Supplementary Material
Acknowledgments
This work was supported in part by the Agency for Healthcare Research and Quality, (AHRQ) Centers for Education and Research on Therapeutics cooperative agreement [U18-HS016956].
Footnotes
Abbreviations: CERTs, Centers for Education & Research on Therapeutics; EMR, electronic medical record; NDP, nursing diagnosis pathway; NGT, nominal group technique; NOF, National Osteoporosis Foundation; QA, quality assurance
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ryan C. Outman, Email: routman@uab.edu.
Jeffrey R. Curtis, Email: jcurtis@uab.edu.
Julie L. Locher, Email: jlocher@uab.edu.
Jeroan J. Allison, Email: Jeroan.Allison@umassedu.edu.
Kenneth G. Saag, Email: ksaag@uab.edu.
Meredith L. Kilgore, Email: mkilgore@uab.edu.
Reference List
- 1.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–75. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 2.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–9. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Curtis JR, Arora T, Matthews RS, Taylor A, Becker DJ, Colon-Emeric C, et al. Is withholding osteoporosis medication after fracture sometimes rational? A comparison of the risk for second fracture versus death. J Am Med Dir Assoc. 2010;11:584–91. doi: 10.1016/j.jamda.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Osteoporosis Foundation. [October 28, 2010];Fast Facts. http://www.nof.org/node/40.
- 5.Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, et al. Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int. 2000;11:83–91. doi: 10.1007/s001980050010. [DOI] [PubMed] [Google Scholar]
- 6.Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–41. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 7.McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, et al. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med. 2001;344:333–40. doi: 10.1056/NEJM200102013440503. [DOI] [PubMed] [Google Scholar]
- 8.Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799–809. doi: 10.1056/NEJMoa074941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA. 1999;282:1344–52. doi: 10.1001/jama.282.14.1344. [DOI] [PubMed] [Google Scholar]
- 10.Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282:637–45. doi: 10.1001/jama.282.7.637. [DOI] [PubMed] [Google Scholar]
- 11.Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–65. doi: 10.1056/NEJMoa0809493. [DOI] [PubMed] [Google Scholar]
- 12.Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA. 1998;280:2077–82. doi: 10.1001/jama.280.24.2077. [DOI] [PubMed] [Google Scholar]
- 13.McClung MR, Wasnich RD, Recker R, Cauley JA, Chesnut CH, 3rd, Ensrud KE, et al. Oral daily ibandronate prevents bone loss in early postmenopausal women without osteoporosis. J Bone Miner Res. 2004;19:11–8. doi: 10.1359/JBMR.0301202. [DOI] [PubMed] [Google Scholar]
- 14.Chesnut CH, 3rd, Silverman S, Andriano K, Genant H, Gimona A, Harris S, et al. A randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: the prevent recurrence of osteoporotic fractures study. PROOF Study Group. Am J Med. 2000;109:267–76. doi: 10.1016/s0002-9343(00)00490-3. [DOI] [PubMed] [Google Scholar]
- 15.Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–41. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 16.Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–22. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 17.Curtis JR, Kim Y, Bryant T, Allison J, Scott D, Saag KG. Osteoporosis in the home health care setting: A window of opportunity? Arthritis Care Res. 2006;55:971–5. doi: 10.1002/art.22349. [DOI] [PubMed] [Google Scholar]
- 18.Feldstein A, Elmer PJ, Orwoll E, Herson M, Hillier T. Bone mineral density measurement and treatment for osteoporosis in older individuals with fractures: a gap in evidence-based practice guideline implementation. Arch Intern Med. 2003;163:2165–72. doi: 10.1001/archinte.163.18.2165. [DOI] [PubMed] [Google Scholar]
- 19.Solomon DH, Finkelstein JS, Katz JN, Mogun H, Avorn J. Underuse of osteoporosis medications in elderly patients with fractures. Am J Med. 2003;115:398–400. doi: 10.1016/s0002-9343(03)00357-7. [DOI] [PubMed] [Google Scholar]
- 20.Andrade SE, Majumdar SR, Chan KA, Buist DS, Go AS, Goodman M, et al. Low frequency of treatment of osteoporosis among postmenopausal women following a fracture. Arch Intern Med. 2003;163:2052–7. doi: 10.1001/archinte.163.17.2052. [DOI] [PubMed] [Google Scholar]
- 21.Majumdar SR. Recent trends in osteoporosis treatment after hip fracture: improving but wholly inadequate. J Rheumatol. 2008;35:190–2. [PubMed] [Google Scholar]
- 22.Berg K, Intrator O. Postacute care following stroke or hip fracture: single services and combinations used by Medicare beneficiaries (1987-1992) J Aging Health. 1999;11:27–48. doi: 10.1177/089826439901100102. [DOI] [PubMed] [Google Scholar]
- 23.Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, et al. Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab. 2000;85:4118–24. doi: 10.1210/jcem.85.11.6953. [DOI] [PubMed] [Google Scholar]
- 24.Curtis JR, Westfall AO, Allison J, Becker A, Melton ME, Freeman A, et al. Challenges in improving the quality of osteoporosis care for long-term glucocorticoid users: a prospective randomized trial. Arch Intern Med. 2007;167:591–6. doi: 10.1001/archinte.167.6.591. [DOI] [PubMed] [Google Scholar]
- 25.Colon-Emeric CS, Lyles KW, House P, Levine DA, Schenck AP, Allison J, et al. Randomized trial to improve fracture prevention in nursing home residents. Am J Med. 2007;120:886–92. doi: 10.1016/j.amjmed.2007.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grimshaw J, Eccles M, Tetroe J. Implementing clinical guidelines: current evidence and future implications. J Contin Educ Health Prof. 2004;24(Suppl 1):S31–7. doi: 10.1002/chp.1340240506. [DOI] [PubMed] [Google Scholar]
- 27.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Affairs (Millwood) 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 28.National Committee for Quality Assurance. State of Health Care Quality 2009 Report. [March 31, 2011];National Committee for Quality Assurance. 2009 Available from: http://www.ncqa.org/tabid/836/Default.aspx.
- 29.MacLean C, Newberry S, Maglione M, McMahon M, Ranganath V, Suttorp M, et al. Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med. 2008;148:197–213. doi: 10.7326/0003-4819-148-3-200802050-00198. [DOI] [PubMed] [Google Scholar]
- 30.Delbecq AL, Van den Ven AH, Gustafson DH. Group Techniques for Program Planning: A Guide to Nominal Group and Delphi Processes. Glenview, IL: Scott Foresman; 1975. [Google Scholar]
- 31.Miller D, Shewchuk R, Elliot TR, Richards S. Nominal group technique: a process for identifying diabetes self-care issues among patients and caregivers. Diabetes Educ. 2000;26:305–10. 12, 14. doi: 10.1177/014572170002600211. [DOI] [PubMed] [Google Scholar]
- 32.Nielsen J, Mack R. Usability Inspection Methods. New York: John Wiley & Sons; 1994. [Google Scholar]
- 33.U.S. Department of Health and Human Services. Office of the Surgeon General: US Department of Health and Human Services. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General; 2004. The 2004 Surgeon General’s Report on Bone Health and Osteoporosis: What it means to you. [Google Scholar]
- 34.Street RL., Jr Information-giving in medical consultations: the influence of patients’ communicative styles and personal characteristics. Soc Sci Med. 1991;32:541–8. doi: 10.1016/0277-9536(91)90288-n. [DOI] [PubMed] [Google Scholar]
- 35.Street RL. Communicative styles and adaptations in physician-parent consultations. Soc Sci Med. 1992;34:1155–63. doi: 10.1016/0277-9536(92)90289-3. [DOI] [PubMed] [Google Scholar]
- 36.Street RL, Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: why some patients are more involved than others. Med Care. 2005;43:960–9. doi: 10.1097/01.mlr.0000178172.40344.70. [DOI] [PubMed] [Google Scholar]
- 37.Street RL, Jr, Voigt B, Geyer C, Jr, Manning T, Swanson GP. Increasing patient involvement in choosing treatment for early breast cancer. Cancer. 1995;76:2275–85. doi: 10.1002/1097-0142(19951201)76:11<2275::aid-cncr2820761115>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 38.Ambulatory Care Quality Alliance. Compendium of Approved Performance Measures. [March 31, 2011];2010 Available from: http://www.aqaalliance.org/files/CompendiumofApprovedMeasures08182009.doc.
- 39.Centers for Medicare & Medicaid Services. Physician Quality Reporting Initiative. [March 31, 2011];Centers for Medicare & Medicaid Services. 2009 Available from: http://www.cms.hhs.gov/pqri/
- 40.Warriner AH, Outman RC, Saag KG, Berry SD, Colon-Emeric C, Flood KL, et al. Management of osteoporosis among home health and long-term care patients with a prior fracture. South Med J. 2009;102:397–404. doi: 10.1097/SMJ.0b013e31819bc1d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McClellan MB, McGinnis JM, Nabel EG, Olsen LM. Evidence-Based Medicine and the Changing Nature of Health Care. Washington, D. C.: The National Academies Press; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


