Abstract
The clinical manifestations of asthma are caused by obstruction of the conducting airways of the lung. Two airway cell types are critical for asthma pathogenesis: epithelial cells and smooth muscle cells. Airway epithelial cells, which are the first line of defense against inhaled pathogens and particles, initiate airway inflammation and produce mucus, an important contributor to airway obstruction. The other main cause of airway obstruction is contraction of airway smooth muscle. Complementary experimental approaches involving cultured cells, animal models, and human clinical studies have provided many insights into diverse mechanisms that contribute to airway epithelial and smooth muscle cell pathology in this complex disease.
Introduction
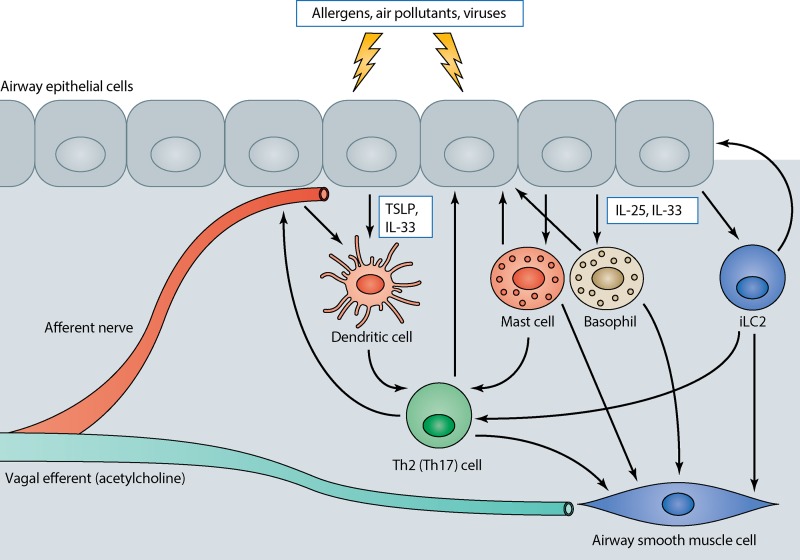
Asthma is a common disease that affects up to 8% of children in the United States (Moorman et al., 2007) and is a major cause of morbidity worldwide. The principal clinical manifestations of asthma are repeated episodes of shortness of breath and wheezing that are at least partially reversible, recurrent cough, and excess airway mucus production. Because asthma involves an integrated response in the conducting airways of the lung to known or unknown triggers, it is a multicellular disease, involving abnormal responses of many different cell types in the lung (Locksley, 2010). Here we focus on the two cell types that are ultimately responsible for the major symptomatic pathology in asthma—epithelial cells that initiate airway inflammation in asthma and are the source of excess airway mucus, and smooth muscle cells that contract excessively to cause symptomatic airway narrowing. The current thinking about cell–cell communications that drive asthma (Fig. 1) is that known and unknown inhaled stimuli (i.e., proteases and other constituents of inhaled allergens, respiratory viruses, and air pollutants) stimulate airway epithelial cells to secrete the cytokines TSLP, interleukin (IL)-25, and IL-33, which act on subepithelial dendritic cells, mast cells, and innate lymphoid cells (iLCs) to recruit both innate and adaptive hematopoietic cells and initiate the release of T helper 2 (Th2) cytokines (principally IL-5 and IL-13; Locksley, 2010; Scanlon and McKenzie, 2012; Bando et al., 2013; Barlow et al., 2013; Nussbaum et al., 2013). Environmental stimuli also activate afferent nerves in the airway epithelium that can themselves release biologically active peptide mediators and also trigger reflex release of acetylcholine from efferent fibers in the vagus nerve. This initial response is amplified by the recruitment and differentiation of subsets of T cells that sustain secretion of these cytokines and in some cases secrete another cytokine, IL-17, at specific strategic sites in the airway wall. The released cytokines act on epithelial cells and smooth muscle cells and drive the pathological responses of these cells that contribute to symptomatic disease. The cell biology underlying the responses of the relevant hematopoietic lineages is not specific to asthma and has been discussed elsewhere (Locksley, 2010; Scanlon and McKenzie, 2012). We focus our discussion on the contributions of epithelial cells and airway smooth muscle cells.
Figure 1.
Cell–cell communication in the airway wall in asthma. Environmental triggers concurrently act on airway afferent nerves (which both release their own peptide mediators and stimulate reflex release of the bronchoconstrictor acetylcholine) and airway epithelial cells to initiate responses in multiple cell types that contribute to the mucous metaplasia and airway smooth muscle contraction that characterize asthma. Epithelial cells release TSLP and IL-33, which act on airway dendritic cells, and IL-25, which together with IL-33 acts on mast cells, basophils, and innate type 2 lymphocytes (iLC2). These secreted products stimulate dendritic cell maturation that facilitates the generation of effector T cells and triggers the release of both direct bronchoconstrictors and Th2 cytokines from innate immune cells, which feed back on both the epithelium and airway smooth muscle and further facilitate amplification of airway inflammation through subsequent adaptive T cell responses.
Cell biology of airway epithelium
The airway is covered with a continuous sheet of epithelial cells (Crystal et al., 2008; Ganesan et al., 2013). Two major airway cell types, ciliated and secretory cells, establish and maintain the mucociliary apparatus, which is critical for preserving airway patency and defending against inhaled pathogens and allergens. The apparatus consists of a mucus gel layer and an underlying periciliary layer. Ciliated cells each project ∼300 motile cilia into the periciliary layer that are critical for propelling the mucus layer up the airway. In addition, cilia are coated with membrane-spanning mucins and tethered mucopolysaccharides that exclude mucus from the periciliary space and promote formation of a distinct mucus layer (Button et al., 2012). Secretory cells produce a different class of mucins, the polymeric gel-forming mucins. The two major airway gel-forming mucins are MUC5AC and MUC5B. Some secretory cells, known as mucous or goblet cells, produce mucins and store them within easily visualized collections of mucin granules, whereas other cells produce and secrete mucins (especially MUC5B) but lack prominent granules. Gel-forming mucins are secreted into the airway lumen and are responsible for the characteristic viscoelastic properties of the mucus gel layer.
Airway epithelial injury and remodeling in asthma
A variety of structural changes in the epithelium and other portions of the airway, termed “airway remodeling,” is frequently seen in individuals with asthma (Elias et al., 1999). These changes include airway wall thickening, epithelial hypertrophy and mucous metaplasia, subepithelial fibrosis, myofibroblast hyperplasia, and smooth muscle cell hyperplasia and hypertrophy. Airway remodeling is thought to represent a response to ongoing tissue injury caused by infectious agents, allergens, or inhaled particulates and by the host responses to these stimuli. Signs of frank epithelial injury, including loss of epithelial integrity, disruption of tight junctions, impairment of barrier function, and cell death, have been identified in some studies and may correlate with asthma severity (Laitinen et al., 1985; Jeffery et al., 1989; Barbato et al., 2006; Holgate, 2007). However, in many individuals asthma symptoms and features of airway remodeling, including mucous metaplasia and subepithelial fibrosis, are seen in the absence of signs of active airway infection or overt tissue injury (Ordoñez et al., 2000), suggesting that other processes account for the persistence of asthma in these individuals. Substantial evidence suggests that the persistence of asthma is driven by ongoing host immune responses that generate mediators driving airway remodeling and airway dysfunction. The epithelium is both a site of production of these mediators and a source of cells that respond to mediators produced by immune cells and other cells within the airway. How airway epithelial cells recognize and respond to viruses, allergens, and other stimuli has been comprehensively reviewed elsewhere (Lambrecht and Hammad, 2012). Here we will focus on the contribution of the epithelium to production of and responses to Th2 cytokines.
Airway epithelial contributions to Th2 responses.
Th2 cytokines, especially IL-13, play critical roles in asthma. Multiple cytokines, including TSLP, GM-CSF, IL-1, IL-25, and IL-33, are produced by the epithelium and promote production of Th2 cytokines by immune cells (Cates et al., 2004; Hammad et al., 2009; Locksley, 2010; Nagarkar et al., 2012). Genome-wide association studies implicate multiple Th2-related genes, including IL13, IL33, and TSLP, in asthma (Moffatt et al., 2010; Torgerson et al., 2011). IL-13 is produced by innate lymphoid cells (Neill et al., 2010; Price et al., 2010; Saenz et al., 2010; Hasnain et al., 2011) and Th2 cells (Grünig et al., 1998; Wills-Karp et al., 1998) during allergic inflammation and by macrophages in a mouse model of virus-induced airway disease (Kim et al., 2008). IL-13 induces characteristic changes in airway epithelial mRNA (Kuperman et al., 2005b; Woodruff et al., 2007; Zhen et al., 2007) and miRNA (Solberg et al., 2012) expression patterns in airway epithelial cells. The IL-13 transcriptional “signature” can be used to identify individuals with “Th2 high” and “Th2 low” asthma (Woodruff et al., 2009). The IL-13–induced protein periostin is secreted basally from airway epithelial cells and can be used as a biomarker for Th2 high asthma (Jia et al., 2012; Parulekar et al., 2014). Roughly half of individuals with asthma are Th2 high, and these individuals have better responses to treatment with inhaled corticosteroids (Woodruff et al., 2009) or anti–IL-13 antibody (Corren et al., 2011). The key drivers of Th2 low asthma remain poorly understood, although Th17 family cytokines may be important (Newcomb and Peebles, 2013).
Mucous metaplasia.
Although mucus is critical for host defense, pathological mucus production is an important contributor to asthma morbidity and mortality. In fatal asthma, airways are often plugged with tenacious mucus plugs that obstruct movement of gas (Kuyper et al., 2003). This catastrophic phenomenon likely reflects increased mucin production and secretion as well as changes in mucin cross-linking, mucus gel hydration, and mucus clearance. Abnormalities in mucus are not limited to severe asthma exacerbations because an increase in intracellular mucin stores (mucous metaplasia) is seen even in individuals with stable, mild to moderate asthma (Ordoñez et al., 2001). In mouse allergic airway disease models of asthma, mucous metaplasia results from increased production and storage of mucins (especially MUC5AC) in preexisting secretory cells, including club cells (Evans et al., 2004), rather than transdifferentiation of ciliated cells (Pardo-Saganta et al., 2013). However, in virus-driven models of asthma mucous cells might arise from transdifferentiation of ciliated cells (Tyner et al., 2006). A variety of stimuli and signaling pathways have been shown to regulate mucin production and secretion in airway epithelial cells.
IL-13 stimulates mucin production in Th2 high asthma.
Direct effects of IL-13 on airway epithelial cells induce mucous metaplasia in human airway epithelial cells in culture (Laoukili et al., 2001; Zhen et al., 2007) and in mouse airway epithelial cells in vivo (Kuperman et al., 2002). IL-13 is necessary for mucous metaplasia in many mouse asthma models (Grünig et al., 1998; Wills-Karp et al., 1998; Tyner et al., 2006). Individuals with Th2 high asthma have elevated levels of bronchial epithelial cell MUC5AC mRNA compared with healthy controls or individuals with Th2 low asthma (Woodruff et al., 2009). Recent transgenic mouse studies demonstrate roles for MUC5AC in clearance of enteric nematode infections (Hasnain et al., 2011) and protection against influenza infection (Ehre et al., 2012). Increased MUC5AC expression is therefore part of an integrated immune response that contributes to host defense against pathogens or inhaled particulates. A less well-recognized feature of Th2-high asthma is the substantial decrease in expression of MUC5B (Woodruff et al., 2009). The recent discovery that MUC5B is required for normal mucociliary clearance and defense against airway infection (Roy et al., 2014) suggests further attention should be directed to the possibility that a reduction in MUC5B may be an important contributor to airway dysfunction in asthma.
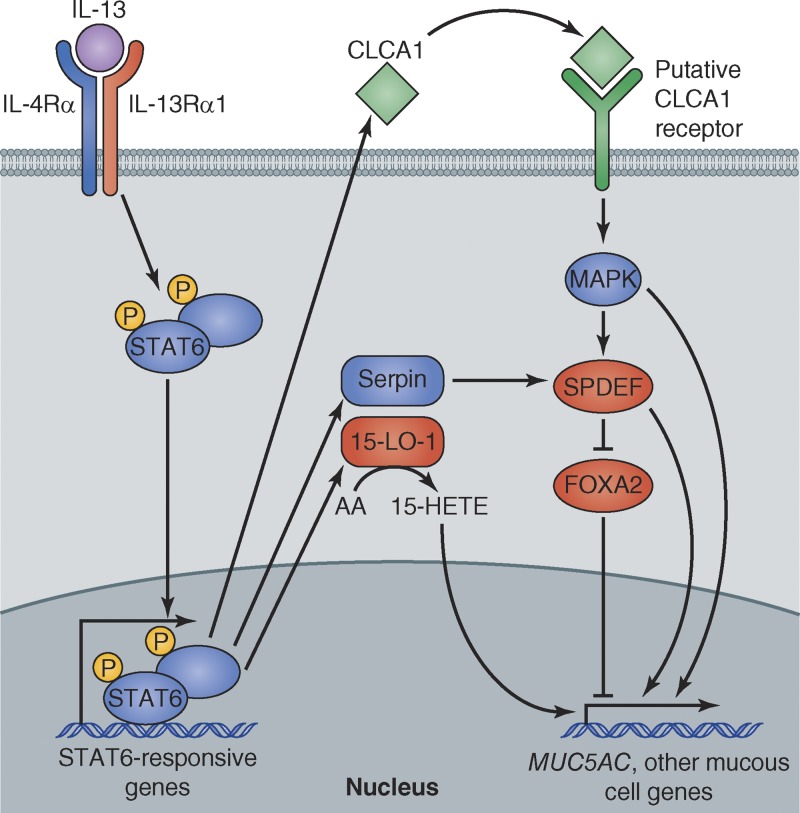
IL-13 is recognized by cell surface receptors expressed on almost all cell types, including airway epithelial cells (Fig. 2). The airway epithelial cell IL-13 receptor that is critical for mucous metaplasia is a heterodimer composed of IL-13Rα1 and IL-4Rα. Removal of this receptor in airway epithelial secretory cells (driven by the CCSP promoter) prevented mucous metaplasia in an allergic asthma model (Kuperman et al., 2005a). IL-13 binding leads to activation of Jak kinases associated with the receptor cytoplasmic domain and subsequent phosphorylation of signal transducer and activator of transcription 6 (STAT6). STAT6 activation is required for IL-13–induced mucous metaplasia (Kuperman et al., 2002).
Figure 2.
Mechanisms of IL-13–induced mucous metaplasia. IL-13 binds to its receptor on the surface of mucous cell progenitors (e.g., club cells) leading to phosphorylation of STAT6 and translocation of STAT6 heterodimers to the nucleus, where they bind to promoters of STAT6-responsive genes. STAT6-dependent processes that contribute to mucous metaplasia include a CLCA1-dependent pathway, a Serpin-dependent pathway, and a 15-lipoxygenase-1–dependent pathway. The transcription factor SPDEF is a master regulator of mucous cell differentiation. It inhibits FOXA2, which represses mucous cell differentiation, and activates transcription of other genes that are expressed in mucous cells.
The series of events that link STAT6 activation to mucous metaplasia are only partly understood. STAT6 does not appear to directly regulate MUC5AC transcription (Young et al., 2007) and the critical direct targets of STAT6 have not been determined. One pathway that depends upon STAT6 activation involves the protein calcium-activated chloride channel 1 (CLCA1). CLCA1 is among the most highly induced genes in airway epithelial cells from individuals with asthma (Hoshino et al., 2002; Toda et al., 2002). Despite its name, CLCA1 does not appear to function as an ion channel but instead undergoes extracellular secretion and cleavage. Extracellular CLCA1 can induce MUC5AC expression via activation of the MAP kinase MAPK13 (p38δ-MAPK; Alevy et al., 2012), although the presumed CLCA1 receptor and the relevant MAPK13 targets have not yet been identified. A second pathway involves the protease inhibitor Serpin3a, the mouse orthologue of human SERPINB3 and SERPINB4. These serpins are induced by IL-13 in a STAT6-dependent fashion (Ray et al., 2005). After allergen challenge, Serpin3a−/− mice had less mucous metaplasia than wild-type mice (Sivaprasad et al., 2011), despite an intact inflammatory response. These results suggest that serpins inhibit proteases that normally degrade one or more proteins required for mucous metaplasia, although the relevant proteases and their protein substrates are not yet known. Another IL-13–induced pathway involves the enzyme 15-lipoxygenase-1 (15-LO-1; Zhao et al., 2009). 15-LO-1 converts arachidonic acid to 15-hydroxyeicosatetraenoic acid, which was shown to enhance MUC5AC expression in human airway epithelial cells.
IL-13– and STAT6-mediated mucous metaplasia depends upon changes in the activity of a network of transcription factors. Allergen-induced IL-13–mediated STAT6 activation leads to increased expression of the SAM-pointed domain–containing Ets-like factor (SPDEF; Park et al., 2007; Chen et al., 2009). The induction of SPDEF depends at least in part on FOXM1, a member of the Forkhead box (FOX) family of transcription factors (Ren et al., 2013). The SPDEF program is also important for mucous metaplasia triggered by other stimuli, including rhinoviruses (Korfhagen et al., 2012). Although SPDEF does not appear to directly regulate mucin gene transcription, SPDEF initiates a transcriptional program that is necessary and sufficient to induce mucous metaplasia. One of the effects of SPDEF is inhibition of the expression of another FOX family gene, FOXA2. In mice, deletion of Foxa2 in mucous cell precursors is sufficient to induce mucous metaplasia, and overexpression of FOXA2 inhibits allergen-induced mucous metaplasia (Zhen et al., 2007; G. Chen et al., 2010). The relationship between IL-13 and FOXA2 is complex. IL-13 inhibits expression of FOXA2, which contributes to mucous metaplasia. However, deletion of Foxa2 in airway epithelial cells during fetal development resulted in Th2 inflammation and production of IL-13 in the airway (G. Chen et al., 2010). The direct targets that are responsible for these effects of FOXA2 are not yet known.
The EGFR pathway induces mucin gene expression and mucous metaplasia.
Epidermal growth factor receptor (EGFR) binds multiple ligands including EGF, TGF-α, heparin-binding EGF, amphiregulin, β-cellulin, and epiregulin. Ligand binding activates the EGFR kinase domain, initiating signaling cascades that are central to many fundamental biological processes, including cell proliferation, differentiation, survival, and migration. EGFR ligands induce expression of MUC5AC in human airway epithelial cell lines and a tyrosine kinase inhibitor that inhibits EGFR kinase prevents mucous metaplasia induced either by an EGFR ligand or by allergen challenge (Takeyama et al., 1999). Subsequent studies showed that bronchial epithelial EGFR levels are increased in asthma and correlate with disease severity (Takeyama et al., 2001a), and that epithelial EGFR signaling contributes to mucous metaplasia in a chronic asthma model (Le Cras et al., 2011).
Various stimuli, including bacterial products (Kohri et al., 2002; Lemjabbar and Basbaum, 2002;Koff et al., 2008), viruses (Tyner et al., 2006; Zhu et al., 2009; Barbier et al., 2012), cigarette smoke (Takeyama et al., 2001b; Basbaum et al., 2002), and inflammatory cell products (Burgel et al., 2001) can activate the EGFR pathway in airway epithelial cells. Some stimuli have been shown to initiate the EGFR signaling cascade by activating the PKC isoforms PKC δ and PKC θ, leading to recruitment of the NADPH oxidase subunits p47phox and p67phox to membrane-associated dual oxidase-1 and the generation of reactive oxygen species (ROS) at the cell surface (Shao and Nadel, 2005). ROS in turn activate latent TGF-α–converting enzyme resulting in cleavage of surface EGFR pro-ligands (Shao et al., 2003). EGFR ligand binding leads to activation of the Ras–Raf–MEK1/2–ERK1/2 pathway and MUC5AC transcriptional induction, which depends upon the Sp1 transcription factor and Sp1-binding sites within the MUC5AC promoter (Takeyama et al., 2000; Perrais et al., 2002). The IL-13 and EGFR pathways make critical but distinct contributions to gene regulation in airway epithelial cells (Zhen et al., 2007). Both pathways inhibit expression of FOXA2, suggesting that this transcription factor may represent a final common pathway for IL-13– and EGFR-induced mucous metaplasia.
Notch signaling regulates mucous cell differentiation.
Notch signaling is also important for mucous metaplasia (Tsao et al., 2011). Notch is a transmembrane receptor that binds to cell-surface ligands in the Delta-like and Jagged families. Ligand binding activates γ-secretase–mediated proteolytic cleavage and liberates the Notch intracellular domain, which enters the nucleus, associates with transcription factors, and drives expression of downstream Notch genes. Genetic manipulation of Notch signaling in mice has different effects depending on the developmental stage. In explanted embryonic lungs, addition of Notch ligand or expression of a constitutively active form of Notch increased MUC5AC-containing mucous cells, whereas a γ-secretase inhibitor reduced mucous cells (Guseh et al., 2009). Notch-induced mucous metaplasia did not require STAT6 activation, suggesting that the Notch and STAT6 pathways may operate in parallel. In contrast, in postnatal mouse lung, disruptions of Notch signaling induced mucous metaplasia (Tsao et al., 2011), a process that principally depends on the Notch ligand Jagged1 (Zhang et al., 2013). The Notch target Hes1 appears to be critical for inhibition of mucous metaplasia and MUC5AC transcription, although inactivation of Hes1 was not sufficient to induce mucous metaplasia (Ou-Yang et al., 2013). The observation that a γ-secretase inhibitor reduced IL-13–induced mucous metaplasia in cultured human airway epithelial cells (Guseh et al., 2009) suggests that further attention to the role of epithelial Notch signaling in asthma is warranted.
The secretory pathway in mucous cells
Mucin monomers are large (∼5,000 amino acid residue) proteins that require extensive processing in the ER and Golgi. Each mucin monomer contains ∼200 cysteine residues that can potentially participate in intra- and intermolecular disulfide bonds. The ER of mucous cells contains specialized molecules that are not widely expressed in other cell types and are required for efficient processing of mucins. One of these is anterior gradient 2 (AGR2) homologue, a member of the protein disulfide isomerase family. An active site cysteine residue in AGR2 forms mixed disulfide bonds with mucins in the ER and mice deficient in AGR2 have profound defects in intestinal mucin production (Park et al., 2009). In a mouse model of allergic asthma, AGR2-deficient mice had reduced mucus production compared with allergen-challenged wild-type mice (Schroeder et al., 2012). The reduction in mucus production was associated with activation of the unfolded protein response, a characteristic response to ER stress (Walter and Ron, 2011). AGR2 may therefore either have a direct role in mucin folding or another function necessary for maintaining normal function of the mucous cell ER. Another molecule found in the mucous cell ER is inositol-requiring enzyme 1β (IRE1β), a transmembrane ER stress sensor. IRE1β is found in mucus-producing cells in the intestine and the airways, but not in other cells. IRE1β regulates AGR2 transcription, and mice deficient in IRE1β had reduced AGR2 expression and impaired airway mucin production in an allergic asthma model (Martino et al., 2013). AGR2 and IRE1β have apparently evolved to meet the unusual demands posed by the need to produce large amounts of mucins.
ORMDL3, a member of the Orm family of transmembrane ER proteins, has also been implicated in asthma. Genetic polymorphisms at loci close to ORMDL3 were strongly associated with asthma in multiple genome-wide association studies (Moffatt et al., 2007; Galanter et al., 2008). Allergen challenge induced ORMDL3 expression in airway epithelial cells in a STAT6-dependent fashion, although ORMDL3 does not appear to be a direct target of STAT6 (Miller et al., 2012). Studies involving overexpression or knockdown of ORDML3 in HEK293 cells indicate that ORMDL3 is involved in regulating ER stress responses and ER-mediated calcium signaling (Cantero-Recasens et al., 2010). In addition, Orm proteins form complexes with serine palmitoyl-CoA transferase (SPT), the first and rate-limiting enzyme in sphingolipid production, and may thereby help coordinate lipid metabolism in the secretory pathway (Breslow et al., 2010). Genetic and pharmacologic reductions in SPT activity induced airway hyperresponsiveness in the absence of inflammation or mucous metaplasia (Worgall et al., 2013). Further studies are required to determine whether ORMDL3’s role in modulating sphingolipid production, ER stress, calcium signaling, or other ER functions in airway epithelial cells or other cells is important in asthma.
Mucins travel from the ER to the Golgi and then are packaged into large granules for secretion. In the Golgi, mucins are extensively O-glycosylated and undergo further multimerization before being released from the cell by regulated exocytosis. Throughout the airways of normal mice and in distal (smaller) airways of humans, basal secretion accounts for most mucin release, and mucin-producing cells retain too little mucin to detect using histological stains. However, mucous cells found in larger airways of humans and allergen-challenged mice contain readily detectable accumulations of mucin-containing granules that can be released by various stimuli, including the P2Y2 receptor ligands ATP and UTP and proteases that cleave protease-activated receptors. Mice lacking the exocytic priming protein Munc13-2 accumulate mucin in secretory cells that normally have minimal intracellular mucin (club cells) but can secrete mucin in response to stimulation (Zhu et al., 2008). In contrast, allergen-challenged mice lacking the low affinity calcium sensor synaptotagmin-2 have a severe defect in acute agonist-stimulated airway mucin secretion, but have preserved basal secretion and do not accumulate mucins in club cells (Tuvim et al., 2009). Agonist-stimulated secretion also depends upon the IL-13–inducible calcium-activated chloride channel TMEM16A, which is increased in mucous cells from individuals with asthma (Huang et al., 2012). Because increased production of MUC5AC via transgenic overexpression was not in itself sufficient to cause airway obstruction (Ehre et al., 2012), it seems likely that qualitative defects in mucin processing, secretion, or hydration that affect the physicochemical properties of mucus contribute to airway obstruction in asthma. Epithelial transport of water and ions, including H+ and bicarbonate, is important in maintaining the normal properties of mucus (E. Chen et al., 2010; Paisley et al., 2010; Garland et al., 2013). Rapid secretion of stored mucin, which is not fully hydrated, may result in the formation of concentrated, rubbery mucus that cannot be cleared normally by cilia or by coughing (Fahy and Dickey, 2010). Hence, IL-13 (Danahay et al., 2002; Nakagami et al., 2008) and other asthma mediators that affect airway epithelial cell water and ion transport could contribute to airway obstruction by altering the physicochemical properties of mucus.
Ciliated cell structure and function in asthma
In comparison with the extensive asthma literature regarding mucous cells, relatively few reports have focused on ciliated cells. One study of epithelial cell strips obtained by endobronchial brushing found decreased ciliary beat frequency and increases in abnormal ciliary beating patterns and ciliary ultrastructural defects in individuals with asthma compared with healthy controls (Thomas et al., 2010). These abnormalities were more pronounced in severe asthma. Ciliary abnormalities were accompanied by increases in the numbers of dead cells and evidence of loss of epithelial structural integrity, which suggests that ciliary dysfunction may be a consequence of a generalized epithelial injury. In any case, these results suggest that ciliary dysfunction might be an important contributor to impaired mucociliary clearance in asthma.
Cell biology of airway smooth muscle in asthma
The excessive airway narrowing that can lead to severe shortness of breath, respiratory failure, and death from asthma is largely due to contraction of the bands of smooth muscle present in the walls of large- and medium-sized conducting airways in the lung. In the large central airways of humans, these bands of muscle are present in the posterior portion of the airways and attach to the anterior airway cartilage rings, but in more peripheral airways smooth muscle is present circumferentially around the airways. In both locations, contraction of smooth muscle, which can be physiologically induced by release of acetylcholine from efferent parasympathetic nerves or by release of histamine and cysteinyl leukotrienes from mast cells and basophils, causes airway narrowing, with the most extensive narrowing in medium-sized airways. In healthy mammals, including humans, physiological responses to release of acetylcholine from efferent nerves or release of histamine and leukotrienes from mast cells and basophils causes only mild and generally asymptomatic airway narrowing. Normal mammals are also generally resistant to marked airway narrowing in response to pharmacologic administration of high concentrations of these contractile agonists directly into the airways. However, people with asthma have a marked increase in sensitivity to all of these agonists that can readily be demonstrated by dramatic increases in airway resistance and associated drops in maximal expiratory airflow rates during forced expiratory maneuvers (Boushey et al., 1980). Recent comparisons between responses to inhaled allergens in allergic asthmatic subjects and other subjects with similarly severe cutaneous immune responses to allergens makes it clear that all allergic humans release largely similar amounts of bronchoconstrictors into the airways (i.e., histamine and leukotrienes), but only asthmatics develop exaggerated airway narrowing in response to these mediators (Becky Kelly et al., 2003).
Mechanisms regulating generation of force by airway smooth muscle actin–myosin coupling
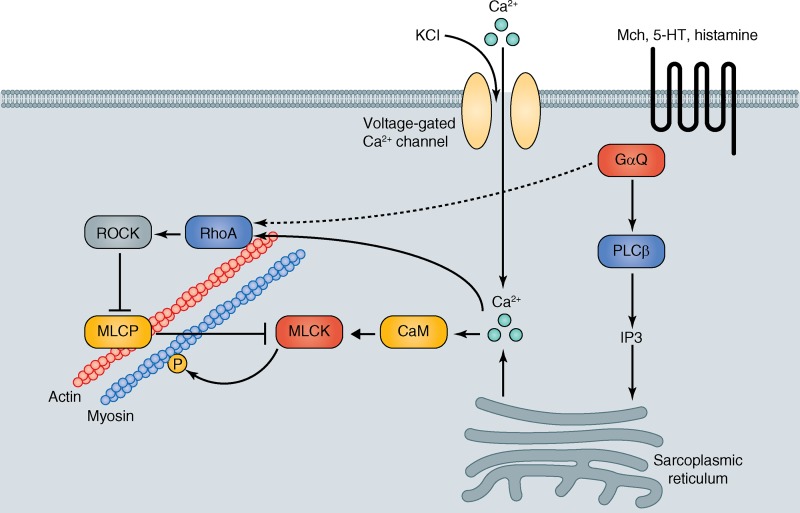
Force generation by airway smooth muscle is mediated by interactions between actin and myosin that depend on phosphorylation of the myosin light chain by the serine–threonine kinase, myosin light chain kinase (Fig. 3). This process is negatively regulated by myosin phosphatase. Increases in intracellular calcium concentration in smooth muscle cells induce contraction by two parallel pathways. When bound to calcium, the serine–threonine kinase calmodulin directly phosphorylates, and thereby activates, myosin light chain kinase. Increased calcium also increases GTP loading of the GTPase, RhoA, which increases the activity of its downstream effector kinases Rho-associated coiled-coil–containing protein kinases 1 and 2 (ROCK 1 and 2). ROCKs directly phosphorylate myosin light chain phosphatase, an effect that inactivates the phosphatase, further enhancing myosin phosphorylation. RhoA can also be activated independently of increases in intracellular calcium.
Figure 3.
Core signaling pathways responsible for airway smooth muscle contraction. Airway smooth muscle contractile force is generated by cyclic cross-bridging of actin and smooth muscle myosin, which depends on myosin phosphorylation. Myosin phosphorylation is regulated by cyclic increases in cytosolic calcium (Ca2+) that activate calmodulin (CaM) to phosphorylate myosin light chain kinase (MLCK), which directly phosphorylates myosin. In parallel, the small GTPase, RhoA, is activated by both calcium-dependent and -independent pathways. Rho directly activates Rho-associated coiled-coil protein kinase (ROCK) which, in turn, phosphorylates and thereby inactivates myosin light chain phosphatase (MLCP), which normally dephosphorylates myosin. The most important physiological pathway for increasing cytosolic calcium in airway smooth muscle involves activation of Gαq by G protein–coupled receptors that respond to extracellular contractile agonists, such as methacholine (Mch), serotonin (5-HT), and histamine. Gαq activates phospholipase C β (PLCβ), which generates IP3 to bind to IP3 receptors on the sarcoplasmic reticulum and release sequestered Ca2+.
There are multiple upstream paths to increased i[Ca] in airway smooth muscle. Acetylcholine, released from post-ganglionic parasympathetic efferent nerves that innervate the muscle, activates G protein–coupled M2 muscarinic receptors, which are coupled to Gαq. GTP-loaded Gαq activates its downstream effector, PLCβ, which phosphorylates PIP2 to generate IP3. IP3, in turn, binds to IP3 receptors on the sarcoplasmic reticulum to trigger translocation of calcium into the cytosol. Other contractile agonists, including histamine, bradykinin, and serotonin (5-HT; the specific agonists and receptors vary across mammalian species) bind to different G protein–coupled receptors to trigger the same pathway. Agonist-induced airway smooth muscle contraction is usually associated with cyclic oscillations in i[Ca], thought to be induced by local changes in cytosolic calcium triggering reuptake of calcium by the sarcoplasmic reticulum, and the magnitude of contractile force induced is most closely associated with the frequency of these calcium oscillations rather than their amplitude (Bergner and Sanderson, 2002).
Increases in cytosolic calcium concentration can also be induced by an influx of calcium from the extracellular space, generally due to the opening of voltage-gated calcium channels in the plasma membrane. These channels can be opened experimentally by increasing the extracellular concentration of potassium ions, which also induces airway smooth muscle contraction. Increased extracellular potassium concentrations also increase release of acetylcholine from post-ganglionic efferent nerves, so proper interpretation of the effects of KCl requires simultaneous addition of a muscarinic antagonist such as atropine.
Regulation of airway smooth muscle force generation by integrin-containing adhesion complexes
For smooth muscle cell contraction to be translated into the force required for airway narrowing, the contracting smooth muscle cell must be firmly tethered to the underlying ECM. Linkage to the ECM is accomplished through the organization of multi-protein complexes nucleated by integrins. The short cytoplasmic domains of integrins can organize surprisingly large multi-protein machines that modulate multiple signaling pathways and link integrins (and thus their ECM ligands) to the actin–myosin cytoskeleton (Yamada and Geiger, 1997; Zaidel-Bar et al., 2007). Many of the contractile agonists that stimulate myosin phosphorylation and actin–myosin interaction simultaneously enhance the formation of integrin signaling complexes, induce actin polymerization at sites of adhesion, and strengthen coupling between the actin–myosin cytoskeleton and the ECM (Mehta and Gunst, 1999; Tang et al., 1999, 2003; Gunst and Fredberg, 2003; Gunst et al., 2003; Opazo Saez et al., 2004). These events appear to also be quite important for generation of maximal contractile force because interventions that inhibit the formation or activity of adhesion complexes can inhibit the strength of contraction without affecting myosin phosphorylation (Mehta and Gunst, 1999; Tang et al., 2003; Opazo Saez et al., 2004).
Lessons from abnormal behavior of airway smooth muscle in animal models
Mice lacking α9β1 integrin in airway smooth muscle.
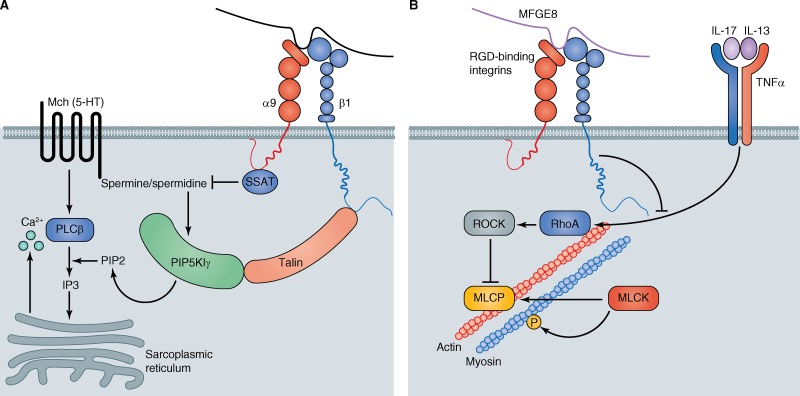
Although there are large differences between the organization of airways in mice and humans, in vivo abnormalities in airway narrowing seen in mouse models do provide some insight into pathways that potentially contribute to abnormal airway smooth muscle contraction in asthma. For the purposes of this review, we will cite three illustrative examples. The integrin α9β1 is highly expressed in airway smooth muscle (Palmer et al., 1993). Conditional knockout of the integrin α9 subunit (uniquely found in the α9β1 integrin) results in a spontaneous increase in in vivo airway responsiveness (as measured by increases in pulmonary resistance in response to intravenous acetylcholine), and to increased contractile responses to cholinergic agonists of both airways in lung slices and tracheal rings studied in an organ bath (Chen et al., 2012). Interestingly, although tracheal rings from these mice also have increased contractile responses to other G protein–coupled receptor agonists (e.g., serotonin), they have normal contractile responses to depolarization with KCl. These findings suggest that loss of α9β1 increases airway responsiveness at some step upstream of calcium release from the sarcoplasmic reticulum (Fig. 4 A). In this case, increased airway responsiveness appears to be due to loss of co-localization of the polyamine-catabolizing enzyme spermidine/spermine N1-acetyltransferase (SSAT), which binds directly to the α9 cytoplasmic domain (Chen et al., 2004), and the lipid kinase, PIP5K1γ, which binds directly to talin, an integrin β1 subunit binding partner. Spermine and spermidine are critical cofactors for PIP5K1γ, so its juxtaposition with SSAT effectively reduces enzymatic activity. PIP5K1γ converts PI4P to PIP2 and is responsible for most of the PIP2 produced in airway smooth muscle cells (Chen et al., 1998). PIP2 is the substrate for IP3 generation by PLCβ, so when α9β1 is present and ligated, contractile agonists that activate receptors coupled to Gαq induce less IP3 generation (Chen et al., 2012) and thus less Ca2+ release through IP3 receptors in the sarcoplasmic reticulum. The importance of this pathway was confirmed by the observations that the frequency of Ca2+ oscillations induced by cholinergic agonists was reduced in lung slices from mice lacking α9β1, and that all of the abnormalities in smooth muscle from these animals could be rescued by addition of a cell-permeable form of PIP2 (Chen et al., 2012).
Figure 4.
Pathways that negatively regulate airway smooth muscle contraction. (A) The integrin α9β1 negatively regulates airway smooth muscle contraction by colocalizing the polyamine-catabolizing enzyme, spermine spermidine acetyltransferase (SSAT), which directly binds to the α9 subunit with the lipid kinase, PIP5K1γ, the major source of PIP2 in airway smooth muscle, which binds to talin, a direct interactor with the β1 subunit. PIP5K1γ depends on spermine and spermidine for maximal activity, so the local breakdown of spermine and spermidine reduces PIP5K1γ activity, thereby decreasing PIP2 concentrations and the amount of IP3 that is generated by activation of contractile G protein–coupled receptors (such as those activated by acetylcholine or serotonin [5-HT]). (B) The secreted scaffold protein, milk fat globule-EGF factor 8 (MFGE8), inhibits the smooth muscle hypercontractility induced by IL-13, IL-17, and tumor necrosis factor α (TNF) by inhibiting the induction and activation of the small GTPase, RhoA. Active RhoA contributes to smooth muscle contraction by directly activating Rho-associated coiled-coil protein kinase (ROCK) which, in turn, phosphorylates and thereby inactivates myosin light chain phosphatase (MLCP), which normally dephosphorylates myosin.
Effects of T cell cytokines on airway smooth muscle contractility.
Several studies conducted over the past 15 years have suggested that cytokines released from T cells can contribute to airway hyperresponsiveness in allergic asthma (Locksley, 2010). The Th2 cytokine IL-13 has been most extensively studied, and can induce both mucous metaplasia and airway hyperresponsiveness when administered directly into the airways of mice (Grünig et al., 1998; Wills-Karp et al., 1998). In vitro, incubation of tracheal rings or lung slices increases narrowing of airways in lung slices and increases force generation by mouse tracheal rings, at least in part by inducing a dramatic increase in expression of the small GTPase, RhoA (Chiba et al., 2009), which is a critical effector of airway smooth muscle contraction (Fig. 4 B). Chronic allergen challenge or direct administration of IL-13 into the airways of mice also increased RhoA expression, in association with induction of airway hyperresponsiveness. A recent study suggested that IL-17 can also increase airway smooth muscle contractility and airway narrowing by induction of RhoA in airway smooth muscle cells (Kudo et al., 2012). In that study, mice lacking the αvβ8 integrin specifically on antigen-presenting dendritic cells were protected from allergen-induced airway hyperresponsiveness. These mice had the same degree of general airway inflammation and mucous metaplasia in response to allergen as wild-type control mice, but had a very specific defect in the generation of antigen-specific Th17 cells, an important source of IL-17 in lungs (Kudo et al., 2012). In vitro, IL-17 was shown to directly increase the contractility of mouse tracheal rings and to increase the levels of RhoA protein and its downstream effector, ROCK2, and to increase phosphorylation of the direct ROCK target, myosin phosphatase. Phosphorylation of myosin phosphatase inhibits its function, and IL-17 was also shown to consequently increase phosphorylation of myosin light chain kinase. Importantly, all of these biochemical effects were dramatically induced in vivo in airway smooth muscle of control mice in response to allergen sensitization and challenge, but all were markedly reduced in mice lacking αvβ8 on dendritic cells. Furthermore, tracheal rings removed from these knockout mice after allergen challenge had decreased in vitro contractility compared with rings from allergen challenged control mice, but this difference in contractility was eliminated by exogenous addition of IL-17. These findings strongly suggest that both IL-13 and IL-17 can contribute to airway hyperresponsiveness by directly inducing RhoA expression in airway smooth muscle (Fig. 4 B). Tumor necrosis factor α, also implicated in asthma pathogenesis, has been shown to increase airway smooth muscle contractility by a similar mechanism (Goto et al., 2009).
Enhanced cytokine-mediated airway smooth muscle contraction in MFGE8-deficient mice.
Milk fat globule EGF factor 8 (MFGE8) is a secreted protein composed of two EGF repeats and two discoidin domains. MFGE8 was originally described to facilitate uptake of apoptotic cells by phagocytes (Hanayama et al., 2004). Mice lacking MFGE8 have normal baseline lung morphology and function, but have exaggerated airway responsiveness after allergen sensitization and challenge (Kudo et al., 2013). However, this abnormality did not appear to be related to any effects on reuptake of apoptotic cells. Immunostaining demonstrated that secreted MFGE8 was concentrated adjacent to airway smooth muscle. Tracheal rings removed from MFGE8 knockout mice had normal contractile responses at baseline, but had markedly enhanced contractile responses after overnight incubation with IL-13, and this increase in contractility could be rescued by addition of recombinant MFGE8 to the muscle bath. Importantly, rescue required the presence of at least one of the discoidin domains and of the integrin-binding RGD motif of the second EGF repeat. In mouse tracheal rings and cultured airway smooth muscle, loss of MFGE8 greatly enhanced the IL-13–induced increase in RhoA protein. These findings suggest that ligation of one or more RGD-binding integrins on airway smooth muscle by extracellular MFGE8 normally serves as a brake on cytokine-mediated RhoA induction and thereby limits maximal cytokine-induced airway hyperresponsiveness (Fig. 4 B). The specific integrin(s) involved in this response, the molecular mechanisms linking integrin ligation to inhibition of RhoA, and the role and binding partner(s) of the MFGE8 discoidin domains that are required for RhoA inhibition all remain to be determined.
Conclusions
Rapid progress has been made toward identifying epithelial and smooth muscle cell molecules and pathways that can produce many of the abnormalities found in individuals with asthma. Because these discoveries were made in diverse experimental systems, we still face major challenges in understanding how these molecules and pathways interact in vivo and in identifying the pathways that are most relevant in people with asthma. Asthma is a heterogeneous disease, and recent progress toward identifying subtypes with distinct pathophysiologic mechanisms promises to focus attention on certain pathways in epithelial and smooth muscle cells (Lötvall et al., 2011). It will be especially important to understand mechanisms underlying severe asthma. Approximately 5–10% of individuals with asthma have severe disease, with symptoms that persist despite standard therapy with bronchodilators and inhaled corticosteroids (Brightling et al., 2012). These individuals have high rates of asthma exacerbations leading to hospitalization and are at relatively high risk for fatal asthma attacks. Continued attention to the study of the cell biology of asthma will be crucial for generating new ideas for asthma prevention and treatment based on normalizing epithelial and smooth muscle function.
Acknowledgments
We thank the UCSF Sandler Asthma Basic Research Center and the National Institutes of Health (grants AI1077439, HL53949, HL099101, HL102292, and HL108596) for supporting our work. Illustrations were provided by Neil Smith, www.neilsmithillustration.co.uk.
The authors declare no competing financial interests.
Footnotes
Abbreviations used in this paper:
- CLCA1
- calcium-activated chloride channel 1
- EGFR
- epidermal growth factor receptor
- FOX
- Forkhead box
- IL
- interleukin
- ROCK
- Rho-associated coiled-coil containing protein kinase
- ROS
- reactive oxygen species
- SPDEF
- SAM-pointed domain–containing Ets-like factor
- STAT6
- signal transducer and activator of transcription 6
- Th2
- T helper 2
References
- Alevy Y.G., Patel A.C., Romero A.G., Patel D.A., Tucker J., Roswit W.T., Miller C.A., Heier R.F., Byers D.E., Brett T.J., Holtzman M.J. 2012. IL-13-induced airway mucus production is attenuated by MAPK13 inhibition. J. Clin. Invest. 122:4555–4568 10.1172/JCI64896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bando J.K., Nussbaum J.C., Liang H.E., Locksley R.M. 2013. Type 2 innate lymphoid cells constitutively express arginase-I in the naive and inflamed lung. J. Leukoc. Biol. 94:877–884 10.1189/jlb.0213084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbato A., Turato G., Baraldo S., Bazzan E., Calabrese F., Panizzolo C., Zanin M.E., Zuin R., Maestrelli P., Fabbri L.M., Saetta M. 2006. Epithelial damage and angiogenesis in the airways of children with asthma. Am. J. Respir. Crit. Care Med. 174:975–981 10.1164/rccm.200602-189OC [DOI] [PubMed] [Google Scholar]
- Barbier D., Garcia-Verdugo I., Pothlichet J., Khazen R., Descamps D., Rousseau K., Thornton D., Si-Tahar M., Touqui L., Chignard M., Sallenave J.M. 2012. Influenza A induces the major secreted airway mucin MUC5AC in a protease-EGFR-extracellular regulated kinase-Sp1-dependent pathway. Am. J. Respir. Cell Mol. Biol. 47:149–157 10.1165/rcmb.2011-0405OC [DOI] [PubMed] [Google Scholar]
- Barlow J.L., Peel S., Fox J., Panova V., Hardman C.S., Camelo A., Bucks C., Wu X., Kane C.M., Neill D.R., et al. 2013. IL-33 is more potent than IL-25 in provoking IL-13-producing nuocytes (type 2 innate lymphoid cells) and airway contraction. J. Allergy Clin. Immunol. 132:933–941 10.1016/j.jaci.2013.05.012 [DOI] [PubMed] [Google Scholar]
- Basbaum C., Li D., Gensch E., Gallup M., Lemjabbar H. 2002. Mechanisms by which gram-positive bacteria and tobacco smoke stimulate mucin induction through the epidermal growth factor receptor (EGFR). Novartis Found. Symp. 248:171–176, discussion :176–180: 277–282 10.1002/0470860790.ch11 [DOI] [PubMed] [Google Scholar]
- Becky Kelly E.A., Busse W.W., Jarjour N.N. 2003. A comparison of the airway response to segmental antigen bronchoprovocation in atopic asthma and allergic rhinitis. J. Allergy Clin. Immunol. 111:79–86 10.1067/mai.2003.28 [DOI] [PubMed] [Google Scholar]
- Bergner A., Sanderson M.J. 2002. Acetylcholine-induced calcium signaling and contraction of airway smooth muscle cells in lung slices. J. Gen. Physiol. 119:187–198 10.1085/jgp.119.2.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boushey H.A., Holtzman M.J., Sheller J.R., Nadel J.A. 1980. Bronchial hyperreactivity. Am. Rev. Respir. Dis. 121:389–413 [DOI] [PubMed] [Google Scholar]
- Breslow D.K., Collins S.R., Bodenmiller B., Aebersold R., Simons K., Shevchenko A., Ejsing C.S., Weissman J.S. 2010. Orm family proteins mediate sphingolipid homeostasis. Nature. 463:1048–1053 10.1038/nature08787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brightling C.E., Gupta S., Gonem S., Siddiqui S. 2012. Lung damage and airway remodelling in severe asthma. Clin. Exp. Allergy. 42:638–649 10.1111/j.1365-2222.2011.03917.x [DOI] [PubMed] [Google Scholar]
- Burgel P.R., Lazarus S.C., Tam D.C., Ueki I.F., Atabai K., Birch M., Nadel J.A. 2001. Human eosinophils induce mucin production in airway epithelial cells via epidermal growth factor receptor activation. J. Immunol. 167:5948–5954 10.4049/jimmunol.167.10.5948 [DOI] [PubMed] [Google Scholar]
- Button B., Cai L.H., Ehre C., Kesimer M., Hill D.B., Sheehan J.K., Boucher R.C., Rubinstein M. 2012. A periciliary brush promotes the lung health by separating the mucus layer from airway epithelia. Science. 337:937–941 10.1126/science.1223012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantero-Recasens G., Fandos C., Rubio-Moscardo F., Valverde M.A., Vicente R. 2010. The asthma-associated ORMDL3 gene product regulates endoplasmic reticulum-mediated calcium signaling and cellular stress. Hum. Mol. Genet. 19:111–121 10.1093/hmg/ddp471 [DOI] [PubMed] [Google Scholar]
- Cates E.C., Fattouh R., Wattie J., Inman M.D., Goncharova S., Coyle A.J., Gutierrez-Ramos J.C., Jordana M. 2004. Intranasal exposure of mice to house dust mite elicits allergic airway inflammation via a GM-CSF-mediated mechanism. J. Immunol. 173:6384–6392 10.4049/jimmunol.173.10.6384 [DOI] [PubMed] [Google Scholar]
- Chen C., Young B.A., Coleman C.S., Pegg A.E., Sheppard D. 2004. Spermidine/spermine N1-acetyltransferase specifically binds to the integrin alpha9 subunit cytoplasmic domain and enhances cell migration. J. Cell Biol. 167:161–170 10.1083/jcb.200312166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Kudo M., Rutaganira F., Takano H., Lee C., Atakilit A., Robinett K.S., Uede T., Wolters P.J., Shokat K.M., et al. 2012. Integrin α9β1 in airway smooth muscle suppresses exaggerated airway narrowing. J. Clin. Invest. 122:2916–2927 10.1172/JCI60387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E.Y., Yang N., Quinton P.M., Chin W.C. 2010. A new role for bicarbonate in mucus formation. Am. J. Physiol. Lung Cell. Mol. Physiol. 299:L542–L549 10.1152/ajplung.00180.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Korfhagen T.R., Xu Y., Kitzmiller J., Wert S.E., Maeda Y., Gregorieff A., Clevers H., Whitsett J.A. 2009. SPDEF is required for mouse pulmonary goblet cell differentiation and regulates a network of genes associated with mucus production. J. Clin. Invest. 119:2914–2924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Wan H., Luo F., Zhang L., Xu Y., Lewkowich I., Wills-Karp M., Whitsett J.A. 2010. Foxa2 programs Th2 cell-mediated innate immunity in the developing lung. J. Immunol. 184:6133–6141 10.4049/jimmunol.1000223 [DOI] [PubMed] [Google Scholar]
- Chen H., Baron C.B., Griffiths T., II, Greeley P., Coburn R.F. 1998. Effects of polyamines and calcium and sodium ions on smooth muscle cytoskeleton-associated phosphatidylinositol (4)-phosphate 5-kinase. J. Cell. Physiol. 177:161–173 [DOI] [PubMed] [Google Scholar]
- Chiba Y., Nakazawa S., Todoroki M., Shinozaki K., Sakai H., Misawa M. 2009. Interleukin-13 augments bronchial smooth muscle contractility with an up-regulation of RhoA protein. Am. J. Respir. Cell Mol. Biol. 40:159–167 10.1165/rcmb.2008-0162OC [DOI] [PubMed] [Google Scholar]
- Corren J., Lemanske R.F., Hanania N.A., Korenblat P.E., Parsey M.V., Arron J.R., Harris J.M., Scheerens H., Wu L.C., Su Z., et al. 2011. Lebrikizumab treatment in adults with asthma. N. Engl. J. Med. 365:1088–1098 10.1056/NEJMoa1106469 [DOI] [PubMed] [Google Scholar]
- Crystal R.G., Randell S.H., Engelhardt J.F., Voynow J., Sunday M.E. 2008. Airway epithelial cells: current concepts and challenges. Proc. Am. Thorac. Soc. 5:772–777 10.1513/pats.200805-041HR [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danahay H., Atherton H., Jones G., Bridges R.J., Poll C.T. 2002. Interleukin-13 induces a hypersecretory ion transport phenotype in human bronchial epithelial cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 282:L226–L236 [DOI] [PubMed] [Google Scholar]
- Ehre C., Worthington E.N., Liesman R.M., Grubb B.R., Barbier D., O’Neal W.K., Sallenave J.M., Pickles R.J., Boucher R.C. 2012. Overexpressing mouse model demonstrates the protective role of Muc5ac in the lungs. Proc. Natl. Acad. Sci. USA. 109:16528–16533 10.1073/pnas.1206552109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elias J.A., Zhu Z., Chupp G., Homer R.J. 1999. Airway remodeling in asthma. J. Clin. Invest. 104:1001–1006 10.1172/JCI8124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans C.M., Williams O.W., Tuvim M.J., Nigam R., Mixides G.P., Blackburn M.R., DeMayo F.J., Burns A.R., Smith C., Reynolds S.D., et al. 2004. Mucin is produced by clara cells in the proximal airways of antigen-challenged mice. Am. J. Respir. Cell Mol. Biol. 31:382–394 10.1165/rcmb.2004-0060OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahy J.V., Dickey B.F. 2010. Airway mucus function and dysfunction. N. Engl. J. Med. 363:2233–2247 10.1056/NEJMra0910061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanter J., Choudhry S., Eng C., Nazario S., Rodríguez-Santana J.R., Casal J., Torres-Palacios A., Salas J., Chapela R., Watson H.G., et al. 2008. ORMDL3 gene is associated with asthma in three ethnically diverse populations. Am. J. Respir. Crit. Care Med. 177:1194–1200 10.1164/rccm.200711-1644OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganesan S., Comstock A.T., Sajjan U.S. 2013. Barrier function of airway tract epithelium. Tissue Barriers. 1:e24997 10.4161/tisb.24997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland A.L., Walton W.G., Coakley R.D., Tan C.D., Gilmore R.C., Hobbs C.A., Tripathy A., Clunes L.A., Bencharit S., Stutts M.J., et al. 2013. Molecular basis for pH-dependent mucosal dehydration in cystic fibrosis airways. Proc. Natl. Acad. Sci. USA. 110:15973–15978 10.1073/pnas.1311999110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto K., Chiba Y., Sakai H., Misawa M. 2009. Tumor necrosis factor-alpha (TNF-alpha) induces upregulation of RhoA via NF-kappaB activation in cultured human bronchial smooth muscle cells. J. Pharmacol. Sci. 110:437–444 10.1254/jphs.09081FP [DOI] [PubMed] [Google Scholar]
- Grünig G., Warnock M., Wakil A.E., Venkayya R., Brombacher F., Rennick D.M., Sheppard D., Mohrs M., Donaldson D.D., Locksley R.M., Corry D.B. 1998. Requirement for IL-13 independently of IL-4 in experimental asthma. Science. 282:2261–2263 10.1126/science.282.5397.2261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunst S.J., Fredberg J.J. 2003. The first three minutes: smooth muscle contraction, cytoskeletal events, and soft glasses. J. Appl. Physiol. 95:413–425 [DOI] [PubMed] [Google Scholar]
- Gunst S.J., Tang D.D., Opazo Saez A. 2003. Cytoskeletal remodeling of the airway smooth muscle cell: a mechanism for adaptation to mechanical forces in the lung. Respir. Physiol. Neurobiol. 137:151–168 10.1016/S1569-9048(03)00144-7 [DOI] [PubMed] [Google Scholar]
- Guseh J.S., Bores S.A., Stanger B.Z., Zhou Q., Anderson W.J., Melton D.A., Rajagopal J. 2009. Notch signaling promotes airway mucous metaplasia and inhibits alveolar development. Development. 136:1751–1759 10.1242/dev.029249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammad H., Chieppa M., Perros F., Willart M.A., Germain R.N., Lambrecht B.N. 2009. House dust mite allergen induces asthma via Toll-like receptor 4 triggering of airway structural cells. Nat. Med. 15:410–416 10.1038/nm.1946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanayama R., Tanaka M., Miyasaka K., Aozasa K., Koike M., Uchiyama Y., Nagata S. 2004. Autoimmune disease and impaired uptake of apoptotic cells in MFG-E8-deficient mice. Science. 304:1147–1150 10.1126/science.1094359 [DOI] [PubMed] [Google Scholar]
- Hasnain S.Z., Evans C.M., Roy M., Gallagher A.L., Kindrachuk K.N., Barron L., Dickey B.F., Wilson M.S., Wynn T.A., Grencis R.K., Thornton D.J. 2011. Muc5ac: a critical component mediating the rejection of enteric nematodes. J. Exp. Med. 208:893–900 10.1084/jem.20102057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holgate S.T. 2007. Epithelium dysfunction in asthma. J. Allergy Clin. Immunol. 120:1233–1244, quiz :1245–1246 10.1016/j.jaci.2007.10.025 [DOI] [PubMed] [Google Scholar]
- Hoshino M., Morita S., Iwashita H., Sagiya Y., Nagi T., Nakanishi A., Ashida Y., Nishimura O., Fujisawa Y., Fujino M. 2002. Increased expression of the human Ca2+-activated Cl- channel 1 (CaCC1) gene in the asthmatic airway. Am. J. Respir. Crit. Care Med. 165:1132–1136 10.1164/ajrccm.165.8.2107068 [DOI] [PubMed] [Google Scholar]
- Huang F., Zhang H., Wu M., Yang H., Kudo M., Peters C.J., Woodruff P.G., Solberg O.D., Donne M.L., Huang X., et al. 2012. Calcium-activated chloride channel TMEM16A modulates mucin secretion and airway smooth muscle contraction. Proc. Natl. Acad. Sci. USA. 109:16354–16359 10.1073/pnas.1214596109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery P.K., Wardlaw A.J., Nelson F.C., Collins J.V., Kay A.B. 1989. Bronchial biopsies in asthma. An ultrastructural, quantitative study and correlation with hyperreactivity. Am. Rev. Respir. Dis. 140:1745–1753 10.1164/ajrccm/140.6.1745 [DOI] [PubMed] [Google Scholar]
- Jia G., Erickson R.W., Choy D.F., Mosesova S., Wu L.C., Solberg O.D., Shikotra A., Carter R., Audusseau S., Hamid Q., et al. Bronchoscopic Exploratory Research Study of Biomarkers in Corticosteroid-refractory Asthma (BOBCAT) Study Group. 2012. Periostin is a systemic biomarker of eosinophilic airway inflammation in asthmatic patients. J. Allergy Clin. Immunol. 130:647–654: e10 10.1016/j.jaci.2012.06.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E.Y., Battaile J.T., Patel A.C., You Y., Agapov E., Grayson M.H., Benoit L.A., Byers D.E., Alevy Y., Tucker J., et al. 2008. Persistent activation of an innate immune response translates respiratory viral infection into chronic lung disease. Nat. Med. 14:633–640 10.1038/nm1770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koff J.L., Shao M.X., Ueki I.F., Nadel J.A. 2008. Multiple TLRs activate EGFR via a signaling cascade to produce innate immune responses in airway epithelium. Am. J. Physiol. Lung Cell. Mol. Physiol. 294:L1068–L1075 10.1152/ajplung.00025.2008 [DOI] [PubMed] [Google Scholar]
- Kohri K., Ueki I.F., Shim J.J., Burgel P.R., Oh Y.M., Tam D.C., Dao-Pick T., Nadel J.A. 2002. Pseudomonas aeruginosa induces MUC5AC production via epidermal growth factor receptor. Eur. Respir. J. 20:1263–1270 10.1183/09031936.02.00001402 [DOI] [PubMed] [Google Scholar]
- Korfhagen T.R., Kitzmiller J., Chen G., Sridharan A., Haitchi H.M., Hegde R.S., Divanovic S., Karp C.L., Whitsett J.A. 2012. SAM-pointed domain ETS factor mediates epithelial cell-intrinsic innate immune signaling during airway mucous metaplasia. Proc. Natl. Acad. Sci. USA. 109:16630–16635 10.1073/pnas.1208092109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudo M., Melton A.C., Chen C., Engler M.B., Huang K.E., Ren X., Wang Y., Bernstein X., Li J.T., Atabai K., et al. 2012. IL-17A produced by αβ T cells drives airway hyper-responsiveness in mice and enhances mouse and human airway smooth muscle contraction. Nat. Med. 18:547–554 10.1038/nm.2684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kudo M., Khalifeh Soltani S.M., Sakuma S.A., McKleroy W., Lee T.H., Woodruff P.G., Lee J.W., Huang K., Chen C., Arjomandi M., et al. 2013. Mfge8 suppresses airway hyperresponsiveness in asthma by regulating smooth muscle contraction. Proc. Natl. Acad. Sci. USA. 110:660–665 10.1073/pnas.1216673110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuperman D.A., Huang X., Koth L.L., Chang G.H., Dolganov G.M., Zhu Z., Elias J.A., Sheppard D., Erle D.J. 2002. Direct effects of interleukin-13 on epithelial cells cause airway hyperreactivity and mucus overproduction in asthma. Nat. Med. 8:885–889 [DOI] [PubMed] [Google Scholar]
- Kuperman D.A., Huang X., Nguyenvu L., Hölscher C., Brombacher F., Erle D.J. 2005a. IL-4 receptor signaling in Clara cells is required for allergen-induced mucus production. J. Immunol. 175:3746–3752 10.4049/jimmunol.175.6.3746 [DOI] [PubMed] [Google Scholar]
- Kuperman D.A., Lewis C.C., Woodruff P.G., Rodriguez M.W., Yang Y.H., Dolganov G.M., Fahy J.V., Erle D.J. 2005b. Dissecting asthma using focused transgenic modeling and functional genomics. J. Allergy Clin. Immunol. 116:305–311 10.1016/j.jaci.2005.03.024 [DOI] [PubMed] [Google Scholar]
- Kuyper L.M., Paré P.D., Hogg J.C., Lambert R.K., Ionescu D., Woods R., Bai T.R. 2003. Characterization of airway plugging in fatal asthma. Am. J. Med. 115:6–11 10.1016/S0002-9343(03)00241-9 [DOI] [PubMed] [Google Scholar]
- Laitinen L.A., Heino M., Laitinen A., Kava T., Haahtela T. 1985. Damage of the airway epithelium and bronchial reactivity in patients with asthma. Am. Rev. Respir. Dis. 131:599–606 [DOI] [PubMed] [Google Scholar]
- Lambrecht B.N., Hammad H. 2012. The airway epithelium in asthma. Nat. Med. 18:684–692 10.1038/nm.2737 [DOI] [PubMed] [Google Scholar]
- Laoukili J., Perret E., Willems T., Minty A., Parthoens E., Houcine O., Coste A., Jorissen M., Marano F., Caput D., Tournier F. 2001. IL-13 alters mucociliary differentiation and ciliary beating of human respiratory epithelial cells. J. Clin. Invest. 108:1817–1824 10.1172/JCI200113557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Cras T.D., Acciani T.H., Mushaben E.M., Kramer E.L., Pastura P.A., Hardie W.D., Korfhagen T.R., Sivaprasad U., Ericksen M., Gibson A.M., et al. 2011. Epithelial EGF receptor signaling mediates airway hyperreactivity and remodeling in a mouse model of chronic asthma. Am. J. Physiol. Lung Cell. Mol. Physiol. 300:L414–L421 10.1152/ajplung.00346.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemjabbar H., Basbaum C. 2002. Platelet-activating factor receptor and ADAM10 mediate responses to Staphylococcus aureus in epithelial cells. Nat. Med. 8:41–46 10.1038/nm0102-41 [DOI] [PubMed] [Google Scholar]
- Locksley R.M. 2010. Asthma and allergic inflammation. Cell. 140:777–783 10.1016/j.cell.2010.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lötvall J., Akdis C.A., Bacharier L.B., Bjermer L., Casale T.B., Custovic A., Lemanske R.F., Jr, Wardlaw A.J., Wenzel S.E., Greenberger P.A. 2011. Asthma endotypes: a new approach to classification of disease entities within the asthma syndrome. J. Allergy Clin. Immunol. 127:355–360 10.1016/j.jaci.2010.11.037 [DOI] [PubMed] [Google Scholar]
- Martino M.B., Jones L., Brighton B., Ehre C., Abdulah L., Davis C.W., Ron D., O’Neal W.K., Ribeiro C.M. 2013. The ER stress transducer IRE1β is required for airway epithelial mucin production. Mucosal Immunol. 6:639–654 10.1038/mi.2012.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta D., Gunst S.J. 1999. Actin polymerization stimulated by contractile activation regulates force development in canine tracheal smooth muscle. J. Physiol. 519:829–840 10.1111/j.1469-7793.1999.0829n.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M., Tam A.B., Cho J.Y., Doherty T.A., Pham A., Khorram N., Rosenthal P., Mueller J.L., Hoffman H.M., Suzukawa M., et al. 2012. ORMDL3 is an inducible lung epithelial gene regulating metalloproteases, chemokines, OAS, and ATF6. Proc. Natl. Acad. Sci. USA. 109:16648–16653 10.1073/pnas.1204151109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffatt M.F., Kabesch M., Liang L., Dixon A.L., Strachan D., Heath S., Depner M., von Berg A., Bufe A., Rietschel E., et al. 2007. Genetic variants regulating ORMDL3 expression contribute to the risk of childhood asthma. Nature. 448:470–473 10.1038/nature06014 [DOI] [PubMed] [Google Scholar]
- Moffatt M.F., Gut I.G., Demenais F., Strachan D.P., Bouzigon E., Heath S., von Mutius E., Farrall M., Lathrop M., Cookson W.O., et al. 2010. A large-scale, consortium-based genomewide association study of asthma. N. Engl. J. Med. 363:1211–1221 10.1056/NEJMoa0906312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorman J.E., Rudd R.A., Johnson C.A., King M., Minor P., Bailey C., Scalia M.R., Akinbami L.J.; Centers for Disease Control and Prevention (CDC). 2007. National surveillance for asthma—United States, 1980-2004. MMWR Surveill. Summ. 56:1–54 [PubMed] [Google Scholar]
- Nagarkar D.R., Poposki J.A., Comeau M.R., Biyasheva A., Avila P.C., Schleimer R.P., Kato A. 2012. Airway epithelial cells activate TH2 cytokine production in mast cells through IL-1 and thymic stromal lymphopoietin. J. Allergy Clin. Immunol. 130:225–232: e4 10.1016/j.jaci.2012.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagami Y., Favoreto S., Jr, Zhen G., Park S.W., Nguyenvu L.T., Kuperman D.A., Dolganov G.M., Huang X., Boushey H.A., Avila P.C., Erle D.J. 2008. The epithelial anion transporter pendrin is induced by allergy and rhinovirus infection, regulates airway surface liquid, and increases airway reactivity and inflammation in an asthma model. J. Immunol. 181:2203–2210 10.4049/jimmunol.181.3.2203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neill D.R., Wong S.H., Bellosi A., Flynn R.J., Daly M., Langford T.K., Bucks C., Kane C.M., Fallon P.G., Pannell R., et al. 2010. Nuocytes represent a new innate effector leukocyte that mediates type-2 immunity. Nature. 464:1367–1370 10.1038/nature08900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb D.C., Peebles R.S., Jr 2013. Th17-mediated inflammation in asthma. Curr. Opin. Immunol. 25:755–760 10.1016/j.coi.2013.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaum J.C., Van Dyken S.J., von Moltke J., Cheng L.E., Mohapatra A., Molofsky A.B., Thornton E.E., Krummel M.F., Chawla A., Liang H.E., Locksley R.M. 2013. Type 2 innate lymphoid cells control eosinophil homeostasis. Nature. 502:245–248 10.1038/nature12526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opazo Saez A., Zhang W., Wu Y., Turner C.E., Tang D.D., Gunst S.J. 2004. Tension development during contractile stimulation of smooth muscle requires recruitment of paxillin and vinculin to the membrane. Am. J. Physiol. Cell Physiol. 286:C433–C447 10.1152/ajpcell.00030.2003 [DOI] [PubMed] [Google Scholar]
- Ordoñez C., Ferrando R., Hyde D.M., Wong H.H., Fahy J.V. 2000. Epithelial desquamation in asthma: artifact or pathology? Am. J. Respir. Crit. Care Med. 162:2324–2329 10.1164/ajrccm.162.6.2001041 [DOI] [PubMed] [Google Scholar]
- Ordoñez C.L., Khashayar R., Wong H.H., Ferrando R., Wu R., Hyde D.M., Hotchkiss J.A., Zhang Y., Novikov A., Dolganov G., Fahy J.V. 2001. Mild and moderate asthma is associated with airway goblet cell hyperplasia and abnormalities in mucin gene expression. Am. J. Respir. Crit. Care Med. 163:517–523 10.1164/ajrccm.163.2.2004039 [DOI] [PubMed] [Google Scholar]
- Ou-Yang H.F., Wu C.G., Qu S.Y., Li Z.K. 2013. Notch signaling downregulates MUC5AC expression in airway epithelial cells through Hes1-dependent mechanisms. Respiration. 86:341–346 10.1159/000350647 [DOI] [PubMed] [Google Scholar]
- Paisley D., Gosling M., Danahay H. 2010. Regulation of airway mucosal hydration. Expert Rev Clin Pharmacol. 3:361–369 10.1586/ecp.10.19 [DOI] [PubMed] [Google Scholar]
- Palmer E.L., Rüegg C., Ferrando R., Pytela R., Sheppard D. 1993. Sequence and tissue distribution of the integrin alpha 9 subunit, a novel partner of beta 1 that is widely distributed in epithelia and muscle. J. Cell Biol. 123:1289–1297 10.1083/jcb.123.5.1289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardo-Saganta A., Law B.M., Gonzalez-Celeiro M., Vinarsky V., Rajagopal J. 2013. Ciliated cells of pseudostratified airway epithelium do not become mucous cells after ovalbumin challenge. Am. J. Respir. Cell Mol. Biol. 48:364–373 10.1165/rcmb.2012-0146OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park K.S., Korfhagen T.R., Bruno M.D., Kitzmiller J.A., Wan H., Wert S.E., Khurana Hershey G.K., Chen G., Whitsett J.A. 2007. SPDEF regulates goblet cell hyperplasia in the airway epithelium. J. Clin. Invest. 117:978–988 10.1172/JCI29176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S.W., Zhen G., Verhaeghe C., Nakagami Y., Nguyenvu L.T., Barczak A.J., Killeen N., Erle D.J. 2009. The protein disulfide isomerase AGR2 is essential for production of intestinal mucus. Proc. Natl. Acad. Sci. USA. 106:6950–6955 10.1073/pnas.0808722106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parulekar A.D., Atik M.A., Hanania N.A. 2014. Periostin, a novel biomarker of TH2-driven asthma. Curr. Opin. Pulm. Med. 20:60–65 10.1097/MCP.0000000000000005 [DOI] [PubMed] [Google Scholar]
- Perrais M., Pigny P., Copin M.C., Aubert J.P., Van Seuningen I. 2002. Induction of MUC2 and MUC5AC mucins by factors of the epidermal growth factor (EGF) family is mediated by EGF receptor/Ras/Raf/extracellular signal-regulated kinase cascade and Sp1. J. Biol. Chem. 277:32258–32267 10.1074/jbc.M204862200 [DOI] [PubMed] [Google Scholar]
- Price A.E., Liang H.E., Sullivan B.M., Reinhardt R.L., Eisley C.J., Erle D.J., Locksley R.M. 2010. Systemically dispersed innate IL-13-expressing cells in type 2 immunity. Proc. Natl. Acad. Sci. USA. 107:11489–11494 10.1073/pnas.1003988107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray R., Choi M., Zhang Z., Silverman G.A., Askew D., Mukherjee A.B. 2005. Uteroglobin suppresses SCCA gene expression associated with allergic asthma. J. Biol. Chem. 280:9761–9764 10.1074/jbc.C400581200 [DOI] [PubMed] [Google Scholar]
- Ren X., Shah T.A., Ustiyan V., Zhang Y., Shinn J., Chen G., Whitsett J.A., Kalin T.V., Kalinichenko V.V. 2013. FOXM1 promotes allergen-induced goblet cell metaplasia and pulmonary inflammation. Mol. Cell. Biol. 33:371–386 10.1128/MCB.00934-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy M.G., Livraghi-Butrico A., Fletcher A.A., McElwee M.M., Evans S.E., Boerner R.M., Alexander S.N., Bellinghausen L.K., Song A.S., Petrova Y.M., et al. 2014. Muc5b is required for airway defence. Nature. 505:412–416 10.1038/nature12807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saenz S.A., Siracusa M.C., Perrigoue J.G., Spencer S.P., Urban J.F., Jr, Tocker J.E., Budelsky A.L., Kleinschek M.A., Kastelein R.A., Kambayashi T., et al. 2010. IL25 elicits a multipotent progenitor cell population that promotes T(H)2 cytokine responses. Nature. 464:1362–1366 10.1038/nature08901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scanlon S.T., McKenzie A.N. 2012. Type 2 innate lymphoid cells: new players in asthma and allergy. Curr. Opin. Immunol. 24:707–712 10.1016/j.coi.2012.08.009 [DOI] [PubMed] [Google Scholar]
- Schroeder B.W., Verhaeghe C., Park S.W., Nguyenvu L.T., Huang X., Zhen G., Erle D.J. 2012. AGR2 is induced in asthma and promotes allergen-induced mucin overproduction. Am. J. Respir. Cell Mol. Biol. 47:178–185 10.1165/rcmb.2011-0421OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao M.X., Nadel J.A. 2005. Dual oxidase 1-dependent MUC5AC mucin expression in cultured human airway epithelial cells. Proc. Natl. Acad. Sci. USA. 102:767–772 10.1073/pnas.0408932102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao M.X., Ueki I.F., Nadel J.A. 2003. Tumor necrosis factor alpha-converting enzyme mediates MUC5AC mucin expression in cultured human airway epithelial cells. Proc. Natl. Acad. Sci. USA. 100:11618–11623 10.1073/pnas.1534804100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivaprasad U., Askew D.J., Ericksen M.B., Gibson A.M., Stier M.T., Brandt E.B., Bass S.A., Daines M.O., Chakir J., Stringer K.F., et al. 2011. A nonredundant role for mouse Serpinb3a in the induction of mucus production in asthma. J. Allergy Clin. Immunol. 127:254–261: e1–e6 10.1016/j.jaci.2010.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg O.D., Ostrin E.J., Love M.I., Peng J.C., Bhakta N.R., Hou L., Nguyen C., Solon M., Nguyen C., Barczak A.J., et al. 2012. Airway epithelial miRNA expression is altered in asthma. Am. J. Respir. Crit. Care Med. 186:965–974 10.1164/rccm.201201-0027OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeyama K., Dabbagh K., Lee H.M., Agustí C., Lausier J.A., Ueki I.F., Grattan K.M., Nadel J.A. 1999. Epidermal growth factor system regulates mucin production in airways. Proc. Natl. Acad. Sci. USA. 96:3081–3086 10.1073/pnas.96.6.3081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeyama K., Dabbagh K., Jeong Shim J., Dao-Pick T., Ueki I.F., Nadel J.A. 2000. Oxidative stress causes mucin synthesis via transactivation of epidermal growth factor receptor: role of neutrophils. J. Immunol. 164:1546–1552 10.4049/jimmunol.164.3.1546 [DOI] [PubMed] [Google Scholar]
- Takeyama K., Fahy J.V., Nadel J.A. 2001a. Relationship of epidermal growth factor receptors to goblet cell production in human bronchi. Am. J. Respir. Crit. Care Med. 163:511–516 10.1164/ajrccm.163.2.2001038 [DOI] [PubMed] [Google Scholar]
- Takeyama K., Jung B., Shim J.J., Burgel P.R., Dao-Pick T., Ueki I.F., Protin U., Kroschel P., Nadel J.A. 2001b. Activation of epidermal growth factor receptors is responsible for mucin synthesis induced by cigarette smoke. Am. J. Physiol. Lung Cell. Mol. Physiol. 280:L165–L172 [DOI] [PubMed] [Google Scholar]
- Tang D., Mehta D., Gunst S.J. 1999. Mechanosensitive tyrosine phosphorylation of paxillin and focal adhesion kinase in tracheal smooth muscle. Am. J. Physiol. 276:C250–C258 [DOI] [PubMed] [Google Scholar]
- Tang D.D., Turner C.E., Gunst S.J. 2003. Expression of non-phosphorylatable paxillin mutants in canine tracheal smooth muscle inhibits tension development. J. Physiol. 553:21–35 10.1113/jphysiol.2003.045047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas B., Rutman A., Hirst R.A., Haldar P., Wardlaw A.J., Bankart J., Brightling C.E., O’Callaghan C. 2010. Ciliary dysfunction and ultrastructural abnormalities are features of severe asthma. J. Allergy Clin. Immunol. 126:722–729: e2 10.1016/j.jaci.2010.05.046 [DOI] [PubMed] [Google Scholar]
- Toda M., Tulic M.K., Levitt R.C., Hamid Q. 2002. A calcium-activated chloride channel (HCLCA1) is strongly related to IL-9 expression and mucus production in bronchial epithelium of patients with asthma. J. Allergy Clin. Immunol. 109:246–250 10.1067/mai.2002.121555 [DOI] [PubMed] [Google Scholar]
- Torgerson D.G., Ampleford E.J., Chiu G.Y., Gauderman W.J., Gignoux C.R., Graves P.E., Himes B.E., Levin A.M., Mathias R.A., Hancock D.B., et al. 2011. Meta-analysis of genome-wide association studies of asthma in ethnically diverse North American populations. Nat. Genet. 43:887–892 10.1038/ng.888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsao P.N., Wei S.C., Wu M.F., Huang M.T., Lin H.Y., Lee M.C., Lin K.M., Wang I.J., Kaartinen V., Yang L.T., Cardoso W.V. 2011. Notch signaling prevents mucous metaplasia in mouse conducting airways during postnatal development. Development. 138:3533–3543 10.1242/dev.063727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuvim M.J., Mospan A.R., Burns K.A., Chua M., Mohler P.J., Melicoff E., Adachi R., Ammar-Aouchiche Z., Davis C.W., Dickey B.F. 2009. Synaptotagmin 2 couples mucin granule exocytosis to Ca2+ signaling from endoplasmic reticulum. J. Biol. Chem. 284:9781–9787 10.1074/jbc.M807849200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyner J.W., Kim E.Y., Ide K., Pelletier M.R., Roswit W.T., Morton J.D., Battaile J.T., Patel A.C., Patterson G.A., Castro M., et al. 2006. Blocking airway mucous cell metaplasia by inhibiting EGFR antiapoptosis and IL-13 transdifferentiation signals. J. Clin. Invest. 116:309–321 10.1172/JCI25167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter P., Ron D. 2011. The unfolded protein response: from stress pathway to homeostatic regulation. Science. 334:1081–1086 10.1126/science.1209038 [DOI] [PubMed] [Google Scholar]
- Wills-Karp M., Luyimbazi J., Xu X., Schofield B., Neben T.Y., Karp C.L., Donaldson D.D. 1998. Interleukin-13: central mediator of allergic asthma. Science. 282:2258–2261 10.1126/science.282.5397.2258 [DOI] [PubMed] [Google Scholar]
- Woodruff P.G., Boushey H.A., Dolganov G.M., Barker C.S., Yang Y.H., Donnelly S., Ellwanger A., Sidhu S.S., Dao-Pick T.P., Pantoja C., et al. 2007. Genome-wide profiling identifies epithelial cell genes associated with asthma and with treatment response to corticosteroids. Proc. Natl. Acad. Sci. USA. 104:15858–15863 10.1073/pnas.0707413104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodruff P.G., Modrek B., Choy D.F., Jia G., Abbas A.R., Ellwanger A., Koth L.L., Arron J.R., Fahy J.V. 2009. T-helper type 2-driven inflammation defines major subphenotypes of asthma. Am. J. Respir. Crit. Care Med. 180:388–395 10.1164/rccm.200903-0392OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worgall T.S., Veerappan A., Sung B., Kim B.I., Weiner E., Bholah R., Silver R.B., Jiang X.C., Worgall S. 2013. Impaired sphingolipid synthesis in the respiratory tract induces airway hyperreactivity. Sci. Transl. Med. 5:186ra67 10.1126/scitranslmed.3005765 [DOI] [PubMed] [Google Scholar]
- Yamada K.M., Geiger B. 1997. Molecular interactions in cell adhesion complexes. Curr. Opin. Cell Biol. 9:76–85 10.1016/S0955-0674(97)80155-X [DOI] [PubMed] [Google Scholar]
- Young H.W., Williams O.W., Chandra D., Bellinghausen L.K., Pérez G., Suárez A., Tuvim M.J., Roy M.G., Alexander S.N., Moghaddam S.J., et al. 2007. Central role of Muc5ac expression in mucous metaplasia and its regulation by conserved 5′ elements. Am. J. Respir. Cell Mol. Biol. 37:273–290 10.1165/rcmb.2005-0460OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaidel-Bar R., Itzkovitz S., Ma’ayan A., Iyengar R., Geiger B. 2007. Functional atlas of the integrin adhesome. Nat. Cell Biol. 9:858–867 10.1038/ncb0807-858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Loch A.J., Radtke F., Egan S.E., Xu K. 2013. Jagged1 is the major regulator of Notch-dependent cell fate in proximal airways. Dev. Dyn. 242:678–686 10.1002/dvdy.23965 [DOI] [PubMed] [Google Scholar]
- Zhao J., Maskrey B., Balzar S., Chibana K., Mustovich A., Hu H., Trudeau J.B., O’Donnell V., Wenzel S.E. 2009. Interleukin-13-induced MUC5AC is regulated by 15-lipoxygenase 1 pathway in human bronchial epithelial cells. Am. J. Respir. Crit. Care Med. 179:782–790 10.1164/rccm.200811-1744OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhen G., Park S.W., Nguyenvu L.T., Rodriguez M.W., Barbeau R., Paquet A.C., Erle D.J. 2007. IL-13 and epidermal growth factor receptor have critical but distinct roles in epithelial cell mucin production. Am. J. Respir. Cell Mol. Biol. 36:244–253 10.1165/rcmb.2006-0180OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu L., Lee P.K., Lee W.M., Zhao Y., Yu D., Chen Y. 2009. Rhinovirus-induced major airway mucin production involves a novel TLR3-EGFR-dependent pathway. Am. J. Respir. Cell Mol. Biol. 40:610–619 10.1165/rcmb.2008-0223OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Ehre C., Abdullah L.H., Sheehan J.K., Roy M., Evans C.M., Dickey B.F., Davis C.W. 2008. Munc13-2−/− baseline secretion defect reveals source of oligomeric mucins in mouse airways. J. Physiol. 586:1977–1992 10.1113/jphysiol.2007.149310 [DOI] [PMC free article] [PubMed] [Google Scholar]