Key Points
CD28 delivers a pro-survival signal to MM cells via regulation of PI3K/Akt, FoxO3a, and Bim.
Blockade of CD28:CD80/CD86 in vivo resensitizes MM cells to chemotherapy and significantly reduces tumor burden.
Abstract
Chemotherapeutic resistance remains a significant hurdle in the treatment of multiple myeloma (MM) and is significantly mediated by interactions between MM cells and stromal cells of the bone marrow microenvironment. Despite the importance of these interactions, the specific molecules and downstream signaling components involved remain incompletely understood. We have previously shown that the prototypic T-cell costimulatory receptor CD28, which is also expressed on MM cells, is a key mediator of MM survival and apoptotic resistance. Crosslinking CD28 by agonistic antibodies or myeloid dendritic cells (DC; these express the CD28 ligands CD80/CD86) prevents apoptosis caused by chemotherapy or serum withdrawal. We now report that CD28 pro-survival signaling is dependent upon downstream activation of phosphatidyl-inositol 3-kinase/Akt, inactivation of the transcription factor FoxO3a, and decreased expression of the pro-apoptotic molecule Bim. Conversely, blocking the CD28–CD80/CD86 interaction between MM cells and DC in vitro abrogates the DC’s ability to protect MM cells against chemotherapy-induced death. Consistent with these observations, in vivo blockade of CD28–CD80/CD86 in the Vk*MYC murine myeloma model sensitizes MM cells to chemotherapy and significantly reduces tumor burden. Taken together, our findings suggest that CD28 is an important mediator of MM survival during stress and can be targeted to overcome chemotherapy resistance.
Introduction
Multiple myeloma (MM), the bone marrow (BM)-resident plasma cell (PC) neoplasm, is the second most common hematologic malignancy after non-Hodgkin lymphoma.1 Although new therapies have improved survival, MM remains almost uniformly fatal and only curable in a small fraction of patients.2,3 Initially, patients are responsive to therapy and experience remission; however, relapses result in MM cells that are progressively resistant to therapy.3,4 Thus, understanding and overcoming resistance mechanisms may lead to development of new therapeutic approaches.
Chemotherapies such as the DNA alkylator melphalan and the proteasome inhibitor bortezomib were developed because of their direct apoptotic effects on MM cells.5,6 However, these agents, thalidomide, and thalidomide derivatives also target the BM microenvironment, pointing to the key role that stroma plays in myeloma survival.6-8 Moreover, primary MM culture in vitro requires stroma, indicating that the BM niche provides essential pro-survival signals.9-11 Thus, identifying key interactions between MM and the microenvironment is essential for understanding and overcoming therapeutic resistance mechanisms.
Broadly, MM–stromal interactions fall into 2 categories. The first consists of soluble pro-survival factors induced from stromal niche cells upon MM interaction, and include interleukin-6 (IL-6),12,13 indolamine-2, 3-dioxygenase,14 APRIL, and B-cell activating factor.14-16 The second category consists of contact-dependent interactions between MM cells and extracellular matrix17,18 or stromal cells.14,19,20 Perhaps best characterized are integrin-dependent cell adhesion–mediated drug resistance17,21 and Notch signaling.22 Both interactions halt cell cycle, regulate apoptotic molecules, and induce chemotherapy resistance. Despite the central importance of cell–cell interactions, the body of literature examining these contacts is small, pointing to a lack of understanding regarding specific molecular components that enhance survival and chemotherapy resistance.
Expression of receptors that support MM survival would be predicted to correlate with worse prognosis or progression, consistent with a pro-survival role under treatment pressure. One such molecule is CD28, best characterized as the prototypic T-cell costimulatory receptor. CD28 activation together with “signal 1” through the T-cell receptor enhances function and survival.23,24 Although expressed on PC and MM cells,25 CD28 function in the B-cell lineage has been largely unexplored. We have reported that CD28 signaling is critical for murine BMPC survival and durable antibody titers, demonstrating CD28 is necessary for normal PC biology26. We also observed that CD28 activation in vitro protects MM cells from chemotherapy-induced death.20 CD28’s role as a pro-survival receptor for MM is consistent with the observation that CD28 is overexpressed on 26.5% of primary MM cells at diagnosis, 59% in medullary relapse, 93% in extramedullary relapse, and 100% of cell lines.27 Moreover, CD28 overexpression is prognostically correlated with worse outcomes after high-dose chemotherapy.28-30 Many CD28+ MM cells also coexpress CD86,27 one of CD28’s ligands. CD86 expression has been separately found to be a poor prognostic indicator,31 raising the possibility that MM uses CD28:CD86 cis interactions to deliver a pro-survival signal. Collectively, these data suggest CD28 supports survival, allowing for disease progression despite treatment.
A pro-survival role for CD28 in MM points to cells that express its ligands CD80/CD86 as possible niche partners. CD80/CD86+ cells include B cells, macrophages, and dendritic cells (DC),24 and we and others have found that macrophages and DC are pro-survival components of the MM niche.14,19,20 We have previously shown that MM–DC coculture transduces a pro-survival signal directly to MM cells and “back-signals” through CD80/CD86 on DCs to induce DC production of IL-6 and indolamine-2, 3-dioxygenase. We hypothesize that blocking CD28 interactions in vivo would inhibit MM-intrinsic pro-survival signals and stromal induction of a “soluble” pro-survival/immunosuppressive microenvironment, doubly sensitizing MM to chemotherapy.
Currently, the CD28 downstream components in myeloma cells are poorly characterized. However, CD28 signaling in T cells is more clearly delineated and involves the phosphatidyl-inositol 3-kinase (PI3K)/Akt pathway.32,33 Similar to T cells, we have reported that CD28 activation in MM cells induces PI3K signaling—leading us to hypothesize that CD28→PI3K→Akt signaling may mediate MM apoptotic resistance.20 This would be consistent with the general role PI3K/Akt plays in MM biology, where it mediates survival and proliferation.34,35 Based on the predictions of this hypothesis, we examined the effects of CD28 inhibition on MM survival in vitro and in vivo, and characterized downstream molecules in this pathway.
Materials and methods
Cells
MM.1S (gift of Dr. Steven Rosen, Robert H. Lurie Cancer Center, Chicago, IL) and U266, RPMI8226, and KMS11 human myeloma cell lines (American Type Culture Collection, Rockville, MD) were cultured as previously described14 in RPMI1640 (CellGro, Corning, NY), 10% fetal bovine serum (Thermo Fisher Scientific Hyclone, Waltham MA), 100 U/mL penicillin, 100 μg/mL streptomycin, and 2 mM L-Glut (all CellGro). Monocytes were purified from human blood using EasySep (Stem Cell Technologies, Vancouver, Canada) or MACS kits (Miltenyi Biotec Inc. Auburn, CA) per manufacturer’s instructions and differentiated to DC as previously described14 with granulocyte macrophage–colony-stimulating factor (Sigma-Aldrich, St. Louis, MO; 10 ng/mL) and IL-4 (R&D, Minneapolis, MN; 1000 U/mL) for 7 days.
DC-MM coculture
A total of 5 × 104 MM.1S, U266, RPMI8226, or KMS11 cells were cultured with 5 × 104 monocyte-derived DC (MoDC) ± melphalan (Sigma-Aldrich; 2-5 μM) for 48 hours in 200 μL in 96-well plates. CTLA4-Ig (100 μg/mL; DNA vector kind gift of Dr. Peter Linsley, AVI Biopharma) or anti-CD28 monoclonal antibodies (mAb) CD28.6 (10 μg/mL; kind gift of Dr. Daniel Olive, INSERM) blocked CD28–CD80/CD86. Cells were stained for CD11b-PE to gate out DC (Beckman Coulter, Brea, CA), Annexin V-fluorescein isothiocyanate (FITC; BioVision, Inc, Milpitas CA), and 7AAD (BD Pharmingen, San Jose, CA).
Animals
Vk*MYC mice were housed and bred at the Division of Laboratory Animal Resources (Roswell Park Cancer Institute, Buffalo, NY) in a pathogen-free barrier facility. Roswell Park Cancer Institute Institutional Animal Care and Use Committee approved all animal experiments.
Myeloma cell isolation
MM/PC were isolated from mice as previously described26 using a CD138+ murine plasma cell isolation kit (Miltenyi Biotech). The CD138+ population was >70% pure.
Antibodies and reagents
Murine BM cells were stained as previously described.26 Polyclonal control hamster immunoglobulin G (IgG) and anti-CD28 mAb (clone PV1; Beckman Coulter; gift from Dr. Carl June; University of Pennsylvania, Philadelphia, PA) were conjugated to Dynabeads goat anti-mouse IgG (Invitrogen, Grand Island, NY) per manufacturer instructions.
For survival, cells were stained with Annexin V-FITC and 7AAD and the double-negative population was determined by flow cytometry (FACSCalibur 2, BD; FCS Express Software). Survival by trypan blue exclusion was assessed as previously described26 for experiments in which addition of antibody-conjugated beads interfere with viability assessment by flow cytometry.
For CD28 lentiviral knockdown, 1 × 105 cells stained with anti-CD28-PE (BD Pharmingen) or appropriate isotype control (BD Pharmingen) were analyzed (FlowJo software).
For intracellular staining, cells were prepared following manufacturer’s instructions using the eBiosciences FoxP3 kit (San Diego, CA) and stained with Thr308-specific anti-phospho-Akt (1:100 dilution, 60 minutes; Cell Signaling, Danvers, MA). Cells were washed and stained with donkey anti-rabbit-FITC (1:100 dilution, 60 minutes; Jackson ImmunoResearch Laboratories, Inc, West Grove, PA). Cells were fixed and assayed by flow cytometry.
CTLA4-Ig was isolated from spent Cos-7 cell medium. CTLA4-Ig protein was quantified using BioRad colorimetric assay (Hercules, CA). Anti-CD28 monoclonal Ab (CD28.2, Beckman Coulter) was used at 10 μg/mL.
LY294002 and Akt Inhibitor II (Calbiochem/Millipore, Billerica, MA) were prepared following manufacturer’s instructions.
Western blots
Western blot analysis was performed as previously described.20 Briefly, cells were lysed using RIPA buffer, protein was quantitated, separated using 10% to 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis gel, electroblotted to nitrocellulose, and probed with antibodies specific for Bim, total FoxO3a, phospho-FoxO3a, total Akt, phospho-Akt, Mcl-1, or actin (all Cell Signaling).
Reverse transcription-polymerase chain reaction (RT-PCR) and quantitative PCR
RNA was prepared using TRIZOL (Invitrogen, Carlsbad, CA) and complementary DNA (cDNA) using the Superscript III kit (Invitrogen) following manufacturer instructions. Bim primers: (forward: 5′-AGAATTCATGGCAAAGCAACCTTCTGATGTAAG-3′ and reverse: 5′-TGATATCAATGCATTCTCCACACCAGGCGGAC-3′), product sizes 610, 450, and 320 bp.36 FoxO3a primers: (forward: 5′- GCCGCGCAGCCAAGAAGAAGG-3′ and reverse 5′-AGTGGGCGATGGCTGGGATGG-3). Actin primers: (forward: 5′-CCCAGCACAATGAAGATCAAGATCAT-3′ and reverse: 5′-ATCTGCTGGAAGGTGG ACAGCGA-3′). Densitometry was performed with Quantity One software.
For quantitative PCR (qPCR), RNA from ∼5 × 105 cells was extracted (Qiagen RNEasy Minikit) following manufacturer’s instructions. cDNA was prepared from 1 µg RNA (Applied Biosystems High Capacity cDNA Reverse Transcription Kit), and qPCR performed (7500 Fast Real-Time PCR System) with Taqman reagents (Applied Biosystems). CD28 messenger RNA (mRNA) quantification probe: Hs00174796_m1. For glyceraldehyde-3-phosphate dehydrogenase (GAPDH) and β-Actin, TaqMan endogenous control probes were used.
ELISA
Total IgG was determined by enzyme-linked immunosorbent assay (ELISA; Bethyl Laboratories, Inc., Montgomery, TX) as previously described.26 In brief, NUNC 96-well plates were precoated with capture antibody in coating buffer overnight at 4°C. Serum was diluted 1:100 000-1:200 000 in sample diluent (Bethyl) and plated following manufacturer’s instructions.
Transfection
MM.1S were transfected with scramble, FoxO3a, or Bim small interfering RNA (siRNA) (siGENOME SMARTpool, Dharmacon Thermo Scientific) using an Amaxa transfection kit. Cells were rested 24-48 hours and plated in experimental conditions for 24-48 hours. Knockdown was confirmed by western blot and RT-PCR.
Lentivirus-containing shRNA infection
CD28 and GAPDH short hairpin RNA (shRNA) clones (shCD28 clone, TRCN0000057679; shGAPDH, TRCN0000025862) were obtained from Open Biosystems. Viral particles were prepared according to manufacturer’s instructions. A total of 400 µL of viral supernatant was applied to 2 × 106 myeloma cells in 2 mL media containing 0.4 µg/mL polybrene, then centrifuged at 2250 rpm for 90 minutes at 37°C. Media was aspirated and cells were resuspended at 1 × 105/mL in complete media in 6-well plates at 3 mL/well.
Statistics
Pairwise comparisons were conducted using the Student t test.
Results
CD28 signaling induced by DC or other MM cells prevents myeloma cell death
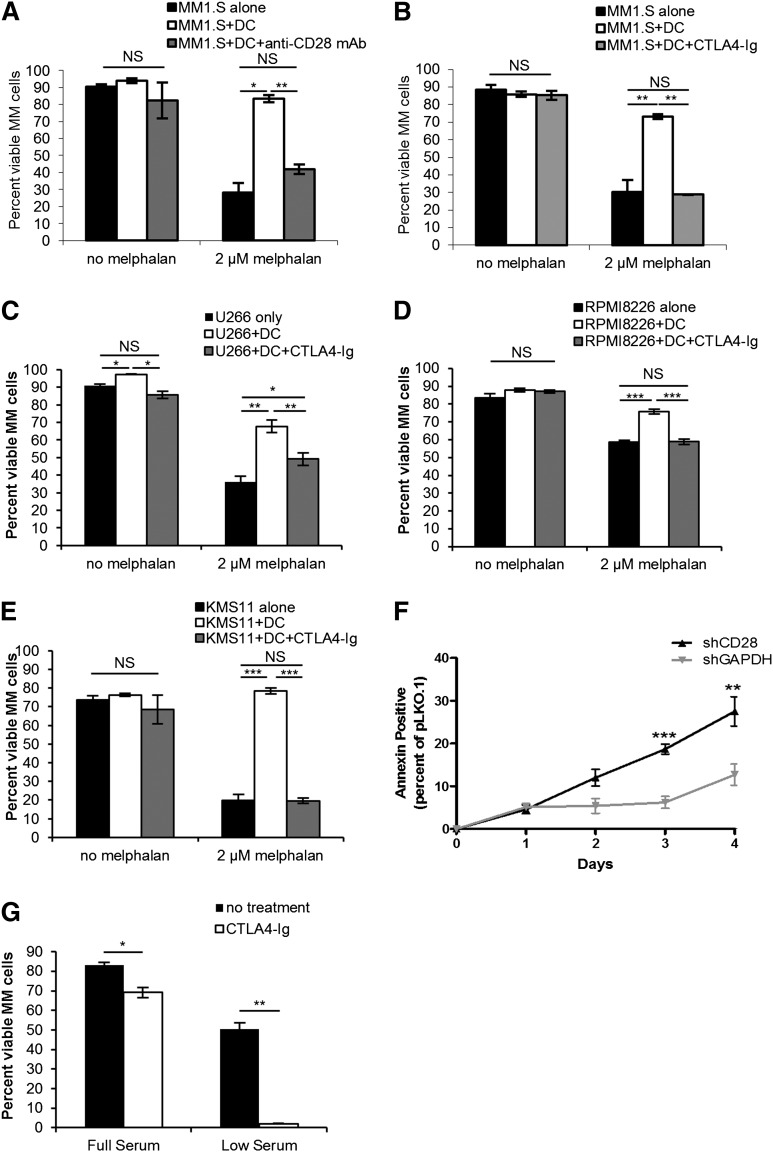
We have previously reported that antibody-mediated CD28 activation inhibits MM apoptosis; however, this is unlikely to completely recapitulate authentic MM–stroma interactions. Because DC express CD80/CD86 and are pro-survival in the BM niche, we examined CD28’s role in this MM–DC interaction. MM.1S myeloma cells were cocultured with human MoDC ± melphalan ± CD28 blocking antibody (Figure 1A). Melphalan was chosen because high-dose melphalan plus autologous stem cell rescue is a therapeutic mainstay for many patients, and thus resistance is predicted to be a main cause of treatment failure. In media alone, MM survival was not significantly different with MoDC or αCD28. Melphalan significantly reduced MM survival, but coculture with MoDC almost completely prevented MM apoptosis. However, CD28 blockade almost completely reversed this protection. On the DC side, we predicted that CTLA4-Ig (consisting of the CTLA4 extracellular domain fused to human IgG Fc) would sensitize MM cells to chemotherapy as it binds to CD80/CD86 and blocks CD28 engagement. Indeed, although melphalan significantly decreased MM survival that was rescued with MoDC, CTLA4-Ig completely abrogated this protection (Figure 1B). We observed a similar dependence upon CD28 signaling for survival in U266, RPMI8226, and KMS11 myeloma lines (Figure 1C-E).These data suggest that even in the molecularly complex MM–DC cellular interactions, CD28 delivers the predominant pro-survival signal.
Figure 1.
CD28 signaling induced by DC or other MM cells prevents myeloma cell death. MM cells (MM.1S) were cultured alone or with DC at a 1:1 ratio ± 2 µM melphalan ± 50 µg/mL of the blocking αCD28 mAb CD28.6 (A) or ± 100 µg/mL CTLA4-Ig (B) or for 72 hours. Cell survival was analyzed by flow cytometry for Annexin V/7AAD staining and DC were gated out using CD11b. U266 (C), RPMI8226 (D), or KMS11 (E) myeloma cells were cultured as in (B) for 72 hours and survival was assessed by flow cytometry. (F) RPMI8226 myeloma cells were infected with lentiviral particles encoding shRNA specific for CD28, GAPDH, or empty vector (pLKO.1) and cultured for 4 days in full serum media. Survival was assessed by Annexin V staining. (G) MM.1S cells were cultured in either 10% serum or 0.2% (low) serum conditions for 5 days ± 100 µg/mL CTLA4-Ig. Fifty percent of the media was changed every other day to prevent nutrient depletion, and new CTLA4-Ig was added with every media change. Cell survival was analyzed by flow cytometry for Annexin V/7AAD staining. Data for panels A and B) are representative of 4 individual experiments; data for panels C-E are representative of 2 individual experiments. *P < .05, **P < .01, ***P < .005. NS, not significant.
Because many myelomas expressing CD28 also coexpress CD8627,31 (see supplemental Figure 1 on the Blood Web site), we asked if cis interactions between myeloma cells are also providing a pro-survival signal. Although melphalan’s ability to kill MM cultured alone (Figures 1A-1E, right black bars) suggests that a cis CD28–CD86 interaction between MM cells is not as potently pro-survival as the trans CD28–CD80/CD86 interaction between MM and DC, a <50% CD28 knockdown (supplemental Figure 2) in a stromally independent MM cell line still leads to >30% death in 96 hours (Figure 1F). The same effect also occurs in other MM lines, including MM.1S (unpublished observation, C.M.G. and L.H.B.). Consistent with this death induction, we were unable to generate stable CD28 knockdowns in MM (data not shown). We further examined this in MM.1S cultured in full serum or under stress in low serum ± CTLA4-Ig. Consistent with Figure 1D, myeloma survival was modestly but significantly decreased with CTLA4-Ig in full serum, but was markedly decreased in low serum (Figure 1G), revealing that the CD28-CD86 MM-MM cis interaction contributes to basal survival and is essential under stress.
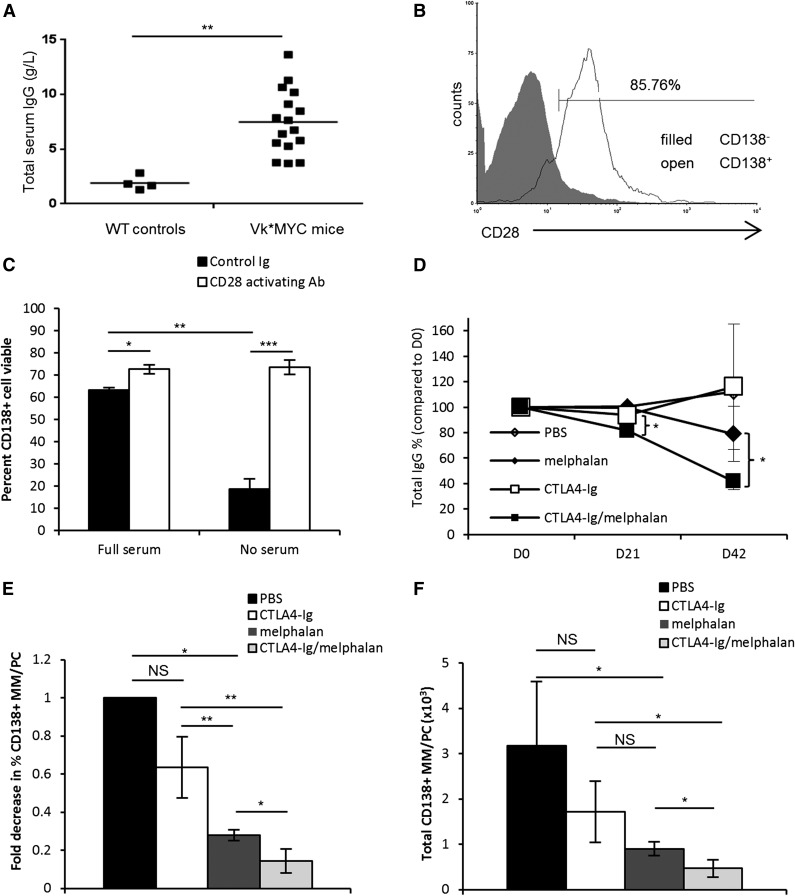
CD28 signaling blockade in vivo sensitizes a murine myeloma model to chemotherapy
The preceding data suggest that despite the complex nature of MM–stroma interactions, CD28 is a key mediator in MM survival in vitro. To examine the potential in vivo role for CD28–CD80/CD86, we used the immunocompetent, endogenously arising Vk*MYC murine myeloma model.37 Vk*MYC mice develop an indolent PC dyscrasia closely mimicking human MM with elevated immunoglobulin levels and M spike.37 Mice with tumor burden (measured by total serum IgG, Figure 2A) have elevated cell numbers expressing PC/MM marker CD138 and coexpressing CD28 (Figure 2B). Isolated CD138+ cells were cultured ± serum ± CD28 activating antibody to examine CD28’s potential pro-survival role (Figure 2C). In the full-serum control, Vk*MYC cells are 63 ± 1.1% viable—with baseline decreased survival pointing to their BM stroma dependence. CD28 activating antibody modestly, but significantly, increases survival. Serum withdrawal drops viability to 19 ± 4.6% but CD28 activation significantly increases this to 73 ± 3.2%—thus, as with human MM, CD28 activation is pro-survival in murine Vk*MYC MM cells in vitro.
Figure 2.
CD28 signaling protects Vk*MYC murine myeloma cells in vitro and blockade sensitizes MM to melphalan in vivo. (A) Seventy-two-week-old Vk*MYC mice or their wild-type (WT) littermate controls were screened by ELISA for total serum IgG levels. (B) Whole bone marrow from Vk*MYC mice was isolated and the percent of myeloma cells was determined using a CD138+CD28+B220−CD38−MHCII−CD3− phenotype. (C) Purified CD138+ cells from disease-bearing Vk*MYC mice were plated for 24 hours in media containing 10% fetal bovine serum (full serum) or no serum. Cells were cultured with either hamster Ig-coated beads (isotype control) or CD28-activating antibody-coated beads (clone PV1) at a ratio of 2 beads:1 cell. Cell viability was assessed by trypan blue exclusion. (D) Based on titers as in panel A, mice were randomized into 4 treatment groups (n = 3-4 mice/group): PBS, melphalan alone (2.0 mg/kg), CTLA4-Ig alone (100 μg/mouse), or melphalan plus CTLA4-Ig. Mice were treated intraperitoneally every third day for 42 days and serum samples were drawn weekly. Total serum IgG was determined by ELISA and was plotted as total IgG percent compared with day 0. (E) Percent MM/PC was determined using multiparametric flow for CD138+CD28+B220−CD38−MHCII−CD3− cells, and fold decrease was calculated compared with the PBS group. (F) Total numbers of MM/PC were calculated by multiplying the percent MM/PC as determined in panel E by the total number of cells counted for each tissue. Data are representative of 2 separate experiments. *P < .05, **P < .01, ***P < .005.
To examine CD28’s role in vivo, we treated diseased Vk*MYC mice (Figure 2A) with phosphate-buffered saline (PBS), melphalan, CTLA4-Ig, or melphalan/CTLA4-Ig. Because melphalan alone effectively reduces tumor burden in this model,37 the dose administered (2.0 mg/kg) was deliberately subtherapeutic to unmask any effect of CTLA4-Ig treatment in enhancing control of the myeloma. PBS or CTLA4-Ig alone did not reduce tumor burden as measured by serum IgG levels (Figure 2D). The latter observation is consistent with the finding that CTLA4-Ig treatment without a death signal has only slight effects on myeloma survival (Figure 1A). Melphalan nonsignificantly reduced tumor burden at day 42. However, CTLA4-Ig/melphalan demonstrated a significant reduction in tumor burden by day 21, with a greater 59% reduction by day 42 (Figure 2D). The change in Ig was mirrored in MM percentage (Figure 2E) and absolute number (Figure 2F) in the BM. CTLA4-Ig treatment alone slightly, but not significantly, decreased percentage and total numbers compared with PBS. Melphalan alone significantly decreased total MM number and percentage. The fact that this did not correlate with a significant decrease in serum IgG at the same time point may reflect the ∼14-day serum immunoglobulin half-life38—ie, that IgG is a lagging indicator of treatment response. CTLA4-Ig and melphalan together reduced myeloma burden most, decreasing numbers 50% more than melphalan alone. Moreover, total number and percentage of T cells (the other major CD28+ population) remained unchanged between treatment groups (supplemental Figure 3), demonstrating this was not nonspecific killing of all CD28+ cells. These results suggest CTLA4-Ig–induced CD28:CD80/CD86 blockade reverses MM chemotherapy resistance in vivo, translating into significantly improved tumor killing.
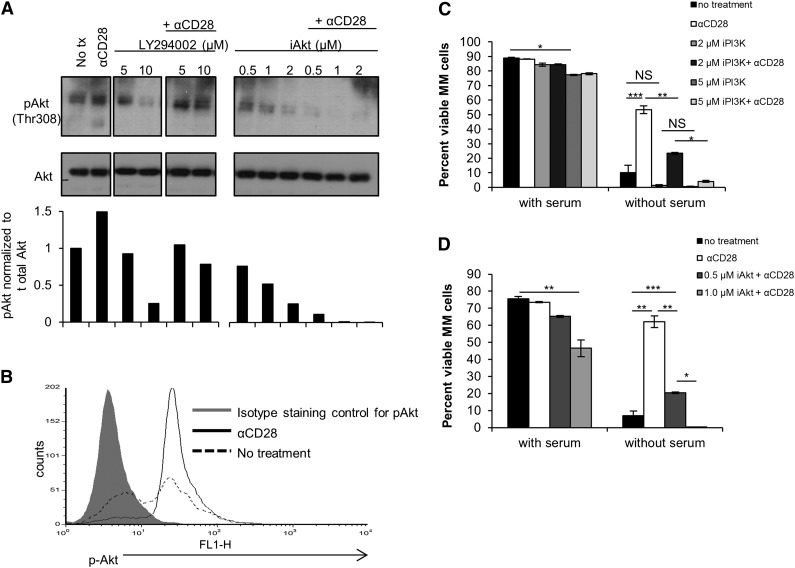
CD28 pro-survival signaling is dependent on PI3K and Akt
The previous data suggest CD28 signaling is critical for MM survival in vitro and in vivo. However, the specific signaling pathway downstream of CD28 in MM is almost completely uncharacterized. We and others have previously shown in MM that PI3K is phosphorylated upon CD28 engagement,20 consistent with T-cell CD28 signaling.32,33 Moreover, generalized PI3K/Akt signaling has been implicated as a pro-survival pathway for MM,39 prompting us to examine PI3K/Akt signaling downstream of CD28. For signaling assays, serum-free conditions were used as a death signal to reduce the influence of serum factors that may also signal via PI3K/Akt, such as IGF-1.40 By western blot (Figure 3A) and intracellular staining (Figure 3B), we confirmed that CD28 activation increases phospho-Akt levels, which is abrogated in a dose-dependent fashion by the PI3K inhibitor LY294002 or the Akt inhibitor iAkt II (Figure 3A). We evaluated PI3K’s role downstream of CD28 (Figure 3C; supplemental Figure 4) and found that in full serum, the 2-μM inhibitor dose had no effect on MM viability, and the 5-μM dose reduced viability 11.6%. In serum-free conditions without PI3K inhibition, viability was significantly reduced, and this was largely reversed with CD28 activation. PI3K inhibition in serum-free conditions does not significantly reduce survival further compared with no treatment. However, PI3K inhibition prevented CD28-mediated pro-survival signaling in a dose-dependent fashion, suggesting PI3K is critical for this pathway. To examine Akt’s functional role, MM.1S were cultured with iAkt II (0.5-1.0 µM) ± CD28 activation ± serum (Figure 3D). Although there was significant survival reduction with Akt inhibition in full serum, the impact of Akt inhibition was substantially greater in serum-free conditions, and CD28’s pro-survival effect was inhibited in a dose-dependent fashion. Together, these data suggest CD28-mediated survival activation is dependent on downstream PI3K/Akt signaling.
Figure 3.
CD28-mediated pro-survival signaling is dependent on PI3K and Akt. (A) MM.1S cells were cultured in full serum ±10 µg/mL CD28 activating mAb (CD28.2) and ± PI3K inhibitor LY294002 or ± iAkt II at the indicated doses. Cells were collected after 2 hours assessed by western blot. (B) MM.1S cells were cultured ± serum ± 10 µg/mL CD28.2 mAb. After 24 hours, cells were isolated, permeabilized, and stained intracellularly for phosphorylated Akt, which was assessed by flow cytometry. (C) MM.1S cells were cultured ± serum ±10 µg/mL CD28 activating mAb (CD28.2), and ± PI3K inhibitor LY294002 at the indicated doses. Cells were collected after 72 hours and viability was assessed via Annexin V and 7AAD staining by flow cytometry. (D) MM.1S cells were cultured ± serum ± 10 µg/mL αCD28.2 and ± Akt inhibitor (Akt inhibitor II) at the indicated doses. Cells were collected after 72 hours and viability was assessed via Annexin V and 7AAD staining by flow cytometry. Data for panels C-D) are representative of 3 independent experiments, and data for panels A-B are representative of 2 independent experiments. *P < .05, **P < .01, ***P < .001.
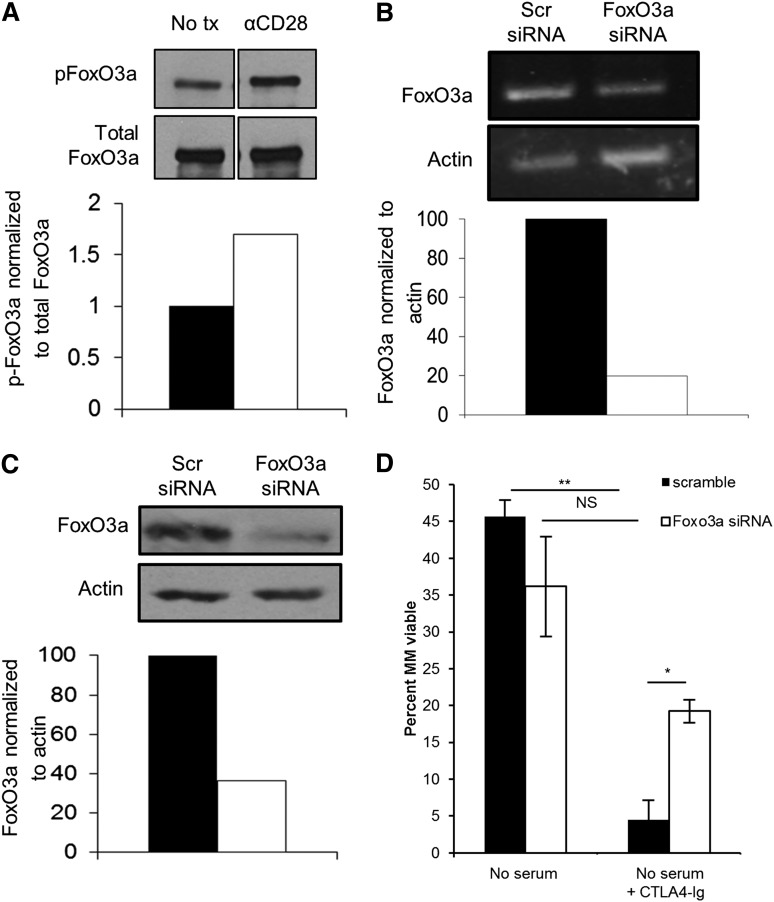
FoxO3a is downstream of CD28 and regulates myeloma cell survival
There are many potential Akt targets that could play a role in myeloma survival. We examined the effects of transcription factor FoxO3a because of its known role in regulating apoptotic molecule expression41,42 and its inhibition by Akt.43 Activated Akt induces FoxO3a phosphorylation—causing FoxO3a nuclear export and degradation.44 Unphosphorylated FoxO3a translocates into the nucleus and acts as a tumor suppressor, mainly through transcriptional upregulation of pro-apoptotic proteins Bim and Puma and downregulation of inhibitory caspase 8 mimic FLIP.41,42,45-47 CD28 signaling inactivates FoxO3a by increasing phospho-FoxO3a levels (Figure 4A). Because unphosphorylated FoxO3a is an apoptosis inducer in other systems,41,46,48 we predicted FoxO3a knockdown (80% by mRNA, 65% by protein, Figure 4B,C) would blunt death induced by blocking MM-MM CD28–CD86 interactions with CTLA4-Ig. In serum-free conditions, scramble and FoxO3a siRNA-treated cells were similarly viable (Figure 4C). Scramble siRNA-treated cell viability was reduced to <10% with CTLA4-Ig (similar to Figure 1A). However, CD28 blockade–induced death is significantly less with FoxO3a knockdown (Figure 4D), indicating that FoxO3a is an important survival/apoptosis mediator downstream of CD28.
Figure 4.
CD28 signaling induces phosphorylation of FoxO3a and knockdown of FoxO3a partially prevents CD28 blockade–induced apoptosis. (A) MM.1S cells were cultured in serum-free media for 24 hours ± 10 μg/mL αCD28.2. Cells were then analyzed by western blot for phospho-FoxO3a (top) or total FoxO3a (bottom). Densitometry was assessed using Quantity One software. (B) MM.1S cells were cultured for 24 hours in melphalan ± 10 µg/mL αCD28.2. Cells were lysed and RNA was collected. Semiquantitative RT-PCR was conducted (top) and assessed by densitometry (bottom). (C) A total of 1 × 106 cells were transfected with FoxO3a or scramble siRNA and FoxO3a expression was assessed by western blot after 48 hours. Densitometry was assessed using Quantity One software and is compared with the scramble siRNA. (D) Cells were transfected with siRNA as in panels B-C; 48 hours later, cells were plated in serum-free medium ± 100 µg/mL CTLA4-Ig. Cells were harvested after 48 hours and survival was assessed by Annexin V/7AAD staining by flow cytometry. Data are representative of 3 separate experiments, except for panel B, which is representative of 2 separate experiments. *P < .05, **P < .01. tx, treatment.
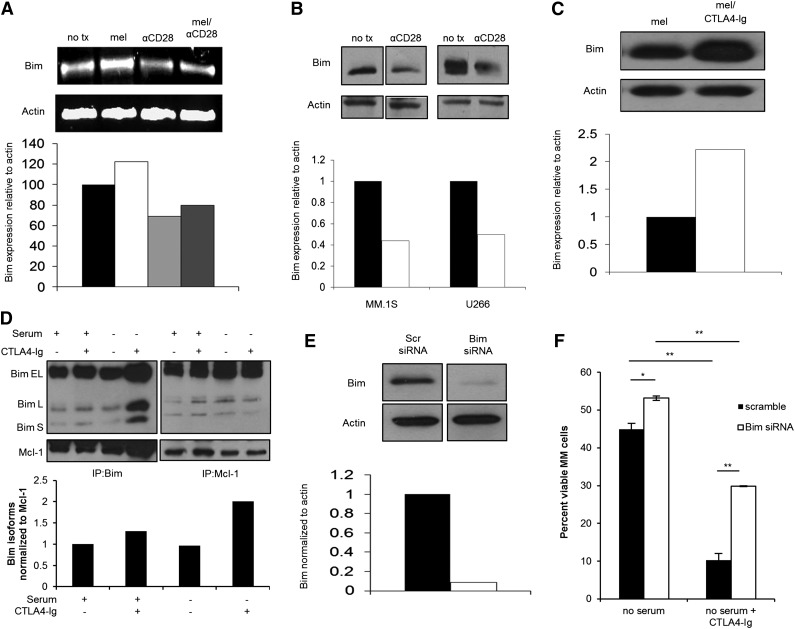
Bim is downstream of CD28 signaling and regulates myeloma cell survival or apoptosis
Our preceding data suggest that apoptotic proteins are downstream of FoxO3a. One likely candidate is the pro-apoptotic protein Bim, which has been implicated in cell adhesion–mediated drug resistance.21 We predicted CD28-mediated Bim regulation would be transcriptional via FoxO3a phosphorylation, and found melphalan treatment increased Bim mRNA by 22% (Figure 5A). CD28 activation decreased Bim mRNA expression by 29% and importantly prevented melphalan-induced Bim upregulation. Bim protein expression in MM.1S and U266 was markedly decreased with CD28 activation (Figure 5B). Conversely, CTLA4-Ig/melphalan doubled Bim protein vs melphalan alone (Figure 5C). CD28 activation in normal murine BMPC also reduced Bim expression (supplemental Figure 4), demonstrating CD28-mediated Bim downregulation is rooted in normal PC biology.
Figure 5.
CD28 signaling regulates Bim expression levels, and knockdown of Bim partially prevents CD28 blockade–induced apoptosis. (A) MM.1S cells were cultured for 72 hours in melphalan ± 10 μg/mL αCD28.2. Cells were lysed and RNA was collected. Semiquantitative RT-PCR was conducted (top) and assessed by densitometry (bottom). (B) MM.1S and U266 cells were cultured for 72 hours in serum-free conditions ± 10 μg/mL αCD28.2. Lysates were made and assessed by western blot. Densitometry was assessed using Quantity One software (bottom). (C) MM.1S cells were cultured for 72 hours in melphalan ± 100 μg/mL CTLA4-Ig. Lysates were made and assessed by western blot (top). Densitometry was assessed using Quantity One software (bottom). (D) U266 cells were cultured in full serum or serum-free media ± 100 μg/mL CTLA4-Ig for 48 hours. Lysates were prepared and Bim (left) or Mcl-1 (right) was immunoprecipitated and analyzed by western blot for Bim or Mcl-1 expression. Densitometry of all 3 Bim isoforms was averaged and compared relative to Mcl-1 in the Bim IP and was performed using Quantity One software (bottom). (E) MM.1S cells were transfected with Bim or scramble siRNA and Bim expression was assessed by western blot after 48 hours (top). Percent silencing was calculated using densitometry (bottom). (F) Cells transfected in panel E were plated in serum-free medium ± 100 µg/mL CTLA4-Ig. Cells were harvested after 48 hours and survival was assessed by Annexin V/7AAD staining on flow cytometry. Data are representative of 3 separate experiments except for panel D, which is representative of 2 separate experiments. **P < .01 ***P < .001.
Most pro-apoptotic proteins are counterbalanced by an anti-apoptotic binding partner that prevents death. The Bim isoforms (extra-long, long, and short) are bound and inactivated by anti-apoptotic molecules, including Mcl-1. Because Bim and Mcl-1 can vary inversely in MM,49 we examined Mcl-1 expression. Surprisingly, we did not observe differences in Mcl-1 with CTLA4-Ig treatment (supplemental Figure 5), suggesting changes in Bim may be sufficient to induce apoptosis. We therefore assessed how newly transcribed Bim may interact with Mcl-1. Because U266 depends upon Mcl-1:Bim interactions for survival,50 we cultured U266 ± serum ± CTLA4-Ig, and coimmunoprecipitated Bim or Mcl-1. Neither CTLA4-Ig nor serum withdrawal changed the amount of Bim bound to Mcl-1 compared with full serum in the Bim immunoprecipitation (Figure 5D, top left). However, CTLA4-Ig and serum withdrawal together markedly increased the Bim isoforms:Mcl-1 ratio (Figure 5D, bottom), indicating this treatment increased total Bim. However, when Mcl-1 is immunoprecipitated, there are no differences in the Bim:Mcl-1 ratio for any treatment, suggesting CTLA4-Ig–induced Bim is not Mcl-1–bound and is therefore able to induce apoptosis.
These data are correlative, so to test Bim’s functional role in the CD28 survival pathway, we silenced Bim (>90%, Figure 5E) and found that scramble siRNA-treated MM.1S cultured in serum-free conditions are 45% alive. Bim siRNA-treated cells had slightly (but significantly) improved survival. CTLA4-Ig reduced scramble-treated cell viability to <10%, but Bim knockdown significantly ameliorated death from CD28 blockade (Figure 5F), suggesting that CD28-mediated Bim regulation is important for survival. However, survival is not completely restored, suggesting other factors downstream of CD28 may play a role in survival.
Discussion
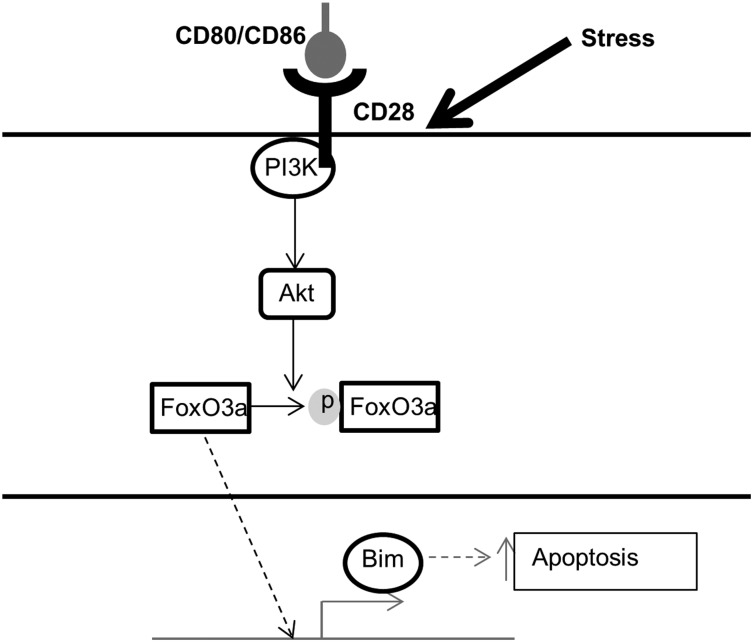
Myeloma survival depends upon interactions between the MM cell and the stromal/cellular compartment of the BM, similar to normal BMPC. We have reported that CD28 signaling is essential for BMPC survival26 and transduces a pro-survival signal directly to MM cells.20 Here, we characterize the specific molecules of CD28’s signaling pathway and identify PI3K/Akt as necessary components (Figure 6). We have shown that PI3K/Akt inhibition abrogated CD28’s pro-survival signal in a dose-dependent fashion. Although it is formally possible that this was due to off-target inhibitor effects, the observation that CD28 induces Akt phosphorylation supports the conclusion that CD28 is activating a PI3K→Akt signal. Because FoxO3a is an Akt target, we examined the FoxO3a regulation downstream of CD28 and found that CD28 activation increased phospho-FoxO3a. Moreover, FoxO3a knockdown prevented most CD28 blockade–induced death, suggesting its role in this pathway. In the final step, we observed that CD28 activation downregulated Bim expression in human MM cells and murine PC—consistent with a role for CD28-mediated Bim regulation in PC and MM biology. Conversely, blocking CD28–CD86 with CTLA4-Ig upregulated Bim expression, correlating with an increase in unbound Bim.
Figure 6.
Proposed mechanism of CD28 signaling in myeloma cells. Schematic of CD28-mediated pro-survival signaling pathway in MM cells. Under stress conditions, CD28 activates PI3K and Akt, which induces the phosphorylation and inactivation of FoxO3a. Phospho-FoxO3a is excluded from the nucleus and cannot enact its transcriptional program, including transcription of the pro-apoptotic molecule Bim. Dashed arrows indicate inactive pathways.
The PI3K/Akt/FoxO3a/Bim pathway is conserved across many malignancies. Signaling via this pathway downstream of sphingosine kinase 1 confers apoptotic resistance in gliomas.48 In paclitaxel-resistant breast cancer cell lines, Akt hyperactivation induces FoxO3a phosphorylation and decreases Bim, resulting in apoptotic resistance.46 Consistent with our findings, Munugalavadla et al have recently demonstrated that PI3K inhibition induced apoptosis, downregulated phospho-FoxO3a, and upregulated Bim in MM cells, although specific receptors delivering this signal were not determined.51 Our data suggest that 1 such receptor in myeloma is CD28. Treatment of MM in vitro with CTLA4-Ig to block tonic CD28 signaling inhibited this PI3K/Akt/FoxO3a/Bim pathway, and sensitized cells to serum starvation and melphalan. This CD28 dependence was recapitulated in vivo with CTLA4-Ig/melphalan. In this work, we did not specifically characterize which cells in the BM microenvironment provide the ligands. Our prior work14,20 and experiments in Figure 1 suggest that DC and MM cells themselves are important sources of CD80 and/or CD86. However, macrophages19 and eosinophils52 are also present in the MM microenvironment and express CD80/CD86. Nonhematopoietic stromal cells also express CD80/CD86,53-55 although this has not been characterized in the myeloma microenvironment. Regardless of ligand source, these experiments suggest blocking CD28:CD80/CD86 is sufficient to sensitize MM cells to chemotherapy. Importantly, the melphalan dose used was subtherapeutic, suggesting that removing the CD28 signal sensitizes MM cells to a dose of melphalan to which they are usually resistant. Because melphalan resistance is clinically correlated with shorter survival times and worse outcomes,56 CD28 blockade may represent a novel approach to resensitize resistant cells to treatment. We have recently shown CD28 activation also conferred resistance to dexamethasone, arsenic trioxide, and bortezomib.14 Therefore, blocking CD28:CD80/CD86 is likely to resensitize MM cells to a range of chemotherapies. Importantly, CTLA4-Ig (abatacept) is already Food and Drug Administration–approved for rheumatoid arthritis and psoriasis57 and could be readily translated for MM treatment.
Our work suggests that CD28-mediated pro-survival signaling is dependent upon FoxO3a regulation and inhibition of Bim expression. Interestingly, although 65% FoxO3a knockdown was sufficient to prevent CD28 blockade–induced death, 90% Bim knockdown did not completely restore survival. This suggests that FoxO3a is essential for CD28’s pro-survival signal, but Bim may not be the only apoptotic mediator downstream of CD28-induced FoxO3a inactivation. This is unsurprising given that FoxO3a regulates other apoptotic molecules such as Puma58 and FLIP42 that may be affected by FoxO3a silencing. Nevertheless, that Bim knockdown increased cell survival 3-fold suggests it is an important component of CD28 pro-survival signaling.
Intriguingly, CD28 and CD86 coexpression appears to be necessary but not sufficient to promote MM survival. This is somewhat unexpected given that CD28+ primary myelomas are also CD86+27 and CD86 expression is a poor prognostic indicator, suggesting this cis interaction is important for the biology of primary MM and not just cell lines. DC possibly deliver qualitatively different trans signal because they express increased adhesion molecules and both ligands. We would therefore speculate that the cis interaction could be central to MM cell survival outside of the BM and development of extramedullary disease.
In summary, we propose that CD28-mediated PI3K/Akt signaling is critical for MM survival and chemotherapy resistance. A better understanding of this pathway, and therefore the mechanism of survival and chemotherapy resistance could potentially point to new therapeutic combinations targeting CD28 signaling. In combination with CTLA4-Ig, inhibitors such as the PI3K inhibitor characterized by Munugalavadla et al may block CD28 signaling necessary for MM survival and resensitize MM cells to chemotherapies.
Acknowledgments
This work was supported in part by the National Institutes of Health (grants CA121044 and AI100157) and the Multiple Myeloma Research Foundation.
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: M.E.M., C.M.G., J.R.N., C.K., L.M.C., D.B., and A.U. performed experiments; M.C., P.L.B., and L.H.B. provided reagents and feedback; and K.L. and M.E.M. designed the research and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Kelvin P. Lee, Jacobs Family Chair of Immunology, Department of Immunology, Roswell Park Cancer Institute, Elm & Carlton St, Buffalo, NY 14263; e-mail: Kelvin.lee@roswellpark.org.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Attal M, Harousseau JL, Leyvraz S, et al. Inter-Groupe Francophone du Myélome (IFM) Maintenance therapy with thalidomide improves survival in patients with multiple myeloma. Blood. 2006;108(10):3289–3294. doi: 10.1182/blood-2006-05-022962. [DOI] [PubMed] [Google Scholar]
- 3.Kumar SK, Rajkumar SV, Dispenzieri A, et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood. 2008;111(5):2516–2520. doi: 10.1182/blood-2007-10-116129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richardson PG, Barlogie B, Berenson J, et al. A phase 2 study of bortezomib in relapsed, refractory myeloma. N Engl J Med. 2003;348(26):2609–2617. doi: 10.1056/NEJMoa030288. [DOI] [PubMed] [Google Scholar]
- 5.Spanswick VJ, Craddock C, Sekhar M, et al. Repair of DNA interstrand crosslinks as a mechanism of clinical resistance to melphalan in multiple myeloma. Blood. 2002;100(1):224–229. doi: 10.1182/blood.v100.1.224. [DOI] [PubMed] [Google Scholar]
- 6.Hideshima T, Richardson PG, Anderson KC. Mechanism of action of proteasome inhibitors and deacetylase inhibitors and the biological basis of synergy in multiple myeloma. Mol Cancer Ther. 2011;10(11):2034–2042. doi: 10.1158/1535-7163.MCT-11-0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hideshima T, Chauhan D, Shima Y, et al. Thalidomide and its analogs overcome drug resistance of human multiple myeloma cells to conventional therapy. Blood. 2000;96(9):2943–2950. [PubMed] [Google Scholar]
- 8.Mitsiades CS, Mitsiades NS, Munshi NC, Richardson PG, Anderson KC. The role of the bone microenvironment in the pathophysiology and therapeutic management of multiple myeloma: interplay of growth factors, their receptors and stromal interactions. Eur J Cancer. 2006;42(11):1564–1573. doi: 10.1016/j.ejca.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 9.Degrassi A, Hilbert DM, Rudikoff S, Anderson AO, Potter M, Coon HG. In vitro culture of primary plasmacytomas requires stromal cell feeder layers. Proc Natl Acad Sci USA. 1993;90(5):2060–2064. doi: 10.1073/pnas.90.5.2060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang XG, Gaillard JP, Robillard N, et al. Reproducible obtaining of human myeloma cell lines as a model for tumor stem cell study in human multiple myeloma. Blood. 1994;83(12):3654–3663. [PubMed] [Google Scholar]
- 11.Caligaris-Cappio F, Gregoretti MG, Ghia P, Bergui L. In vitro growth of human multiple myeloma: implications for biology and therapy. Hematol Oncol Clin North Am. 1992;6(2):257–271. [PubMed] [Google Scholar]
- 12.Hideshima T, Nakamura N, Chauhan D, Anderson KC. Biologic sequelae of interleukin-6 induced PI3-K/Akt signaling in multiple myeloma. Oncogene. 2001;20(42):5991–6000. doi: 10.1038/sj.onc.1204833. [DOI] [PubMed] [Google Scholar]
- 13.Hirano T, Ishihara K, Hibi M. Roles of STAT3 in mediating the cell growth, differentiation and survival signals relayed through the IL-6 family of cytokine receptors. Oncogene. 2000;19(21):2548–2556. doi: 10.1038/sj.onc.1203551. [DOI] [PubMed] [Google Scholar]
- 14.Nair JR, Carlson LM, Koorella C, et al. CD28 expressed on malignant plasma cells induces a prosurvival and immunosuppressive microenvironment. J Immunol. 2011;187(3):1243–1253. doi: 10.4049/jimmunol.1100016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moreaux J, Legouffe E, Jourdan E, et al. BAFF and APRIL protect myeloma cells from apoptosis induced by interleukin 6 deprivation and dexamethasone. Blood. 2004;103(8):3148–3157. doi: 10.1182/blood-2003-06-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tai YT, Li XF, Breitkreutz I, et al. Role of B-cell-activating factor in adhesion and growth of human multiple myeloma cells in the bone marrow microenvironment. Cancer Res. 2006;66(13):6675–6682. doi: 10.1158/0008-5472.CAN-06-0190. [DOI] [PubMed] [Google Scholar]
- 17.Damiano JS, Cress AE, Hazlehurst LA, Shtil AA, Dalton WS. Cell adhesion mediated drug resistance (CAM-DR): role of integrins and resistance to apoptosis in human myeloma cell lines. Blood. 1999;93(5):1658–1667. [PMC free article] [PubMed] [Google Scholar]
- 18.Damiano JS, Dalton WS. Integrin-mediated drug resistance in multiple myeloma. Leuk Lymphoma. 2000;38(1-2):71–81. doi: 10.3109/10428190009060320. [DOI] [PubMed] [Google Scholar]
- 19.Zheng Y, Cai Z, Wang S, et al. Macrophages are an abundant component of myeloma microenvironment and protect myeloma cells from chemotherapy drug-induced apoptosis. Blood. 2009;114(17):3625–3628. doi: 10.1182/blood-2009-05-220285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bahlis NJ, King AM, Kolonias D, et al. CD28-mediated regulation of multiple myeloma cell proliferation and survival. Blood. 2007;109(11):5002–5010. doi: 10.1182/blood-2006-03-012542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hazlehurst LA, Enkemann SA, Beam CA, et al. Genotypic and phenotypic comparisons of de novo and acquired melphalan resistance in an isogenic multiple myeloma cell line model. Cancer Res. 2003;63(22):7900–7906. [PubMed] [Google Scholar]
- 22.Nefedova Y, Cheng P, Alsina M, Dalton WS, Gabrilovich DI. Involvement of Notch-1 signaling in bone marrow stroma-mediated de novo drug resistance of myeloma and other malignant lymphoid cell lines. Blood. 2004;103(9):3503–3510. doi: 10.1182/blood-2003-07-2340. [DOI] [PubMed] [Google Scholar]
- 23.Rudd CE, Taylor A, Schneider H. CD28 and CTLA-4 coreceptor expression and signal transduction. Immunol Rev. 2009;229(1):12–26. doi: 10.1111/j.1600-065X.2009.00770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sharpe AH, Freeman GJ. The B7-CD28 superfamily. Nat Rev Immunol. 2002;2(2):116–126. doi: 10.1038/nri727. [DOI] [PubMed] [Google Scholar]
- 25.Kozbor D, Moretta A, Messner HA, Moretta L, Croce CM. Tp44 molecules involved in antigen-independent T cell activation are expressed on human plasma cells. J Immunol. 1987;138(12):4128–4132. [PubMed] [Google Scholar]
- 26.Rozanski CH, Arens R, Carlson LM, et al. Sustained antibody responses depend on CD28 function in bone marrow-resident plasma cells. J Exp Med. 2011;208(7):1435–1446. doi: 10.1084/jem.20110040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robillard N, Jego G, Pellat-Deceunynck C, et al. CD28, a marker associated with tumoral expansion in multiple myeloma. Clin Cancer Res. 1998;4(6):1521–1526. [PubMed] [Google Scholar]
- 28.Almeida J, Orfao A, Ocqueteau M, et al. High-sensitive immunophenotyping and DNA ploidy studies for the investigation of minimal residual disease in multiple myeloma. Br J Haematol. 1999;107(1):121–131. doi: 10.1046/j.1365-2141.1999.01685.x. [DOI] [PubMed] [Google Scholar]
- 29.Paiva B, Vidriales MB, Cerveró J, et al. GEM (Grupo Español de MM)/PETHEMA (Programa para el Estudio de la Terapéutica en Hemopatías Malignas) Cooperative Study Groups. Multiparameter flow cytometric remission is the most relevant prognostic factor for multiple myeloma patients who undergo autologous stem cell transplantation. Blood. 2008;112(10):4017–4023. doi: 10.1182/blood-2008-05-159624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mateo G, Castellanos M, Rasillo A, et al. Genetic abnormalities and patterns of antigenic expression in multiple myeloma. Clin Cancer Res. 2005;11(10):3661–3667. doi: 10.1158/1078-0432.CCR-04-1489. [DOI] [PubMed] [Google Scholar]
- 31.Pope B, Brown RD, Gibson J, Yuen E, Joshua D. B7-2-positive myeloma: incidence, clinical characteristics, prognostic significance, and implications for tumor immunotherapy. Blood. 2000;96(4):1274–1279. [PubMed] [Google Scholar]
- 32.Friend LD, Shah DD, Deppong C, et al. A dose-dependent requirement for the proline motif of CD28 in cellular and humoral immunity revealed by a targeted knockin mutant. J Exp Med. 2006;203(9):2121–2133. doi: 10.1084/jem.20052230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burr JS, Savage ND, Messah GE, et al. Cutting edge: distinct motifs within CD28 regulate T cell proliferation and induction of Bcl-XL. J Immunol. 2001;166(9):5331–5335. doi: 10.4049/jimmunol.166.9.5331. [DOI] [PubMed] [Google Scholar]
- 34.Pene F, Claessens YE, Muller O, et al. Role of the phosphatidylinositol 3-kinase/Akt and mTOR/P70S6-kinase pathways in the proliferation and apoptosis in multiple myeloma. Oncogene. 2002;21(43):6587–6597. doi: 10.1038/sj.onc.1205923. [DOI] [PubMed] [Google Scholar]
- 35.Hideshima T, Catley L, Yasui H, et al. Perifosine, an oral bioactive novel alkylphospholipid, inhibits Akt and induces in vitro and in vivo cytotoxicity in human multiple myeloma cells. Blood. 2006;107(10):4053–4062. doi: 10.1182/blood-2005-08-3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marani M, Tenev T, Hancock D, Downward J, Lemoine NR. Identification of novel isoforms of the BH3 domain protein Bim which directly activate Bax to trigger apoptosis. Mol Cell Biol. 2002;22(11):3577–3589. doi: 10.1128/MCB.22.11.3577-3589.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chesi M, Robbiani DF, Sebag M, et al. AID-dependent activation of a MYC transgene induces multiple myeloma in a conditional mouse model of post-germinal center malignancies. Cancer Cell. 2008;13(2):167–180. doi: 10.1016/j.ccr.2008.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vieira P, Rajewsky K. The half-lives of serum immunoglobulins in adult mice. Eur J Immunol. 1988;18(2):313–316. doi: 10.1002/eji.1830180221. [DOI] [PubMed] [Google Scholar]
- 39.Peterson TR, Laplante M, Thoreen CC, et al. DEPTOR is an mTOR inhibitor frequently overexpressed in multiple myeloma cells and required for their survival. Cell. 2009;137(5):873–886. doi: 10.1016/j.cell.2009.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Menu E, Kooijman R, Van Valckenborgh E, et al. Specific roles for the PI3K and the MEK-ERK pathway in IGF-1-stimulated chemotaxis, VEGF secretion and proliferation of multiple myeloma cells: study in the 5T33MM model. Br J Cancer. 2004;90(5):1076–1083. doi: 10.1038/sj.bjc.6601613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhu S, Evans S, Yan B, et al. Transcriptional regulation of Bim by FOXO3a and Akt mediates scleroderma serum-induced apoptosis in endothelial progenitor cells. Circulation. 2008;118(21):2156–2165. doi: 10.1161/CIRCULATIONAHA.108.787200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Skurk C, Maatz H, Kim HS, et al. The Akt-regulated forkhead transcription factor FOXO3a controls endothelial cell viability through modulation of the caspase-8 inhibitor FLIP. J Biol Chem. 2004;279(2):1513–1525. doi: 10.1074/jbc.M304736200. [DOI] [PubMed] [Google Scholar]
- 43.Greer EL, Brunet A. FOXO transcription factors at the interface between longevity and tumor suppression. Oncogene. 2005;24(50):7410–7425. doi: 10.1038/sj.onc.1209086. [DOI] [PubMed] [Google Scholar]
- 44.Van Der Heide LP, Hoekman MF, Smidt MP. The ins and outs of FoxO shuttling: mechanisms of FoxO translocation and transcriptional regulation. Biochem J. 2004;380(Pt 2):297–309. doi: 10.1042/BJ20040167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gilley J, Coffer PJ, Ham J. FOXO transcription factors directly activate bim gene expression and promote apoptosis in sympathetic neurons. J Cell Biol. 2003;162(4):613–622. doi: 10.1083/jcb.200303026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sunters A, Fernández de Mattos S, Stahl M, et al. FoxO3a transcriptional regulation of Bim controls apoptosis in paclitaxel-treated breast cancer cell lines. J Biol Chem. 2003;278(50):49795–49805. doi: 10.1074/jbc.M309523200. [DOI] [PubMed] [Google Scholar]
- 47.Urbich C, Knau A, Fichtlscherer S, et al. FOXO-dependent expression of the proapoptotic protein Bim: pivotal role for apoptosis signaling in endothelial progenitor cells. FASEB J. 2005;19(8):974–976. doi: 10.1096/fj.04-2727fje. [DOI] [PubMed] [Google Scholar]
- 48.Guan H, Song L, Cai J, et al. Sphingosine kinase 1 regulates the Akt/FOXO3a/Bim pathway and contributes to apoptosis resistance in glioma cells. PLoS ONE. 2011;6(5):e19946. doi: 10.1371/journal.pone.0019946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gomez-Bougie P, Bataille R, Amiot M. The imbalance between Bim and Mcl-1 expression controls the survival of human myeloma cells. Eur J Immunol. 2004;34(11):3156–3164. doi: 10.1002/eji.200424981. [DOI] [PubMed] [Google Scholar]
- 50.Morales AA, Kurtoglu M, Matulis SM, et al. Distribution of Bim determines Mcl-1 dependence or codependence with Bcl-xL/Bcl-2 in Mcl-1-expressing myeloma cells. Blood. 2011;118(5):1329–1339. doi: 10.1182/blood-2011-01-327197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Munugalavadla V, Mariathasan S, Slaga D, et al. The PI3K inhibitor GDC-0941 combines with existing clinical regimens for superior activity in multiple myeloma. Oncogene. 2014;33(3):316–325. doi: 10.1038/onc.2012.594. [DOI] [PubMed] [Google Scholar]
- 52.Wong TW, Kita H, Hanson CA, Walters DK, Arendt BK, Jelinek DF. Induction of malignant plasma cell proliferation by eosinophils. PLoS ONE. 2013;8(7):e70554. doi: 10.1371/journal.pone.0070554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davis TA, Craighead N, Williams AJ, Scadron A, June CH, Lee KP. Primary porcine endothelial cells express membrane-bound B7-2 (CD86) and a soluble factor that co-stimulate cyclosporin A-resistant and CD28-dependent human T cell proliferation. Int Immunol. 1996;8(7):1099–1111. doi: 10.1093/intimm/8.7.1099. [DOI] [PubMed] [Google Scholar]
- 54.Stagg J, Pommey S, Eliopoulos N, Galipeau J. Interferon-gamma-stimulated marrow stromal cells: a new type of nonhematopoietic antigen-presenting cell. Blood. 2006;107(6):2570–2577. doi: 10.1182/blood-2005-07-2793. [DOI] [PubMed] [Google Scholar]
- 55.Abe M, Shintani Y, Eto Y, Harada K, Kosaka M, Matsumoto T. Potent induction of activin A secretion from monocytes and bone marrow stromal fibroblasts by cognate interaction with activated T cells. J Leukoc Biol. 2002;72(2):347–352. [PubMed] [Google Scholar]
- 56.Alexanian R, Bergsagel DE, Migliore PJ, Vaughn WK, Howe CD. Melphalan therapy for plasma cell myeloma. Blood. 1968;31(1):1–10. [PubMed] [Google Scholar]
- 57.Ruderman EM, Pope RM. The evolving clinical profile of abatacept (CTLA4-Ig): a novel co-stimulatory modulator for the treatment of rheumatoid arthritis. Arthritis Res Ther. 2005;7(Suppl 2):S21–S25. doi: 10.1186/ar1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.You H, Pellegrini M, Tsuchihara K, et al. FOXO3a-dependent regulation of Puma in response to cytokine/growth factor withdrawal. J Exp Med. 2006;203(7):1657–1663. doi: 10.1084/jem.20060353. [DOI] [PMC free article] [PubMed] [Google Scholar]