Abstract
Serotonin syndrome and neuroleptic malignant syndrome are two drug toxidromes that have often overlapping and confusing clinical pictures. We report a case of a young man who presented with alteration of mental status, autonomic instability and neuromuscular hyperexcitability following ingestion of multiple psychiatric and antiepileptic medications. The patient satisfied criteria for serotonin syndrome and neuroleptic malignant syndrome, and based on the characteristic clinical features, laboratory findings and clinical course it was concluded that the patient had both toxidromes. The patient was managed with cyproheptadine and supportive measures, and recovered over the course of 3 weeks. A brief review of literature highlighting the diagnostic clues as well as the importance of recognising and distinguishing the often missed and confounding diagnoses follows.
Background
Serotonin syndrome (SS) and neuroleptic malignant syndrome (NMS) are relatively rare, life-threatening adverse reactions to psychotropic medications. SS is a result of excessive stimulation of serotoninergic receptors in the peripheral and central nervous system (CNS), as a consequence of a variety of proserotinergic agents.1 2 NMS is on the other hand an idiopathic drug reaction to antipsychotics.3 It is important to be aware of the fact that both these uncommon diagnoses can often be missed, in part due to the fact that a significant proportion of prescribing doctors are not familiar with SS.4 As there is no specific diagnostic test, a high index of suspicion and an active effort to rule out other possible diagnoses is essential.
Although culprit agents are often very useful in differentiating the two syndromes, polypharmacy, as in the case described, can make this valueless. SS is predominately a hyperkinetic syndrome with characteristic lower limb hyper-reflexia as opposed to the marked rigidity and hyporeflexia in NMS; however, several other overlapping clinical features make the two entities difficult to differentiate. Laboratory features have been described as being valuable to distinguish the two similarly presenting toxidromes, but are overall non-specific. There is a considerable difference in the overall clinical course that can be useful in separating the two; however, this is often not possible to assess during the first consultation and needs periodic review and frequent clinical evaluations to determine. Owing to the possible calamitous outcomes, patients should be recognised early, monitored closely and if necessary managed aggressively. The importance of differentiating the two is even further heightened by the fact that bromocriptine, recommended in NMS has been shown to worsen SS and should be avoided; moreover, some neuroleptics have been suggested as agents in SS but can potentially precipitate and worsen NMS. Early and careful consideration of both diagnoses in the acute and critical care setting is recommended and an algorithm to handle such scenarios has been suggested.5
Case presentation
A 19-year-old male patient presented with a 4-month history of steadily worsening hallucinations and delusions. For these symptoms he was initially treated by a psychiatrist and started on valproate, lithium, olanzapine, risperidone and clonazepam.
On the second day of starting the medication he developed excessive perspiration, rigors, high-grade continuous fever, agitation and aggressive behaviour. Initially considering this as an aggravation of his psychiatric behaviour the psychiatrist continued with the medications, which were eventually stopped after 4 days.
Over the next 4–5 days of continuing medications his condition deteriorated so that he was completely non-responsive, akinetic and had no oral intake. He continued to have high-grade continuous fever and also developed diarrhoea. The patient was transferred to a hospital with a working diagnosis of metabolic versus infectious encephalopathy. There was no history of headache, photophobia, neck stiffness, vomiting, diplopia, jaundice, reduced urine output, convulsions, abnormal movements or posturing. There was no history of illicit drug use.
The patient had been treated for a psychiatric illness about 2 years before this presentation but he was not on any medications for more than 18 months. On transfer to our service the patient was lying immobile in bed and not responding to commands. He had a temperature of 105°F (not responding to acetaminophen), was tachycardic (pulse 112/min) and tachypnoeic (respiratory rate 28/min). His blood pressure was 130/82 mm Hg. Also carpopedal spam was noted (figure 1) although Chvostek's sign was negative.
Figure 1.

Carpopedal spasm was noted, corresponding to the hypocalcaemia.
On a more detailed neurological examination, Glasgow Coma Scale was 6/15 (M4V1E1). A limited cranial nerve examination in the comatose patient revealed no abnormality. Pupils were noted to be bilaterally equal, round in shape, dilated and sluggishly reacting to light. Hypertonia was obvious in all four limbs (lead pipe rigidity) and hyper-reflexia including bilateral sustained ankle clonus was elicited (video 1). No other catatonic features such as waxy flexibility, posturing, persistence or automatic obedience were noted. Planter reflexes were down going. Also of note were hyperkinetic bowel sounds on auscultation of the abdomen.
Displays sustained elicitable ankle clonus.
Investigations
Laboratory investigations revealed haemoglobin of 11.1 g/dL (13–18) normocytic and normochromic indices, raised leucocyte count of 15 300/mm3 (4000–11 000/mm3), elevated erythrocyte sedimentation rate 32 mm at the end of first hour and C reactive protein 67 mg/dL (<6) and S creatinine 0.7 mg/dL (0.5–1.2). Liver function tests revealed normal bilirubin values (total 1 mg/dL; 0.1–1.2) but moderately elevated transaminases serum glutamic pyruvic transaminase 324 U/L (<40) and serum glutamic oxaloacetic transaminase 210 U/L (<40). Na+ (140 mEq/L, 135–145), K+ (3.9, 3.5–5.5) Cl− (101 mEq/L, 96–104) and HCO3 (23.2 mEq/L, 22–28) were in normal ranges, however serum calcium was low (total 6.3 mg/dL, 8.4–10.3 and ionised 3.17 mg/dL, 4.75–5.3) while serum phosphorus 2.8 mg/dL (2.6–4.5 mg) and serum magnesium 1.8 mg/dL (1.6–2.3) as well as serum parathormone levels were within normal levels. Serum creatine kinase levels were elevated 15 000 U/L (24–95) and serum iron was decreased to 30 μg/dL (49–181).
Blood cultures and cerebrospinal fluid (CSF) analysis were normal. MRI of the brain did not reveal any abnormalities. EEG showed mild diffuse slowing but no epileptic activity. Serum thyroid-stimulating hormone was normal, urine porphobilinogen was negative and serum ceruloplasmin was within normal limits. Serum lithium levels were within therapeutic range (1.4 mmol/L, 0.5–1.5). A urine toxicological screen was run to rule out drug abuse. An ultrasound examination of the abdomen was normal. However, a chest roentgenogram revealed a paracardiac shadow suggestive of consolidation on the right.
Differential diagnosis
Although the patient did have evidence of an additional infectious process, probably pneumonia, it was unlikely to be the underlying cause of his dramatic presentation. Other infectious causes such as meningitis and encephalitis were ruled out by CSF and neuroimaging studies. Considering the temporal association of the symptoms following the psychotropic medication ingestion a drug toxidrome was considered as a strong possibility. Hyperthermia can be a complication of malignant catatonia or agitated delirium and was also considered. Based on the presentation and medication history, both SS (valproic acid, lithium and ondansetron) and NMS (risperidone, olanzapine and lithium) were possible.
Treatment
All psychotropic medications were stopped. The patient was supported with intravenous fluids, sedation and antimicrobial medication for probable aspiration pneumonia. Hypocalcaemia was corrected. Cyproheptadine was started via nasogastric tube in recommended doses for SS. Dantrolene was considered but was not available.
Outcome and follow-up
Within 24 h of cessation of the serotonergic drugs and starting cyproheptadine the patient improved significantly. Mydriasis, tremulousness, hyper-reflexia, fever and clonus resolved almost completely. However, there was a persistent akinetic mute state with marked lead pipe rigidity that lasted for more than 2 weeks after stopping the antipsychotic medications, and gradually improved. Going through the patient's charts and discharge records from the previous admitting facility a graph of the symptoms was prepared against time. Hyperkinesia (in the form of clonus and tremulousness), mydriasis and gastrointestinal symptoms were compared with hypertonia and bradykinesia; two distinctive patterns were apparent (figure 2).
Figure 2.
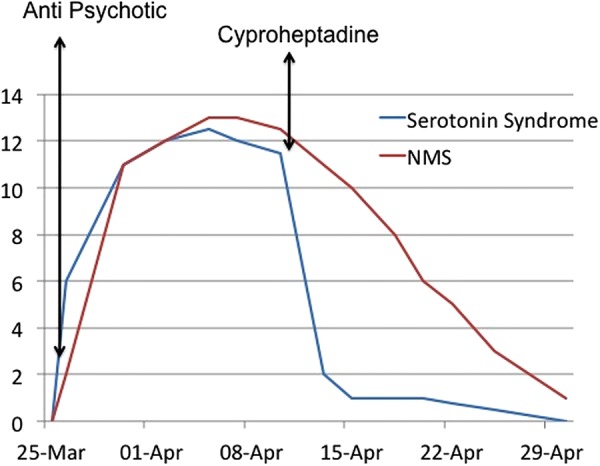
Graph showing clinical course of the serotonin syndrome (tremulousness, mydriasis, hyper-reflexia and hyperactive bowel sounds) and neuroleptic malignant syndrome (NMS; rigidity and bradykinesia) with respect to administration of culprit medication and treatment is plotted.
Discussion
SS and NMS are adverse drug reactions to psychotropic medications with an often-confusing, similar clinical picture.6 Identifying both syndromes early and stopping the culprit medication is of paramount importance as both can be life-threatening.7 Although there are no diagnostic tests, criteria have been suggested and should be applied in any clinical scenario following recent initiation or stepping up of doses of serotonergic medications or antipsychotics. Ruling out other possibilities including CNS infections, heatstroke and thyrotoxicosis is paramount as the clinical pictures can overlap considerably and the diagnoses are chiefly those of exclusion.1–3 Idiopathic malignant catatonia and agitated delirium are psychiatric causes of a similar presentation, as well as risk factors for NMS; hence omitting antipsychotics is a must whenever suspected.3
SS is believed to be due to excess serotonin activity in the CNS as a result of excess precursors of 5-hydroxytryptamine (5-HT) and its agonists, increased release of 5-HT, decreased uptake or lower metabolism.4 Numerous agents besides serotonergic antidepressants including antimicrobials such as linezolid, antiemetics ondansetron; analgesics such as fentanyl and dietary supplements such as tryptophan have been implicated. In the case described the state of serotonin overactivity could be due to inhibition of serotonin uptake (ondansetron),1 activation of serotonin receptors (lithium)1 or an increase in serotonin release (valproate).4 8 Although the precise pathophysiology of NMS is not well understood, an antipsychotic-induced central dopaminergic blockade is likely to play a pivotal role. Sympathoadrenal dysfunction is also proposed to play a significant role.3 9
Differentiating SS and NMS can be a diagnostic challenge, but clinical course, signs and laboratory findings may be useful.10 Altered mentation, autonomic disturbances including hyperthermia, tachycardia, tachypnoea and fluctuating blood pressure and neuromuscular hyperexcitability are prominent features of both syndromes. Important distinguishing clinical features include hyper-reflexia (often in the form of clonus, more marked in the lower extremities), ocular clonus and tremors in SS, whereas NMS is a bradykinetic syndrome characterised by uniform ‘lead-pipe’ rigidity and hyporeflexia.2 4 In addition, although there is not a considerable overlap in causative medications, polypharmacy as in the case reported can muddy the waters considerably. Symptoms of SS are also frequently seen within the first 24 h of starting serotonergic agents and resolve within a few days of starting treatment and omitting the medication. On the other hand NMS can often be slower in onset and usually takes 9–14 days to remit in spite of appropriate treatment.6 10
While there is no diagnostic test for either of the syndromes, using laboratory values to separate the two has been proposed to be very useful. High creatine kinase levels, electrolyte disturbances especially hypocalcaemia, low iron levels, leucocytosis and proteinuria are seen in more than 75% of patients with NMS.6 10 However, as most of these are attributable to rhabdomyolysis, they can also be seen in severe SS and cannot be relied on too heavily.
The most important step in the management of SS and NMS is stopping the offending agent.7 Although patients with mild SS can be managed on outpatient basis and close follow-up, many patients require inpatient management including intravenous fluids, sedatives, stabilising vital signs and external cooling as acetaminophen will not be effective. Although it has not been tried in randomised trials cyproheptadine is used usually via nasogastric tube feeds.1 2 4 7 Other agents that can be tried include chlorpromazine and olanzapine. Dantrolene is recommended in NMS.3 However, dantrolene is an orphan drug and is not available in several countries; we were unable to source it despite active efforts. Dopaminergic agents such as bromocriptine are more easily available; however, bromocriptine has been associated with SS and hence must be used with caution especially when the diagnosis is unclear as in our case.5 6
Our case highlights the importance of increasing awareness to prevent delays in diagnosis of this potential life-threatening disease. We concluded that based on the considerable overlap in the patient’s inciting drug therapy, the characteristic clinical and laboratory picture, and the biphasic course of the illness including the response to therapy, we were dealing with an overlap between NMS and SS. This recognition is important as it has considerable implications on prognosis as well as selection of agents as some drugs used in NMS such as bromocriptine can worsen SS and likewise chlorpromazine has been used for SS but is contraindicated in patients with NMS. Identifying this clinical picture and using an algorithm similar to the one used in our case is important.5 Pharmacogenomics research, physician education, improved prescribing practices and the use of technology to prevent drug interactions and avoid multidrug regimens can all contribute to prevention and early recognition of such adverse drug events.4 9 11
Learning points.
Serotonin syndrome and neuroleptic malignant syndrome have overlapping presentations and can be a source of considerable diagnostic confusion, especially in cases of polypharmacy.
Diagnostic criteria, specific clinical features, identifying causative agents and laboratory investigations can be used to differentiate the two syndromes.
As these drug reactions may be life-threatening early suspicion and prompt institution of therapy including recommended agents is paramount.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Volpi-Abadie J, Kaye AM, Kaye AD. Serotonin syndrome. Ochsner J 2013;13:533–40 [PMC free article] [PubMed] [Google Scholar]
- 2.Iqbal MM, Basil MJ, Kaplan J, et al. Overview of serotonin syndrome. Ann Clin Psychiatry 2012;24:310–18 [PubMed] [Google Scholar]
- 3.Strawn JR, Keck PE, Jr, Caroff SN. Neuroleptic malignant syndrome. Am J Psychiatry 2007;164:870–6 [DOI] [PubMed] [Google Scholar]
- 4.Boyer EW, Shannon M. The serotonin syndrome. N Engl J Med 2005;352:1112–20 [DOI] [PubMed] [Google Scholar]
- 5.Kaufman KR, Levitt MJ, Schiltz JF, et al. Neuroleptic malignant syndrome and serotonin syndrome in the critical care setting: case analysis. Ann Clin Psychiatry 2006;18:201–4 [DOI] [PubMed] [Google Scholar]
- 6.Perry PJ, Wilborn CA. Serotonin syndrome vs neuroleptic malignant syndrome: a contrast of causes, diagnoses, and management. Ann Clin Psychiatry 2012;24:155–62 [PubMed] [Google Scholar]
- 7.Suarez-Contreras V, Freeman WD. Treatment of four psychiatric emergencies in the ICU. Crit Care Med 2013;41:e20. [DOI] [PubMed] [Google Scholar]
- 8.Löscher W. Basic pharmacology of valproate: a review after 35 years of clinical use for the treatment of epilepsy. CNS Drugs 2002;16:669–94 [DOI] [PubMed] [Google Scholar]
- 9.Margetić B, Aukst-Margetić B. Neuroleptic malignant syndrome and its controversies. Pharmacoepidemiol Drug Saf 2010;19:429–35 [DOI] [PubMed] [Google Scholar]
- 10.Kimmel R. Serotonin syndrome or NMS? Clues to diagnosis. Curr Psychiatry 2010;9:69 [Google Scholar]
- 11.Ables AZ, Nagubilli R. Prevention, diagnosis, and management of serotonin syndrome. Am Fam Physician 2010;81:1139–42 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Displays sustained elicitable ankle clonus.


