Abstract
Objective
Breast cancer is the most frequent malignant tumor among women in the industrialized world. The vast majority of these tumors can now be successfully treated. A subset of breast cancer survivors report quality of life (QOL) difficulties well after treatment is completed. The current study examined how individual differences in attachment style and self-regulatory capacity (as indexed by RSA) were associated quality of life among post-treatment breast cancer survivors.
Methods
Women who had completed treatment for stage 0-IIIA breast cancer within the past two years participated in the study (N = 96). RSA was assessed using Electrocardiography (ECG) data that was continuously measured non-invasively for 10 minutes. Attachment orientation was measured using a modified version of the Experiences in Close relationships Scale, and Overall QOL by the Functional Assessment of Cancer Therapy-Breast scale.
Results
Breast cancer survivors with more attachment anxiety reported poorer QOL than those with less attachment anxiety. Women who were more avoidantly attached also reported poorer QOL compared with those who were less avoidantly attached. Furthermore, attachment avoidance interacted with RSA to predict QOL such that those with higher attachment avoidance were only vulnerable to poorer QOL if they also had lower self-regulatory capacity, as indexed by lower RSA.
Conclusion
A better understanding of how attachment style and RSA contribute to breast cancer survivor QOL will help identify people at risk for QOL problems after treatment completion.
Keywords: Cancer survivorship, Psycho-oncology, Attachment Theory, Quality of Life, Respiratory Sinus Arrhythmia, Self-regulation
Breast cancer is the most frequent malignant tumor among women in the industrialized world. The vast majority of these tumors can now be successfully treated [1]. However, a subset of breast cancer survivors report quality of life (QOL) difficulties well after treatment is completed [2-4]. Accordingly, it is important to understand why some survivors are more at risk for QOL issues than others.
Attachment theory may be a useful framework for understanding QOL difficulties among breast cancer survivors; attachment theory provides a basis for understanding differences in both physical and emotional well-being in response to stress, which has been empirically supported in a number of non-cancer populations [5-8]. Specifically, attachment theory suggests that people who have responsive and supportive parents during childhood develop a sense of emotional security that lasts into adulthood, while those who have unresponsive and unsupportive parents develop a sense of emotional insecurity [9, 10]. There are two patterns of attachment insecurity: attachment anxiety and attachment avoidance [11].
People with high attachment anxiety use “hyperactivating” emotional coping strategies, essentially exaggerating negative experiences [12-15]. Prior research using a non-cancer population demonstrated that people with more attachment anxiety consistently report poorer emotional well-being after a stressful life event compared with their less anxiously attached counterparts [5-8]. Attachment anxiety has also been linked to more physical health symptoms, such as pain [16-21]. Accordingly, breast cancer survivors with higher attachment anxiety may be particularly vulnerable to post-treatment QOL difficulties.
In contrast to the hyperactivating emotional style of anxiously attached individuals, people with high attachment avoidance are uncomfortable depending on others for support and use “deactivating” coping strategies that inhibit or suppress distressing experiences [12, 13]. Attachment avoidance is not consistently related to physical or emotional well-being [21-26], perhaps because suppressing negative emotional experiences is difficult and often unsuccessful. Accordingly, attachment avoidance and the corresponding desire for emotion suppression may only be maladaptive for those who cannot effectively self-regulate their emotions.
Recently developed models have identified parasympathetic nervous system activity, which can be indexed by the variability in heart rate attributable to respiration, as an important contributor to self-regulation. [27, 28]. Briefly, heart rate increases and decreases with one's breathing, a pattern known as respiratory sinus arrhythmia (RSA). According to both polyvagal theory and the neurovisceral integration model, a set of brain structures and circuits called the ventral vagus complex play a key role in parasympathetic modulation of emotion and physiological responses [27, 28]. Accordingly, resting RSA levels reflect an individual's capacity for self-regulation because they provide an index of tonic parasympathetic influence over heart rate [27, 28].
In support of the argument that avoidant attachment is maladaptive for those who are unable to successfully suppress their emotions, recent work demonstrated that the association between attachment avoidance and well-being depends upon self-regulatory capacity, as indexed by RSA[5]. For example, among adolescents with lower RSA, those with more attachment avoidance had poorer loss adjustment [5].
The current study examined how individual differences in breast cancer survivor's attachment style and self-regulatory capacity (as indexed by RSA) were associated with quality of life (QOL) among cancer survivors [29]. We expected that women who were more anxiously attached would experience poorer quality of life compared with those who were less anxiously attached. We also hypothesized that the effect of attachment avoidance on QOL would depend on self-regulatory capacity.
Participants
The study data were drawn from the baseline sample of 96 women who participated in a randomized controlled trial (RCT) addressing the potential benefits of yoga for breast cancer survivors. Participants were recruited through breast cancer clinics and media announcements. Eligible women had completed treatment for stage 0-IIIA breast cancer within the past two years (except for tamoxifen/aromatase inhibitors) and were at least two months post-surgery, radiation, or chemotherapy (whichever occurred last). Screening exclusions included a prior history of breast or any other cancer except basal or squamous cell skin carcinomas, more than five hours a week of vigorous physical exercise, diabetes, chronic obstructive pulmonary disease, uncontrolled hypertension, evidence of liver or kidney failure, and symptomatic ischemic heart disease. Furthermore, women could not have practiced yoga for more than 3 months prior to enrolling in the study. All data were collected before women were randomized for the intervention. The Ohio State Biomedical Research Review Committee approved the project; all subjects gave written informed consent prior to participation.
Questionnaires
Attachment orientation was measured using a modified version of the Experiences in Close relationships Scale (i.e. ECR-M16) [30]. The ECR-M16 was designed to assess attachment orientation in patients of diverse ages across a variety of medical settings. The 16-item self-report measure evaluates attachment orientations within peoples' close relationships; it contains two 8-item subscales, one assessing attachment anxiety and the other assessing attachment avoidance. The anxiety subscale includes items such as “I worry about being abandoned” and “I need a lot of reassurance that I am loved by people with whom I feel close to.” The following items are representative of the avoidance scale: “I get uncomfortable when other people want to be very close to me,” and “I don't feel comfortable opening up to other people.” Cronbach's alpha in our sample was .89 for attachment anxiety and .91 for attachment avoidance.
Overall QOL was assessed by the Functional Assessment of Cancer Therapy-Breast scale (FACT-B) [29]. The FACT-B assesses physical, functional, emotional, social or family, and general well-being (Fact-General scale), plus a breast cancer-specific scale that indexes quality of life problems explicit to having had breast cancer such as breast pain. Consistent with prior literature, all of the items were summed to create the Fact-B total score. [31]. Cronbach's alpha in our sample was .82.
The Charlson index was used to assess medical comorbidities [32]. It is a widely used measure that reliably indexes 19 major medical conditions that increase mortality risk.
The Interpersonal Support Evaluation List (ISEL) provided a comprehensive measure of perceived social support [33]. Items are rated on a four-point scale (i.e. definitely false, probably false, probably true, and definitely true). The ISEL measures the perceived availability of the following kinds of support: emotional (someone to confide in), belonging (people with whom one can do things with), self-esteem (positive social comparison), and tangible (provision of material aid). The Cronbach's alpha for the total score was .93.
Participants answered questions about their age, race, smoking status, and weekly average alcohol consumption. Body mass index (BMI; kg/m2) was calculated from height and weight data obtained during the visit.
Breast cancer stage was obtained through the Cancer Registry or electronic medical records. Breast cancer stage takes into account the size of the tumor, whether the cancer is invasive or non-invasive, whether the cancer is in the lymph nodes (and how many lymph nodes are involved), and whether the cancer has spread to other parts of the body [34]. Importantly, five year survival rates are based on cancer stage. Additionally, the work-up recommendations and cancer treatment procedures are dictated by cancer stage according to the National Comprehensive Cancer Network (NCCN) guidelines.
RSA
To assess RSA, Electrocardiography (ECG) data was continuously measured non-invasively for 10 minutes in a sitting position with the Polar s810 wristwatch and Wearlink 31 belt band; the 1000 Hz sampling rate provides valid and reliable ECG data [35, 36]. Before analyzing the ECG data, we preprocessed the raw interbeat intervals for artifacts using KUBIOS heart rate variability analysis software [37]. The KUBIOS software produced values for vagally-mediated (parasympathetic) RSA using the time-domain method, square root of mean successive differences (RMSSD) between R-Waves (which indexes RSA). RMSSD was determined by calculating the differences between consecutive interbeat (RR) intervals before squaring and summing them; the values are then averaged and the square root obtained [38, 39]. All procedures followed the recommendations of the Task Force of the European Society of Cardiology and the North American Society of Pacing Electrophysiology [38].
RSA measured during a resting state (resting RSA) has been associated with adaptive coping strategies, negative emotional traits such as depression and anxiety, and regulation of negative affect [40-42]. On the other hand, changes in RSA in response to an acute task seem to be closely related to regulatory effort/strength and stress reactivity (depending upon the type of task) [27, 28, 43, 44]. Accordingly, resting RSA was chosen for the current study because the outcome was quality of life after treatment rather than in response to a specific stressor.
Analytic Method
Using ordinary least squared multiple regressions, we addressed whether attachment anxiety predicted the Fact-B total score, and whether attachment avoidance interacted with RSA to predict the QOL index. All independent variables were grand mean centered. We examined residuals to confirm that they distributed normally. In all analyses, we adjusted for age, BMI, cancer stage, comorbidities, time since treatment ended, and cardiovascular medication status (use of beta blockers, diuretics, or calcium channel blockers vs. none). We included the main effects of attachment anxiety, attachment avoidance, and RSA in the first step of the model. To test for moderation, we added the interaction between attachment avoidance and RSA in the second step of the model. We also tested for an interaction between attachment anxiety and RSA. None of the anxiety by RSA interactions were significant and thus the interaction term was omitted from the analysis. Attachment insecurity is associated with less perceived support [45]; in ancillary analyses, we included perceived support in the final regression models to determine if perceived support altered the findings.
Results
Means and standard deviations for all study variables are presented in Table 1. Table 2 summarizes the zero-order correlations between the study variables. First, we tested QOL using the FACT-B total score (see Table 3). Women with more attachment anxiety reported poorer QOL than those with less attachment anxiety. Likewise women with more attachment avoidance reported poorer (QOL) than those with less attachment avoidance. The interaction between attachment avoidance and RSA predicting QOL was significant. As expected, among women with lower RSA, those with higher attachment avoidance reported worse QOL than women with lower attachment avoidance (b = -.77, t = -3.19, p = .002). However, the association between attachment avoidance and QOL was not significant for those with higher RSA (b = .13, t = .50, p = .62).
Table 1.
Study sample characteristics.
| Characteristic | n= 96 |
|---|---|
|
| |
| Number(%) or Mean(SD) | |
| Ethnicity | |
| Asian | 3(3.1) |
| Black | 11(11.5) |
| White | 81(84.4) |
| Native American | 1(1.0) |
| Marital Status | |
| Single | 11(11.5) |
| Married | 68(70.8) |
| Common Law | 1(1.0) |
| Separated/Divorced/Widowed | 16(16.7) |
| Cancer Stage | |
| Stage 0 | 10(10.4) |
| Stage 1 | 41(42.7) |
| Stage 2A | 29(30.2) |
| Stage 2B | 6(6.3) |
| Stage 3A | 10(10.4) |
| Type of Treatment | |
| Surgery Only | 12(12.5) |
| Surgery + Radiation | 27(28.1) |
| Surgery + Chemotherapy | 25(26.0) |
| Surgery + Chemotherapy + Radiation | 32(33.3) |
| Tamoxifen | |
| No | 62(64.6) |
| Yes | 34(35.4) |
| Aromatase Inhibitor | |
| No | 59(61.5) |
| Yes | 37(38.5) |
| Cardiac Meds | |
| No | 78(81.3) |
| Yes | 18(18.8) |
| Age | 51.83(9.47) |
| BMI | 27.97(6.06) |
| ECR 16 anxiety scale | 20.37(8.88) |
| ECR 16 avoidance scale | 21.54(8.36) |
| RMSSD (ms) | 27.48(17.92) |
| Months since treatment ended | 10.56(7.71) |
Table 2.
Raw correlations between study variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Attachment anxiety | --- | ||||||||
| 2. Attachment avoidance | .388*** | --- | |||||||
| 3.RSA | -.117 | .001 | --- | ||||||
| 4. Age | -.029 | -.014 | -.251 | --- | |||||
| 5. Cancer Stage | -.097 | -.026 | -.024 | -.080 | --- | ||||
| 6. BMI | .037 | -.072 | -.166 | .136 | -.057 | --- | |||
| 7. Comorbidities | -.004 | -.021 | -.106 | .158 | .068 | -.007 | --- | ||
| 8. Time Since Tx | .013 | .059 | -.055 | .075 | -.146 | .131 | .032 | --- | |
| 9. Cardiac Meds | .077 | -.025 | -.067 | .360*** | .087 | .257* | .230* | .132 | --- |
| 10 Fact-B Total Score | -.397** | -.312** | .079 | .003 | -.183 | -.210* | -.087 | -.052 | -.108 |
Note.
p<.05,
p<.01,
p<.001
Table 3.
Linear regression output for primary analyses.
| Fact B total Score | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Model | Variable | b | SE | p | R2change | 95% CI |
|
| ||||||
| Step 1 | Cancer Stage | -2.732 | 1.564 | .084 | .027 | -5.843, .379 |
| Comorbidities | -3.221 | 3.518 | .363 | .008 | -10.218, 3.775 | |
| Cardiac Meds | -1.577 | 4.861 | .746 | .001 | -11.243, 8.089 | |
| BMI | -.576 | .296 | .055 | .033 | -1.165, .014 | |
| Age | .096 | .196 | .627 | .002 | -.295, .486 | |
| Time Since Tx | -.075 | .221 | .736 | .001 | -.513, .364 | |
| RSA | 1.341 | 2.737 | .625 | .002 | -4.102, 6.783 | |
| Anxiety | -.568 | .208 | .008 | .063 | -.983, -.153 | |
| Avoidance | -.444 | .220 | .047 | .036 | -.881, -.007 | |
| F | 3.361 | .001 | ||||
| df | (9,84) | |||||
| R2 | .265 | |||||
|
| ||||||
| Step 2 | Cancer Stage | -3.061 | 1.543 | .051 | .034 | -6.131, .008 |
| Comorbidities | -3.096 | 3.453 | .372 | .007 | -9.963, 3.771 | |
| Cardiac Meds | -1.810 | 4.77 | .705 | .002 | -11.298, 7.678 | |
| BMI | -.601 | .291 | .042 | .036 | -1.180, -.022 | |
| Age | .120 | .193 | .536 | .004 | -.264, .504 | |
| Time Since Tx | -.179 | .222 | .423 | .006 | -.621, .263 | |
| RSA | .853 | 2.69 | .753 | .001 | -4.509, 6.214 | |
| Anxiety | -.585 | .205 | .005 | .097 | -.993, -.178 | |
| Avoidance | -.408 | .216 | .063 | .030 | -.838, .022 | |
| Avoidance × RSA | .718 | .348 | .042 | .036 | .026, 1.410 | |
| F | 3.567 | .001 | ||||
| df | (10, 83) | |||||
| R2 | .301 | |||||
In ancillary analyses, we added social support to the regression model as a last step. Perceived social support was associated with better quality of life (b = .39, t = 2.67, p = .001). Consistent with the primary analyses, attachment anxiety was associated with poorer QOL (b = -.49, t = -2.46, p = .016), even with perceived social support included in the model. Furthermore, the interaction between attachment avoidance and RSA predicting QOL was still significant (b = .84, t = 2.48, p = .015).
Discussion
Breast cancer survivors with more attachment anxiety reported poorer QOL than those with less attachment anxiety. Women who were more avoidantly attached also reported poorer QOL compared with those who were less avoidantly attached. Furthermore, attachment avoidance interacted with RSA to predict QOL such that those with higher attachment avoidance were only vulnerable to poorer QOL if they also had lower self-regulatory capacity, as indexed by lower RSA. Attachment anxiety has been previously linked to both emotional well-being after a stressful life event and more physical symptoms among people without a history of cancer [5-8]. Attachment avoidance was also recently related to poorer loss adjustment, but only for those with lower RSA [5]. The current study extends prior work in an important new direction by demonstrating that attachment anxiety and avoidance are risk factors for poor QOL among breast cancer survivors. A subset of breast cancer survivors experience QOL of life issues long after treatment completion. Accordingly, the current results demonstrate that attachment anxiety and the combination of attachment avoidance and low RSA are risk factors for poor QOL among an already vulnerable population. Future work should examine this relationship over time to determine if attachment insecurity and RSA before treatment predict post-treatment quality of life.
RSA was not directly related to quality of life among cancer survivors. Rather, RSA interacted with attachment avoidance to predict quality of life. These findings are consistent with work in developmental psychology suggesting that RSA interacts with psychosocial and environmental differences to predict health outcomes [46, 47]. A broader understanding of why RSA is differentially predictive of health outcomes is imperative for future quality of life research.
There is considerable evidence demonstrating that social support plays an important role in both the mental and physical health outcomes of cancer survivors such that those with more social support have a better quality of life compared with those who have less support [48]. Attachment theory suggests that previous interactions with close relationship partners contribute to the development of one's willingness and ability to use others for support [9, 10]. However, perceptions of support did not explain the associations between attachment insecurity and quality life. Accordingly, attachment insecurity is a unique predictor of quality of life over and above its relationship with social support.
Recent work demonstrated that those who were abused or neglected as children experienced more cancer-specific psychological distress, more fatigue, and poorer physical, emotional, functional, and breast cancer specific well-being after treatment [49]. Attachment insecurity to one's parents has been linked to child maltreatment [50, 51]. The current study investigated attachment relationships to other adults, which theoretically are based on an individuals' earliest attachment to his/her caregiver [52]. Accordingly, the current investigation may add to the emerging literature demonstrating a link between early life stress and post-treatment quality of life among cancer survivors [49]. However, attachment orientations do become “updated” over time based on people's current relationships [53-55]. Accordingly, someone's attachment orientation in adulthood is not necessarily reflective of their childhood attachment relationships.
RSA is theorized to reflect self-regulatory capacity. Having poor self-regulatory capacity, as indexed by lower RSA, has been associated with maladaptive coping strategies, negative emotional traits, poor regulation of negative affect, and depressive symptoms [40-42]. These characteristics have clear links to emotional well-being after a cancer diagnosis and its treatment. Indeed, one's capacity to regulate negative affect may reduce distressing thoughts that are common among breast cancer survivors such as fears of cancer recurrence, feelings of unattractiveness, and heightened preoccupation with death [2, 56-60]. Furthermore, chronic pain and fatigue, two of the most common physical problems among cancer survivors, are clearly related depression and one's ability to regulate negative affect [61-63]. Accordingly, RSA and these other factors likely simultaneously contribute to breast cancer survivor's physical well-being.
We did not control for respiration rate or depth, which can alter the validity of the RSA assessment [64]. We used the root mean square of successive differences (RMSSD) rather than HF-HRV because RMSSD is recommended for studies that do not control for respiratory rate and respiratory depth; RMSSD is less affected by changes in breathing frequency than HF-HRV [65]. Finally, we assessed RMSSD during a resting baseline assessment, which further reduces risk of respiratory artifacts.
We focused exclusively on female breast cancer survivors; thus, we do not know if our findings generalize to men. Future work assessing cancers that predominately affect males are needed in order to generalize our results to men. Additionally, our sample was predominately white, another limitation of our study that could be addressed in future work with a more diverse sample. Finally, our study design was cross-sectional. Additional research that prospectively examines the associations among attachment style, HRV, and QOL before and after cancer treatment would be beneficial to better understand the direction of these relationships. Well after treatment-related problems subside, many breast cancer survivors report QOL difficulties. This research demonstrated that attachment anxiety is a risk factor for poor QOL among breast cancer survivors. In addition, attachment avoidance enhances risk for QOL problems among people with lower self-regulatory capacity, as indexed by lower RSA. A better understanding of how attachment style and RSA contribute to breast cancer survivor QOL will help in identifying who is most at risk for quality of life difficulties after treatment.
Figure 1.
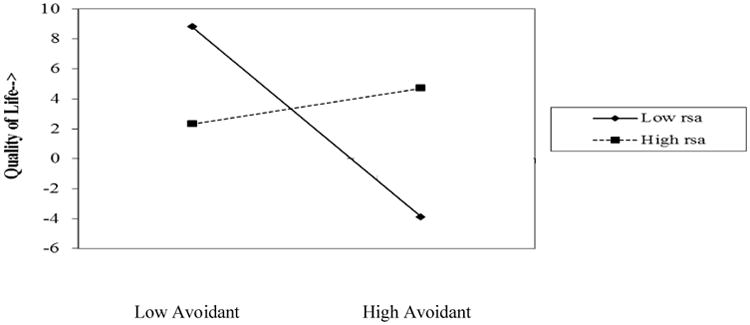
The moderating role of RSA in the relationship between attachment avoidance and quality of life. Regression lines for individuals scoring 1 SD above and below the sample means are plotted on each of the predictor variables.
Acknowledgments
Work on this paper was supported in part by NIH grants R01CA126857, R01 CA131029, NCRR Grant UL1RR025755, which funds the Clinical Research Center, the Ohio State Comprehensive Cancer Center Core Grant CA16058, senior mentorship award K05 CA172296 and American Cancer Society Postdoctoral Fellowship Grants PF-11-007-01-CPPB and 121911-PF-12-040-01-CPPB awarded to the first and second author, respectively.
References
- 1.Ekmektzoglou KA, et al. Breast cancer: from the earliest times through to the end of the 20th century. European Journal Of Obstetrics, Gynecology, And Reproductive Biology. 2009;145(1):3–8. doi: 10.1016/j.ejogrb.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 2.Ganz PA, et al. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. Journal of the National Cancer Institute. 2002;94(1):39–49. doi: 10.1093/jnci/94.1.39. [DOI] [PubMed] [Google Scholar]
- 3.Palmer SC, et al. Experience of trauma, distress, and posttraumatic stress disorder among breast cancer patients. Psychosomatic Medicine. 2004;66(2):258. doi: 10.1097/01.psy.0000116755.71033.10. [DOI] [PubMed] [Google Scholar]
- 4.Epplein M, et al. Quality of life after breast cancer diagnosis and survival. Journal of Clinical Oncology. 2011;29(4):406–412. doi: 10.1200/JCO.2010.30.6951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fagundes CP, Diamond LM, Allen KP. Adolescent attachment insecurity and parasympathetic functioning predict future loss adjustment. Personality and Social Psychology Bulletin. 2012;38(6):821–832. doi: 10.1177/0146167212437429. [DOI] [PubMed] [Google Scholar]
- 6.Wayment HA, Vierthaler J. Attachment style and bereavement reactions. Journal of Loss &Trauma. 2002;7(2):129–149. [Google Scholar]
- 7.Davis D, Shaver PR, Vernon ML. Physical, emotional, and behavioral reactions to breaking up: The roles of gender, age, emotional involvement, and attachment style. Personality and Social Psychology Bulletin. 2003;29(7):871–884. doi: 10.1177/0146167203029007006. [DOI] [PubMed] [Google Scholar]
- 8.Mikulincer M, Florian V. The relationship between adult attachment styles and emotional and cognitive reactions to stressful events. Attachment theory and close relationships. 1998;143:165. [Google Scholar]
- 9.Thompson RA. Early Attachment and Later Development. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. Guilford; New York, NY: 1999. pp. 265–286. [Google Scholar]
- 10.Mikulincer M, Shaver PR. An attachment and behavioral systems perspective on social support. Journal of Social and Personal Relationships. 2009;26(1):7–19. [Google Scholar]
- 11.Mikulincer M, Shaver PR. Attachment in adulthood: Structure, dynamics, and change. New York, NY US: Guilford Press; 2007. Attachment in adulthood: Structure, dynamics, and change. [Google Scholar]
- 12.Brennan KA, Clark CL, Shaver PR. Self-report measurement of adult attachment: An integrative overview. In: Simpson JA, Rholes WS, editors. Attachment theory and close relationships. Guilford press; New York: 1998. pp. 46–76. [Google Scholar]
- 13.Fraley RC, Shaver PR. Adult romantic attachment: Theoretical developments, emerging controversies, and unanswered questions. Review of General Psychology. 2000;4:132–154. [Google Scholar]
- 14.Diamond LM. Contributions of psychophysiology to research on adult attachment: Review and recommendations. Personality and Social Psychology Review. 2001;5:276–295. [Google Scholar]
- 15.Diamond L, Fagundes C. Psychobiological research on attachment. Journal of Social and Personal Relationships. 2010;27(2):218. [Google Scholar]
- 16.Feeney J. Implications of attachment style for patterns of health and illness. Child: care, health and development. 2000;26(4):277–288. doi: 10.1046/j.1365-2214.2000.00146.x. [DOI] [PubMed] [Google Scholar]
- 17.Maunder RG, Hunter JJ. Attachment relationships as determinants of physical health. Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry. 2008;36(1):11–32. doi: 10.1521/jaap.2008.36.1.11. [DOI] [PubMed] [Google Scholar]
- 18.Maunder RG, Hunter JJ. Attachment and psychosomatic medicine: developmental contributions to stress and disease. Psychosomatic medicine. 2001;63(4):556–567. doi: 10.1097/00006842-200107000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Ciechanowski PS, et al. Attachment theory: a model for health care utilization and somatization. Psychosomatic Medicine. 2002;64(4):660–667. doi: 10.1097/01.psy.0000021948.90613.76. [DOI] [PubMed] [Google Scholar]
- 20.Meredith PJ, Strong J, Feeney JA. The relationship of adult attachment to emotion, catastrophizing, control, threshold and tolerance, in experimentally-induced pain. Pain. 2006;120(1):44–52. doi: 10.1016/j.pain.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 21.Meredith P, Strong J, Feeney JA. Adult attachment, anxiety, and pain self-efficacy as predictors of pain intensity and disability. Pain. 2006;123(1):146–154. doi: 10.1016/j.pain.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 22.Fagundes CP. Getting over you: Contributions of attachment theory for postbreakup emotional adjustment. Personal Relationships. 2012;19(1):37–50. [Google Scholar]
- 23.Cicero V, et al. The role of attachment dimensions and perceived social support in predicting adjustment to cancer. Psycho-Oncology. 2009;18(10):1045–1052. doi: 10.1002/pon.1390. [DOI] [PubMed] [Google Scholar]
- 24.Macdonald G, Kingsbury R. Does physical pain augment anxious attachment? Journal of Social and Personal Relationships. 2006;23(2):291–304. [Google Scholar]
- 25.McWilliams L, Asmundson G. Assessing individual differences in attention to pain: Psychometric properties of the Pain Vigilance and Awareness Questionnaire modified for a non-clinical pain sample. Personality and individual differences. 2001;31(2):239–246. [Google Scholar]
- 26.McWilliams LA, Asmundson G. The relationship of adult attachment dimensions to pain-related fear, hypervigilance, and catastrophizing. Pain. 2007;127(1-2):27. doi: 10.1016/j.pain.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 27.Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders. 2000;61(3):201–216. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- 28.Porges SW. The polyvagal theory: phylogenetic substrates of a social nervous system. International Journal of Psychophysiology. 2001;42(2):123–146. doi: 10.1016/s0167-8760(01)00162-3. [DOI] [PubMed] [Google Scholar]
- 29.Brady MJ, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol. 1997;15(3):974–86. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- 30.Lo C, et al. Measuring attachment security in patients with advanced cancer: Psychometric properties of a modified and brief experiences in Close Relationships Scale. Psycho-Oncology. 2009;18(5):490–499. doi: 10.1002/pon.1417. [DOI] [PubMed] [Google Scholar]
- 31.Courneya KS, et al. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: Cardiopulmonary and quality of life outcomes. Journal of Clinical Oncology. 2003;21(9):1660–1668. doi: 10.1200/JCO.2003.04.093. [DOI] [PubMed] [Google Scholar]
- 32.Charlson M, et al. Validation of a combined comorbidity index. Journal of Clinical Epidemiology. 1994;47(11):1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 33.Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- 34.Edge SB, et al., editors. AJCC Cancer Staging Manual. 7th. Springer; New York: 2010. [Google Scholar]
- 35.Nunan D, et al. Validity and Reliability of Short-Term Heart-Rate Variability from the Polar S810. Medicine and Science in Sports and Exercise. 2009;41(1):243–250. doi: 10.1249/MSS.0b013e318184a4b1. [DOI] [PubMed] [Google Scholar]
- 36.Gamelin F, Berthoin S, Bosquet L. Validity of the polar S810 heart rate monitor to measure RR intervals at rest. Medicine and Science in Sports and Exercise. 2006;38(5):887. doi: 10.1249/01.mss.0000218135.79476.9c. [DOI] [PubMed] [Google Scholar]
- 37.Tarvainen M, et al. Kubios HRV—A Software for Advanced Heart Rate Variability Analysis. Springer; 2009. [Google Scholar]
- 38.Malik M, et al. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation. 1996;93(5):1043. [PubMed] [Google Scholar]
- 39.Stein P, et al. Heart rate variability: a measure of cardiac autonomic tone. American heart journal. 1994;127(5):1376–1381. doi: 10.1016/0002-8703(94)90059-0. [DOI] [PubMed] [Google Scholar]
- 40.Fabes RA, Eisenberg N. Regulatory control and adults' stress-related responses to daily life events. Journal of personality and social psychology. 1997;73(5):1107. doi: 10.1037//0022-3514.73.5.1107. [DOI] [PubMed] [Google Scholar]
- 41.Thayer JF, Brosschot JF. Psychosomatics and psychopathology: looking up and down from the brain. Psychoneuroendocrinology. 2005;30(10):1050–1058. doi: 10.1016/j.psyneuen.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 42.Tang D, Schmeichel BJ. Stopping anger and anxiety: Evidence that inhibitory ability predicts negative emotional responding. Cognition & emotion. 2013:1–11. doi: 10.1080/02699931.2013.799459. ahead-of-print. [DOI] [PubMed] [Google Scholar]
- 43.Segerstrom SC, Nes LS. Heart rate variability reflects self-regulatory strength, effort, and fatigue. Psychological science. 2007;18(3):275–281. doi: 10.1111/j.1467-9280.2007.01888.x. [DOI] [PubMed] [Google Scholar]
- 44.Thayer JF, Lane RD. Claude Bernard and the heart–brain connection: Further elaboration of a model of neurovisceral integration. Neuroscience & Biobehavioral Reviews. 2009;33(2):81–88. doi: 10.1016/j.neubiorev.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 45.Priel B, Shamai D. Attachment style and perceived social support: Effects on affect regulation. Personality and Individual Differences. 1995;19(2):235–241. [Google Scholar]
- 46.El-Sheikh M. Does poor vagal tone exacerbate child maladjustment in the context of parental problem drinking? A longitudinal examination. Journal of abnormal psychology. 2005;114(4):735. doi: 10.1037/0021-843X.114.4.735. [DOI] [PubMed] [Google Scholar]
- 47.El-Sheikh M, et al. Marital conflict and children's externalizing behavior: Pathways involving interactions between parasympathetic and sympathetic nervous system activity. Monographs of the Society for Research in Child Development. 2009;74(1):vii. doi: 10.1111/j.1540-5834.2009.00501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nausheen B, et al. Social support and cancer progression: a systematic review. Journal of Psychosomatic Research. 2009;67(5):403–415. doi: 10.1016/j.jpsychores.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 49.Fagundes CP, et al. Child maltreatment and breast cancer survivors: Social support makes a difference for quality of life, fatigue and cancer stress. European Journal of Cancer. 2012;48(5):728–736. doi: 10.1016/j.ejca.2011.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.George C. A representational perspective of child abuse and prevention: Internal working models of attachment and caregiving. Child Abuse & Neglect. 1996;20(5):411–424. doi: 10.1016/0145-2134(96)00016-6. [DOI] [PubMed] [Google Scholar]
- 51.Cassidy J, Berlin LJ. The insecure/ambivalent pattern of attachment: Theory and research. Child development. 1994;65(4):971–991. [PubMed] [Google Scholar]
- 52.Fraley RC, Waller NG, Brennan KA. An item response theory analysis of self-report measures of adult attachment. Journal of Personality and Social Psychology. 2000;78(2):350–65. doi: 10.1037//0022-3514.78.2.350. [DOI] [PubMed] [Google Scholar]
- 53.Baldwin MW, Fehr B. On the instability of attachment style ratings. Personal Relationships. 1995;2(3):247–261. [Google Scholar]
- 54.Collins NL, Read SJ. Cognitive representations of attachment: The structure and function of working models. In: Bartholomew K, Perlman D, editors. Advances in personal relationships: A research annual. Jessica Kingsley Publishers; London: 1994. pp. 53–90. [Google Scholar]
- 55.La Guardia JG, et al. Within-person variation in security of attachment: A self-determination theory perspective on attachment, need fulfillment, and well-being. Journal of Personality and Social Psychology. 2000;79:367–84. doi: 10.1037//0022-3514.79.3.367. [DOI] [PubMed] [Google Scholar]
- 56.Schag C, et al. Characteristics of women at risk for psychosocial distress in the year after breast cancer. Journal of Clinical Oncology. 1993;11(4):783. doi: 10.1200/JCO.1993.11.4.783. [DOI] [PubMed] [Google Scholar]
- 57.Fallowfield LJ, et al. Assessment of quality of life in women undergoing hormonal therapy for breast cancer: validation of an endocrine symptom subscale for the FACT B. Breast cancer research and treatment. 1999;55(2):187–197. doi: 10.1023/a:1006263818115. [DOI] [PubMed] [Google Scholar]
- 58.Brady MJ, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. Journal of Clinical Oncology. 1997;15(3):974. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- 59.Cleeland CS, et al. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919–2925. doi: 10.1002/cncr.11382. [DOI] [PubMed] [Google Scholar]
- 60.Van Harten W, et al. Assessment of rehabilitation needs in cancer patients. International Journal of Rehabilitation Research. 1998;21(3):247. doi: 10.1097/00004356-199809000-00001. [DOI] [PubMed] [Google Scholar]
- 61.Bower JE, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106(4):751–758. doi: 10.1002/cncr.21671. [DOI] [PubMed] [Google Scholar]
- 62.Wang HL, et al. Predictors of cancer-related pain improvement over time. Psychosomatic Medicine. 2012;74(6):642–647. doi: 10.1097/PSY.0b013e3182590904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cella D, et al. Cancer-related fatigue: prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. Journal of clinical oncology. 2001;19(14):3385–3391. doi: 10.1200/JCO.2001.19.14.3385. [DOI] [PubMed] [Google Scholar]
- 64.Berntson GG. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology. 1997;34:623–648. doi: 10.1111/j.1469-8986.1997.tb02140.x. [DOI] [PubMed] [Google Scholar]
- 65.Penttila J, et al. Time domain, geometrical and frequency domain analysis of cardiac vagal outflow: effects of various respiratory patterns. Clinical Physiology. 2001;21(3):365–376. doi: 10.1046/j.1365-2281.2001.00337.x. [DOI] [PubMed] [Google Scholar]


