Insulin is an anabolic hormone with powerful metabolic effects. The events after insulin binds to its receptor are highly regulated and specific. Defining the key steps that lead to the specificity in insulin signaling presents a major challenge to biochemical research, but the outcome should offer new therapeutic approaches for treatment of patients suffering from insulin-resistant states, including type 2 diabetes.
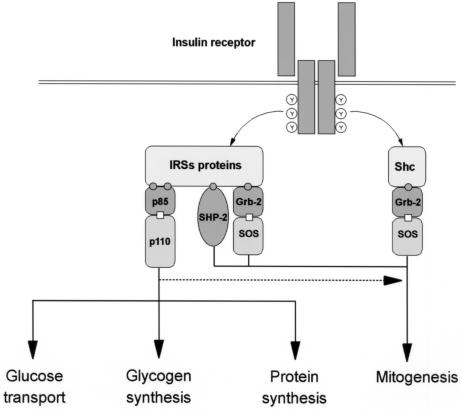
The insulin receptor belongs to the large family of growth factor receptors with intrinsic tyrosine kinase activity. Following insulin binding, the receptor undergoes autophosphorylation on multiple tyrosine residues. This results in activation of the receptor kinase and tyrosine phosphorylation of a family of insulin receptor substrate (IRS) proteins. These substrates are commonly referred to as docking proteins, since several other intracellular proteins bind to the phosphorylated substrates, thereby transmitting the signal downstream. Like other growth factors, insulin uses phosphorylation and the resultant protein–protein interactions as essential tools to transmit and compartmentalize its signal. These intracellular protein–protein interactions are pivotal in transmitting the signal from the receptor to the final cellular effect, such as translocation of vesicles containing GLUT4 glucose transporters from the intracellular pool to the plasma membrane, activation of glycogen or protein synthesis, and initiation of specific gene transcription (Figure 1). In this article, we review some of our current understanding about early insulin signal transduction through the network of IRS interacting proteins and the mechanisms that may modify insulin signal transduction in insulin-resistant states, especially obesity and type 2 diabetes.
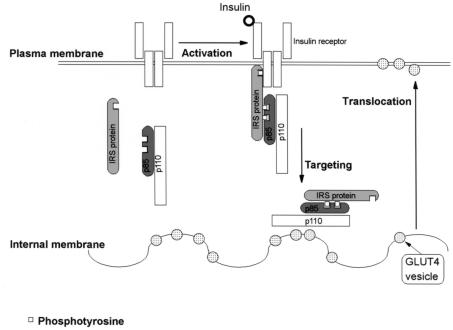
Figure 1.
Schematic illustration of major signaling pathways of insulin action. The phosphorylated insulin receptor binds and phosphorylates IRS proteins and Shc, which bind differentially to various downstream signaling proteins. PI3-kinase is critical for metabolic actions of insulin, such as glucose transport, glycogen synthesis, and protein synthesis, whereas Grb-2/SOS complex, which activates the MAP kinase cascade, is critical in mitogenic response. PI3-kinase probably modulates the mitogenic response as well.
Protein–protein interactions
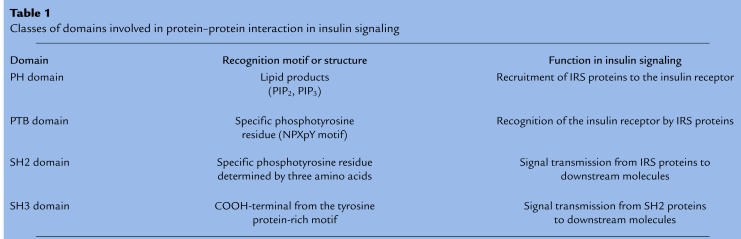
Some of the best-characterized protein interaction domains involved in insulin signaling are the PH (pleckstrin homology), PTB (phosphotyrosine binding), SH2, and SH3 domains (1) (Table 1). Other, less-characterized domains (e.g., LIM, PDZ, NOTCH, and WW) may also prove to be relevant (2). These interaction domains exist in the natural tertiary structure of proteins. In other cases, the domains for interaction are created by posttranslational covalent modification of the protein. The most common examples of the latter are the effects of phosphorylation of proteins on tyrosine or serine/threonine residues and the lipid modification by prenylation or fatty acid acylation
Table 1.
Classes of domains involved in protein–protein interaction in insulin signaling
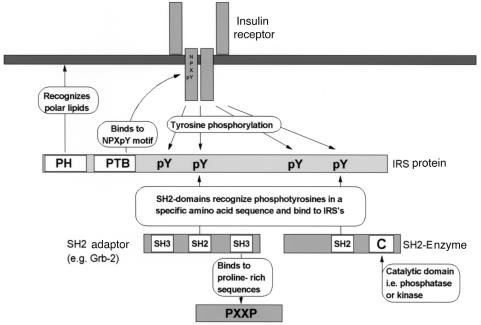
Figure 2 illustrates how signal transduction is transmitted from the receptor downstream using different types of domains. PH domains, which are found in most of the proteins that interact with the insulin receptor, bind to charged headgroups of specific phosphatidylinositides and are thereby targeted preferentially to membrane structures. PH domains in the IRS proteins target the proteins to the membrane adjacent to the insulin receptor (3). PTB domains, also found in IRS proteins, recognize the phosphotyrosine in the amino acid sequence asparagine-proline-any amino acid-phosphotyrosine (NPXpY), often present in tyrosine kinase receptors, including insulin receptor (4, 5).
Figure 2.
Protein–protein interaction domains involved in insulin signal transduction. A typical IRS protein contains a PH domain, which targets the protein in plasma membrane, and a PTB domain, which binds to NPXpY motif in the β subunit of the insulin receptor. SH2 domains of SH2 adaptors and SH2 enzymes bind to multiple phosphotyrosines of IRS proteins. SH2 adaptors frequently possess SH3 domains that recognize PXXP motifs of other intracellular proteins, leading to further downstream signal transduction.
Most of the intracellular partners of the insulin receptor substrates contain Src homology 2 (SH2) domains. These domains are also phosphotyrosine binding cassettes but tend to have higher binding affinity than PTB domains and recognize specific amino acid patterns, making a more rigid protein–protein interaction possible. SH2 domains consist of roughly 100 amino acids, including a highly conserved phosphotyrosine binding pocket (FLAVRES sequence) (6). The specificity of the binding is regulated by the few amino acids COOH-terminal to the phosphotyrosine. The SH2 domains of PI3-kinase recognize at least four pYMXM motifs in tyrosine-phosphorylated IRS-1. The SH2 domain of the adaptor protein Grb-2 and the SH2 domain of the phosphotyrosine phosphatase SHP-2 bind other sequences, including pYVNI, pYIDL, and pYASI sequences (1). In addition to these adaptor proteins, other SH2 proteins, such as Crk (adaptor), Nck (adaptor), Fyn (tyrosine kinase), and Csk (tyrosine kinase), bind to tyrosine residues on IRS proteins through their specific SH2 domains. SH3 domains are often present in these SH2 adaptor proteins. SH3 domains bind to proline-rich sequences with the consensus sequence PXXP with a specific helix structure and provide a link between the adaptor protein and its downstream targets or associated catalytic subunits (6).
It should be kept in mind that many of these recognition elements bind signaling proteins to a specific target, be it another protein, a membrane or cytoskeletal structure, or, as with transcription factors, a specific nucleotide sequence, with amazing accuracy. Many signaling proteins contain more than one of these domains, as well as other recognition elements. There are numerous proteins, which bind to other proteins with unknown mechanisms or undefined domains. These include the 14-3-3 proteins, the transforming protein simian virus 40 (SV40) large T antigen, Ca2+ ATPase, and β integrin, discussed in detail below.
Insulin signal transduction network
Insulin receptor
The insulin receptor is a heterotetramer consisting of two ligand-binding α subunits and two tyrosine kinase β subunits (7–9). Insulin binding leads to activation of the tyrosine kinase of one of the two β subunits and a rapid cascade of autophosphorylation of the receptor itself. Several crucial tyrosine residues are phosphorylated in a fully activated insulin receptor. Phosphotyrosine at site 960 of the β subunit just inside the membrane creates an NPXpY-recognition motif for the PTB domain of the IRS proteins. Modification of this tyrosine completely inhibits subsequent phosphorylation of IRS-1 and other insulin receptor substrates and leads to loss of most insulin-dependent biological actions (10). Interestingly, this NPXY sequence is also a receptor internalization motif found in many members of the tyrosine kinase receptor family, the low-density lipoprotein receptor (11–13), and the transferrin receptor (14), all of which are internalized in a ligand-dependent fashion. Although most data suggest that internalization is not required for insulin action, internalization could contribute to the compartmentalization of some insulin signals.
Insulin-like growth factor-1 (IGF-1) receptor has a similar structure to the insulin receptor and even forms chimeric hybrids with the insulin receptor (15). Physiologically, however, insulin and IGF-1 serve very different functions. How this occurs is still unclear, but one possibility is an additional phosphorylation site in the COOH-terminus of the insulin receptor, not present in the IGF-1 receptor, which could potentially interact with PI3-kinase or some other SH2 proteins (16). There are also other differences that could contribute to the specificity of signaling.
Insulin receptor substrates
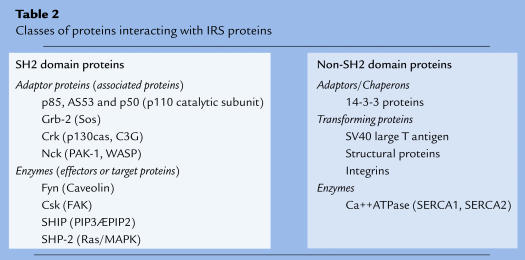
Insulin receptor substrates are a growing family of proteins that are phosphorylated by the activated insulin receptor. To date, nine members of this family have been identified, including IRS-1 (17, 18), IRS-2 (19), IRS-3 (20), and IRS-4 (21), which are generally viewed as the most specific for insulin signaling; Gab-1 (22); Shc, which has three isoforms (23); and p62dok (24). Figure 2 shows the relationship between structure and function of a typical IRS protein. The NH2-terminal PH domain, involved in the targeting of the IRS proteins to the membrane and the insulin receptor, is found in all proteins in this family, except the Shc. All of the substrates, except Gab-1, have a PTB domain located just COOH-terminal to the PH domain. The PTB domain is critical for recognition of the NPXpY sequence in the insulin receptor. Thus, in most substrates, both a PTB domain and a PH domain contribute to the interaction with the receptor, presumably cooperating with other domains in IRS proteins. From the functional point of view, all proteins in this family bind to the autophosphorylated insulin receptor only transiently and then dissociate, after which they can be recognized by SH2 domains of several proteins (Table 2). During interaction with the insulin receptor, the IRS proteins are phosphorylated on several tyrosine residues by the insulin receptor, creating binding sites for multiple SH2 domain proteins (1).
Table 2.
Classes of proteins interacting with IRS proteins
Shc binds to the activated insulin receptor and is phosphorylated by a mechanism similar to IRS-1. Shc contains a special PTB domain, which makes phosphorylation possible even without a PH domain. Also, unlike other members of the insulin receptor substrate family, Shc contains only a single phosphorylation site that binds an adaptor protein, Grb-2. This can lead to activation of a Ras/MAP kinase (MAPK) pathway and stimulation of the mitogenic signaling pathway (23). Compared with other growth factor stimuli, insulin is a weak stimulator of Shc tyrosine phosphorylation.
Gab-1 is a high-molecular-weight protein, like the IRS proteins, that contains a PH domain and several phosphorylation sites but has no PTB domain. Gab-1 is heavily phosphorylated by the epidermal growth factor receptor, but poorly by the insulin receptor (22). The biological function of Gab-1 is unknown, although it is expressed in many mammalian tissues.
p62dok was originally described as a protein that could be phosphorylated by several receptor tyrosine kinases (24), including the insulin receptor, however, its role in insulin signaling has not been determined. Recently, phosphorylated p62dok was demonstrated to associate with the GTPase-activating protein (GAP) for Ras. Since phosphorylated p62dok does not have any putative PI3-kinase binding sites, it is unlikely to have a role in the metabolic actions of insulin.
Grb-IR is a recently discovered SH2 domain protein that may translocate from the cytosol to the plasma membrane and bind directly to the tyrosine-phosphorylated insulin receptor (25). Grb-IR binds to the critical NPEpY960 in the juxtamembrane region of the insulin receptor through its SH2 domain. It also contains an additional binding site located in the phosphorylated kinase activation loop of the insulin receptor but is only very slightly phosphorylated by insulin receptor. Overexpression of Grb-IR inhibits insulin- and IGF-1–induced mitogenic effects, as well as PI3-kinase activation. It is not known whether it acts solely as an inhibitor of insulin receptor or whether its interaction with the insulin receptor has distinct cellular effects.
SH2 adaptor proteins
SH2 adaptor proteins recognize and bind to tyrosine-phosphorylated proteins by their SH2 domains. They do not possess intrinsic enzymatic activity but relay the ligand signal by additional protein–protein interactions. The regulatory subunits of PI3-kinase, as well as Grb2, are well-known examples of adaptor proteins. However, several other potentially important adaptor proteins have been described (Table 2). Since many of these were identified as cellular homologues of oncogenes, they are represented by three-letter acronyms, such as Crk and Nck.
PI3-kinase regulatory subunits.
PI3-kinase is a lipid kinase and a key element in the pathway leading to metabolic effects of insulin. PI3-kinase consists of a regulatory subunit responsible for binding to insulin receptor substrates and a catalytic subunit responsible for phosphorylation of phosphatidylinositols found in cellular membranes. There are at least eight different isoforms of the regulatory subunit. Six are derived by alternative splicing of the p85α gene. These include p85α (26), AS53 (also called p55α) (27, 28), and p50α, each of which occurs with and without a spliced insert (27). Two other isoforms, p85β (26) and p55PIK (29), are derived from separate genes. Each of these regulatory subunits associates with IRS proteins in response to insulin and transduces the signal from IRS proteins to PI3-kinase activation. Whereas p85α is ubiquitously expressed and thought to be responsible for ligand-dependent PI3-kinase signaling in many tissues, the other regulatory subunit isoforms are differentially expressed in various tissues (27, 28). Thus, each regulatory subunit might have a specific function dependent on its specific affinity to IRS proteins and ability to regulate PI3-kinase activity. It is also possible that each isoform participates in specific subcellular compartmentalization.
Inhibition of PI3-kinase activity using a dominant-negative mutant (30), or pharmacological agents such as wortmannin or LY294002 (31), abolishes insulin-stimulated glucose uptake and inhibits GLUT4 vesicle translocation to the plasma membrane. Many other cellular effects of insulin, such as antilipolysis, activation of fatty acid synthesis, acetyl CoA-carboxylase, glycogen synthase, Akt phosphorylation, glycogen synthase kinase 3β inactivation, and stimulation of protein synthesis and DNA synthesis, are also inhibited by PI3-kinase suppression (32)
PI3-kinase is activated by many other hormonal stimuli, which do not mimic insulin action. This raises the question, what are the insulin-specific features of PI3-kinase activation? Figure 3 shows some of these features. First, in contrast to other growth factors, the insulin receptor does not bind PI3-kinase directly but rather uses docking proteins, such as IRS proteins, as a relay mechanism. This results in activation of PI3-kinase in a different compartment of the cell than is the case of other growth factors. Indeed, translocation of PI3-kinase activity from the cytosol to intracellular membranes has been reported following insulin stimulation (33, 34). Second, the membrane surface area of the endoplasmic reticulum is large and thus has a greater pool of lipid substrates for PI3-kinase than the plasma membrane. Thus, it is possible that in vivo, insulin signal produces more PI3-kinase products than other hormones (34).
Figure 3.
Unique spatial compartmentalization of insulin signal transduction. Insulin receptor uses IRS proteins to activate PI3-kinase. Activated insulin receptor binds transiently IRS proteins, which becomes phosphorylated and thereafter bind the regulatory subunits (p85) of PI3-kinase. The IRS-1/PI3-kinase complex translocates to internal membranes, which provide abundant substrates for PI3-kinase and are in close proximity to the GLUT4 vesicle pool, which translocates to the plasma membrane in response to insulin.
Grb2.
Grb2 is one of the best-characterized SH2 adaptor proteins. Grb2 is a 27-kDa molecule with an SH3–SH2–SH3 domain structure (Figure 2) (35). Grb2 constitutively associates with Sos, the guanine nucleotide exchange factor for plasma membrane–bound Ras (36). Docking of Grb2 to IRS proteins recruits Sos to Ras, resulting in activation of its GTPase (37). This leads to subsequent activation of the serine/threonine kinase cascade known as the MAPK cascade. This cascade relays the signal from the plasma membrane to the nucleus and is the essential signaling pathway for mitogenesis.
In most growth factor receptor signaling pathways, Grb2 binds to a tyrosine residue on the receptor or the substrate Shc through its SH2 domain in a phosphorylation-dependent manner. Following insulin stimulation, Grb2 binds to both IRS proteins and to Shc, and it is not clear which pathway is more important for its activity (37, 38). In either case, the Grb2/Sos complex does not seem to be tightly fixed to the plasma membrane in response to insulin. This might contribute to the relatively weak mitogenic effect of insulin as compared with other growth factor–dependent signaling. Grb2 has also been reported to associate with other guanine nucleotide exchange factors, such as C3G, that may be involved in c-Jun kinase activation (39, 40).
Crk and Nck.
IRS proteins also bind several other adaptor proteins and proto-oncogenes whose roles are just beginning to unfold. Crk was originally identified as an oncogene product v-Crk. The cellular homologues of v-Crk are known as Crk-I (SH2–SH3 domain structure) and Crk-II (SH2–SH3–SH3) and are derived by alternative splicing from a single gene (41). Crk has been reported to associate with tyrosine-phosphorylated proteins, such as p130Cas and paxillin (42, 43), involved in the rearrangement of cytoskeletal components, through its SH2 domain. Recently, Crk has also been shown to bind to IRS-1 in an insulin-dependent manner (44). Crk uses its SH3 domains to bind to the guanine nucleotide exchange factors Sos and C3G, the latter of which activates the c-Jun kinase, leading to induction of transformation (40).
Nck is a 47-kDa multiadapter protein with an SH3–SH3–SH3–SH2 domain structure. Nck associates with IRS-1 (45), many different tyrosine kinases, several serine/threonine kinases through its SH2 domain, as well as Sos through its SH3 domains (46–48). Since overexpression of Nck results in transformation of cells, Nck may transmit the mitogenic signals from IRS proteins by interacting with these kinases and Sos.
SH2 enzymes
SH2 enzymes bind to tyrosine-phosphorylated proteins through their SH2 domains but also possess an intrinsic catalytic domain (usually a kinase or phosphatase domain). A large group of these proteins belong to a family of proto-oncogenes, or protein kinases regulating mitogenesis, including Fyn, c-Cbl, and Csk. Other SH2 domain partners of IRS proteins may modulate PI3-kinase activity (SHIP) or the level of tyrosine phosphorylation (SHP-2) by producing dephosphorylation of their representative substrates (Table 2). In general, the catalytic activity of each these SH2 enzymes is increased upon binding to the phosphorylated IRS proteins
Fyn/Cbl/CAP complex.
Fyn is a cytoplasmic protein tyrosine kinase that can be activated by association with other phosphotyrosine proteins through its SH2 domain or by dephosphorylation of its COOH-terminal tyrosine. Fyn is not activated directly by the insulin receptor, but rather by interaction with IRS-1 (49) and another insulin receptor substrate, c-Cbl (50). The latter protein contains a PTB domain and binds to SH2 adaptor proteins Grb2, Crk, and the p85 subunit of PI3-kinase; however, its physiological role still remains unclear (51). c-Cbl is tyrosine-phosphorylated, binds to Fyn upon insulin stimulation, and is translocated to small invaginations of the plasma membrane, called caveolae, after insulin stimulation (50). Recently, it was shown that Fyn is one of the kinases responsible for the phosphorylation of caveolin (50, 52), a protein present in caveolae. Insulin is unique in its ability to phosphorylate two isoforms of caveolin; this does not occur in response to other growth factors (50).
It has also been demonstrated that a c-Cbl–associated protein (CAP) that has three sequential SH3 domains is specifically expressed in insulin-responsive cell types and associates with both c-Cbl and the insulin receptor (53). Thiazolidinediones (TZDs), the class of insulin sensitizers that act through the nuclear receptor PPAR-γ, increase CAP expression levels and c-Cbl phosphorylation significantly in adipocytes (54), possibly contributing to their insulin-sensitizing effect.
Csk.
The COOH-terminal Src kinase (Csk) is a cytoplasmic tyrosine kinase that inactivates Src-type kinases by tyrosine phosphorylation (55). Csk has been reported to associate with IRS-1 through its SH2 domain and promote dephosphorylation of the focal adhesion kinase (FAK) in an insulin-dependent manner (56). FAK is one of the key players for cell–cell interaction and cell–extracellular matrix interaction in integrin and other growth factor signaling pathways. Thus, it is likely that Csk is involved in the insulin-induced rearrangement of cytoskeletal components by altering FAK activity in insulin signaling (57).
SHIP.
PI3-kinase activation produces PIP2 and PIP3. These are thought to act as second messengers for some biological responses of insulin and other growth factors by binding to PH domains of downstream molecules, such as serine/threonine kinases Akt/PKB and their activator PDK1 (58, 59). Recently, a 145-kDa protein, SHIP (SH2-containing inositol 5-phosphatase), has been identified as a specific phosphatase for 5′-phosphate of PIP4 and PIP3, converting the latter to PIP2 (60). Overexpression of SHIP by microinjection inhibits insulin-induced glucose transport and DNA synthesis, suggesting that PIP3, rather than PIP2, is the major mediator of PI3-kinase–dependent biological actions of insulin (61). SHIP contains multiple interaction domains with an SH2-phosphatase-NPXY-NPXY proline-rich domain structure. SHIP becomes tyrosine-phosphorylated following stimulation of cells with insulin, growth factors, and cytokines, after which it binds to the PTB domain of Shc. In the case of insulin, it is unclear whether SHIP associates with IRS proteins or the insulin receptor, although a recent report has demonstrated SHIP association with IRS-2 in response to erythropoietin (62).
SHP-2.
SHP-2 (previously known as SH-PTP2, PTP1D, or Syp) is a phosphotyrosine phosphatase that binds to the COOH-terminal phosphotyrosines of IRS proteins (63). It has two SH2 domains and is ubiquitously expressed. Based on in vitro studies with phosphotyrosine peptides corresponding to the binding site of SHP-2, the phosphatase activity of SHP-2 is increased upon binding to IRS-1. The physiological substrates for SHP-2 are not known, but overexpression of SHP-2 modulates cell adhesion and migration, as well as insulin activation of the Ras/MAP-kinase pathway (64, 65).
Proteins interacting with IRS proteins by unknown mechanisms
There are a number of proteins that associate with IRS proteins by unknown mechanisms. These proteins include adaptors (14-3-3 proteins), transforming proteins (SV40 large T antigen), structural proteins (integrins), and enzymes (the Ca2+ ATPases SERCA1 and SERCA2) (Table 2).
14-3-3 proteins were originally shown to activate tryptophan/tyrosine hydroxylases and modulate protein kinase C activity (66). Recently, 14-3-3 proteins have been found to associate with several oncogene products and cell-cycle control proteins, although roles of these interactions are still unclear (67). Several isoforms of 14-3-3 proteins (β, ε, and ζ) have also been shown to associate with IRS-1, presumably through one of the several RXRXXpS motifs of IRS-1. Since these motifs are located in the PTB domain and close to the YXXM motifs, it is possible that the interaction between 14-3-3 and IRS proteins modulates the recognition of IRS proteins by the insulin receptor or the PI3-kinase activity associated with IRS proteins (68, 69)
The large T antigen of SV40 is a multifunctional protein that is essential in both the virus lytic cycle and the oncogenic transformation of cells by SV40 (70). IRS-1 and SV40 associate in a manner critical for the transformation process. IRS-1 and SV40 large T-antigen proteins are capable when coexpressed, but not by themselves, of inducing oncogenic transformation (71). In some cells, this process is regulated by IGF-1.
Insulin and IGF-1 stimulation also promote association between IRS-1 and αVβ3 integrin (vitronectin receptor) (72). In smooth muscle cells, blocking ligand occupancy of αVβ3 integrin reduces IGF-1–induced IRS-1 phosphorylation (73). Recently, β1 integrins have also been reported to enhance IRS-1 phosphorylation and interaction, but not glucose transport, with downstream molecules such as PI3-kinase and Akt (74). These results suggest that integrins and insulin/IGF-1 receptor signaling pathways converge at an early point in the signaling cascade around the IRS proteins.
The Ca2+ ATPase of adult fast-twitch skeletal muscle (SERCA1) has also been shown to interact with tyrosine-phosphorylated IRS-1 by expression screening (75). A similar interaction also occurs with SERCA2 (cardiac muscle isoform). Both of these associate with IRS-1 and IRS-2 through an SH2-like domain and the pYGSS motif on the IRS proteins. Since an inhibitor against SERCA induces apoptosis in some cell lines (76), the IRS/SERCA complex might be involved in an insulin- and IGF-1–dependent antiapoptotic effect.
Alterations in protein–protein interactions in insulin-resistant states
As we learn more and more about the regulation of the insulin signaling network, a key question is, how is insulin signaling regulated in the pathophysiology of human disease? Recent studies in both animals and human tissues have demonstrated that both genetic and nongenetic factors can regulate insulin signaling by changing the sequence, expression level, or covalent modification of proteins involved in the intracellular network of insulin action.
Genetic alterations in the insulin signaling proteins
Insulin receptor.
Naturally occurring mutations of the insulin receptor are rare, and the phenotype, when present, is usually a syndrome of extreme insulin resistance, such as leprechaunism or the type A syndrome of insulin resistance and acanthosis nigricans. Since the first reports in 1988 (77, 78), over 100 such cases have been identified. Genomic analysis has indicated that mutations of the insulin receptor itself do not play an important role in the pathophysiology of typical type 2 diabetes or obesity. For a complete review of this subject, see ref. 79.
IRS-1.
IRS-1 was the first insulin receptor substrate identified and the first to be found to have multiple natural polymorphisms (80–84). Polymorphisms of IRS-1 are significantly more common in type 2 diabetic patients than in controls and include the G972R (glycine 972→arginine), S892G, G819R, R1221C, and A513P variants (80, 81). Of these, the G972R polymorphism is the most common and has been studied most extensively. This polymorphism is found in Caucasian populations, with a prevalence of 5.8% in normal and 10.7% in type 2 diabetic patients, respectively. In Caucasian populations, obese carriers of this polymorphism show decreased insulin sensitivity during an oral glucose tolerance test, and an individual homozygous for the codon 972 mutation had a diabetic response to dexamethasone challenge. The polymorphism G972R does not occur in Pima Indians (85).
Because the G972R polymorphism is associated with type 2 diabetes, lies between two potential tyrosine phosphorylation sites involved in binding of the p85 subunit of PI3-kinase, and potentially interferes with PI3-kinase binding to IRS-1, a series of in vitro experiments have been performed to explore the molecular effects of this sequence change (86). Indeed, expression of G972R variant of IRS-1 in 32D(IR) cells causes a specific defect in binding of the p85 subunit of PI3-kinase to IRS-1, and a 36% decrease in IRS-1–associated PI3-kinase activity (86). Insulin-stimulated IRS-1 tyrosine phosphorylation is normal, consistent with the idea that G972R interferes with the interaction between IRS-1 and the SH2 domains of PI3-kinase. The net effect is a 35–40% decrease in insulin’s final biological effect in these cells: stimulation of mitogenesis.
In Japanese type 2 diabetic patients, several additional polymorphisms have been described, including P190R, M209T, and S809F polymorphisms, and silent nucleotide variants L142 and G625 A804 (82). While the prevalence of each of these polymorphisms alone is not different between patients and healthy controls, the combined prevalence of these polymorphisms, along with the G972R polymorphism, is threefold greater compared with healthy controls (29.5 vs. 8.5%; P < 0.05). In vitro, 32D cells expressing these variants also show reduced PI3-kinase activation (87). In a euglycemic, hyperinsulinemic clamp, the insulin sensitivity in the carriers versus noncarriers of these polymorphism carriers is decreased 29.5% in type 2 diabetics and 22% in healthy subjects
Other insulin receptor substrates and PI3-kinase.
Recently, two polymorphisms in IRS-2 have been described in the Caucasian population: a substitution of G1057D and G879S. Amino acid polymorphisms of IRS-4 are also common in the Caucasian population. However, neither of these polymorphisms is associated with type 2 diabetes or insulin resistance (88, 89).
A common polymorphism of the p85α subunit of PI3-kinase changes methionine in position 326 to isoleucine. In one study, 31% of Caucasians carried the mutation in its heterozygous form and 2% in its homozygous form. This polymorphism occurs in a region between the SH3 domain and the first SH2 domain, but the functional effects have not been studied in vitro. Although the frequency is not increased in diabetes, homozygous individuals do exhibit a 32% reduction in insulin sensitivity compared with wild-type and heterozygous carriers in an intravenous glucose tolerance test (90).
Other modulators of insulin signaling
Peroxisome proliferator–activated receptor γ (PPAR-γ).
PPAR-γ is a nuclear receptor that appears to be an important regulator of adipogenesis (91). PPAR-γ has two isoforms, γ1 and γ2. PPAR-γ1 is ubiquitously expressed, whereas PPAR-γ2 is expressed mainly in adipose tissue (91). Although PPAR-γ is not directly a part of the insulin signaling pathway, insulin sensitizers, such as troglitazone and pioglitazone, bind to PPAR-γ with high affinity, activating the regulation of gene transcription. A rare, naturally occurring mutation of PPAR-γ (P115Q) in the immediate vicinity of an important regulatory phosphorylation site results in a constitutively active PPAR-γ (92). Carriers of this mutation suffer from extreme obesity without significant insulin resistance. In vitro, overexpression of P115Q in 3T3-L1 fibroblasts leads to rapid differentiation into adipocytes. Therefore, this rare form of obesity results from a constitutively active form of PPAR-γ, which leads to increased adipogenesis but simultaneously sensitizes the whole body to insulin action. Interestingly, another mutation in the unique region PPAR-γ2 (P12A) was recently reported to be associated with lower body mass index and improved insulin sensitivity (93).
Plasma cell differentiation factor-1 (PC-1).
PC-1 is a membrane glycoprotein with ectonucleotide pyrophosphatase activity that seems to act as an intrinsic inhibitor of insulin receptor tyrosine kinase activity (94, 95). In healthy subjects with no clinically significant defects in glucose metabolism, PC-1 expression in muscle negatively correlates with insulin sensitivity in intravenous insulin tolerance test and in vitro stimulation of muscle insulin receptor tyrosine kinase activity (96, 97). It has been reported that PC-1 overexpression in skeletal muscle of obese subjects explains downregulation of insulin receptor tyrosine phosphorylation better than it does the decrease in insulin receptor expression, but this requires further investigation (98). Whether genetic factors regulate the expression level of PC-1 is not known.
Rad.
Rad (Ras associated with diabetes) was originally cloned as a message overexpressed in the skeletal muscle of type 2 diabetic patients (99). Rad belongs to a unique branch of the Ras superfamily of GTPases and in vitro has a GTP-hydrolyzing activity (99). The Rad gene, designated RAD1, has been found to contain certain trinucleotide repeat polymorphisms. Based on the number of trinucleotide repeats found in RAD1, 10 alleles can be divided into four subclasses, I–IV. The minor classes (I, II, and IV) of RAD1 are associated with type 2 diabetes in the Caucasian population (100). Some individuals with type 2 diabetes have been identified with a high expression level of Rad. In cultured myotubes and adipocytes, overexpression of Rad decreases insulin-dependent glucose uptake (101). Rad is also an insulin-regulated gene (102).
Acquired factors
Obese human subjects have decreased insulin receptor expression level and tyrosine kinase activity in skeletal muscle (103) and adipocytes (104). Similar findings have been reported in type 2 diabetic patients in skeletal muscle (103) and the liver (105).
Insulin receptor expression is regulated by rates of synthesis, internalization, and degradation, whereas its tyrosine kinase activity is, in addition, regulated by posttranslational modifications of the receptor, especially serine/threonine and tyrosine phosphorylation. Both insulin receptor expression and tyrosine kinase activities are restored by weight loss, which also improves insulin sensitivity. In type 2 diabetes, however, the restoration of insulin sensitivity is not complete, suggesting the existence of an additional postreceptor defect of insulin signaling (106). In animal models of both genetic and acquired obesity, insulin receptor number in the liver is decreased and can be corrected by ameliorating hyperinsulinemia (107). These data suggest that downregulation of insulin receptor expression and tyrosine kinase activity is secondary to obesity, or more likely, hyperinsulinemia, which accompanies it. In addition to decreased insulin receptor expression and tyrosine kinase activity, however, several additional mechanisms may contribute to the insulin resistance associated with obesity, including changes in membrane lipids secondary to hyperlipidemia (108).
Less is known about the exact sites of postreceptor resistance in obesity and diabetes. In severely obese patients (body mass index of 52 kg/m2), IRS-1 expression level in skeletal muscle is reduced to 54% of that in nonobese patients (109). In the less-obese type 2 diabetic patients, IRS-1 expression appears to be reduced in adipocytes (110) but unaltered in skeletal muscle (111, 112). IRS-2 expression, on the other hand, is not altered in adipocytes, where it becomes the main docking protein for PI3-kinase (110). Despite these variable data concerning IRS protein expression, the uniform finding is that IRS-1–associated tyrosine phosphorylation and PI3-kinase activity is decreased in skeletal muscle and adipocytes both in obesity and type 2 diabetes (109–112). In both genetic (113–116) and induced (117, 118) rodent models of obesity, insulin-stimulated phosphorylation of the insulin receptor and IRS-1 is decreased in muscle.
Additional alterations in the insulin signaling cascade found in hyperinsulinemic models of obesity include alternative splicing of the PI3-kinase regulatory subunits in the liver (114, 115). Downregulation in the p85α and a twofold increase in the p50α expression are found in both leptin-deficient ob/ob mice (115) and in Zucker fatty rats (114). AS53 in the liver of ob/ob mice is dramatically upregulated, whereas in Zucker fatty rats, it is downregulated by approximately 50%. This might affect the routing or compartmentalization of the insulin signal in these models. Whether changes in alternative splicing of PI3-kinase regulatory subunits also occur in human obesity is not known.
Hyperinsulinemia.
Hyperinsulinemia is the classic indicator of insulin resistance and may itself contribute to the insulin resistance in type 2 diabetes and obesity. Amelioration of hyperinsulinemia in animal models by streptozotocin corrects insulin receptor expression levels (107). Moreover, insulin receptor levels are normal or only mildly impaired in type 1 diabetes (119, 120) and are generally increased in animal models of hypoinsulinemic diabetes (120). These data suggest that downregulation of the insulin receptor occurs as a result of increased internalization and degradation after insulin binds to its receptor, thus leading to secondary insulin resistance (106).
Counterregulatory hormones and adrenergic system.
Counterregulatory hormones (epinephrine, norepinephrine, cortisol, glucagon, and growth hormone) play a significant role in antagonizing insulin action after hypoglycemia (121). It is not clear whether increased sympathetic nervous system activity, commonly found in insulin resistance syndrome (122), contributes to decreased insulin signaling. However, in brown adipocytes (Klein, J., and Kahn, C.R., unpublished data) and white adipocytes (123), stimulation of the β-adrenergic receptor decreases insulin-stimulated PI3-kinase activity. Desensitization of β-adrenergic receptors by isoproterenol increases insulin-stimulated glucose uptake in white adipocytes (124). A naturally occurring mutation of the β3-adrenergic receptor (W64R) has been associated with increased abdominal obesity and early-onset type 2 diabetes (125), although this remains controversial. In isolated human omental adipocytes, the W64R variant shows decreased β agonist–induced lipolysis (126), providing a hypothesis as to why omental adipocity may be increased in patients carrying this variant.
Tumor necrosis factor-α (TNF–α).
TNF-α was first identified as an endogenous cytokine produced by macrophages and lymphocytes after inflammatory stimulation. TNF-α is expressed in many types of cells, including adipose tissue (127, 128). Adipocytes of obese animals and humans overexpress TNF-α in positive correlation to body mass index and hyperinsulinemia, and weight reduction decreases TNF-α expression (127–130). Although this local release of TNF-α has little effect on systemic TNF-α concentrations, local concentrations of free and membrane-bound TNF-α are likely to be increased in obesity. TNF-α appears to impair insulin signaling by increasing serine phosphorylation of IRS-1 (and possibly other IRS proteins) (127, 128, 131). Serine-phosphorylated IRS-1 inhibits insulin receptor tyrosine kinase activity, which leads to impaired downstream signaling (128). It has been hypothesized that TNF-α–induced serine phosphorylation of IRS-1 causes an additional insulin receptor inhibitory factor (possibly a tyrosine phosphatase or an inhibitor of serine phosphatases) to bind to IRS-1 and mediate the inhibition of the insulin receptor kinase (128). Complete lack of TNF-α signaling in mice with a targeted mutation of both TNF-α receptor isoforms, p55 and p75, results in improved insulin sensitivity (132). The p55 receptor isoform appears to have a stronger impact.
Leptin.
Leptin is a 16-kDa protein secreted from adipose tissue. Leptin is the product of the defective obesity gene identified by positional cloning in the obese, hyperinsulinemic ob/ob mouse (133). Circulating leptin concentrations in humans correlate closely with fasting insulin concentrations and the percentage of body fat, making leptin a marker of obesity and the insulin resistance syndrome.
The leptin receptor is a member of the cytokine family of receptors and occurs in five isoforms (OB-RA,B,C,D,and E). Only OB-RB, also known as the long form of the leptin receptor (OB-RL), has been shown to possess significant signaling capacity (134). The long form receptor is selectively expressed in the arcuate and ventromedial nuclei of the hypothalamus, known to regulate feeding behavior. However, low levels of OB-RL are also detectable in many peripheral tissues, such as the liver, gastrointestinal tract, and pancreatic β cell. Given that leptin reduces food intake and increases energy expenditure, its possible peripheral effects on insulin action are of particular interest.
Leptin infusion acutely increases glucose infusion rate significantly during a euglycemic, hyperinsulinemic clamp in rats (135). Intracerebroventricular injection of leptin increases muscle glucose uptake without increasing systemic leptin concentrations; denervation abolishes this effect (136, 137). Interestingly, leptin decreases insulin secretion from the β cells, possibly by a direct mechanism (138). Whether leptin regulates insulin signaling, directly or indirectly, remains an unanswered question.
Glucose and other nutrients.
Hyperglycemia itself impairs tissue insulin sensitivity, as well as insulin secretion from the pancreatic β cells, a phenomenon commonly known as glucose toxicity (139). In type 1 diabetic patients, 24 hours of hyperglycemia decreases insulin sensitivity 26–35% in a subsequent euglycemic, hyperinsulinemic clamp (140). In type 1 diabetic patients (141) and partially pancreatectomized diabetic rats (142), correction of hyperglycemia normalizes insulin sensitivity. There are currently two major theories explaining hyperglycemia-induced insulin resistance: the hexosamine pathway and the activation of protein kinase C.
Following its uptake, 2–4% of glucose is shunted to the hexosamine pathway by the enzyme glutamine:fructose-1,6-diphosphate amidotransferase (GFA) (143). Infusion of glucosamine into rats bypasses the GFA reaction and induces insulin resistance but does not further impair insulin resistance in partially pancreatectomized rats (144, 145). This suggests that glucosamine and hyperglycemia share a common mechanism leading to insulin resistance (144). The increased flux through the hexosamine pathway increases tissue concentration of a hexosamine metabolite, UDP-GlcNAc, which correlates closely with the observed induction of insulin resistance (146). This may lead to O-linked glycosylation of proteins on serine and threonine residues, and thus compete with serine and threonine phosphorylation of these sites (143). Several nuclear transcription factors, of which Sp1 is the best characterized, are among the targets of this glycosylation (147). This provides a mechanism by which hyperglycemia could interfere with insulin and other signal transduction pathways that are regulated by serine and threonine phosphorylation. Activation of the hexosamine pathway may also occur by free fatty acids, uridine, or overexpression of GFA, and result in insulin resistance (148, 149). The ability of a variety of nutrients to activate the hexosamine pathway has led to the theory that this pathway serves as a general nutrient sensing pathway, through which hyperglycemia or hyperlipidemia could decrease insulin sensitivity of cells when nutrient excess prevails (148). In cell culture, omission of glutamine (a cofactor of GFA) from the media, or addition of glutamine analogues, blunts the desensitizing effect of glucose on insulin sensitivity (150). Glucosamine infusion for two to six hours will decrease insulin-stimulated IRS-1 tyrosine phosphorylation, PI3-kinase activation, and activation of glycogen synthase in a manner that parallels the decrease in insulin-stimulated glucose uptake in skeletal muscle. This effect can be seen both in acute and chronic stimulation with insulin (151) (Patti, M.E., personal communication).
Protein kinase C (PKC) is a serine kinase that has a number of potential substrates, including the insulin receptor (152). PKC is activated by the intracellular metabolite diacylglycerol (DAG), the concentration of which increases in a glucose-dependent manner during exposure of isolated muscles to hyperinsulinemia (153). In NIH3T3 cells overexpressing the insulin receptor, insulin desensitization by glucose can be blocked by PKC inhibitors and thiazolidinediones (154). PKC activation by DAG can lead to serine phosphorylation of the insulin receptor, a mechanism similar to the effect of TNF-α (155), although the resulting insulin resistance can be blocked differentially by PKC inhibitors, which do not block TNF-α–induced insulin resistance, or by PTPase inhibitors, which do not block PKC-induced insulin resistance (156). In vivo data showing that inhibition of PKC reduces hyperglycemia-induced insulin resistance is still, however, lacking. It is likely that the activation of PKC is important in the development of diabetic microvascular complications (157), and thus, PKC inhibitors are now under intense investigation as potential therapy for diabetic microvascular complications.
Phosphotyrosine phosphatases (PTPases).
PTPases are responsible for dephosphorylation of the insulin receptor and its substrates, and hence, turning off the insulin signal. To date, no insulin receptor–specific phosphatase has been identified. Total membrane-bound tyrosine phosphatase activity is increased in skeletal muscle of type 2 diabetic patients (158). Immunodepletion experiments in muscles from these diabetic patients and obese individuals suggest that especially two phosphatases, protein-tyrosine phosphatase 1B (PTP-1B) and leukocyte antigen–related (LAR) phosphatase, are mainly responsible for this increase (159). The insulin receptor and IRS-1 are dephosphorylated by both of these phosphatases, and therefore, they are candidate targets for therapeutic interventions to increase insulin sensitivity (160).
Lessons from knockout animal models
Evaluating how insulin sensitivity affects whole body glucohomeostasis has been a major challenge for diabetes research. One approach has been to use targeted disruption of several insulin signaling proteins, such as the insulin receptor, IRS-1, and IRS-2. Targeted disruption of the insulin receptor is lethal after a few days of birth in homozygous animals, whereas heterozygous animals have almost no phenotype (161, 162). Disruption of IRS-1 results in retarded growth (due to IGF-1 resistance), but only mild insulin resistance and impaired glucose tolerance without diabetes (163, 164). Disruption of IRS-2 also leads to insulin resistance, but in this case, there is also a reduction in β-cell mass, leading to diabetes (165). Combination of the heterozygous insulin receptor knockout with the heterozygous IRS-1 knockout leads to more severe insulin resistance and a phenotype that includes a delayed onset of diabetes similar to human type 2 diabetes (166). This is a pure form of insulin resistance with elevated insulin levels. Interestingly, only about 40% of these mice develop diabetes, suggesting the importance of additional background genes.
Tissue-specific disruption of the insulin receptor gives a more detailed view of how glucose homeostasis is regulated in a tissue-specific manner in vivo. Muscle-specific disruption of the insulin receptor (MIRKO) in mice results in severe insulin resistance in isolated skeletal muscles, but at the whole body level, glucose tolerance is near normal (74). Indeed, the major metabolic disturbances found in the MIRKO mouse are increased body fat, elevated triglycerides, and slightly elevated free fatty acid levels. β cell–specific disruption of the insulin gene (βIRKO) has a more severe phenotype than the MIRKO, with severely impaired glucose tolerance and a loss of first-phase insulin secretion in the glucose tolerance test (167). These animal models demonstrate that insulin serves an important role in β-cell function and suggest that insulin resistance at the β-cell level may contribute to the altered insulin secretion in type 2 diabetes. Additional data from these and other models should help us to clarify how glucose homeostasis is regulated and define some defects in signaling proteins responsible for insulin resistance in type 2 diabetes.
Implications
It should be clear from this review that although the insulin signaling network is complex, modern cell biology and biochemistry are starting to turn this basic knowledge of the insulin signal transduction pathways into an understanding of how these pathways can be regulated in human disease. The challenge for basic research is to characterize the specific events that translate insulin binding to the diverse metabolic effects, and to reveal the nature of insulin resistance in the pathophysiology in various disease states.
Protein modification and protein–protein interactions provide a number of mechanisms by which insulin signal transduction can be impaired in type 2 diabetes. Regardless of the underlying mechanism, the resulting insulin resistance has diverse consequences. The main defects in type 2 diabetes are peripheral insulin resistance and insufficient compensation of pancreatic β cells. In the face of increased glucose output from the liver and decreased peripheral glucose utilization, the insufficient insulin secretion from the β cells results in glucose intolerance and frank diabetes. The question has been, which of the two defects — peripheral insulin resistance or β-cell insulin secretion — is the primary defect in type 2 diabetes (168)? The recent findings in mice with β cell–specific disruption of the insulin receptor (βIRKO mice) suggests that impaired insulin secretion might be a result of insulin resistance in the β cells themselves (167). The loss of first-phase insulin secretion after glucose challenge seen in these mice resembles that seen in human type 2 diabetes (167). These data suggest that signals mediated by the insulin receptor are essential for the release of insulin secretory vesicles. Indeed, a combination of insulin resistance in muscle, liver, adipose tissue, and β cells may create the phenotype of type 2 diabetes.
What is the cause of insulin resistance in diabetes? The inheritable nature of the disease points out that genetic factors must exist. A vast number of candidate genes for glucose and lipid metabolism, as well as signaling proteins, have been tested, but no single major susceptibility gene for classical type 2 diabetes has been thus far identified. It is likely that type 2 diabetes consists of several subtypes of the disease, where a combination of different mechanisms impairs insulin sensitivity.
Table 3 summarizes molecular mechanisms that may play a role in some insulin-resistant states in humans. Most of these mechanisms are associated with insulin resistance in type 2 diabetes and obesity, and many of them are induced by environmental factors. Nevertheless, genetic defects of various steps of insulin signaling, even if relatively minor, could impair glucose homeostasis significantly when a environmental factors coexist. It is important not to underestimate the potential role of sequence polymorphisms in the signaling proteins associated with type 2 diabetes. Even if a single polymorphism can explain only a small fraction of the total insulin resistance, a combination of polymorphisms may account for the multifactorial nature of this disease. Therefore, an assortment of mild genetic defects that merely modify the insulin signaling cascade may be a more likely scenario for the inheritable defect and the coexisting precipitating factors, such as obesity, precipitate the phenotype of impaired glucose tolerance and diabetes. As the basic mechanisms of insulin signaling unfold, we will have increasing possibilities to specifically evaluate, and eventually modulate, these abnormalities.
Table 3.
Molecular mechanisms of insulin resistance and their relationship to insulin-resistant states in humans
Acknowledgments
This work was supported by National institutes of Health grants DK-31036, DK-33201, and DK-45935. A. Virkamäki is the recipient of the Sigrid Juselius Fellowship and the Albert Renold Fellowship from the European Association for the Study of Diabetes.
References
- 1.White MF. The IRS-signalling system: a network of docking proteins that mediate insulin action. Mol Cell Biochem. 1998;182:3–11. [PubMed] [Google Scholar]
- 2.Sudol M. From SRC homology domains to other signaling modules: proposal of the ‘protein recognition code’. Oncogene. 1998;17:1469–1474. doi: 10.1038/sj.onc.1202182. [DOI] [PubMed] [Google Scholar]
- 3.Yenush L, et al. The pleckstrin homology domain is the principle link between the insulin receptor and IRS-1. J Biol Chem. 1996;271:24300–24306. doi: 10.1074/jbc.271.39.24300. [DOI] [PubMed] [Google Scholar]
- 4.Wolf G, et al. The PTB domains of IRS-1 and Shc have distinct but overlapping specificities. J Biol Chem. 1995;270:27407–27410. doi: 10.1074/jbc.270.46.27407. [DOI] [PubMed] [Google Scholar]
- 5.Eck MJ, Dhe-Paganon S, Trub T, Nolte RT, Shoelson SE. Structure of the IRS-1 PTB domain bound to the juxtamembrane region of the insulin receptor. Cell. 1996;85:695–705. doi: 10.1016/s0092-8674(00)81236-2. [DOI] [PubMed] [Google Scholar]
- 6.Pawson T, Olivier P, Rozakis-Adcock M, McGlade J, Henkemeyer M. Proteins with SH2 and SH3 domains couple receptor tyrosine kinases to intracellular signalling pathways. Philos Trans R Soc Lond B Biol Sci. 1993;340:279–285. doi: 10.1098/rstb.1993.0069. [DOI] [PubMed] [Google Scholar]
- 7.Ebina Y, et al. The human insulin receptor cDNA: the structural basis for hormone activated transmembrane signalling. Cell. 1985;40:747–758. doi: 10.1016/0092-8674(85)90334-4. [DOI] [PubMed] [Google Scholar]
- 8.Ullrich A, et al. Human insulin receptor and its relationship to the tyrosine kinase family of oncogenes. Nature. 1985;313:756–761. doi: 10.1038/313756a0. [DOI] [PubMed] [Google Scholar]
- 9.Kasuga M, Fujita-Yamaguchi Y, Blithe DL, Kahn CR. Tyrosine-specific protein kinase activity is associated with the purified insulin receptor. Proc Natl Acad Sci USA. 1983;80:2137–2141. doi: 10.1073/pnas.80.8.2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White MF, et al. Mutation of the insulin receptor at tyrosine 960 inhibits signal transmission but does not affect its tyrosine kinase activity. Cell. 1988;54:641–649. doi: 10.1016/s0092-8674(88)80008-4. [DOI] [PubMed] [Google Scholar]
- 11.Backer JM, Kahn CR, Cahill DA, Ullrich A, White MF. Receptor-mediated internalization of insulin requires a 12-amino acid sequence in the juxtamembrane region of the insulin receptor β-subunit. J Biol Chem. 1990;265:16450–16454. [PubMed] [Google Scholar]
- 12.Chen WJ, Goldstein JL, Brown MS. NPXY, a sequence often found in cytoplasmic tails, is required for coated pit-mediated internalization of the low density lipoprotein receptor. J Biol Chem. 1990;265:3116–3123. [PubMed] [Google Scholar]
- 13.Bansal A, Gierasch LM. The NPXY internalization signal of the LDL receptor adopts a reverse-turn conformation. Cell. 1991;67:1195–1201. doi: 10.1016/0092-8674(91)90295-a. [DOI] [PubMed] [Google Scholar]
- 14.Collawn JF, et al. Transferrin receptor internalization sequence YXRF implicates a tight turn as the structural recognition motif for endocytosis. Cell. 1990;63:1061–1072. doi: 10.1016/0092-8674(90)90509-d. [DOI] [PubMed] [Google Scholar]
- 15.Frattali AL, Treadway JL, Pessin JE. Insulin/IGF-1 hybrid receptors: implications for the dominant- negative phenotype in syndromes of insulin resistance. J Cell Biochem. 1992;48:43–50. doi: 10.1002/jcb.240480108. [DOI] [PubMed] [Google Scholar]
- 16.Van Horn DJ, Myers MG, Jr, Backer JM. Direct activation of the phosphatidylinositol 3′-kinase by the insulin receptor. J Biochem. 1994;269:29–32. [PubMed] [Google Scholar]
- 17.Sun XJ, et al. The expression and function of IRS-1 in insulin signal transmission. J Biol Chem. 1992;267:22662–22672. [PubMed] [Google Scholar]
- 18.Rothenberg PL, et al. Purification and partial sequence analysis of pp185, the major cellular substrate of the insulin receptor tyrosine kinase. J Biol Chem. 1991;266:8302–8311. [PubMed] [Google Scholar]
- 19.Sun XJ, et al. Role of IRS-2 in insulin and cytokine signalling. Nature. 1995;377:173–177. doi: 10.1038/377173a0. [DOI] [PubMed] [Google Scholar]
- 20.Lavan BE, Lane WS, Lienhard GE. The 60-kDa phosphotyrosine protein in insulin-treated adipocytes is a new member of the insulin receptor substrate family. J Biol Chem. 1997;272:11439–11443. doi: 10.1074/jbc.272.17.11439. [DOI] [PubMed] [Google Scholar]
- 21.Lavan BE, et al. A novel 160 kDa phosphotyrosine protein in insulin-treated embryonic kidney cells is a new member of the insulin receptor substrate family. J Biol Chem. 1997;272:21403–21407. doi: 10.1074/jbc.272.34.21403. [DOI] [PubMed] [Google Scholar]
- 22.Holgado-Madruga M, Emlet DR, Moscatello DK, Godwin AK, Wong AJ. A Grb2-associated docking protein in EGF- and insulin-receptor signalling. Nature. 1996;379:560–563. doi: 10.1038/379560a0. [DOI] [PubMed] [Google Scholar]
- 23.Pelicci G, et al. A novel transforming protein (SHC) with an SH2 domain is implicated in mitogenic signal transduction. Cell. 1992;70:93–104. doi: 10.1016/0092-8674(92)90536-l. [DOI] [PubMed] [Google Scholar]
- 24.Carpino N, et al. p62dok: a constitutively tyrosine-phosphorylated, GAP-associated protein in chronic myelogenous leukemia progenitor cells. Cell. 1997;88:197–204. doi: 10.1016/s0092-8674(00)81840-1. [DOI] [PubMed] [Google Scholar]
- 25.Liu F, Roth RA. Grb-IR: a SH2 domain-containing protein that binds to the insulin receptor and inhibits its function. Proc Natl Acad Sci USA. 1995;92:10287–10291. doi: 10.1073/pnas.92.22.10287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Otsu M, et al. Characterization of two 85 kD proteins that associate with receptor tyrosine kinases, middle-T/pp60c-src complexes and PI3-kinase. Cell. 1991;65:91–104. doi: 10.1016/0092-8674(91)90411-q. [DOI] [PubMed] [Google Scholar]
- 27.Antonetti DA, Algenstaedt P, Kahn CR. Insulin receptor substrate 1 binds two novel splice variants of the regulatory subunit of phosphatidylinositol 3-kinase in muscle and brain. Mol Cell Biol. 1996;16:2195–2203. doi: 10.1128/mcb.16.5.2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Inukai K, et al. p85α gene generates three isoforms of regulatory subunit for phosphatidylinositol 3-kinase (PI 3-kinase), p50α, p55α, and p85α, with different PI 3-kinase activity elevating responses to insulin. J Biol Chem. 1997;272:7873–7882. doi: 10.1074/jbc.272.12.7873. [DOI] [PubMed] [Google Scholar]
- 29.Pons S, et al. The structure and function of p55PIK reveals a new regulatory subunit for the phosphatidylinositol-3 kinase. Mol Cell Biol. 1995;15:4453–4465. doi: 10.1128/mcb.15.8.4453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hara K, et al. 1-Phosphatidylinositol 3-kinase activity is required for insulin-stimulated glucose transport but not for ras activation in CHO cells. Proc Natl Acad Sci USA. 1994;91:7415–7419. doi: 10.1073/pnas.91.16.7415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okada T, Kawano Y, Sakakibara T, Hazeki O, Ui M. Essential role of phosphatidylinositol 3-kinase in insulin-induced glucose transport and antilipolysis in rat adipocytes: studies with a selective inhibitor wortmannin. J Biol Chem. 1994;269:3568–3573. [PubMed] [Google Scholar]
- 32.Alessi DR, Downes CP. The role of PI 3-kinase in insulin action. Biochim Biophys Acta. 1998;1436:151–164. doi: 10.1016/s0005-2760(98)00133-7. [DOI] [PubMed] [Google Scholar]
- 33.Inoue G, Cheatham B, Emkey R, Kahn CR. Dynamics of insulin signaling in 3T3-L1 adipocytes: differential compartmentalization and trafficking of insulin receptor substrate (IRS)-1 and IRS-2. J Biol Chem. 1998;273:11548–11555. doi: 10.1074/jbc.273.19.11548. [DOI] [PubMed] [Google Scholar]
- 34.Clark SF, Martin S, Carozzi AJ, Hill MM, James DE. Intracellular localization of phosphatidylinositol 3-kinase and insulin receptor substrate-1 in adipocytes: potential involvement of a membrane skeleton. J Cell Biol. 1998;140:1211–1225. doi: 10.1083/jcb.140.5.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lowenstein EJ, et al. The SH2 and SH3 domain-containing proteins GRB2 links receptor tyrosine kinases to ras signaling. Cell. 1992;70:431–442. doi: 10.1016/0092-8674(92)90167-b. [DOI] [PubMed] [Google Scholar]
- 36.Furman WL, et al. Antibodies to distal carboxyl terminal epitopes in the v-fms-coded glycoprotein do not cross-react with the c-fms gene product. Virology. 1986;152:432–445. doi: 10.1016/0042-6822(86)90145-5. [DOI] [PubMed] [Google Scholar]
- 37.Skolnik EY, et al. The function of GRB2 in linking the insulin receptor to ras signaling pathways. Science. 1993;260:1953–1955. doi: 10.1126/science.8316835. [DOI] [PubMed] [Google Scholar]
- 38.Myers MG, Jr, et al. The role of IRS-1/GRB2 complexes in insulin signaling. Mol Cell Biol. 1994;14:3577–3587. doi: 10.1128/mcb.14.6.3577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tanaka S, et al. C3G, a guanine nucleotide-releasing protein expressed ubiquitously, binds to the Src homology 3 domains of CRK and GRB2/ASH proteins. Proc Natl Acad Sci USA. 1994;91:3443–3447. doi: 10.1073/pnas.91.8.3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tanaka S, Ouchi T, Hanafusa H. Downstream of Crk adaptor signaling pathway: activation of Jun kinase by v-Crk through the guanine nucleotide exchange protein C3G. Proc Natl Acad Sci USA. 1997;94:2356–2361. doi: 10.1073/pnas.94.6.2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mayer BJ, Hamaguchi M, Hanafusa H. A novel viral oncogene with structural similarity to phospholipase C. Nature. 1988;332:272–275. doi: 10.1038/332272a0. [DOI] [PubMed] [Google Scholar]
- 42.Sakai R, et al. A novel signaling molecule, p130, forms stable complexes in vivo with v-Crk and v-Src in a tyrosine phosphorylation-dependent manner. EMBO J. 1994;13:3748–3756. doi: 10.1002/j.1460-2075.1994.tb06684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matsuda M, et al. Interaction between the amino-terminal SH3 domain of CRK and its natural target proteins. J Biol Chem. 1996;271:14468–14472. doi: 10.1074/jbc.271.24.14468. [DOI] [PubMed] [Google Scholar]
- 44.Beitner-Johnson D, et al. The proto-oncogene product c-Crk associates with insulin receptor substrate-1 and 4PS. J Biol Chem. 1996;271:9287–9290. doi: 10.1074/jbc.271.16.9287. [DOI] [PubMed] [Google Scholar]
- 45.Lee CH, et al. Nck associates with the SH2 domain docking proteins IRS-1 in insulin stimulated cells. Proc Natl Acad Sci USA. 1993;90:11713–11717. doi: 10.1073/pnas.90.24.11713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hu Q, Milfay D, Williams LT. Binding of NCK to SOS and activation of ras-dependent gene expression. Mol Cell Biol. 1995;15:1169–1174. doi: 10.1128/mcb.15.3.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Quilliam LA, et al. Isolation of a NCK-associated kinase, PRK2, an SH3-binding protein and potential effector of Rho protein signaling. J Biol Chem. 1996;271:28772–28776. doi: 10.1074/jbc.271.46.28772. [DOI] [PubMed] [Google Scholar]
- 48.Bokoch GM, et al. Interaction of the Nck adapter protein with p21-activated kinase (PAK1) J Biol Chem. 1996;271:25746–25749. doi: 10.1074/jbc.271.42.25746. [DOI] [PubMed] [Google Scholar]
- 49.Sun XJ, et al. The fyn tyrosine kinase binds IRS-1 and forms a distinct signaling complex during insulin stimulation. J Biol Chem. 1996;271:10583–10587. doi: 10.1074/jbc.271.18.10583. [DOI] [PubMed] [Google Scholar]
- 50.Mastick CC, Saltiel AR. Insulin-stimulated tyrosine phosphorylation of caveolin is specific for the differentiated adipocyte phenotype in 3T3-L1 cells. J Biol Chem. 1997;272:20706–20714. doi: 10.1074/jbc.272.33.20706. [DOI] [PubMed] [Google Scholar]
- 51.Liu YC, Altman A. Cbl: complex formation and functional implications. Cell Signal. 1998;10:377–385. doi: 10.1016/s0898-6568(97)00179-4. [DOI] [PubMed] [Google Scholar]
- 52.Wary KK, Mariotti A, Zurzolo C, Giancotti FG. A requirement for caveolin-1 and associated kinase Fyn in integrin signaling and anchorage-dependent cell growth. Cell. 1998;94:625–634. doi: 10.1016/s0092-8674(00)81604-9. [DOI] [PubMed] [Google Scholar]
- 53.Ribon V, Printen JA, Hoffman NG, Kay BK, Saltiel AR. A novel, multifunctional c-Cbl binding protein in insulin receptor signaling in 3T3-L1 adipocytes. Mol Cell Biol. 1998;18:872–879. doi: 10.1128/mcb.18.2.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ribon V, Johnson JH, Camp HS, Saltiel AR. Thiazolidinediones and insulin resistance: peroxisome proliferator activated receptor gamma activation stimulates expression of the CAP gene. Proc Natl Acad Sci USA. 1998;95:14751–14756. doi: 10.1073/pnas.95.25.14751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu X, Pawson T. Biochemistry of the Src protein-tyrosine kinase: regulation by SH2 and SH3 domains. Recent Prog Horm Res. 1994;49:149–160. doi: 10.1016/b978-0-12-571149-4.50011-8. [DOI] [PubMed] [Google Scholar]
- 56.Tobe K, et al. Csk enhances insulin-stimulated dephosphorylation of focal adhesion proteins. Mol Cell Biol. 1996;16:4765–4772. doi: 10.1128/mcb.16.9.4765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Baron V, Calleja V, Ferrari P, Alengrin F, Van Obberghen E. p125Fak focal adhesion kinase is a substrate for the insulin and insulin-like growth factor-1 tyrosine kinase receptors. J Biol Chem. 1998;273:7162–7168. doi: 10.1074/jbc.273.12.7162. [DOI] [PubMed] [Google Scholar]
- 58.Cohen P, Alessi DR, Cross DA. PDK1, one of the missing links in insulin signal transduction? Growth Regul. 1997;410:3–10. doi: 10.1016/s0014-5793(97)00490-0. [DOI] [PubMed] [Google Scholar]
- 59.Coffer PJ, Jin J, Woodgett JR. Protein kinase B (c-Akt): a multifunctional mediator of phosphatidylinositol 3-kinase activation. Biochem J. 1998;335:1–13. doi: 10.1042/bj3350001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Erneux C, Govaerts C, Communi D, Pesesse X. The diversity and possible functions of the inositol polyphosphate 5-phosphatases. Biochim Biophys Acta. 1998;1436:185–199. doi: 10.1016/s0005-2760(98)00132-5. [DOI] [PubMed] [Google Scholar]
- 61.Vollenweider P, et al. An SH2 domain-containing 5′ inositol phosphatase inhibits insulin-induced GLUT4 translocation and growth factor-induced actin filament. Mol Cell Biol. 1999;19:1081–1091. doi: 10.1128/mcb.19.2.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Verdier F, et al. Erythropoietin induces the tyrosine phosphorylation of insulin receptor substrate-2. An alternate pathway for erythropoietin-induced phosphatidylinositol 3-kinase activation. J Biol Chem. 1997;272:26173–26178. doi: 10.1074/jbc.272.42.26173. [DOI] [PubMed] [Google Scholar]
- 63.Gale NW, Kaplan S, Lowenstein EJ, Schlessinger J, Bar-Sagi D. Grb2 mediates the EGF-dependent activation of guanine nucleotide exchange on Ras. Nature. 1993;363:88–92. doi: 10.1038/363088a0. [DOI] [PubMed] [Google Scholar]
- 64.Xiao S, et al. Syp (SH-PTP2) is a positive mediator of growth factor-stimulated mitogenic signal transduction. J Biol Chem. 1994;269:21244–21248. [PubMed] [Google Scholar]
- 65.Noguchi T, Matozaki T, Horita K, Fujioka Y, Kasuga M. Role of SH-PTP2, a protein-tyrosine phosphatase with Src homology 2 domains, in insulin-stimulated ras activation. Mol Cell Biol. 1994;14:6674–6682. doi: 10.1128/mcb.14.10.6674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Burbelo PD, Hall A. 14-3-3 proteins. Hot numbers in signal transduction. Curr Biol. 1995;5:95–96. doi: 10.1016/s0960-9822(95)00022-4. [DOI] [PubMed] [Google Scholar]
- 67.Yaffe MB, et al. The structural basis for 14-3-3 phosphopeptide binding specificity. Cell. 1997;91:961–971. doi: 10.1016/s0092-8674(00)80487-0. [DOI] [PubMed] [Google Scholar]
- 68.Noguchi T, et al. Characterization of a 115-kDa protein that binds to SH-PTP2, a protein tyrosine phosphatase with Src homology 2 domains, in Chinese hamster ovary cells. J Biol Chem. 1996;271:27652–27658. doi: 10.1074/jbc.271.44.27652. [DOI] [PubMed] [Google Scholar]
- 69.Ogihara T, et al. 14-3-3 protein binds to insulin receptor substrate-1, one of the binding sites of which is in the phosphotyrosine binding domain. J Biol Chem. 1997;272:25267–25274. doi: 10.1074/jbc.272.40.25267. [DOI] [PubMed] [Google Scholar]
- 70.Pipas JM. Common and unique features of T antigens encoded by the polyomavirus group. J Virol. 1992;66:3979–3985. doi: 10.1128/jvi.66.7.3979-3985.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhou-Li, F., Xu, S.Q., Dews, M., and Baserga, R. 1997. Co-operation of simian virus 40 T antigen and insulin receptor substrate-1 in protection from apoptosis induced by interleukin-3 withdrawal. Oncogene. 961–970. [DOI] [PubMed]
- 72.Vuori K, Ruoslahti E. Association of insulin receptor substrate-1 with integrins. Science. 1994;266:1576–1578. doi: 10.1126/science.7527156. [DOI] [PubMed] [Google Scholar]
- 73.Zheng B, Clemmons DR. Blocking ligand occupancy of the alphaVbeta3 integrin inhibits insulin-like growth factor I signaling in vascular smooth muscle cells. Proc Natl Acad Sci USA. 1998;95:11217–11222. doi: 10.1073/pnas.95.19.11217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bruning JC, et al. A muscle specific insulin receptor knockout challenges the current concepts of glucose disposal and NIDDM pathogenesis. Mol Cell. 1998;2:559–569. doi: 10.1016/s1097-2765(00)80155-0. [DOI] [PubMed] [Google Scholar]
- 75.Algenstaedt P, Antonetti DA, Yaffe MB, Kahn CR. Insulin receptor substrate proteins create a link between the tyrosine phosphorylation cascade and the Ca2+-ATPases in muscle and heart. J Biol Chem. 1997;272:23696–23702. doi: 10.1074/jbc.272.38.23696. [DOI] [PubMed] [Google Scholar]
- 76.Zhou YP, et al. Apoptosis in insulin-secreting cells. Evidence for the role of intracellular Ca2+ stores and arachidonic acid metabolism. J Clin Invest. 1998;101:1623–1632. doi: 10.1172/JCI1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kadowaki T, et al. Two mutant alleles of the insulin receptor gene in a patient with extreme insulin resistance. Science. 1988;240:787–790. doi: 10.1126/science.2834824. [DOI] [PubMed] [Google Scholar]
- 78.Yoshimasa Y, et al. Insulin-resistant diabetes due to a point mutation that prevents insulin proreceptor processing. Science. 1988;240:784–787. doi: 10.1126/science.3283938. [DOI] [PubMed] [Google Scholar]
- 79.Krook A, O’Rahilly S. Mutant insulin receptors in syndromes of insulin resistance [review] Bailliers Clin Enodrinol Metab. 1996;10:97–122. doi: 10.1016/s0950-351x(96)80330-2. [DOI] [PubMed] [Google Scholar]
- 80.Almind K, et al. Amino acid polymorphisms of insulin receptor substrate-1 in non-insulin-dependent diabetes mellitus. Lancet. 1993;342:828–832. doi: 10.1016/0140-6736(93)92694-o. [DOI] [PubMed] [Google Scholar]
- 81.Laakso M, Malkki M, Kekalainen P, Kuusisto J, Deeb SS. Insulin receptor substrate-1 variants in non-insulin-dependent diabetes. J Clin Invest. 1994;94:1141–1146. doi: 10.1172/JCI117429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ura S, et al. Molecular scanning of the IRS-1 gene in Japanese patients with non-insulin-dependent diabetes mellitus: Identification of five novel mutations in IRS-1 gene. Diabetologia. 1996;39:600–608. doi: 10.1007/BF00403308. [DOI] [PubMed] [Google Scholar]
- 83.Hager J, Zouali H, Velho G, Froguel P. Insulin receptor substrate (IRS-1) gene polymorphism in French NIDDM families. Lancet. 1993;342:1430. doi: 10.1016/0140-6736(93)92793-s. [DOI] [PubMed] [Google Scholar]
- 84.Imai Y, et al. Variant sequences of insulin receptor substrate-1 in patients with noninsulin dependent diabetes mellitus. J Clin Endocrinol Metab. 1994;79:1655–1658. doi: 10.1210/jcem.79.6.7989470. [DOI] [PubMed] [Google Scholar]
- 85.Celi FS, et al. Lack of IRS-1 codon 513 and 972 polymorphism in Pima Indians. J Clin Endocrinol Metab. 1995;80:2827–2829. doi: 10.1210/jcem.80.9.7673431. [DOI] [PubMed] [Google Scholar]
- 86.Almind K, Inoue G, Pedersen O, Kahn CR. A common amino acid polymorphism in insulin receptor substrate-1 causes impaired insulin signaling. Evidence from transfection studies. J Clin Invest. 1996;97:2569–2575. doi: 10.1172/JCI118705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yoshimura R, et al. Impact of natural IRS-1 mutations of insulin signals: mutations of IRS-1 in the PTB domain and near SH2 protein binding sites result in impaired function at different steps of IRS-1 signaling. Diabetes. 1997;46:929–936. doi: 10.2337/diab.46.6.929. [DOI] [PubMed] [Google Scholar]
- 88.Kalidas K, et al. Mapping of the human insulin receptor substrate-2 gene, identification of a linked polymorphic marker and linkage analysis in families with Type 2 diabetes: no evidence for a major susceptibility role. Diabetologia. 1998;41:1389–1391. doi: 10.1007/s001250051081. [DOI] [PubMed] [Google Scholar]
- 89.Almind K, et al. Common amino acid substitutions in insulin receptor substrate-4 are not associated with Type II diabetes mellitus or insulin resistance. Diabetologia. 1998;41:969–974. doi: 10.1007/s001250051015. [DOI] [PubMed] [Google Scholar]
- 90.Hansen T, et al. Identification of a common amino acid polymorphism in the -85α regulatory subunit of phosphatidylinositol 3-kinase: effects on glucose disappearance constant, glucose effectiveness and the insulin sensitivity index. Diabetes. 1997;46:494–501. doi: 10.2337/diab.46.3.494. [DOI] [PubMed] [Google Scholar]
- 91.Spiegelman BM. PPARγ: adipogenic regulator and thiazolidinedione receptor. Diabetes. 1998;47:507–514. doi: 10.2337/diabetes.47.4.507. [DOI] [PubMed] [Google Scholar]
- 92.Ristow M, Muller-Wieland D, Pfeiffer A, Krone W, Kahn CR. Obesity associated with a mutation in a genetic regulator of adipocyte differentiation. N Engl J Med. 1998;339:953–959. doi: 10.1056/NEJM199810013391403. [DOI] [PubMed] [Google Scholar]
- 93.Deeb SS, et al. A Pro12Ala substitution in PPARγ2 associated with decreased receptor activity, lower body mass index and improved insulin sensitivity. Nat Genet. 1998;20:284–287. doi: 10.1038/3099. [DOI] [PubMed] [Google Scholar]
- 94.Maddux BA, et al. Membrane glycoprotein PC-1 in the insulin resistance of non-insulin dependent diabetes mellitus. Nature. 1995;373:448–451. doi: 10.1038/373448a0. [DOI] [PubMed] [Google Scholar]
- 95.Goldfine ID, et al. Membrane glycoprotein PC-1 and insulin resistance. Mol Cell Biochem. 1998;182:177–184. [PubMed] [Google Scholar]
- 96.Frittitta L, et al. Elevated PC-1 content in cultured skin fibroblasts correlates with decreased in vivo and in vitro insulin action in nondiabetic subjects: Evidence that PC-1 may be an intrinsic factor in impaired insulin receptor signaling. Diabetes. 1998;47:1095–1100. doi: 10.2337/diabetes.47.7.1095. [DOI] [PubMed] [Google Scholar]
- 97.Kumakura S, Maddux BA, Sung CK. Overexpression of membrane glycoprotein PC-1 can influence insulin action at a post-receptor site. J Cell Biochem. 1998;3:366–377. doi: 10.1002/(sici)1097-4644(19980301)68:3<366::aid-jcb7>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 98.Youngren JF, et al. Skeletal muscle content of membrane glycoprotein pc-1 in obesity. relationship to muscle glucose transport. Diabetes. 1996;10:1324–1328. doi: 10.2337/diab.45.10.1324. [DOI] [PubMed] [Google Scholar]
- 99.Reynet C, Kahn CR. Rad: a member of the ras family overexpressed in muscle of type II diabetic humans. Science. 1993;262:1441–1444. doi: 10.1126/science.8248782. [DOI] [PubMed] [Google Scholar]
- 100.Doria A, et al. Trinucleotide repeats at the rad locus: allele distributions in NIDDM and mapping to a 3-cM region on chromosome 16q. Diabetes. 1995;44:243–247. doi: 10.2337/diab.44.2.243. [DOI] [PubMed] [Google Scholar]
- 101.Moyers JS, Bilan PJ, Reynet C, Kahn CR. Overexpression of Rad inhibits glucose uptake in cultured muscle and fat cells. J Biol Chem. 1996;271:23111–23116. doi: 10.1074/jbc.271.38.23111. [DOI] [PubMed] [Google Scholar]
- 102.Laville M, et al. Acute regulation by insulin of phosphatidylinositol-3-kinase, Rad, Glut4, and lipoprotein lipase mRNA levels in human muscle. J Clin Invest. 1996;98:43–49. doi: 10.1172/JCI118775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Caro JF, et al. Insulin receptor kinase in human skeletal muscle from obese subjects with and without non-insulin-dependent diabetes. J Clin Invest. 1987;79:1330–1337. doi: 10.1172/JCI112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Olefsky JM. Decreased insulin binding to adipocytes and circulating monocytes from obese subjects. J Clin Invest. 1976;57:1165–1172. doi: 10.1172/JCI108384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Caro JF, et al. Studies on the mechanism of insulin resistance in the liver from humans with noninsulin-dependent diabetes. J Clin Invest. 1986;78:249–258. doi: 10.1172/JCI112558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Freidenberg GR, Reichart DR, Olefsky JM, Henry RR. Reversibility of defective adipocyte insulin receptor kinase activity in non-insulin-dependent diabetes mellitus. Effect of weight loss. J Clin Invest. 1988;82:1398–1406. doi: 10.1172/JCI113744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hurrell DG, Pedersen O, Kahn CR. Alterations in the hepatic insulin receptor kinase in genetic and acquired obesity in rats. Endocrinology. 1989;125:2454–2462. doi: 10.1210/endo-125-5-2454. [DOI] [PubMed] [Google Scholar]
- 108.Cremel G, et al. Lipid modulation of insulin receptor tyrosine kinase activity in cultured cells, animals, and reconstituted systems. Ann NY Acad Sci. 1993;683:164–171. doi: 10.1111/j.1749-6632.1993.tb35702.x. [DOI] [PubMed] [Google Scholar]
- 109.Goodyear LJ, et al. Insulin receptor phosphorylation, insulin receptor substrate-1 phosphorylation, and phosphatidylinositol 3-kinase activity are decreased in intact skeletal muscle strips from obese subjects. J Clin Invest. 1995;95:2195–2204. doi: 10.1172/JCI117909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rondinone CM, et al. Insulin receptor substrate (IRS) 1 is reduced and IRS-2 is the main docking protein for phosphatidylinositol 3-kinase in adipocytes from subjects with non-insulin-dependent diabetes mellitus. Proc Natl Acad Sci USA. 1997;94:4171–4175. doi: 10.1073/pnas.94.8.4171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bjornholm M, Kawano Y, Lehtihet M, Zierath JR. Insulin receptor substrate-1 phosphorylation and phosphatidylinositol 3-kinase activity in skeletal muscle from NIDDM subjects after in vivo insulin stimulation. Diabetes. 1997;46:524–527. doi: 10.2337/diab.46.3.524. [DOI] [PubMed] [Google Scholar]
- 112.Zierath JR, Krook A, Wallberg-Henriksson H. Insulin action in skeletal muscle from patients with NIDDM. Mol Cell Biochem. 1998;182:153–160. [PubMed] [Google Scholar]
- 113.Friedman JE, et al. Reduced insulin receptor signaling in the obese spontaneously hypertensive Koletsky rat. Am J Physiol. 1997;273:E1014–E1023. doi: 10.1152/ajpendo.1997.273.5.E1014. [DOI] [PubMed] [Google Scholar]
- 114.Anai M, et al. Altered expression levels and impaired steps in the pathway to phosphatidylinositol 3-kinase activation via insulin receptor substrates 1 and 2 in Zucker fatty rats. Diabetes. 1998;47:13–23. doi: 10.2337/diab.47.1.13. [DOI] [PubMed] [Google Scholar]
- 115.Kerouz NJ, Horsch D, Pons S, Kahn CR. Differential regulation of insulin receptor substrates-1 and -2 (IRS-1 and IRS-2) and phosphatidylinositol 3-kinase isoforms in liver and muscle of the obese diabetic (ob/ob) mouse. J Clin Invest. 1997;100:3164–3172. doi: 10.1172/JCI119872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hayakawa T, Shiraki T, Morimoto T, Shii K, Ikeda H. Pioglitazone improves insulin signaling defects in skeletal muscle from Wistar fatty (fa/fa) rats. Biochem Biophys Res Commun. 1996;223:439–444. doi: 10.1006/bbrc.1996.0912. [DOI] [PubMed] [Google Scholar]
- 117.Folli F, Saad MJA, Becker JM, Kahn CR. Regulation of phosphatidylinositol 3-kinase activity in liver and muscle of animal models of insulin-resistant and insulin-deficient diabetes mellitus. J Clin Invest. 1993;92:1787–1794. doi: 10.1172/JCI116768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Heydrick SJ, Gautier N, Olichon-Berthe C, Van Obberghen E, Le Marchand-Brustel Y. Early alteration of insulin stimulation of PI 3-kinase in muscle and adipocyte from gold thioglucose obese mice. Am J Physiol. 1995;268:E604–E612. doi: 10.1152/ajpendo.1995.268.4.E604. [DOI] [PubMed] [Google Scholar]
- 119.Hjollund E, Pedersen O, Richelsen B, Beck-Nielsen H, Sorensen NS. Glucose transport and metabolism in adipocytes from newly diagnosed untreated insulin-dependent diabetics. Severely impaired basal and postinsulin binding activities. J Clin Invest. 1985;76:2091–2096. doi: 10.1172/JCI112213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pedersen O, Hjollund E. Insulin receptor binding to fat and blood cells and insulin action in fat cells from insulin-dependent diabetics. Diabetes. 1982;31:706–715. doi: 10.2337/diab.31.8.706. [DOI] [PubMed] [Google Scholar]
- 121.Gerich JE. Lilly lecture 1988. Glucose counterregulation and its impact on diabetes mellitus. Diabetes. 1988;37:1608–1617. doi: 10.2337/diab.37.12.1608. [DOI] [PubMed] [Google Scholar]
- 122.Reaven GM, Lithell H, Landsberg L. Hypertension and associated metabolic abnormalities — the role of insulin resistance and the sympathoadrenal system. N Engl J Med. 1996;334:374–381. doi: 10.1056/NEJM199602083340607. [DOI] [PubMed] [Google Scholar]
- 123.Ohsaka Y, Tokumitsu Y, Nomura Y. Suppression of insulin-stimulated phosphatidylinositol 3-kinase activity by the β3-adrenoceptor agonist CL316243 in rat adipocytes. Growth Regul. 1997;402:246–250. doi: 10.1016/s0014-5793(97)00007-0. [DOI] [PubMed] [Google Scholar]
- 124.Green A, Carroll RM, Dobias SB. Desensitization of β-adrenergic receptors in adipocytes causes increased insulin sensitivity of glucose transport. Am J Physiol. 1996;271:E271–E276. doi: 10.1152/ajpendo.1996.271.2.E271. [DOI] [PubMed] [Google Scholar]
- 125.Widen E, et al. Association of a polymorphism in the β3-adrenergic-receptor gene with features of the insulin resistance syndrome in Finns. N Engl J Med. 1995;333:348–351. doi: 10.1056/NEJM199508103330604. [DOI] [PubMed] [Google Scholar]
- 126.Umekawa T, et al. Trp64Arg mutation of β3-adrenoceptor gene deteriorates lipolysis induced by β3-adrenoceptor agonist in human omental adipocytes. Diabetes. 1999;48:117–120. doi: 10.2337/diabetes.48.1.117. [DOI] [PubMed] [Google Scholar]
- 127.Hotamisligil GS, Spiegelman BM. Tumor necrosis factor α: a key component of the obesity-diabetes link. Diabetes. 1994;43:1271–1278. doi: 10.2337/diab.43.11.1271. [DOI] [PubMed] [Google Scholar]
- 128.Peraldi P, Spiegelman B. TNF-α and insulin resistance: summary and future prospects. Mol Cell Biochem. 1998;182:169–175. [PubMed] [Google Scholar]
- 129.Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumor necrosis factor-α in human obesity and insulin resistance. J Clin Invest. 1995;95:2409–2415. doi: 10.1172/JCI117936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-α: direct role in obesity-linked insulin resistance. Science. 1993;259:87–91. doi: 10.1126/science.7678183. [DOI] [PubMed] [Google Scholar]
- 131.Kanety H, Feinstein R, Papa MZ, Hemi R, Karasik A. Tumor necrosis factor α-induced phosphorylation of insulin receptor substrate-1 (IRS-1). Possible mechanism for suppression of insulin-stimulated tyrosine phosphorylation of IRS-1. J Biol Chem. 1995;270:23780–23784. doi: 10.1074/jbc.270.40.23780. [DOI] [PubMed] [Google Scholar]
- 132.Uysal KT, Wiesbrock SM, Hotamisligil GS. Functional analysis of tumor necrosis factor (TNF) receptors in TNF-alpha-mediated insulin resistance in genetic obesity. Endocrinology. 1998;139:4832–4838. doi: 10.1210/endo.139.12.6337. [DOI] [PubMed] [Google Scholar]
- 133.Zhang Y, et al. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–432. doi: 10.1038/372425a0. [DOI] [PubMed] [Google Scholar]
- 134.Tartaglia LA. The leptin receptor. J Biol Chem. 1997;272:6093–6096. doi: 10.1074/jbc.272.10.6093. [DOI] [PubMed] [Google Scholar]
- 135.Sivitz WI, Walsh SA, Morgan DA, Thomas MJ, Haynes WG. Effects of leptin on insulin sensitivity in normal rats. Endocrinology. 1997;138:3395–3401. doi: 10.1210/endo.138.8.5327. [DOI] [PubMed] [Google Scholar]
- 136.Kamohara S, Burcelln R, Halaas JL, Friedman JM, Charron MJ. Acute stimulation of glucose metabolism in mice by leptin treatment. Nature. 1997;389:374–377. doi: 10.1038/38717. [DOI] [PubMed] [Google Scholar]
- 137.Shi ZQ, Nelson A, Whitcomb L, Wang J, Cohen AM. Intracerebroventricular administration of leptin markedly enhances insulin sensitivity and systemic glucose utilization in conscious rats. Metabolism. 1998;47:1274–1280. doi: 10.1016/s0026-0495(98)90336-5. [DOI] [PubMed] [Google Scholar]
- 138.Poitout V, Rouault C, Guerre-Millo M, Reach G. Does leptin regulate insulin secretion? Diabetes Metab. 1998;24:321–326. [PubMed] [Google Scholar]
- 139.Rossetti L. Glucose toxicity: the implications of hyperglycemia in the pathophysiology of diabetes mellitus. Clin Invest Med. 1995;18:255–260. [PubMed] [Google Scholar]
- 140.Vuorinen-Markkola H, Koivisto VA, Yki-Jarvinen H. Mechanisms of hyperglycemia-induced insulin resistance in whole body and skeletal muscle of type I diabetic patients. Diabetes. 1992;41:571–580. doi: 10.2337/diab.41.5.571. [DOI] [PubMed] [Google Scholar]
- 141.Yki-Jarvinen H, Helve E, Koivisto VA. Hyperglycemia decreases glucose uptake in type I diabetes. Diabetes. 1987;36:892–896. doi: 10.2337/diab.36.8.892. [DOI] [PubMed] [Google Scholar]
- 142.Rossetti L, Smith D, Shulman GI, Papachristou D, DeFronzo RA. Correction of hyperglycemia with phlorizin normalizes tissue sensitivity to insulin in diabetic rats. J Clin Invest. 1987;79:1510–1515. doi: 10.1172/JCI112981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.McClain DA, Crook ED. Hexosamines and insulin resistance. Diabetes. 1996;45:1003–1009. doi: 10.2337/diab.45.8.1003. [DOI] [PubMed] [Google Scholar]
- 144.Rossetti L, Hawkins M, Chen W, Gindi J, Barzilai N. In vivo glucosamine infusion induces insulin resistance in normoglycemic but not in hyperglycemic conscious rats. J Clin Invest. 1995;96:132–140. doi: 10.1172/JCI118013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Virkamaki A, et al. Activation of the hexosamine pathway by glucosamine in vivo induces insulin resistance in multiple insulin sensitive tissues. Endocrinology. 1997;138:2501–2507. doi: 10.1210/endo.138.6.5172. [DOI] [PubMed] [Google Scholar]
- 146.Hawkins M, Angelov I, Liu R, Barzilai N, Rossetti L. The tissue concentration of UDP-N-acetylglucosamine modulates the stimulatory effect of insulin on skeletal muscle glucose uptake. J Biol Chem. 1997;272:4889–4895. doi: 10.1074/jbc.272.8.4889. [DOI] [PubMed] [Google Scholar]
- 147.Snow DM, Hart GW. Nuclear and cytoplasmic glycosylation. Int Rev Cytol. 1998;181:43–74. doi: 10.1016/s0074-7696(08)60416-7. [DOI] [PubMed] [Google Scholar]
- 148.Wang J, Liu R, Hawkins M, Barzilai N, Rossetti L. A nutrient-sensing pathway regulates leptin gene expression in muscle and fat. Nature. 1998;393:684–688. doi: 10.1038/31474. [DOI] [PubMed] [Google Scholar]
- 149.Hebert LF, Jr, et al. Overexpression of glutamine: fructose-6-phosphate amidotransferase in transgenic mice leads to insulin resistance. J Clin Invest. 1996;98:930–936. doi: 10.1172/JCI118876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Marshall S, Bacote V, Traxinger RR. Discovery of a metabolic pathway mediating glucose-induced desensitization of the glucose transport system. Role of hexosamine biosynthesis in the induction of insulin resistance. J Biol Chem. 1991;266:4706–4712. [PubMed] [Google Scholar]
- 151.Kim YB, et al. Glucosamine infusion in rats rapidly impairs insulin stimulation of phosphoinositide 3-kinase but does not alter activation of Akt/protein kinase B in skeletal muscle. Diabetes. 1999;48:310–320. doi: 10.2337/diabetes.48.2.310. [DOI] [PubMed] [Google Scholar]
- 152.Newton AC. Protein kinase C: structure, function, and regulation. J Biol Chem. 1995;270:28495–28498. doi: 10.1074/jbc.270.48.28495. [DOI] [PubMed] [Google Scholar]
- 153.Chen KS, Heydrick SJ, Brown ML, Friel JC, Ruderman NB. Insulin increases a biochemically distinct pool of diacylglycerol in the rat soleus muscle. Am J Physiol. 1994;266:E479–E485. doi: 10.1152/ajpendo.1994.266.3.E479. [DOI] [PubMed] [Google Scholar]
- 154.Haring HU, et al. Modulation of insulin receptor signaling. Potential mechanisms of a cross talk between bradykinin and the insulin receptor [review] Diabetes. 1996;45(Suppl. 1):S115–S119. doi: 10.2337/diab.45.1.s115. [DOI] [PubMed] [Google Scholar]
- 155.Kellerer M, Haring HU. Pathogenesis of human resistance: modulation of the insulin signal at receptor level [review] Diabetes Res Clin Pract. 1995;28(Suppl.):S173–S177. doi: 10.1016/0168-8227(95)01070-t. [DOI] [PubMed] [Google Scholar]
- 156.Kroder G, et al. Tumor necrosis factor-— and hyperglycemia-induced insulin resistance. J Clin Invest. 1996;97:1471–1477. doi: 10.1172/JCI118569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Murphy M, McGinty A, Godson C. Protein kinases C: potential targets for intervention in diabetic nephropathy. Curr Opin Nephrol Hypertens. 1998;7:563–570. doi: 10.1097/00041552-199809000-00013. [DOI] [PubMed] [Google Scholar]
- 158.Urano T, Emkey R, Feig LA. Ral-GTPases mediate a distinct downstream signaling pathway from Ras that facilitates cellular transformation. EMBO J. 1996;15:810–816. [PMC free article] [PubMed] [Google Scholar]
- 159.Ahmad F, Azevedo J, Cortright R, Dohm GL, Goldstein BJ. Alterations in skeletal muscle protein-tyrosine phosphatase activity and expression in insulin-resistant human obesity and diabetes. J Clin Invest. 1997;100:449–458. doi: 10.1172/JCI119552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Goldstein BJ, Ahmad F, Ding W, Li PM, Zhang WR. Regulation of the insulin signalling pathway by cellular protein-tyrosine phosphatases. Mol Cell Biochem. 1998;182:91–99. [PubMed] [Google Scholar]
- 161.Accili D, et al. Early neonatal death in mice homozygous for a null allele of the insulin receptor gene. Nat Genet. 1996;12:106–109. doi: 10.1038/ng0196-106. [DOI] [PubMed] [Google Scholar]
- 162.Joshi RL, et al. Targeted disruption of the insulin receptor gene in the mouse results in neonatal lethality. EMBO J. 1996;15:1542–1547. [PMC free article] [PubMed] [Google Scholar]
- 163.Araki E, et al. Alternative pathway of insulin signalling in mice with targeted disruption of the IRS-1 gene. Nature. 1994;372:186–190. doi: 10.1038/372186a0. [DOI] [PubMed] [Google Scholar]
- 164.Tamemoto H, et al. Insulin resistance and growth retardation in mice lacking insulin receptor substrate-1. Nature. 1994;372:182–186. doi: 10.1038/372182a0. [DOI] [PubMed] [Google Scholar]
- 165.Withers DJ, et al. Disruption of IRS-2 causes type 2 diabetes in mice. Nature. 1998;391:900–903. doi: 10.1038/36116. [DOI] [PubMed] [Google Scholar]
- 166.Bruning JC, et al. Development of a novel polygenic model of NIDDM in mice heterozygous for IR and IRS-1 null alleles. Cell. 1997;88:561–572. doi: 10.1016/s0092-8674(00)81896-6. [DOI] [PubMed] [Google Scholar]
- 167.Kulkarni RN, et al. Tissue-specific knockout of the insulin receptor in pancreatic β cells creates an insulin secretory defect similar to that in Type 2 diabetes. Cell. 1999;96:329–339. doi: 10.1016/s0092-8674(00)80546-2. [DOI] [PubMed] [Google Scholar]
- 168.Ferrannini E. Insulin resistance versus insulin deficiency in non-insulin-dependent diabetes mellitus: problems and prospects. Endocr Rev. 1998;19:477–490. doi: 10.1210/edrv.19.4.0336. [DOI] [PubMed] [Google Scholar]